Abstract
Disparities in nutrition, such as poor diet quality and inadequate nutrient intake, arise from multiple factors and are related to adverse health outcomes such as obesity, diabetes, cardiovascular disease, and some cancers. The aim of the current perspective is to present a nutrition-centric socioecological framework that delineates determinants and factors that contribute to diet and nutrition-related disparities among disadvantaged populations. The Nutrition Health Disparities Framework (NHDF) describes the domains (biological, behavioral, physical/built environment, sociocultural environment, and healthcare system) that influence nutrition-related health disparities through the lens of each level of influence (that is, individual, interpersonal, community, and societal). On the basis of the scientific literature, the authors engaged in consensus decision making in selecting nutrition-related determinants of health within each domain and socioecological level when creating the NHDF. The framework identifies how neighborhood food availability and access (individual/built environment) intersect with cultural norms and practices (interpersonal/sociocultural environment) to influence dietary behaviors, exposures, and risk of diet-related diseases. In addition, the NHDF shows how factors such as genetic predisposition (individual/biology), family dietary practices (interpersonal/behavioral), and food marketing policies (societal) may impact the consumption of unhealthy foods and beverages and increase chronic disease risk. Family and peer norms (interpersonal/behavior) related to breastfeeding and early childhood nutrition interact with resource-poor environments such as lack of access to preventive healthcare settings (societal/healthcare system) and low usage of federal nutrition programs (societal/behavioral), which may increase risk of poor nutrition during childhood and food insecurity. The NHDF describes the synergistic interrelationships among factors at different levels of the socioecological model that influence nutrition-related outcomes and exacerbate health disparities. The framework is a useful resource for nutrition researchers, practitioners, food industry leaders, and policymakers interested in improving diet-related health outcomes and promoting health equity in diverse populations.
Keywords: Nutrition Health Disparities Framework, social determinants of health, socioecological model, diet quality, health equity
Statement of Significance.
There is a critical need to address nutrition health disparities and reduce chronic disease risk. This perspective proposes the Nutrition Health Disparities Framework to examine synergistic interrelationships across levels of influence that impact nutrition health disparities. The framework can inform the development of multilevel nutrition interventions to improve health equity in diverse populations.
Introduction
Disparities in dietary intake and diet-related diseases such as obesity, cardiovascular disease, hypertension, diabetes, and some types of cancer are prevalent in the United States and globally [1]. These nutrition and diet-related health disparities are driven by multiple factors and are embedded in social determinants of health (SDOH) and structural factors. These include poverty, lack of access to quality education and employment, poor quality housing, unfavorable work and neighborhood conditions, transportation issues, environmental racism, neighborhood violence, and the clustering of disadvantaged groups [2]. These same social factors underscore the disparities observed during the COVID-19 pandemic [3] compounded by the fact that existing nutrition and diet-related diseases (for example, obesity) also exacerbate morbidity and mortality from the virus [4]. Factors at the individual level (for example, socioeconomic status, employment, and coping skills) and cultural practices and experiences (for example, family or community culinary traditions) can influence eating habits, and dietary preferences and are themselves influenced by social and structural factors that contribute to diet-related health disparities. Therefore, addressing the multiple intersecting factors that influence dietary patterns and their contribution to these diet-related health disparities is essential for developing effective interventions to reduce health disparities and promote health equity.
In addition, neighborhood racial segregation is associated with unhealthy food environments (for example, food deserts and swamps), which contribute to nutrition health disparities. Populations from racial/ethnic minority groups are more likely to be affected by neighborhood-level factors that impede access to healthy foods and have fewer constraints regarding marketing and the density of unhealthy foods and beverages, including fast food and alcohol. Many disadvantaged populations in under-resourced neighborhoods also have limited access to supermarkets, impacting diet quality [5]. Characteristics of an individual’s food environment, such as lack of grocery stores and the presence of fast-food restaurants, are associated with an increased risk of several chronic diseases such as obesity, hypertension, cardiovascular disease, diabetes [6], and some cancers [7]. Moreover, socioeconomic factors, such as the higher cost of purchasing healthy foods, contribute to disparities in diet quality [8].
Related to the psychosocial perspective, research also suggests that experiencing discrimination can negatively impact diet quality and nutrient intake [9,10]. One study found that prior exposure to discrimination was associated with a worse diet and lower medication adherence among hypertensive Black/African Americans [11]. Stress is a potential pathway for the relationship between neighborhood environmental factors, discrimination, violent crime, and health outcomes such as glycemic control [12]. Understanding the SDOH and structural factors that influence diet quality at every level and their interaction is essential to improving health and reducing diet-related health disparities. Moreover, the significant drivers of nutrition health disparities (for example, socioeconomic status, race/ethnicity, discrimination, disabilities, health literacy, and cultural characteristics) are also associated with lower access to healthcare, which reflects current and historical systemic racism and bias [13,14]. The association between diet quality and healthcare was illustrated by a recent study that found that food-insecure adults who consumed low-quality diets or had increased diet-related comorbidities were less likely to use outpatient healthcare and had poorer physical and mental health [15]. Those who experience food insecurity, inconsistent access to enough food, or inadequate food quality, tend to have greater healthcare utilization and significantly higher annual healthcare expenditures than individuals who are not food insecure [16]. Factors influencing access to outpatient healthcare are intertwined with racism, discrimination, and socioeconomic factors [15]. Identifying the drivers of diet-related diseases and their interaction with health outcomes and the healthcare system is essential for promoting health equity.
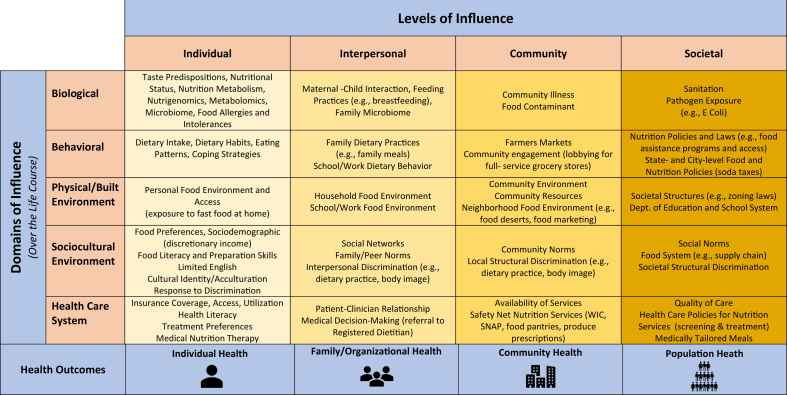
This article reviews the state of the science supporting the NIH Nutrition Health Disparities Framework (NHDF) (Figure 1). It was inspired by the National Institute on Minority Health and Health Disparities’ Minority Health and Health Disparities Research Framework designed to conceptualize factors relevant to understanding and reducing health disparities. Specifically, the framework is a multilevel, multidomain model that depicts various health determinants pertinent to understanding and addressing minority health and health disparities and promoting health equity [17]. The NHDF builds upon the Minority Health and Health Disparities Research Framework to understand the synergistic interrelationships across the domains that influence nutrition-related health disparities (biological, behavioral, physical/built environment, sociocultural environment, and healthcare system) through the lens of each level of influence (individual, interpersonal, community, and societal). In this article, we present this new framework and offer examples from the research literature to illustrate how the NHDF can inform the understanding of multilevel determinants of nutrition disparities and the development and testing of multilevel interventions to address those disparities. The authors engaged in consensus decision making in selecting nutrition-related determinants of health within each domain and SE level. The examples provided are based on scientific literature to illustrate the interaction between the levels of influence and various domains and are not intended to be a comprehensive review of the literature. We particularly highlight research examples representative of the NIH’s health disparities populations (racial and ethnic minorities, populations with lower socioeconomic status, rural communities, sexual and gender minorities, and those with disabilities), as well as various stages of the life course. We note that there is some overlap of determinants across domains, further highlighting their interconnectedness and the importance of taking a more holistic approach to understanding and addressing nutrition disparities.
FIGURE 1.
The Nutrition Health Disparities Research Framework highlights examples of multiple factors and their intersection that are relevant to understanding and addressing nutrition-related health disparities. The National Institutes of Health's definition of health disparities populations includes race and ethnic minorty groups, people with lower socioeconomic status, underserved rural communities, sexual and gender minority groups, and people with disabilities. In addition, other fundamental characteristics such as sex/gender and geographic region are included in the framework.
Overall, this framework can serve as an essential resource for nutrition researchers, practitioners, food industry leaders, and policymakers to inform the development of multilevel nutrition interventions to improve diet quality, diet-related health outcomes, and health equity in diverse populations.
Biological Domain
At the individual level, there are many biological factors, including the gut microbiota and genetic predisposition, that are examples of contributors to nutrition-related disparities. A review of the scientific literature noted variability in microbial composition among different populations, with those consuming Western diets having more Bacteroides than Prevotella bacteria, the latter of which is protective against disease [18]. This review suggests that individual dietary factors that affect biology, such as microbial composition, are also influenced by community-level factors and could lead to nutrition-related disparities. Race and ethnic differences in vitamin D metabolism and their associations with genetic ancestry have been reported in many studies [19,20]. A review by Hsu et al. [21] identified differences between White and Black/African American participants regarding concentrations of 25-hydroxyvitamin D, fibroblast growth factor-23, parathyroid hormone, and 1,25-dihydroxy vitamin D. The authors concluded that markers of vitamin D metabolism vary significantly by race and ethnicity, may serve to maintain bone and mineral homeostasis across ranges of 25-hydroxyvitamin D production, and may be attributable to genetic ancestry.
Biological and interpersonal factors can impact diet-related disparities and chronic disease risk. At the interpersonal level, researchers have shown that individual gut and oral microbiomes are transmitted within households and between spouses, with notable sex differences. For example, research shows that females harbor strains more closely related to their families and social contacts than males [22]. A small study among a Mexican American agricultural population found a high abundance of Streptococcus spp. in breast milk and the child’s oral microbiome at 5 y of age [23]. The mother’s prepregnancy BMI (kg/m2) correlated with the abundance of Streptococcus spp. and microbial diversity in breast milk [23]. In addition, a systematic review revealed that maternal diet during pregnancy and lactation might reduce risk of immune-mediated diseases in the child [24]. Specifically, the study found that supplements such as probiotics or fish oil may prevent allergies or autoimmune diseases. However, for most low-income and vulnerable populations, the cost of dietary supplements may be prohibitive, thus increasing risk of disparities in chronic diseases and conditions. These studies suggest interpersonal interactions, such as shared susceptibilities between mother and child, may influence children’s early-life microbial exposures, nutrition, and health-related outcomes. Also, it highlights the interplay between multiple levels of influence, including maternal BMI (individual level), maternal diet during pregnancy and lactation (interpersonal level), overlaid by structural barriers that impede access (community level), and affordability of supplements (societal level) and their effects on child health.
At the community level, differences in susceptibility to foodborne illness and food safety risks have been reported in minority and low-socioeconomic populations in the United States and globally [25]. A higher incidence of listeriosis was reported in Black/African Americans and Asians than in Whites [26]. Similarly, evidence of socioeconomic disparities in nitrate levels in the United States’ drinking water was reported in Hispanic/Latino residents and low-income communities [27]. Differences in environmental exposures, including pesticides and endocrine-disrupting chemicals, were associated with various diseases (for example, diabetes and cancer) [28,29]. Specifically, one study assessed carcinogenic contaminants in community water systems in both California and Texas and observed a greater cancer risk of communities with a higher portion of Hispanics/Latinos and Black/African Americans [30].
At the societal level, scientific evidence suggests that failure to develop, implement, and enforce policies can negatively impact the environmental health of racial/ethnic populations and those living in low-income, underserved communities. For example, failed policies at the federal and local governments resulted in increased exposure to environmental lead in Black/African Americans and Puerto Rican children residing in redlined impoverished neighborhoods in New York City [31]. One study documented the complex policy and regulatory challenges with tribal, federal, state, and county jurisdiction in restoring deteriorating municipal water and wastewater infrastructure in American Indian communities [32]. Opportunities exist to strengthen and equitably enforce policies that impact communities that have been economically and socially marginalized to reduce diet-related disparities and chronic diseases. A prime example is the Flint water crisis that led to contamination in predominantly Black/African American communities in Flint, Michigan [33]. This example highlights the intersecting levels of influence that exacerbated the ill-effects in these severely impacted predominately Black/African American communities. Levels of influence include lead contamination in these geographically defined communities (community level), failure of local government to respond (societal level), and increased intake of sugar-sweetened beverages because of contaminated water (individual level and behavioral domain) [34], which negatively impact diet quality among a population that already experiences challenges to accessing healthcare (healthcare system), and high rates of morbidity and mortality from chronic diseases.
Behavioral Domain
Dietary behaviors and poor eating patterns contributing to health disparities result from a complex interplay individual, interpersonal, community, and societal factors. Although behaviors are often considered an individual choice, diet is shaped by a host of additional reinforcing factors, ranging from peer and family relationships to community resources and societal norms, practices, and policies, including those impacting the cost of food, availability and access to food retailers, and media and advertising exposure. Food choice is quite complex and embedded in a broader context of activities in one’s daily life, which is ultimately shaped by the food and social environments [35].
Behavioral factors at the individual level, such as dietary intake, eating patterns, and coping strategies (e.g., excessive alcohol consumption), contribute to and perpetuate diet-related health disparities [36]. Poor diet-related behaviors that contribute to chronic disease include low intake of fruits, vegetables, whole grains, and fatty fish, paralleled with increased intake of processed foods high in saturated fat, sodium, and added sugars, and overconsumption of sugar-sweetened beverages [1]. Because of the economic drivers of food prices, these processed foods are often more widely available and cheaper than healthier food options. An individual’s socioeconomic status is, therefore, a critical influencer of their dietary behavior and disparities in dietary intake. Research suggests that adolescents from low- and middle-income households consume more snacks with added sugar when compared with those from high-income households, and those living in low-income households were less likely to consume milk and fruit as snacks [37]. For some older adults, food insecurity may be associated with lower-income and poor diet quality [38]. Research on adherence to dietary patterns that promote health (e.g., Dietary Approaches to Stop Hypertension diet) shows that Black/African American adults have lower dietary quality scores than other racial and ethnic groups [39,40]. Exposure to stress and dietary coping strategies may be another driver of these disparities, with research suggesting that diverse racial and ethnic groups are susceptible to stress-induced unhealthy eating patterns [41]. Similar trends have been shown in disabled adult females [42] and children with intellectual disabilities showing lower intakes of fruit and vegetables than children without disabilities [43]. Time scarcity at the individual level is especially important for populations of lower socioeconomic status and plays a critical role in food consumption patterns, such as decreases in food preparation at home and increases in fast food consumption [44].
Interpersonal relationships, including peers and family members, can also shape dietary behaviors. During childhood, dietary habits and preferences are shaped by the foods served in the home, family meals, and in the school food environment [45,46]. Studies suggest that parents’ diet and parenting style play a significant role in shaping children’s dietary quality and intake [47], with more authoritarian parenting practices related to higher BMI percentiles among Black/African American adolescents [48]. Meanwhile, findings among children with intellectual disabilities demonstrated that children with parents using restrictive practices were less likely to develop unhealthy eating behaviors compared with parents who less frequently used these parenting practices [49]. Household composition (for example, intergenerational households) and household members’ dietary needs and preferences can also shape dietary behaviors.
Communities are often first conceptualized geographically. However, today’s increasingly interconnected context offers many ways to define communities, and shared interests, concerns, or priorities may more broadly characterize their collective behaviors and scope of influence on diet-related health outcomes. One mode of community influence is participating as research partners to develop or evaluate interventions to promote healthy diet and nutrition. Studies suggest that effective approaches for shaping the food environment may include tailored, culturally adaptive, actionable interventions that account for the diverse community characteristics, perspectives, and interests (for example, residents, consumers, producers, and retailers). Evidence from the research community can inform recommendations supporting program or policy changes to address diet-related diseases. Communities motivated by collective interests may then form coalitions, implement new programs or interventions [50], or advocate for societal-level policies [51,52] to address healthy food access (for example, food-related inequities accentuated during the COVID-19 pandemic) or dietary equity.
In response to community action advocacy, universal or targeted policies at the societal level—such as those on taxes [53], subsidies, packaging, financial incentives, behavioral economic strategies [54], or availability and promotion of programs [53,55,56]—can impact dietary behavior [57]. In some instances, policies and programs aimed at addressing diet-related health disparities—such as Supplemental Nutrition Assistance Program-Education (SNAP-Ed)—may achieve local success by improving food security across rural or urban communities [56], yet have limited efficacy in supporting nutritious purchases across all racial or ethnic participants [58]. Although impactful, a policy approach to promoting healthy dietary behaviors may require a long-term, integrated systems view. Regulatory and legislative actions have varied scopes and success, acting through the federal, tribal, state [59], or local government [60]. For example, evidence suggests that the most effective interventions in American Indians' nutrition-related outcomes combine multilevel policies that govern the food supply with educational strategies [55]. Furthermore, the influence of policy on behaviors is dynamic and, at times, multidirectional [53]. Although policies can influence diet-related behaviors, importantly, policies may also motivate behavior changes in collective and influencial players such as retailers, producers, industries, or businesses. These sectors are also active participants in shaping the food environments in which people live and work, and can advocate for policies reflecting their best interests.
Physical/Built Environment Domain
The built environment—that is, the physical surroundings where we live, learn, work, and play—has an integral role in affecting nutrition-related health disparities at the individual, interpersonal, community, and societal levels. On an individual level, the built environment directly impacts what foods individuals have access to and should be considered in rural, urban, and suburban interventions and community planning practices. For example, studies suggest that closer and more frequent proximity to fast-food restaurants in urban [5] and rural settings [61], which are often predominant in lower socioeconomic status and minority neighborhoods, can increase an individual’s fast-food exposure and consumption [5,62]. Similar patterns are seen for unhealthy alcohol use in disadvantaged neighborhoods and vary by race/ethnicity and rurality [63]. Transportation options can further impact exposures: food deserts and limitations on walking and public transportation, especially for those with disabilities, to convey groceries may limit healthier food accessibility [61,64,65], although easy access to transportation and multiple stores within a geographic location can increase exposure to desired, valued foods [66].
Similar built environment factors come into play at the interpersonal level in household, school, and workplace food environments. For example, in predominantly low-socioeconomic status neighborhoods, increasing availability of supermarkets and healthy and affordable food options in the built environment [5], including through the presence of The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC)–certified stores [67], can have a positive impact on parental purchases, exposures within the home for their children, and in reducing childhood racial/ethnic health disparities [68]. In the school setting, limited healthy foods and increased availability of unhealthy beverages, snacks, and meals are associated with fewer servings of produce consumption by adolescents [69]. On college campuses, students may face financial constraints, and the convenience and affordability of on-campus foods, limited transportation to off-campus grocery stores, and alternate options can directly impact food accessibility [64].
At the community level, the built environment includes community resources and the community and neighborhood food environments (for example, food deserts, and food marketing). Studies have found associations between neighborhood food environment and poor health outcomes in populations with the highest obesity rates in the United States—people of low-socioeconomic status, racial/ethnic minorities, rural residents [70], and those with disabilities [71]. However, interventions that aim only to address unidimensional aspects of food access at the community level (for example, opening new grocery stores) have shown inconsistent findings related to improved diet quality [72,73]. To understand this further, researchers have explored how food environments differentially affect social groups by supporting access to healthy, affordable food for some communities [74], including how retail food environment intervention strategies could better align with traditional foods among American Indians [75]. Barriers and facilitators of equitable access to healthy foods are also relevant in the emerging online grocery environment [76].
At the societal level, the built environment is defined and impacted by multiple societal structures, including policies, zoning, and marketing. The racial, ethnic, and economic injustice in the United States food system has been influenced by laws and zoning that led to housing discrimination (for example, redlining) and persistent food inaccessibility issues [77]. The historical practice of redlining has lingering effects on racial segregation, contributing to disparities in access to community resources that promote healthy behaviors. More recent federal and state policies have led to some benefits, but wide disparities for racial/ethnic minority subgroups remain [61,78]. In addition, many studies have shown that marketing can influence food and beverage consumption. Children from minority and socioeconomically disadvantaged backgrounds are disproportionately exposed to unhealthy food advertising through media and marketing that is targeted to their communities, and researchers have advocated for regulations to restrict harmful food advertising to children to improve children’s diets and reduce inequities in dietary intake [79,80]. For example, one study among Hispanics/Latinos found that they faced disadvantages regarding healthy lifestyle messaging and health-promoting food environments [81]. Finally, disparities in young children’s social and physical childcare environments persist, with gaps in resource allocation and policies for health equity [82]. An example highlighting the interplay between multiple levels of influence could include families living in geographic areas with limited access to affordable and healthy food options, such as food deserts. In this environment, proximity to fast-food restaurants can increase the intake of these foods (individual level). The lack of available grocery stores or supermarkets can negatively impact parental purchases of healthy food for the family (interpersonal), and a lack of green space and sidewalks can affect levels of physical activity (community-level). Structural interventions to address food deserts should target barriers (for example, zoning laws) to eliminate housing discrimination (societal level) leading to improvements in food access, diet quality, and overall health.
Sociocultural Domain
The sociocultural environment refers to beliefs, attitudes, norms, and values held by individuals, families, social networks, organizations, communities, and societies that create a particular social climate related to food, eating, and nutrition. The social environment, in turn, drives nutrition-related behaviors, practices, policies, and laws across all socioecological levels.
At the individual level, sociodemographic characteristics and cultural factors affect food accessibility, preferences, and behaviors. For example, historical and cultural norms influence home food preparation methods that could contribute to disease (for example, the use of lard instead of vegetable oil). Higher socioeconomic status and educational attainment, which are associated with greater health literacy and holding health-conscious beliefs, are associated with healthier diets as well as adherence to recommended dietary restrictions for individuals with chronic conditions [83,84]. Among immigrant populations in the United States, acculturation is associated with higher consumption of processed foods and fast food, whereas adherence to traditional cultures is associated with greater fruit and vegetable consumption, fiber consumption, and home-cooked meals [[85], [86], [87]]. Interventions to promote adherence to traditional cooking and dietary practices may improve diet quality among immigrants and their families.
At the interpersonal level, the immediate social environment within families and peer groups can predict eating behavior and nutrition. Family norms and social support around fruit and vegetable intake are associated with greater individual intake among low-income adults [88]. Others found that social networks (for example, interactions with family, friends, and neighbors) were associated with higher fruit and vegetable intake and better nutritional status among older adults [89,90]. The experience of discrimination within schools and workplaces is associated with greater food insecurity among females, even after controlling for other relevant sociodemographic factors [91]. Experiencing weight-related teasing, more prevalent among racial/ethnic minorities and those of lower socioeconomic status, is associated with disordered eating and unhealthy weight control behaviors [92]. In addition, interpersonal discrimination is associated with alcohol use/abuse and unhealthy diet and eating behaviors [93]. Simulation modeling suggests that social network norms regarding healthy eating are critical to the success of upstream policy interventions, such as improving school meal quality to reduce racial disparities in obesity [94].
Communities, whether they are residential neighborhoods, cities, counties, or online groups, can also shape nutrition-related outcomes. A sense of community cohesion and connectedness, which may result in increased resource and knowledge sharing, is associated with decreased food insecurity and may mitigate racial/ethnic disparities [95,96]. Community connectedness may contribute to increases in body esteem for sexual and gender minorities, which can help protect against disordered eating [97]. Community norms and social support around fruit and vegetable intake also increase consumption, even after controlling for family and peer norms [88]. Behavioral economic nudges such as product placement of healthy foods and beverages in neighborhood corner stores may influence purchasing behaviors in low-income communities [98].
At the societal level, food production and distribution practices and policies can contribute to nutrition-related disparities. Highly processed foods with low production costs are disproportionately offered to low-socioeconomic status, racial/ethnic minorities, and rural communities, whereas higher-cost fresh and organic foods are less available. Food availability in disadvantaged communities can lead to stereotypes about food preferences and can be used to justify maintaining options limited to low-cost, highly processed foods [99]. Targeted marketing of unhealthy and fast foods that conform to food preference stereotypes in racial/ethnic minorities and lower socioeconomic status populations contributes to poor nutrition and food insecurity [100]. Societal stigma toward using government assistance may contribute to limited uptake of benefits, such as SNAP and WIC, and racially biased monitoring and revocation of these benefits for racial/ethnic minority families can further limit access [95].
Healthcare System Domain
The healthcare system plays a critical role in influencing diet-related disparities associated with poor dietary quality and adverse health outcomes, particularly for disadvantaged populations at high risk of chronic diseases. At the individual level, healthcare-based interventions focused on health literacy and self-efficacy may improve health-related behaviors [101]. However, the success of these programs depends on access to care, knowledge/skills to comprehend messages, and availability of resources at the individual level to address diet-related behaviors while considering socioeconomic status when examining disparities in health-related skills and behaviors [102]. Research opportunities within healthcare settings include comparative effectiveness trials of medical nutrition therapy interventions in various population subgroups, improved identification of barriers to dietary adherence, innovative approaches for behavior modification, patient-centered counseling, and connections to appropriate resources for individuals who report food insecurity [103].
At the interpersonal level, patient–provider interactions, integration of the nutrition care process, effective communication, and patient-centered decision making directly inform healthcare outcomes and behaviors [[104], [105], [106]]. Healthcare providers vary in their awareness of the connections between food insecurity, chronic health conditions, disabilities, health outcomes, communication strategies, and unconscious biases in patient care. Limited clinical awareness of these factors plays significant roles in the appropriate identification and resolution of nutrition-related disparities. Medical nutrition therapy barriers in clinical and community settings include program and staffing costs, reimbursement concerns, sociocultural norms, and organizational structures [104,107,108]. Further research on interventions designed to 1) improve patient–provider communication, 2) identify systemic barriers, 3) improve access to healthcare, 4) identify and implement best practices and tools to screen for food insecurity, 5) enhance training to counter racial and gender-based implicit biases, 6) improve the efficiency of the nutrition referral process to clinicians and federal nutrition assistance programs, and 7) enhance a greater understanding of patient-level factors impacting screening and treatment decisions will be necessary to overcome disparities.
At the community level, healthcare systems can serve as direct links to social services and community groups addressing food insecurity; however, efforts to assure community engagement are critical, including recognition that food insecurity co-occurs with other social needs [[109], [110], [111]]. Best practices for implementing these services are needed, including systematic screening procedures, continuous identification of community assets and resources, staff training, and methods for referring patients to the community and other resources while assuring privacy and dignity. Barriers to resource connections at the community level include inadequate resources and difficulty accessing programs, low health literacy and language accessibility, stigma and discrimination, and fear of immigration policies [112,113]. Future research using sustainable implementation models is needed to establish a strong evidence base on the effectiveness of screening and referrals to community-based services.
At the societal level, increasing access to healthy foods and integration of medical nutrition therapy and food assistance policies and programs have the potential to advance equity in nutrition and access to healthy, affordable foods for all [114,115]. Current challenges include restrictive nutrition assistance eligibility criteria and burdensome enrollment procedures [116]. Systemic changes are needed to expand access to these programs to include vulnerable populations such as individuals with mobility disabilities, populations with limited retail options for healthy foods, low-wage workers and single-parent households with limited time availability, and individuals with transportation limitations. Opportunities exist to develop and implement novel federal and state-level reimbursement and payment models, such as the Medicaid 1115 and 1915 waivers, with flexibility to incentivize screening and referral procedures for food insecurity. Stabilizing financial, technical, and policy support for nutrition assistance programs and incorporating SDOH principles and barriers into medical education curricula will be critical to reaching these goals [116].
Nutrition Disparity Example: Black/African American and Hispanic/Latino Teenagers with Obesity
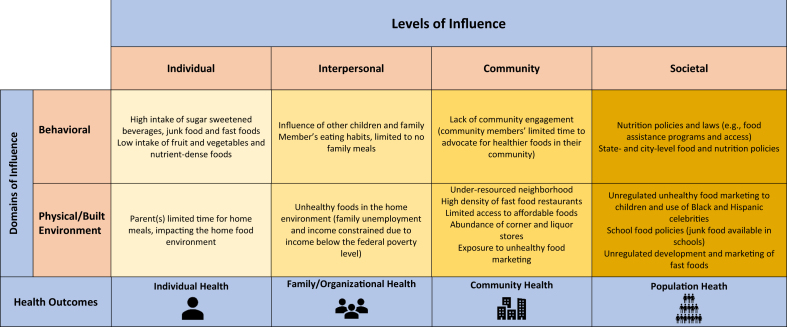
Because childhood obesity is a severe problem in the United States, we highlight an example of the multiple determinants of obesity among Black/African American and Hispanic/Latino teenagers using the NHDF, specifically focusing on the behavioral and physical/built environment domains (Figure 2). This example focuses on an impoverished neighborhood with higher proportions of residents from diverse racial and ethnic groups with overweight or obesity and has reported food insecurity (individual level). Many of the families in this community are underemployed, have an income below the federal poverty level, and face many stressors as they try to balance competing demands to survive. On the basis of December 2023 United States Bureau of Labor Statistics estimates, the unemployment rate is 3.7% in the United States, with higher percentages for Black/African American individuals (5.2%), followed by individuals from Hispanic/Latino groups (5.0%) compared with Whites (3.5%) [117]. Being unemployed or underemployed is a social stressor that has deleterious effects on families’ health and can contribute to food insecurity, worsening nutrition, and increasing obesity risk [118]. Although there are federal policies for food assistance programs (for example, SNAP) to address food insecurity (societal level), lack of and limited access to transportation to the nearest service center, limited time availability, and stigma may be barriers to accessing these nutrition services. Because of the constraints of limited resources and competing job demands, many families are also unable to have meals together. Research has shown that family meals (interpersonal level) are associated with better diet quality (behavioral level) and reduced obesity risk among youth, especially Black/African American teenagers [119,120]. In this case study, many teenagers ate meals without parental engagement (interpersonal level). This negative behavior, as well as issues with emotional eating, weight bias, and stress, can devastate nutrition and health.
FIGURE 2.
The Nutrition Health Disparities Research Framework provides an example of multiple factors within the behavioral and physical/built environment that contribute to childhood obesity among racial and ethnic minorities.
Because of the legacy of historical government redlining and racial neighborhood segregation, the family has low access to affordable, healthy foods (due to the lack of full-service grocery stores), limited resources for physical activity (for example, lack of parks, and sidewalks), and ready access to poor quality food options (for example, alcohol, sugar-sweetened beverages, and fatty meats) (community level). After school, many teenagers frequently visit neighborhood corner stores and fast-food restaurants, subsequently consuming cheap, caloric-dense, and ultra-processed foods and snacks. Moreover, they were also exposed to unhealthy food marketing through media advertisements. On average, research suggests that Black/African American children are exposed to 1.58 more hours of screen time per day compared with their White counterparts [121]. According to a 2019 Rudd Center Study, Black/African American youth are exposed to 75% more fast-food advertisements than their White counterparts [80]. Food and beverage marketing targeting Hispanic/Latino youth reveals significantly more frequent advertising on Spanish network TV, and those that encourage the consumption of low-nutrient and calorie-dense foods and beverages [81]. Black/African American and Hispanic/Latino celebrities are also used to attract and market to young, particularly Black/African American and Hispanic/Latino consumers. Overall, the interactions and synergistic relationships between these described factors can negatively impact nutrition-related health outcomes and widen obesity disparities among youth. Unfortunately, without direct intervention at multiple levels of influence outlined in the NHDF, many Black/African American and Hispanic/Latino teenagers with obesity are at persistent risk of nutrition- and obesity-related chronic diseases such as type 2 diabetes, cardiovascular disease, and cancer throughout their life course. This example describes the complexity associated with the design of interventions that address not only the individual but also the community and societal levels that are broad in scope and could have significant reach in improving diet quality, reducing obesity risk, and improving health equity.
Discussion
We discussed the NHDF framework and provided examples to illustrate how the framework can inform the understanding of the multilevel determinants of nutrition disparities. In this section, we use the framework to highlight key considerations for researchers and practitioners interested in designing interventions to address nutrition health disparities. We discuss and provide examples highlighting the importance of 1) developing multilevel interventions and systems approaches, 2) identifying accurate measures specific to the community, 3) conducting community-engaged research, and 4) having a diverse nutrition workforce to address the challenges of nutrition health disparities.
Importance of multilevel interventions
Addressing the complexities underlying the causes of diet-related health disparities requires a multifaceted, multilevel, and systems approach [122,123]. Historically, community-based dietary interventions have been shown to be ineffective or have demonstrated limited biologically meaningful impact because they have operated within the individual-level and/or interpersonal domains, failing to account for the interacting systems that contribute to diet-related behaviors and disparities [124]. At the same time, dietary interventions that exclusively involve environmental or policy changes may also be ineffective if not accompanied by corresponding changes in diet-related knowledge, attitudes, and behaviors among individuals and families. Taking a multilevel, systems approach includes the incorporation of the domains and levels of influence within the NHDF, such as the biological factors, individual and family behaviors, larger societal forces, sociocultural factors, the built environment, and healthcare access [125].
Below, we highlight exemplary studies that take a multifaceted, multilevel approach. This includes Shape Up Somerville, which had a whole-of-community intervention to address childhood obesity and included engagement with school administrators, parents, school food service providers, before- and after-school programs, healthcare providers, restaurants, and local media [126]. The Baltimore Healthy Stores study is another community-based program that included multiple components in the corner store setting—increased stock of more nutritious foods, point-of-purchase promotions, signage for healthy choices, and interactive nutrition education sessions with consumers [127]. Both are excellent examples of intervention research that targets multiple domains of the NHDF.
Aiming to understand and address these interwoven root causes of diet- and nutrition-related disparities, the NIH has increasingly invested in this area of research through specific initiatives. NIH’s recent and current Notices of Funding Opportunities include the Time-Sensitive Obesity Policy and Program Evaluation, which encourages research to examine the potential impact of new policies or programs likely to influence obesity-related behaviors [128]. Also, relevant Notices of Special Interest include “Stimulating Research to Understand and Address Hunger, Food and Nutrition Insecurity” [129], “Preventive Interventions to Address Cardiometabolic Risk Factors in Populations that Experience Health Disparities” [130], and “Using Systems Science Methodologies to Protect and Improve Child and Reproductive Population Health” [131]. Notices of Special Interest are linked to research project (R01) awards and other projects performed by the applicant in an area of their specific interest (for example, K awards) and provide an opportunity to conduct research using the NHDF.
Measures: importance of accuracy, representation across heterogeneous communities
When conducting research within the aforementioned levels and domains of the NHDF, it is essential to consider study participants’ characteristics, such as age, sex, race/ethnicity, health literacy, cultural beliefs and practices, and the appropriateness of chosen assessment measures. For example, access to technology and the selection of nutrition measures are dependent on population health literacy as well as cultural appropriateness of the measurement tools and databases, especially when intervening to change dietary patterns [132]. Although the utilization of similar tools across studies could allow for more direct comparability of findings, the validity, precision, and accuracy of an assessment measure may not be appropriate across heterogeneous communities. The choice of measures should represent the study population and ideally be developed in consultation with the communities represented in the study. Assessment measures may need to be modified, and researchers may thus need to step back and reconsider developing, adapting, and applying tools from different approaches.
The National Collaborative on Childhood Obesity Research convened a workshop in 2019 to discuss why the assessment of diet and physical activity among children, families, and communities at high risk of obesity needs to be conducted differently from measurement in other populations and communities, and particularly how SDOH can be incorporated into measurement approaches [133]. To address recommendations from these discussions, a Decision Tree was developed to guide considerations for creating new and adapting existing measures for high-risk groups [134]. Other areas warrant additional research, especially the development of methods and guidance to accommodate the need to balance standardization against tailoring and supporting efforts to ensure that measures and their implementation are culturally appropriate. In all aspects, researchers should identify the appropriate measures that align with the study objectives, population, and contexts in which the study is conducted.
Community-engaged research
When working in communities that experience nutrition and diet-related disparities and those that have historically been disenfranchised or excluded, community-engaged research involving community-based organizations and key interest groups is an approach to ensure inclusivity in research. Community engagement (community level) in research is defined as “a process of inclusive participation that supports mutual respect of values, actions, strategies, and opinions for authentic partnerships” [135] and includes diverse voices, built-in learning opportunities, and continuous communication [51]. Well-designed and implemented community-engaged research projects [135] have been shown to advance community goals and minimize risk of re-traumatization in communities, which is critical for research aiming to reduce diet-related disparities. Given constraints on time, adequate compensation, and resources for involvement in research (e.g., childcare services) may be important to consider when conducting community-engaged research in communities experiencing health disparities. Community-engaged approaches may also help to train a well-prepared workforce of culturally sensitive practitioners with a deeper knowledge of SDOH and better insights on effective strategies to address health and social injustice. Systematic reviews have found the effectiveness of community interventions to increase fruit and vegetable consumption most successful when implemented as part of a multicomponent program [136]. Given the complex, multifactorial causes of diet-related disparities, the involvement of a variety of perspectives is critical to the success and potential public health impact of interventions.
Despite growing recognition of the importance of community engagement, nutrition professionals require tools to implement and evaluate interventions through approaches purposely paired with community partners or interest groups. Also, it is essential to build awareness of newly emerging opportunities to support community-engaged research driven by community priorities and connect them to spaces where community assets and wisdom already exist and can be leveraged to address nutrition-related health disparities. One such opportunity is through the NIH Common Fund’s Community Partnerships to Advance Science for Society (ComPASS) Program [137]. Supporting research to improve health outcomes in communities affected by health disparities and inform social policies, systems, (societal level), and practices (behavioral level) to achieve optimal health, ComPASS uses a broad strategy to address structural factors that impact multiple dimensions of health, enabling communities and researchers to work collaboratively as equal partners in all phases of the research process.
Diversity in the nutrition workforce
A strong and diverse workforce reflective of communities and their populations will be critical in addressing the complex, multilevel challenges driving nutrition-related health disparities. Enhancing diversity among nutrition professionals, healthcare providers, policymakers, and researchers, possibly to resemble the communities they serve, can bring different perspectives and lived experiences with the potential to develop innovative strategies and collaborations that meet the needs of individuals, families, and communities at risk for nutrition-related health disparities. Novel efforts and commitments seeking to attract individuals early in the educational spectrum (e.g., career fair exposure in middle and high school) and retain them throughout their careers are critical for growing and diversifying the nutrition workforce; however, programs designed to improve the culture and environment in the workplace, augment effective mentoring strategies, and retain and reward individuals from diverse backgrounds throughout their career trajectory are also needed. An effort to achieve diversity in the nutrition research workforce is the NIH-funded consortium, Bringing Resources to Increase Diversity, Growth, Excellence, and Scholarship for Nutrition, Obesity, and Diabetes Research, which provides career development programs for early career scholars from diverse backgrounds [138]. Such programs designed to advance and sustain diversity will need rigorous evaluation plans to identify the most efficacious approaches so that programs proven to meet the needs of communities and partners in a scalable, sustainable manner continue to be supported, disseminated, and implemented. Based on research goals, the NHDF (Figure 1) can be used to identify mechanisms that can inform the development of multilevel nutrition interventions to prevent or reduce health disparities in diverse populations.
Conclusions
Given the disproportionate burden of diet-related diseases and poor diet quality among disadvantaged populations in the United States, frameworks are needed to better understand how these disparities are perpetuated, with the ultimate goal of guiding the development of effective interventions to address these nutritional health disparities. Essential to this process are community partnerships, a diverse workforce, structural and policy-level changes, and the collective will and determination to eliminate health disparities. To this end, this article reviews the NHDF to understand how multilevel determinants contribute to nutrition-related health disparities and the complexities of these interrelated factors. This framework expands our understanding of the synergistic relationships between the biological, behavioral, environmental, sociocultural, and healthcare domains and among factors at different levels of the socioecological model. It helps elucidate how these intersecting factors influence diet quality and exacerbate nutrition-related health disparities and diet-related chronic disease.
There is a critical need for multidisciplinary partnerships to create a comprehensive research agenda to reduce hunger, improve diet quality, increase access to healthy food, and eliminate health disparities. National efforts include the 2022 White House Conference on Hunger, Nutrition, and Health [139], which is developing partnerships with community-based organizations, the healthcare community, nonprofit organizations, and food companies to end hunger and reduce diet-related diseases and disparities. The NHDF is a resource that can be used by various entities such as researchers, practitioners, food industry leaders, and policymakers to inform the identification of viable intervention targets to tackle nutrition-related health disparities and, ultimately, advance nutrition equity.
Author contributions
The authors’ contributions were as follows – TAC, AB: developed the outline and focus of the article and all authors: wrote, reviewed, and commented on drafts of the manuscript, and read and approved the final manuscript.
Conflict of interest
The authors report no conflicts of interest.
Funding
This research is funded by the National Institutes of Health.
Disclaimers
The opinions expressed in this article are those of the authors and do not necessarily represent the official views of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
References
- 1.Afshin A., Sur P.J., Fay K.A., Cornaby L., Ferrara G., Salama J.S., et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thornton P.L., Kumanyika S.K., Gregg E.W., Araneta M.R., Baskin M.L., Chin M.H., et al. New research directions on disparities in obesity and type 2 diabetes. Ann. N. Y. Acad. Sci. 2020;1461(1):5–24. doi: 10.1111/nyas.14270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paremoer L., Nandi S., Serag H., Baum F. COVID-19 pandemic and the social determinants of health. BMJ. 2021;372:n129. doi: 10.1136/bmj.n129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwok S., Adam S., Ho J.H., Iqbal Z., Turkington P., Razvi S., et al. Obesity: a critical risk factor in the COVID-19 pandemic. Clin. Obes. 2020;10(6) doi: 10.1111/cob.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Han J., Schwartz A.E., Elbel B. Does proximity to fast food cause childhood obesity? Evidence from public housing. Reg. Sci. Urban. Econ. 2020;84 doi: 10.1016/j.regsciurbeco.2020.103565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corona G., Dubowitz T., Troxel W.M., Ghosh-Dastidar M., Rockette-Wagner B., Gary-Webb T.L. Neighborhood food environment associated with cardiometabolic health among predominately low-income, Urban, Black Women. Ethn. Dis. 2021;31(4):537–546. doi: 10.18865/ed.31.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Masdor N.A., Mohammed Nawi A., Hod R., Wong Z., Makpol S., Chin S.F. The link between food environment and colorectal cancer: a systematic review. Nutrients. 2022;14(19):3954. doi: 10.3390/nu14193954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Darmon N., Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr. Rev. 2015;73(10):643–660. doi: 10.1093/nutrit/nuv027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chisolm D.J., Bell B.A., Yamoah O., Freedman D.A. Racialized experiences differentiate food security among African American adults. Nurs. Res. 2021;70(5S Suppl 1):S13–S20. doi: 10.1097/NNR.0000000000000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burke M.P., Jones S.J., Frongillo E.A., Fram M.S., Blake C.E., Freedman D.A. Severity of household food insecurity and lifetime racial discrimination among African-American households in South Carolina, Ethn. Health. 2018;23(3):276–292. doi: 10.1080/13557858.2016.1263286. [DOI] [PubMed] [Google Scholar]
- 11.Forsyth J.M., Schoenthaler A., Ogedegbe G., Ravenell J. Perceived racial discrimination and adoption of health behaviors in hypertensive Black Americans: the CAATCH trial. J. Health Care Poor Underserved. 2014;25(1):276–291. doi: 10.1353/hpu.2014.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Egede J.K., Campbell J.A., Walker R.J., Egede L.E. Perceived stress as a pathway for the relationship between neighborhood factors and glycemic control in adults with diabetes. Am. J. Health Promot. 2022;36(2):269–278. doi: 10.1177/08901171211050369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Serchen J., Doherty R., Atiq O., Hilden D. Health and Public Policy Committee of the American College of Physicians, A comprehensive policy framework to understand and address disparities and discrimination in health and health care: a policy article from the American College of Physicians. Ann. Intern. Med. 2021;174(4):529–532. doi: 10.7326/M20-7219. [DOI] [PubMed] [Google Scholar]
- 14.Satia J.A. Diet-related disparities: understanding the problem and accelerating solutions. J. Am. Diet. Assoc. 2009;109(4):610–615. doi: 10.1016/j.jada.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jia J., Fung V., Meigs J.B., Thorndike A.N. Food insecurity, dietary quality, and health care utilization in lower-income adults: a cross-sectional study. J. Acad. Nutr. Diet. 2021;121(11):2177. doi: 10.1016/j.jand.2021.06.001. 2186.e3. [DOI] [PubMed] [Google Scholar]
- 16.Dean E.B., French M.T., Mortensen K. Food insecurity, health care utilization, and health care expenditures. Health Serv. Res. 2020;55(Suppl 2):883–893. doi: 10.1111/1475-6773.13283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alvidrez J., Castille D., Laude-Sharp M., Rosario A., Tabor D. The National Institute on Minority Health and Health Disparities Research Framework. Am. J. Public Health. 2019;109(S1):S16–S20. doi: 10.2105/AJPH.2018.304883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frame L.A., Costa E., Jackson S.A. Current explorations of nutrition and the gut microbiome: a comprehensive evaluation of the review literature. Nutr. Rev. 2020;78(10):798–812. doi: 10.1093/nutrit/nuz106. [DOI] [PubMed] [Google Scholar]
- 19.Freedman B.I., Register T.C. Effect of race and genetics on vitamin D metabolism, bone and vascular health. Nat. Rev. Nephrol. 2012;8(8):459–466. doi: 10.1038/nrneph.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robinson-Cohen C., Hoofnagle A.N., Ix J.H., Sachs M.C., Tracy R.P., Siscovick D.S., et al. Racial differences in the association of serum 25-hydroxyvitamin D concentration with coronary heart disease events. JAMA. 2013;310(2):179–188. doi: 10.1001/jama.2013.7228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsu S., Hoofnagle A.N., Gupta D.K., Gutierrez O.M., Peralta C.A., Shea S., et al. Race, ancestry, and vitamin D metabolism: the multi-ethnic study of atherosclerosis. J. Clin. Endocrinol. Metab. 2020;105(12):e4337–e4350. doi: 10.1210/clinem/dgaa612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brito I.L., Gurry T., Zhao S., Huang K., Young S.K., Shea T.P., et al. Transmission of human-associated microbiota along family and social networks. Nat. Microbiol. 2019;4(6):964–971. doi: 10.1038/s41564-019-0409-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davé V., Street K., Francis S., Bradman A., Riley L., Eskenazi B., et al. Bacterial microbiome of breast milk and child saliva from low-income Mexican-American women and children. Pediatr. Res. 2016;79(6):846–854. doi: 10.1038/pr.2016.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garcia-Larsen V., Ierodiakonou D., Jarrold K., Cunha S., Chivinge J., Robinson Z., et al. Diet during pregnancy and infancy and risk of allergic or autoimmune disease: a systematic review and meta-analysis. PLOS Med. 2018;15(2) doi: 10.1371/journal.pmed.1002507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Quinlan J.J. Foodborne illness incidence rates and food safety risks for populations of low socioeconomic status and minority race/ethnicity: a review of the literature. Int. J. Environ. Res. Public Health. 2013;10(8):3634–3652. doi: 10.3390/ijerph10083634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pohl A.M., Pouillot R., Bazaco M.C., Wolpert B.J., Healy J.M., Bruce B.B., et al. Differences among incidence rates of invasive listeriosis in the U.S. FoodNet population by age, sex, race/ethnicity, and pregnancy status, 2008–2016. Foodborne Pathog. Dis. 2019;16(4):290–297. doi: 10.1089/fpd.2018.2548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schaider L.A., Swetschinski L., Campbell C., Rudel R.A. Environmental justice and drinking water quality: are there socioeconomic disparities in nitrate levels in U.S. drinking water? Environ. Health. 2019;18(1):3. doi: 10.1186/s12940-018-0442-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matich E.K., Laryea J.A., Seely K.A., Stahr S., Su L.J., Hsu P.C. Association between pesticide exposure and colorectal cancer risk and incidence: a systematic review. Ecotoxicol. Environ. Saf. 2021;219 doi: 10.1016/j.ecoenv.2021.112327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ruiz D., Becerra M., Jagai J.S., Ard K., Sargis R.M. Disparities in environmental exposures to endocrine-disrupting chemicals and diabetes risk in vulnerable populations. Diabetes Care. 2017;41(1):193–205. doi: 10.2337/dc16-2765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Uche U.I., Evans S., Rundquist S., Campbell C., Naidenko O.V. Community-level analysis of drinking water data highlights the importance of drinking water metrics for the State, Federal Environmental Health Justice Priorities in the United States. Int. J. Environ. Res. Public Health. 2021;18(19) doi: 10.3390/ijerph181910401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karp R.J. Redlining and lead poisoning: causes and consequences. J. Health Care Poor Underserved. 2023;34(1):431–446. doi: 10.1353/hpu.2023.0028. [DOI] [PubMed] [Google Scholar]
- 32.Doyle J.T., Kindness L., Realbird J., Eggers M.J., Camper A.K. Challenges and opportunities for tribal waters: addressing disparities in safe public drinking water on the crow reservation in Montana, USA. Int. J. Environ. Res. Public Health. 2018;15(4):567. doi: 10.3390/ijerph15040567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Henderson S., Wells R. Environmental racism and the contamination of Black lives: a literature review. J. Afr. Am. Stud. 2021;25(1):134–151. [Google Scholar]
- 34.Wierda M., Amini R., Kruger D.J. Before and after the Flint water crisis: changes in the consumption of sugary beverages in residents affected by lead contamination. J. Health Care Poor Underserved. 2022;33(1):317–331. doi: 10.1353/hpu.2022.0023. [DOI] [PubMed] [Google Scholar]
- 35.Blake C.E., Frongillo E.A., Warren A.M., Constantinides S.V., Rampalli K.K., Bhandari S. Elaborating the science of food choice for rapidly changing food systems in low-and middle-income countries. Glob. Food Sec. 2021;28(100503):1–7. [Google Scholar]
- 36.Joseph P.V., Zhou Y., Brooks B., McDuffie C., Agarwal K., Chao A.M. Relationships among alcohol drinking patterns, macronutrient composition, and caloric intake: national health and nutrition examination survey 2017–2018. Alcohol Alcohol. 2022;57(5):559–565. doi: 10.1093/alcalc/agac009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gangrade N., Figueroa J., Leak T.M. Socioeconomic disparities in foods/beverages and nutrients consumed by U.S. adolescents when snacking: national health and nutrition examination survey 2005–2018. Nutrients. 2021;13(8):2530. doi: 10.3390/nu13082530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leung C.W., Wolfson J.A. Food insecurity among older adults: 10-year national trends and associations with diet quality. J. Am. Geriatr. Soc. 2021;69(4):964–971. doi: 10.1111/jgs.16971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Monsivais P., Rehm C.D., Drewnowski A. The DASH diet and diet costs among ethnic and racial groups in the United States. JAMA Intern. Med. 2013;173(20):1922–1924. doi: 10.1001/jamainternmed.2013.9479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rehm C.D., Peñalvo J.L., Afshin A., Mozaffarian D. Dietary intake among US adults, 1999–2012. JAMA. 2016;315(23):2542–2553. doi: 10.1001/jama.2016.7491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kazmierski K.F.M., Gillespie M.L., Kuo S., Zurita T., Felix D., Rao U. Stress-induced eating among racial/ethnic groups in the United States: a systematic review. J. Racial Ethn. Health Disparities. 2021;8(4):912–926. doi: 10.1007/s40615-020-00849-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deierlein A.L., Litvak J., Stein C.R. Dietary quality and diet-related factors among female adults of reproductive age with and without disabilities participating in the national health and nutrition examination surveys, 2013–2018. J. Acad. Nutr. Diet. 2023;23(2):263–275. doi: 10.1016/j.jand.2022.07.010. [DOI] [PubMed] [Google Scholar]
- 43.Bandini L.G., Curtin C., Phillips S.M., Rogers G.T., Eliasziw M., Perelli J., et al. Nutrient adequacy, dietary patterns and diet quality among children with and without intellectual disabilities. J. Intellect. Disabil. Res. 2021;65(10):898–911. doi: 10.1111/jir.12871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jabs J., Devine C.M. Time scarcity and food choices: an overview. Appetite. 2006;47(2):196–204. doi: 10.1016/j.appet.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 45.Glanz K., Metcalfe J.J., Folta S.C., Brown A., Fiese B. Diet and health benefits associated with in-home eating and sharing meals at home: a systematic review. Int. J. Environ. Res. Public Health. 2021;18(4):1577. doi: 10.3390/ijerph18041577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wordell D., Daratha K., Mandal B., Bindler R., Butkus S.N. Changes in a middle school food environment affect food behavior and food choices. J. Acad. Nutr. Diet. 2012;112(1):137–141. doi: 10.1016/j.jada.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 47.Linde J.A., Horning Dehmer M.L., Lee J., Friend S., Flattum C., Arcan C., et al. Associations of parent dietary role modeling with children’s diet quality in a rural setting: baseline data from the NU-HOME study. Appetite. 2022;174 doi: 10.1016/j.appet.2022.106007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Monroe-Lord L., Anderson A., Jones B.L., Richards R., Reicks M., Gunther C., Banna J., et al. Relationship between family racial/ethnic backgrounds, parenting practices and styles, and adolescent eating behaviors. Int. J. Environ. Res. Public Health. 2022;19(12):7388. doi: 10.3390/ijerph19127388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sun Y., Supriya R., Gao Y., Yu S., Wang A., Ou X., et al. The relationships between parenting practices and child health-related behaviors in children with intellectual disability: the moderating role of child body weight status. Nutrients. 2022;14(24):5206. doi: 10.3390/nu14245206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Payán D.D., Lewis L.B., Illum J., Hawkins B., Sloane D.C. United for health to improve urban food environments across five underserved communities: a cross-sector coalition approach. BMC Public Health. 2022;22(1):888. doi: 10.1186/s12889-022-13245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dailey A., Davidson K., Gaskin K., Cooper L., Schell B., Gagliardi Y., et al. Responding to food insecurity and community crises through food policy council partnerships in a rural setting. Prog. Commun. Health Partnersh. 2022;16(2s):39–44. doi: 10.1353/cpr.2022.0037. [DOI] [PubMed] [Google Scholar]
- 52.Thorndike A.N., Gardner C.D., Kendrick K.B., Seligman H.K., Yaroch A.L., Gomes A.V., et al. Strengthening US food policies and programs to promote equity in nutrition security: a policy statement from the American Heart Association. Circulation. 2022;145(24):e1077–e1093. doi: 10.1161/CIR.0000000000001072. [DOI] [PubMed] [Google Scholar]
- 53.Valizadeh P., Popkin B.M., Ng S.W. Linking a sugar-sweetened beverage tax with fruit and vegetable subsidies: a simulation analysis of the impact on the poor. Am. J. Clin. Nutr. 2022;115(1):244–255. doi: 10.1093/ajcn/nqab330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Costa-Font J., Hockley T., Rudisill C. Cambridge University Press; Cambridge, UK: 2023. Behavioural Incentive Design for Health Policy: Steering for Health. [Google Scholar]
- 55.Browne J., Lock M., Walker T., Egan M., Backholer K. Effects of food policy actions on Indigenous Peoples’ nutrition-related outcomes: a systematic review. BMJ Glob. Health. 2020;5(8) doi: 10.1136/bmjgh-2020-002442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rivera R.L., Dunne J., Maulding M.K., Wang Q., Savaiano D.A., Nickols-Richardson S.M., et al. Exploring the association of urban or rural county status and environmental, nutrition- and lifestyle-related resources with the efficacy of SNAP-Ed (Supplemental Nutrition Assistance Program-Education) to improve food security. Public Health Nutr. 2018;21(5):957–966. doi: 10.1017/S1368980017003391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Huang Y., Pomeranz J., Wilde P., Capewell S., Gaziano T., O’Flaherty M., et al. Adoption and design of emerging dietary policies to improve cardiometabolic health in the US. Curr. Atheroscler. Rep. 2018;20(5):25. doi: 10.1007/s11883-018-0726-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grummon A.H., Taillie L.S. Supplemental Nutrition Assistance Program participation and racial/ethnic disparities in food and beverage purchases. Public Health Nutr. 2018;21(18):3377–3385. doi: 10.1017/S1368980018002598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lacko A.M., Guilkey D., Popkin B., Ng S.W. Associations among select state policies and the nutritional quality of household packaged food purchases in the United States from 2008 through 2017. J. Acad. Nutr. Diet. 2022;122(4):731. doi: 10.1016/j.jand.2021.09.017. 744.e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moran A.J., Gu Y., Clynes S., Goheer A., Roberto C.A., Palmer A. Associations between governmental policies to improve the nutritional quality of supermarket purchases and individual, retailer, and community health outcomes: an integrative review. Int. J. Environ. Res. Public Health. 2020;17(20):7493. doi: 10.3390/ijerph17207493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dunn R.A., Sharkey J.R., Horel S. The effect of fast-food availability on fast-food consumption and obesity among rural residents: an analysis by race/ethnicity, Econ. Hum. Biol. 2012;10(1):1–13. doi: 10.1016/j.ehb.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 62.Chen X., Clark J. Measuring space–time access to food retailers: a case of temporal access disparity in Franklin County, Ohio, Prof. Geogr. 2016;68(2):175–188. [Google Scholar]
- 63.Edmonds A.T., Rhew I.C., Jones-Smith J., Chan K.C.G., De Castro A.B., Rubinsky A.D., et al. Neighborhood disadvantage, patterns of unhealthy alcohol use, and differential associations by gender, race/ethnicity, and rurality: a study of veterans health administration patients. J. Stud. Alcohol Drugs. 2022;83(6):867–878. doi: 10.15288/jsad.21-00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dhillon J., Diaz Rios L.K., Aldaz K., De La Cruz N., Vu E., Asad Asghar S., et al. We don’t have a lot of healthy options: Food Environment Perceptions of First-Year, Minority College Students Attending a Food Desert Campus. Nutrients. 2019;11(4):816. doi: 10.3390/nu11040816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schwartz N., Buliung R., Wilson K. Disability and food access and insecurity: a scoping review of the literature. Health Place. 2019;57:107–121. doi: 10.1016/j.healthplace.2019.03.011. [DOI] [PubMed] [Google Scholar]
- 66.Berggreen-Clausen A., Hseing Pha S., Mölsted Alvesson H., Andersson A., Daivadanam M. Food environment interactions after migration: a scoping review on low- and middle-income country immigrants in high-income countries. Public Health Nutr. 2022;25(1):136–158. doi: 10.1017/S1368980021003943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moffat L.F., Ritchie L.D., Gosliner W., Plank K.R., Au L.E. Perceived produce availability and child fruit and vegetable intake: the healthy communities study. Nutrients. 2021;13(11):3681. doi: 10.3390/nu13113681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Johnson K.A., Jones-Smith J., Curriero F.C., Cheskin L.J., Benjamin-Neelon S.E., Perin J., et al. Low-income Black and Hispanic children’s neighborhood food environments and weight trajectories in early childhood. Acad. Pediatr. 2020;20(6):784–792. doi: 10.1016/j.acap.2019.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gustafson A., Jilcott Pitts S., Mcdonald J., Ford H., Connelly P., Gillespie R., et al. Direct effects of the home, school, and consumer food environments on the association between food purchasing patterns and dietary intake among rural adolescents in Kentucky and North Carolina, 2017. Int. J. Environ. Res. Public Health. 2017;14(10):1255. doi: 10.3390/ijerph14101255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kraft A.N., Thatcher E.J., Zenk S.N. Neighborhood food environment and health outcomes in U.S. low-socioeconomic status, racial/ethnic minority, and rural populations: a systematic review. J. Health Care Poor Underserved. 2020;31(3):1078–1114. doi: 10.1353/hpu.2020.0083. [DOI] [PubMed] [Google Scholar]
- 71.Centers for Disease Control and Prevention Disability and Obesity. 2023 https://www.cdc.gov/ncbddd/disabilityandhealth/obesity.html [Internet] [cited]. Available from: [Google Scholar]
- 72.McKinnon R.A., Reedy J., Morrissette M.A., Lytle L.A., Yaroch A.L. Measures of the food environment: a compilation of the literature, 1990–2007. Am. J. Prev. Med. 2009;36(4 Suppl):S124–S133. doi: 10.1016/j.amepre.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 73.Caspi C.E., Sorensen G., Subramanian S.V., Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18(5):1172–1187. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Diehl J.A., Heard D., Lockhart S., Main D.S. Access in the food environment: a health equity approach reveals unequal opportunity. J. Plan. Educ. Res. 2020;40(1):69–81. [Google Scholar]
- 75.Luongo G., Skinner K., Phillipps B., Yu Z., Martin D., Mah C.L. The retail food environment, store foods, and diet and health among indigenous populations: a scoping review. Curr. Obes. Rep. 2020;9(3):288–306. doi: 10.1007/s13679-020-00399-6. [DOI] [PubMed] [Google Scholar]
- 76.Trude A.C.B., Lowery C.M., Ali S.H., Vedovato G.M. An equity-oriented systematic review of online grocery shopping among low-income populations: implications for policy and research. Nutr. Rev. 2022;80(5):1294–1310. doi: 10.1093/nutrit/nuab122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shaker Y., Grineski S.E., Collins TW., Flores A.B. Redlining, racism and food access in US urban cores. Agric. Hum. Values. 2023;40(1):101–112. doi: 10.1007/s10460-022-10340-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Matsuzaki M., Sánchez B.N., Rebanal R.D., Gittelsohn J., Sanchez-Vaznaugh E.V. California and federal school nutrition policies and obesity among children of Pacific Islander, American Indian/Alaska Native, and Filipino origins: interrupted time series analysis. PLOS Med. 2021;18(5) doi: 10.1371/journal.pmed.1003596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Backholer K., Gupta A., Zorbas C., Bennett R., Huse O., Chung A., et al. Differential exposure to, and potential impact of, unhealthy advertising to children by socio-economic and ethnic groups: a systematic review of the evidence. Obes. Rev. 2021;22(3) doi: 10.1111/obr.13144. [DOI] [PubMed] [Google Scholar]
- 80.Harris J., Fleming-Milici F., Phaneuf L., Jensen M., Choi Y.Y., McCann M., et al. UConn Rudd Center for Food Policy & Obesity, Storrs, CT. 2021. Fast food advertising: billions in spending, continued high exposure by youth, in FAST FOOD F.A.C.T.S. [Google Scholar]
- 81.Adeigbe R.T., Baldwin S., Gallion K., Grier S., Ramirez A.G. Food and beverage marketing to Latinos: a systematic literature review. Health Educ. Behav. 2015;42(5):569–582. doi: 10.1177/1090198114557122. [DOI] [PubMed] [Google Scholar]
- 82.Larson N., Ayers Looby A., Frost N., Nanney M.S., Story M. What can be learned from existing investigations of weight-related practices and policies with the potential to impact disparities in US child-care settings? A narrative review and call for surveillance and evaluation efforts. J. Acad. Nutr. Diet. 2017;117(10):1554–1577. doi: 10.1016/j.jand.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 83.Desbouys L., Méjean C., De Henauw S., Castetbon K. Socio-economic and cultural disparities in diet among adolescents and young adults: a systematic review. Public Health Nutr. 2020;23(5):843–860. doi: 10.1017/S1368980019002362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mora N., Golden S.H. Understanding cultural influences on dietary habits in Asian, Middle Eastern, and Latino patients with type 2 diabetes: a review of current literature and future directions. Curr. Diab. Rep. 2017;17(12):126. doi: 10.1007/s11892-017-0952-6. [DOI] [PubMed] [Google Scholar]
- 85.Bekelman T.A., Johnson S.L., Taylor C.A. Differences in diet quality and snack intakes among non-Hispanic White and Mexican American adolescents from different acculturation groups. J. Racil Ethn. Health Disparities. 2020;7(6):1090–1099. doi: 10.1007/s40615-020-00732-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Heer M.M., Winham D.M. Bean preferences vary by acculturation level among Latinas and by ethnicity with non-Hispanic White women. Int. J. Environ. Res. Public Health. 2020;17(6):2100. doi: 10.3390/ijerph17062100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Martin C.L., Tate D.F., Schaffner A., Brannen A., Hatley K.E., Diamond M., et al. Acculturation influences postpartum eating, activity, and weight retention in low-income Hispanic women. J. Womens Health. 2017;26(12):1333–1339. doi: 10.1089/jwh.2016.6154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dulin A., Risica P.M., Mello J., Ahmed R., Carey K.B., Cardel M., et al. Examining neighborhood and interpersonal norms and social support on fruit and vegetable intake in low-income communities. BMC Public Health. 2018;18(1):455. doi: 10.1186/s12889-018-5356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Choi Y.J., Ailshire J.A., Crimmins E.M. Living alone, social networks in neighbourhoods, and daily fruit and vegetable consumption among middle-aged and older adults in the USA. Public Health Nutr. 2020;23(18):3315–3323. doi: 10.1017/S1368980020002475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Asamane E.A., Greig C.A., Thompson J.L. Social networks and their influences on nutrient intake, nutritional status and physical function in community-dwelling ethnically diverse older adults: a mixed-methods longitudinal study. BMC Public Health. 2020;20(1):1011. doi: 10.1186/s12889-020-09153-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Phojanakong P., Brown Weida E., Grimaldi G., Lê-Scherban F., Chilton M. Experiences of racial and ethnic discrimination are associated with food insecurity and poor health. Int. J. Environ. Res. Public Health. 2019;16(22):4369. doi: 10.3390/ijerph16224369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hooper L., Puhl R., Eisenberg M.E., Crow S., Neumark-Sztainer D. Weight teasing experienced during adolescence and young adulthood: cross-sectional and longitudinal associations with disordered eating behaviors in an ethnically/racially and socioeconomically diverse sample. Int. J. Eat. Disord. 2021;54(8):1449–1462. doi: 10.1002/eat.23534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pascoe E.A., Lattanner M.R., Richman L.S. Meta-analysis of interpersonal discrimination and health-related behaviors. Health Psychol. 2022;41(5):319–331. doi: 10.1037/hea0001147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Orr M.G., Galea S., Riddle M., Kaplan G.A. Reducing racial disparities in obesity: simulating the effects of improved education and social network influence on diet behavior. Ann. Epidemiol. 2014;24(8):563–569. doi: 10.1016/j.annepidem.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 95.Bowen S., Elliott S., Hardison-Moody A. The structural roots of food insecurity: how racism is a fundamental cause of food insecurity. Sociol. Compass. 2021;15(7) [Google Scholar]
- 96.Denney J.T., Kimbro R.T., Heck K., Cubbin C. Social cohesion and food insecurity: insights from the Geographic Research on Wellbeing (GROW) study, Matern. Child Health J. 2017;21(2):343–350. doi: 10.1007/s10995-016-2119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jhe G.B., Mereish E.H., Gordon A.R., Woulfe J.M., Katz-Wise S.L. Associations between anti-bisexual minority stress and body esteem and emotional eating among bi+ individuals: the protective role of individual- and community-level factors, Eat. Behav. 2021;43 doi: 10.1016/j.eatbeh.2021.101575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wong M.S., Nau C., Kharmats A.Y., Vedovato G.M., Cheskin L.J., Gittelsohn J., et al. Using a computational model to quantify the potential impact of changing the placement of healthy beverages in stores as an intervention to "Nudge" adolescent behavior choice. BMC Public Health. 2015;15:1284. doi: 10.1186/s12889-015-2626-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Neff R.A., Palmer A.M., Mckenzie S.E., Lawrence R.S. Food systems and public health disparities. J. Hunger Environ. Nutr. 2009;4(3–4):282–314. doi: 10.1080/19320240903337041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Earnshaw V.A., Karpyn A. Understanding stigma and food inequity: a conceptual framework to inform research, intervention, and policy. Transl. Behav. Med. 2020;10(6):1350–1357. doi: 10.1093/tbm/ibaa087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Guntzviller L.M., King A.J., Jensen J.D., Davis L.A. Self-efficacy, health literacy, and nutrition and exercise behaviors in a low-income, Hispanic population. J. Immigr. Minor. Health. 2017;19(2):489–493. doi: 10.1007/s10903-016-0384-4. [DOI] [PubMed] [Google Scholar]
- 102.Nelson L.A., Ackerman M.T., Greevy R.A., Wallston K.A., Mayberry L.S. Beyond race disparities: accounting for socioeconomic status in diabetes self-care. Am. J. Prev. Med. 2019;57(1):111–116. doi: 10.1016/j.amepre.2019.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.The N.S., Crandell J.L., Thomas J., Couch S.C., Shah A.S., Maahs D.M., et al. Correlates of medical nutrition therapy and cardiovascular outcomes in youth with type 1 diabetes. J. Nutr. Educ. Behav. 2013;45(6):661–668. doi: 10.1016/j.jneb.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Porter G.C., Schwab R., Hill J.L., Bartee T., Heelan K.A., Michaud T.L., et al. Examining the feasibility and characteristics of realistic weight management support for patients: focus groups with rural, micropolitan, and metropolitan primary care providers. Prev. Med. Rep. 2021;23 doi: 10.1016/j.pmedr.2021.101390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Reid H.W., Lin O.M., Fabbro R.L., Johnson K.S., Svetkey L.P., Olsen M.K., et al. Racial differences in patient perception of interactions with providers are associated with health outcomes in type II diabetes. Patient Educ. Couns. 2021;104(8):1993–2003. doi: 10.1016/j.pec.2021.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tinius R.A., López J.D., Cade W.T., Stein R.I., Haire-Joshu D., Cahill A.G. Patient and obstetric provider communication regarding weight gain management among socioeconomically disadvantaged African American women who are overweight/obese. Women Health. 2020;60(2):156–167. doi: 10.1080/03630242.2019.1616044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bradbury D., Chisholm A., Watson P.M., Bundy C., Bradbury N., Birtwistle S. Barriers and facilitators to health care professionals discussing child weight with parents: a meta-synthesis of qualitative studies. Br. J. Health Psychol. 2018;23(3):701–722. doi: 10.1111/bjhp.12312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Thomas T.W., Golin C., Samuel-Hodge C.D., Kirkman M.S., Golden S.D., Lightfoot A.F. Race and gender differences in abnormal blood glucose screening and clinician response to prediabetes: a mixed-methods assessment. Prev. Med. 2021;148 doi: 10.1016/j.ypmed.2021.106587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Carpenter A., Kuchera A.M., Krall J.S. Connecting families at risk for food insecurity with nutrition assistance through a clinical-community direct referral model. J. Nutr. Educ. Behav. 2022;54(2):181–185. doi: 10.1016/j.jneb.2021.09.014. [DOI] [PubMed] [Google Scholar]
- 110.De Marchis E.H., Torres J.M., Benesch T., Fichtenberg C., Allen I.E., Whitaker E.M., et al. Interventions addressing food insecurity in health care settings: a systematic review. Ann. Fam. Med. 2019;17(5):436–447. doi: 10.1370/afm.2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Escobar E.R., Pathak S., Blanchard C.M. Peer reviewed: screening and referral care delivery services and unmet health-related social needs: a systematic review. Prev. Chronic Dis. 2021;18:E78. doi: 10.5888/pcd18.200569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fraze T.K., Brewster A.L., Lewis V.A., Beidler L.B., Murray G.F., Colla C.H. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US physician practices and hospitals. JAMA Netw. Open. 2019;2(9) doi: 10.1001/jamanetworkopen.2019.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Steeves-Reece A.L., Totten A.M., Broadwell K.D., Richardson D.M., Nicolaidis C., Davis M.M. Social needs resource connections: a systematic review of barriers, facilitators, and evaluation. Am. J. Prev. Med. 2022;62(5):e303–e315. doi: 10.1016/j.amepre.2021.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Downer S., Berkowitz S.A., Harlan T.S., Olstad D.L., Mozaffarian D. Food is medicine: actions to integrate food and nutrition into healthcare. BMJ. 2020;369:m2482. doi: 10.1136/bmj.m2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.White J.J. Care for food-insecure enrollees in Medicare Advantage vs traditional Medicare. Am. J. Manag. Care. 2021;27:7. doi: 10.37765/ajmc.2021.88707. [DOI] [PubMed] [Google Scholar]
- 116.Serchen J., Atiq O., Hilden D. Health and Public Policy Committee of the American College of Physicians, Strengthening food and nutrition security to promote public health in the United States: a position paper from the American College of Physicians. Ann. Intern. Med. 2022;175(8):1170–1171. doi: 10.7326/M22-0390. [DOI] [PubMed] [Google Scholar]
- 117.Employment Situation Summary US Bureau of Labor Statistics. Department of Labor. August 2023 https://www.bls.gov/news.release/empsit.nr0.htm [Internet] [cited]. Available from: [Google Scholar]
- 118.Pratap P., Dickson A., Love M., Zanoni J., Donato C., Flynn M.A., et al. Public health impacts of underemployment and unemployment in the United States: exploring perceptions, gaps and opportunities. Int. J. Environ. Res. Public Health. 2021;18(19) doi: 10.3390/ijerph181910021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Walton K., Horton N.J., Rifas-Shiman S.L., Field A.E., Austin S.B., Haycraft E., et al. Exploring the role of family functioning in the association between frequency of family dinners and dietary intake among adolescents and young adults. JAMA Netw. Open. 2018;1(7) doi: 10.1001/jamanetworkopen.2018.5217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Berge J.M., Wall M., Hsueh T.-F., Fulkerson J.A., Larson N., Neumark-Sztainer D. The protective role of family meals for youth obesity: 10-year longitudinal associations. J. Pediatr. 2015;166(2):296–301. doi: 10.1016/j.jpeds.2014.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Nagata J.M., Ganson K.T., Iyer P., Chu J., Baker F.C., Pettee Gabriel K., et al. Sociodemographic correlates of contemporary screen time use among 9- and 10-year-old children. J. Pediatr. 2022;240:213. doi: 10.1016/j.jpeds.2021.08.077. 220.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Compernolle S., De Cocker K., Lakerveld J., Mackenbach J.D., Nijpels G., Oppert J.M., et al. A RE-AIM evaluation of evidence-based multi-level interventions to improve obesity-related behaviours in adults: a systematic review (the SPOTLIGHT project) Int. J. Behav. Nutr. Phys. Act. 2014;11(1):1–13. doi: 10.1186/s12966-014-0147-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kumanyika S.K. A framework for increasing equity impact in obesity prevention. Am. J. Public Health. 2019;109(10):1350–1357. doi: 10.2105/AJPH.2019.305221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Garcia L.M., Hunter R.F., De La Haye K., Economos C.D., King A.C. An action-oriented framework for systems-based solutions aimed at childhood obesity prevention in US Latinx and Latin American populations. Obes. Rev. 2021;22 doi: 10.1111/obr.13241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lee B.Y., Bartsch S.M., Mui Y., Haidari L.A., Spiker M.L., Gittelsohn J. A systems approach to obesity. Nutr. Rev. 2017;75(Suppl_1):94–106. doi: 10.1093/nutrit/nuw049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Economos C.D., Hyatt R.R., Must A., Goldberg J.P., Kuder J., Naumova E.N., et al. Shape Up Somerville two-year results: a community-based environmental change intervention sustains weight reduction in children. Prev. Med. 2013;57(4):322–327. doi: 10.1016/j.ypmed.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 127.Gittelsohn J., Song H.J., Suratkar S., Kumar M.B., Henry E.G., Sharma S., et al. An urban food store intervention positively affects food-related psychosocial variables and food behaviors. Health Educ. Behav. 2010;37(3):390–402. doi: 10.1177/1090198109343886. [DOI] [PubMed] [Google Scholar]
- 128.National Institutes of Health PAR-21-305, Time-sensitive obesity policy and program evaluation. 2021 https://grants.nih.gov/grants/guide/pa-files/PAR-21–305.html [Internet] [cited]. Available from: [Google Scholar]
- 129.National Institutes of Health NOT-OD-22–135, Notice of Special Interest (NOSI): stimulating research to understand and address hunger. Food and Nutrition Insecurity. 2022 https://grants.nih.gov/grants/guide/notice-files/not-od-22–135.html [Internet] [cited]. Available from: [Google Scholar]
- 130.National Institutes of Health NOT-OD-22-154, Notice of special interest: preventive interventions to address cardiometabolic risk factors in populations that experience health disparities. 2022 https://grants.nih.gov/grants/guide/notice-files/NOT-OD-22–154.html [Internet] [cited]. Available from: [Google Scholar]
- 131.National Institutes of Health NOT-HD-20-032, Notice of special interest: using systems science methodologies to protect and improve child and reproductive population health. 2021 https://grants.nih.gov/grants/guide/notice-files/NOT-HD-20–032.html [Internet] [cited]. Available from: [Google Scholar]
- 132.Carbone E.T., Zoellner J.M. Nutrition and health literacy: a systematic review to inform nutrition research and practice. J. Acad. Nutr. Diet. 2012;112(2):254–265. doi: 10.1016/j.jada.2011.08.042. [DOI] [PubMed] [Google Scholar]
- 133.Ballard R., Arteaga S.S., Berrigan D., Devlin H.M., Galuska D.A., Hamner H.C., et al. Advancing measurement to address childhood obesity: results of 3 workshops. Am. J. Prev. Med. 2021;61(6):e296–e304. doi: 10.1016/j.amepre.2021.05.025. [DOI] [PubMed] [Google Scholar]
- 134.National Collaborative on Childhood Obesity Research Measures for children at high risk for obesity [Internet] https://www.nccor.org/projects/measures-for-children-at-high-risk-for-obesity/decision-tree/2023 [cited]. Available from:
- 135.Ahmed S.M., Palermo A.G. Community engagement in research: frameworks for education and peer review. Am. J. Public Health. 2010;100(8):1380–1387. doi: 10.2105/AJPH.2009.178137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ciliska D., Miles E., O’brien M.A., Turl C., Tomasik H.H., Donovan U., et al. Effectiveness of community-based interventions to increase fruit and vegetable consumption. J. Nutr. Educ. 2000;32(6):341–352. [Google Scholar]
- 137.National Institutes of Health Community Partnerships to Advance Science for Society (ComPASS) 2023 https://commonfund.nih.gov/compass [Internet] [cited]. Available from: [Google Scholar]
- 138.National Institutes of Health RFA-DK-20-034, Program to advance the career development of scientists from diverse backgrounds conducting nutrition, obesity, diabetes, and related research. 2020 https://grants.nih.gov/grants/guide/rfa-files/rfa-dk-20–034.html [Internet] [cited]. Available from: [Google Scholar]
- 139.Psota T., Maniscalco S., Kijek M., Ohlhorst S.D. Driving transformative change to end hunger and reduce diet-related diseases and disparities: the White House Conference on Hunger, Nutrition, and Health. Am. J. Clin. Nutr. 2023;117(4):649–658. doi: 10.1016/j.ajcnut.2023.01.013. [DOI] [PubMed] [Google Scholar]