Abstract
Background and Objectives
Social well-being of older adults living in low-income housing was disproportionately affected by the coronavirus disease 2019 pandemic. We explored low-income residents’ experiences of social isolation and loneliness and strategies to remain socially connected during the pandemic.
Research Design and Methods
As part of a larger, 3-phase user-centered design study, we conducted a qualitative study using focus groups to gain insights into social isolation experiences and the role of information and communication technologies (ICTs), including smart speakers, in social connectedness (N = 25, 76% African American). We also collected survey data to describe social isolation, loneliness, and current ICT use in the sample. Participants included both smart speaker users and nonusers.
Results
Experiences of social isolation and loneliness varied by participants’ sociodemographic characteristics and previous experiences with smart speakers. Qualitative analysis showed participants demonstrated coping strategies developed during the pandemic to adapt to new norms of connecting with others, including technology-enabled social interactions. Participants expressed a strong desire to build community together in their facilities and highlighted the potential role of smart speakers in making meaningful social connections, encompassing safety checks to have a means for emergencies, and providing a virtual companion. Access, digital literacy, training, security, and privacy issues were discussed as factors affecting their adoption of new ICT for enhanced social connectedness.
Discussion and Implications
This study highlights the importance of understanding the unique social isolation experience, demographics, and social determinants of health of low-income residents to develop ICT-based interventions for social connectedness.
Keywords: Disparities (health, racial), Focus groups, Information technology, Social well-being
In early 2020, the coronavirus disease 2019 (COVID-19) pandemic led to abrupt disruptions in our daily lives. National lockdowns were implemented as a public health measure to curtail the spread of the new virus and protect community members from the severe impact of the disease. However, lockdowns brought unintended, negative health outcomes to many older adults, especially regarding social isolation and activity restrictions (Fuller & Huseth-Zosel, 2021; Heid et al., 2021). Many older adults living in congregate housing experienced difficulties adapting to a sudden loss of social interactions due to visitor restriction policies, the cessation of community events to meet physical distancing guidelines and specific sociodemographic and contextual factors (Sargent et al., 2022; Winship et al., 2022).
Social connectedness in older adulthood is a critical factor in determining quality of life and longevity (National Academies of Sciences, Engineering, and Medicine [NASEM], 2020). Social isolation, as a structural indicator of social connectedness, refers to a “pervasive lack of social contact or communication, participation in social activities, or having a confidant” (Holt-Lunstad et al., 2015, p. 229), whereas loneliness, as a functional indicator, pertains to a subjective feeling resulting from a perceived deficit in quantity or quality of social relationships (NASEM, 2020). Individuals lacking social connections can feel lonely, but social isolation does not always lead to feelings of loneliness. Social isolation and loneliness are associated with an increased risk of adverse health outcomes, such as cardiovascular diseases and mortality (Holt-Lunstad et al., 2015; Hu et al., 2021; NASEM, 2020). Yet, an estimated 7.7 million older adults in the United States are affected by social isolation (Cudjoe et al., 2020) due to retirement, cognitive and physical disabilities, loss of significant others, and changes in living situations, although the estimates vary depending on the definition and measurement (Nicholson et al., 2020). Experiences of loneliness are also prevalent among older adults, with an estimated 17%–57% of Americans aged 65 and older reporting loneliness (Donovan et al., 2017; Musich et al., 2015; Perissinotto et al., 2012).
The Richmond Health and Wellness Program (RHWP), on which the current study was based, is an interprofessional care model that provides care coordination and health risk assessment to address the unmet needs of older adults living alone in low-income housing (Parsons et al., 2019). These apartment buildings are subsidized by the U.S. Department of Housing and Urban (HUD) and other sectors. The RHWP operates weekly clinics in several low-income housing buildings. The program enrollees are primarily African American (70%), have comorbidities (50%), have low health literacy (70%), and report issues of poverty and adverse social determinants of health, such as food insecurity and high emergency department utilization rates (Coe et al., 2018; Diallo et al., 2020; Sargent et al., 2022). Low-income residents are at increased risk for social isolation (Diallo et al., 2020) because they often have chronic disease burdens, disabilities, and lack of transportation, social and financial capital, and smartphone and Internet access (Parsons et al., 2019; Winship et al., 2022). These factors can significantly affect the ability of individuals to engage in meaningful social interactions and maintain them over time. Importantly, the varied backgrounds and experiences of low-income residents resulted in a diversity of responses to pandemic-induced social isolation.
A wide body of research demonstrates that information and communication technologies (ICTs) have the potential to decrease loneliness and reduce social isolation (Cotten et al., 2013; Poscia et al., 2018; Sims et al., 2017). However, recent reviews reported inconsistent findings as to whether ICTs are efficacious in increasing social connectedness and mitigating loneliness among older adults (Ibarra et al., 2020; Petersen et al., 2023). Many of the studies included in these reviews focused on facilitating interactions between older adults and their family and friends and were dependent on existing social capital, which was not readily available to the majority of our low-income residents pre- and midpandemic. Recently, there has been increasing interest in the use of an automated conversational agent in interventions for older adults. A smart speaker is an internet-enabled output device controlled by spoken commands and is capable of streaming audio content, relaying information, and communicating with other devices. Compared to conventional interfaces many digital tools rely on (e.g., a keyboard or mouse), smart speakers may provide a more effective user interface for older adults by allowing voice interactions with a conversational agent. This feature can be beneficial to those with a lack of social capital, vision impairments, physical disabilities, or dexterity issues. Evidence suggests that older adults held a positive view toward smart speakers and actively interacted with a virtual agent by asking practical questions or managing daily tasks—whether they live in low-income housing (Chung et al., 2021) or not (Kowalski et al., 2019; Pradhan et al., 2019). Smart speakers with a conversational agent hold promise to improve the experience of social connection and engagement and mitigate loneliness among older adults by giving a sense that they are not alone, providing a communication tool, and increasing social bonds (Corbett et al., 2021; Jones et al., 2021; O’Brien et al., 2022; Reis et al., 2017).
This is part of an iterative user-centered design study (Voice2Connect) to examine how smart speaker technologies can support the needs for social connectedness among low-income residents. The COVID-19 pandemic has accelerated digital technology integration into the lives of older adults. ICTs have become crucial for getting information, keeping in contact with others, sharing experiences with people one cannot see in person, and seeking support and healthcare. Meanwhile, rapid digital transformation has revealed digital inequities between the rich and poor, the privileged and disadvantaged, and the old and young (Litchfield et al., 2021). During the pandemic, older adults living alone in low-income communities were less likely to meet their information and communication needs due to challenges with digital access, lack of trusted information sources, low levels of literacy or internet skills, and limited technology support (Litchfield et al., 2021; van Deursen, 2020). Therefore, we report the findings from the first phase focus groups, where we explored low-income residents’ experience of social isolation and loneliness and what strategies they sought to remain socially connected. This phase of data collection focused on improving our understanding of low-income residents’ perceptions of smart speaker-based approaches to improve social connectedness. The participants’ feedback described here encompasses their experiences and expectations towards the technology’s potential in fostering social connections. Our research questions were:
How were social isolation and loneliness experienced during the pandemic by older adults living alone in low-income housing?
What strategies did they use to remain socially connected?
What was the role of technology (especially smart speakers) in social connectedness?
Design and Methods
Study Design
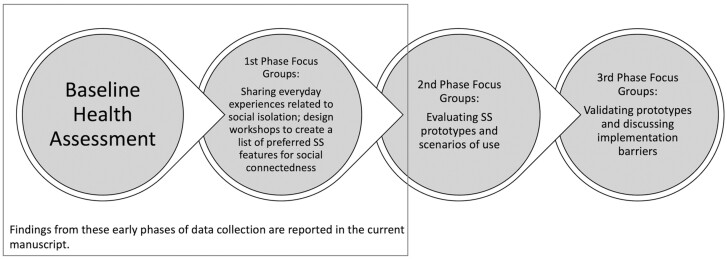
This is a qualitative study with survey data collected to describe the sample, but not used systematically in analysis. This study is part of a larger, 3-phase user-centered design project (Voice2Connect) to develop low-fidelity prototypes and scenarios of use of smart speaker-based functions that can promote social connectedness in low-income residents living alone (Figure 1). The parent study consisted of three phases. In Phase 1, we held five focus groups to explore obstacles to establishing or maintaining social contacts and engagements, barriers to staying connected with others, ICT integration into daily life, and overall perception of smart speakers followed by brainstorming activities to identify a set of smart speaker-based tasks perceived as useful for improving social connectedness. The feedback from the first phase was integrated into the development of prototypes and related scenarios of use. We brought these prototype ideas to Phase 2 focus groups (total groups, N = 5) and sought overall perceptions of the proposed designs of smart speaker-based functions for social connectedness, suggestions for improving the system functionalities, and potential privacy concerns. Based on participant feedback, we refined the details of the prototype scenarios and presented them at Phase 3 focus groups (total groups, N = 4) to validate the design concept and elicit suggestions for future system implementation in the low-income senior housing setting. This paper reports primarily the thematic analysis findings of focus groups in the first phase.
Figure 1.
Data collection process of the parent study. SS = smart speaker.
Study Setting
Our study sites included three facilities in Richmond, VA, that house older adults living on a limited income. All study procedures were approved by the Institutional Review Board at Virginia Commonwealth University (VCU), and all participants provided informed consent.
Participants
We primarily recruited study participants using a list of wellness visit participants with the RHWP due to the COVID-19 precautions at study sites at the time of recruitment (March–July 2021). The housing representatives in three housing facilities (A, B, and C) posted study flyers on the community bulletin boards. In addition to telephone recruitment of RHWP participants, we visited Facility A for in-person recruitment when the RHWP clinic was held, we maintained a weekly study booth near the entrance of Facility B for a month, and we held an information session in the courtyard of Facility C. Detailed descriptions of recruitment procedures are reported elsewhere (Demiris et al., 2022).
We engaged two groups of study participants—smart speaker users and nonusers. We recruited “user” participants (at least 1 month of smart speaker use) from Facility A, where smart speakers had been deployed in some apartments, and recruited nonuser participants from all buildings. Eligibility criteria included 55 years or older, and having the ability to speak and read English. Exclusion criteria were as follows: planning to move out of the facility 6 months after consenting, score ≤8 on a short version of the Montreal Cognitive Assessment (mini MoCA, www.mocatest.org/paper), severe visual and hearing impairment requiring assistance in participating in focus groups where interactive audiovisual materials were used for technology design workshops, and being diagnosed with a terminal illness due to the requirement for long-term enrollment in an iterative study. However, none of the screened participants met these exclusion criteria. Participants received a $20 gift card at each visit.
Study Procedures
The screening (Section 1 of Supplementary Material) and baseline surveys were conducted via telephone by trained research assistants (RAs). Once the individual passed screening questions, we scheduled a subsequent phone visit to screen their cognitive function using the mini MoCA. If they were found eligible for the study, the phone visit continued with the baseline questionnaires. The current manuscript is based on some of the findings from the baseline health assessment and the first phase focus group sessions (Figure 1).
Quantitative Data Collection
Because the phone-based survey was the only option for data collection during the pandemic, we chose a brief version of instruments, if available, to decrease participant burden. We used an online tool (REDCap, Nashville, TN) to enter questionnaire data. The phone-based survey assessed demographics, ICT ownership and experience, social well-being (social isolation, loneliness, satisfaction with current social interaction levels; Supplementary Material, Section 2), and other health-related variables. This manuscript only reports on demographics, social well-being, and technology experience questionnaire data.
Focus Group Interviews
After the baseline assessment, we invited participants to attend the first phase focus group sessions between April and July 2021. Of those enrolled, 25 participated. We limited the number of participants in each group to not exceed six people to facilitate brainstorming of technology ideas and more intimate sharing (Halcomb et al., 2007). We stratified focus groups by housing facility for participant convenience, as most participants had limited transportation access. However, due to the facility-mandated COVID-19 physical distancing rules, we changed the meeting location (except for Group #5) from a community room in each facility to a specific location on the university campus. We provided a van ride to those who did not own a car. We used a semistructured interview guide (Supplementary Material, Section 3) developed by the team. Two RAs (R. E. Wood, N. Mansion) trained in qualitative methods facilitated discussions. Focus group sessions lasted for 1–1.5 hr.
Data Analysis
We conducted an inductive thematic analysis (Boyatzis, 1998; Thomas, 2006) to analyze the qualitative data. Audio recordings of the interviews were professionally transcribed and imported into Atlas.ti software (Version 9) for coding. We selected this software based on its extensive functionality for organizing, coding, linking, and memoing that facilitated efficient coding, deeper understanding, and theme development. Three researchers (J. Chung, T. Gendron, and J. Winship) began data analysis by independently reading the transcripts and highlighting words/phrases representing what was being said. The coding team met to discuss “precodes,” which each researcher identified as preliminary themes related to participants’ lived experience of social isolation, loneliness, and rapid digital transformation, then developed the initial codebook consisting of definitions of codes and related subcategories through team discussion. The team met regularly to discuss coding, revise the codebook every time a particular code was identified, and reconcile any discrepancies. Finally, through an iterative consensual process, the team grouped the codes into themes. To ensure rigor and trustworthiness (Lincoln & Guba, 1985), the qualitative analysis process involved four techniques: the use of three coders and consensus achieved with coding for dependability; detailed descriptions of the study sample and the use of quotes to support themes for transferability; peer debriefing by providing written and oral records of identified themes to obtain an external check on the research process, findings, and interpretations against the raw data for credibility; and an audit trail and reflexivity journaling to capture thought processes and thematic development for replicability (Nowell et al., 2017; Thorne, 2016).
Results
Participant Characteristics
Five focus groups involved 25 older adults (Table 1). Table 2 summarizes the participant characteristics. The average age of the participants was 69.8 years old; 44% were female. More than two-thirds of the participants were Black/African American; 68% had a high school education or less.
Table 1.
First Phase Focus Groups
| Focus Group # | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Housing facility | A | A | B | A | C |
| Number of participants | 6 | 5 | 6 | 5 | 3 |
| Current smart speaker user | Yes | Yes | No | No | No |
Table 2.
Participant Characteristics
| Variable | All focus group participants (N = 25) | Smart speaker users (n = 12) | Smart speaker nonusers (n = 13) |
|---|---|---|---|
| n (%) or Mean ± SD | |||
| Age | 69.8 ± 6.0 (range: 61–86) | 68.9 ± 5.8 (range: 60–80) | 70.7 ± 6.4 (range: 61–86) |
| Female | 11 (44) | 7 (58.4) | 4 (30.8) |
| Race | |||
| Black/African American | 19 (76) | 7 (58.4) | 12 (92.3) |
| White | 5 (20) | 4 (33.3) | 1 (7.7) |
| Other | 1 (4) | 1 (8.3) | 0 |
| Education | |||
| Less than high school | 5 (20) | 1 (8.3) | 4 (30.8) |
| High school diploma/GED | 12 (48) | 6 (50.0) | 6 (46.2) |
| Some college | 6 (24) | 4 (33.3) | 2 (15.4) |
| Bachelor’s degree | 1 (4) | 1 (8.3) | 0 |
| Graduate or professional degree | 1 (4) | 0 (0) | 1 (7.7) |
| Housing facility | |||
| A | 17 (68) | 12 (100) | 5 (38.5) |
| B | 5 (20) | 0 | 5 (38.5) |
| C | 3 (12) | 0 | 3 (23.1) |
| Living at the current apartment (years) | 5.8 ± 3.4 | 6.2 ± 5.8 | 5.5 ± 4.0 |
| Health characteristics | |||
| Visual impairment | 6 (24) | 1 (8.3) | 5 (38.5) |
| Hearing impairment | 1 (4) | 0 | 1 (7.7) |
| Social networks, loneliness, and satisfaction | |||
| Lubben Social Network Scale-6 items (LSNS-6) | 14.8 ± 6.6 | 15.7 ± 5.3 | 13.9 ± 7.8 |
| Social isolation (LSNS-6 < 12) | 9 (36) | 3 (25) | 6 (46.2) |
| UCLA Loneliness Scale Short Form | 4.8 ± 1.9 | 5.3 ± 1.4 | 4.4 ± 2.2 |
| Loneliness (UCLA-3 ≥ 6) | 9 (36) | 6 (50) | 3 (23.1) |
| Participation in any organizations, religious groups or committees, yes | 11 (44) | 6 (50) | 5 (38.5) |
| Satisfaction with the current social relationships | |||
| Very dissatisfied | 9 (36) | 5 (41.7) | 4 (30.8) |
| Somewhat dissatisfied | 3 (12) | 2 (16.7) | 1 (7.7) |
| Satisfied | 13 (52) | 5 (41.7) | 8 (61.5) |
| Technology use experience | |||
| Smartphone ownership | 18 (72) | 12 (100) | 6 (46.2) |
| Laptop/computer ownership | 12 (48) | 9 (75) | 3 (23.1) |
| Internet use experience | |||
| Yes | 14 (56) | 10 (83.3) | 4 (30.8) |
| Never | 11 (44) | 2 (16.7) | 9 (69.2) |
| Daily internet users | 12 (48) | 8 (66.7) | 4 (30.8) |
| Smart speaker use (users only) | |||
| Smart speaker use period (months) | 13.9 ± 4.8 (range: 11–24) | ||
| Smart speaker use frequency | |||
| Daily | 6 (24) | ||
| Every few days | 2 (8) | ||
| A few times a month | 1 (4) | ||
| Once a month or less often | 3 (12) | ||
| Smart speaker usage, by command | |||
| Music | 12 (100) | ||
| Weather | 9 (75) | ||
| Information or learning facts | 8 (66.7) | ||
| Alarm/Reminder/Timer | 6 (50.0) | ||
| News | 5 (41.7) | ||
| Games | 3 (25) | ||
| Audio books | 3 (25) | ||
| Audio (e.g., Bluetooth speaker) | 2 (13.3) | ||
| Music trivia | 2 (13.3) | ||
| Shopping | 2 (13.3) | ||
| Inspirational stories | 1 (8.3) | ||
| Connecting to someone | 0 | ||
Note: GED = General Educational Development, N = the total number of participants, n = the number of participants in each group, SD = Standard Deviation, UCLA = University of California at Los Angeles.
Of the participants, 36% reported social isolation and 36% reported loneliness; 44% reported their participation in organizations, religious groups, or committees. Participants reported varied levels of satisfaction with the current level of social interactions. The percentage of smartphone ownership was 72%. However, the smart speaker nonuser group reported a lower percentage in all technology ownership and internet use than users. Twelve participants (48%) owned a smart speaker, and they had been using the device for about 14 months on average. The frequency of smart speaker use varied, ranging from daily (24%) to once a month or less often (12%). Smart speaker use was limited to simple tasks or commands, such as music, weather, information, news, and alarm or reminders; none reported using smart speakers for connecting to another smart speaker user.
Qualitative Findings
Varied impact of COVID-19 on social connectedness
Participants discussed the experience of social isolation and loneliness in the context of the pandemic. Participants across groups agreed there were severe disruptions in social activities, such as stopping weekly wellness clinics at the building, community events, education sessions, or church services, leading to frustrations. One person said, “I felt isolated with just the average things that you would normally do, like go to a movie, go to a restaurant. There was very little to do, so you relied on the phone” (FGI#2). They lost contact with significant others due to restrictions and social distancing rules imposed by the housing facility.
Participants expressed a desire for more social connections. Some participants who maintained contact with others preferred in-person meetings over virtual visits. Another shared her emotional challenge related to missed opportunities to see her grandchildren grow: “They’re little. They’re growing up. I’m missing their first step, their first word, their lost tooth from my five-year-old. And for me that’s been really, really hard. I don’t care that much about other things, but that’s been really hard” (FGI#3). However, we observed differences in participant perspectives of the pandemic impact on the level of social interactions or loneliness. Individuals who had family to check in expressed their satisfaction with the current level of connections even though the interactions were primarily virtual.
Concerns about foreseen risks of social isolation in the context of living alone
Older adults discussed experiences of social isolation in the nonpandemic context as well. All of our participants lived alone in low-income housing (average duration of living at the current facility = 5.8 years), and not everyone had family members nearby or that they could contact remotely. Participants were worried about foreseen health risks of being alone and expressed concerns about their fellow residents who are isolated or who do not engage with others. There was a strong sense of building a community together and making their living environment more lively through various activities to ensure the safety of others, for example, a “get-to-know-me session” (FGI#1), messages from the office or fellow residents, and connecting people with community resources and social opportunities. More importantly, people voiced a strong need to check in on each other:
… And then my floor, on our side of the floor, what we did was we all kept an eye on everybody at our end. And if you didn’t see this person for two or three days, you might knock because there’s no place to go. (FGI#2)
Many participants felt the need for tools or interventions that mitigate the risk of living alone, and they voiced the need for using smart speakers for identifying at-risk individuals to prevent adverse health outcomes, such as falling. Overall, participants across groups agreed the most important reason for adopting smart speakers would be to get help in emergency situations. Smart speaker users expressed their frustration about the inability to receive emergency assistance from a smart speaker-based system deployed in their facility, which diverged from their original expectations regarding its role.
Social network selectivity
Some participants expressed their views about the intentional pursuit of keeping a small network and purposeful slowdown in social life. One person related this perception to his aging experience: “it seems that as I get older … I don’t want to be in touch with as many people. I don’t find it necessary to be in touch with as many people like when I was younger” (FGI#2), resulting in their desire to control their social life. Some were content with the current level of social engagement and did not feel isolated even during the pandemic, expressing confidence in making connections when needed.
Finding own ways to keep connected with others during the pandemic
Participants stated that most social groups they had been in contact with were unavailable during the pandemic. As a result, they had to stay in touch with a small number of people they had access to via phone or video conferencing technology, such as family, friends, or church members, or by in-person contacts, such as residents in the same building. A few people maintained the level of in-person contact as they had done prepandemic. One person even mentioned a delivery man as a person she saw on a typical day when there were restrictions on social events and leisure activities. There was a consensus across groups on the significance of church members in social connectedness. Examples of activities performed with or by their church members include calling to make sure they “hear the service,” virtual bible study, prayer requests using text messages, and “doing a reconciliation thing with racism” (FGI#1).
Participants shared how they adapted to the new normal of living and being confined at home. Some people were trying to balance gains and losses for instance. One person decided to be hopeful and to visit “other places you could go” when not being able to go to “certain restaurants and movies” (FGI#2). Another commented that persistent effort to pursue a positive attitude was a crucial strategy for emotional well-being. Some participants shared how trying to “go outside and sit in the sun and just say hello to everybody” (FGI#1) was helpful to make them feel connected because “that really saved my sanity” and “it made me feel human for a while” (FGI#1).
The role of smart speakers and ICT use in enhancing social connectedness
Many participants shared that social activities through ICTs helped them feel connected, such as phone calls, video conferencing, text messaging, and Facebook groups. The pandemic brought them a new opportunity to expand their social network through technology. Although a variety of technology tools and diverse social activities via technology were reported by the members in Groups #1–4, a cell phone was the only technology tool reported by Group #5.
No one reported using the smart speaker for social connection purposes. Most participants did not know about the “drop-in” feature that enables checking in with another user, but they agreed on its crucial role in ensuring everyone is safe. Again, this feature was mentioned in the context of living alone. Some participants acknowledged a positive impact of a conversational agent on their mood and sense of companionship—whether it’s for fun, learning, or simple reminders. Another person said, “I would want Alexa to tell me good morning, to tell me God loves me. I’m worth continuing to go on. Just because I might be feeling lonely, now my loneliness is getting ready to go into depression. So if Alexa keeps telling me that I’m worth keeping going on, that’ll help me build myself up and feel some inner self-worth to continue to make it through that day” (FGI #4). Additionally, people shared their ideas of how smart speakers can help connect people for various social activities, such as going for a walk or grocery shopping.
Participants across groups expressed their desire to use smart speakers to make the housing community more viable and connected so that their isolated neighbors can feel less lonely and know what resources and opportunities are available for increased social participation. Group #5 participants were very vocal about this need. People agreed that seeing each other’s faces through a screen on digital technology (e.g., Zoom or Echo Show) helps them feel more connected than a phone call.
Factors affecting technology acceptance and use for enhancing social connectedness
Despite the potential of ICTs in promoting social connectedness, smart speaker nonusers shared concerns about privacy invasion or unauthorized access to personal data due to technological advances. Furthermore, participants expressed a fear of losing control caused by improvements in artificial intelligence (AI), leading to the perceived need to recognize the limitations of the smart speaker. The possibility of becoming overly dependent on AI technology prevented nonusers from adopting smart speaker technology: “My thing is it’s dumbing up the human race. Because you used to have to think and you had to use logic. Now all you got to do is say, ‘Alexa, Google, tell me this. Tell me that.’ And your brain cells—I was told if you don’t use them, you lose them. That’s what I was told” (FGI#3). Additionally, participants commented on how fast technologies are advancing, resulting in being “tired of learning new things” (FGI#1). This sentiment made some folks lose their interest in new technologies. Nevertheless, smart speaker nonusers showed curiosity about smart speakers and asked various questions about how it works: “That technology sounds like something I’d enjoy using. Is it very expensive?” (FGI#3).
Despite the high interest in smart speakers, participants discussed how negative technology experiences due to unreliable functions or lack of tech support made them hesitant to adopt new technology, particularly among Group #4 participants (nonusers in Facility A where smart speakers were deployed in several apartment units). Participants also made comments related to difficulty learning and adapting to technology: “Because I’m very illiterate to all this computer—I can’t even operate my phone. If you told me to delete the phone number off my phone, I wouldn’t even know how to do that” (FGI #4).
Discussion and Implications
Older adults living alone in low-income housing were at increased risk of social isolation and loneliness prior to the COVID-19 pandemic (Carbone et al., 2022; Finlay & Kobayashi, 2018). This study shows that low-income residents who lived alone experienced a high level of social disruptions in everyday life during the early stages of the pandemic. Social activities were canceled, visitors were not allowed, and many did not have a car, which limited outdoor trips or made them rely on public transportation or a long walk. Consequently, participants expressed distress, isolation, loneliness, sadness, and dissatisfaction with social relationships, although the perceived level of the pandemic impact on their lives varied. Overall, participants voiced the need for programs, services, or technology tools that could enable social interactions in their living environment and expressed an interest in adopting smart speakers for promoting social connectedness by facilitating conversations and connecting with social resources, but in a more meaningful and selective way that meets the goal of forming emotionally fulfilling relations (Finlay & Kobayashi, 2018; Luo et al., 2022).
Prior research reported that building broader, diverse networks and regular engagement in social activities lowers the loneliness of living alone (Schafer et al., 2022). The current study found that low-income, predominantly racial minority older adults who lived alone had a strong desire to promote a sense of community and belonging in their facilities. Importantly, participants felt that, beyond socialization purposes, making social connections with other residents was critical to ensuring their safety and survival in case of emergencies or unexpected health events. Participants expressed genuine concerns about peer residents being confined in their apartments and having no contact with others. Participants discussed the potential of smart speakers to address intersecting health and social needs. However, it became obvious that resources to address social isolation are lacking in low-income housing. Given that the impact of social isolation is more detrimental to the health and well-being of low-income residents due to social determinants of health (Caspi et al., 2013; Coe et al., 2018), finding creative ways to address this issue in the intersection of housing type, living alone, race, and income status is imperative.
Despite these challenges, our participants demonstrated resilience to the lockdown by using various coping strategies, such as finding alternative options to keep socially connected, learning how to use ICTs, practicing hopefulness, and maintaining a positive attitude. These strategies can fit into either problem- or emotion-focused coping categories explained in the Transactional Theory of Stress and Coping (Lazarus & Folkman, 1984). Lazarus and Folkman distinguished these two ways of coping in their original version; problem-focused coping behaviors address the stressor itself, whereas emotion-focused behaviors focus on adjusting their own response or perspective of the stressor. However, the differentiation between problem- and emotion-focused coping has faced criticism because many coping behaviors can serve dual functions (Stanisławski, 2019). Our findings underscore that many low-income residents who lived alone were forced to adapt to an isolated situation. The forced nature of the adaptation enabled a long-overdue ICT adoption among older adults who experienced digital exclusion prepandemic. For example, our participants shared how the pandemic led them to learn and adopt a new technology to continue social life and accept a new way of connecting (e.g., prayer sharing via text room). These new learning opportunities not only guided problem-solving but also facilitated emotional coping. For instance, our participants demonstrated ICT-based coping strategies that directly addressed the issue of social isolation by adopting new way of connecting and actively participating in online support groups. This, in turn, helped to reduce emotional distress and depression.
Recent literature reviews suggest that older adults at risk of loneliness and social isolation can benefit from the use of ICT as these provide means for social connectivity by strengthening existing relationships and facilitating leisure activities, which foster new connections (Balki et al., 2022; Petersen et al., 2023). Although these reviews provide an overview of the current state of ICT-based social connectedness interventions and their effectiveness on social isolation and loneliness, only a limited number of instances showing the use of conversational agents were included. This observation suggests that research related to social connectedness through conversational agents may still be in its early stages. An emerging body of the literature indicates that smart speakers offer a range of applications for social connectedness, including video calling to connect with family and friends and surrogating companionship that alleviates feelings of loneliness (Corbett et al., 2021; Jones et al., 2021). Although no participants reported using the smart speaker for connecting with other humans, a few perceived the conversational agent, Alexa, as a companion through simple conversations (e.g., “Good morning”). This is a unique functionality of smart speakers, allowing users to embody anthropomorphic qualities and promote empathy (Morrow et al., 2021). These qualities are essential for establishing rapport and ensuring long-term engagement. Future research should examine the relationships between types and amounts of interactions with conversational agents and its effect on social isolation and loneliness.
The current study contributes to the limited literature on the impact of the ICT intervention on social connectedness among low-income residents. Our participants exhibited a greater inclination toward utilizing smart speakers to mitigate the practical consequences of social isolation (e.g., accessing help in emergencies) rather than alleviating the internal experience of loneliness. Safety and injury prevention was a top priority for this group in technology adoption because they had to rely on limited assistance for day-to-day management and emergency health events, which was aligned with prior research about design considerations of robots for low-income older adults (Sefcik et al., 2018). The safety feature should be emphasized when designing ICTs including smart speaker-based applications for socially vulnerable older adults. Examples include applications that provide a virtual space for making connections for future help, send a reminder of the potential risk of social isolation by measuring sedentary time through health tracking technology integrated with the smart speaker, or provide the feedback about the level of social engagement through social signal detection (e.g., laughter) or automatic speech recognition (Laranjo et al., 2018).
As our data indicate, however, participants’ ability to overcome that challenge and beliefs in the benefits of ICTs varied. Furthermore, participants—particularly smart speaker nonusers—shared uncertainty about cybersecurity and privacy of AI-enabled technology due to its surveilling nature. The literature shows that privacy, obtrusiveness, and security concerns are important factors affecting in-home technology adoption among older adults (Chung et al., 2016). However, much of the technology adoption research has been conducted with predominantly Caucasian, highly educated older adults living in affluent communities, limiting our understanding of low-income, racial/ethnic minority older adults’ privacy and security attitudes and needs. This group of older adults may be at increased risk of privacy and security risks due to limited technical knowledge and experience, low technology confidence, and lack of technical support and training (Hunsaker & Hargittai, 2018; Schreurs et al., 2017). In order for smart speakers to be designed and used appropriately, there is a need to address potential privacy and security concerns about the interactions with AI-enabled conversational agents in the user’s living context and to provide support and user-centered training for improved competence and more in-depth sociotechnical understanding of smart speaker use in their lives.
Several limitations to this study must be noted. First, the use of the convenience sample, where the respondents’ characteristics had not been systematically or purposefully selected, was a limitation. Compared to the demographic profile of older adults living in HUD-subsidized senior housing (Ewen et al., 2017; Lehning et al., 2023), our sample exhibited a relatively younger age distribution, a higher representation of Black or African Americans, and a lower proportion of female participants. Additionally, a relatively heterogeneous sample was used in terms of education level, disability, social isolation and loneliness, and technology ownership. Thus, the findings may not generalize to larger populations of low-income residents within or external to the United States. Second, there is a possibility that participants may have underreported loneliness and social isolation experiences during the focus group sessions due to the related social stigma. Last, selection bias is possible because residents who were the most isolated and lonely were less likely to participate in technology design research (Waycott et al., 2016). This may be attributed to our limited recruitment strategies during the pandemic, primarily through a university-based interprofessional wellness program (Parsons et al., 2019). Despite this, even among participants who agreed to participate, they experienced social disruptions due to the pandemic (Winship et al., 2022). Although self-reported isolation levels were not as high as we expected, their insights still provided valuable understanding of the role of digital tools. Therefore, a comprehensive investigation is needed to explore the broader sociotechnical context influencing the decision of older adults with social isolation and loneliness not to participate in technology design and evaluation studies, such as personal circumstances, preferences, social contexts, and technology access.
Conclusion
This study provides insight into ICT integration into social life, including challenges encountered, concerns regarding smart speaker use for fostering social connectedness, and strategies to enhance the adoption and learning of novel ICTs, particularly among low-income minority older adults. The growth of technological tools to support and improve quality of life is aligned with the desire expressed by older adult participants for programs that will enable meaningful social interactions. However, there is a discrepancy between the development and innovation in technological tools for older adults and what older people actually want (Mannheim et al., 2019). The current study provides guidance to gerontechnologists and computer solution designers about how ICTs must fit within target user needs and context. Assessing user needs, specific preferences, and privacy concerns in their sociocultural context is significant to inform how to build smart speaker algorithms and functionalities. It is also an essential component of testing innovative interventions based on these new functions to promote social connectedness in low-income residents. Future advocacy and policy should focus on the development of guidelines for research and design of digital technology. These guidelines should highlight the need to include older adults in all stages of development that recognize the social and cultural context of use with a focus on growth-oriented opportunities for older people.
Supplementary Material
Acknowledgment
The authors thank all the participants in the study who made outdoor trips to participate in focus group sessions. The authors express their gratitude to Greg Ford, Director of Program Development and Implementation at Beacon Communities; Normal Dorsett, Senior Community Coordinator at A Winn Residential Managed Community; and Kate Noon, Director of Senior Services at Better Housing Coalition at the time of participant recruitment and data collection. We are also grateful to Katherine Falls, Director of Clinical Operations at Richmond Health and Wellness Program. Without their support, this research would not have been possible.
Contributor Information
Jane Chung, School of Nursing, Virginia Commonwealth University, Richmond, Virginia, USA.
Tracey Gendron, Department of Gerontology, College of Health Professions, Virginia Commonwealth University, Richmond, Virginia, USA; Virginia Center on Aging, College of Health Professions, Virginia Commonwealth University, Richmond, Virginia, USA.
Jodi Winship, Department of Occupational Therapy, College of Health Professions, Virginia Commonwealth University, Richmond, Virginia, USA.
Rachel E Wood, School of Nursing, Virginia Commonwealth University, Richmond, Virginia, USA.
Natalie Mansion, Richmond Health and Wellness Program, School of Nursing, Virginia Commonwealth University, Richmond, Virginia, USA.
Pamela Parsons, School of Nursing, Virginia Commonwealth University, Richmond, Virginia, USA; Richmond Health and Wellness Program, School of Nursing, Virginia Commonwealth University, Richmond, Virginia, USA.
George Demiris, School of Nursing, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
Funding
This work was supported by the National Institutes of Health [R03AG069816 to J. Chung].
Conflict of Interest
None.
Data Availability
The study materials, analytic methods, and data are available from the corresponding author on reasonable request. The parent study “Voice2Connect” was not preregistered.
Author Contributions
Jane Chung (Conceptualization [Lead], Data curation [Lead], Formal analysis [Lead], Funding acquisition [Lead], Investigation [Lead], Methodology [Lead], Project administration [Lead], Resources [Lead], Software [Lead], Supervision [Lead], Validation [Lead], Writing—original draft [Lead], Writing—review & editing [Lead]), Tracey Gendron (Conceptualization [Supporting], Formal analysis-Equal, Funding acquisition [Supporting], Investigation [Supporting], Methodology [Supporting], Writing—original draft [Supporting], Writing—review & editing [Supporting]), Jodi Winship (Conceptualization [Equal], Formal analysis [Equal], Funding acquisition-Supporting, Investigation [Equal], Methodology [Supporting], Project administration [Supporting], Resources [Supporting], Supervision [Supporting], Validation [Supporting], Writing—review & editing [Equal]), Rachel Wood (Investigation [Supporting], Project administration [Equal], Writing—review & editing [Supporting]), Natalie Mansion (Formal analysis [Supporting], Project administration [Supporting], Writing—review & editing [Supporting]), Pamela Parsons (Investigation [Supporting], Project administration [Supporting], Resources [Equal], Writing—review & editing [Supporting]), and George Demiris (Conceptualization [Supporting], Methodology [Supporting], Supervision [Supporting], Validation [Supporting], Writing—review & editing [Equal])
References
- Balki, E., Hayes, N., & Holland, C. (2022). Effectiveness of technology interventions in addressing social isolation, connectedness, and loneliness in older adults: Systematic umbrella review. JMIR Aging, 5(4), e40125. 10.2196/40125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyatzis, R. E. (1998). Transforming qualitative information: Thematic analysis and code development. Sage Publications. [Google Scholar]
- Carbone, J. T., Clift, J., Wyllie, T., & Smyth, A. (2022). Housing unit type and perceived social isolation among senior housing community residents. Gerontologist, 62(6), 889–899. 10.1093/geront/gnab184 [DOI] [PubMed] [Google Scholar]
- Caspi, C. E., Kawachi, I., Subramanian, S. V., Tucker-Seeley, R., & Sorensen, G. (2013). The social environment and walking behavior among low-income housing residents. Social Science & Medicine, 80, 76–84. 10.1016/j.socscimed.2012.11.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung, J., Bleich, M., Wheeler, D., Winship, J., McDowell, B., Baker, D., & Parsons, P. (2021). Attitudes and perceptions towards voice-operated smart speakers among low-income senior housing residents: Comparison of pre- and post-installation surveys. Gerontology and Geriatric Medicine, 7, 1–9. 10.1177/23337214211005869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung, J., Demiris, G., & Thompson, H. J. (2016). Ethical considerations regarding the use of smart home technologies for older adults: An integrative review. Annual Review of Nursing Research, 34(1), 155–181. 10.1891/0739-6686.34.155 [DOI] [PubMed] [Google Scholar]
- Coe, A. B., Moczygemba, L. R., Ogbonna, K. C., Parsons, P. L., Slattum, P. W., & Mazmanian, P. E. (2018). Low-income senior housing residents’ emergency department use and care transition problems. Journal of Pharmacy Practice, 31(6), 610–616. 10.1177/0897190017734763 [DOI] [PubMed] [Google Scholar]
- Corbett, C. F., Wright, P. J., Jones, K., & Parmer, M. (2021). Voice-activated virtual home assistant use and social isolation and loneliness among older adults: Mini review. Frontiers in Public Health, 9, 742012. 10.3389/fpubh.2021.742012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotten, S. R., Anderson, W. A., & McCullough, B. M. (2013). Impact of internet use on loneliness and contact with others among older adults: Cross-sectional analysis. Journal of Medical Internet Research, 15(2), e39–e13. 10.2196/jmir.2306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cudjoe, T. K. M., Roth, D. L., Szanton, S. L., Wolff, J. L., Boyd, C. M., & Thorpe, R. J. (2020). The epidemiology of social isolation: National health and aging trends study. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(1), 107–113. 10.1093/geronb/gby037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demiris, G., Chung, J., & Tunner, A. (2022). Using informatics to engage vulnerable populations in research: Lessons learned from the COVID-19 pandemic. Studies in Health Technology and Informatics, 290, 858–861. 10.3233/SHTI220201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diallo, A. F., Falls, K., Hicks, K., McQueen Gibson, E., Obaid, R., Slattum, P., Zanjani, F., Price, E., & Parsons, P. (2020). The Healthy Meal Program: A food insecurity screening and referral program for urban dwelling older adults. Public Health Nursing, 37(5), 671–676. 10.1111/phn.12778. 10.1111/phn.12778 [DOI] [PubMed] [Google Scholar]
- Donovan, N. J., Wu, Q., Rentz, D. M., Sperling, R. A., Marshall, G. A., & Glymour, M. M. (2017). Loneliness, depression and cognitive function in older US adults. International Journal of Geriatric Psychiatry, 32(5), 564–573. 10.1002/gps.4495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewen, H. H., Washington, T. R., Emerson, K. G., Carswell, A. T., & Smith, M. L. (2017). Variation in older adult characteristics by residence type and use of home- and community-based services. International Journal of Environmental Research and Public Health, 14(3), 330. 10.3390/ijerph14030330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlay, J. M., & Kobayashi, L. C. (2018). Social isolation and loneliness in later life: A parallel convergent mixed-methods case study of older adults and their residential contexts in the Minneapolis metropolitan area, USA. Social Science & Medicine, 208(March), 25–33. 10.1016/j.socscimed.2018.05.010 [DOI] [PubMed] [Google Scholar]
- Fuller, H. R., & Huseth-Zosel, A. (2021). Older adults’ loneliness in early COVID-19 social distancing: Implications of rurality. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 77(7), e100–e105. 10.1093/geronb/gbab053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halcomb, E. J., Gholizadeh, L., DiGiacomo, M., Phillips, J., & Davidson, P. M. (2007). Literature review: Considerations in undertaking focus group research with culturally and linguistically diverse groups. Journal of Clinical Nursing, 16(6), 1000–1011. 10.1111/j.1365-2702.2006.01760.x [DOI] [PubMed] [Google Scholar]
- Heid, A. R., Cartwright, F., Wilson-Genderson, M., & Pruchno, R. (2021). Challenges experienced by older people during the initial months of the COVID-19 pandemic. Gerontologist, 61(1), 48–58. 10.1093/geront/gnaa138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., & Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10(2), 227–237. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- Hu, J., Fitzgerald, S. M., Owen, A. J., Ryan, J., Joyce, J., Chowdhury, E., Reid, C. M., Britt, C., Woods, R. L., McNeil, J. J., & Freak-Poli, R. (2021). Social isolation, social support, loneliness and cardiovascular disease risk factors: A cross-sectional study among older adults. International Journal of Geriatric Psychiatry, 36(11), 1795–1809. 10.1002/gps.5601 [DOI] [PubMed] [Google Scholar]
- Hunsaker, A., & Hargittai, E. (2018). A review of Internet use among older adults. New Media & Society, 20(10), 3937–3954. 10.1177/1461444818787348 [DOI] [Google Scholar]
- Ibarra, F., Baez, M., Cernuzzi, L., & Casati, F. (2020). A systematic review on technology-supported interventions to improve old-age social wellbeing: Loneliness, social isolation, and connectedness. Journal of Healthcare Engineering, 2020, 2036842. 10.1155/2020/2036842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, V. K., Hanus, M., Yan, C., Shade, M. Y., Blaskewicz Boron, J., & Maschieri Bicudo, R. (2021). Reducing loneliness among aging adults: The roles of personal voice assistants and anthropomorphic interactions. Frontiers in Public Health, 9, 750736. 10.3389/fpubh.2021.750736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalski, J., Jaskulska, A., Skorupska, K., Abramczuk, K., Biele, C., Kopeć, W., & Marasek, K. (2019). Older adults and voice interaction: A pilot study with google home. 2019 CHI Conference on Human Factors in Computing Systems, 1–6. 10.1145/3290607.3312973 [DOI]
- Laranjo, L., Dunn, A. G., Tong, H. L., Kocaballi, A. B., Chen, J., Bashir, R., Surian, D., Gallego, B., Magrabi, F., Lau, A. Y. S., & Coiera, E. (2018). Conversational agents in healthcare: A systematic review. Journal of the American Medical Informatics Association: JAMIA, 25(9), 1248–1258. 10.1093/jamia/ocy072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus, S., & Folkman. (1984). Stress, appraisal and coping. Springer. [Google Scholar]
- Lehning, A., Kim, K., Park, S., & Dunkle, R. (2023). Preference to age in place in low-income senior housing. Journal of Gerontological Social Work, 66(4), 567–582. 10.1080/01634372.2022.2130490 [DOI] [PubMed] [Google Scholar]
- Lincoln, Y. S., & Guba, E. (1985). Naturalistic inquiry. SAGE Publications. [Google Scholar]
- Litchfield, I., Shukla, D., & Greenfield, S. (2021). Impact of COVID-19 on the digital divide: A rapid review. BMJ Open, 11(10), e053440–9. 10.1136/bmjopen-2021-053440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo, M., Macdonald, B., & Hülür, G. (2022). Not “The More The Merrier”: Diminishing returns to daily face-to-face social interaction frequency for well-being in older age. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 77(8), 1431–1441. 10.1093/geronb/gbac010 [DOI] [PubMed] [Google Scholar]
- Mannheim, I., Schwartz, E., Xi, W., Buttigieg, S. C., McDonnell-Naughton, M., Wouters, E. J. M., & van Zaalen, Y. (2019). Inclusion of older adults in the research and design of digital technology. International Journal of Environmental Research and Public Health, 16(19), 3718. 10.3390/ijerph16193718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow, D. G., Lane, H. C., & Rogers, W. A. (2021). A framework for design of conversational agents to support health self-care for older adults. Human Factors, 63(3), 369–378. 10.1177/0018720820964085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musich, S., Wang, S. S., Hawkins, K., & Yeh, C. S. (2015). The impact of loneliness on quality of life and patient satisfaction among older, sicker adults. Gerontology and Geriatric Medicine, 1(January-December), 233372141558211. 10.1177/2333721415582119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2020). Social isolation and loneliness in older adults: Opportunities for the health care system. National Academies Press (US). [PubMed] [Google Scholar]
- Nicholson, N. R., Feinn, R., Casey, E. A., Dixon, J., & Meeks, S. (2020). Psychometric evaluation of the Social Isolation scale in older adults. Gerontologist, 60(7), E491–E501. 10.1093/geront/gnz083 [DOI] [PubMed] [Google Scholar]
- Nowell, L. S., Norris, J. M., White, D. E., & Moules, N. J. (2017). Thematic analysis: Striving to meet the trustworthiness criteria. International Journal of Qualitative Methods, 16, 160940691773384–13. 10.1177/1609406917733847 [DOI] [Google Scholar]
- O’Brien, K., Light, S. W., Bradley, S., & Lindquist, L. (2022). Optimizing voice-controlled intelligent personal assistants for use by home-bound older adults. Journal of the American Geriatrics Society, 70(5), 1504–1509. 10.1111/jgs.17625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons, P. L., Slattum, P. W., & Bleich, M. (2019). Main- streaming health and wellness: The RHWP innovation model to complement primary care. Nursing Forum, 54(2), 263–269. 10.1111/nuf.12326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perissinotto, C. M., Stijacic Cenzer, I., & Covinsky, K. E. (2012). Loneliness in older persons: A predictor of functional decline and death. Archives of Internal Medicine, 172(14), 1078–1083. 10.1001/archinternmed.2012.1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen, B., Khalili-Mahani, N., Murphy, C., Sawchuk, K., Phillips, N., Li, K. Z. H., & Hebblethwaite, S. (2023). The association between information and communication technologies, loneliness and social connectedness: A scoping review. Frontiers in Psychology, 14, 1063146. 10.3389/fpsyg.2023.1063146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poscia, A., Stojanovic, J., La Milia, D. I., Duplaga, M., Grysztar, M., Moscato, U., Onder, G., Collamati, A., Ricciardi, W., & Magnavita, N. (2018). Interventions targeting loneliness and social isolation among the older people: An update systematic review. Experimental Gerontology, 102, 133–144. 10.1016/j.exger.2017.11.017 [DOI] [PubMed] [Google Scholar]
- Pradhan, A., Findlater, L., & Lazar, A. (2019). “Phantom Friend” or “Just a Box with Information”: Personification and ontological categorization of smart speaker-based voice assistants by older adults. Proceedings of the ACM on Human-Computer Interaction, 3(CSCW), 1–21. 10.1145/335931634322658 [DOI] [Google Scholar]
- Reis, A., Paulino, D., Paredes, H., & Barroso, J. (2017). Using intelligent personal assistants to strengthen the elderlies’ social bonds. In Antona M. & Stephanidis C. (Eds.), Universal access in human–computer interaction. Human and technological environments (pp. 593–602). Springer International Publishing. 10.1007/978-3-319-58700-4_48 [DOI] [Google Scholar]
- Sargent, L., Zanjani, F., Winship, J., Gendron, T., Mackiewicz, M., Diallo, A., Waters, L., Battle, K., Ford, G., Falls, K., Chung, J., Price, E. T., Cisewski, M., & Parsons, P.; VCU iCubed Core. (2022). Socioeconomic effects on psychosocial factors among low-income older adults. Gerontology and Geriatric Medicine, 8, 233372142210848. 10.1177/23337214221084866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer, M. H., Sun, H., & Lee, J. A. (2022). Compensatory connections? Living alone, loneliness, and the buffering role of social connection among older American and European adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 77(8), 1550–1560. 10.1093/geronb/gbab217 [DOI] [PubMed] [Google Scholar]
- Schreurs, K., Quan-Haase, A., & Martin, K. (2017). Problematizing the digital literacy paradox in the context of older adults’ ICT use: Aging, media discourse, and self-determination. Canadian Journal of Communication, 42(2), 359–377. 10.22230/cjc.2017v42n2a3130 [DOI] [Google Scholar]
- Sefcik, J. S., Johnson, M. J., Yim, M., Lau, T., Vivio, N., Mucchiani, C., & Cacchione, P. Z. (2018). Stakeholders’ perceptions sought to inform the development of a low-cost mobile robot for older adults: A qualitative descriptive study. Clinical Nursing Research, 27(1), 61–80. 10.1177/1054773817730517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims, T., Reed, A. E., & Carr, D. C. (2017). Information and communication technology use is related to higher well-being among the oldest-old. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 72(5), 761–770. 10.1093/geronb/gbw130 [DOI] [PubMed] [Google Scholar]
- Stanisławski, K. (2019). The Coping Circumplex Model: An integrative model of the structure of coping with stress. Frontiers in Psychology, 10, 694. 10.3389/fpsyg.2019.00694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, D. R. (2006). A general inductive approach for analyzing qualitative evaluation data. American Journal of Evaluation, 27, 237–246. 10.1177/1098214005283748 [DOI] [Google Scholar]
- Thorne, S. (2016). Interpretive description: Qualitative research for applied practice (2nd ed.). Routledge. [Google Scholar]
- van Deursen, A. J. A. M. (2020). Digital inequality during a pandemic: Quantitative study of differences in COVID-19-related internet uses and outcomes among the general population. Journal of Medical Internet Research, 22(8), 1–13. 10.2196/20073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waycott, J., Vetere, F., Pedell, S., Morgans, A., Ozanne, E., & Kulik, L. (2016). Not for me: Older adults choosing not to participate in a social isolation intervention. Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems, 745–757. 10.1145/2858036.2858458 [DOI]
- Winship, J. M., Gendron, T., Waters, L., Chung, J., Battle, K., Cisewski, M., Gregory, M., Sargent, L., Zanjani, F., Slattum, P., Mackiewicz, M., Diallo, A., Ford, G., Falls, K., Price, E. T., & Parsons, P. L. (2022). COVID in context: The lived experience of Richmond’s low-income older adults. Gerontology and Geriatric Medicine, 8, 233372142210792. 10.1177/23337214221079208 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The study materials, analytic methods, and data are available from the corresponding author on reasonable request. The parent study “Voice2Connect” was not preregistered.