Abstract
Adoptive cellular immunotherapy of cancer has been limited to date mostly due to the poor immunogenicity of tumor cells, the immunocompromised status of cancer patients in advanced stages of their disease, and difficulties in raising sufficient numbers of autologous tumor-specific T lymphocytes. On the other hand, the slow tumor penetration and short half-life of exogenously administered tumor-specific monoclonal antibodies have provided major obstacles for an effective destruction of tumor cells by the humoral effector arm of the immune system. Attempts to improve the efficacy of adoptive cellular cancer immunotherapy have led to the development of novel strategies that combine advantages of T cell-based (i.e., efficient tumor penetration, cytokine release and cytotoxicity) and antibody-based (high specificity for tumor-associated antigens) immunotherapy by grafting cytotoxic T lymphocytes (CTLs) with chimeric receptors composed of antibody fragments (which recognize tumor-cell antigens) and a cellular activation motif. Antigen recognition is therefore not restricted by major histocompatibility genes, as the physiological T-cell receptor, but rather is directed to native cell surface structures. Since the requirements of major histocompatibility complex (MHC) restriction in the interaction of effector cells with target cells are bypassed, the tumor cell–binding of CTLs grafted with chimeric receptors is not affected by down-regulation of HLA class I antigens and by defects in the antigen-processing machinery. Ligand binding by the chimeric receptor triggers phosphorylation of immunoglobulin tyrosine activation motifs (ITAMs) in the cytoplasmic region of the molecule and this activates a signaling cascade that is required for the induction of cytotoxicity, cytokine secretion and proliferation. Here, the authors discuss the potential of lymphocytes grafted with chimeric antigen receptors in the immunotherapy of malignant disease.
Keywords: Cancer immunotherapy, Chimeric antigen receptors, Costimulatory molecules, Single-chain Fv, Tumor immunosurveillance
Introduction
In order for the immune system to react against tumor cells, it must have antigens (tumor-associated antigens [TAAs]) that are recognized as foreign. Studies in animal models have shown that CD8+ T cells are critical effectors that have the capability of recognizing TAAs and eradicating tumors in vivo. Cytotoxic T lymphocytes (CTLs) recognize 8–10 amino acid–long TAA-derived peptide fragments. TAAs, as well as other cellular proteins, are degraded in the cytoplasm by proteasomes into short peptides, which are then transported into the endoplasmic reticulum where they complex with newly synthesized major histocompatibility complex (MHC) class I molecules. These peptide–MHC class I antigen complexes are then transported to the cell surface for presentation to CD8+ T cells [1].
Major histocompatibility complex class I antigens are lost or down-regulated in many types of human tumors. The frequency of altered HLA class I antigen expression in human tumors is summarized as loss and/or down-regulation of monomorphic determinants or selective down-regulation of one or more allospecificity(ies) [2, 3]. MHC class I antigen down-regulation in tumor cells represents a major mechanism of escape from immunosurveillance. This notion was supported by the enhanced growth of tumor cells which had down-regulated MHC class I antigen expression following transfection with antisense DNA [4] and by the loss of tumorigenicity of aggressive MHC class I–negative mouse tumor cells following transfection with MHC class I genes [5].
For several years, much effort has been directed toward establishing adoptive cellular immunotherapy as a major modality in cancer treatment. Lymphokine-activated killer (LAK) cells and tumor-infiltrating lymphocytes (TILs) have shown therapeutic responses in clinical trials, although they were observed in only a limited number of treated patients. Tumor-specific MHC-restricted CTLs have been isolated, primarily specific for melanoma, but the availability of tumor-specific lymphocytes against more common types of cancer for adoptive therapy has been limited due to difficulties in generating these tumor-specific CTLs. The humoral effector arm of the immune system has also been demonstrated to be involved in the destruction of tumor cells, mostly via monoclonal antibodies (mAbs) raised against TAAs. Appreciation of the complementary nature of T cell– and antibody-based immunotherapy stimulated interest in developing approaches that combine their advantages and minimize their limitations. This trend led to the development of immunotherapy with bispecific mAbs, which mediate cellular destruction of tumor cells by binding tumor target cells with one domain and effector cells with the other one. Another approach, merging T-cell functions with antibody specificities, was to create engineered T-cell receptors (TCRs) composed of single-chain variable domains of mAbs (scFv) fused to signaling components of the TCR-CD3 complex (TCR ζ chain) or the low-affinity receptor for IgG, FcγR III (CD16) (γ chain). This approach therefore combines the antigen-binding capabilities of antibodies (e.g., non-MHC-restricted recognition of TAAs) with the potent antitumor activity of T cells (e.g., cytotoxicity). This should enable the generation of antitumor responses against tumor variants with MHC class I antigen decrease or loss through the production of specific T cells against any antigen for which an mAb exists and would generalize the use of adoptive immunotherapy for several types of cancer. The review below will analyze tumor cell targeting by chimeric gene products consisting of a tumor-specific antibody moiety and a lymphocyte-derived signaling domain.
Targeting of tumor cells by lymphocytes bearing chimeric antigen receptors
Adoptive cellular immunotherapy uses the administration of immune effector cells (e.g., T lymphocytes) for the treatment of cancer. LAK cells and TILs have shown therapeutic responses in clinical trials, although these were observed in only a small fraction of the patients treated [6, 7]. TILs primarily from melanoma [6, 8] and later from other types of cancer [9, 10] have also been used as a source for the isolation of tumor-specific MHC-restricted CTLs, but the availability of such tumor-specific lymphocytes in large numbers has been hampered mostly due to technical difficulties. Another practical limitation in the clinical use of TILs in adoptive immunotherapy is that patients’ lymphocytes usually inefficiently respond to their own tumors so that the generation of large numbers of functional TILs with specific autologous tumor reactivity has proven difficult. To circumvent the limitations associated with the availability of large numbers of autologous tumor–specific lymphocytes, new approaches were designed to target T cells to important protein molecules expressed on the cell surface of tumor cells. Broadening of the range of tumor specificity has been primarily obtained by combining the lytic capacity of T cells with the selectivity of tumor-specific mAbs. Bispecific antibodies (BsAbs) specifically targeting T cells with tumor targets, discussed in the previous section, have been initially employed in this direction. However, the use of mAbs for therapy may be hampered by the inaccessibility of solid tumors to antibody penetration [11]. Moreover, BsAb-redirected CTLs retain the BsAbs for only limited periods of time (2–3 days) due to their dissociation from the CTL surface [12, 13]. Moreover, BsAb-redirected CTLs lose signal-transducing and therefore lytic capacity following target cell recognition, lysis, and TCR-CD3 complex clustering [12].
Another approach for redirecting T-cell responses to TAAs includes the genetic manipulation of the recognition specificity of T cells by grafting the recognition specificity of an antibody onto the signaling components of the TCR-CD3 complex [14–16], or the low-affinity receptor for IgG, FcγRIII, to create chimeric antigen receptors (CARs).
Chimeric antigen receptors
The methodology for constructing chimeric antigen receptors (CARs) was first established by fusing immunoglobulin variable (V) genes to the constant domains of the α and β chains of TCRs [17]. Subsequently, other CAR designs joined the coding sequence of an antibody-derived single-chain Fv (scFv) targeting a TAA to the transmembrane and intracytoplasmic sequences of T-cell–signaling molecules [18, 19]. The design of such chimeric constructs was based on previous findings showing that ζ and γ signaling moieties fused to other (than scFv) extracellular domains could be expressed as functional receptors [20–22]. The scFv/ζ or γ chimeric genes were then transfected into CTLs, thereby conferring on them the capacity to specifically target, in a non-MHC-restricted fashion, tumor cells expressing that particular TAA. Thus, such CARs combine the advantage of antibody specificity with the homing, tissue penetration, and target cell destruction mediated by T cells.
Construction of CARs
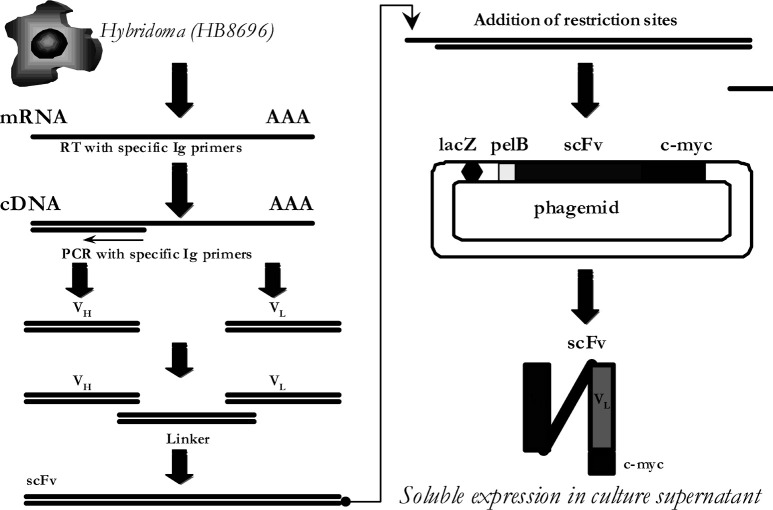
Chimeric antigen receptors genes comprise a recognition unit with a transmembrane part and a cytoplasmic signaling domain for cellular activation. The extracellular recognition domains may be derived from an immunoglobulin scFv or a ligand-binding domain of a heterologous receptor. With respect to the later, several reports [23–25] have previously described an HIV-specific CAR composed of the extracellular domain of CD4 fused to ζ chain. CD4 binds to the gp120 moiety of the HIV envelope protein expressed on the surface of virally infected cells. When CD4 ζ was introduced into mature human CD8+ T cells via retroviral-mediated transduction, cytotoxic function could be efficiently and specifically detected against gp120-expressing cells in vitro. In a similar fashion, Nolan et al. [16] designed a CAR consisting of non-antibody-derived domains as extracellular recognition unit targeting cancer cells expressing the carcinoembryonic antigen (CEA). However, the vast majority of CARs use scFv-based constructs that comprise the V regions of the heavy and light chains of an mAb joined together by a flexible peptide linker [26]. We have recently succeeded in the construction of an scFv recognizing HER-2/neu expressed on tumor cell lines of different histological type [27, 28] (Fig. 1). For this, total cellular RNA was isolated from the hybridoma cells HB8696 producing murine anti-HER-2/neu mAb. In the second step, we synthesized VH and VL cDNAs using specific oligonucleotide Ig primers.
Fig. 1.
Construction of single-chain Fv fragment. mRNA was isolated from the murine hybridoma cells HB8696 producing anti-HER-2/neu mAb, followed by synthesis of first strand cDNA. PCR amplification was performed for both Ig heavy and light chains with the use of cDNA as a template. Sets of sense and antisense PCR primers were designed to amplify the VH and VL regions. After the first round of PCR, VH and VL genes were purified and on a second round PCR these were linked by a (Gly4 Ser)3 linker. The assembled scFv PCR products were ligated into the pHEN1 phagemid, which also contained the c-myc tag peptide as a recognition marker. E. Coli transformed with the pHEN1-scFv produced soluble scFv, which was isolated and purified from culture supernatants
Subsequently, for the construction of the scFv fragment of anti-HER-2/neu, the VH and VL cDNAs were specifically amplified and assembled as an scFv with a suitable linker. The assembled scFv fragment was inserted into the phagemid pHEN1 and expressed in E. Coli. The pHEN1 phagemid also contained the c-myc tag peptide so that the binding of our scFv on HER-2/neu+ tumor cells could be detected by an anti-myc mAb.
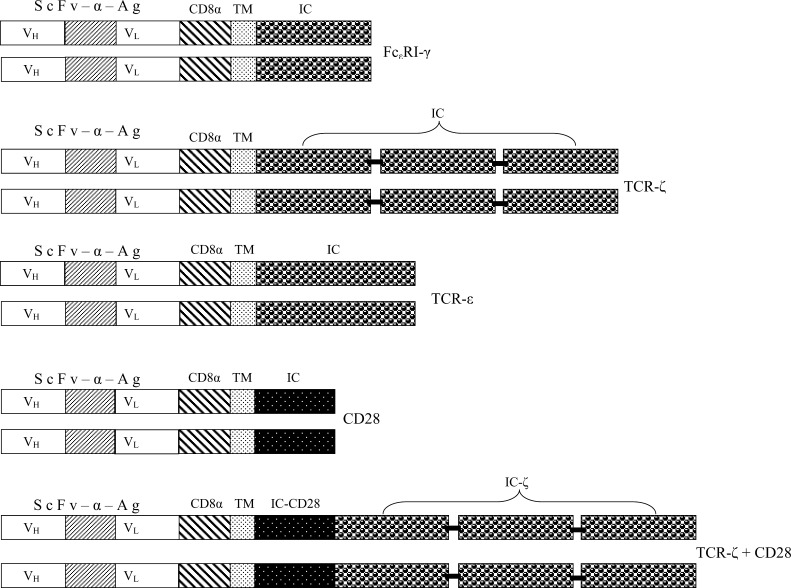
The structural requirements for efficient targeting of tumor cells by CARs may differ according to the tumor antigen recognized and the tumor-antigen recognition domain itself. In general, by increasing the distance between the recognition domain and the membrane by the insertion of a flexible spacer segment, we may enhance the binding capacity by providing better access to the target protein [23, 24, 29]. However, this should not be considered a general rule since we have recently demonstrated the capacity of MD.45 hybridoma cells engrafted with CARs harboring a HER-2/neu–recognizing scFv fused to ζ- or γ-signaling chains, without a linker in between, to efficiently lyse both in vitro and in vivo HER-2/neu–expressing tumor cell lines [27, 28]. Similar to this, Hombach et al. [30] recently reported on the construction of recombinant immunoreceptors with specificity for CEA which upon transduction could redirect peripheral blood mononuclear cells (PBMCs) to an MHC-independent antitumor response. On the other hand, CARs with anti-HER-2/neu or anti-CEA scFv linked to the ζ- or γ- signaling domains via CD8α Ig-like hinge region have been also reported to successfully redirect the specificity of lymphocytes toward HER-2/neu– or CEA-expressing tumor cells. Since in these reports the scFvs for either of the tumor antigens recognized were derived from different mAbs, it can be assumed that the utilization or not of a flexible linker between the recognition and signaling regions may depend on the binding affinity of the tumor-specific mAb from which the scFvs are derived. A schematic presentation of CAR is given in Fig. 2.
Fig. 2.
Schematic representation of a scFv (anti-HER-2/neu)-ζ or -γ construct. The Moloney murine leukemia virus 5′ long terminal repeat (LTR) controls the expression of the CAR scFv (HB8696) ζ or γ, which consists of an N-terminal heavy chain leader peptide (L), the HER-2/neu–specific single-chain antibody scFv (hb8696), an myc-tag (shown in Fig. 1), the hinge region of CD8 α chain, and the CD3 ζ or FcɛRI γ chain. The neomycin-resistance gene for G418 selection of transduced cells is driven by the SV40 early promoter
Signaling mediated by CARs
Different signaling moieties have been successfully used as transducing units for cellular activation in CARs (Table 1 and Fig. 3). These belong to the family of proteins that include the structurally and functionally related TCR- and FcR-associated ζ and γ polypeptides, respectively [23]. Engagement of TCRs and FcR on T cells and natural killer (NK) cells, respectively, are critical events in initiating host immune defense against virally infected cells and also tumor cells [31–33]. The signaling events downstream of both TCR and FcR involve rapid phosphorylation of Ig tyrosine activation motifs (ITAMs) situated in the cytoplasmic domains of these immune receptor complexes and the subsequent activation of Scr family and ZAP-70 and Syk kinases [34–36]. Each ITAM sequence contains a pair of YXXL motifs separated by seven amino acids. It is these variable flanking amino acids that ultimately dictate, through recruitment of specific protein kinases, the signaling capability and function of the γ and ζ chains [37, 38]. The subsequent induction of multiple downstream signaling cascades leads to cell activation and stimulation of critical biological effector functions such as cytolysis, cytokine release, and phagocytosis [39, 40]. During the course of tumor progression, host T cells appear to be immunosuppressed so that they do not respond, or poorly respond, to activating stimuli [21]. Such defects in immune function are, at least partly, attributed to abnormal expression of signal-transduction molecules [41, 42]. Since CARs are dependent on TCR proximal protein tyrosine kinases for signaling, the approach of genetic manipulation of patients’ T cells with CARs would be problematic. To bypass this problem, Fitzer-Atlas et al. [43] constructed a chimeric receptor that joins the extracellular scFv to an intracellular protein tyrosine kinase for signal transduction. Stimulation through the scFv-protein tyrosine kinase receptor bypassed defective TCR-proximal events and directly accessed T-cell effector mechanisms.
Table 1.
Tumor antigens targeted by lymphocytes grafted with CARs containing various signaling units
| Signaling molecule | Recognition unit | Target antigen | References |
|---|---|---|---|
| TCR-ζ | Fab or scFv | HER-2/neu | [27, 28, 44, 48] |
| CEA | [1, 78, 81] | ||
| TAG-72 | [71] | ||
| GD3 | [42] | ||
| PSMA | [81] | ||
| EGP2 | [76] | ||
| GD2 | [82] | ||
| CD19 | [74] | ||
| FcɛRI-γ | scFv | CEA | [45, 69] |
| EGP40 | [83] | ||
| FBP | [72, 73] | ||
| G250 | [37, 84] | ||
| EGP2 | [76] | ||
| PTK | scFv | TNP | [23] |
| TCR-ɛ | Fab | GD3 | [42] |
| CD28 | scFv | GD2 | [85] |
| TCR-ζ and CD28 | scFv | CEA | [30] |
| PSMA | [59] | ||
| HER-2/neu | [1] |
Fig. 3.
Examples of CARs. CARs interact with their antigen (Ag)-binding regions of Ig (scFv-α-Ag) that consist of VH and VL chains linked by a short peptide linker. CD8 α chain functions in many cases as a flexible linker. CARs also incorporate the transmembrane (TM) and intracellular (IC) signaling domains of the Fcγ, TCR, and CD28, as shown
Signaling through CARs follows a similar pathway to that observed after triggering TCRs with MHC-peptide complexes [33, 35] that results in cellular activation characterized by cytokine production and cytolysis of tumor cells expressing the relevant antigen by perforin- and Fas ligand–dependent mechanisms [14–16, 19, 26, 27, 29, 30, 44–47]. Cytokine production by the CAR-modified lymphocytes seems to be critical for tumor eradication in vivo. In a recent report, Darcy et al. [45] transduced primary lymphocytes from gene-knockout mice with CAR-recognizing CEA and demonstrated that IFN-γ is essential for achieving tumor eradication by inducing mechanisms resulting in activation of the innate arm of immunity and/or inhibition of tumor angiogenesis. Similar results were produced by Nolan et al. [16] who transduced CD4+ Jurkat T cells or primary CD8+ T cells with four different constructs targeting CEA, three of which (Fαb-ζ, scFv-ζ, and Fαb-ɛ) showed specific binding on CEA-expressing tumor cells followed by IL-2 secretion and expression of cytotoxicity by the transduced cells. In contrast, sFv-ɛ was inert solely against cellular targets for steric reasons unique to this construct and did not activate the transduced cells to produce IL-2.
We have provided the γ chain of Fc(ɛ)RI or the ζ chain of TCR with an extracellular recognition domain (scFv) from an anti-HER-2/neu mAb produced by the HB8696 hybridoma (Figs. 1 and 2) [27, 28]. Retroviral gene transfer was used to stably integrate and express the chimeric construct in the H-2b allospecific murine MD.45 CTL hybridoma. MD.45-HER/γ or ζ cells were capable of specifically recognizing HER-2/neu+ tumors derived from different types of human cancers. Such recognition led to tumor cell lysis and cytokine release by the MD.45-HER cells. Thus, our approach exploited the scFv (anti-HER-2/neu) as the antigen-recognition unit and the potent cytotoxic responses of T lymphocytes and/or the ability of T cells to secrete cytokines upon activation at the target site, thus recruiting, regulating, and amplifying other branches of the immune system.
Chimeric constructs containing a single-chain antibody directed against the human ErbB-2 receptor have been previously demonstrated to redirect T-cell specificity toward mouse epithelial cells transformed to express the human ErbB-2 as well as against human MDA-MB453 breast cancer cells constitutively expressing ErbB-2 [44, 48]. In those studies the recognition function was contributed by the scFv domain derived from the mAb FRP5 [49] that is specific for the extracellular domain of ErbB-2, whereas the signaling component was provided by the ζ chain of the TCR. Our constructs, although recognizing the same receptor, differ in the scFv, which is derived from an anti-HER-2/neu mAb produced by the HB8696 hybridoma. Whether these constructs recognize different epitopes on the extracellular domain of HER-2/neu, or not, is not known. Competitive-binding inhibition experiments on HER-2/neu+ tumor cell lines utilizing both scFv may clarify this point. However, irrespective of this, our published data demonstrate that the HER-2/neu epitope recognized by our scFv is expressed on tumor cell lines from various types of HER-2/neu+ human cancers (i.e., breast, ovary, colon, and renal) thus making its use in future therapeutic interventions more attractive.
In our studies [27, 28], we have also evaluated the in vivo antitumor activity of MD.45-HER cells by using various SCID mouse / human tumor models. A strong antitumor effect of MD.45-HER was observed in vivo when these cells were implanted simultaneously with HER-2/neu+ human tumor cell lines and for the following 2 days (one injection per day) in SCID mice. Tumor growth was considerably reduced, and treated mice survived over 4 months as compared to approximately 1-month survival in the control group. The antitumor effect observed was not due to the administration of the MD.45 cells per se, but dependent on the transduction of the scFv (anti-HER-2/neu)/γ or ζ-fusion gene. MD.45 cells transduced with fusion gene scFv (anti-TNP)/γ or ζ to recognize TNP did not affect tumor growth. Furthermore, the in vivo antitumor effect of MD-45-HER cells was specific for HER-2/neu–expressing tumor cell lines, since the growth of melanoma cell line FM3 which does not express HER-2/neu was not affected by MD.45-HER cells, whereas the growth of HER-2/neu–transfected FM3 cells was delayed to an extent similar to that in other models used (i.e., SKBR3, SKOV3, A-498, and HCT116). Another interesting point which came out of our studies is that the MD.45-HER cells must have the ability to traffic and target tumor cells in vivo since these were given i.p., whereas the HER-2/neu+ tumor cells were given s.c. It is also important to note that the in vivo antitumor activity was observed in the absence of exogenously added IL-2, demonstrating that the IL-2 (and most probably IFN-γ) produced by the MD.45-HER cells upon encountering the tumor cells (as shown in in vitro experiments) was sufficient to support their in vivo activity. This is an important issue, since, clinically, IL-2 administration has been associated with significant toxicity.
CAR including costimulatory genes
The engagement of ζ- or γ-signaling chains, although sufficient to induce tumoricidal activity, may not suffice to elicit substantial lymphocyte activation (measured by IL-2 secretion) in the absence of a concomitant costimulatory signal. A number of molecules with costimulatory signaling capacity in T cells have been identified, including CD2 [50], CD4 and CD8 [51], CD5 [52], and CD28 [53, 54]. CD28 in particular has been shown to play a key role in the activation of naïve T cells through interaction with members of the B7 family of molecules expressed on antigen-presenting cells [55]. The short intracellular domain of CD28 serves to initiate a signal transduction cascade, which is distinct from the primary signal initiated by the TCR. On binding of the extracellular domain of CD28 to B7, the intracellular domain of CD28 becomes phosphorylated at the tyrosine residue in a motif that conforms to the consensus amino acid sequence YMXM. This is a member of a subgroup of so-called intracellular tyrosine-based activation motifs that serve to recruit the receptor-specific signaling proteins containing phosphotyrosine-binding SH2 domains. Three molecules to date have been shown to bind phosphorylated CD28: the regulatory subunit (p85) of phosphatidylinositol 3′-kinase, the tyrosine kinase ITK (inducible T-cell kinase), and the adaptor molecule grb-2 [56]. The mechanism by which ligand binding leads to phosphorylation and recruitment of molecules capable of mediating intracellular signaling is not completely understood, but at least in some circumstances, receptor oligomerization may be sufficient to initiate signal transduction.
Engineering human T cells so that they receive a costimulatory signal in a tumor antigen-dependent manner may be extremely valuable. An important development in this respect has been the successful cross-linking of a chimeric receptor comprising a CD8 extracellular domain and a CD28 intracellular domain, which led to activation of phosphatidylinositol 3′-kinase and enhanced IL-2 production in Jurkat cells [57]. A chimeric receptor [24] similar to those described above, with an extracellular scFv-binding domain, but with a CD28 intracellular domain in place of the TCR ζ chain, has been shown to deliver costimulatory signals similar to those elicited by cross-linking of unmodified CD28 when combined with stimulation via the TCR-CD3 complex. In the same report, double transfectants expressing scFv-CD28 and scFv-ζ chimeric receptors, with specificities for different haptens, were shown to produce maximal levels of IL-2 in response to specific antigens. In another report, Finney et al. [58] sought to investigate the concept of providing primary and costimulatory signaling from a single gene product. They described single-chain chimeric receptors with scFv antibody extracellular domains and intracellular sequences comprising the signaling region of CD28 in series with the signaling region of the ζ chain from the TCR complex. Extracellular-binding specificity for the constructs was provided by the engineered human scFv derived from P67 [16], a mAb with specificity for human CD33, which is in clinical trials as a drug conjugate for treatment of acute myeloid leukemia. Spacers were used to distance the extracellular-binding domain from the membrane [29] and comprise the hinge region from human IgG1 with either the CH2 and CH3 domains from IgG1 [23, 24] or part of the extracellular region of CD28. Such constructs contained the primary signaling and costimulatory regions, respectively, either proximal or distal to the membrane; the transmembrane sequence was taken from the region proximal to the membrane in either case. Constructs with the CD28-signaling domain proximal to the ζ chain and distal to the membrane, were found to be expressed more efficiently in Jurkat cells than in constructs with the opposite orientation and were capable of mediating up to 20 times more IL-2 production on stimulation with solid-phase antigen when compared with transfectants expressing chimeric receptors with ζ-chain intracellular signaling only. In a similar fashion, Maher et al. [59] combined activation and costimulatory functions within a single receptor recognizing the prostate-specific membrane antigen (PSMA) by constructing scFv-based receptors that comprise both the TCR ζ chain and CD28 sequences. CD4+ and CD8+ T cells transduced with such constructs displayed increased production of IL-2, high proliferation rates, and killing of PSMA-expressing tumor cells. In another study, Hombach et al. [30] by integrating both CD28- and CD3ζ-signaling domains into one combined immunoreceptor molecule targeting CEA on tumor cells, demonstrated that T cells grafted with this combined CD28-CD3 secreted high amounts of IL-2 upon antigen binding without B7-CD28 costimulation. These data suggested that both MHC-independent cellular activation and CD28 costimulation for complete T-cell activation can be delivered by one recombinant molecule although receptor-mediated target cell lysis did not require CD28 costimulation to allow killing of B7-negative tumor cells [1, 30].
CAR expression on NK cells as an alternative method for cancer immunotherapy
Natural killer (NK) cells play an essential role in the cellular-based immune defense of virus-infected and neoplastic cells. NK cells do not rearrange their immune receptor genes, and the cytotoxicity toward tumor and virally infected cells is not MHC-restricted [60]. Activated NK cells, typically expanded from the peripheral blood and activated by a variety of cytokines also including IL-2, IL-15, IL-12, and IL-18 or mixtures thereof [61] are sometimes also referred to as LAK cells. For years activated NK cells have been explored with respect to their efficacy in anticancer therapy [47, 62], but, except for a few cases [63], no clear clinical benefit has been shown. However, as understanding of the interactions of NK cells and tumor cells advances, the use of activated NK cells might be reconsidered with more sophisticated approaches that deal with mechanisms which prevent tumor cells to escape immune surveillance.
The highly cytotoxic NK cell line NK-92 seems to be an attractive alternative for use in adoptive immunotherapy because it continuously grows in media supplemented with IL-2, and therefore can be expanded in large numbers [64]. It was also shown to exhibit substantial antitumor activity against a wide range of malignancies in vitro [64] and in humanized mouse models in vivo [65].
Similar to activated NK cells, NK-92 cells express typical NK cell surface receptors [66], but in a direct comparison, they display a much higher cytolytic activity against a broad spectrum of tumor targets [66]. NK-92 cells are also characterized by an almost complete lack of killer cell immunoglobulin-like receptors (KIRs), yet they conserve perforin and granzyme B–mediated cytolytic activity [64, 66]. Although a large variety of malignant cells are effectively killed by NK-92 cells, no toxicity against nonmalignant allogeneic cells has been observed [65].
To further enhance the antitumoral activity of NK-92 cells and expand the range of tumor entities suitable for NK-92–based therapies, Uherek et al. [67] generated genetically modified NK-92 cells expressing a CAR specific for the HER-2/neu antigen. The CAR consisted of the HER-2/neu–specific scFv (FRP5) antibody fragment [49], a flexible hinge region derived from the CD8, and the ζ-signaling chain of the TCR. Transduced NK-92-scFv (FRP5)-ζ cells specifically and efficiently lysed HER-2/neu–expressing tumor cells, which were completely resistant to the cytolytic activity of parental NK-92 cells [49]. These results demonstrated that NK-cell resistance could be overcome by expression of this particular CAR alone. In addition, specific antitumoral effects were also observed in vivo when the NK-92-scFv (FRP5)-ζ cells were administered into nude mice, which were inoculated with HER-2/neu–transformed fibroblasts [67]. Meanwhile, variants of NK-92 cells engineered to express CARs targeting B-cell lymphoma or HIV epitopes are currently under investigation. Thus, further development of retargeted NK-92 variants might provide a potential new modality in cellular cancer immunotherapy.
CTLs grafted with CARs for cancer immunotherapy: pros and cons
Immunogenicity of tumors is dependent on the expression of tumor antigens that can be recognized by the host immune system as foreign. Ideally, for the generation of a specific antitumor response, these novel antigens should not be found on normal cells. They also should be presented in an appropriate manner to the immune system of the host. In cases in which these requirements have been fulfilled, adoptive immunotherapy experiments using tumor-specific T lymphocytes have shown that successful treatment of tumor-bearing animals is possible. However, potential drawbacks for adoptive tumor therapy based on T cells are also well described: (1) the ineffective presentation of TAAs by down-regulation of MHC molecules on tumor cells [68], and (2) the presentation of antigen in the absence of costimulatory molecules leading to T-cell anergy [41]. Therefore, the major advantage of using CTLs grafted with CARs is that these provide us with the opportunity to direct T cells against any antigen for which a mAb exists and thus, to generalize the use of adoptive immunotherapy in a variety of malignant diseases. Since the requirements of MHC restriction in the interaction of effector cells with target cells are bypassed, the tumor cell binding of CTLs grafted with CARs is not affected by down-regulation of HLA class I antigens and by defects in the antigen-processing machinery—abnormalities frequently associated with malignant transformation of cells [41]. On the other hand, the expression of CARs also containing CD28 genes in CTLs demonstrated that both MHC-independent cellular activation and CD28 costimulation for complete T-cell activation can be delivered by one recombinant receptor molecule, resulting in lysis of B7-negative tumor cells [1, 30]. Another advantage in using CTLs transduced with CARs is that these, upon activation with the specific antigen, produce cytokines which recruit and activate other elements of the immune system and so in this way induce a more massive immune response to tumor cells [69]. In addition, CARs are constitutively expressed by the transduced CTLs, and grafted CTLs have been shown in animal tumor models to home to tumor sites [70]. More important, CAR-transduced CTLs exhibit high levels of cytotoxicity despite the low surface expression of the transduced chimeric gene [23]. The high lytic activity may be explained by the high affinity of the chimeric receptor relative to that of the TCR for the antigen on the tumor target cells [23, 70]. Moreover, this low expression of scFv/γ receptors may prove advantageous from a clinical point of view, as it might lower the human antimouse antibody responses in patients after transfusion of the transduced CTLs. It is also interesting to note that CTLs transduced with CARs have the potential to recycle their lytic potential by continuously synthesizing the transduced chimeric receptor [23], thereby demonstrating their capacity to enter multiple lytic cycles with their specific tumor targets. Over the past decade, CARs directed against a variety of tumor antigens have been developed (Table 1). Most importantly, CAR-mediated cytolysis has not only been achieved in T-cell hybridomas, but also in primary mouse and human T cells, as well as patient-derived primary T cells. Furthermore, the in vivo efficacy of mouse CAR–modified effectors cells has been demonstrated for the tumor antigens HER-2/neu [27, 28, 44], the colorectal CEA [1, 45], the adenocarcinoma antigen TAG-72 [71], and the ovarian carcinoma antigens FBP [72, 73]. In addition, human peripheral blood lymphocytes that are targeted to the CD19 antigen were shown to eliminate established Burkitt’s lymphomas after adoptive transfer in SCID mice [74], showing for the first time in vivo efficacy of genetically directed human primary T cells.
There are several limitations to the use of CAR-transduced T cells. The first is that the antigen recognized must be expressed on the cell surface. Tumor cells can down-regulate the expression of antigens that are recognized by TCRs [41]. The ability of tumor cells to modulate their surface antigens provides an obstacle to the use of tumor antigen-specific T cells in cancer immunotherapy. An additional limitation is indicated by the strength of the activation signal provided by the different CARs. Haynes et al. [69] demonstrated superior signaling efficacy of scFv containing TCR-ζ vs FcɛRI-γ, which was due to the number of ITAMs contained within their cytoplasmic domains. Besides the nature of the ITAM-containing domain, various other variables may determine signaling capacity, also including transmembrane association with other molecules regulating signal transduction, affinity for antigen, and a physical link with other surface molecules [16, 29, 69, 70]. Finally, the question of how efficiently CTLs can be transduced to express CARs must also be taken into consideration. All these parameters must, therefore, be investigated for the exact characterization of every newly developed CAR. Differences in susceptibility to stimulation between preactivated and resting T cells also provide an additional limitation to the approach utilizing CTLs grafted with CARs [18]. Naïve T cells from mice transgenic with a CD3 ζ-chain receptor activated via their endogenous TCR-CD3 complexes were able to kill with high specificity and efficacy via their scFv/ζ receptor [18]. In contrast, resting T cells from the same mice could not be triggered via the chimeric scFv/ζ receptor to display any effector functions even in the presence of costimulus via CD28 or CD4. This may be important for the progeny of bone marrow cells transduced to express chimeric receptors, which will have to be preactivated to become susceptible through the signaling domain of the CAR [75].
Several clinical trials using lymphocytes engineered to express CARs have been implemented; however, so far, no positive clinical responses have been noted [23, 76]. One major obstacle to this form of therapy is the presence of high serum levels of soluble monovalent antigen, which upon binding to grafted cells would render them anergic. Thus such kinds of therapy would be restricted to patients with low levels of soluble tumor antigen. The antigenic diversity in tumor cell populations may also hamper positive clinical results. The use of lymphocytes grafted with CARs recognizing more than one antigen may circumvent this problem. Preclinical studies have demonstrated the capacity of T cells expressing bispecific CARs to lyse tumor cells expressing both CEA and TAG-72 [23] or HIV-infected cells expressing wild-type and mutant envelope proteins [77]. Another limitation of CARs is their potential immunogenicity. Since the scFv is most often derived from a mAb of murine origin, this might trigger a host immune response and therefore accelerate T-cell clearance. Humanizing the mouse portions of CARs or by using previously humanized scFvs [26, 78] may offer a solution to this problem. Another aspect that should be taken into consideration when utilizing lymphocytes grafted with CARs in clinical trials is that T cells of cancer patients may possess abnormalities in their TCR-mediated signaling [79, 80]. Thus the question to be addressed is whether potential downstream defects in the signaling cascade will impair signal transduction initiated by the chimeric receptor(s).
Conclusions
Despite these outstanding questions, the genetic engineering of primary T cells creates new prospects for the investigation of T-cell biology, tumor immunity, and cancer immunotherapy. The transduction of T cells with genes that encode antigen receptors enables the recognition of antigens that are either poorly immunogenic or ignored by the immune system. An important feature of T cell–expressing CARs is that they, like antibodies per se, recognize antigen in an MHC-unrestricted manner. Hence, in contrast to conventional T cells, which recognize their ligand via their endogenous MHC-restricted TCR, the CAR-dictated specificity and antitumor activity is not adversely affected by tumor cells that down-regulate their MHC complex or for other reasons do not express MHC-restricted antigens. Additional advantages in redirected T-cell therapy involving expression of CARs over other immunotherapies are: (1) the abundance of naïve T cells available for gene transfer, and (2) the variety of TAAs expressed on a broad spectrum of tumors. Moreover, increasing T-cell expansion, offsetting anergizing or proapoptotic signals, expanding the range of tumoricidal functions, and protecting T cells against the suppressive effects of the tumor microenvironment are additional important aspects for enhancing the antitumoral activities of T cells expressing CARs. Clinical trials should help us to determine the true effectiveness of those approaches and to establish the optimal protocols for cancer immunotherapy. Finally, further development of retargeted NK-92 variants might result in the generation of potent cell-based therapeutics for the treatment of various malignancies.
Abbreviations
- BsAb
Bispecific antibody
- CAR
Chimeric antigen receptor
- CTL
Cytotoxic T lymphocyte
- MHC
Major histocompatibility complex
- mAb
Monoclonal antibody
- scFv
Single-chain variable domains of a mAb
- TAA
Tumor-associated antigen
- TCR
T-cell receptor
Footnotes
This article forms part of the Symposium in Writing “Tumor escape from the immune response” published in Vol. 53.
References
- 1.Haynes Blood. 2002;100:3155. doi: 10.1182/blood-2002-04-1041. [DOI] [PubMed] [Google Scholar]
- 2.Browning Tissue Antigens. 1996;47:364. doi: 10.1111/j.1399-0039.1996.tb02571.x. [DOI] [PubMed] [Google Scholar]
- 3.Garrido Immunol Today. 1997;18:89. doi: 10.1016/s0167-5699(96)10075-x. [DOI] [PubMed] [Google Scholar]
- 4.Hui Nature. 1984;311:750. doi: 10.1038/311750a0. [DOI] [PubMed] [Google Scholar]
- 5.Hui Bioessays. 1989;11:22. [Google Scholar]
- 6.Rosenberg J Natl Cancer Inst. 1994;86:1159. doi: 10.1093/jnci/86.15.1159. [DOI] [PubMed] [Google Scholar]
- 7.Stofer G, Goey SH, Batchelor D, Eggermont AD, Lamers C, Gratama JW, Bolhuis RCH (1992) EORTC genitourinary group monograph no. 11. In: Schroeder FH (ed) Recent progress in bladder and kidney cancer: treatment of disseminated renal cell cancer with combinations of interleukin-2, lymphokine-activated killer cells, and a-interferon. Wiley-Liss, New York, pp 225 [PubMed]
- 8.Rosenberg J Clin Oncol. 1992;10:180. doi: 10.1200/JCO.1992.10.2.180. [DOI] [PubMed] [Google Scholar]
- 9.Baxevanis Cancer. 1994;74:1275. doi: 10.1002/1097-0142(19940815)74:4<1275::aid-cncr2820740416>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 10.Baxevanis Crit Rev Oncol Hematol. 1994;16:157. doi: 10.1016/1040-8428(94)90069-8. [DOI] [PubMed] [Google Scholar]
- 11.Jain J Natl Cancer Inst. 1989;81:570. doi: 10.1093/jnci/81.8.570. [DOI] [PubMed] [Google Scholar]
- 12.Blank-Voorthuis J Immunol. 1993;151:2904. [PubMed] [Google Scholar]
- 13.Lanzavecchia Eur J Immunol. 1987;17:105. doi: 10.1002/eji.1830170118. [DOI] [PubMed] [Google Scholar]
- 14.Brocker Eur J Immunol. 1993;23:1435. doi: 10.1002/eji.1830230705. [DOI] [PubMed] [Google Scholar]
- 15.Eshhar Proc Natl Acad Sci U S A. 1993;90:720. [Google Scholar]
- 16.Nolan Clin Cancer Res. 1999;5:3928. [PubMed] [Google Scholar]
- 17.Kuwana Biochem Biophys Res Commun. 1989;149:960. [Google Scholar]
- 18.Brocker Adv Immunol. 1998;68:257. doi: 10.1016/s0065-2776(08)60561-1. [DOI] [PubMed] [Google Scholar]
- 19.Eshhar Cancer Immunol Immunother. 1997;45:131. doi: 10.1007/s002620050415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Irving Cell. 1991;64:891. doi: 10.1016/0092-8674(91)90314-O. [DOI] [PubMed] [Google Scholar]
- 21.Letourneur Proc Natl Acad Sci U S A. 1991;88:8905. doi: 10.1073/pnas.88.20.8905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Romeo Cell. 1991;64:1037. doi: 10.1016/0092-8674(91)90327-U. [DOI] [PubMed] [Google Scholar]
- 23.Alvarez-Vallina Curr Gene Ther. 2001;1:385. doi: 10.2174/1566523013348418. [DOI] [PubMed] [Google Scholar]
- 24.Alvarez-Vallina Eur J Immunol. 1996;26:2304. doi: 10.1002/eji.1830261006. [DOI] [PubMed] [Google Scholar]
- 25.Roberts J Immunol. 1998;1:375. [Google Scholar]
- 26.Hoogenboom Immunol Rev. 1992;130:41. doi: 10.1111/j.1600-065x.1992.tb01520.x. [DOI] [PubMed] [Google Scholar]
- 27.Gritzapis Br J Cancer. 2003;88:1292. doi: 10.1038/sj.bjc.6600888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mamalaki Cancer Immunol Immunother. 2003;52:513. doi: 10.1007/s00262-002-0371-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moritz Gene Ther. 1995;2:539. [PubMed] [Google Scholar]
- 30.Hombach J Immunol. 2001;167:6123. doi: 10.4049/jimmunol.167.11.6123. [DOI] [PubMed] [Google Scholar]
- 31.Daeron Annu Rev Immunol. 1997;15:203. doi: 10.1146/annurev.immunol.15.1.203. [DOI] [PubMed] [Google Scholar]
- 32.Klausner Cell. 1991;64:875. doi: 10.1016/0092-8674(91)90310-U. [DOI] [PubMed] [Google Scholar]
- 33.Quian Curr Opin Cell Biol. 1997;9:205. doi: 10.1016/s0955-0674(97)80064-6. [DOI] [PubMed] [Google Scholar]
- 34.Wange Immunity. 1996;5:197. doi: 10.1016/S1074-7613(00)80315-5. [DOI] [PubMed] [Google Scholar]
- 35.Weiss Cell. 1994;76:263. doi: 10.1016/0092-8674(94)90334-4. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Cell. 1998;92:83. doi: 10.1016/S0092-8674(00)80901-0. [DOI] [PubMed] [Google Scholar]
- 37.Weijtens J Immunol. 1996;157:836. [PubMed] [Google Scholar]
- 38.Zoller J Immunol. 1997;158:1650. [PubMed] [Google Scholar]
- 39.Indik Blood. 1995;86:4389. [PubMed] [Google Scholar]
- 40.Wegener Cell. 1992;68:83. doi: 10.1016/0092-8674(92)90208-T. [DOI] [PubMed] [Google Scholar]
- 41.Pawelec Crit Rev Oncog. 1997;8:111. doi: 10.1615/critrevoncog.v8.i2-3.10. [DOI] [PubMed] [Google Scholar]
- 42.Yun Neoplasia. 2000;2:449. doi: 10.1038/sj.neo.7900108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fitzer-Atlas J Immunol. 1998;160:145. [PubMed] [Google Scholar]
- 44.Altenschmidt J Immunol. 1997;159:5509. [PubMed] [Google Scholar]
- 45.Darcy J Immunol. 2000;164:3705. [Google Scholar]
- 46.Darcy Eur J Immunol. 1998;28:1663. doi: 10.1002/(SICI)1521-4141(199805)28:05<1663::AID-IMMU1663>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 47.Nagayama Bone Marrow Transplant. 1999;23:183. doi: 10.1038/sj.bmt.1701550. [DOI] [PubMed] [Google Scholar]
- 48.Moritz Proc Natl Acad Sci U S A. 1994;91:4318. [Google Scholar]
- 49.Wels Cancer Res. 1992;52:6310. [PubMed] [Google Scholar]
- 50.Biever Annu Rev Immunol. 1989;7:759. [Google Scholar]
- 51.Janeway Annu Rev Immunol. 1992;10:645. doi: 10.1146/annurev.iy.10.040192.003241. [DOI] [PubMed] [Google Scholar]
- 52.Alberoia-Ila J Immunol. 1992;148:1287. [PubMed] [Google Scholar]
- 53.Lenschow Annu Rev Immunol. 1996;14:233. doi: 10.1146/annurev.immunol.14.1.233. [DOI] [PubMed] [Google Scholar]
- 54.Vandenberghe J Exp Med. 1992;175:951. doi: 10.1084/jem.175.4.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Harding J Exp Med. 1993;177:1791. doi: 10.1084/jem.177.6.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rudd Immunity. 1996;4:527. doi: 10.1016/S1074-7613(00)80479-3. [DOI] [PubMed] [Google Scholar]
- 57.Stein Mol Cell Biol. 1994;14:3392. doi: 10.1128/mcb.14.5.3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Finney J Immunol. 1998;161:2791. [PubMed] [Google Scholar]
- 59.Maher J, Brentjens RJ, Gunset G, Riviere I, Sadelain M (2002) Human T-lymphocyte cytotoxicity and proliferation directed by a single chimeric TCRJ/CD28 receptor. Nat Biotechnol 70 [DOI] [PubMed]
- 60.Bennett Adv Immunol. 1987;41:333. doi: 10.1016/s0065-2776(08)60034-6. [DOI] [PubMed] [Google Scholar]
- 61.Smyth Nat Rev Immunol. 2002;2:850. doi: 10.1038/nrc928. [DOI] [Google Scholar]
- 62.Rosenberg SA, Lotze MT, Yang JC, Topalian SL, Chang AE, Schwartzentruber DJ, Aebersold P, Leitman S, Linehan WM, Seip LA, et al. Prospective randomized trial of high-dose interleukin-2 alone or in combination with lymphokine-activated killer cells for the treatment of patients with advanced cancer. J Natl Cancer Inst. 1993;85:622. doi: 10.1093/jnci/85.8.622. [DOI] [PubMed] [Google Scholar]
- 63.Whiteside Curr Top Microbiol Immunol. 1998;230:221. doi: 10.1007/978-3-642-46859-9_13. [DOI] [PubMed] [Google Scholar]
- 64.Tonn J Hematother Stem Cell Res. 2001;10:535. doi: 10.1089/15258160152509145. [DOI] [PubMed] [Google Scholar]
- 65.Klingemann Biol Blood Marrow Transplant. 1996;2:68. [PubMed] [Google Scholar]
- 66.Gong Leukemia. 1994;8:652. [PubMed] [Google Scholar]
- 67.Uherek Blood. 2002;100:1265. [PubMed] [Google Scholar]
- 68.Soliger Immunol Today. 1997;18:292. doi: 10.1016/s0167-5699(97)01052-9. [DOI] [PubMed] [Google Scholar]
- 69.Haynes J Immunol. 2001;166:182. [Google Scholar]
- 70.Sadelain Nat Rev Cancer. 2003;3:35. doi: 10.1038/nrc971. [DOI] [PubMed] [Google Scholar]
- 71.McGuinness Hum Gene Ther. 1999;10:165. doi: 10.1089/10430349950018968. [DOI] [PubMed] [Google Scholar]
- 72.Hwu Cancer Res. 1995;55:3369. [PubMed] [Google Scholar]
- 73.Wang Nat Med. 1998;4:168. [Google Scholar]
- 74.Brentjens Blood. 2002;100:577. [Google Scholar]
- 75.Abken Immunol Today. 1998;19:2. doi: 10.1016/S0167-5699(97)01191-2. [DOI] [PubMed] [Google Scholar]
- 76.Ren-Heidenreich Curr Gene. 2001;Ther:253. doi: 10.2174/1566523013348607. [DOI] [PubMed] [Google Scholar]
- 77.Patel Gene Ther. 1999;6:412. doi: 10.1038/sj.gt.3300831. [DOI] [PubMed] [Google Scholar]
- 78.Hombach Int J Cancer. 2000;88:120. doi: 10.1002/1097-0215(20001001)88:1<115::AID-IJC18>3.3.CO;2-5. [DOI] [Google Scholar]
- 79.Levey Immunol Today. 1996;17:365. doi: 10.1016/0167-5699(96)10013-X. [DOI] [PubMed] [Google Scholar]
- 80.Zier Immunol Today. 1996;17:39. doi: 10.1016/0167-5699(96)80567-6. [DOI] [PubMed] [Google Scholar]
- 81.Gong Neoplasia. 1999;1:127. doi: 10.1038/sj.neo.7900018. [DOI] [Google Scholar]
- 82.Rossig Blood. 2002;99:2016. doi: 10.1182/blood.V99.6.2009. [DOI] [Google Scholar]
- 83.Daly Cancer Gene Ther. 2000;7:291. doi: 10.1038/sj.cgt.7700121. [DOI] [PubMed] [Google Scholar]
- 84.Weijtens Gene Ther. 2000;7:35. doi: 10.1038/sj.gt.3301051. [DOI] [PubMed] [Google Scholar]
- 85.Krause J Exp Med. 1998;188:626. doi: 10.1084/jem.188.4.619. [DOI] [PMC free article] [PubMed] [Google Scholar]