Abstract
Introduction
Domino osteoporotic vertebral fracture (OVF) is as a subsequent fracture that develops within 3 months before the initial OVF heals. There is limited evidence regarding the efficacy of osteoanabolic agents on its treatment. This study evaluated the effects of bisphosphonates and anabolic agents teriparatide and romosozumab on subsequent domino OVF.
Methods
This was post hoc analysis of a prospective, multicenter, observational study conducted across 8 hospitals, enrolling 144 patients with conservatively treated OVF, grouped into patients receiving bisphosphonate (BP, n = 55), teriparatide (TPTD, n = 62), and romosozumab (Romo, n = 27). The primary outcome was the incidence of subsequent OVF at 3 and 12 months, whereas the secondary outcomes included the incidence of pseudoarthrosis and progression of vertebral collapse (VC). Pseudoarthrosis was classified as stable or unstable based on vertebral instability.
Results
The use of osteoanabolic agents did not reduce the incidence of subsequent OVF at 3 and 12 months. There were no significant differences in the background data or type of conservative treatment among the three groups. However, the TPTD and Romo groups had significantly lower rates of unstable pseudarthrosis (p = 0.03). Additionally, there were no significant differences in VC progression between groups, but it tended to be higher in the BP group than the TPTD and Romo group (p = 0.07).
Conclusion
Osteoanabolic agents were beneficial in reducing unstable pseudoarthrosis, but were not more effective than bisphosphonates in the development of subsequent domino OVF. A more comprehensive approach to the treatment of osteoporosis is needed to prevent domino OVFs.
Keywords: Domino osteoporotic vertebral fracture, Osteoanabolic agent, Teriparatide, Romosozumab
Highlights
-
•
Teriparatide and romosozumab were not more effective than bisphosphonates in the development of domino OVF.
-
•
Osteoanabolic agents were more beneficial in reducing unstable pseudoarthrosis than were bisphosphonates.
-
•
Osteoanabolic agents may have contributed to bony bridge formation to the adjacent vertebra.
1. Introduction
The incidence of osteoporotic vertebral fractures (OVFs) is the highest among fragility fractures (Balasubramanian et al., 2019). Meanwhile, the incidence of subsequent vertebral fractures (VF) after an initial OVF increases with age, and the risk of subsequent fractures is highest immediately after the initial fracture (Banefelt et al., 2019; van Geel et al., 2010). Recent studies have emphasized the concept of imminent fractures, which are fractures that occur within 2 years after an initial fracture (Balasubramanian et al., 2019; Roux and Briot, 2017; van Geel et al., 2010; Wong et al., 2022). Clinical VF poses the highest risk of subsequent fracture, with a 14 % risk within one year for older women (Balasubramanian et al., 2019). Previously, we have proposed domino OVF as a secondary fracture that develops within 3 months before the initial OVF heals (Kusukawa et al., 2023; Yamaura et al., 2023). Subsequent domino OVF had an incidence of 13.6 % and negatively impacted quality of life (QOL) (Kusukawa et al., 2023). Therefore, preventing refractures after an initial OVF is essential for QOL. The prevalence of OVFs is also a major risk factor associated with an increased risk of subsequent OVFs (Hagino et al., 2013; Lindsay et al., 2001). Immediate care of osteoporosis is crucial for the initial treatment of OVF, but only a few patients receive treatment for osteoporosis at the time of injury (Kusukawa et al., 2023). Currently, osteoanabolic agents, teriparatide (TPTD) or romosozmab (Romo), are being used more frequently as first-line treatments for patients with a very high risk of fracture. (Kostenuik et al., 2023), but there is no evidence on their effects on domino OVF. This study aimed to evaluate the effects of osteoanabolic agents, including TPTD and Romo, on subsequent domino OVF, bony union, and progression of vertebral collapse (VC) after initial OVF.
2. Material and methods
2.1. Study design and patient selection
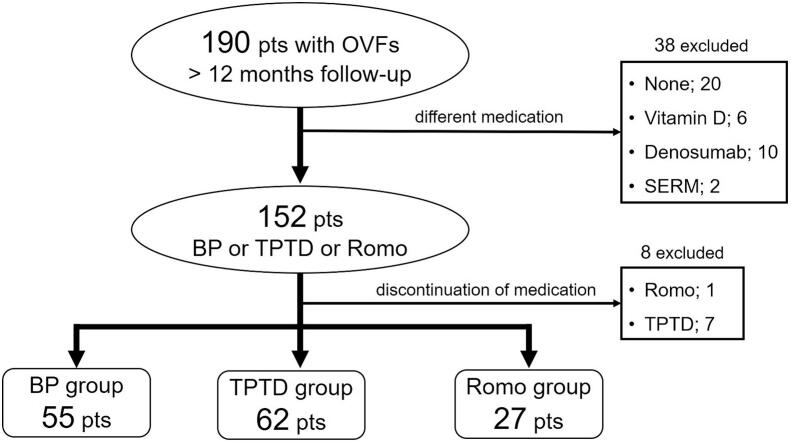
This is a post hoc analysis of a multicenter, prospective, observational study (Kusukawa et al., 2023), which included 277 patients diagnosed with OVF confirmed via magnetic resonance imaging (MRI), who underwent conservative treatment between May 2020 and May 2022. The inclusion criteria for this analysis were as follows: acute OVF occurring within 3 weeks, age > 60 years, use of osteoanabolic agents (TPTD and Romo) or bisphosphonates (BP), and a minimum follow-up of 12 months. The study included multiple acute OVFs at baseline. The exclusion criteria for the original study and therefore also for this analysis were as follows: prevalent OVFs (>3), pathologic fractures, spinal infections, surgery required for progression of VC, and discontinuation of osteoporosis treatment due to side effects. This study was approved by the Institutional Ethical Committee (IRB No.3562), and all patients provided informed consent. Initially, 190 patients with at least 12 months of follow-up were included. We did not perform a power analysis because this study was a post-hoc analysis of the subsequent domino OVF study. We excluded 38 patients who received other treatments for osteoporosis, including activated vitamin D3 (n = 6), denosumab (n = 10), and selective estrogen receptor modulators (n = 2), no treatment (n = 20), as well as 8 patients who discontinued osteoporosis treatment (TPTD group, n = 7; Romo group, n = 1). Finally, the study involved 144 patients who received treatment with BP (n = 55), TPTD (n = 62), and Romo (n = 27) (Fig. 1). Twenty-two patients (81.5 %) in the Romo group and forty patients (61.5 %) in the BP group received active vitamin D3. The TPTD group included patients who received daily 20-μg TPTD (Forteo®; Eli Lilly, Japan) (n = 20), once-weekly 56.5-μg TPTD (n = 17), and twice-weekly 56.5-μg TPTD administration (Teribone®; Asahi Kasei Pharma, Japan) (n = 25). The attending physicians determined the selection of medication for osteoporosis. Osteoanabolic agents were recommended for cases of more severe osteoporosis, with multiple acute OVFs at baseline, and prevalent multiple OVF at a high risk of domino OVF. TPTD was not given for elderly patients who found it difficult to self-inject. Romo was not given to patients with a history of cardiovascular ischemic events. Serum levels of procollagen type 1 amino-terminal propeptide (P1NP) and tartrate-resistant acid phosphatase 5b (TRACP5b) were measured at baseline.
Fig. 1.
Flowchart of conservative treatment for osteoporotic vertebral fracture.
2.2. Radiographic and clinical assessment
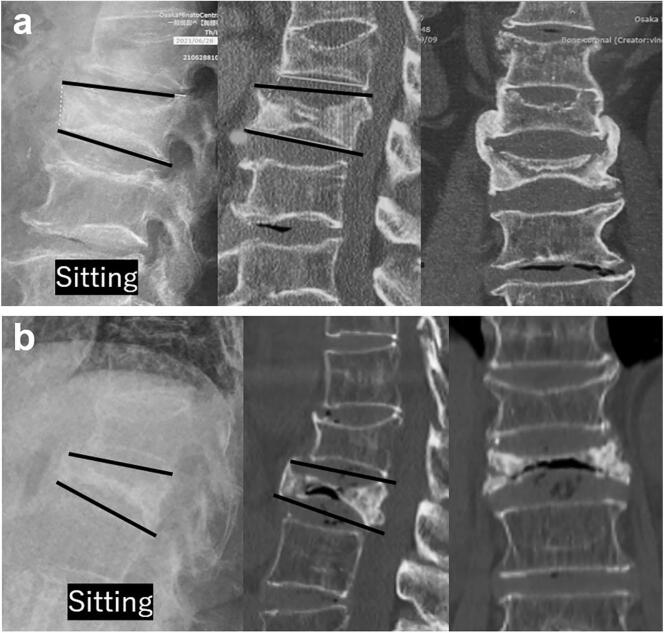
Clinical, demographic, and radiographic data were obtained from medical records. To detect subsequent OVF, all patients underwent MRI scans at baseline, 3 months, and 12 months. Computed tomography (CT) was performed to assess bone union at 12 months. Pseudoarthrosis was defined as the presence of an intervertebral vacuum cleft on CT or a fluid sign on MRI, and cases were classified as either stable or unstable. The criteria for unstable pseudoarthrosis include 1) vertebral instability >3°, measured in both sitting and supine positions, and 2) the lack of bridge formation to the adjacent vertebra. This classification system is based on objective criteria and avoids subjective evaluations (Fig. 2a, b). The severity of VC was classified based on the Genant semiquantitative (SQ) grading system. (Genant et al., 1993), and VC progression was defined as progression from SQ grade 0 or 1 at baseline to SQ grade 3 at 12 months. Patient data was blinded, and subjective evaluation of CT imaging and MRI, including vertebral fracture, SQ grade, and pseudarthrosis, was diagnosed by six orthopaedic spine surgeons (K.M, M.T., T.K., T.Y., K.N. and M.H. with 22, 9, 9, 8, 7, and 7 years of experience, respectively). A diagnosis was determined if four out of six were in agreement. However, if three or fewer agreed, a decision was made by discussion among the six surgeons. Bone mineral density (BMD) was measured using dual-energy X-ray absorptiometry for the lumbar spine (L2–4) and total hip at baseline and 12 months. Clinical outcomes were evaluated using the visual analogue scale (VAS) and Oswestry Disability Index (ODI) at baseline, 3 months, and 12 months.
Fig. 2.
a. Stable pseudoarthorosis case (a). Lateral standing position of X-ray and prone position of CT showed changes in kyphotic angle (KA) <3°. Bridge formation was evidenced in the coronal plane of the CT scan, as depicted in the rightmost image of panel a.
b. Unstable pseudoarthorosis case. (b) Change in kyphotic angle (KA) > 3° and presence of intervertebral vacuum cleft.
2.3. Primary and secondary outcome measures
The primary outcome of the study was the incidence of subsequent OVF at 3 and 12 months. The secondary outcomes included the incidence of pseudoarthrosis, VC progression (SQ grade 3), change in BMD at 12 months, and VAS and ODI scores. The incidence of subsequent OVF was calculated per patient. The incidence of VC progression and pseudoarthrosis was calculated per vertebra.
2.4. Statistical analysis
The study analyzed the differences among the three groups using one-way analysis of variance with Tukey's post hoc test. Differences between baseline and 3 or 12 months were analyzed using the Wilcoxon sum rank test. For categorical variables, the chi-square test or Fisher's exact test was used. All statistical analyses were performed using JMP Pro software (Version 15; SAS Institute Inc.), with P < 0.05 considered statistically significant.
3. Results
3.1. Baseline characteristics, bone health assessment, and conservative treatment
There were no significant differences in baseline characteristics, including age, sex, body mass index, lumbar and total hip BMD, TRACP5b, and P1NP (Table 1). The number of prevalent OVFs and multiple acute OVFs were not significantly different among the three groups at baseline (Table 2). At baseline, the Romo group had significantly more cases of SQ grade 3 VC versus the BP and TPTD groups. The three groups were not significantly different in terms of previous antiresorptive therapy and equivalent types of conservative treatment, including hospitalization and brace type. Previous osteoporosis therapy is defined as a history of osteoporosis treatment for more than one year. One patient received denosumab as previous osteoporosis therapy, while four patients received selective estrogen receptor modulators (Table 2).
Table 1.
Baseline patient characteristics.
| Characteristics | BP group (n = 55) |
TPTD group (n = 62) |
Romo group (n = 27) |
p-value |
|---|---|---|---|---|
| Age (yrs) | 78.6 ± 7.7 | 79.8 ± 7.3 | 79.5 ± 7.5 | 0.69 |
| Sex (female) [n, (%)] | 46 (84) | 52 (84) | 17 (63) | 0.07 |
| Height (cm) | 152.8 ± 8.7 | 152.2 ± 8.0 | 154.1 ± 8.0 | 0.61 |
| Body weight (kg) | 51.5 ± 8.9 | 52.7 ± 8.7 | 50.7 ± 9.5 | 0.58 |
| Body mass index (kg/m2) | 22.1 ± 3.4 | 22.8 ± 3.2 | 21.3 ± 3.3 | 0.21 |
| Lumbar BMD (L2–4) (g/cm2) | 0.81 ± 0.13 | 0.80 ± 0.15 | 0.84 ± 0.17 | 0.58 |
| Total hip BMD (g/cm2) | 0.64 ± 0.02 | 0.60 ± 0.02 | 0.63 ± 0.13 | 0.16 |
| T-score < −2.5 | 28 (51) | 39 (63) | 15 (56) | 0.41 |
| TRACP5b (mU/dL) | 457.5 ± 224.9 | 517 ± 179 | 473.7 ± 214.2 | 0.13 |
| P1NP (μg/L) | 70.3 ± 48.1 | 87.2 ± 100.8 | 75.8 ± 54.4 | 0.52 |
Values are presented as mean ± standard deviations or %. BP; bisphosphonates, TPTD; teriparatide, Romo; romosozumab, BMD; bone mineral density, OVF; osteoporotic vertebral fracture, TRACP; tartrate-resistant acid phosphatase, P1NP; type 1 amino-terminal propeptide.
Table 2.
Baseline severity of osteoporosis and type of conservative treatment.
| Variable | BP group (n = 55) |
TPTD group (n = 62) |
Romo group (n = 27) |
p-value |
|---|---|---|---|---|
| Prevalent OVFs [n, (%)] | 0.18 | |||
| 0 | 33 (60) | 34 (55) | 13 (48) | |
| 1 | 16 (29) | 21 (34) | 7 (26) | |
| 2 | 6 (11) | 4 (6) | 6 (22) | |
| 3 | 0 | 3 (5) | 1 (4) | |
| Multiple acute OVFs [n, (%)] | 7 (13) | 13 (21) | 6 (22) | 0.41 |
| SQ grade 3 [n, (%)] | 3 (5) | 9 (15) | 8 (30) | 0.01⁎ |
| Previous osteoporosis therapy | 0.97 | |||
| BP [n, (%)] | 7 (13) | 8 (13) | 3 (11) | |
| Risedronate (n) | 2 | 1 | 0 | |
| Minodronate (n) | 1 | 2 | 2 | |
| Alendronate (n) | 4 | 5 | 1 | |
| Denosumab (n) | 1 | 0 | 0 | |
| SERM (n) | 3 | 0 | 1 | |
| Hospitalization (yes) [n, (%)] | 23 (42) | 36 (58) | 12 (44) | 0.18 |
| Type of brace [n, (%)] | 0.06 | |||
| Hard | 27 (49) | 34 (55) | 7 (26) | |
| Soft | 26 (47) | 27 (44) | 17 (63) | |
| Other | 2 (4) | 1 (2) | 3 (11) |
Multiple acute OVFs is >1 OVF within the 3 weeks of study enrollment; prevalent OVFs are OVFs before the 3 weeks of study enrollment. Values are presented as number or %. BP; bisphosphonates, TPTD; teriparatide, Romo; romosozumab, BMD; bone mineral density, OVF; osteoporotic vertebral fracture, SQ; semiquantitative, SERM; selective estrogen receptor modulator ⁎; p < 0.05.
3.2. Primary outcomes
The primary and secondary outcomes are shown in Table 3. There was no significant difference across all groups in the incidence of subsequent OVF at 3 months (BP: 9.1 %, TPTD: 8.1 %, Romo: 14.8 %, p = 0.60) and at 12 months (BP: 12.7 %, TPTD: 11.3 %, Romo: 14.8 %, p = 0.89).
Table 3.
Primary and secondary outcomes in the three groups.
| Variable | BP group (n = 55) |
TPTD group (n = 62) |
Romo group (n = 27) |
p-value |
|---|---|---|---|---|
| Subsequent OVF | ||||
| 3 months [n, (%)] | 5 (9.1) | 5 (8.1) | 4 (14.8) | 0.60 |
| 12 months [n, (%)] | 7 (12.7) | 7 (11.3) | 4 (14.8) | 0.89 |
| VC progression | n = 64 | n = 78 | n = 31 | 0.07 |
| SQ grade 3 [n, (%)] | 25 (39.1) | 19 (24.3) | 6 (19.4) | |
| BMD change at 12 months (%) | ||||
| Lumbar (L2–4) | 6.3 ± 8.1 | 8.1 ± 7.4 | 8.8 ± 11.2 | 0.18 |
| Total hip | −2.8 ± 7.9 | −0.9 ± 7.5 | −0.4 ± 7.3 | 0.39 |
| Pseudarthrosis | n = 67 | n = 87 | n = 40 | |
| Total [n, (%)] | 13 (19.4) | 15 (17.2) | 6 (15) | 0.84 |
| Unstable type [n, (%)] | 11 (16.4) | 4 (4.6) | 2 (5) | 0.03⁎ |
BP; bisphosphonates, TPTD; teriparatide, Romo; romosozumab, OVF; osteoporotic vertebral fracture, VC; vertebral collapse, SQ; semiquantitative, BMD; bone mineral density.
3.3. Secondary outcomes
No significant difference in VC progression for SQ grade 3 was observed among the three groups (BP: 39.1 %, TPTD: 24.3 %, Romo: 19.4 %, p = 0.07). Pseudarthrosis was also not significantly different among the groups (BP: 19.4 %, TPTD: 17.2 %, Romo: 15 %, p = 0.84). However, unstable pseudarthrosis was significantly higher in the BP group than in the TPTD and Romo groups (16.5 % vs. 4.6 % and 5 %, respectively; p = 0.03). There were no significant differences in lumbar or total hip BMD changes between the BP, TPTD, and Romo groups (lumbar BMD change: 6.3 % vs. 8.1 % vs. 8.8 %, p = 0.18; total hip BMD change: −2.8 % vs. −0.9 % vs. −0.4 %, p = 0.18). In all 3 groups, VAS and ODI showed significant improvement at 3 and 12 months compared to baseline (p < 0.01). There were no significant differences in VAS and ODI between the three groups at any time point (Table 4).
Table 4.
The results of VAS score and ODI at baseline, 3 months, and 12 months across the three groups.
| Variable | BP (n = 55) |
TPTD (n = 62) |
Romo (n = 27) |
p-value |
|---|---|---|---|---|
| VAS score | ||||
| Baseline | 65.5 ± 19.6 | 69.7 ± 24.6 | 62.5 ± 29.7 | 0.35 |
| 3 months | 42.4 ± 30.3 | 33.2 ± 23.1 | 28.6 ± 22.9 | 0.07 |
| 12 months | 23.7 ± 4.6 | 30.8 ± 26.2 | 24.7 ± 24.5 | 0.34 |
| ODI (%) | ||||
| Baseline | 46.1 ± 16.7 | 53.9 ± 20.4 | 48.5 ± 23.2 | 0.21 |
| 3 months | 28.3 ± 20.4 | 34.9 ± 18.9 | 29.8 ± 19.32 | 0.26 |
| 12 months | 20.7 ± 19.3 | 30.9 ± 19.6 | 27.2 ± 21.4 | 0.11 |
VAS; visual analogue scale, ODI; Oswestry Disability Index, BP; bisphosphonates, TPTD; teriparatide, Romo; romosozumab.
4. Discussion
In this study, osteoanabolic agents did not provide any advantage over BP in preventing subsequent domino OVF within 3 months. Some reasons for these results are as follows. First, the administration period could be too short to provide a substantial anabolic effect in the TPTD group. A histomorphometric analysis revealed that bone formation significantly increases at least 3 months after TPTD treatment (Sawakami et al., 2022). Second, in previous reports, a higher prevalence of OVF was associated with an increased risk of subsequent OVF (Hagino et al., 2013; Lindsay et al., 2001). The anabolic agent group may have included patients with more severe osteoporosis. Nevertheless, the risk factors for subsequent domino OVF remain unclear and may be multifactorial. Although there was no statistically significant difference in subsequent domino OVF among the three groups, the Romo group showed a trend toward more use of soft bracing (63 %) than the BP (47 %) or TPTD (44 %) groups. Paradoxically, no subsequent OVFs were observed in the Romo group between 3 and 12 months. Notably, Inose et al. indicated that a soft brace was associated with a higher risk of subsequent OVF (Inose et al., 2021). Most of the anabolic effect of romosozumab appears within the first 3 months, and is over by the 6 months. However, using osteoanabolic agents alone to prevent domino OVFs is difficult because the pathogenesis of domino OVF may have multifactorial causes, such as mechanical instability due to osteoporosis medication and stress concentration caused by kyphotic deformity.
Several studies have demonstrated the advantages of TPTD over BP or naïve in terms of VC progression, bone healing, and pain (Ikeda et al., 2020; Iwata et al., 2017; Kitaguchi et al., 2019; Nair et al., 2023; Tsuchie et al., 2016). In particular, several reports have demonstrated earlier bone union after treatment with TPTD than with BP (Kitaguchi et al., 2019; Nair et al., 2023; Shigenobu et al., 2019). The incidence of nonunion or pseudoarthrosis ranges from 9.8 % to 19.6 %, and intervertebral cleft or gas is commonly seen on radiographs, CT, or MRI (Inose et al., 2020; Takahashi et al., 2016; Tsujio et al., 2011; Wakao et al., 2023). However, diagnosing pseudarthrosis based on the presence of a cleft or fluid on static images is challenging, prompting us to classify them as either stable or unstable based on dynamic factors evaluated using X-rays in the lateral sitting position. Our study showed that the conventional definition of pseudarthrosis was equivalent among all groups at 12 months, as well as a comparable incidence of pseudoarthrosis to previous reports (Inose et al., 2020; Takahashi et al., 2016; Tsujio et al., 2011; Wakao et al., 2023). Notably, the TPTD and Romo groups had a significantly lower incidence of unstable pseudoarthrosis versus the BP group (4.6 % and 5 % vs.14.6 %). Our results were also lower than those of previous studies of pseudoarthrosis (Inose et al., 2020; Wakao et al., 2023), which was defined as the presence of an intervertebral cleft in the seated position and an incidence of 9.8 % (Wakao et al., 2023). This was likely due to our definition of pseudoarthrosis and the use of antiosteoporotic medication. In addition, most studies used BP as a medication for osteoporosis, but in our study, 62.8 % of patients used osteoanabolic agents. In particular, little is known about the effects of Romo on bone union for conservative treatment of OVF. Hayashi et al. demonstrated that TPTD treatment had a significantly higher union rate versus Romo at 6 months (Hayashi, 2023). Conversely, Park et al. reported a significant decrease in the numerical rating scale for back pain in the Romo group compared to the TPTD group, but radiographic outcomes were equivalent (Park et al., 2023). Our study demonstrated unstable pseudarthrosis was significantly higher in the BP group than in the TPTD and Romo groups. Also, our results showed that the TPTD and Romo groups were superior to the BP group in terms of bone healing at 12 months, suggesting that osteoanabolic agents may have contributed to the formation of a bony bridge to the adjacent vertebra.
The VC progression leads to delayed union and causes residual back pain (Yasuda et al., 2017). In this study, there were no significant differences among groups in VC progression, but tended to be higher in the BP groups (39.1 %) than the TPTD (24.3 %) and Romo groups (19.4 %). Hoshino et al. (2013) reported that VC progression was found in 31.2 % of patients and was associated with middle-column injury, while Okuwaki et al. demonstrated its correlation with posterior wall injury, vertebral instability, and vitamin D levels (Okuwaki et al., 2022). Hence, the progression of VC is related to the severity of OVF at baseline. Recent comparative studies between BP and TPTD have shown similar progression of VC (Ikeda et al., 2020; Iwata et al., 2017). Studies have concluded that VC progresses immediately after a fracture (Ikeda et al., 2020), and thus it can occur before osteoanabolic agents have an effect on vertebral mechanical strength. In our study, VC progression was not significantly reduced after treatment with TPTD and Romo.
There was no significant difference in the change in lumbar and total hip BMD among the three groups after 12 months. BMD, particularly total hip BMD, decreased in all 3 groups after 12 months. The reasons for our results are as follows. First, the baseline population of this study included patients with severe osteoporosis, such as prevalent OVFs, multiple OVFs, and severe VC (SQ grade 3). Second, disuse or decline of walking ability after OVF may affect decreased BMD, with age- and sex-related heterogeneity compared to previous reports. Notably, however, the VAS score and ODI significantly improved at 3 and 12 months in all 3 groups, suggesting that the type of osteoporosis medication did not affect the patient's QOL after 12 months of conservative treatment.
This study had several limitations. First, the original cohort study did not include a placebo or control group. Additionally, patients with severe VC at baseline were significantly different among the three groups. To prove the efficacy of osteoanabolic agents, randomized prospective studies are required to corroborate our findings. Second, since this was a multicenter study, the type of brace and medication were not standardized; differences in the type of conservative treatment may have affected our outcomes. Third, the follow-up period of 12 months may not be sufficient to observe the natural course of OVF. Longer follow-up is required to consider kyphotic deformity and spinal alignment after OVF. Forth, the denosumab group was excluded due to the small number of patients in this study. Denosumab may have been administered to patients with more severe osteoporosis than bisphosphonates. In addition, twenty patients with no osteoporosis medication were excluded. There were no clear criteria for the management of osteoporosis medications. Fifth, the original study excluded subjects with >3 prevalent OVFs who were likely at high risk for subsequent domino OVFs, so such subjects were not available for this analysis. Despite these limitations, this observational study of conservative treatment for OVF is clinically significant and may support the selection of osteoporosis treatment.
In summary, although the osteoanabolic agents were not more effective than the bisphosphonates in the development of domino OVF, they significantly reduced the occurrence of unstable pseudoarthrosis. A prospective, randomized, controlled study is needed to assess the efficacy of osteoanabolic agents for subsequent OVFs. A more comprehensive approach to the treatment of osteoporosis is needed to prevent domino OVF.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Keishi Maruo: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation. Tomoyuki Kusukawa: Data curation. Masakazu Toi: Data curation. Tetsuto Yamaura: Investigation, Data curation. Masaru Hatano: Investigation. Hayato Oishi: Investigation. Kazuma Nagao: Investigation. Fumihiro Arizumi: Investigation. Kazuya Kishima: Investigation. Norichika Yoshie: Investigation. Toshiya Tachibana: Supervision.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability
The data that has been used is confidential.
References
- Balasubramanian A., Zhang J., Chen L., Wenkert D., Daigle S.G., Grauer A., Curtis J.R. Risk of subsequent fracture after prior fracture among older women. Osteoporos. Int. 2019;30(1):79–92. doi: 10.1007/s00198-018-4732-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banefelt J., Akesson K.E., Spangeus A., Ljunggren O., Karlsson L., Strom O., Ortsater G., Libanati C., Toth E. Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos. Int. 2019;30(3):601–609. doi: 10.1007/s00198-019-04852-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genant H.K., Wu C.Y., van Kuijk C., Nevitt M.C. Vertebral fracture assessment using a semiquantitative technique. J. Bone Miner. Res. 1993;8(9):1137–1148. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- Hagino H., Shiraki M., Fukunaga M., Nakano T., Takaoka K., Ohashi Y., Nakamura T., Matsumoto T. Number and severity of prevalent vertebral fractures and the risk of subsequent vertebral fractures in Japanese women with osteoporosis: results from the minodronate trial. J. Bone Miner. Metab. 2013;31(5):544–550. doi: 10.1007/s00774-013-0439-8. [DOI] [PubMed] [Google Scholar]
- Hayashi K. Efficacy of three teriparatide preparations and romosozumab, osteogenesis promoters, in the treatment of fresh vertebral fractures: A retrospective observational study. Drugs Real World Outcomes. 2023;10(4):631–637. doi: 10.1007/s40801-023-00385-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoshino M., Tsujio T., Terai H., Namikawa T., Kato M., Matsumura A., Suzuki A., Takayama K., Takaoka K., Nakamura H. Impact of initial conservative treatment interventions on the outcomes of patients with osteoporotic vertebral fractures. Spine (Phila Pa 1976) 2013;38(11):E641–E648. doi: 10.1097/BRS.0b013e31828ced9d. [DOI] [PubMed] [Google Scholar]
- Ikeda S., Nakamura E., Narusawa K., Fukuda F., Matsumoto H., Nakai K., Sakata T., Yoshioka T., Fujino Y., Sakai A., Investigators K.T.W.S. Comparison of once-weekly teriparatide and alendronate against new osteoporotic vertebral fractures at week 12. J. Bone Miner. Metab. 2020;38(1):44–53. doi: 10.1007/s00774-019-01023-x. [DOI] [PubMed] [Google Scholar]
- Inose H., Kato T., Ichimura S., Nakamura H., Hoshino M., Togawa D., Hirano T., Tokuhashi Y., Ohba T., Haro H., Tsuji T., Sato K., Sasao Y., Takahata M., Otani K., Momoshima S., Yuasa M., Hirai T., Yoshii T., Okawa A. Risk factors of nonunion after acute osteoporotic vertebral fractures: A prospective multicenter cohort study. Spine (Phila Pa 1976) 2020;45(13):895–902. doi: 10.1097/BRS.0000000000003413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inose H., Kato T., Ichimura S., Nakamura H., Hoshino M., Togawa D., Hirano T., Tokuhashi Y., Ohba T., Haro H., Tsuji T., Sato K., Sasao Y., Takahata M., Otani K., Momoshima S., Takahashi K., Yuasa M., Hirai T.…Okawa A. Risk factors for subsequent vertebral fracture after acute osteoporotic vertebral fractures. Eur. Spine J. 2021;30(9):2698–2707. doi: 10.1007/s00586-021-06741-3. [DOI] [PubMed] [Google Scholar]
- Iwata A., Kanayama M., Oha F., Hashimoto T., Iwasaki N. Effect of teriparatide (rh-PTH 1-34) versus bisphosphonate on the healing of osteoporotic vertebral compression fracture: A retrospective comparative study. BMC Musculoskelet. Disord. 2017;18(1):148. doi: 10.1186/s12891-017-1509-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitaguchi K., Kashii M., Ebina K., Sasaki S., Tsukamoto Y., Yoshikawa H., Murase T. Effects of weekly teriparatide administration for vertebral stability and bony union in patients with acute osteoporotic vertebral fractures. Asian Spine J. 2019;13(5):763–771. doi: 10.31616/asj.2018.0311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostenuik P.J., Binkley N., Anderson P.A. Advances in osteoporosis therapy: focus on osteoanabolic agents, secondary fracture prevention, and perioperative bone health. Curr. Osteoporos. Rep. 2023;21(4):386–400. doi: 10.1007/s11914-023-00793-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kusukawa T., Maruo K., Toi M., Yamaura T., Hatano M., Nagao K., Oishi H., Horinouchi Y., Arizumi F., Kishima K., Yoshie N., Tachibana T. Subsequent domino osteoporotic vertebral fractures adversely affect short-term health-related quality of life: A prospective multicenter study. Medicina (Kaunas) 2023;59(3) doi: 10.3390/medicina59030590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay R., Silverman S.L., Cooper C., Hanley D.A., Barton I., Broy S.B., Licata A., Benhamou L., Geusens P., Flowers K., Stracke H., Seeman E. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001;285(3):320–323. doi: 10.1001/jama.285.3.320. [DOI] [PubMed] [Google Scholar]
- Nair V.V., Kundnani V., Shetty A., Anand M., Jain M., Dewnany N. Is teriparatide superior in treating osteoporotic vertebral compression fractures in comparison to bisphosphonates treatment alone: A 2-year retrospective analysis. Asian Spine J. 2023;17(6):1098–1107. doi: 10.31616/asj.2023.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuwaki S., Funayama T., Ikumi A., Shibao Y., Miura K., Noguchi H., Takahashi H., Koda M., Tatsumura M., Kawamura H., Yamazaki M. Risk factors affecting vertebral collapse and kyphotic progression in postmenopausal osteoporotic vertebral fractures. J. Bone Miner. Metab. 2022;40(2):301–307. doi: 10.1007/s00774-021-01283-6. [DOI] [PubMed] [Google Scholar]
- Park D., Kim S.E., Shin H.K., Seo J., Joo J.K., Kim C., Lee S.H., Park J.H. Comparison of the efficacy of Romosozumab and Teriparatide for the Management of Osteoporotic Vertebral Compression Fractures. Neurospine. 2023;20(4):1217–1223. doi: 10.14245/ns.2347030.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux C., Briot K. Imminent fracture risk. Osteoporos. Int. 2017;28(6):1765–1769. doi: 10.1007/s00198-017-3976-5. [DOI] [PubMed] [Google Scholar]
- Sawakami K., Watanabe K., Hasegawa K., Yamamoto N., Shimakura T., Ohashi M., Shoji H., Mizouchi T., Tanaka Y., Segawa H., Ishikawa S., Hirano T., Kawashima H., Endo N., Takahashi H.E. Neoadjuvant teriparatide therapy targeting the osteoporotic spine: influence of administration period from the perspective of bone histomorphometry. J. Neurosurg. Spine. 2022;36(3):429–439. doi: 10.3171/2021.5.SPINE202003. [DOI] [PubMed] [Google Scholar]
- Shigenobu K., Hashimoto T., Kanayama M., Ohha H., Yamane S. The efficacy of osteoporotic treatment in patients with new spinal vertebral compression fracture pain, ADL, QOL, bone metabolism and fracture-healing - in comparison with weekly teriparatide with bisphosphonate. Bone Rep. 2019;11 doi: 10.1016/j.bonr.2019.100217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi S., Hoshino M., Takayama K., Iseki K., Sasaoka R., Tsujio T., Yasuda H., Sasaki T., Kanematsu F., Kono H., Toyoda H., Nakamura H. Predicting delayed union in osteoporotic vertebral fractures with consecutive magnetic resonance imaging in the acute phase: A multicenter cohort study. Osteoporos. Int. 2016;27(12):3567–3575. doi: 10.1007/s00198-016-3687-3. [DOI] [PubMed] [Google Scholar]
- Tsuchie H., Miyakoshi N., Kasukawa Y., Nishi T., Abe H., Segawa T., Shimada Y. The effect of teriparatide to alleviate pain and to prevent vertebral collapse after fresh osteoporotic vertebral fracture. J. Bone Miner. Metab. 2016;34(1):86–91. doi: 10.1007/s00774-014-0646-y. [DOI] [PubMed] [Google Scholar]
- Tsujio T., Nakamura H., Terai H., Hoshino M., Namikawa T., Matsumura A., Kato M., Suzuki A., Takayama K., Fukushima W., Kondo K., Hirota Y., Takaoka K. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: A prospective multicenter study. Spine (Phila Pa 1976) 2011;36(15):1229–1235. doi: 10.1097/BRS.0b013e3181f29e8d. [DOI] [PubMed] [Google Scholar]
- van Geel T.A., Huntjens K.M., van den Bergh J.P., Dinant G.J., Geusens P.P. Timing of subsequent fractures after an initial fracture. Curr. Osteoporos. Rep. 2010;8(3):118–122. doi: 10.1007/s11914-010-0023-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakao N., Sakai Y., Watanabe T., Osada N., Sugiura T., Iida H., Ozawa Y., Murotani K. Spinal pseudoarthrosis following osteoporotic vertebral fracture: prevalence, risk factors, and influence on patients’ activities of daily living 1 year after injury. Arch Osteoporos. 2023;18(1):45. doi: 10.1007/s11657-023-01236-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong R.M.Y., Wong P.Y., Liu C., Wong H.W., Chung Y.L., Chow S.K.H., Law S.W., Cheung W.H. The imminent risk of a fracture-existing worldwide data: A systematic review and meta-analysis. Osteoporos. Int. 2022;33(12):2453–2466. doi: 10.1007/s00198-022-06473-0. [DOI] [PubMed] [Google Scholar]
- Yamaura T., Arizumi F., Maruo K., Kishima K., Yoshie N., Kusukawa T., Imamura F., Tachibana T. Adjacent vertebral Hounsfield unit value of acute osteoporotic vertebral fracture is a risk factor for concomitant domino osteoporotic vertebral fractures. J. Orthop. Sci. 2023;28(3):536–542. doi: 10.1016/j.jos.2022.02.001. [DOI] [PubMed] [Google Scholar]
- Yasuda H., Hoshino M., Tsujio T., Terai H., Namikawa T., Kato M., Matsumura A., Suzuki A., Takayama K., Takahashi S., Nakamura H. Difference of clinical course between cases with bone union and those with delayed union following osteoporotic vertebral fractures. Arch. Osteoporos. 2017;13(1):3. doi: 10.1007/s11657-017-0411-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.