Introduction
Lung ultrasound (LUS) was introduced to intensive care units and emergency departments more than 20 years ago, primarily as a tool for the assessment of patients with acute dyspnoea.1,2 Since then, it has gained popularity as a quick point-of-care examination enabling clinicians to answer crucial clinical questions. Over the last decade, the cardiology community has acknowledged the potential of LUS and expanded its use further, to assist with the diagnosis and management of patients with heart failure (HF).3–5
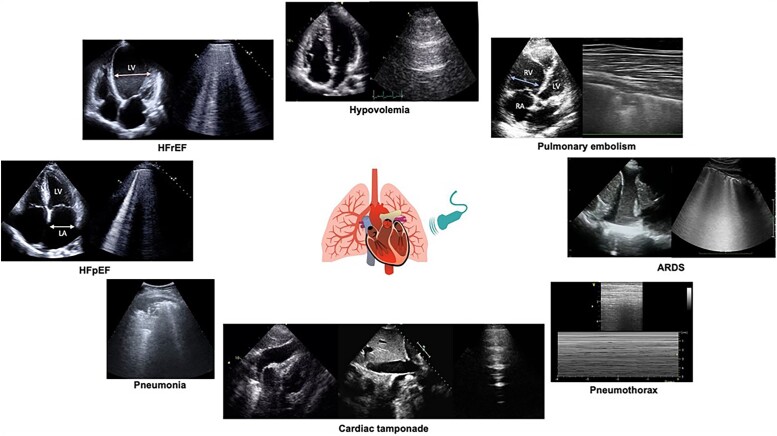
The importance of recognizing and treating pulmonary congestion is a cornerstone in the management of patients with HF.6 LUS is a versatile, high sensitivity point-of-care examination to detect pulmonary deaeration due to increased extravascular lung water. It has many advantages to the extent that an integrated cardiopulmonary ultrasound exam is likely to become the reference standard in HF care. This approach allows the aetiology of HF to be defined, through the assessment of cardiac structure and function by echocardiography, at the same time as the assessment of pulmonary congestion provided by LUS. In addition, it facilitates the exclusion of other highly prevalent conditions that may mimic/overlap with HF (e.g. pneumonia, acute lung injury/acute respiratory distress syndrome [ALI/ARDS], and pneumothorax).
LUS in HF: the findings
B-lines and pleural effusions
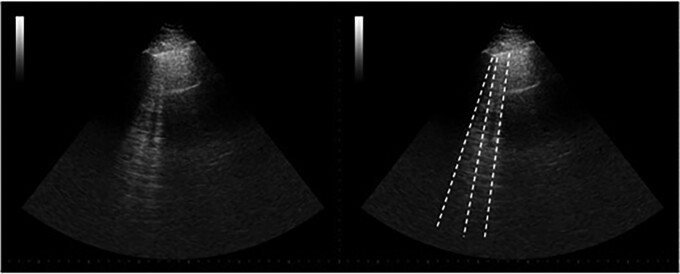
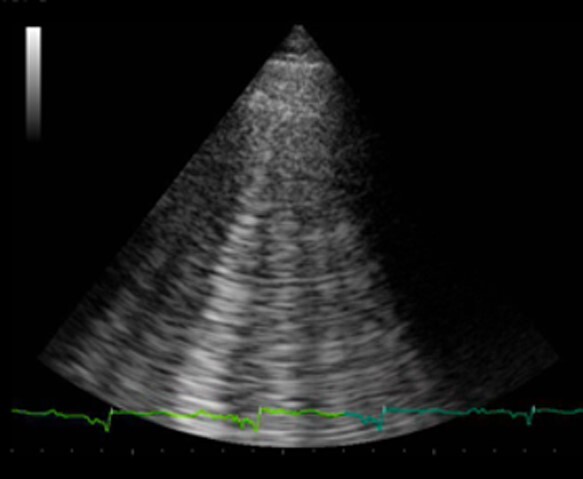
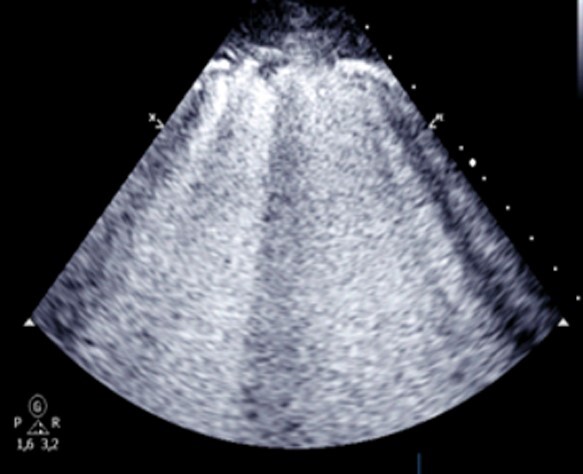
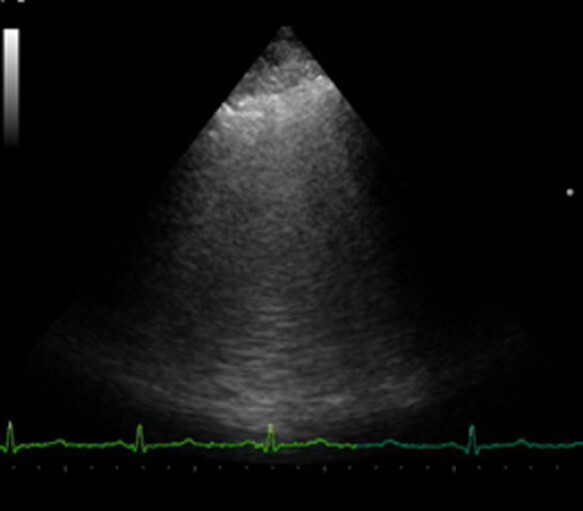
In a fully aerated lung, the only anatomical structure that can be visualized is the pleura, which appears as a smooth, hyperechoic horizontal line that moves synchronously with respiration. This line is called ‘pleural line’ and its movement is the ‘lung sliding’, providing visual assessment of lung excursion during ventilation. The sonographic pattern of the aerated lung also includes parallel, hyperechoic, horizontal lines that can be seen at regular intervals from the pleural line (A-lines, Figure 1, Supplementary data online, Video S1).7 When the air content in the lung decreases and lung density increases, vertical reverberation artefacts appear (B-lines, Figure 2, Supplementary data online, Video S2). B-lines originate from the pleural line and move synchronously with respiration, are laser-like in shape and extend towards the bottom of the US sector as displayed on the screen.8 B-lines are present in patients with HF and pulmonary oedema9 where an increasing number of visualized B-lines are associated with a decreasing air/water content ratio.10–12
Figure 1.
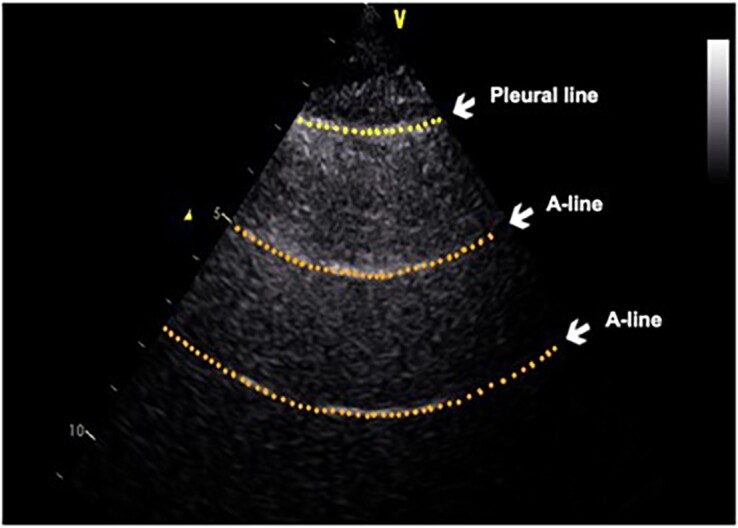
The sonographic pattern of a normally aerated lung with the pleural line (upper dotted yellow line) and A-lines (lower dotted orange lines).
Figure 2.
B-lines indicated by dotted white lines.
B-lines are not specific for cardiogenic pulmonary oedema and can be detected in patients with non-cardiogenic pulmonary oedema, including those with end stage renal disease and in ALI/ARDS,13 but also in pulmonary fibrosis (interstitial lung disease)14 and interstitial pneumonia. Some sonographic characteristics can help differentiate these various causes of B-lines5 (Table 1).
Table 1.
Different LUS features in different conditions where multiple B-lines are present
| Cardiogenic pulmonary oedema | ALI/ARDS | Interstitial pneumonia | Interstitial pulmonary fibrosis | |
|---|---|---|---|---|
|
|
|
|
|
| B-lines distribution |
|
|
|
|
| Pleural line appearance |
|
|
|
|
| Consolidations |
|
|
|
|
| Pleural effusion |
|
|
|
|
ALI, acute lung injury; ARDS, acute respiratory distress syndrome.
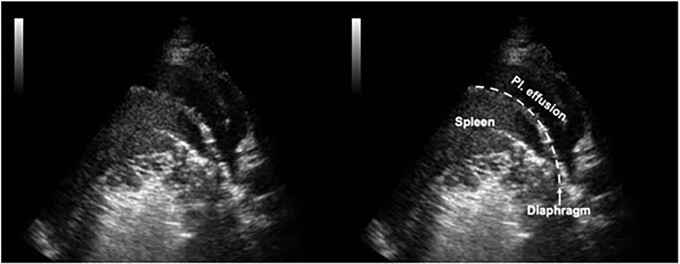
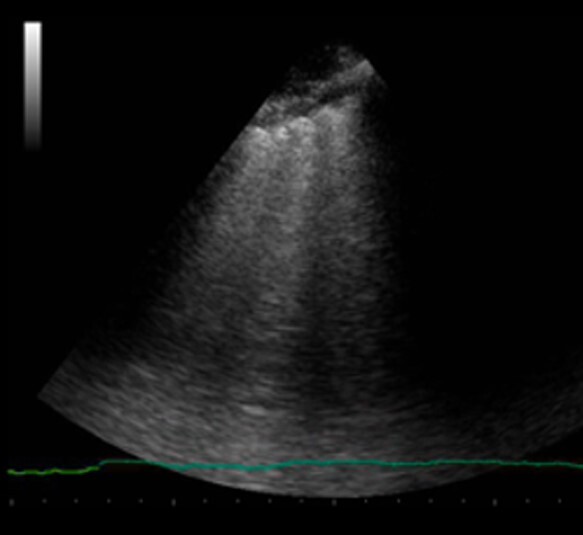
Pleural effusion can be easily detected by LUS, placing the phased-array transducer on the surface of the chest wall in an intercostal space, and is displayed as an anechoic space above the diaphragm. Pleural effusion is advised to be sought at first in the dependent zones, i.e. lateral and posterior chest wall (e.g. posterior axillary line) at the level of costophrenic angles (Figure 3 and Supplementary data online, Video S3), which also allows other causes of chest X-ray radio-opacity, such as consolidation, mass, or an elevated hemidiaphragm to be ruled out (Figure 4 and Supplementary data online, Video S4). LUS is more sensitive than chest X-ray in detecting pleural effusions, when using computed tomography as the reference standard,15,16 and can determine the volume of pleural effusion and monitor its evolution. LUS can also provide information on its likely nature by differentiating between simple and complex effusions, and can help guide the optimal site for needle thoracentesis.
Figure 3.
The left costophrenic angle with pleural effusion.
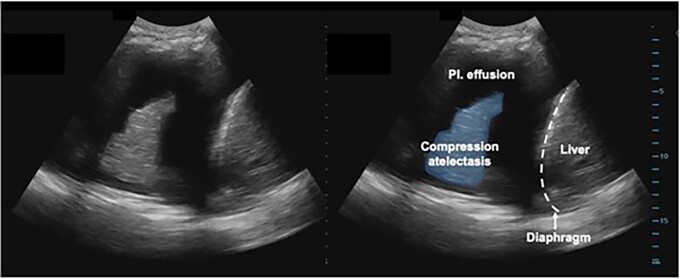
Figure 4.
Pleural effusion with compression atelectasis.
Other sonographic features of congestion
The pathophysiology of congestion in HF includes the different stages of haemodynamic, pulmonary, and systemic congestion,17 which can be all assessed by ultrasound. Traditional echocardiography provides indicators of haemodynamic congestion, including a dilated left atrium, a high E/e′, elevated pulmonary artery systolic pressure, and dilated inferior vena cava (IVC). B-lines on LUS are a sign of pulmonary congestion (increased extravascular lung water) due to left-sided HF, independent of—yet closely related with haemodynamic congestion. Chronically elevated left-sided filling pressures eventually result in a rise in right atrial pressures and IVC distension. An IVC smaller than 21 mm that collapses >50% during inspiration suggests normal right atrial pressures,18 although this measurement should be interpreted in the context of the overall patient’s underlying pathophysiological and haemodynamic status and integrated with other echocardiographic findings; an increased IVC diameter can identify intravascular volume expansion prior to changes in symptoms or body weight, and predicts a high risk of rehospitalization for HF or death in patients with acute or chronic HF.19,20
Using a high-frequency linear transducer, the internal jugular vein (IJV) diameter can be measured. When congestion is severe, IJV distensibility, provoked by Valsalva manoeuvre, is markedly reduced, indicating a poor prognosis.21 Congestion in other organs can be also assessed by ultrasound, such as the kidneys. A comprehensive review of these novel techniques and their potential clinical utility can be found elsewhere.22 Recently, the venous excess ultrasound (VExUS) score, including Doppler evaluation of the IVC, hepatic veins, portal vein, and renal venous flow, has been proposed to assess presence and severity of venous congestion.23 Whereas systemic venous congestion (as assessed by IVC, IJV, hepatic veins, portal veins, and renal veins) can be present in both right- and left-sided HF, LUS B-lines indicate pulmonary congestion due to left-sided HF.
Other sonographic features of deaeration
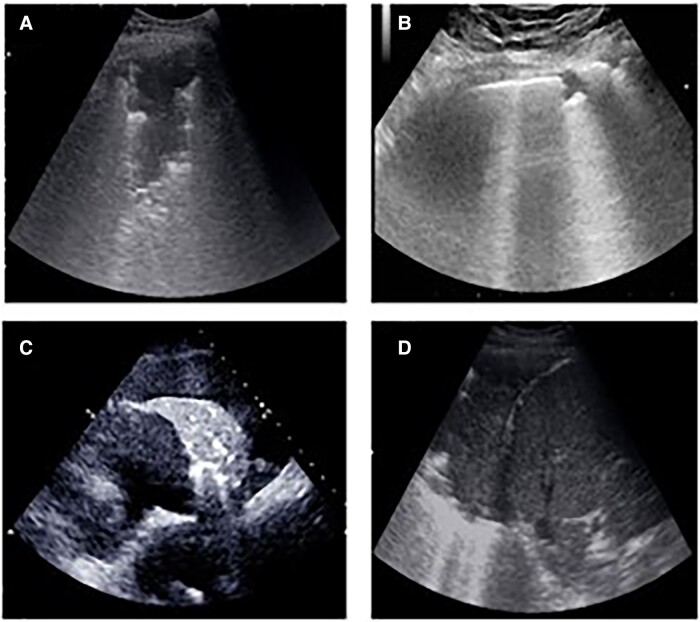
When the pulmonary air content is completely dissipated in areas of pulmonary consolidation, the lung parenchyma can be directly visualized (Figure 5 and Supplementary data online, Video S5) with a hypoechoic or tissue-like pattern. Different aetiologies of consolidations may have also different sonographic appearance (Figure 5). Compression atelectasis is frequent in patients with HF; here, a large cardiogenic pleural effusion causes direct compression of the pulmonary parenchyma.4
Figure 5.
Different patterns of consolidation at LUS: A) pneumonia; B) pulmonary infarction; C) compression atelectasis; D) obstructive atelectasis.
On occasion, a focal interstitial syndrome (i.e. multiple B-lines localized only in a single area of the chest) can suggest pneumonia. These are thought to represent either the very early phases of pneumonia with the partial deaeration LUS pattern (B-lines) preceding the total deaeration LUS pattern (consolidation), or the focal oedema surrounding any consolidation.
LUS in HF: the technique
Whenever possible, it is advised to perform LUS exams with a standardized approach, to facilitate interpretation and monitoring, as well as reproducibility.24 Several LUS protocols have been described, with a variable number of examination areas of the chest (‘zones’) to be examined, ranging from 4 to 2825–27 (Figure 6). Currently, the eight-zone scanning protocol is the most widely used, balancing the need for a simplified, rapid protocol, and good accuracy;8 with studies suggesting it the most appropriate approach across multiple settings, including the diagnosis of HF (with the 8-zone C-index non-inferior to the 28-zone C-index),28 and for risk stratification.29
Figure 6.
Different LUS scanning protocols, ranging from 4 to 28 zones; the imaging protocol should be performed on both hemithoraces (in the 28-zone protocol, the left hemithorax does not include the fifth intercostal space).
When integrating LUS during stress echocardiography, a simplified four-zone scanning protocol is often used, placing the probe at the third intercostal space along the anterior axillary and mid-axillary lines.30,31
In adult patients, both phased-array or convex transducers are sufficient to assess B-lines. If available, the abdominal preset (for the convex transducer) and the cardiac preset (for the phased-array transducer) usually provide adequate image quality. Some machines have also a dedicated lung preset. The transducer should be placed in the intercostal space either perpendicular (longitudinal and sagittal) or in parallel orientation (transverse) to the ribs. Imaging depth depends on the size of the patient, but is usually set at ∼15–18 cm.22 Once the transducer position and gain settings are optimized for visualization of the pleural line and B-lines, it is advised to keep the transducer in the same location for at least one respiratory cycle. When a movie clip is recorded, the suggested length is of ∼6 s.32,33 In each chest zone, the operator should scan all accessible chest surface to increase sensitivity.
During the examination, patients can be positioned either sitting upright, semi-recumbent, or supine; however, it is preferred to scan patients in the same position if serial examinations are being performed.34 In those thoracic zones where a pleural effusion is visualized, B-lines cannot be assessed, and the presence of pleural effusions should be described in the LUS report instead.
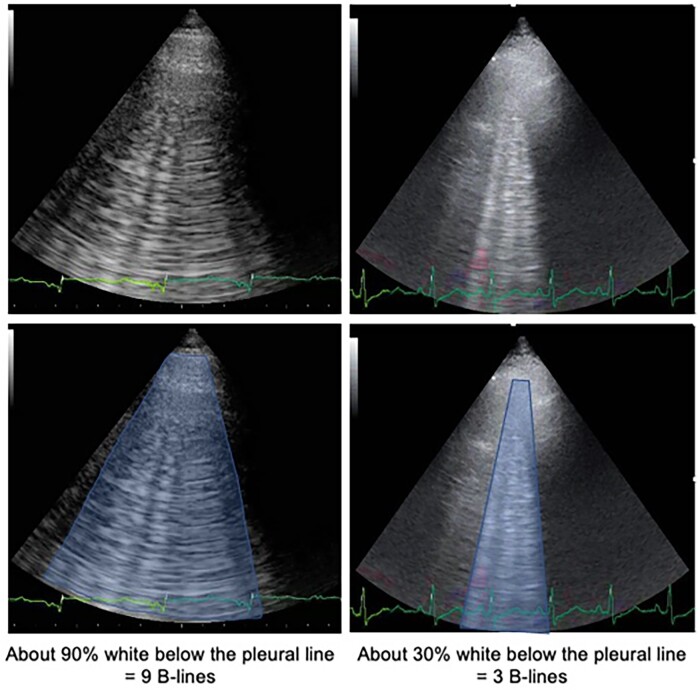
There are two main approaches to quantify B-lines: score- or count-based methods. Score-based methods consider a minimum number of B-lines in one thoracic zone as a ‘positive’ zone (typically at least three B-lines),8 then, the number of positive zones are added up.25 Count-based methods entail that B-lines are counted to obtain a number for each thoracic zone: B-lines can be counted one by one27,34 or, when confluent and overlapping, their number can be estimated from the percentage of space they occupy on the screen below the pleural line, divided by 10 (i.e. if ∼60% of the screen below the pleural line is occupied by B-lines, it would conventionally count as six B-lines, up to a maximum of 10 per zone) (Figure 7). It is advised to count B-lines in the worst (less aerated/with more B-lines) point of each thoracic zone, then, the number of B-lines in each zone can be summed up to obtain a total B-line count.4,8,35,36 All these methods have demonstrated good intra- and inter-observer agreement.37,38
Figure 7.
How to quantify B-lines.
Key points: To evaluate pulmonary congestion in patients with suspected or established HF, using a phased-array or convex probe may be appropriate (including handheld ultrasound devices), in sagittal or transverse orientations (transducer perpendicular or parallel to the intercostal space), ideally following the eight-zone protocol and maintaining the patient in the same position during serial examinations.
Clinical applications
Acute heart failure
Diagnosis: ruling in/out acute cardiogenic dyspnoea
The typical LUS pattern of a patient with acute HF and pulmonary oedema is the presence of ‘multiple’ (at least three B-lines in one chest zone), ‘diffuse’ (at least two positive zones per hemithorax), and ‘bilateral’ B-lines. It is important to distinguish this pattern from the presence of a few patchy B-lines, especially when located at the lung bases, that can be seen even in healthy subjects, and which therefore do not qualify as ‘multiple’, ‘diffuse’, and ‘bilateral’.
LUS is a rapid diagnostic test, which takes <5 min. Among patients hospitalized with acute dyspnoea, LUS has demonstrated high diagnostic accuracy for acute HF, with a sensitivity of 94–97% and a specificity of 97%25,26 that has been shown to be superior to both clinical assessment (i.e. history, physical examination, electrocardiogram, and arterial blood gas) and the chest X-ray, even when there is superimposed pneumonia.25,39,40 Indeed, LUS is superior to chest X-ray alone (sensitivity of 91.8% vs. 76.5% and a specificity of 92.3% vs. 87.0%),41 and has higher accuracy than clinical assessment even when integrated with ‘traditional’ diagnostic tests (i.e. natriuretic peptides and chest X-ray) to diagnose acute HF.25,26
Monitoring: assessing decongestion
A higher number of B-lines on admission for an episode of acute HF is associated with greater risk, regardless of left ventricular ejection fraction (LVEF) and presence of HF signs and symptoms.42 This suggests that B-lines might be a potential target for treatment but also useful to monitor response to decongestive therapies.
Changes in B-lines are very dynamic and, for those who respond to diuretic therapy and other treatments, the number of B-lines decreases rapidly,27,43,44 regardless of the aetiology of acute HF.45 Serial LUS can guide titration of diuretic therapy, leading to more rapid relief of congestion and, potentially, shortening the length of hospital stay.46–48 Resolution of pulmonary congestion detected by ultrasound during HF hospitalization is associated with improved survival (combined endpoint of 6 month all-cause death or acute heart failure rehospitalization).48,49 However, at the moment, there is no evidence that titrating diuretic therapy based on B-lines can improve morbidity and mortality in patients hospitalized with HF.47
Although pleural effusions are typically monitored by chest X-ray in patients with acute HF, serial ultrasound scans are also effective in quantifying changes in the size of pleural effusion associated with decongestive therapy without exposing patients to radiation.50
Prognosis: determining the timing of discharge
Up to 45% of patients hospitalized with acute HF are either readmitted for HF or die within 12 months of discharge.51 Those with a higher degree of residual congestion, including pulmonary congestion, at the time of discharge, are at particularly high risk.51,52 The importance of optimizing decongestion during a HF hospitalization is consequently highlighted in the 2021 ESC Guidelines.6 Patients with a high number of B-lines at discharge are at higher risk of readmission or premature death than those discharged without or with only mild pulmonary congestion.35,36,52–54 Prior studies investigating the prevalence and prognostic value of B-lines at discharge in patients hospitalized with HF have employed 4, 8, or 28-zone LUS protocols; specific cut-off values for these protocols are summarized in Table 2. Collectively, these findings suggest that LUS may detect subclinical pulmonary congestion pre-discharge in patients with acute HF, irrespective of ejection fraction, and identify those at greater risk for subsequent adverse outcomes. In addition to B-lines, pleural effusion can be detected with ultrasound in approximately half of the patients discharged after an acute HF episode,27 but it is unclear whether this finding is associated with an increased risk of cardiovascular events post-discharge.56
Table 2.
Overview of select pre-discharge imaging protocols and cut-off values in acute HF
| Number of zones | B-line cut-off | Ultrasound equipment | HF readmission or death | Reference |
|---|---|---|---|---|
| 4 | ≥7 B-lines | High-end system; phased-array | 90 days: Adj. HR 3.03 (95% CI 1.45 to 6.31) |
Platz 201927 |
| 8 | ≥1 zone with ≥3 B-lines (one positive zone) on each hemithorax | High-end system; phased-array | 90 days: Adj. HR 3.30 (95% CI 1.00 to 10.91) |
Coiro 201535 |
| 28 | >15 B-lines | High-end system; phased-array | 180 days: Adj. HR 11.74 (95% CI 1.30 to 106.16) |
Gargani 201536 |
Adj., adjusted; CI, confidence interval; HF, heart failure; HR, hazard ratio.
Key points: The LUS pattern of pulmonary oedema in acute left-sided HF consists of the presence of multiple (at least three B-lines), diffuse (in at least two zones per hemithorax), and bilateral B-lines. Using LUS may be appropriate in patients with acute dyspnoea to rule in or rule out pulmonary oedema in suspected acute left-sided HF. Using LUS may be appropriate to detect persistent pulmonary congestion prior to discharge in patients hospitalized with acute HF, to identify those at higher risk of readmission for HF or death.
Chronic heart failure
During follow-up: guidance of diuretic therapy
The 2021 ESC Guidelines do not recommend serial echocardiography or assessment of B-lines in ambulatory patients with HF unless clinical deterioration is suspected. Indeed, many of those with HF who attend routine clinical appointments usually feel well, do not report any symptoms, and are free of congestion at clinical examination.57 However, decompensation is clinically silent in most patients and is often only recognized late, at a point when congestion demands urgent action. Thus, LUS could potentially be implemented in the routine clinical evaluation of outpatients, to facilitate early detection of subclinical congestion. In a single-centre, single-blind, randomized clinical trial, a LUS-guided strategy significantly improved the combined endpoint of urgent visit, rehospitalization, and death at 6 months after an acute HF episode.58 Subsequently, the CLUSTER-HF trial also showed that LUS-guided treatment was associated with a 45% risk reduction in the primary endpoint (a composite of urgent HF visits, rehospitalization for worsening HF, and death from any cause), mainly driven by a reduction in urgent HF visits.59 Another trial that randomized outpatients with chronic HF demonstrated a substantial reduction in hospitalizations for acute HF (by 56% at 90 days), as well as decreasing NT-proBNP concentrations and improving quality of life in those patients whose treatment was guided by LUS.60 A summary of the clinical utility of LUS in acute and chronic heart failure is shown in Table 3.
Table 3.
LUS in acute and chronic heart failure
| Aim | LUS picture | Advantages | |
|---|---|---|---|
| Acute heart failure | |||
| Diagnosis | Rule in and rule out acute left-sided HF in patients with dyspnoea. | Multiple, diffuse, bilateral B-lines rule in AHF. Absence of multiple, diffuse, bilateral B-lines rules out AHF. |
LUS improves diagnostic accuracy compared with standard strategy (chest X-ray + NT-proBNP). LUS reduces time to correct diagnosis. LUS detects subclinical pulmonary congestion in patients with HF who have mild or absent signs and symptoms. |
| Monitoring | Monitor decongestion during AHF hospitalization. | Reduction of the number of B-lines. Reduction of the size of pleural effusion, if any. |
Bedside monitoring to support decision-making in diuretic therapy and fluid management. A significant reduction of B-lines during hospitalization is associated with a lower risk of rehospitalization for AHF and death at 6 months. |
| Prognosis | Determine the timing of discharge. Detect persistent subclinical congestion at discharge to identify patients at higher risk of rehospitalization for AHF or death. |
Persistent B-lines at discharge, even with resolved signs and symptoms of HF. | A high number of B-lines at discharge predict rehospitalization for AHF and death at 3 months. |
| Chronic heart failure | |||
| During follow-up | Guide diuretic therapy after discharge. | Reduction of the number of B-lines. Reduction of the size of pleural effusion, if any. |
LUS-guided therapy might reduce risk of urgent HF visits and hospital admission for AHF. |
| Prognosis | Identification of patients at higher risk of rehospitalization for AHF or death. | Presence of B-lines at out-office visits, even without signs and symptoms of HF. | An elevated number of B-lines in outpatients predict hospitalization for AHF and death at 6 months. |
LUS, lung ultrasound; HF, heart failure; AHF, acute heart failure.
Key points: Integrating LUS into the routine evaluation of ambulatory patients with HF may be appropriate to titrate diuretic therapy and reduce HF-related adverse outcomes, in particular, the need for urgent visits.
During stress echocardiography
LUS can be easily performed during exercise testing, including stress echocardiography.31,61,62 The number of B-lines increases during exercise in patients with HF more than in controls.63,64 In patients with heart failure with reduced ejection fraction (HFrEF), peak B-lines are closely associated with resting NT-proBNP, peak VO2, and stress pulmonary artery systolic pressure.61 In patients with heart failure with preserved ejection fraction (HFpEF), the development of pulmonary congestion as measured by B-lines upon exercise correlates with exercise-induced worsening of diastolic function (particularly with peak E/e′ and global strain rate during late diastole).65 Haemodynamic studies further suggest that the acute development of pulmonary congestion during stress is related to an increase in pulmonary capillary hydrostatic pressure and systemic venous hypertension.66 Therefore, LUS during exercise can quantify the pulmonary congestion secondary to the raise in stress-induced intracardiac/pulmonary pressures.
Detecting a higher number of B-lines at peak exercise is associated with a greater risk of HF hospitalization and death in patients with both HFrEF61 and HFpEF. Overall, these findings suggest that LUS may complement standard exercise testing to improve HF diagnosis and risk stratification.67,68
In patients with chest pain and acute myocardial infarction
Patients with acute coronary syndromes may develop pulmonary congestion, especially during or soon after an ST-elevation myocardial infarction. A recent systematic review suggests that a high number of B-lines is a common finding in patients hospitalized with an acute coronary syndrome and identifies patients more likely to have adverse in-hospital and long-term outcomes.69 Whether assessment of B-lines might guide use of therapies that reduce pulmonary congestion after a myocardial infarction and improve morbidity and mortality in the short-term and long-term remains to be determined.
In patients with shock/hypotension
LUS can provide vital information when integrated with echocardiography in the assessment of hypotension and various types of shock, with the potential of detecting the underlying cause, and improving the quality of care delivered to critically ill patients.
In hypovolaemic shock, the presence of a normal LUS pattern confirms the presence of ‘dry’ lungs that has a very high negative predictive value in ruling out a cardiogenic cause of hypotension2,70 (Figure 8). Patients in cardiogenic shock due to LV failure or mitral/aortic valvular heart disease eventually develop pulmonary congestion that would appear by LUS as multiple, diffuse, and bilateral B-lines, associated with a regular pleural line13 (Figure 8).
Figure 8.
Integrated cardiopulmonary ultrasound for the differential diagnosis of respiratory and circulatory failure.
In patients with a pneumothorax, LUS has superior diagnostic sensitivity (88% vs. 52%) and similar specificity (99% vs. 100%) to chest X-ray.71 The combination of the absence of lung sliding (generating the barcode sign on M-mode), absence of B-lines, and the presence of a lung point (the transition point between a LUS pattern with lung sliding and without lung sliding) would suggest a pneumothorax as the cause of hypotension/shock (Figure 8).8 The visualization of a normal LUS pattern along with non-compressible peripheral deep veins due to a thrombus would suggest pulmonary embolism, especially when coupled with RV dilatation and dysfunction.72 Moreover, triangular/polygonal hypoechogenic peripheral consolidations with sharp margins may be detected, as the sonographic appearance of pulmonary infarctions (Figure 8).73
In septic shock, the lungs are a frequent source of sepsis, due to lobar pneumonia that can be diagnosed with LUS with high sensitivity, through the visualization of consolidations often with dynamic air bronchograms, commonly at the most dependant zones of the lungs, with or without adjacent pleural effusion. The presence of punctiform echoes within an otherwise anechogenic pleural effusion could indicate exudative pleural effusion/empyema.74 The lungs can develop B-lines due to ARDS because of septic shock of extrapulmonary origin. LUS can be very useful in monitoring areation/deareation, assessing disease progression and recruitment in ALI/ARDS (including COVID-19 pneumonia).75 LUS can be performed also during transoesophageal echocardiography through dedicated views of the posterior regions of the lungs where lung consolidations and pleural effusions are most often seen, with promising preliminary results.76
Key points: In patients with shock/hypotension, LUS can complement the standard clinical evaluation to improve diagnostic accuracy.
Integrated cardiopulmonary ultrasound
How to integrate echocardiography and LUS
Transthoracic echocardiography is guidelines-recommended as a key investigation in HF6 for the assessment of cardiac structure and function, defining HF phenotype based on LVEF measurement, as well identifying potential underlying aetiologies and mechanisms, and guiding the introduction of treatment. The 2021 ESC Guidelines also mention the use of LUS in acute settings to confirm a diagnosis of HF, especially when natriuretic peptide testing is not available,6 since pulmonary congestion is one of the main causes of hospital admission in patients with HF.17
Integrating cardiac and pulmonary assessments on ultrasound can help understand and identify the pulmonary consequences of structural or functional cardiac pathology, and potentially individualize patient management. Real-time interpretation of B-lines, together with the non-invasive haemodynamic signs that can be measured by echocardiography, can provide simultaneous assessments of the cardiac and pulmonary state, leading to more accurate diagnosis and earlier treatment initiation.77,78 The number of B-lines is related to invasive left ventricular end-diastolic pressure measurements,79 to E/e′,80 to tricuspid regurgitation velocity,42 to right ventricular (RV) function, and RV–pulmonary artery coupling.81 However, in patients with the same haemodynamic profile, the degree of pulmonary congestion as detected by B-lines can vary markedly. Therefore, echocardiography is useful to understand the aetiology of HF, whereas LUS B-lines are especially useful to detect the degree of pulmonary congestion. The routine assessment of B-lines may be particularly appropriate when either a high-end ultrasound machine or the expertise for more complex echocardiographic analyses is not readily available or when cardiac image quality is poor and initial diagnosis difficult. Therefore, whenever possible, these two aspects of the patient’s compensation status—haemodynamic congestion and pulmonary congestion—17 can be evaluated in an integrated ultrasound cardiopulmonary examination (Table 4). This approach can also provide concomitant information regarding perfusion (by the LV outflow tract time-velocity integral as a non-invasive index of cardiac output) and pulmonary congestion (by B-lines), in a less invasive way compared with right heart catheterization. The integration of B-lines with IVC is also valuable and integrates different information, since IVC diameter and collapsibility index are proxies for right atrial pressure, but also reflects intravascular volume status, whereas B-lines reflect extravascular lung water, which can be present in patients with either a normal or a dilated IVC.19
Table 4.
How to integrate echocardiographic and pulmonary findings to assess congestion status
| E/e′ and other echocardiographic signs of increased left ventricular filling pressures | B-lines | |
|---|---|---|
Normal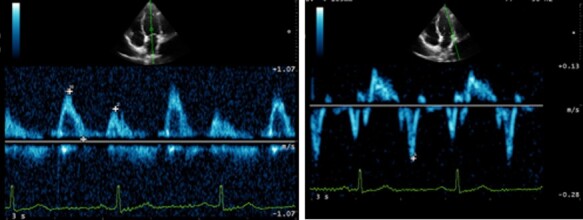
|
No B-lines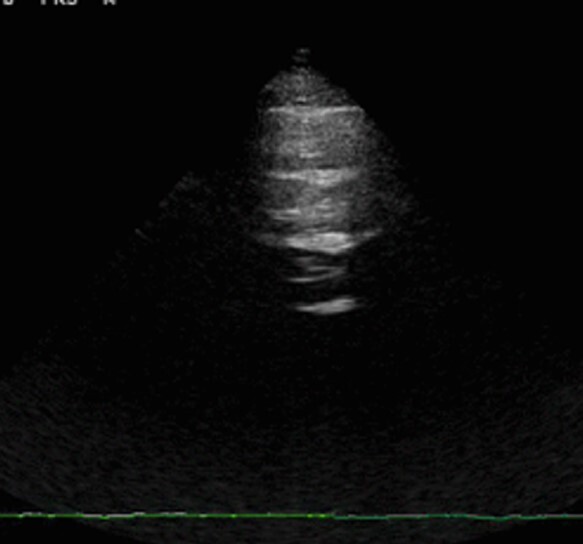
|
No congestion |
Increased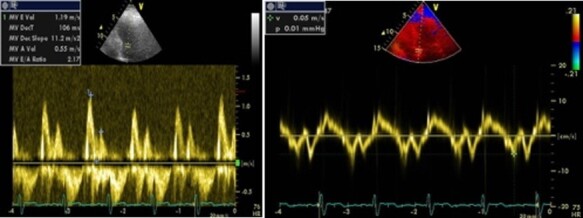
|
No B-lines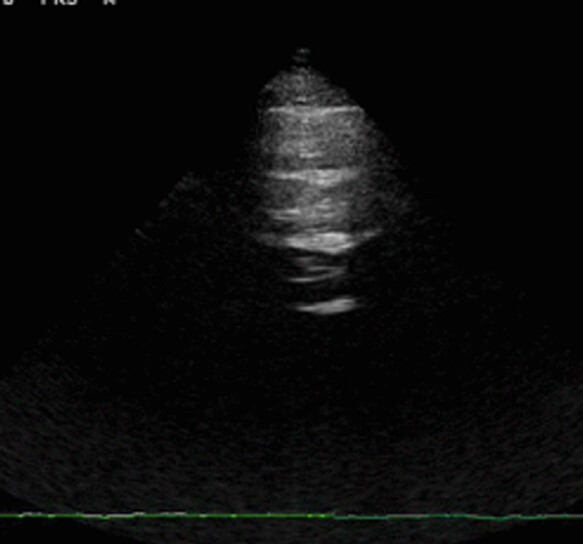
|
Haemodynamic congestion |
Increased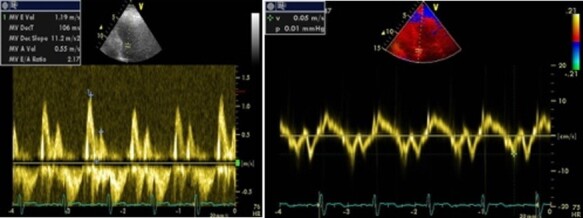
|
Multiple diffuse bilateral B-lines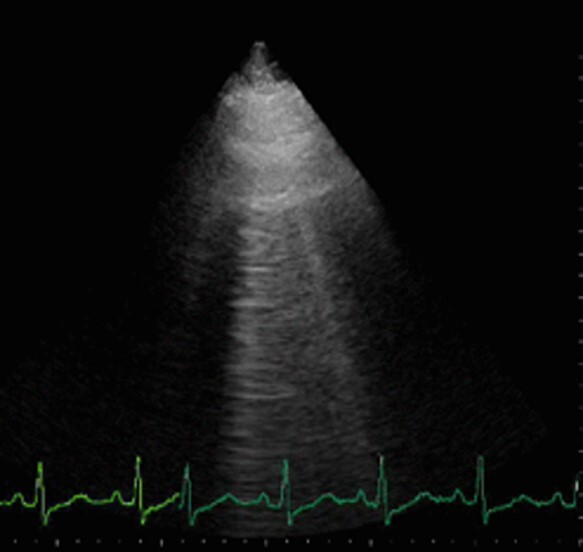
|
Haemodynamic and pulmonary congestion |
Normal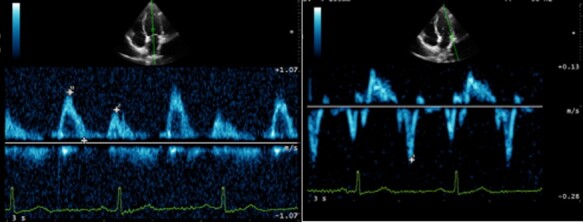
|
Multiple diffuse bilateral B-lines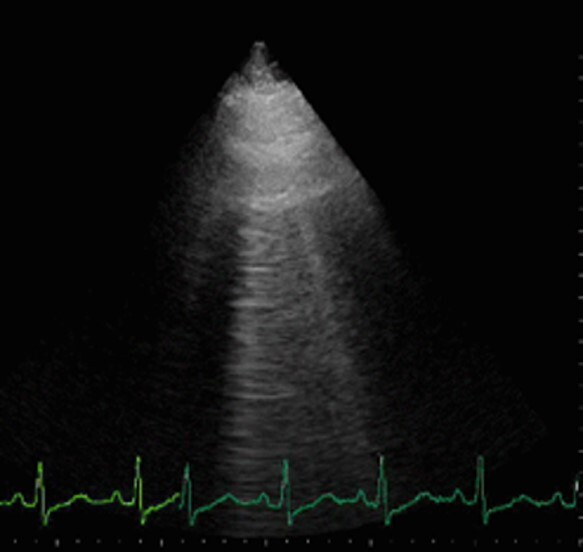
|
Pulmonary congestion without haemodynamic congestion (check for ALI/ARDS or other causes of B-lines) |
ALI, acute lung injury; ARDS, acute respiratory distress syndrome.
Key points: When evaluating patients with known or suspected HF, it is advised to integrate LUS B-lines in the echocardiographic assessment to provide information about the degree of pulmonary congestion, in both acute and chronic settings.
LUS in FoCUS
Focus cardiac ultrasound (FoCUS) is a point-of-care cardiac ultrasound examination performed according to a standardized, but restricted, scanning protocol in patients presenting with circulatory or respiratory compromise, chest pain or trauma, dyspnoea, syncope, or cardiac arrest.82 The FoCUS scanning protocol comprises five echocardiographic views sufficient for crude assessment of left and right ventricular size and function, pericardial effusion, and intravascular volume status.
Since cardiovascular and pulmonary diseases frequently coexist and may share clinical presentations, LUS may help in the differential diagnosis of acute dyspnoea and haemodynamic instability and is therefore an integral part of the FoCUS examination.82 The presence of multiple, diffuse, and bilateral B-lines in a dyspnoeic patient with LV dysfunction is almost unequivocally consistent with HFrEF. In the presence of left atrial dilation and/or visually-detected LV hypertrophy, multiple, diffuse, and bilateral B-lines may indicate HFpEF, and natriuretic peptide measurement and a comprehensive echocardiography should be ordered for further evaulation.82 Figure 8 summarizes the main situations of respiratory and circulatory failure, where LUS integrated with FoCUS can be of particular value.
Key points: Whenever possible, it is advised to integrate assessment of B-lines and pleural effusion into the FoCUS examination since it may help in the differential diagnosis of acute dyspnoea and haemodynamic instability.
Pitfalls
As with every diagnostic technique, there are some limitations with LUS examinations, which should be acknowledged to master this tool. There are still uncertainties about the exact physical origin of B-lines,11 although they are clearly related to a partial deaeration of the pulmonary parenchyma. LUS is an easy to learn ultrasound technique, with a short learning curve that can be limited to about 20 exams,83,84 but some training is needed to ensure reproducibility and the correct interpretation of findings. Initiatives that would ensure quality standards and safe patient care, for instance, a LUS certification programme, could facilitate the standardization of this procedure for both clinicians and other healthcare professionals involved in the care of patients with HF, who can successfully assess B-lines.85,86 B-lines are artefacts: although no clinically significant differences have been reported by using different machines and settings, attention should be paid to avoid magnification or deletion of artefactual images. Different LUS scanning protocols have been proposed and used, in research and in clinical practice, as previously discussed.
Probably, the main pitfall is the clinical interpretation of B-lines in the absence of an established diagnosis. B-lines are not specific for cardiogenic pulmonary oedema: being a sign of partial pulmonary deaeration, they can be present in patients with interstitial lung disease, such as pulmonary fibrosis, as well as ALI/ARDS, and interstitial pneumonia (including COVID-19 pneumonia). As highlighted in Table 1, there are some LUS features that can help differentiate these conditions, taking into account that a strong integration with clinical and other routine diagnostic findings is mandatory. This point further reinforces the need for LUS training, to ensure that healthcare providers will not categorize every patient with B-lines as having HF.
Importantly, the absence of substantial pulmonary congestion on ultrasound does not exclude HF, particularly in the context of severe obesity or isolated right-sided HF; therefore, clinicians should not forget to evaluate systemic/venous congestion.87
Gaps in current evidence
In recent years, major advances have been made in our understanding of the utility of LUS as an imaging tool in the diagnosis, monitoring, and risk stratification of patients with HF, but areas with lack of evidence remain. Table 5 lists selected topics that deserve to be addressed in future clinical research.
Table 5.
Gaps in current evidence
| Setting | Trials/studies needed | Main questions to be addressed |
|---|---|---|
| Acute heart failure | Additional randomized trials assessing whether LUS can improve the diagnosis and characterization of patients with AHF beyond traditional approaches. |
|
| Chronic heart failure | Development and validation of diagnostic protocols assessing the utility of LUS at rest or during exercise in the diagnosis of HFpEF. |
|
| Acute coronary syndromes | Additional randomized trials assessing whether LUS can improve the diagnosis of the aetiology of chest pain beyond traditional approaches. |
|
AHF, acute heart failure; HF, heart failure; HFrEF, heart failure with reduced ejection fraction; HFpEF, heart failure with preserved ejection fraction; LUS, lung ultrasound.
While waiting for additional evidence regarding the clinical utility of LUS, especially in titrating diuretic therapy, we already have solid data supporting the use of this tool in daily clinical practice to complement either FoCUS or comprehensive echocardiography in the assessment and management of patients with HF.
Conclusions
LUS is an easy to learn, rapid, and versatile point-of-care diagnostic method. B-lines on LUS are the sonographic sign of a partially deaerated lung, which can be detected in patients with HF, providing a semiquantitative evaluation of pulmonary interstitial oedema.
Sonographic B-lines are useful for the diagnosis, monitoring, and prognostic assessment of patients with HF. Therefore, it would be important to integrate routine evaluation of B-lines and pleural effusions into standard transthoracic echocardiographic protocols in patients with suspected or confirmed HF, as well as in the FoCUS examination. This integrated cardiopulmonary ultrasound approach has the potential to improve clinical management and outcomes, but further research is required.
Supplementary data
Supplementary data is available at European Heart Journal - Cardiovascular Imaging online.
Supplementary Material
Contributor Information
Luna Gargani, Department of Surgical, Medical and Molecular Pathology and Critical Care Medicine, University of Pisa, via Paradisa 2 5614, Pisa, Italy.
Nicolas Girerd, Université de Lorraine, Centre d'Investigations Cliniques Plurithématique 1433, Institut Lorrain du Cœur et des Vaisseaux Louis Mathieu, CHRU de Nancy, INSERM DCAC, F-CRIN INI-CRCT, Nancy, France.
Elke Platz, Cardiovascular Division, Brigham and Women’s Hospital and Harvard Medical School, Boston, USA.
Pierpaolo Pellicori, School of Cardiovascular and Metabolic Health, University of Glasgow, Glasgow, UK.
Ivan Stankovic, Clinical Hospital Centre Zemun, Faculty of Medicine, University of Belgrade, Serbia.
Alberto Palazzuoli, Cardiovascular Diseases Unit, Cardio-Thoracic and Vascular Department, Le Scotte Hospital, University of Siena, Italy.
Emanuele Pivetta, Medicina d'Urgenza-MECAU, Presidio Molinette, A.O.U. Città della Salute e della Scienza di Torino, Italy; Department of Medical Sciences, University of Turin, Turin, Italy.
Marcelo Haertel Miglioranza, EcoHaertel - Hospital Mae de Deus, Porto Alegre, Brazil; Federal University of Health Sciences of Porto Alegre, Porto Alegre, Brazil.
Hatem Soliman-Aboumarie, Department of Cardiothoracic Anaesthesia and Critical Care, Harefield Hospital, Royal Brompton and Harefield Hospitals, Guy’s and St Thomas NHS Foundation Trust, London, UK; School of Cardiovascular Medicine and Sciences, King’s College London, UK.
Eustachio Agricola, Cardiovascular Imaging Unit, Cardio-Thoracic-Vascular Department, San Raffaele Hospital, Vita-Salute University, Milan, Italy.
Giovanni Volpicelli, Department of Emergency Medicine, San Luigi Gonzaga University Hospital, Torino, Italy.
Susanna Price, Departments of Cardiology & Intensive Care, Royal Brompton & Harefield Hospitals, Guy’s and St Thomas NHS Foundation Trust, National Heart and Lung Institute, Imperial College London, London, UK.
Erwan Donal, University of Rennes, CHU Rennes, Inserm, Rennes, France.
Bernard Cosyns, Department of Cardiology, Universitair Ziekenhuis Brussel, Jette, Brussels, Belgium.
Aleksandar N Neskovic, Clinical Hospital Centre Zemun, Faculty of Medicine, University of Belgrade, Serbia.
This document was reviewed by members of the 2020–2022 EACVI Scientific Documents Committee:
Magnus Bäck, Philippe B Bertrand, Marc Dweck, Niall Keenan, and Leyla Elif Sade
Funding
None declared.
Data availability
No new data were generated or analysed in support of this research.
References
- 1. Lichtenstein D, Mezière G. A lung ultrasound sign allowing bedside distinction between pulmonary edema and COPD: the comet-tail artifact. Intensive Care Med 1998;24:1331–4. [DOI] [PubMed] [Google Scholar]
- 2. Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 2008;134:117–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Picano E, Frassi F, Agricola E, Gligorova S, Gargani L, Mottola G. Ultrasound lung comets: a clinically useful sign of extravascular lung water. J Am Soc Echocardiogr 2006;19:356–63 [DOI] [PubMed] [Google Scholar]
- 4. Gargani L. Ultrasound of the lungs: more than a room with a view. Heart Fail Clin 2019;15:297–303. [DOI] [PubMed] [Google Scholar]
- 5. Gargani L. Lung ultrasound: a new tool for the cardiologist. Cardiovasc Ultrasound 2011;9:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42:3599–726. [DOI] [PubMed] [Google Scholar]
- 7. Gargani L, Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound 2014;12:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 2012;38:577–91. [DOI] [PubMed] [Google Scholar]
- 9. Lichtenstein D, Mezière G, Biderman P, Gepner A, Barré O. The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 1997;156:1640–6. [DOI] [PubMed] [Google Scholar]
- 10. Jambrik Z, Gargani L, Adamicza Á, Kaszaki J, Varga A, Forster T et al. B-lines quantify the lung water content: a lung ultrasound versus lung gravimetry study in acute lung injury. Ultrasound Med Biol 2010;36:2004–10. [DOI] [PubMed] [Google Scholar]
- 11. Soldati G, Inchingolo R, Smargiassi A, Sher S, Nenna R, Inchingolo CD et al. Ex vivo lung sonography: morphologic-ultrasound relationship. Ultrasound Med Biol 2012;38:1169–79. [DOI] [PubMed] [Google Scholar]
- 12. Gargani L, Lionetti V, Di Cristofano C, Bevilacqua G, Recchia FA, Picano E. Early detection of acute lung injury uncoupled to hypoxemia in pigs using ultrasound lung comets. Crit Care Med 2007;35:2769–74. [DOI] [PubMed] [Google Scholar]
- 13. Copetti R, Soldati G, Copetti P. Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound 2008;6:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gargani L, Bruni C, Romei C, Frumento P, Moreo A, Agoston G et al. Prognostic value of lung ultrasound B-lines in systemic sclerosis. Chest 2020;158:1515–25. [DOI] [PubMed] [Google Scholar]
- 15. Balik M, Plasil P, Waldauf P, Pazout J, Fric M, Otahal M et al. Ultrasound estimation of volume of pleural fluid in mechanically ventilated patients. Intensive Care Med 2006;32:318–21. [DOI] [PubMed] [Google Scholar]
- 16. Roch A, Bojan M, Michelet P, Romain F, Bregeon F, Papazian L et al. Usefulness of ultrasonography in predicting pleural effusions >500 mL in patients receiving mechanical ventilation. Chest 2005;127:224–32. [DOI] [PubMed] [Google Scholar]
- 17. Gheorghiade M, Follath F, Ponikowski P, Barsuk JH, Blair JE, Cleland JG et al. Assessing and grading congestion in acute heart failure: a scientific statement from the acute heart failure committee of the heart failure association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. Eur J Heart Fail 2010;12:423–33. [DOI] [PubMed] [Google Scholar]
- 18. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 2010;23:685–713. [DOI] [PubMed] [Google Scholar]
- 19. Pellicori P, Carubelli V, Zhang J, Castiello T, Sherwi N, Clark AL et al. IVC diameter in patients with chronic heart failure: relationships and prognostic significance. JACC Cardiovasc Imaging 2013;6:16–28. [DOI] [PubMed] [Google Scholar]
- 20. Pellicori P, Shah P, Cuthbert J, Urbinati A, Zhang J, Kallvikbacka-Bennett A et al. Prevalence, pattern and clinical relevance of ultrasound indices of congestion in outpatients with heart failure. Eur J Heart Fail 2019;21:904–16. [DOI] [PubMed] [Google Scholar]
- 21. Pellicori P, Kallvikbacka-Bennett A, Dierckx R, Zhang J, Putzu P, Cuthbert J et al. Prognostic significance of ultrasound-assessed jugular vein distensibility in heart failure. Heart 2015;101:1149–58. [DOI] [PubMed] [Google Scholar]
- 22. Pellicori P, Platz E, Dauw J, Ter Maaten JM, Martens P, Pivetta E et al. Ultrasound imaging of congestion in heart failure: examinations beyond the heart. Eur J Heart Fail 2021;23:703–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Beaubien-Souligny W, Rola P, Haycock K, Bouchard J, Lamarche Y, Spiegel R et al. Quantifying systemic congestion with point-of-care ultrasound: development of the venous excess ultrasound grading system. Ultrasound J 2020;12:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Platz E, Jhund PS, Girerd N, Pivetta E, McMurray JJ V, Peacock WF et al. Expert consensus document: reporting checklist for quantification of pulmonary congestion by lung ultrasound in heart failure. Eur J Heart Fail 2019;21:844–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pivetta E, Goffi A, Lupia E, Tizzani M, Porrino G, Ferreri E et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the emergency department—a SIMEU multicenter study. Chest 2015;148:202–10. [DOI] [PubMed] [Google Scholar]
- 26. Pivetta E, Goffi A, Nazerian P, Castagno D, Tozzetti C, Tizzani P et al. Lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: a randomized controlled trial. Eur J Heart Fail 2019;21:754–66. [DOI] [PubMed] [Google Scholar]
- 27. Platz E, Campbell RT, Claggett B, Lewis EF, Groarke JD, Docherty KF et al. Lung ultrasound in acute heart failure: prevalence of pulmonary congestion and short- and long-term outcomes. JACC Heart Fail 2019;7:849–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Buessler A, Chouihed T, Duarte K, Bassand A, Huot-Marchand M, Gottwalles Y et al. Accuracy of several lung ultrasound methods for the diagnosis of acute heart failure in the ED: a multicenter prospective study. Chest 2020;157:99–110. [DOI] [PubMed] [Google Scholar]
- 29. Rastogi T, Bozec E, Pellicori P, Bayes-Genis A, Coiro S, Domingo M et al. Prognostic value and therapeutic utility of lung ultrasound in acute and chronic heart failure: a meta-analysis. JACC Cardiovasc Imaging 2022;15:950–2. [DOI] [PubMed] [Google Scholar]
- 30. Scali MC, Zagatina A, Simova I, Zhuravskaya N, Ciampi Q, Paterni M et al. B-lines with lung ultrasound: the optimal scan technique at rest and during stress. Ultrasound Med Biol 2017;43:2558–66. [DOI] [PubMed] [Google Scholar]
- 31. Merli E, Ciampi Q, Scali MC, Zagatina A, Merlo PM, Arbucci R et al. Pulmonary congestion during exercise stress echocardiography in ischemic and heart failure patients. Circ Cardiovasc Imaging 2022;15:e013558. [DOI] [PubMed] [Google Scholar]
- 32. Pivetta E, Baldassa F, Masellis S, Bovaro F, Lupia E, Maule MM. Sources of variability in the detection of B-lines, using lung ultrasound. Ultrasound Med Biol 2018;44:1212–6. [DOI] [PubMed] [Google Scholar]
- 33. Platz E, Pivetta E, Merz AA, Peck J, Rivero J, Cheng S. Impact of device selection and clip duration on lung ultrasound assessment in patients with heart failure. Am J Emerg Med 2015;33:1552–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Frasure SE, Matilsky DK, Siadecki SD, Platz E, Saul T, Lewiss RE. Impact of patient positioning on lung ultrasound findings in acute heart failure. Eur Heart J Acute Cardiovasc Care 2015;4:326–32. [DOI] [PubMed] [Google Scholar]
- 35. Coiro S, Rossignol P, Ambrosio G, Carluccio E, Alunni G, Murrone A et al. Prognostic value of residual pulmonary congestion at discharge assessed by lung ultrasound imaging in heart failure. Eur J Heart Fail 2015;17:1172–81. [DOI] [PubMed] [Google Scholar]
- 36. Gargani L, Pang PSS, Frassi F, Miglioranza MH, Dini FLL, Landi P et al. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: a lung ultrasound study. Cardiovasc Ultrasound 2015;13:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jambrik Z, Monti S, Coppola V, Agricola E, Mottola G, Miniati M et al. Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol 2004;93:1265–70. [DOI] [PubMed] [Google Scholar]
- 38. Gargani L, Sicari R, Raciti M, Serasini L, Passera M, Torino C et al. Efficacy of a remote web-based lung ultrasound training for nephrologists and cardiologists: a LUST trial sub-project. Nephrol Dial Transplant 2016;31:1982–8. [DOI] [PubMed] [Google Scholar]
- 39. Cibinel GA, Casoli G, Elia F, Padoan M, Pivetta E, Lupia E et al. Diagnostic accuracy and reproducibility of pleural and lung ultrasound in discriminating cardiogenic causes of acute dyspnea in the emergency department. Intern Emerg Med 2012;7:65–70. [DOI] [PubMed] [Google Scholar]
- 40. Mazzola M, Pugliese NR, Zavagli M, De Biase N, Bandini G, Barbarisi G et al. Diagnostic and prognostic value of lung ultrasound B-lines in acute heart failure with concomitant pneumonia. Front Cardiovasc Med 2021;8:693912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chiu L, Jairam MP, Chow R, Chiu N, Shen M, Alhassan A et al. Meta-analysis of point-of-care lung ultrasonography versus chest radiography in adults with symptoms of acute decompensated heart failure. Am J Cardiol 2022;174:89–95. [DOI] [PubMed] [Google Scholar]
- 42. Gargani L, Pugliese NR, Frassi F, Frumento P, Poggianti E, Mazzola M et al. Prognostic value of lung ultrasound in patients hospitalized for heart disease irrespective of symptoms and ejection fraction. ESC Heart Fail 2021;8:2660–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Volpicelli G, Caramello V, Cardinale L, Mussa A, Bar F, Frascisco MF. Bedside ultrasound of the lung for the monitoring of acute decompensated heart failure. Am J Emerg Med 2008;26:585–91. [DOI] [PubMed] [Google Scholar]
- 44. Cortellaro F, Ceriani E, Spinelli M, Campanella C, Bossi I, Coen D et al. Lung ultrasound for monitoring cardiogenic pulmonary edema. Intern Emerg Med 2016;12:1011–7. [DOI] [PubMed] [Google Scholar]
- 45. Martindale JL, Secko M, Kilpatrick JF, Ian S, Paladino L, Aherne A et al. Serial sonographic assessment of pulmonary edema in patients with hypertensive acute heart failure. J Ultrasound Med 2017;37:337–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mozzini C, Di Dio Perna M, Perna D, Pesce G, Garbin U, Meschi T et al. Lung ultrasound in internal medicine efficiently drives the management of patients with heart failure and speeds up the discharge time inferior cave vein collassability index. Intern Emerg Med 2017;13:27–33. [DOI] [PubMed] [Google Scholar]
- 47. Pang PS, Russell FM, Ehrman R, Ferre R, Gargani L, Levy PD et al. Lung Ultrasound-Guided Emergency Department Management of Acute Heart Failure (BLUSHED-AHF): a randomized controlled pilot trial. JACC Heart Fail 2021;9:638–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Öhman J, Harjola VP, Karjalainen P, Lassus J. Focused echocardiography and lung ultrasound protocol for guiding treatment in acute heart failure. ESC Heart Fail 2018;5:120–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Öhman J, Harjola VP, Karjalainen P, Lassus J. Assessment of early treatment response by rapid cardiothoracic ultrasound in acute heart failure: cardiac filling pressures, pulmonary congestion and mortality. Eur Heart J Acute Cardiovasc Care 2018;7:311–20. [DOI] [PubMed] [Google Scholar]
- 50. Brogi E, Gargani L, Bignami E, Barbariol F, Marra A, Forfori F et al. Thoracic ultrasound for pleural effusion in the intensive care unit: a narrative review from diagnosis to treatment. Critical Care 2017;21:325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ambrosy AP, Pang PS, Khan S, Konstam MA, Fonarow GC, Traver B et al. Clinical course and predictive value of congestion during hospitalization in patients admitted for worsening signs and symptoms of heart failure with reduced ejection fraction: findings from the EVEREST trial. Eur Heart J 2013;34:835–43. [DOI] [PubMed] [Google Scholar]
- 52. Chioncel O, Mebazaa A, Maggioni AP, Harjola VP, Rosano G, Laroche C et al. Acute heart failure congestion and perfusion status—impact of the clinical classification on in-hospital and long-term outcomes; insights from the ESC-EORP-HFA Heart Failure Long-Term Registry. Eur J Heart Fail 2019;21:1338–52. [DOI] [PubMed] [Google Scholar]
- 53. Cogliati C, Casazza G, Ceriani E, Torzillo D, Furlotti S, Bossi I et al. Lung ultrasound and short-term prognosis in heart failure patients. Int J Cardiol 2016;218:104–8. [DOI] [PubMed] [Google Scholar]
- 54. Palazzuoli A, Ruocco G, Beltrami M, Nuti R, Cleland JG. Combined use of lung ultrasound, B-type natriuretic peptide, and echocardiography for outcome prediction in patients with acute HFrEF and HFpEF. Clin Res Cardiol 2018;107:586–96. [DOI] [PubMed] [Google Scholar]
- 55. Coiro S, Porot G, Rossignol P, Ambrosio G, Carluccio E, Tritto I et al. Prognostic value of pulmonary congestion assessed by lung ultrasound imaging during heart failure hospitalisation: a two-centre cohort study. Sci Rep 2016;6:39426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lindner M, Thomas R, Claggett B, Lewis EF, Groarke J, Merz AA et al. Quantification of pleural effusions on thoracic ultrasound in acute heart failure. Eur Heart J Acute Cardiovasc Care 2020;9:513–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Pellicori P, Cleland JGF, Zhang J, Kallvikbacka-Bennett A, Urbinati A, Shah P et al. Cardiac dysfunction, congestion and loop diuretics: their relationship to prognosis in heart failure. Cardiovasc Drugs Ther 2016;30:599–609. [DOI] [PubMed] [Google Scholar]
- 58. Rivas-Lasarte M, Álvarez-García J, Fernández-Martínez J, Maestro A, López-López L, Solé-González E et al. Lung ultrasound-guided treatment in ambulatory patients with heart failure: a randomized controlled clinical trial (LUS-HF study). Eur J Heart Fail 2019;21:1605–13. [DOI] [PubMed] [Google Scholar]
- 59. Araiza-Garaygordobil D, Gopar-Nieto R, Martinez-Amezcua P, Cabello-López A, Alanis-Estrada G, Luna-Herbert A et al. A randomized controlled trial of lung ultrasound-guided therapy in heart failure (CLUSTER-HF study). Am Heart J 2020;227:31–9. [DOI] [PubMed] [Google Scholar]
- 60. Marini C, Fragasso G, Italia L, Sisakian H, Tufaro V, Ingallina G et al. Lung ultrasound-guided therapy reduces acute decompensation events in chronic heart failure. Heart 2020;106:1934–9. [DOI] [PubMed] [Google Scholar]
- 61. Scali MC, Cortigiani L, Simionuc A, Gregori D, Marzilli M, Picano E. Exercise-induced B-lines identify worse functional and prognostic stage in heart failure patients with depressed left ventricular ejection fraction. Eur J Heart Fail 2017;19:1468–78. [DOI] [PubMed] [Google Scholar]
- 62. Agricola E, Picano E, Oppizzi M, Pisani M, Meris A, Fragasso G et al. Assessment of stress-induced pulmonary interstitial edema by chest ultrasound during exercise echocardiography and its correlation with left ventricular function. J Am Soc Echocardiogr 2006;19:457–63. [DOI] [PubMed] [Google Scholar]
- 63. Simonovic D, Coiro S, Carluccio E, Girerd N, Deljanin-Ilic M, Cattadori G et al. Exercise elicits dynamic changes in extravascular lung water and haemodynamic congestion in heart failure patients with preserved ejection fraction. Eur J Heart Fail 2018;20:1366–9. [DOI] [PubMed] [Google Scholar]
- 64. Pugliese NR, Mazzola M, Fabiani I, Gargani L, De Biase N, Pedrinelli R et al. Haemodynamic and metabolic phenotyping of hypertensive patients with and without heart failure by combining cardiopulmonary and echocardiographic stress test. Eur J Heart Fail 2020;22:458–68. [DOI] [PubMed] [Google Scholar]
- 65. Simonovic D, Coiro S, Deljanin-Ilic M, Kobayashi M, Carluccio E, Girerd N et al. Exercise-induced B-lines in heart failure with preserved ejection fraction occur along with diastolic function worsening. ESC Heart Fail 2021;8:5068–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Reddy YNV, Obokata M, Wiley B, Koepp KE, Jorgenson CC, Egbe A et al. The haemodynamic basis of lung congestion during exercise in heart failure with preserved ejection fraction. Eur Heart J 2019;40:3721–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Coiro S, Simonovic D, Deljanin-Ilic M, Duarte K, Carluccio E, Cattadori G et al. Prognostic value of dynamic changes in pulmonary congestion during exercise stress echocardiography in heart failure with preserved ejection fraction. Circ Heart Fail 2020;13:e006769. [DOI] [PubMed] [Google Scholar]
- 68. Pugliese NR, De Biase N, Gargani L, Mazzola M, Conte L, Fabiani I et al. Predicting the transition to and progression of heart failure with preserved ejection fraction: a weighted risk score using bio-humoural, cardiopulmonary, and echocardiographic stress testing. Eur J Prev Cardiol 2021;28:1650–61. [DOI] [PubMed] [Google Scholar]
- 69. Lindner M, Lindsey A, Bain PA, Platz E. Prevalence and prognostic importance of lung ultrasound findings in acute coronary syndrome: a systematic review. Echocardiography 2021;38:2069–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Lancellotti P, Price S, Edvardsen T, Cosyns B, Neskovic AN, Dulgheru R et al. The use of echocardiography in acute cardiovascular care: recommendations of the European Association of Cardiovascular Imaging and the Acute Cardiovascular Care Association. Eur Heart J Cardiovasc Imaging 2015;16:119–46. [DOI] [PubMed] [Google Scholar]
- 71. Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest 2011;140:859–66. [DOI] [PubMed] [Google Scholar]
- 72. Nazerian P, Vanni S, Volpicelli G, Gigli C, Zanobetti M, Bartolucci M et al. Accuracy of point-of-care multiorgan ultrasonography for the diagnosis of pulmonary embolism. Chest 2013;145:950–7. [DOI] [PubMed] [Google Scholar]
- 73. Copetti R, Cominotto F, Meduri S, Orso D. The ‘survived lung:’ an ultrasound sign of ‘bubbly consolidation’ pulmonary infarction. Ultrasound Med Biol 2020;46:2546–50. [DOI] [PubMed] [Google Scholar]
- 74. Lichtenstein DA. Ultrasound in the management of thoracic disease. Crit Care Med 2007;35:S250–61. [DOI] [PubMed] [Google Scholar]
- 75. Gargani L, Soliman-Aboumarie H, Volpicelli G, Corradi F, Pastore MC, Cameli M. Why, when, and how to use lung ultrasound during the COVID-19 pandemic: enthusiasm and caution. Eur Heart J Cardiovasc Imaging 2020;21:941–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Cavayas YA, Girard M, Desjardins G, Denault AY. Transesophageal lung ultrasonography: a novel technique for investigating hypoxemia. Can J Anesthesia 2016;63:1266–76. [DOI] [PubMed] [Google Scholar]
- 77. Russell FM, Ehrman RR, Cosby K, Ansari A, Tseeng S, Christain E et al. Diagnosing acute heart failure in patients with undifferentiated dyspnea: a lung and cardiac ultrasound (LuCUS) protocol. Acad Emerg Med 2015;22:182–91. [DOI] [PubMed] [Google Scholar]
- 78. Čelutkienė J, Lainscak M, Anderson L, Gayat E, Grapsa J, Harjola VP et al. Imaging in patients with suspected acute heart failure: timeline approach position statement on behalf of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2020;22:181–95. [DOI] [PubMed] [Google Scholar]
- 79. Hubert A, Girerd N, Le Breton H, Galli E, Latar I, Fournet M et al. Diagnostic accuracy of lung ultrasound for identification of elevated left ventricular filling pressure. Int J Cardiol 2019;281:62–8. [DOI] [PubMed] [Google Scholar]
- 80. Miglioranza MH, Gargani L, Sant’anna RT, Rover MM, Martins VM, Mantovani A et al. Lung ultrasound for the evaluation of pulmonary congestion in outpatients: a comparison with clinical assessment, natriuretic peptides, and echocardiography. JACC Cardiovasc Imaging 2013;6:1141–51. [DOI] [PubMed] [Google Scholar]
- 81. Kobayashi M, Gargani L, Palazzuoli A, Ambrosio G, Bayés-Genis A, Lupon J et al. Association between right-sided cardiac function and ultrasound-based pulmonary congestion on acutely decompensated heart failure: findings from a pooled analysis of four cohort studies. Clin Res Cardiol 2021;110:1181–92. [DOI] [PubMed] [Google Scholar]
- 82. Neskovic AN, Skinner H, Price S, Via G, De Hert S, Stankovic I et al. Focus cardiac ultrasound core curriculum and core syllabus of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2018;19:475–81. [DOI] [PubMed] [Google Scholar]
- 83. Bedetti G, Gargani L, Corbisiero A, Frassi F, Poggianti E, Mottola G. Evaluation of ultrasound lung comets by hand-held echocardiography. Cardiovasc Ultrasound 2006;4:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Noble VE, Lamhaut L, Capp R, Bosson N, Liteplo A, Marx JS et al. Evaluation of a thoracic ultrasound training module for the detection of pneumothorax and pulmonary edema by prehospital physician care providers. BMC Med Educ 2009;9:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Zisis G, Yang Y, Huynh Q, Whitmore K, Lay M, Wright L et al. Nurse-provided lung and inferior vena cava assessment in patients with heart failure. J Am Coll Cardiol 2022;80:513–23. [DOI] [PubMed] [Google Scholar]
- 86. de Souza LAM, Paredes RG, Giraldi T, Franco MH, de Carvalho-Filho MA, Cecilio-Fernandes D et al. Implementation and assessment of lung ultrasound training curriculum for physiotherapists with a focus on image acquisition and calculation of an aeration score. Ultrasound Med Biol 2022;48:2119–27. [DOI] [PubMed] [Google Scholar]
- 87. Palazzuoli A, Ruocco G, Franci B, Evangelista I, Lucani B, Nuti R et al. Ultrasound indices of congestion in patients with acute heart failure according to body mass index. Clin Res Cardiol 2020;109:1423–33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No new data were generated or analysed in support of this research.