Abstract
Objective.
To identify changes in opioid prescribing across a diverse array of medical specialties after the release of the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain.
Design.
Interrupted time-series analysis of data from a commercial prescribing database.
Subjects.
De-identified recipients of opioid prescriptions dispensed at U.S. retail pharmacies between 2015 and 2019.
Methods.
Opioid dispensing data were obtained from the IQVIA Longitudinal Prescription (LRx) database, representing more than 800 million opioid prescriptions. Monthly dispensing rates, dosage in morphine milligram equivalents (MME), and mean prescription duration were calculated across 29 medical specialties. Changes in dispensing after the release of the 2016 CDC Guideline were assessed through interrupted time-series analysis.
Results.
Declining trends in opioid dispensing accelerated in 24 of 29 specialty groups after the release of the CDC Guideline (P < 0.05 for 15 groups). Decreases were greatest among family medicine clinicians, where declines accelerated by 4.4 prescriptions per month per 100,000 persons (P = 0.005), and surgeons, where declines accelerated by 3.6 prescriptions per month per 100,000 (P = 0.003).
Conclusions.
These results illustrate that clinicians likely to provide primary care exhibited the greatest decreases in opioid dispensing. However, specialties outside the scope of the CDC Guideline (e.g., surgery) also exhibited accelerated decreases in prescribing. These declines illustrate that specialties beyond primary care could have interest in evaluating opioid prescribing practices, supporting the importance of specialty-specific guidance that balances the individualized risks and benefits of opioids and the role of non-opioid treatments.
Keywords: Opioid, Drug Prescription, Specialization, Physicians’ Practice Patterns, Interrupted Time-Series Analysis, Practice Guidelines
Introduction
Since 1999, almost 500,000 deaths in the United States have resulted from opioid overdoses [1]. Although prescription opioids can be beneficial, their use can also present serious risks, including overdose and opioid use disorder. In 2019, more than 25% of opioid overdose deaths involved a prescription opioid [1].
Opioid prescribing practices have evolved in recent history. Dispensed opioid prescriptions in the United States increased from 72.4 per 100 persons in 2006 to 81.2 in 2010, when mean morphine milligram equivalents (MME) per capita were four times higher than in 1999 [2]. This period coincided with increases in rates of opioid overdose deaths [1], emergency department visits related to opioid use [3], and opioid use disorder [4].
To provide recommendations for pain management for adults in primary care settings, the U.S. Centers for Disease Control and Prevention (CDC) released in 2016 its Guideline for Prescribing Opioids for Chronic Pain (the CDC Guideline) [5]. The CDC Guideline provides evidence-based recommendations for the use of opioids in treating chronic pain in primary care settings (excluding cancer and palliative care) for patients 18 years of age and older and aims to improve patient–clinician communication about opioid therapy, improve the safety and effectiveness of pain management, and reduce the risks associated with long-term opioid use.
Although opioid prescribing began to decline in 2012 [2], the release of the CDC Guideline has been associated with accelerated temporal declines in opioid prescribing at a national level [6]. During 2012–2016, dispensed opioid prescriptions per 100,000 persons declined at a rate of 23 fewer prescriptions per month; after the release of the CDC Guideline, prescribing declined by 57 fewer prescriptions per month, a statistically significant acceleration [6]. Although this observation might have been related to secular trends in prescribing, accelerated declines in opioid prescribing exceeded changes in prescribing of other medications (e.g., benzodiazepines) during the same time period [6]. However, substantial variation exists in opioid prescribing by medical specialty [7]. During 2016–2017, the mean number of prescriptions dispensed was 215 per prescriber but ranged as high as 1,314 prescriptions per pain medicine specialist and as low as 14 prescriptions per pediatrician [7].
To date, the extent of prescribing changes among primary care practitioners (the intended audience of the CDC Guideline) and medical specialists after the release of the CDC Guideline has not been examined. In the assessment of policy change interventions, interrupted time-series analysis offers one of the most robust and commonly used statistical approaches for evaluating temporal changes in aggregate data [8]. Using interrupted time-series analysis, the present study aims to assess changes in opioid prescribing after the release of the CDC Guideline among medical disciplines likely to practice primary care, as well as among a variety of non–primary care specialties.
Methods
Study Sample
Opioid dispensing data from the IQVIA Longitudinal Prescription (LRx) database were available for 2015 through 2019. The LRx database is comprised of de-identified transaction-level prescription data capturing 92% of dispensed retail pharmacy prescriptions in the United States (representing more than 800 million opioid prescriptions in the time period examined). All prescriptions from clinicians that could not be classified by practice setting or specialty (e.g., nurse practitioners and physician assistants) were excluded from this analysis (detailed in Supplementary Data Table S1), as were all prescriptions for buprenorphine-containing and propoxyphene products.
Measures
Prescriber specialty was classified into 29 specialty groups based on similarity of practice (detailed in Supplementary Data Table S1). Prescriptions were aggregated by specialty and calendar month to define five measures of opioid dispensing. Total MME for each prescription was calculated as the product of prescription quantity (doses), strength/concentration per dose prescribed, and MME conversion factor [9]; daily MME was calculated as total MME divided by prescription duration (in days). High-dosage prescriptions were defined as any prescription for which daily MME exceeded 90 [6]. Total and high-dosage dispensing rates were calculated as the number of prescriptions dispensed each month (standardized to a 30-day month length) divided by monthly U.S. population (per 100,000, estimated from the U.S. Census Bureau [10]), and mean daily MME and prescription durations were calculated by specialty and month dispensed.
Statistical Analysis
Changes in opioid dispensing after publication of the CDC Guideline in March 2016 were assessed through interrupted time-series analysis with segmented regressions [11], a robust quasi-experimental design for evaluating the temporal impact of interventions without a control group. The pre-Guideline period was defined as January 2015 to February 2016, and the post-Guideline period was defined as March 2016 to December 2019. An interim period was not included, as available data suggested that post-Guideline declines have persisted for several years [6]. Ordinary least-squares regression was used to fit aggregated outcome measures by month, with additional terms for changes in slope (denoted as βG) and intercept after the release of the CDC Guideline (March 2016 to December 2019). Changes in level for each outcome (denoted as Δβ0) were calculated as the absolute difference in intercept for the post-Guideline period compared with the pre-Guideline period. Prais-Winsten estimation was used to account for serial autocorrelation. Data preparation and aggregation were performed in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA), and statistical analyses were performed in R version 3.6 (R Core Team, Vienna, Austria). This study was reviewed by the CDC and determined to meet the definition of research as defined in U.S. Department of Health and Human Services (HHS) regulation 45 Code of Federal Regulations (CFR) 46.102(l) but did not involve human subjects as defined in 45 CFR 46.103(e). Thus, institutional review board review was not required.
Results
Population Characteristics
From 2015 to 2019, approximately 810 million opioid prescriptions in this database were dispensed to more than 38 million patients each year. After exclusion of prescriptions from clinicians who could not be classified by practice setting or specialty (e.g., nurse practitioners and physician assistants), 654 million dispensed prescriptions remained for analysis (see Supplementary Data Figure S1). A plurality of dispensed prescriptions were provided by clinicians in the family medicine category (20–23% of prescriptions each year), followed by internal medicine, surgery, and pain medicine (Table 1).
Table 1.
Patient characteristics and opioid prescriptions dispensed by clinician specialty—United States, 2015–2019
| 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|
|
| |||||
| Unique patients, n | 51,839,740 | 50,396,992 | 47,194,550 | 42,167,675 | 38,785,488 |
| Median patient age, years (IQR) | 50 (34–63) | 51(35–64) | 52 (36–65) | 53 (37–66) | 54 (38–67) |
| Prescriptions dispensed by clinician specialty,* n (% of year) | |||||
| Addiction medicine | 102,028 (0.1) | 78,116 (0) | 64,049 (0) | 54,340 (0) | 44,697 (0) |
| Allergy and immunology | 61,265 (0) | 54,803 (0) | 45,401 (0) | 38,519 (0) | 29,817(0) |
| Anesthesiology | 4,897,660 (2.6) | 4,878,812 (2.7) | 4,833,182 (2.9) | 4,703,532 (3.2) | 4,515,705 (3.4) |
| Cardiology | 650,224 (0.4) | 574,224 (0.3) | 490,889 (0.3) | 393,354 (0.3) | 324,330 (0.2) |
| Dentist | 11,006,821 (5.9) | 10,509,265 (5.9) | 9,591,642 (5.8) | 8,071,631 (5.5) | 6,912,110 (5.2) |
| Emergency medicine | 9,941,826 (5.4) | 8,662,408 (4.9) | 7,009,580 (4.2) | 5,339,165 (3.6) | 4,621,728 (3.5) |
| Endocrinology | 181,765 (0.1) | 156,568 (0.1) | 127,774 (0.1) | 101,395 (0.1) | 80,045 (0.1) |
| Family medicine | 43,187,701 (23.3) | 40,140,352 (22.6) | 36,378,414 (22) | 31,124,681 (21.2) | 27,193,125 (20.3) |
| Gastroenterology/hepatology | 481,785 (0.3) | 427,948 (0.2) | 366,848 (0.2) | 316,932 (0.2) | 271,648 (0.2) |
| Infectious disease | 283,830 (0.2) | 248,764 (0.1) | 213,224 (0.1) | 177,130 (0.1) | 153,016 (0.1) |
| Internal medicine | 26,172,276 (14.1) | 24,344,359 (13.7) | 22,075,183 (13.3) | 19,040,633 (13) | 16,886,394 (12.6) |
| Nephrology | 492,609 (0.3) | 438,449 (0.2) | 384,979 (0.2) | 310,639 (0.2) | 256,108 (0.2) |
| Neurology | 26,835 (0) | 22,021 (0) | 19,796 (0) | 17,867 (0) | 15,934 (0) |
| OB/GYN | 3,659,783 (2) | 3,453,439 (1.9) | 3,078,663 (1.9) | 2,671,186 (1.8) | 2,352,254 (1.8) |
| Occupational medicine | 303,899 (0.2) | 244,420 (0.1) | 195,519 (0.1) | 162,524 (0.1) | 125,450 (0.1) |
| Oncology and/or hematology | 2,508,954 (1.4) | 2,427,626 (1.4) | 2,308,691 (1.4) | 2,131,539 (1.5) | 1,992,104 (1.5) |
| Ophthalmology | 317,540 (0.2) | 296,553 (0.2) | 272,670 (0.2) | 239,229 (0.2) | 207,136 (0.2) |
| Other | 2,921,288 (1.6) | 2,713,280 (1.5) | 2,426,311 (1.5) | 2,089,162 (1.4) | 1,855,075 (1.4) |
| Pain medicine | 10,893,243 (5.9) | 11,210,359 (6.3) | 11,198,678 (6.8) | 10,684,290 (7.3) | 9,990,168 (7.5) |
| Palliative care | 183,298 (0.1) | 184,893 (0.1) | 194,245 (0.1) | 216,435 (0.1) | 234,174 (0.2) |
| Pediatric hematology/oncology | 39,280 (0) | 37,815 (0) | 36,228 (0) | 33,716 (0) | 33,376 (0) |
| Pediatric subspecialties (other) | 186,226 (0.1) | 161,269 (0.1) | 135,974 (0.1) | 106,905 (0.1) | 87,751 (0.1) |
| Pediatrics | 1,094,021 (0.6) | 987,990 (0.6) | 873,785 (0.5) | 744,626 (0.5) | 657,573 (0.5) |
| Physical medicine and rehabilitation | 6,389,513 (3.4) | 6,240,101 (3.5) | 5,941,914 (3.6) | 5,467,999 (3.7) | 5,067,217(3.8) |
| Podiatry | 1,372,353 (0.7) | 1,308,946 (0.7) | 1,191,054 (0.7) | 1,033,757 (0.7) | 949,606 (0.7) |
| Psychiatry | 405,023 (0.2) | 350,577 (0.2) | 306,935 (0.2) | 251,830 (0.2) | 208,384 (0.2) |
| Pulmonary / critical care medicine | 487,556 (0.3) | 448,233 (0.3) | 387,558 (0.2) | 309,139 (0.2) | 265,839 (0.2) |
| Rheumatology | 3,032,587(1.6) | 2,803,972 (1.6) | 2,545,385 (1.5) | 2,237,216 (1.5) | 1,971,806 (1.5) |
| Surgery | 23,783,222 (12.8) | 22,658,351 (12.7) | 20,685,321 (12.5) | 18,296,381 (12.5) | 16,810,191 (12.5) |
IQR = interquartile range.
Clinician specialty groups are detailed in Supplementary Data Table S1.
Pre-Guideline Prescribing Trends
Between January 2015 and February 2016 (before publication of the CDC Guideline), total monthly dispensing exhibited declining trends in 25 of 29 specialties (P < 0.05 for 15 of 25; Supplementary Data Figure S2), largely mirrored by trends in high-dosage dispensing (24 of 29, P < 0.05 for 17 of 24), total monthly MME (25 of 29, P < 0.05 for 15 of 25), and mean daily MME (21 of 29, P < 0.05 for 11 of 21), illustrated for all outcomes in Figure 2. Initial declines in total monthly dispensing were greatest in family medicine (5.4 fewer prescriptions per month per 100,000) and internal medicine (2.9 fewer prescriptions per month per 100,000), and these trends were paralleled by decreases in other measures of dispensing (Figure 2).
Figure 2.
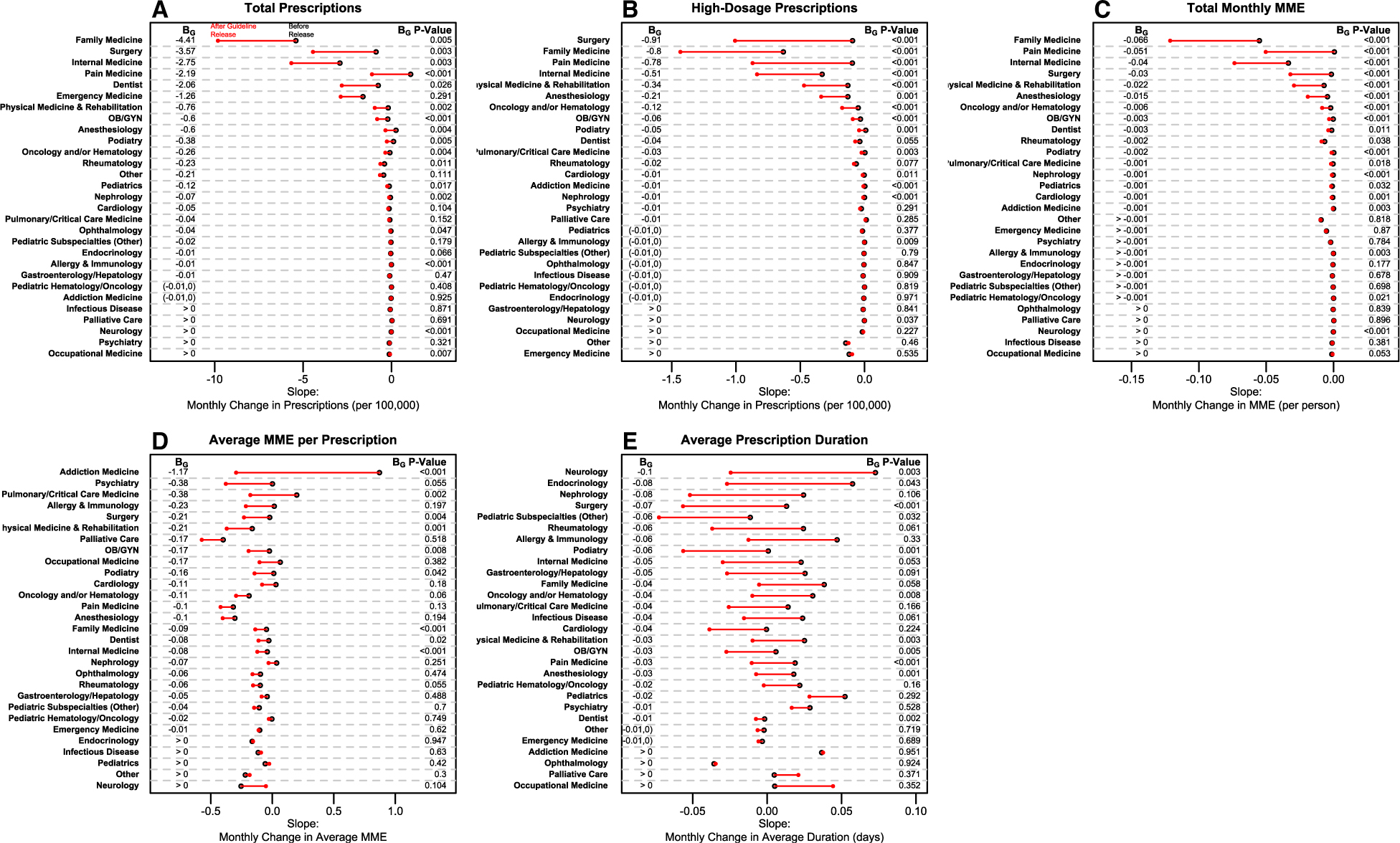
Trends in opioid prescription dispensing characteristics by provider specialty—United States, 2015–2019. Each panel represents, for 29 provider specialties, the slope of modeled trendlines in opioid dispensing characteristics before the release (black, open circles) and after the release (red, solid circles) of the CDC Guideline, sorted by greatest declines after release. Faster declines after the release of the CDC Guideline occurred in specialties where red, solid circles appear to the left of black, open circles. Solid lines illustrate the change in slope after the release of the CDC Guideline (BG), which are reported on the left of each panel; values listed as “(−0.01, 0)” indicate slope estimates in the range of (−0.01, 0). P values for each specialty’s BG are reported on the right of each panel. Panel A illustrates monthly changes in total opioid prescriptions dispensed per 100,000 population. Panel B illustrates monthly changes in high-dose opioid prescriptions dispensed per 100,000 population. Panel C illustrates monthly changes in total MME dispensed per 1 population. Panel D represents monthly changes in mean MME per prescription dispensed. Panel E represents monthly changes in mean duration of dispensed prescriptions as measured in days. Clinician specialty groups are detailed in Supplementary Data Table S1.
Post-Guideline Prescribing Trends
Initial trends in total dispensing rates declined faster after the release of the CDC Guideline in 24 of 29 specialties (P < 0.05 for 15 of 24). Figure 1 illustrates trends in total dispensing, high-dose dispensing, and total monthly MME for the four specialties in which declines accelerated most after the release of the CDC Guideline. Decreases accelerated most in family medicine (−4.41 prescriptions per month per 100,000; P = 0.005), surgery (−3.57 prescriptions per month per 100,000; P = 0.003), and internal medicine (−2.75 prescriptions per month per 100,000; P = 0.003). Additional notable changes were observed in pain medicine, where declining trends in high-dosage dispensing (−0.78 prescriptions per month per 100,000; P < 0.001) and total MME (−0.05 MME per month; P < 0.001) accelerated. Slopes and changes in slope results for all five outcomes are illustrated in Figure 2 for each specialty. The greatest declines after the release of the CDC Guideline in average MME per prescription were observed in addiction medicine (−1.17 MME per prescription per month, P < 0.001), and the greatest declines in average prescription duration were observed in neurology (−0.10 days per month, P = 0.003).
Figure 1.
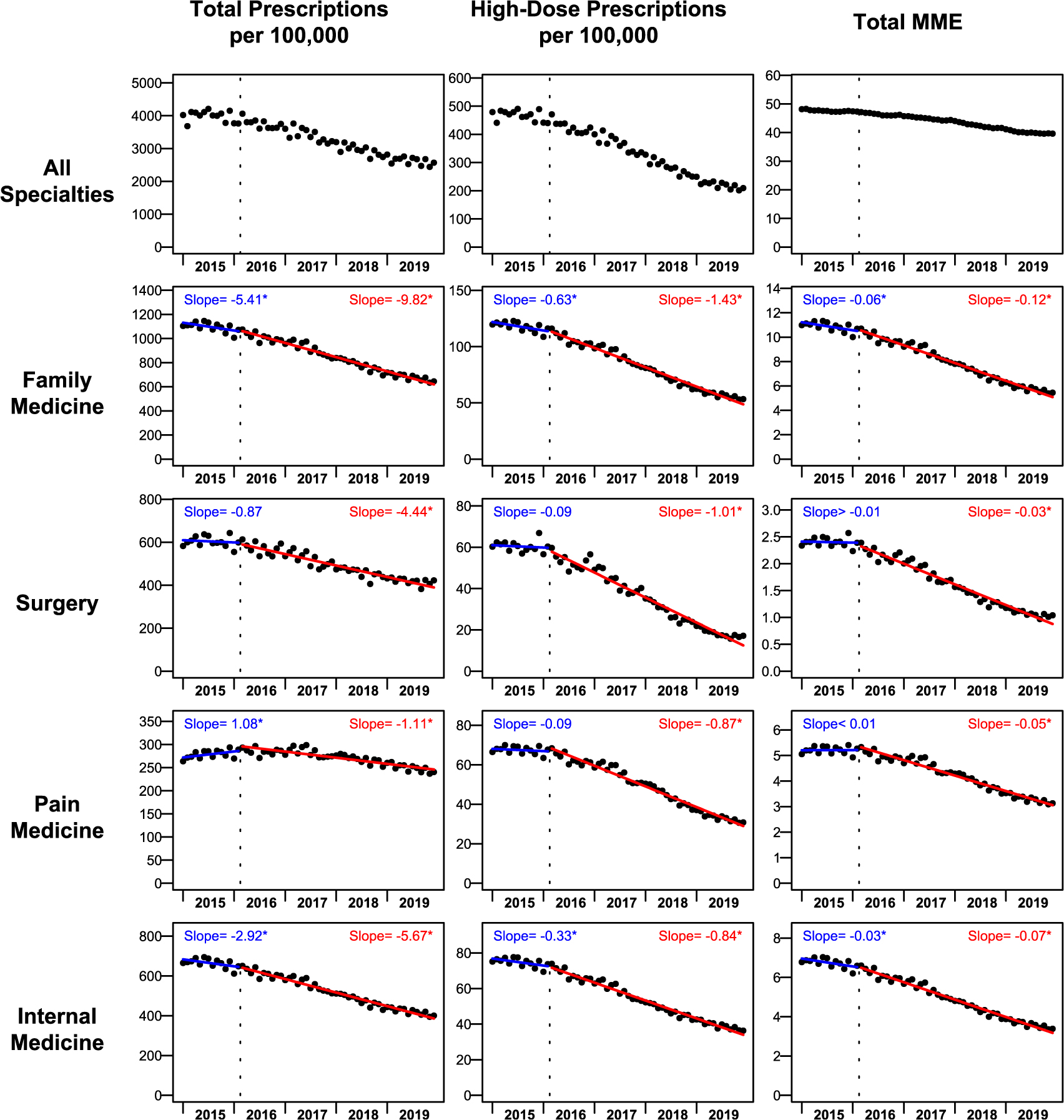
Total monthly opioid prescriptions dispensed per 100,000, high-dose prescriptions dispensed per 100,000, and total monthly MME dispensed per person by clinician specialty—United States, 2015–2019. Monthly trends in three characteristics of opioid dispensing (number of prescriptions, number of high-dose prescriptions, and total MME) are illustrated across all clinician specialties (top row) and for the four specialties (lower four rows) in which dispensing changed most after the release of the CDC Guideline in March 2016 (denoted by the dotted line). Each point represents prescriptions dispensed for one calendar month, standardized to a 30-day month length. Numbers of monthly prescriptions dispensed (left column) and high-dose prescriptions dispensed (middle column) are presented per 100,000 population; total monthly MME dispensed (right column) is presented per 1 population. Modeled monthly trendlines are depicted for before the release (blue lines) and after the release (red lines) of the CDC Guideline, accompanied by slopes estimated for each trendline. Asterisks (*) indicate statistically significant (P < 0.05) coefficients for slope (before release, blue) or change in slope (after release, red) for each statistic reported. Clinician specialty groups are detailed in Supplementary Data Table S1.
Small but significant increases after the release of the CDC Guideline were observed in occupational medicine for total prescriptions per 100,000 (0.04 more prescriptions per month per 100,000, P = 0.007) and in neurology for high-dosage prescriptions (0.001 more prescriptions per month per 100,000, P = 0.037) and for total MME (0.001 more MME per month, P < 0.001) (Figure 2).
In addition to changes in monthly trends after the release of the CDC Guideline (changes in slope), changes in the level of prescribing outcomes (changes in intercept) after the release of the CDC Guideline are presented in Supplementary Data Table S2. Prescribing by occupational medicine specialists demonstrated the greatest overall decline across multiple outcomes after the release of the CDC Guideline: total monthly prescriptions per 100,000 (−0.89 prescriptions per 100,000, P < 0.001), total MME (−0.01 MME, P = 0.004), and average prescription duration (−0.54 days, P = 0.32).
Discussion
This analysis illustrates temporal trends in opioid dispensing among medical specialties in the periods before and after the release of the 2016 CDC Guideline [5]. Monthly dispensing rates were declining at the time of the CDC Guideline release [6], with declines observed across most medical specialties. These results demonstrate that accelerated national declines after the release of the CDC Guideline [6] were driven largely by declines in primary care specialties (i.e., family practice and internal medicine), those specifically targeted by the CDC Guideline; declines in annual opioid dispensing in these two specialties accounted for 50% of reductions across all specialties after the release of the CDC Guideline.
The present report represents the first findings of associations between the release of the CDC Guideline and changes in multiple opioid dispensing characteristics by distinct medical specialties. However, this work builds on other recent studies that have examined the impacts of the CDC Guideline. Declining national trends in opioid prescribing were shown to have accelerated after the release of the CDC Guideline, exceeding changes seen in the prescribing of other medications [6]. Among opioid-naïve patients with chronic pain, the duration of initial opioid prescriptions (which had been increasing) began decreasing after the release of the CDC Guideline [12], as did prescribing of doses of at least 50 MME per day [13]. As declines observed after the release of the CDC Guideline were similar across patients with different chronic pain indications (e.g., chronic headache and osteoarthritis), questions remain about the tailored patient-specific implementation of the CDC Guideline [14].
Additionally, the present findings indicate that specialties beyond primary care (e.g., surgery) also exhibited accelerated declines after the release of the CDC Guideline. These findings corroborate recent reports about declines in specific disciplines (such as surgery [15] and emergency medicine [16]) and expand on these findings by evaluating a wide range of specialties with unique and variable perspectives on the benefit–risk balance of opioid prescribing (such as addiction medicine, pain management, palliative care, and hematology/oncology). Collectively, these findings suggest that although the CDC Guideline was targeted specifically to primary care practitioners, clinicians in other specialties might have implemented aspects of the CDC Guideline intended for primary care settings (as the result of changes in individual prescribing or health system changes reinforcing the CDC Guideline [13]), resulting in concurrent accelerated declines. Alternatively, this could indicate that the CDC Guideline and other efforts at that time aimed at curbing excessive opioid prescribing and reducing opioid overdoses might have prompted specialists to independently reexamine their prescribing practices. This highlights the importance of specialty-specific guidance for opioid prescribing.
The analyses presented here have limitations. These data capture only prescriptions dispensed from retail pharmacies but do not capture mail-order, long-term care prescriptions, prescriptions dispensed from federally funded facilities (e.g., facilities affiliated with the Indian Health Service or Department of Veterans Affairs), or prescriptions that were written but not filled. Also excluded from this analysis were prescriptions from clinicians for whom a medical specialty could not be categorized (e.g., nurse practitioners and physician assistants), accounting for approximately 19% of dispensed opioid prescriptions. Although a majority of nurse practitioners and physician assistants practice specialties providing primary care [17, 18], they constitute a minority of all primary care practitioners [19] and might be unlikely to impact the direction of primary results observed. These data do not capture patient-level indicators, such as the clinical indications for a prescription or whether a patient took a full prescription when dispensed. In the absence of clinical indications, it is not possible to ascertain whether the reductions observed were due to decreases in non–evidence-based prescribing. Additionally, these analyses use ecological data to evaluate temporal trends; observed changes in opioid dispensing after March 2016 could be the result of a variety of factors in addition to (or separate from) the CDC Guideline, such as increased attention to opioid prescribing at the federal, state, and local levels during this period. Without a concurrent control group for comparison, this analysis cannot exclude the potential association between secular factors in prescribing trends and the results observed here. Such secular factors could include concurrent changes in opioid policies, such as increased resources funded through the 21st Century Cures Act (December 2016) and increased utilization of prescription drug monitoring programs (available in all states by April 2017). Therefore, these results should not be viewed as causal, as historical biases and other trends might have contributed to the differences observed. Finally, this study did not examine trends in non-opioid or nonpharmacological treatments for pain, and therefore it could not assess whether decreases in opioid dispensing were offset by increases in other modalities for adequate pain management.
Conclusions
These findings serve to further contextualize changes in national opioid prescribing after the release of the CDC Guideline. This analysis offers evidence that declining trends in opioid dispensing accelerated among specialties likely to provide primary care, the intended audience of the CDC Guideline. These results also suggest that specialties beyond primary care also experienced accelerated declines in opioid dispensing after the release of the CDC Guideline, underscoring the importance of specialty-specific translation materials and trainings. Clinical management of pain requires integrated care, and use of prescription opioids should be based on an individualized assessment that balances the potential risks and benefits of opioid use along with other pain treatment modalities. The CDC Guideline provides a framework to support primary care practitioners in providing optimal care.
Supplementary Material
Funding sources:
No funding sources to declare for this report.
Footnotes
Conflicts of interest and financial disclosure: All authors report no conflict of interest. No financial disclosures were reported by the authors of this paper.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
Supplementary Data
Supplementary Data may be found online at http://pain-medicine.oxfordjournals.org.
References
- 1.Hedegaard H, Miniño AM, Warner M. Drug Overdose Deaths in the United States, 1999–2019. NCHS Data Brief, No 394. Hyattsville, MD: National Center for Health Statistics; 2020. [Google Scholar]
- 2.Guy GP Jr, Zhang K, Bohm MK, et al. Vital signs: Changes in opioid prescribing in the United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017;66(26):697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC). Emergency department visits involving nonmedical use of selected prescription drugs—United States, 2004–2008. MMWR Morb Mortal Wkly Rep 2010;59(23):705–9. [PubMed] [Google Scholar]
- 4.Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003–2013. JAMA 2015;314 (14):1468–78. [DOI] [PubMed] [Google Scholar]
- 5.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep 2016;65(1):1–49. [DOI] [PubMed] [Google Scholar]
- 6.Bohnert ASB, Guy GP Jr, Losby JL. Opioid prescribing in the United States before and after the Centers for Disease Control and Prevention’s 2016 opioid guideline. Ann Intern Med 2018;169(6):367–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guy GP Jr, Zhang K. Opioid prescribing by specialty and volume in the U.S. Am J Prev Med 2018;55(5):e153–e155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jandoc R, Burden AM, Mamdani M, Levesque LE, Cadarette SM. Interrupted time series analysis in drug utilization research is increasing: Systematic review and recommendations. J Clin Epi 2015;68(8):950–6. [DOI] [PubMed] [Google Scholar]
- 9.National Center for Injury Prevention and Control. CDC Compilation of Benzodiazepines, Muscle Relaxants, Stimulants, Zolpidem, and Opioid Analgesics with Oral Morphine Milligram Equivalent Conversion Factors, 2018 Version. Atlanta, GA: Centers for Disease Control and Prevention; 2018. Available at: https://www.cdc.gov/drugoverdose/resources/data.html (accessed May 12, 2022). [Google Scholar]
- 10.U.S. Census Bureau. 2018 National and State Population Estimates (Table 1. Monthly Population Estimates for the United States: April 1, 2010 to December 1, 2019). Washington, DC: U.S. Census Bureau; 2018. Available at: http://www2.census.gov/programs-surveys/popest/tables/2010-2018/national/totals/na-est2018-01.xlsx (accessed May 12, 2022). [Google Scholar]
- 11.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27(4):299–309. [DOI] [PubMed] [Google Scholar]
- 12.Goldstick JE, Guy GP, Losby JL, et al. Changes in initial opioid prescribing practices after the 2016 release of the CDC Guideline for Prescribing Opioids for Chronic Pain. JAMA Netw Open 2021;4(7):e2116860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Togun AT, Karaca-Mandic P, Wurtz R, Jeffery MM, Beebe T. Association of 3 CDC opioid prescription guidelines for chronic pain and 2 payer pharmacy coverage changes on opioid initiation practices. J Manag Care Spec Pharm 2021;27(10):1352–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Townsend T, Cerdá M, Bohnert A, Lagisetty P, Haffajee RL. CDC guideline for opioid prescribing associated with reduced dispensing to certain patients with chronic pain. Health Aff (Millwood) 2021;40(11):1766–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sutherland TN, Wunsch H, Pinto R, et al. Association of the 2016 US Centers for Disease Control and Prevention opioid prescribing guideline with changes in opioid dispensing after surgery. JAMA Netw Open 2021;4(6):e2111826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dayer LE, Breckling MN, Kling BS, et al. Association of the “CDC Guideline for Prescribing Opioids for Chronic Pain” with emergency department opioid prescribing. J Emerg Med 2019;57(5):597–602. [DOI] [PubMed] [Google Scholar]
- 17.National Commission on Certification of Physician Assistants. Statistical Profile of Certified PAs: Annual Report; 2020. Available at: https://www.nccpa.net/wp-content/uploads/2022/02/2020-Statistical-Profile-of-Recently-Certified-PAs-Final-2_23_22.pdf (accessed May 12, 2022).
- 18.American Academy of Nurse Practitioners. Findings from 2020 Survey Show Nurse Practitioners (NPs) Continue to Provide Quality Health Care during the Pandemic. AANP News; 2021. Available at: https://www.aanp.org/news-feed/findings-from-2020-survey-show-nurse-practitioners-nps-continue-to-provide-quality-health-care-during-the-pandemic (accessed May 12, 2022). [Google Scholar]
- 19.Willis J, Antono B, Bazemore A, et al. The State of Primary Care in the United States: A Chartbook of Facts and Statistics; 2020. Available at: https://www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/PrimaryCareChartbook2021.pdf (accessed May 12, 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


