Abstract
Introduction
Benign lipomatous tumors are soft tissue tumors that exhibit a predominant adipocytic phenotype. Lipomas are the archetype and are the most common benign soft tissue tumors in adults but relatively uncommon in children. Their sex incidence is equivocal. They sometimes occur in combination with other mesenchymal elements, giving rise to variants including fibrolipoma, angiolipoma, myolipoma, spindle cell lipoma, chondroid lipoma, osteolipoma, and chondrolipoma. Their clinical significance is mainly due to the cosmetic disfigurement of patients and the differential diagnosis of malignant soft tissue tumors. Occasionally, due to their large size or presence near vital organs, they may cause life-threatening and/or excruciating pressure symptoms.
This study was purposed to address the dearth of local studies on the clinical and morphological characteristics of benign lipomatous tumors in Nigerians, to compare these with those of other populations, and to establish baseline data.
Materials and methods
This was a retrospective study of all benign lipomatous tumors seen in the anatomic pathology and forensic medicine department of Asokoro District Hospital, Abuja, Federal Capital Territory, Nigeria, over an eight-year period. Surgical pathology reports were retrieved for patients’ biodata and clinical information. The appropriate slides were retrieved, and reviewed, and new sections were cut where necessary. The tumors were classified according to the 2020 World Health Organization (WHO) guidelines and categorized based on size as small, medium, or giant. The data obtained were analyzed, and the results were presented as tables, bar charts, ratios, and percentages.
Results
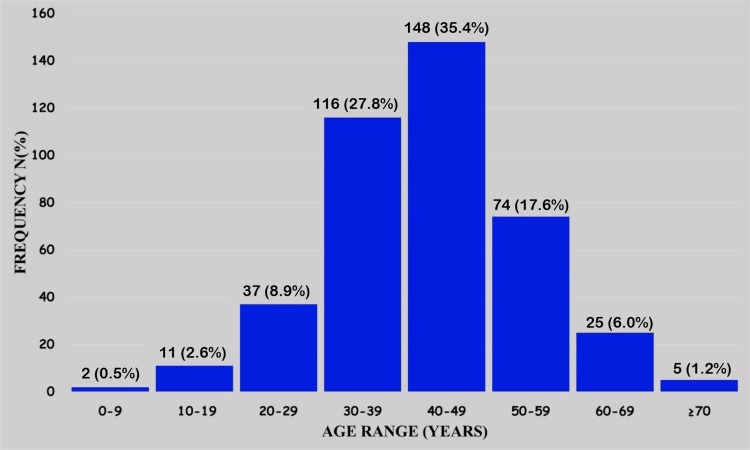
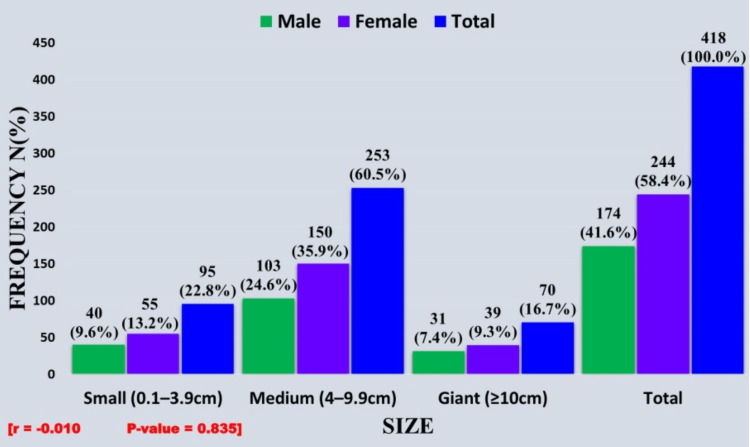
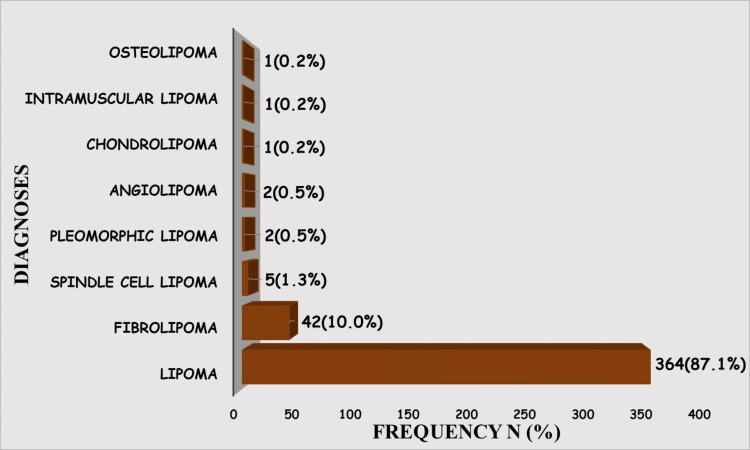
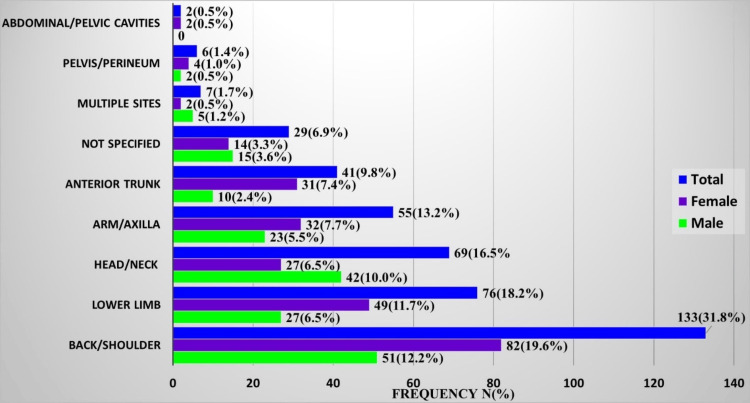
Four hundred and eighteen cases met the inclusion criteria. Of these, 58.4% (244/418), occurred in females, while 41.6% (174/418) occurred in males. The age range was six to 91 years, while the median age was 42 years. The least number of cases, 0.5% (2/418), were seen in patients aged less than 10 years, while the majority, 35.4% (148/418), occurred in the fifth decade, followed by 27.8% (116/418) in the fourth. Size-wise, the majority of tumors, 60% (253/418), were medium, followed by small, 22.8% (95/418). Giant-sized tumors significantly accounted for 16.7% (70/418) of the cases. The diagnostic spectrum comprised conventional lipoma and variants such as fibrolipoma, spindle cell lipoma, pleomorphic lipoma, angiolipoma, chondrolipoma, intramuscular lipoma, and osteolipoma. Lipoma and fibrolipoma dominated with 87.1% (364/418) and 10.0% (42/418), respectively, while the rest accounted for <3%. The majority, 31.8% (133/418), occurred in the back/shoulder region, followed by the lower limb with 18.2% (76/418). Only two cases occurred in the abdominal/pelvic region. More tumors occurred in females in all the regions except the head and neck, which had a male-to-female ratio of 1.5:1. Multiple site tumors were more common in males in a ratio of 2.5:1. Most, 41.1% (39/95), of the small-sized tumors, occurred in the head/neck region, largely involving the face, 48.7% (19/39).
Conclusion
Our study showed many similarities in the clinical and morphological features of benign lipomatous tumors between Nigerians and other regions of the world. A notable finding, however, was the significantly higher proportion of giant benign lipomatous tumors when compared to studies from other regions, a finding that warrants further studies.
Keywords: lipoma variants, lipoma, nigeria, benign lipomatous, soft tissue
Introduction
Soft tissue is defined as the supportive tissue of various organs and the non-epithelial, extra-skeletal structures exclusive to lymphohematopoietic tissues [1]. It includes fibrous connective tissue, adipose tissue, skeletal muscle, blood/lymph vessels, and, by convention, the peripheral nervous system because tumors arising from nerves clinically resemble soft tissue masses and pose similar problems in differential diagnosis and therapy [1]. Embryologically, soft tissue is derived principally from the mesoderm, while peripheral nerves arise from the neuroectoderm [1]. Both benign and malignant tumors arise from soft tissue and are typically classified more according to the adult tissue they resemble than their histogenesis since the concept of histogenesis is not sustainable in some of these tumors [2].
Lipomatous tumors are soft tissue tumors with a predominant adipocytic component, and lipomas are the benign form [3]. Lipomas consist of adipocytes arranged in lobules and separated by septa of fibrous connective tissue [1]. They are occasionally associated with other mesenchymal elements, giving rise to different histopathological variants including fibrolipoma, angiolipoma, myolipoma, spindle cell lipoma, chondroid lipoma, osteolipoma, and chondrolipoma [3-5]. Lipomas are the most common soft tissue tumors, occur anywhere on the body, and are usually asymptomatic and superficial [6, 7]. They usually occur in adults above 30 years, peaking between ages 40 and 60 years, with variable statistics as to incidence in males and females [1]. They are, however, uncommon in children [1]. Being mostly asymptomatic, lipomas in subcutaneous locations are clinically significant because of the cosmetic discomfort and distress patients experience [8]. Lipomas in deeper locations, on the other hand, present with symptoms ranging from slight discomfort in joints and intramuscular locations to life-threatening respiratory distress related to bronchial obstruction when in endobronchial or parenchymal locations [8]. The major treatment for lipoma is surgical excision. However, in cases where malignancy is suspected, an initial incisional biopsy is done to establish a histological diagnosis.
The literature on the demographics, clinical features (site and size), and morphological characteristics of lipomas in Nigeria is very scanty, as so far only one study has been found in the literature [9]. Rather, a plethora of authors have reported on unusual sites and/or variants of lipomas [10-13]. This study attempts to fill that void by describing the clinical and morphological features of lipomas as seen in a district hospital in Nigeria to compare them with those of other populations and establish baseline data.
Materials and methods
Study location and design
This was a retrospective study of all benign lipomatous tumors seen in the anatomic pathology and forensic medicine department of Asokoro District Hospital, Abuja, Federal Capital Territory (FCT), Nigeria, over an eight-year period from January 1, 2015, to December 31, 2022. Asokoro District Hospital is a quasi-tertiary center that serves as a referral center for cases from primary and secondary healthcare facilities in the FCT and other neighboring states such as Kogi, Nasarawa, and Niger States. It also provides teaching hospital services to the College of Health Sciences of Nile University of Nigeria, Abuja, FCT, Nigeria. Surgical pathology reports of patients diagnosed with benign lipomatous tumors during the study period were retrieved and scrutinized for macroscopic features. Patients’ biodata and clinical information were retrieved from electronic archives. The appropriate slides were retrieved, and reviewed, and new sections were cut from formalin-fixed, paraffin-embedded blocks in cases where such slides were missing or faded. All biopsies had been fixed in 10% neutral buffered formalin. The retrieved and freshly cut slides were reviewed by three pathologists with concurrence in equivocal cases in order to minimize interobserver variations.
Inclusion and exclusion criteria
Inclusion Criteria
Cases where the patient’s complete biodata and clinical information, along with a pathology report of lipoma/benign lipomatous tumors, were available and the slides were successfully reviewed were selected for the study. Also selected were cases that met the above criteria but for which only information on the tumor site was available.
Exclusion Criteria
Cases with the complete absence of either the patient’s biodata or clinical information and cases with missing slides for which the paraffin-embedded tissue blocks could not be found were excluded from the study.
Diagnostic criteria
The tumors were classified according to the 2020 World Health Organization (WHO) Classification of Soft Tissue Tumors [14]. The tumors were categorized based on size as small, medium, or giant, according to the definitions of Charifa et al. and Serpell et al. [15,16]. The specific sites of the tumors were grouped for convenience into regions as follows: head/neck, anterior trunk, back/shoulder, arm/axilla, pelvis/perineum, lower limb, and abdominal/pelvic cavities. Those that occurred at multiple sites were grouped, and those that met the inclusion criteria but for whom the location was not specified were categorized as not specified.
Statistical analysis
All data were entered in a spreadsheet using the Microsoft Office 365 version of the Excel software program (Microsoft Corporation, Redmond, WA) and analyzed with IBM SPSS Statistics for Windows, version 24.0 (IBM Corporation, Armonk, NY). Continuous variables were summarized using descriptive statistics, including range, median, mean ± standard deviation, and confidence interval, and analyzed using the chi-square test statistic. A p-value <0.05 was considered statistically significant. The results were displayed using tables and charts.
Ethical consideration
Ethical clearance was obtained from the medical ethics committee of Asokoro District Hospital (approval number: FCT/HHSS/HMB/ADH/139/23.)
Results
A total of 418 cases of benign lipomatous tumors diagnosed within the study period met the inclusion criteria. Of these, 58.4% (244/418) occurred in females, while 41.6% (174/418) occurred in males, giving a male-to-female ratio of 1:1.4.
The mean (mean±SD) of the patients’ ages was 41.9±11.6 years, with a range of six to 91 years, while the median age was 42 years. The confidence interval was 40.9-43.1. The least number of cases were seen in patients aged less than 10 years, who accounted for just 0.5% (2/418), and these occurred on the neck and back, respectively, of a male aged six years and a female aged eight years. The majority of the cases occurred in the 40-49 year age range with 35.4% (148/418), followed by the 30-39 year age range with 27.8% (116/418). Indeed, both age ranges combined accounted for 63.2% (264/418) of cases (Figure 1)
Figure 1. Cases of benign lipomatous tumors distributed according to age.
In terms of size, the largest tumor was a fibrolipoma, which measured 24 x 16 x 12cm and was located in the right thigh of a 45-year-old male, while the smallest was a lipoma, which measured 0.6 x 0.5 x 0.2cm and was located in the left popliteal fossa of a 50-year-old male. The mean size of the tumors was 6.4±3.6cm with a range of 1 cm to 24 cm, while the median size was 6 cm. The confidence interval was 6.1-6.8.1. Medium-sized tumors (4 cm-9.9 cm) accounted for 60% (253/418) of cases and were therefore in the majority. The relationship between the size of the tumor and the sex of the patients was not statistically significant (Figure 2).
Figure 2. Distribution of benign lipomatous tumors as per size and sex.
In the various size groups, the majority of the tumors were seen in the 40-49 year age range as follows: small, 38.9% (37/95); medium, 31.2% (79/253); and giant, 45.7% (32/70). Thus, the relationship between the age of patients and the size of the tumor was not statistically significant as it followed the overall age distribution. However, the correlation coefficient (r = -0.0019) indicates a weak negative association between age and tumor size (Table 1).
Table 1. Distribution of benign lipomatous tumors as per age and size.
| Age range (years) | Size | ||
| Small (0.1 cm–3.9 cm) n(%) | Medium (4 cm–9.9 cm) n(%) | Giant (≥10cm) n(%) | |
| 0–9 | 0 (0.0) | 2 (0.8) | 0 (0.0) |
| 10–19 | 4 (4.2) | 5 (2.0) | 2 (2.9) |
| 20–29 | 7 (7.4) | 26 (10.3) | 4 (5.7) |
| 30–39 | 22(23.2) | 78(30.8) | 16(22.8) |
| 40–49 | 37(38.9) | 79(31.2) | 32(45.7) |
| 50–59 | 18 (18.9) | 45 (17.8) | 11 (15.7) |
| 60–69 | 7 (7.4) | 15 (5.9) | 3 (4.3) |
| ≥70 | 0 (0.0) | 3 (1.2) | 2 (2.9) |
| Total | 95 (100.0) | 253 (100.0) | 70 (100.0) |
| Correlation coefficient (r) = –0.0019 | |||
| P–value = 0.990 | |||
The diagnostic spectrum of tumors was varied and comprised a significant representation of conventional lipoma and lipoma variants, including fibrolipoma, spindle cell lipoma, pleomorphic lipoma, angiolipoma, chondrolipoma, intramuscular lipoma, and osteolipoma. Lipoma and fibrolipoma dominated with 87.1% (364/418) and 10.0% (42/418), respectively. The other diagnoses combined were less than 3% (Figure 3).
Figure 3. Diagnostic spectrum of benign lipomatous tumors.
The relationship between diagnoses and the size of these benign lipomatous tumors was not statistically significant. In keeping with the overall size and number distribution, both lipoma and fibrolipoma, which were the most frequent diagnoses, occurred more in the medium size category, at 62.4% (227/364) and 54.8% (23/42), respectively (Table 2).
Table 2. Distribution of benign lipomatous tumors according to the diagnosis and size.
| Diagnoses | Size | Total n(%) | ||
| Small n(%) | Medium n(%) | Giant n(%) | ||
| Lipoma | 77 (21.2) | 227 (62.4) | 60 (16.4) | 364 (100) |
| Fibrolipoma | 11 (26.2) | 23 (54.8) | 8 (19.0) | 42 (100) |
| Spindle cell lipoma | 3 (60.0) | 1 (20.0) | 1 (20.0) | 5 (100) |
| Angiolipoma | 1 (50.0) | 0 (0.0) | 1 (50.0) | 2 (100) |
| Pleomorphic lipoma | 1 (50.0) | 1 (50.0) | 0 (0.0) | 2 (100) |
| Chondrolipoma | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 (100) |
| Intramuscular lipoma | 0 (0.0) | 1 (100.0) | 0 (0.0) | 1 (100) |
| Osteolipoma | 0 (0.0) | 1 (100.0) | 0 (0.0) | 1 (100) |
| Chi-square = 17.308 | ||||
| P–value = 0.696 | ||||
The relationship between the region or site and the sex distribution of these tumors was statistically significant. Overall, the commonest region of occurrence was the back/shoulder region with 31.8% (133/418) of cases, followed by the lower limb region with 18.2% (76/418). In keeping with the general sex distribution, more tumors occurred in females in all the regions except the head and neck, which had more tumors in males in a ratio of 1.5:1. Cases in which tumors occurred at multiple sites also showed a male preponderance with a ratio of 2.5:1 (Figure 4).
Figure 4. Distribution of benign lipomatous tumors according to the region of occurrence and sex.
The highest number of tumors occurred in the back and shoulders, both accounting for 21.1% (88/418), with a male-to-female ratio of 1:1.5. The least number, 0.5% (2/418), occurred in the abdominal/pelvic cavity in two females. In the lower limb region, the majority of the tumors, 64.5% (49/76), occurred in the thigh with a male-to-female ratio of 1:2. In the anterior trunk region, the chest with 46.3% (19/41) was the most frequent site of occurrence, with a male-to-female ratio of 1:3. However, in the breast, of the 12 cases seen, 11 occurred in females (Table 3).
Table 3. Distribution of benign lipomatous tumors according to region/site of occurrence and sex .
| Site | Frequency | Total n(%) | |
| Male n(%) | Female n(%) | ||
| Head/Neck region | |||
| Face | 15 (21.7) | 8 (11.6) | 23 (33.3) |
| Neck | 11 (15.9) | 13 (18.8) | 24 (34.8) |
| Scalp | 12 (17.4) | 2 (2.9) | 14 (20.3) |
| Eye | 2 (2.9) | 2 (2.9) | 4 (5.8) |
| Ear | 1 (1.4) | 1 (1.4) | 2 (2.9) |
| Lower lip | 1 (1.4) | 1 (1.4) | 2 (2.9) |
| Total n(%) | 42 (60.9) | 27 (39.1) | 69 (100) |
| Back/Shoulder region | |||
| Back | 34 (25.6) | 44 (33.1) | 78 (58.6) |
| Shoulder | 16 (12.0) | 29 (21.8) | 45 (33.8) |
| Scapular | 1 (0.8) | 9 (6.8) | 10 (7.5) |
| 51 (38.3) | 82 (61.7) | 133 (100.0) | |
| Arm/Axilla region | |||
| Arm | 19 (4.5) | 24 (5.7) | 43 (10.3) |
| Axilla | 4 (1.0) | 8 (1.9) | 12 (2.9) |
| Total | 23 (5.5) | 32 (7.7) | 55 (13.2) |
| Anterior trunk region | |||
| Chest | 6 (14.6) | 13 (31.7) | 19 (46.3) |
| Anterior abdominal wall | 3 (7.3) | 7 (17.1) | 10 (24.4) |
| Breast | 1 (2.4) | 11 (26.8) | 12 (29.3) |
| Total | 10 (24.4) | 31 (75.6) | 41 (100.0) |
| Lower limb region | |||
| Gluteus | 8 (10.5) | 10 (13.2) | 18 (23.7) |
| Leg | 3 (3.9) | 6 (7.9) | 9 (11.8) |
| Thigh | 16 (21.1) | 33 (43.4) | 49 (64.5) |
| Total | 27 (35.5) | 49 (64.5) | 76 (100.0) |
| Pelvis/Perineum | |||
| Perineum | 2 (33.3) | 2 (33.3) | 4 (66.7) |
| Vulva | 0 (0.0) | 2 (33.3) | 2 (33.3) |
| Total | 2 (33.3) | 4 (66.7) | 6 (100.0) |
| Abdominal/Pelvic cavities | |||
| Omentum | 0 (0.0) | 1 (50.0) | 1 (0.2) |
| Ovary | 0 (0.0) | 1 (50.0) | 1 (0.2) |
| Total | 0 (0.0) | 2 (100.0) | 2 (100.0) |
| Multiple sites | |||
| Multiple sites | 5 (71.4) | 2 (28.6) | 7 (100.0) |
| Not specified | |||
| Not specified | 15 (51.7) | 14 (48.3) | 29 (100.0) |
| Chi-square = 22.195 | |||
| P–value = 0.005 (significant at 95%) | |||
The association between the region/site and the size of the tumors was statistically significant. More of the small tumors, 41.1% (39/95), were seen in the head/neck region, with the face, 20.0% (19/95), accounting for the majority of these. Unusual locations in the face included the conjunctiva, eyelid, and lower lip. The next most common region of small tumor location was the lower limb, which had 17.9% (17/95), and the thigh, 14.7% (14/95), had the highest number in this region. The medium-sized tumors were commonest in the back/shoulder region with 34.9 (88/253) while significant numbers occurred in the arm/axilla, 16.6% (42/253), and lower limb, 16.2% (41/253), regions. Out of the 30 medium-sized tumors seen in the head/neck region, 60% (18/30) occurred in the neck. The back/shoulder region, with 44.3% (31/70), was the most frequent location of giant-sized tumors, followed by the lower limb region, which had 25.7% (18/70), with the majority of these (14/18) occurring in the thigh (Table 4).
Table 4. Distribution of benign lipomatous tumors as per region/site of occurrence and size.
| Region | Site | Size | |||||
| Small n(%) | Total n(%) | Medium n(%) | Total n(%) | Giant n(%) | Total n(%) | ||
| Head/ Neck | Face | 19 (4.5) | 39 (9.3) | 4 (1.0) | 30 (7.2) | 0 (0.0) | 0 (0.0) |
| Neck | 5 (1.2) | 18 (4.3) | 0 (0.0) | ||||
| Scalp | 8 (1.9) | 7 (1.7) | 0 (0.0) | ||||
| Eye | 4 (1.0) | 0 (0.0) | 0 (0.0) | ||||
| Ear | 1 (0.2) | 1 (0.2) | 0 (0.0) | ||||
| Lower Lip | 2 (0.5) | 0 (0.0) | 0 (0.0) | ||||
| Back/Shoulder | Back | 8 (1.9) | 14 (3.3) | 46 (11.0) | 88 (21.1) | 24 (5.7) | 31 (7.4) |
| Shoulder | 4 (1.0) | 37 (8.9) | 4 (1.0) | ||||
| Scapular | 2 (0.5) | 5 (1.2) | 3 (0.7) | ||||
| Perineum/ Pelvis | Perineum | 2 (0.5) | 2 (0.5) | 2 (0.5) | 3 (0.7) | 0 (0.0) | 1 (0.2) |
| Vulva | 0 (0.0) | 1 (0.2) | 1 (0.2) | ||||
| Lower Limb | Gluteus | 2 (0.5) | 17 (4.1) | 14 (3.3) | 41 (9.8) | 2 (0.5) | 18 (4.3) |
| Leg | 1 (0.2) | 6 (1.4) | 2 (0.5) | ||||
| Thigh | 14 (3.3) | 21 (5.0) | 14 (3.3) | ||||
| Anterior trunk | Chest | 1 (0.2) | 7 (1.7) | 17 (4.1) | 28 (6.7) | 1 (0.2) | 6 (1.4) |
| Anterior abdominal wall | 2 (0.5) | 4 (1.0) | 4 (1.0) | ||||
| Breast | 4 (1.0) | 7 (1.7) | 1 (0.2) | ||||
| Arm/Axilla | Arm | 6 (1.4) | 7 (1.7) | 33 (7.9) | 42 (10.0) | 4 (1.0) | 6 (1.4) |
| Axilla | 1 (0.2) | 9 (2.2) | 2 (0.5) | ||||
| Abdominal/ Pelvic cavities | Omentum | 1 (0.2) | 2 (0.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Ovary | 1 (0.2) | 0 (0.0) | 0 (0.0) | ||||
| Multiple sites | Multiple sites | 1 (0.2) | 1 (0.2) | 4 (1.0) | 4 (1.0) | 2 (0.5) | 2 (0.5) |
| Not specified | Not specified | 6 (1.4) | 6 (1.4) | 17 (4.1) | 17 (4.1) | 6 (1.4) | 6 (1.4) |
| Total | 95 (22.7) | 253 (60.5) | 70 (16.7) | ||||
| Chi-square = 77.035 | |||||||
| P–value = 0.001 (significant at 95%) | |||||||
The relationship between the region/site distribution and the specific diagnoses of the tumors was statistically significant. In keeping with the overall site distribution, the most common tumors, which were lipomas, were more common in the back/shoulder region with 34.8% (127/364), while fibrolipomas occurred more frequently in the lower limb with 28.6% (12/42). Three other tumors occurred two times or more, namely spindle cell lipoma, which occurred five times (twice each in the neck and thigh and once in the back); pleomorphic lipoma, which occurred once each in the scalp and right thigh; and angiolipoma, which occurred once each in the perineum and right arm (Table 5 and Figure 5).
Table 5. Distribution of benign lipomatous tumors according to the region/site of occurrence and diagnosis.
| Region | Site | Diagnoses | |||||||
| Chondrolipoma | Fibrolipoma | Spindle cell lipoma | Lipoma | Pleomorphic lipoma | Angiolipoma | Osteolipoma | Intramuscular lipoma | ||
| Head and neck | Face | 0 (0.0) | 4 (9.5) | 0 (0.0) | 18 (4.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Neck | 0 (0.0) | 3 (7.1) | 2 (40.0) | 19 (5.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Scalp | 0 (0.0) | 2 (4.8) | 0 (0.0) | 12 (3.3) | 1 (50.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Eye | 0 (0.0) | 0 (0.0) | 0 (0.0) | 4(1.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Ear | 0 (0.0) | 1 (2.4) | 0 (0.0) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Lower lip | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Back/Shoulder | Back | 0 (0.0) | 2 (4.8) | 1 (20.0) | 75 (20.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Shoulder | 0 (0.0) | 3 (7.1) | 0 (0.0) | 42 (11.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Scapular | 0 (0.0) | 0 (0.0) | 0 (0.0) | 10 (2.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Perineum/Pelvis | Perineum | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (0.8) | 0 (0.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) |
| Vulva | 0 (0.0) | 1 (2.4) | 0 (0.0) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Lower limb | Gluteus | 0 (0.0) | 2 (4.8) | 0 (0.0) | 16 (4.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Leg | 0 (0.0) | 0 (0.0) | 0 (0.0) | 8 (2.2) | 0 (0.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) | |
| Thigh | 0 (0.0) | 10 (23.8) | 2 (40.0) | 35 (9.6) | 1 (50.0) | 0 (0.0) | 0 (0.0) | 1 (100.0) | |
| Anterior trunk | Chest | 0 (0.0) | 0 (0.0) | 0 (0.0) | 19 (5.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Anterior abdominal wall | 0 (0.0) | 1 (2.4) | 0 (0.0) | 9 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Breast | 0 (0.0) | 0 (0.0) | 0 (0.0) | 12 (3.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Arm/Axilla | Arm | 0 (0.0) | 5 (11.9) | 0 (0.0) | 37 (10.2) | 0 (0.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) |
| Axilla | 0 (0.0) | 1 (2.4) | 0 (0.0) | 11 (3.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Abdominal/Pelvic cavities | Omentum | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Ovary | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Multiple sites | Multiple sites | 0 (0.0) | 2 (4.8) | 0 (0.0) | 5 (1.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Not specified | Not specified | 0 (0.0) | 5 (11.9) | 0 (0.0) | 24 (6.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Total n(%) | 1 (100.0) | 42 (100.0) | 5 (100.0) | 364 (100) | 2 (100.0) | 2 (100.0) | 1 (100.0) | 1 (100.0) | |
| Chi-square = 79.039 | |||||||||
| P–value = 0.023 (significant at 95%) | |||||||||
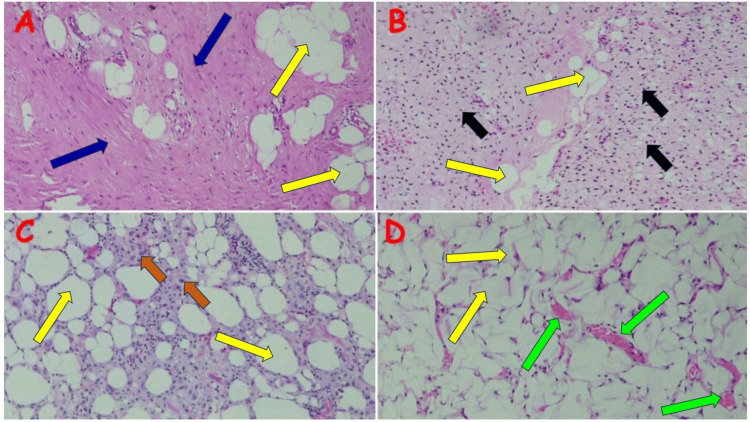
Figure 5. Fibrolipoma and other lipoma variants.
(A) Giant fibrolipoma in the right thigh of a 45-year-old male; note the lobules of mature adipocytes (yellow arrows) traversed by vascularized fibrous tissue bands (blue arrows). (B) Spindle cell lipoma in the right thigh of a 35-year-old female; note the admixture of mature adipocytes (yellow arrows) and spindle-shaped cells (black arrows) set in the fibromyxoid stroma. (C) Pleomorphic lipoma on the scalp of a 36-year-old male; note the variably sized adipocytes (yellow arrows) set in the hyalinized spindle cell stroma, admixed with numerous floret cells (brown arrows). (D) Angiolipoma in the right arm of a 19-year-old female; note the admixture of mature adipocytes (yellow arrows) and often ectatic capillary-type blood vessels, which occasionally contain bright pink fibrin (green arrows).
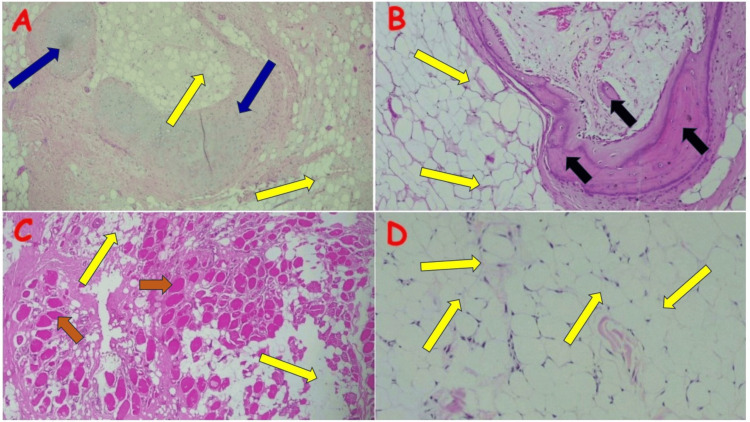
The rare lipoma variants diagnosed tended to also occur in unusual locations. Chondrolipoma occurred in the lower lip of a 50-year-old male [10]. The only osteolipoma diagnosed was in the right foot of a 19-year-old male, while the intramuscular lipoma occurred in the left thigh of a 37-year-old male. The conventional lipoma also occurred at unusual sites, including the conjunctiva, ovary, lower lip, and right middle finger (Figure 6).
Figure 6. Other rare lipoma variants and conventional lipoma .
(A) Chondrolipoma in the lower lip of a 50-year-old male [10]; note the mature adipose tissue (yellow arrows) separated by faintly basophilic fibrous septae admixed with foci of metaplastic hyaline cartilage (blue arrows). (B) Osteolipoma in the right foot of a 19-year-old male; note the lobules of mature adipocytes (yellow arrows) admixed with and completely surrounding the trabeculae of mature bone (black arrows). (C) Intramuscular lipoma in the left thigh of a 37-year-old male; note the mature adipocytes (yellow arrows) interdigitating with skeletal muscle fibers (brown arrows). (D) Conventional lipoma on the right conjunctiva of a 40-year-old male; note the lobules of mature adipocytes (yellow arrows) demarcated into lobules by delicate fibrous strands.
Image A: Reproduced with permission from Ezike KN, Okwudire-Ejeh IA, Essien LO, Chukwu FO [10]
Discussion
Benign lipomatous tumors are mesenchymal tumors, composed of mature, histologically benign adipocytes, occasionally admixed with other mesenchymal elements such as fibroblasts, blood vessels, chondroblasts, smooth muscle, skeletal muscles, and other heterologous elements [4,8]. They are, however, histogenetically distinct from entities like lipomatous mixed tumors and mature cystic teratoma, which are skin adnexal and germ cell tumors, respectively, but exhibit significant adipocytic differentiation [17,18]. The pathophysiology of benign lipomatous tumors is not fully understood. However, two theories, including the genetic and the trauma pathogenesis theories, are postulated. The most common genetic abnormality seen in these tumors is the rearrangement of chromosome 12, which contains the DNA damage-inducible transcript 3 (DDIT3) gene, whose protein family, enhancer binding protein, is involved in the growth arrest of fat cells [19]. Etiologically, an association has been made between trauma and lipoma formation with the action of growth factors and cytokines released in response implicated in its pathogenesis; however, this has not been unequivocally demonstrated [8]. Neither the demonstrated genetic abnormalities, including chromosome 12 rearrangements, nor the trauma pathogenesis theory have any significant association with the sex or age of patients who develop lipomas or the tumor site, size, or depth [20].
There is no consensus on the overall sex incidence of benign lipomatous tumors. While some authorities and researchers say it is more common in males, others report an equal incidence, and some report a female preponderance [8, 9,20,21]. Our study with a male-to-female ratio of 1:1.5 aligns with the female preponderance. Within different compartments, however, variations in sex incidence have been reported. For example, according to many studies, head and neck lipomas are more prevalent in males, and similar to these studies, our study showed a higher prevalence in males, with a ratio of 1.5:1 [22-25].
Benign lipomatous tumors occur in all age groups and demographics but are more common in persons aged 30-60 years [1,2,9,16,24-26]. Our study, with findings from 81% of cases within this age range, did not buck this trend. These tumors, however, seem to peak at an earlier age in Nigerians, in keeping with an earlier Nigerian study by Dauda et al. [9], unlike studies in Indian and Swedish populations that showed a peak incidence in the 40-60-year range, respectively [26,27].
Giant benign lipomatous tumors (greater than 10 cm in widest diameter) are rare, and the vast majority of benign lipomatous tumors are considered small to medium-sized, measuring less than 6 cm in widest diameter [1,2,27]. Our study showed a relatively high proportion of giant lipomas (16%) in contrast with the 0.01% and 0.07% reported by Rydholm et al. and Mello et al., respectively [27,28]. The reasons for this are unclear, however, our cases occurred almost exclusively in a Black African population, while the two studies referenced above were in Latin American and European populations, respectively. A racial or genetic predisposition to giant lipomas may, therefore, be a factor in our study population. It is also possible that patients in our study tended to ignore the swelling until it reached a larger size [29]. Further research is required to test this hypothesis.
The relationship between the size of these tumors and the sex of the patients is not statistically significant, and our findings corroborate the same [27]. In terms of size and site of the tumors, our series showed that the back and shoulders had larger tumors than the head and neck region, findings similar to other studies both within and outside Nigeria [9,27].
The differential diagnoses of benign lipomatous tumors depend on site and depth and range from sebaceous cysts and abscesses in superficial locations to liposarcoma, including atypical lipomatous tumors, dermatofibroma, dermatofibrosarcoma protuberance (DFSP), neurofibroma, etc., in subfascial and deep locations [1,8]. Conversely, benign lipomatous tumors should be considered in the differential diagnosis of all superficial masses and masses located in specific compartments of the body.
Limitations
The major limitation of the study was that it was hospital-based and therefore analyzed only the cases that underwent surgical excision. As a result, the findings may not reflect the true prevalence and incidence of benign lipomatous tumors within the population. Another limitation is the retrospective nature of the study design, which was associated with incomplete data, especially tumor location, with possible distortion of the location statistics.
Conclusions
Our study demonstrates that the clinical and morphological features of benign lipomatous features in Nigerians are generally similar to findings reported from other regions of the world. A notable finding, however, was the significantly higher proportion of giant benign lipomatous tumors when compared to studies from these other regions. Multicenter studies are required to corroborate this finding and determine whether or not a racial or genetic predisposition to giant lipomas exists in our population. Furthermore, surgical excision of these tumors should be encouraged not only for cosmetic reasons and/or pressure symptoms but also because of the need to rule out malignant differential diagnoses.
Acknowledgments
The authors wish to thank Mr. Alex Adeyemo, data analyst and statistician with the University of Abuja, Gwagwalada, Abuja, Nigeria, for his assistance with the data analysis. All relevant data are available upon reasonable request.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Kevin N. Ezike, Ijeoma A. Okwudire-Ejeh, Bamnan Dallang
Acquisition, analysis, or interpretation of data: Kevin N. Ezike, Ijeoma A. Okwudire-Ejeh, Sule I. Ahmed, Iliya K. Salu, Michael E. Aghahowa, Umar M. Umar
Drafting of the manuscript: Kevin N. Ezike, Ijeoma A. Okwudire-Ejeh, Bamnan Dallang
Critical review of the manuscript for important intellectual content: Kevin N. Ezike, Ijeoma A. Okwudire-Ejeh, Sule I. Ahmed, Iliya K. Salu, Michael E. Aghahowa, Umar M. Umar
Human Ethics
Consent was obtained or waived by all participants in this study. Medical Ethics Committee of Asokoro District Hospital, Federal Capital Territory Administration (FCTA), Abuja issued approval FCT/HHSS/HMB/ADH/139/23
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Enzinger and Weiss’s Soft Tissue Tumors. New York City: Elsevier; 2007. General considerations; pp. 1–15. [Google Scholar]
- 2.Fletcher CDM. Diagnostic Histopathology of Tumors. Vol. 2. Philadelphia, PA: Elsevier Saunders; 2015. Tumors of soft tissue; pp. 1796–1870. [Google Scholar]
- 3.Horvai A. Robbins and Cotran Pathologic Basis of Disease. Philadelphia, PA: Elsevier Saunders; 2015. Bones, joints, and soft tissue tumors; pp. 1180–1226. [Google Scholar]
- 4.Enzinger and Weiss’s Soft Tissue Tumors. New York City: Elsevier; 2007. Benign lipomatous tumors; pp. 429–477. [Google Scholar]
- 5.Osteolipoma: a rare lesion in the oral cavity. Castilho RM, Squarize CH, Nunes FD, Pinto Júnior DS. Br J Oral Maxillofac Surg. 2004;42:363–364. doi: 10.1016/j.bjoms.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Chondrolipoma: report of a rare intra oral variant with review of histiogenetic concepts. Raj V, Dwivedi N, Sah K, Chandra S. J Oral Maxillofac Pathol. 2014;18:276–280. doi: 10.4103/0973-029X.140785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oral soft tissue lipomas: a case series. Bandéca MC, de Pádua JM, Nadalin MR, Ozório JE, Silva-Sousa YT, da Cruz Perez DE. https://www.cda-adc.ca/jcda/vol-73/issue-5/431.pdf. J Can Dent Assoc. 2007;73:431–434. [PubMed] [Google Scholar]
- 8.Lipomas. [ Feb; 2023 ]. 2022. https://emedicine.medscape.com/article/191233 https://emedicine.medscape.com/article/191233
- 9.A critical review of the pattern of lipomas at Jos University Teaching Hospital. Dauda MA, Kokong DD, Yakubu D, Akpa PO, Ochigbo AJ, Ewenreuzo LC, Ojo EO. https://www.ajol.info/index.php/jjm/article/view/143912/133617 Jos J Med. 2015;9:15–18. [Google Scholar]
- 10.Chondrolipoma of the lip: a case report from a secondary health care center in Nigeria. Ezike KN, Okwudire-Ejeh IA, Essien LO, Chukwu FO. Jos J Med. 2020;11:101147. [Google Scholar]
- 11.Buccal soft tissue lipoma in an adult Nigerian: a case report and literature review. Adoga AA, Nimkur TL, Manasseh AN, Echejoh GO. J Med Case Rep. 2008;2:382. doi: 10.1186/1752-1947-2-382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giant lipomas. A report of two cases. Emegoakor CD, Echezona CN, Onwukamuche ME, Nzeakor HO. https://journals.lww.com/njgp/fulltext/2017/15020/giant_lipomas__a_report_of_two_cases.6.aspx Niger J Gen Pract. 2017;15:46–49. [Google Scholar]
- 13.Lipoma of the breast: an uncommon occurrence. Nwashilli NJ, Ugiagbe EE. https://go.gale.com/ps/i.do?id=GALE%7CA477199825&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=11165898&p=HRCA&sw=w&userGroupName=anon%7E5ed1481c&aty=open-web-entry#:~:text=Lipomas%20rarely%20occur%20in%20the,excision%20on%20histology%20as%20lipoma. Niger J Surg Sci. 2016;26:12–14. [Google Scholar]
- 14.Soft tissue general WHO classification. [ Mar; 2024 ]. 2022. https://www.pathologyoutlines.com/topic/softtissuewhoclassification.html. https://www.pathologyoutlines.com/topic/softtissuewhoclassification.html.
- 15.Review of large deep lipomatous tumours. Serpell JW, Chen RY. ANZ J Surg. 2007;77:524–529. doi: 10.1111/j.1445-2197.2007.04042.x. [DOI] [PubMed] [Google Scholar]
- 16.Charifa A, Azmat CE, Badri T. Treasure Island, FL: StatPearls [Internet], StatPearls Publishing; [ Mar; 2024 ]. 2024. Lipoma Pathology. [PubMed] [Google Scholar]
- 17.World Health Organization. WHO Classification of Skin Tumours. Lyon, France: IARC Publications; 2018. Appendageal tumours; pp. 153–222. [Google Scholar]
- 18.An ovarian mature cystic teratoma evolving in squamous cell carcinoma: a case report and review of the literature. Goudeli C, Varytimiadi A, Koufopoulos N, Syrios J, Terzakis E. Gynecol Oncol Rep. 2017;19:27–30. doi: 10.1016/j.gore.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Human translocation liposarcoma-CCAAT/enhancer binding protein (C/EBP) homologous protein (TLS-CHOP) oncoprotein prevents adipocyte differentiation by directly interfering with C/EBPbeta function. Adelmant G, Gilbert JD, Freytag SO. J Biol Chem. 1998;273:15574–15581. doi: 10.1074/jbc.273.25.15574. [DOI] [PubMed] [Google Scholar]
- 20.Comparison of chromosomal patterns with clinical features in 165 lipomas: a report of the CHAMP study group. Willén H, Akerman M, Dal Cin P, et al. Cancer Genet Cytogenet. 1998;102:46–49. doi: 10.1016/s0165-4608(97)00292-6. [DOI] [PubMed] [Google Scholar]
- 21.Cutaneous lipomas. [ Mar; 2024 ]. 2020. https://emedicine.medscape.com/article/1057855-overview#a6 https://emedicine.medscape.com/article/1057855-overview#a6
- 22.Lipomas of the head and neck: presentation variability and diagnostic work-up. El-Monem MH, Gaafar AH, Magdy EA. J Laryngol Otol. 2006;120:47–55. doi: 10.1017/S0022215105004597. [DOI] [PubMed] [Google Scholar]
- 23.Clinico-surgical characteristics of head and neck lipomas. Kim JS, Choi MS, Lee SJ, Park BC. Dermatol Surg. 2018;44:893–895. doi: 10.1097/DSS.0000000000001395. [DOI] [PubMed] [Google Scholar]
- 24.A clinicopathological study of lipomas of the head and neck. Ndukwe KC, Ugboko VI, Somotun G, Adebiyi KE, Fatusi OA. Nig J SurgRes. 2003;5:12–17. [Google Scholar]
- 25.Head and neck lipomas: a clinicopathologic analysis of 36 cases. Aregbesola SB, Famurewa BA, Soyele OO, Komolafe AO. https://www.researchgate.net/publication/337416220_Head_and_neck_lipomas_A_clinicopathologic_analysis_of_36_cases J Cancer Res Exp Oncol. 2019;11:1–5. [Google Scholar]
- 26.Epidemiology of subcutaneous lipomas. Sarla GS. Online Turk J Health Sci. 2019;4:350–359. [Google Scholar]
- 27.Size, site and clinical incidence of lipoma. Factors in the differential diagnosis of lipoma and sarcoma. Rydholm A, Berg NO. Acta Orthop Scand. 1983;54:929–934. doi: 10.3109/17453678308992936. [DOI] [PubMed] [Google Scholar]
- 28.Giant lipomas: a 14-case series. Mello DF, Manica MZ, Júnior AH. Rev Bras Cir Plást. 2015;30:33–37. [Google Scholar]
- 29.Giant lipoma of the scalp in Aba, South East Nigeria: a case report. Eleweke N. https://www.researchgate.net/publication/355293677_Giant_Lipoma_of_the_Scalp_in_Aba_South_East_Nigeria_A_Case_Report Open Access Lib J. 2021;8:1–6. [Google Scholar]