Abstract
Introduction
Chatbots emulate human-like interactions and may usefully provide on-demand access to tailored smoking cessation support. We have developed a prototype smartphone application-based smoking cessation chatbot, named Quin, grounded in real-world, evidence-, and theory-based smoking cessation counseling sessions.
Methods
Conversation topics and interactions in Quitline counseling sessions (N = 30; 18 h) were characterized using thematic, content, and proponent analyses of transcripts. Quin was created by programming this content using a chatbot framework which interacts with users via speech to text. Reiterative changes and additions were made to the conversation structure and dialogue following regular consultation with a multidisciplinary team from relevant fields, and from evidence-based resources.
Results
Chatbot conversations were encoded into initial and scheduled follow-up “appointments.” Collection of demographic information, and smoking and quit history, informed tailored discussion about pharmacotherapy preferences, behavioral strategies, and social and professional support to form a quit plan. Follow-up appointments were programmed to check in on user progress, review elements of the quit plan, answer questions, and solve issues. Quin was programmed to include teachable moments and educational content to enhance health literacy and informed decision-making. Personal agency is encouraged through exploration and self-reflection of users’ personal behaviors, experiences, preferences, and ideas.
Conclusions
Quin’s successful development represents a movement toward improving access to personalized smoking cessation support. Qualitative foundations of Quin provide greater insight into the smoking cessation counseling relationship and enhances the conversational ability of the technology. The prototype chatbot will be refined through beta-testing with end users and stakeholders prior to evaluation in a clinical trial.
Implications
Our novel study provides transparent description of the translation of qualitative evidence of real-world smoking cessation counseling sessions into the design and development of a prototype smoking cessation chatbot. The successful iterative development of Quin not only embodies the science and art of health promotion, but also a step forward in expanding the reach of tailored, evidence based, in-pocket support for people who want to quit smoking.
Introduction
Tobacco dependence is a chronic relapse-remitting condition.1 Unassisted smoking cessation attempts have a high failure rate (96%–97%) and successful smoking cessation often requires multiple quit attempts.2 Smoking cessation support increases the success rate of individual quit attempts.3 While there is strong evidence for the effectiveness of pharmacotherapy alone,4,5 the likelihood of successful quitting further increases with the addition of behavioral support.6 However, engagement with professional support services is often limited by the level of individual awareness7 and accessibility.8,9 Due to low uptake of professional assistance,10,11 other services, and digital platforms have been developed to enhance the reach of behavioral interventions.
We have observed the technological advancement of platforms for smoking cessation assistance expand from a single computer-generated tailored letter,12 to telephone counseling,13 internet14- and text-message (SMS)15 based programs, and smartphone applications with various features.16 Mobile smoking cessation (mCessation) apps combine the important benefits of SMS and internet-based interventions, such as providing on-demand, in-pocket access, and mimicking social support.17–19 There is currently an abundance of mCessation apps available for download, and a rising trend in their use has been observed.20,21 However, many lack evidence of clinical effectiveness, are not tailored or intuitive, and are of low quality.22,23 Despite their accessibility and reach, there is currently insufficient evidence to routinely prescribe mCessation apps for usual care,16,22 and consumer-led design and development research to support clinical effectiveness is limited.24,25 As such, we need to consider how mCessation technology can be improved to provide effective personalized support and increase user engagement.
Conversational artificial intelligence (AI), such as chatbots, dialogue systems, and conversational agents, can converse with users via audio and/or text without human input. These AI systems employ machine learning and natural language processing (NLP) algorithms to create a human-like dialogue. Modern chatbots typically use a combination of two approaches; (1) a rule-based approach, which relies on rules defined by expert knowledge (eg, a conversation tree); and (2) a probabilistic approach which ascertains how to classify answers and potentially how to generate responses through exposure to training text.26 As AI systems learn to adapt to users’ personalities, these interactions tend to become even more effortless and tailored.
Mohr’s “Model of Supportive Accountability” states that engagement with digital health interventions is promoted with the addition of human support by cultivating a sense of personal accountability to a competent, trustworthy, and caring coach.27 In contrast to mCessation interventions, there is evidence to support the effectiveness of proactive telephone-based smoking cessation counseling13 whereby counselors are primarily trained to deliver motivational interviewing (MI) techniques and/or cognitive behavioral therapy (CBT) alongside evidence-based information.28 However uptake and reach of these services relies on clients’ willingness and capacity to engage with an unknown counselor, and previous research has highlighted feelings of shame, guilt, and stigma associated with these interactions.29 A chatbot programmed to provide tailored support, delivered via a mCessation app, may be more appealing and accessible for people hesitant to use standard telephone services. Encouragingly, previous research has shown people interact with, and disclose information to, chatbots in similar ways as they do humans.30 Therefore, translation of practical and effective smoking cessation counseling into chatbot technology may help to improve the quality of mCessation interventions and provide a highly accessible and potentially comparable option for those who do not want to engage with professional services, but need support.
The development and use of conversational AI systems for smoking cessation is an emerging area of research and the current literature highlights many opportunities for progress. Publicly available smoking cessation chatbots include Florence,31Bella,32 and Alex AI,33 yet there are no publications describing their development or clinical trials to support their effectiveness and acceptability. A recent scoping review of chatbots for smoking cessation found limited low-quality evidence to support the effectiveness of their use in usual care, but found anecdotal evidence of their benefits to smoking cessation and user engagement.34 Randomized controlled trials of conversational AI for smoking cessation are often limited by low follow-up rates and there is significant heterogeneity between interventions and study designs.35 Furthermore, there is limited evidence describing the development methods for smoking cessation chatbots.26 Development of mCessation apps often employs a “top-down” approach, in that behavior change theories or frameworks are incorporated into the apps by the researchers with little or no input from the end user during development.36–38 This can be problematic as consumers and researchers may place differing values on specific app functions.39 Therefore, this study aims to develop a prototype smartphone application-based smoking cessation chatbot, named Quin, using a co-design approach grounded in real-world, evidence-based smoking cessation counseling sessions to effectively incorporate the experiences, needs and knowledge of consumers, and other stakeholders.
Method
Ethical Considerations
This study was approved by The Prince Charles Hospital Human Research Ethics Committee (Project ID: 50620). A waiver of obtaining individual informed consent from Quitline clients was obtained via a Public Health Act 2005 (PHA 50620) application, and a formal agreement between HM and Quitline (Queensland Health) was executed, prior to accessing the audio files.
Sample Frame and Client Characteristics
This study used a purposive sample of recorded telephone-counseling sessions from an administrative dataset selected and provided by Quitline (Queensland Health). All Quitline calls are recorded for quality assurance and training, and this is explained to clients at the beginning of each call. Thirty audio files were provided based on demographic characteristics (eg, age, sex, rural/remote location, and Indigenous status), and were manually transcribed verbatim with identifiable information redacted.
Calls were completed by 23 individual counselors (Female, n = 21; Male, n = 2) between January and March 2019. The sample contained 18 h of audio, and call length ranged from 16 to 56 min (Mean = 36 min, SD = 10 min). The 30 transcripts included 26 initial calls and four support calls. Type of call was determined during analysis and was not known during purposive sampling. Additional details regarding client demographics, smoking behaviors, and quit histories have been published elsewhere.40
Transcript Analysis
Individual files were imported to NVivo (Version 12), and coded topics (with relevant statements, questions, and responses) were also transferred to and collated in sequence in Microsoft Excel for each transcript.
First, thematic analysis of transcripts was completed by two members of the study team (HB and SL) to explore conversation topics and themes, and to identify question topics asked by clients during the calls. Methods and results have been published elsewhere.40
Second, a content analysis quantified and collated topics in order of occurrence for individual transcripts, and mapped to conversation stage, to inform basic structure of a counseling conversation. For each call, the total number of topics was divided into thirds to reflect the beginning, middle, and end of conversations. Topic occurrences were mapped to these time periods. Initial and follow-up calls were analyzed separately. Descriptive statistics for each topic were calculated including total prevalence and prevalence across time periods, number of transcripts, and number of transcripts where the topic was repeated more than once.
Third, a proponent analysis41 was completed to explore content (who said what) within themes and topics, with appropriate statements, questions, and responses from counselors and clients used to inform chatbot interaction.
Chatbot Development
Quin was created by a multidisciplinary team from the fields of thoracic medicine, smoking cessation, health psychology, computer science, health promotion, tobacco control, and public health. The technical development of Quin was undertaken by an experienced computer scientist (DI), with assistance from vacation students and a public health PhD student (HB). In CSIRO’s previous chatbot development, we have found the personality, preferred vocabulary, and sentence structure of the person developing the responses is evident in the chatbot through subtle language cues.41,42 Thus, the benefit of multiple contributors allowed Quin to develop a distinct personality in its responses.
Skeleton structure and content was mapped to a flowchart using Lucidchart software, in which the conversation progressed through categories of themes, and users were prompted through the chatbot content. Iterative changes and additions were made to the structure and content following regular collaborative consultation with the team. These consultations also included comparisons with information from evidence-based resources to ensure breadth and accuracy of information.
The chatbot content was programmed using a chatbot framework, known as CSIBot, which was developed by the Commonwealth Scientific and Industrial Research Organisation (CSIRO), Australia. The framework consists of a collection of NLP algorithms and has been used for other health chatbots including EDNA for genetic counseling,41 and HARLIE42 for autism spectrum disorder. Additionally, this framework can function in a mobile application or web-based service.
The case-based reasoner is the primary response system and works on the structure (syntax) of human communication using two main algorithms; (1) syntactic matching; and (2) sentiment analysis. Syntactic matching analyses the utterance received and examines word order and the current context of the conversation to determine the most appropriate response. The radix tree data structure is used to store the responses and the various human stimuli that solicit the particular response43 (Figure S1). This is a common data structure in computer science that allows for compression of textual data while preserving fast search times. Nodes of the tree are the possible words of the human utterances (or wildcard matching syntax). Traversal of the radix tree structure returns a template response that may include wildcard substitutions and additional operations for the chatbot to do (eg, log to an internal database). For example, the user tells Quin that they live with someone who smokes, Quin queries their relationship to that person (if not already stated) and asks if the person will be supportive of their quit attempt (Figure 1).
Figure 1.
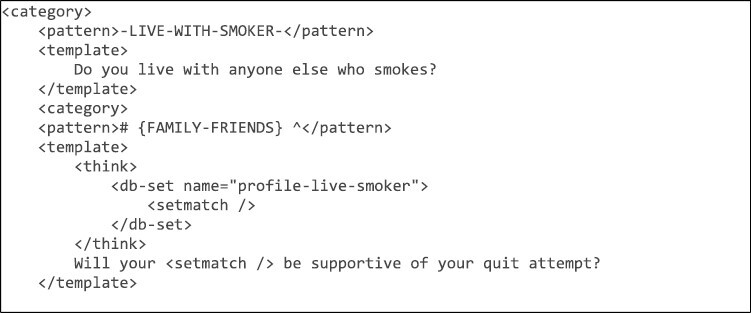
Example of syntactic matching within Quin.
The likelihood of a negative sentiment is identified using the sentiment analysis algorithm, which informs Quin’s response. For example, when exploring previous pharmacotherapy use, Quin can detect and acknowledge a negative experience (Figure S2).
The chatbot uses the Google Cloud speech-to-text service. Speech utterances converted by this service are not logged. The chatbot can recognize and respond in speech or text. Text input by the user is also available when difficulties with speech recognition arise. Screenshots of Quin’s user interface are included in Figure S3. The Quin user interface includes links to educational videos and Quitline services, the ability to upload motivational images, cost analysis to track savings, health diary to track cigarettes smoked and cravings, games for distractions, a “To-Do List” based on the agreed quit plan, and an editable summary of the profile information collected within the chatbot dialogue. All dialogs are currently stored on Google Cloud Firebase for debugging purposes and users also can send feedback to the server. The user can export dialogs to PDF locally on the device, and delete data if they wish to restart the process.
Results
Smoking cessation counseling interactions that could be delivered by Quin, and conversation design, were determined using the combination of analyses and programmed accordingly.
Translating Conversation Flow and Interactions
Building upon the 7 themes and 35 topics identified in our previous study,40 results from the content analysis and proponent analysis provided further detail to inform Quin’s conversation flow and interactions, respectively.
Content Analysis and Conversation Flow
The mean number of topics for initial and support calls, were 28 (Min 13; Max 41) and 23 (Min 19; Max 28), respectively. The five most prevalent topics within initial calls were: (1) Routines, triggers, and strategies (n = 72); (2) Smoking and quit history (n = 63); (3) Quitline program (n = 47); (4) Planning to quit and goal setting (n = 42); and (5) Motivation for quitting (n = 37). “Routines, triggers and strategies” was also the most prevalent topic across the middle and end stages of conversations, while “Smoking and quit history” was the most and second most common topic within the beginning and middle stages of conversations, respectively. Topics that were exclusive to the end stage of conversations included “Reinforcing quit plan,” and “Reflection and feedback” (Figure S4).
Similarly, “Routines, triggers and cravings” (n = 13), and “Smoking and quit history” (n = 7) were the most prevalent topics occurring across all three stages of support call conversations. Discussions about “Current attempt” occurred exclusively at the beginning of support call conversations, while other topics were exclusive to the end of conversations including: “Confidence to quit”; “Personal life”; “Professional support”; “Reflection and feedback”; and “Scheduling follow up” (Figure S5).
Skeleton conversation structures for Quin’s initial (Figure 2) and follow-up (Figure S6) appointment conversations were guided by this information, with particular focus on topics exclusive to certain conversation stages. Given “Routine, triggers and cravings” and “Smoking and quit history” were pervasive throughout conversations, effort was made to collect and refer to this information provided by users where appropriate within Quin’s dialogue.
Figure 2.
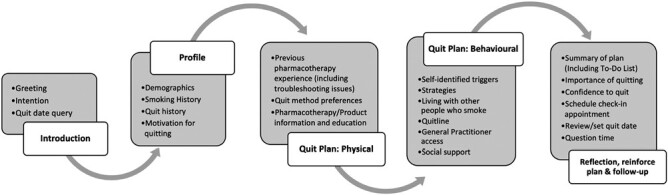
Quin initial appointment conversation structure.
Interactions with Quin
Interactions identified in the proponent analysis across all themes were able to be delivered by a chatbot. See Table 1 for examples of transcript dialogue between counselors and clients, and Quin’s equivalent interactions. Quin was programmed to sequentially move through a workflow of topics or allow users to ask specific questions. Interactive buttons, text input or speech input facilitate the user progression through the chatbot interaction. Users can opt-out at any stage of the conversation, but profile information previously collected is stored. Upon reopening of the app, Quin allows users to pick up from the end of the profile (if completed) or start over completely.
Table 1.
Examples of Transcript Dialogue (Counsellor and Client) and Equivalent Quin Dialogue/Response
| Theme | Counsellor proponent | Quin proponent | Client proponent | Quin response/data linkage |
|---|---|---|---|---|
| Client details and building rapport | I see that you’re of Aboriginal origin, is that correct? We have Aboriginal counsellors that work here at Quitline . . . [T1] |
Are you of Aboriginal and/or Torres Strait Islander origin? | Yes |
Quitline information
They also offer Indigenous counsellors if you would prefer to speak to them. |
| Client history and motivation to quit | What’s got you wanted to quit at the moment? [T13] | What is motivating/has motivated you to quit smoking? | Cost | Extra cash is a great reward for quitting smoking! Are you saving up for something? |
| Understanding nicotine dependence | Do you know how nicotine works in your brain or anything like that? [T3] | Just before we start. It’s good to know how nicotine works in our body so the products we might talk about make more sense. Can I quickly tell you about this? | No (Counsellor proponent) Yes (Quin proponent) |
Nicotine is that addictive part of tobacco. When you have cigarette, you get that hit of nicotine that reaches your brain within seconds through your bloodstream and triggers the reward centre . . . (cont) |
| Pharmacotherapy | So based on that, we would recommend for you to use . . . both the patches and oral products. [T11] | Based on how many cigarettes you are currently smoking and how soon after waking you have a cigarette, I’m thinking you would benefit from using a combination of NRT patch and oral NRT. We’ll cover this a bit later. | N/A | N/A |
| Behavioral aspects of quitting | With that morning coffee though, how are you going to cope with changing out that one? What are you going to do and commit to? [T15] | Have you thought about changing your coffee/tea routine? . . . How do you think you might manage avoiding cigarettes with your coffee or tea? | Go for a walk or something | Good thinking |
| Additional support and smoking cessation resources | Alright and so I know you said that your partner smokes as well. What sort of support will they be able to provide? [T13] | Do you live with anyone else who smokes? Will your [FAMILY-FRIENDS] be supportive of your quit? |
That’s the hardest bit | [SENTIMENT ANALYSIS] This can be really tricky. We can talk about this a little later. |
| Planning, goal setting, and follow-up | So, in terms of quitting smoking, did you have an idea when you would like to be doing that? [T4] | Have you set a quit date? | This Thursday. (Counsellor proponent) Yes (Quin proponent) |
Great, it’s motivating to have a goal. What date did you decide on? [CALENDAR WIDGET] |
[T], transcript number; NRT, nicotine replacement therapy.
Quin begins the initial conversation by introducing itself, determining users’ intent (including querying if a quit date has been set) and asking the user to type in their name for spelling accuracy. The syntactic matching algorithm detects their name and responds to the user by referring to them by name going forward.
Quin then navigates the user through creation of a profile (demographic information, smoking and quit history, motivation/s for quitting), and formulation of a quit plan including pharmacotherapy experiences and preferences, behavioral strategies for self-identified triggers, and social and professional support structures. Quit plan information is repeated back to the user for confirmation toward the end of the initial conversation and a summary “To-do” checklist is accessible in the side-bar. As observed in Quitline practice, Quin then ends the initial conversation by gauging importance of quitting for the user and their confidence (or quit self-efficacy) on a 10-point-scale, suggesting a timeframe (days) for a follow-up appointment, confirming self-selected quit date or encouraging setting one if not previously done, and allowing for question-time.
Follow-up appointments are programmed to draw upon quit plan information and check in on user’s progress. Users are first asked how they are going with their quit attempt. For users who have quit or cut down, Quin confirms elements of the quit plan including type of pharmacotherapy and if any issues/side effects are being experienced, strategies for managing cues and triggers, engagement with professional support, and level of social support. Reasons for inaction or relapse are explored and solutions suggested for those who have not yet started or had quit but slipped up, respectively.
Questions or issues raised by clients within the counseling transcripts were coded so that Quin could respond appropriately in the chatbot dialogue. Quin replies with an “Ok” when it does not have a response to a declarative utterance. When issues or questions raised are outside of the scope of interaction with Quin, in that the chatbot is not coded with the appropriate response or does not understand the utterance after two attempts, the user is encouraged to speak with their health professional or Quitline.
Tailoring the Conversation and Quit Plan
As identified in the content analysis, review of the client’s smoking and quit history information permeates throughout the typical counseling conversation in order to personalize quit plans. This created a challenge to see if Quin could collect this history and use it in a meaningful way to inform and deliver tailored recommendations and interactions/dialogue.
A large proportion of Quin’s initial conversation is dedicated to gathering information on users’ demographics, current or past smoking behavior/s, and their experience with quitting including pharmacotherapy use, professional support, and reasons for relapse. The chatbot is programmed to detect and draw upon this information in many instances. Detailed examples are outlined in Table 2. Two questions regarding smoking history provide scores to determine heaviness of smoking, and results inform Quin’s recommendation for type of pharmacotherapy as well as length of time to next appointment. Quin also refers to demographic and quit history information throughout the initial conversation, including via syntactic matching algorithms and sentiment analyses.
Table 2.
Examples of Data Linkage/Personalization Within Quin Dialogue
| Category | Subcategory | Dialogue | Later category | Question/Statement |
|---|---|---|---|---|
| Demographic | Living situation | Q: Do you live with anyone else who smokes? [SYNTACTIC MATCHING] U: Yes, my husband Q: Will your husband be supportive of your quit attempt? [SENTIMENT ANALYSIS] |
Social support |
Positive sentiment
Q: It’s really great that your husband is going to assist you along the way. How do you think they may help you? |
| Quit history | Most successful/longest attempt | Q: Did you use anything to help you? U: NRT patches |
Previous experience/s with pharmacotherapy | Q: You mentioned using NRT patches in the past during your longest quit attempt. Did you experience any side effects? |
| Support | Q: Did you have anyone who helped you during any of your quit attempts? U: Quitline |
Quitline | Q: How long ago did you contact Quitline? Q: Tell me how it went? |
|
| Smoking history | Cigarettes per day + Time to first cigarette |
Q: So [Name], how many cigarettes are you smoking per day—on average? U: Response (HSI score) Less than 10 (0) 11–20 (1) 21–30 (2) Greater than 30 (3) Q: How soon after you wake up in the morning do you usually have your first cigarette of the day U: Response (HSI Score) Greater than 5 min (3) 5–30 min (2) After 30 min (1) |
End of smoking history |
HSI high dependence (combined value = 5 or 6)
HSI medium dependence (combined value = 2, 3, or 4) Q: Based on how many cigarettes you are currently smoking and how soon after waking you have a cigarette, I’m thinking you would benefit from using a combination of a NRT patch and oral NRT, or a stop smoking medication. We’ll cover this a bit later. HSI low dependence (combined value = 0 or 1) Q: Based on how many cigarettes you are currently smoking and how soon after waking you have a cigarette, I’m thinking you would benefit from using some form of NRT. We’ll cover this a bit later. |
Q, Quin; U, user; HSI, heaviness of smoking index; NRT, nicotine replacement therapy.
Teachable Moments and User Education
Educational opportunities were purposively programmed into the chatbot to use teachable moments and encourage informed decision-making. Teachable moments were both voluntary and involuntary for the user and included written information within the dialogue and embedded links to educational videos. For example, in response to user’s time to first cigarette response, Quin automatically says “. . . The longer this morning’s cigarette is delayed the better, as it generally makes quitting a bit easier.” Whereas other educational opportunities regarding pharmacotherapy and behavioral strategies often require consent or selection from the user. For example, before discussing pharmacotherapy options, Quin attempts to educate users about the physiology of nicotine dependence by asking “Just before we start. It’s good to know how nicotine works in our body so the products we might talk about make more sense. Can I quickly tell you about this?.” Similarly, users are given the option to learn more about the pharmacotherapy option/s they are interested in before confirming their plan to encourage informed decision-making. Furthermore, the chatbot has also been programmed to explore, detect and address common misconceptions about and previous issues/side effects relating with pharmacotherapies.
Promoting Self-reflection and Client Agency
Exploration of users’ personal behaviors, experiences, and ideas encourages a sense of agency. While Quin guides users sequentially through the dialogue, it is the user who has ultimate control over their quit plan. Following completion of each section, Quin provides a summary of the information given and asks the user to review and confirm it has understood correctly, with the option to edit if necessary.
In many instances, Quin’s dialogue prompts user to self-reflect through direct and open-ended questions. Motivations are explored and users are given the option to upload an image as a reminder, following which Quin also asks why the user chose that image and provides positive reinforcement as a result of syntactic matching. For example, if an utterance relating to family or friends is detected, Quin responds with “Staying strong for other people is commendable.” Enquiries into previous experience with pharmacotherapy allows the user to consider any side effects/issues they may have had, and what they like or didn’t like about the product/s, before indicating if they might want to try that product again. This discussion also prioritizes pharmacotherapy the user has previously indicated they had side effects/issues as a means of addressing misconceptions or providing ways to manage or prevent side effects. Users are also asked to consider personal triggers leading to relapse. Quin then provides information and examples of management strategies for these cues/triggers, and asks the user to think about what strategy would work best for them. For example, “How do you think you might manage avoiding cigarettes without your coffee or tea?.” In the case of a user living with someone who smokes, Quin guides the user to reflect upon what this person could do to better support them when quitting (eg, smoke-free areas in the home) and encourages them to discuss these ideas with them.
Discussion
The multifaceted and iterative translation of practical smoking cessation counseling and behavior change strategies into a mobile app chatbot represents the science and art of health promotion. Through a combination of analyses of clinical data alongside oversight from a multidisciplinary team, the successful development of Quin is a step forward in expanding the reach of tailored, evidence-based, in-pocket support for people who want to quit smoking.
This is the first paper to provide a transparent description of the translation of qualitative evidence into the design and development of a prototype smoking cessation chatbot. Mobile health (mHealth) is an emerging area of research which has yet to attain the methodological maturity seen in, for example, randomized clinical drug trials. The vast majority of mHealth research focuses on clinical validation and there is a distinct lack of upstream research regarding the development of such technologies, which may ultimately influence the downstream results of clinical validation. Previous research has described the design, training, and testing of a MI chatbot,26 but employed a “top-down” design approach whereby the chatbot design was driven by a behavior change model alone rather than real-world consumer and stakeholder experiences. To our knowledge, this “bottom-up” approach to dialogue design using counseling transcripts has been used by one other chatbot for genetic counseling.41 Additionally, a user-centered approach has been employed in the design of other mobile health interventions for smoking cessation, but qualitative investigations were limited from the outset of the design process44 or not undertaken until after the top-down approach was used.45 The qualitative foundations of Quin allow for greater insight into the smoking cessation counseling relationship, structure and style, inherently underpinned by behavior change models, and enhances the conversational ability of the technology by drawing upon practical examples of smoking cessation counseling dialogue.
Quin’s accessibility is a key advantage, yet its purpose is not to replace existing counseling services but rather to complement, support, and potentially integrate into primary care. The more effective, and thus preferred, method of telephone-based services is on a proactive basis,13 in that the service initiates client contact following referral. However, the time between referral and initial contact can vary depending on the capacity of the service, and client motivation to quit can potentially wane during this time. Quin can act as an intermediary support to initiate a conversation about quitting, thus sustaining motivation until professional support becomes available, or as an on-demand assistant outside of service hours. Furthermore, from an interoperability perspective, information collected by Quin could be shared between telephone-counseling services and primary care (eg, General Practitioners) to monitor progress and improve service efficiency.
Quin, as an anonymous digital coach, may also be preferred by people who want to quit smoking but are reluctant to access counseling due to feelings of stigma, guilt, and shame.29 Previous research has found non-completion of Quitline programs was associated with cognitive barriers and discomfort with the telephone-counseling experience.46 The advantage of Quin, and conversational AI in general, is that the user can rely on it being neutral and not forming any personal opinions, and hence may be an attractive option for people hesitant to engage with human-delivered support services. Encouragingly, recent qualitative evidence found users attributed human-like characteristics and behaviors to an app-based smoking cessation chatbot, which fostered a sense of accountability despite knowing it was automated technology.47 Users also reported a greater sense of support from the chatbot compared to that from family and friends, but also expressed a need for tailored interactions unique to situations47 which was a key objective of Quin’s conversation design.
When considering appropriate AI systems to support smoking cessation, we must prioritize the inherent complexity of health behavior change. AI is challenged in this aspect as multiple intersecting biological, social, and environmental determinants contribute to individuals’ health,48 and as such we must acknowledge the limits of this technology. A predictive model alone, such as a machine learning algorithm, may be limited in the degree of personalization and tailoring to the user in health behavior applications. In contrast to this, the syntactic matching and template response system used in Quin allows developers a greater level of control over the conversation pathway and chatbot responses, tailored to the user. However, it is not without its limitations. This system requires comprehensive coding of all potential utterances to ensure ease and accuracy of syntactic matching, the counseling conversation needs to follow a defined structure, and responses will need to be reviewed and updated on a regular basis to ensure they are consistent with current health advice. For example, we have observed changes in the use of e-cigarettes as both a potential smoking cessation aid and as a public health issue since the outset of Quin’s development. While the foundations of the Quin prototype are based on counseling conversations from 2019, the benefit of this technology is that the content is easily modifiable and adaptable to new information. Future work can therefore seek to make iterations to the chatbot based on new evidence (ie, vaping cessation advice) or tailor to specific demographic groups. While in its infancy we expect to find gaps in information, but with increasing amounts of testing from a diverse range of people Quin will gain more knowledge and become more comprehensive and fluid in its interactions.
This study is part of a multiphase program of co-design research. While there is wide variability in co-design methods,49 our approach is based on a three-stage model that seeks to promote digital inclusion50: (1) Understanding and defining user and stakeholder needs and experiences; (2) Ideas and prototype; and (3) Iterative testing and delivery. Earlier qualitative studies completed as part of stage 1 determined features liked and disliked by users from a sample of reviews of currently available mCessation applications,39 and conversation themes, topics and client questions within Quitline calls.40 Purposive sampling of Quitline calls by demographic characteristics rather than by call type may be a limitation of Quin’s development in that more support calls would improve data saturation. However, given the high degree of personalization required for smoking cessation counseling, the broader analysis of themes, topics, and basic structure of a support call provides a good foundation for further modification and improvements as we move forward in our program of research. The next phase (ie, stage 3) of Quin’s development is to test it among focus groups of smoking cessation clinicians and people who smoke. Feedback will inform iterative changes to produce a mature prototype for clinical testing in a single-arm intervention trial, followed by a randomized controlled trial (stage 3). Prior to clinical testing the mature prototype dialogue and content will be assessed to determine level of adherence to clinical guidelines, and readability of chatbot responses. Additionally, MI principles and techniques will be strengthened by identifying practical examples from the Quitline sample and assessing the fidelity of the mature prototype prior to trial. The co-design approach allows us to better understand priorities and experiences of consumers and stakeholders through meaningful engagement, and opens a dialogue for collaboration and sharing of ideas. In doing so it assists in ensuring Quin is appropriate and acceptable to the target population, which in turn may improve its effectiveness.
Conclusion
Grounded in real-world smoking cessation counseling interactions and built using a complex chatbot framework, Quin is a prototype mHealth chatbot designed to provide in-pocket access to personalized smoking cessation advice. Chatbot interactions have been designed to promote educational opportunities, informed decision-making, user self-reflection, and self-agency. While the potential of Quin to provide meaningful and effective smoking cessation assistance is yet to be tested, its development represents a novel step toward accessible tailored support and future integration of mHealth interventions into healthcare services.
Supplementary Material
Acknowledgments
We would like to thank vacation students Tristan Hurree and Pranavie Vijayakumar for their assistance during the initial phases of chatbot development. We would also like to acknowledge Quitline (Queensland Health) for their assistance in providing the data used in this study. This was the extent of their contribution to this study, and they had no role in study design, data analysis, data interpretation, manuscript writing, or decision to submit.
Contributor Information
Hollie Bendotti, Thoracic Research Centre, Faculty of Medicine, University of Queensland, Chermside, Queensland, Australia; The Australian e-Health Research Centre, Commonwealth Scientific and Industrial Research Organisation, Herston, Queensland, Australia.
David Ireland, The Australian e-Health Research Centre, Commonwealth Scientific and Industrial Research Organisation, Herston, Queensland, Australia.
Sheleigh Lawler, School of Public Health, Faculty of Medicine, University of Queensland, Herston, Queensland, Australia.
David Oates, The Australian e-Health Research Centre, Commonwealth Scientific and Industrial Research Organisation, Herston, Queensland, Australia.
Coral Gartner, NHMRC Centre of Research Excellence on Achieving the Tobacco Endgame, School of Public Health, University of Queensland, Herston, Queensland, Australia.
Henry M Marshall, Thoracic Research Centre, Faculty of Medicine, University of Queensland, Chermside, Queensland, Australia; Department of Thoracic Medicine, The Prince Charles Hospital, Metro North Hospital and Health Service, Chermside, Queensland, Australia.
Funding
This work was supported by an Investigator grant (GNT1178331) from the National Health and Medical Research Council (NHMRC) awarded to HM. HB receives a top-up scholarship from the Commonwealth Scientific and Industrial Research Organisation, and funding from a New Investigator grant from The Prince Charles Hospital Foundation (NI2021-31). CG receives funding from NHMRC grants (GNT1198301, GNT2019252) and is supported by an ARC Future Fellowship (FT220100186).
Declaration of Interests
HM is the Convenor of the Tobacco Control Specialist Interest Group, Thoracic Society of Australia and New Zealand, and a member of the Cancer Council Victoria Quit Centre Advisory Committee. CG is the President of Society for Research on Nicotine and Tobacco Oceania Chapter.
Author Contributions
Hollie Bendotti (Conceptualization [Equal], Data curation [Lead], Formal analysis [Lead], Investigation [Equal], Methodology [Equal], Project administration [Lead], Visualization [Equal], Writing—original draft [Lead], Writing—review & editing [Supporting]), David Ireland (Conceptualization [Equal], Methodology [Equal], Resources [Lead], Software [Lead], Supervision [Equal], Writing—review & editing [Equal]), Sheleigh Lawler (Conceptualization [Equal], Formal analysis [Equal], Investigation [Equal], Methodology [Equal], Supervision [Equal], Visualization [Equal], Writing—review & editing [Equal]), David Oates (Methodology [Equal], Software [Equal]), Coral Gartner (Conceptualization [Equal], Investigation [Supporting], Methodology [Equal], Supervision [Equal], Writing—review & editing [Equal]), and Henry Marshall (Conceptualization [Equal], Formal analysis [Equal], Funding acquisition [Lead], Investigation [Equal], Methodology [Equal], Supervision [Equal], Writing—review & editing [Equal])
Data Availability
Data sharing is not possible due to ethical considerations and agreements with the data custodian. The qualitative data is of a personal/sensitive nature and access to transcripts is only limited to the study team on approved servers.
References
- 1. Steinberg MB, Schmelzer AC, Richardson DL, Foulds J.. The case for treating tobacco dependence as a chronic disease. Ann Intern Med. 2008;148(7):554–556. [DOI] [PubMed] [Google Scholar]
- 2. Hughes JR, Keely J, Naud S.. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38. [DOI] [PubMed] [Google Scholar]
- 3. Chaiton M, Diemert L, Cohen JE, et al. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open. 2016;6(6):e011045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T.. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst Rev. 2018;(5):CD000146. doi: 10.1002/14651858.CD000146.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Howes S, Hartmann-Boyce J, Livingstone-Banks J, Hong B, Lindson N.. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2020;(4):CD000031. doi: 10.1002/14651858.CD000031.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hartmann-Boyce J, Hong B, Livingstone-Banks J, Wheat H, Fanshawe TR.. Additional behavioural support as an adjunct to pharmacotherapy for smoking cessation. Cochrane Database Syst Rev. 2019;6(6):CD009670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Roddy E, Antoniak M, Britton J, Molyneux A, Lewis S.. Barriers and motivators to gaining access to smoking cessation services amongst deprived smokers – a qualitative study. BMC Health Serv Res. 2006;6(1):147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tall JA, Brew BK, Saurman E, Jones TC.. Implementing an anti-smoking program in rural-remote communities: challenges and strategies. Rural Remote Health. 2015;15(4):3516. [PubMed] [Google Scholar]
- 9. Hutcheson TD, Greiner KA, Ellerbeck EF, et al. Understanding smoking cessation in rural communities. J Rural Health. 2008;24(2):116–124. [DOI] [PubMed] [Google Scholar]
- 10. Smith AL, Chapman S, Dunlop SM.. What do we know about unassisted smoking cessation in Australia? A systematic review, 2005-2012. Tob Control. 2015;24(1):18–27. [DOI] [PubMed] [Google Scholar]
- 11. Soulakova JN, Crockett LJ.. Unassisted quitting and smoking cessation methods used in the United States: analyses of 2010-2011 tobacco use supplement to the current population survey data. Nicotine Tob Res. 2017;20(1):30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Strecher VJ, Kreuter M, Den Boer DJ, et al. The effects of computer-tailored smoking cessation messages in family practice settings. J Fam Pract. 1994;39(3):262–270. [PubMed] [Google Scholar]
- 13. Matkin W, Ordóñez-Mena JM, Hartmann-Boyce J.. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2019;(5):CD002850. doi: 10.1002/14651858.CD002850.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Taylor GMJ, Dalili MN, Semwal M, et al. Internet-based interventions for smoking cessation. Cochrane Database Syst Rev. 2017;(9):CD007078. doi: 10.1002/14651858.CD007078.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y.. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2016;(4):CD006611. doi: 10.1002/14651858.CD006611.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Barnett A, Ding H, Hay KE, et al. The effectiveness of smartphone applications to aid smoking cessation: a meta-analysis. Clinical eHealth. 2020;3:69–81. doi: 10.1016/j.ceh.2020.09.001 [DOI] [Google Scholar]
- 17. Abroms LC, Lee Westmaas J, Bontemps-Jones J, Ramani R, Mellerson J.. A content analysis of popular smartphone apps for smoking cessation. Am J Prev Med. 2013;45(6):732–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Buller DB, Borland R, Bettinghaus EP, Shane JH, Zimmerman DE.. Randomized trial of a smartphone mobile application compared to text messaging to support smoking cessation. Telemed J E Health. 2014;20(3):206–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chen YF, Madan J, Welton N, et al. Effectiveness and cost-effectiveness of computer and other electronic aids for smoking cessation: a systematic review and network meta-analysis. Health Technol Assess. 2012;16(38):1–205, iii. [DOI] [PubMed] [Google Scholar]
- 20. Australian Institute of Health and Welfare. National Drug Strategy Household Survey 2019. AIHW. Canberra: AIHW; 2020. https://www.aihw.gov.au/reports/illicit-use-of-drugs/national-drug-strategy-household-survey-2019/contents/table-of-contentsAccessed October 14, 2020. [Google Scholar]
- 21. Australian Institute of Health and Welfare. National Drug Strategy Household Survey 2019. In: AIHW, ed. Tobacco Smoking Chapter: Supplementary Data Tables, Canberra: AIHW; 2019. [Google Scholar]
- 22. Whittaker R, McRobbie H, Bullen C, et al. Mobile phone text messaging and app-based interventions for smoking cessation. Cochrane Database Syst Rev. 2019;(10):CD006611. doi: 10.1002/14651858.CD006611.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thornton L, Quinn C, Birrell L, et al. Free smoking cessation mobile apps available in Australia: a quality review and content analysis. Aust N Z J Public Health. 2017;41(6):625–630. [DOI] [PubMed] [Google Scholar]
- 24. Baskerville NB, Struik LL, Dash D.. Crush the crave: development and formative evaluation of a smartphone app for smoking cessation. JMIR Mhealth Uhealth. 2018;6(3):e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hoeppner BB, Hoeppner SS, Kelly L, Schick M, Kelly JF.. Smiling instead of smoking: development of a positive psychology smoking cessation smartphone app for non-daily smokers. Int J Behav Med. 2017;24(5):683–693. [DOI] [PubMed] [Google Scholar]
- 26. Almusharraf F, Rose J, Selby P.. Engaging unmotivated smokers to move toward quitting: design of motivational interviewing–based chatbot through iterative interactions. J Med Internet Res. 2020;22(11):e20251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mohr DC, Cuijpers P, Lehman K.. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J Med Internet Res. 2011;13(1):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. World Health Organization. Geneva, Switzerland: Training for Tobacco Quit Line Counsellors: Telephone Counselling. World Health Organization. Published 2014. https://www.who.int/publications/i/item/training-for-tobacco-quit-line-counsellors-telephone-counselling. Accessed June 9, 2021. [Google Scholar]
- 29. Boland VC, Mattick RP, McRobbie H, Siahpush M, Courtney RJ.. “I’m not strong enough; I’m not good enough. I can’t do this, I’m failing”: a qualitative study of low-socioeconomic status smokers’ experiences with accessing cessation support and the role for alternative technology-based support. Int J Equity Health. 2017;16(1):196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ho A, Hancock J, Miner AS.. Psychological, relational, and emotional effects of self-disclosure after conversations with a chatbot. J Commun. 2018;68(4):712–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. World Health Organization. Using AI to quit tobacco. Published 2021. https://www.who.int/news-room/spotlight/using-ai-to-quit-tobacco. Accessed June 9, 2021.
- 32. Solutions4Health. Quit with Bella. Solutions4Health. Published 2018. https://www.quitwithbella.com/. Accessed 2022.
- 33. Alex Therapeutics AB. Alex. Alex Therapeutics AB. Published 2021. https://www.alexquitsmoking.com/. Accessed 2022.
- 34. Whittaker R, Dobson R, Garner K.. Chatbots for smoking cessation: scoping review. J Med Internet Res. 2022;24(9):e35556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. He L, Balaji D, Wiers RW, Antheunis ML, Krahmer E.. Effectiveness and acceptability of conversational agents for smoking cessation: a systematic review and meta-analysis. Nicotine Tob Res. 2022;25(7):ntac281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bricker JB, Mull KE, Kientz JA, et al. Randomized, controlled pilot trial of a smartphone app for smoking cessation using acceptance and commitment therapy. Drug Alcohol Depend. 2014;143:87–94. doi: 10.1016/j.drugalcdep.2014.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Perski O, Crane D, Beard E, Brown J.. Does the addition of a supportive chatbot promote user engagement with a smoking cessation app? An experimental study. Digit Health. 2019;5:2055207619880676. doi: 10.1177/2055207619880676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. BinDhim NF, McGeechan K, Trevena L.. Smartphone Smoking Cessation Application (SSC App) trial: a multicountry double-blind automated randomised controlled trial of a smoking cessation decision-aid “app”. BMJ Open. 2018;8(1):e017105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bendotti H, Lawler S, Ireland D, et al. What do people want in a smoking cessation app? An analysis of user reviews and app quality. Nicotine Tob Res. 2022;24(2):169–177. [DOI] [PubMed] [Google Scholar]
- 40. Bendotti H, Lawler S, Gartner C, Ireland D, Marshall HM.. Smoking cessation counseling in practice: a qualitative analysis of Quitline conversations in Queensland, Australia. Health Educ Behav. 2023: doi: 10.1177/10901981231206068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ireland D, Bradford D, Szepe E, et al. Introducing Edna: a trainee chatbot designed to support communication about additional (secondary) genomic findings. Patient Educ Couns. 2021;104(4):739–749. [DOI] [PubMed] [Google Scholar]
- 42. Ireland D, Atay C, Liddle J, et al. Hello harlie: enabling speech monitoring through chat-bot conversations. Stud Health Technol Inform. 2016;227:55–60. [PubMed] [Google Scholar]
- 43. Askitis N, Sinha R.. Engineering scalable, cache and space efficient tries for strings. VLDB J. 2010;19(5):633–660. [Google Scholar]
- 44. Vilardaga R, Rizo J, Zeng E, et al. User-centered design of learn to quit, a smoking cessation smartphone app for people with serious mental illness. JMIR Serious Games. 2018;6(1):e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Klein P, Lawn S, Tsourtos G, van Agteren J.. Tailoring of a smartphone smoking cessation app (Kickit) for serious mental illness populations: qualitative study. JMIR Hum Factors. 2019;6(3):e14023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Solomon LJ, Hughes JR, Livingston A, et al. Cognitive barriers to calling a smoking quitline. Nicotine Tob Res. 2009;11(11):1339–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Alphonse A, Stewart K, Brown J, Perski O.. Exploring users’ experiences with a quick-response chatbot within a popular smoking cessation smartphone app: semistructured interview study. JMIR Form Res. 2022;6(7):e36869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Marmot M, Wilkinson R.. Social Determinants of Health. Oxford: Oxford University Press 2nd ed; 2005. [Google Scholar]
- 49. Slattery P, Saeri AK, Bragge P.. Research co-design in health: a rapid overview of reviews. Health Res Policy Syst. 2020;18(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Goods Things Foundation NHS. How to Co-Design digital inclusion in Health: a pathfinder model. United Kingdom. 2019. Publisher Good Things Foundation NHS. https://digital-health-lab.org/codesign-in-health. Accessed June 9, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not possible due to ethical considerations and agreements with the data custodian. The qualitative data is of a personal/sensitive nature and access to transcripts is only limited to the study team on approved servers.


