Abstract
INTRODUCTION
Though urology attracts well-qualified applicants, students are not typically provided exposure to this smaller specialty until later in their medical education. While simulation-based training continues to supplement medical education, there is a lack of programming to teach specialty-specific procedural skills to medical students and those outside the specialty. We report a half-day simulation and didactic-based approach to increase exposure to urology to interested second-year medical students.
METHODS
A half-day didactic- and simulation-based session was offered to second-year medical students (N=57). After a didactic-based overview of the specialty performed by urology providers and a surgical educator, the students participated in small-group simulations, including hands-on simulations. The students completed a post-curriculum survey measuring knowledge gains and soliciting feedback on the session.
RESULTS
Students were 57.1% Caucasian, 66.7% female, with a mean age of 24.2 years; 80% stated they were potentially interested in pursuing a surgical specialty such as urology prior to the start of the session. Students reported pre- to post-curriculum gains in knowledge (mean=37%) about a career in urology and basic urologic procedures (p<0.001). Participants were also likely to recommend the curriculum to their peers (p<0.001).
CONCLUSIONS
Given that exposure to urology in medical school is usually limited and offered later in training, a half-day didactic- and simulation-based experience for second-year students provides an early introduction and experience within the specialty and its common bedside procedures.
INTRODUCTION
Urology is a competitive surgical specialty, with applicant numbers consistently exceeding those of available positions.1–3 Despite the incremental increase in the number of residency positions offered across the U.S. training programs, during the past 10 years, there has not been an associated increase in the total number of applicants as one might expect.1,4 Interestingly, this has been observed not just in urology but in other surgical fields as well.5,6 This becomes more troublesome with the continued trend of an aging urology workforce and predicted future shortages.4 There are a number of different barriers that may prevent interest in the field. The presence of educational barriers, such as the need for early exposure to urology, high USMLE scores, and a strong research background, is well-documented.1,7 There are also gender barriers, with urology remaining a male-dominated field despite improvements in recent years.1,3,7,8 In addition, there is a significant cost associated with completing rotations and applying to urology residency, estimated to be upwards of $7000, leading to socioeconomic barriers to applying to the field.1,4–8
In addition to these factors, a significant barrier to ramp up interest and applications to the field urology and other surgical fields is a lack of exposure in medical education, with as few as 5% of institutions having a required clinical rotation in urology in third- and fourth-year medical training, and 50% of medical schools not having any clinical exposure to the field.1,9–13 One approach to begin overcoming these hurdles is with earlier, preclinical exposure to urology.
Different methods have been proposed for promoting early exposure to urology. Virtual didactic programs have shown some success increasing knowledge and interest in the field based on surveys administered in the study;14 however, as a surgical specialty, it is critical to educate students not just on the medical knowledge but on the hands-on skills. There is evidence to suggest this approach — with direct interactions with students, including simulations — may improve student confidence and knowledge, and spark an interest in the field.15–18
In this study, we aimed to improve early exposure for medical students to the field of urology with a half-day workshop that included a combined didactic and hands-on simulation session as part of a ‘career exploration week’ for second-year medical students at our institution.
METHODS
Study sample
Fifty-seven second-year medical students at our institution participated in one of five half-day didactic and simulation workshops as part of a ‘career exploration week’ single urology session. Students were 57.1% Caucasian, 33.3% male, 87.5% non-Hispanic or Latino, with a mean age of 24.1 years (standard deviation [SD ] 1.21). Twenty-eight (80%) students reported that they were potentially interested in pursuing a surgical specialty such as urology prior to the start of the session. Additional demographics and descriptive variables of the study sample are reported in Table 1. Given that demographics did not differ across groups, metrics have been collapsed for further data analysis moving forward.
Table 1.
Demographic and descriptive sample summary
| Timepoint 1 (Oct. 2021) | Timepoint 2 (March 2022) | Timepoint 3 (Oct. 2022) | Timepoint 4 (Nov. 2022) | Timepoint 5 (Feb. 2023) | All timepoints (cumulative) | |
|---|---|---|---|---|---|---|
|
| ||||||
| Gender | ||||||
| Male | n=4 (33.3%) | n=6 (85.7%) | n=10 (66.7%) | n=0 (0.0%) | n=12 (66.7%) | n=20 (33.3%) |
| Female | n=8 (66.7%) | n=1 (14.3%) | n=5 (33.3%) | n=5 (100%) | n=6 (33.3%) | n=19 (66.7%) |
|
| ||||||
| Age | Mean 23.9 years | Mean 24.57 years | Mean 24.3 years | Mean 23.25 years | Mean 24.72 years | Mean 24.1 years |
| SD 1.24 | SD 1.40 | SD 1.17 | SD 0.5 | SD 1.56 | SD 1.21 | |
| Range 23–27 | Range 23–27 | Range 23–26 | Range 23–24 | Range 23–28 | Range 23–27 | |
|
| ||||||
| Race | ||||||
| Caucasian | n=8 (66.7%) | n=6 (85.7%) | n=9 (64.3%) | n=2 (40%) | n=7 (38.9%) | n=32 (57.14%) |
| Asian | n=2 (16.7%) | n=0 (0.0%) | n=3 (21.4%) | n=2 (40%) | n=5 (27.8%) | n=12 (21.4%) |
| Black/African American | n=1 (8.3%) | n=1 (14.3%) | n=2 (14.3%) | n=1 (20%) | n=3 (16.7%) | n=8 (14.28%) |
| Other | n=0 (0.0%) | n=0 (0.0%) | n=0 (0.0%) | n=0 (0.0%) | n=2 (11.11%) | n=2 (3.57%) |
| Multi-race | n=1 (8.3%) | n=0 (0.0%) | n=0 (0.0%) | n=0 (0.0%) | n=1 (5.6%) | n=2 (3.57%) |
|
| ||||||
| Undergraduate Major | ||||||
| Natural science | n=6 (50%) | n=4 (57.14%) | n=8 (50%) | n=3 (75%) | n=7 (35%) | n=21 (53.85%) |
| Other science | n=4 (33.3%) | n=3 (42.86%) | n=8 (50%) | n=1 (25%) | n=9 (45%) | n=16 (41.02%) |
| Other | n=2 (16.7%) | n=0 (0.0%) | n=0 (0.0%) | n=0 (0.0%) | n=4 (20%) | n=2 (5.13%) |
|
| ||||||
| Intended specialty | Dermatology: n=2 (11.8%) ENT: n=1 (5.8%) General surgery: n=3 (17.65%) Neurology: n=1 (5.8%) OB/GYN: n=3 (17.65%) Plastic surgery: n=1 (5.8%) Urology: n=4 (23.5%) Unsure: n=2 (11.8%) |
General surgery: n=2 (25%) OB/GYN: n=1 (12.5%) Ophthalmology: n=2 (25%) Radiology: n=1 (12.5%) Unsure: n=2 (25%) |
Anesthesiology: n=2 (11.1%) EM: n=1 (5.6%) ENT: n=1 (5.6%) General surgery: n=5 (27.8%) Internal medicine: n=1(5.6%) Ophthalmology: n=1 (5.6%) Orthopedic: n=1 (5.6%) Pediatrics: n=1 (5.6%) Plastic surgery: n=1 (5.6%) Urology: n=1 (5.6%) Unsure: n=3 (16.7%) |
Dermatology: n=1 (16.7%) G.I.: n=1 (16.7%) General surgery: n=1 (16.7%) Unsure: n=3 (50%) |
Anesthesiology: n=2 (11.1%) EM: n=2 (11.1%) GI: n=1 (5.6%) General surgery: n=1(5.6%) OB/GYN: n=2 (11.1%) Ophthalmology: n=1 (5.6%) Orthopedic: n=2 (11.1%) Plastic surgery: n=1 (5.6%) Radiology: n=2 (11.1%) Urology: n=1 (5.6%) Unsure: n=3 (16.7%) |
Anesthesiology: n=2 (4.5%) Dermatology: n=3 (6.8%) EM: n=1 (2.3%) ENT: n=2 (4.5%) General surgery: n=11 (25%) Neurology: n=1 (2.3%) OB/GYN: n=4 (9.09%) Ophthalmology: n=3 (6.8%) Plastic surgery: n=2 (4.5%) Radiology: n=1 (2.3%) Urology: n=5 (11.4%) Unsure: n=10 (22.7%) |
|
| ||||||
| Intended Specialty | ||||||
| Surgical | n=12 (80%) | n=5 (83.3%) | n=11 (73.3%) | n=1 (33.3%) | n=11 (84.6 %) | n=28 (80%) |
| Non-surgical | n=3 (20%) | n=1 (16.7%) | n=4 (26.7%) | n=2 (66.7%) | n=2 (15.38%) | n=7 (20%) |
| Urology | n=4 (26.7%) | n=0 (0.0%) | n=1 (6.7%) | n=0 (0.0%) | n=1(7.14%) | n=5 (14.3%) |
| Non-urology | n=11 (73.3%) | n=6 (100%) | n=14 (93.3%) | n=3 (100%) | n=13 (92.86%) | n=30 (85.7%) |
|
| ||||||
| Current level of interest in surgery (Likert scale: 1–10) | Mean 8.25 | Mean 8.71 | Mean 8 | Mean 8 | Mean 6.94 | Mean 8.21 |
| SD 1.22 | SD 0.76 | SD 2.80 | SD 1.87 | SD 2.48 | SD 1.96 | |
| Range 6–10 | Range 8–10 | Range 2–10 | Range 6–10 | Range 2–10 | Range 2–10 | |
|
| ||||||
| Current level of interest in urology (Likert scale: 1–10 | Mean 7.2 | Mean 5.7 | Mean 6.2 | Mean 6.2 | Mean 5.89 | Mean 6.4 |
| SD 1.19 | SD 1.60 | SD 2.14 | SD 1.30 | SD 1.97 | SD 1.73 | |
| Range 6–9 | Range 3–8 | Range 2–9 | Range 5–8 | Range 1–9 | Range 2–9 | |
Note that some students indicated multiple specialties of interest.
SD: standard deviation.
Curriculum design
The curriculum took place during a dedicated block as part of our College of Medicine’s pre-established ‘career exploration week,’ which provides dedicated, protected education time for second-year medical students to attend additional education sessions by specialty. The didactics portion of the session took place in a conference room of our Health Sciences Library and the simulation portion took place at the simulation and clinical skills center housed in that same location, which also provided all models and equipment. Because identifying information was not collected from participants as part of this study, institutional review board approval was not needed.
The half-day workshop was developed by the department’s education specialist PhD, with previous input from the department’s clerkship directors, and consisted of three components
Component 1 was a 60-minute didactic overview of urology as a specialty. The interactive presentation was led by two providers (either two fellows or a fellow and senior resident) and the education specialist. Content included a general description of urology; types of patients, diagnoses, presentations, and procedures seen in urology; length and description of training; match statistics and process; examples of post-residency training and employment options; examples of technology and surgical procedures; and quality-of-life metrics, such as practice options, compensation, lifestyle considerations, and personal perspectives.
Following the didactic overview, component 2 consisted of small groups rotating across simulation stations for 90 minutes. These stations were staffed by the same two providers who presented the didactic overview. The procedures reviewed were male and female urinary catheterization; bimanual and speculum examination of a female patient; digital rectal examination of male patient; and examination of male external genitalia.
Component 3 was a 30-minute question-and-answer period. This was time for open-ended questions from the students, with some prepared questions from the education specialist, who moderated the session. Questions were typically about lifestyle and a day-in-the-life of our providers, as well as inquiries about motivation for entering the specialty, pursuing a fellowship, and pursuing an academic trajectory.
Curriculum evaluation
At the end of the half-day session, all students completed a post-curriculum paper-and-pencil survey (Appendix; available at cuaj.ca). This questionnaire was internally developed by the department’s education specialist, who has more than 11 years of experience with survey design, curriculum design and evaluation, and behavioral metrics. The survey solicited quantitative and qualitative responses. The survey asked students to provide demographic and descriptive information (eight questions, open answer and multiple-choice formats), current interest in both surgery and urology (two questions, 10-point scale), satisfaction with current training (two questions, five-point Likert scale), pre- and post-curriculum knowledge (six questions, five-point Likert scale), satisfaction with the curriculum (11 questions, five-point Likert-scale), and any additional feedback or suggestions for the session (two questions, open answer/free text response). The questionnaire took approximately five minutes to complete. Although it was voluntary, 100% of participants filled out the evaluation across both sessions.
Statistical analysis
All data was performed using SPSS Statistics software (IBM SPSS Statistics, version 27.0. Armonk, NYm U.S.). Data are presented as means (SD) or proportions (percentages). Per study objectives, analyses were primarily descriptive and exploratory in nature. Analyses were performed comparing independent group differences (those interested in surgery vs. those who were not) via Chi-squared tests for categorical variables or independent t-tests for continuous variables. Paired-samples t-tests were used to compare two variables from the same group (e.g., pre- vs. post-knowledge) and single-sample t-tests were used to compare single group means (e.g., gains=post-pre) to a predetermined standard (e.g., zero). Linear and logistic regression modeling was conducted to examine predictors for outcome variables of interest.
RESULTS
Current surgical training and ability
Students were asked to whether they were satisfied/dissatisfied with their current surgical training and abilities prior to participation in the curriculum. On average, students rated their satisfaction with their training to date as neutral (mean 2.98/5, p=0.439), but reported they were not satisfied with their current surgical abilities (mean 2.50/5, p<0.001).
Gains in content knowledge
Students reported their pre-curriculum and post-curriculum knowledge across the following topics via a five-point Likert-scale from 1=novice to 5=expert: types of patients and cases a urologist manages; practice options; type of surgeries and equipment a urologist uses; Foley catheter placement; pelvic examination; and information about the OSU Department of Urology. Results appear in Figure 1. Students reported low knowledge prior to participation in the curriculum (p<0.001) and significant gains in knowledge across these topics and skills following participation (p<0.001). Regression modeling on a cumulative ‘gains’ score (average post metrics minus average pre metrics) indicated no significant impact of any demographic or descriptive variables (model: R2=0.728, p=0.061).
Figure 1.
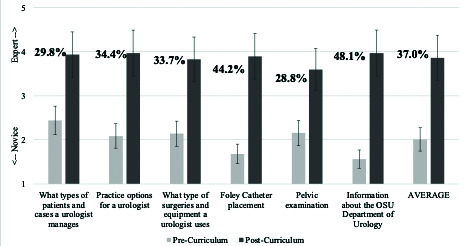
Students reported pre- to post-curriculum gains in knowledge (mean=41%) about a career in urology and basic urologic procedures (p<0.001) via Likert-scale questions. Error bars represent standard error of the mean.
Curriculum evaluation
Results appear in Figure 2. Students reported that the curriculum helped them understand urology as a specialty (p<0.001), helped them understand what a career in urology would look like (p<0.001), helped them learn how to perform common procedures in this specialty (p<0.001), gave them a good overview of the urology program at our institution (p<0.001), was generally beneficial to their education (p<0.001), was beneficial to their ability to work with a team (p<0.001), and that they would recommend it to their peers (p<0.001). They also felt that it was intellectually challenging (p<0.001), increased their knowledge of the subject matter (p<0.001), gave them the opportunity to practice the skills taught in the course (p<0.001), and improved their problem-solving (p<0.001). Regression modeling on whether the curriculum was beneficial to students’ education indicated no significant impact of any demographic or descriptive variables (model: R2=0.253, p=0.905). Similarly, independent t-tests compared those students who indicated an interest in surgery vs. those who did not and there were no differences in satisfaction with the curriculum (all p>0.1).
Figure 2.
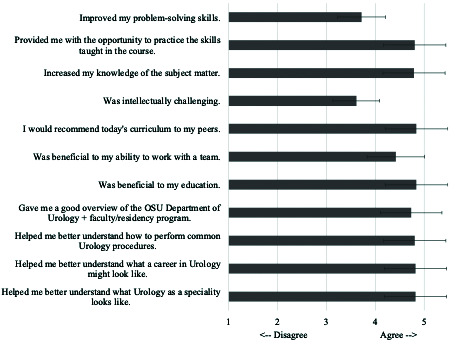
Students overwhelmingly rated the curriculum very highly (all p<0.001) and beneficial to their understanding of urology as a specialty, as well as beneficial to their medical education more broadly.
Qualitative feedback and suggestions
Student qualitative responses to the two open-ended questions at the end of the survey evaluation are recorded in Table 2. Thirty-six of the 57 students who participated (63.2%) left qualitative feedback on the session and most of the comments could be classified as positive (i.e., “This was great” or “X was helpful”), with additional comments and feedback speaking to the usefulness of additional components to include in future iterations.
Table 2.
Qualitative short answers given by students on the curriculum evaluation
| Additional comments/feedback? | Is there anything not reviewed in today’s session that would be useful to incorporate in future versions or for career exploration week? |
|---|---|
| Loved doing the simulation. Super cool way to learn vital procedures. | Suturing and rotating with the specialty. |
| I thought that this selective was very well thought out and increased my interest in urology. | Maybe more simulation time but overall great, and I really enjoyed the small-group setting |
| This was great! Would love a suturing clinic but I understand that’s hard to fit into this. | Digital rectal exams on simulation lab models. |
| I really enjoyed the Q+A time because it’s not often can we get info about specialties from actual department members. | More stories from urologists about how they knew they wanted to do urology, and what we as medical students can do now to be more competitive. |
| All components of this session were so helpful. I feel like I got to learn a lot about urology as a specialty, about the OSU urology department in particular, and got to learn some exciting clinical skills. Thanks for not making this “death by PowerPoint” | Maybe including PowerPoint slides that correspond to the simulation. |
| I really enjoyed the two simulation stations and the hands-on component. | Involvement with surgical simulations. |
| Simulations were helpful. | I thought this was run as perfect as possible. I appreciate that we got to do some hands-on work. |
| The more simulations or procedures, the better. | Shadowing in the clinic or OR would have been cool. |
| The question-and-answer portion, as well as the Foley catheter simulation were both great. | Would love the ability to practice on the DaVinci. |
| I thought this was very well-organized and I really appreciated the hands-on simulation. Would be nice to invite a female resident in the future. | Some time at the surgical suites would be amazing. |
| I really enjoyed the session. I would have benefited from a little more time with the Foley catheter. Otherwise, great session. | More time/models for simulations. |
| This was great! Thank you. | Seeing procedures in OR/clinic. |
| Really appreciated the hands-on activities. | Female lifestyle in urology, family planning as a urology resident/attending. |
| Really well-organized and executed. Very fun and informative. | More about research. |
| Great presentation. Excellent work! | As someone interested in surgery, some simulation related to urologic procedures would have been attention-grabbing. |
| The panel was amazing! They were excited to talk with us and were very helpful in answering all the questions. | I think today was fantastic. Thank you for your time and help. |
| I loved the style of the presentation and how much the residents/fellows were willing to offer. | More female representation and application. |
| Great session, even though I do not have much interest in urology. | Some examples of using the tech since it is relatively unique to urology. |
| Thank you for bringing very informative, enthusiastic speakers. | Maybe a simulation with urology tech (i.e., lasers, etc.) |
| Female physicians/residents would be great. | I thought it was great. |
| Great session. | More about the residency application and process. |
| This session was great. I really hadn’t thought about urology as a field, especially due to my gender, and it was great to meet women in the field. | Seeing an actual case if possible. |
| Really enjoyed today’s presentation. | Female perspective. |
| This was amazing. | |
| Appreciated the time of all the doctors and to hear from non-clinical staff about considerations for applications/rotations. | |
| Thank you for your time. | |
| Thank you all for your time. | |
| The overview PowerPoint should be condensed. It felt down cut. |
For the didactics portion, students suggested specifically reviewing clinical information relevant to the simulations they participated in, as well as additional information from the providers about their motivation for pursuing urology and what made them/makes students a competitive applicant.
For the simulation portion, students suggested additional simulation time, suturing, rotating through actual clinics and operating rooms, and exposure to the robotic surgery platforms. Broadly, a couple of suggestions touched on the demographic makeup of the presenters themselves, who tended to be our endourology/minimally invasive surgery fellow (male) and a resident physician on their research month rotation (male), indicating a greater number of female urologists would also be useful and wanted.
DISCUSSION
Urology is often under-represented in medical school curriculums, with some medical students reporting minimal or no exposure to urology in their training, whether that be didactic lectures and/or clinic experience. 10–12 Exposure at our institution is similar to that of many other locations, in which there is no required clinical rotations,11,12 although interested students have the opportunity to participate in urology electives during their core surgical and family medicine rotations in their third and fourth year of medical school.
Our voluntary, in-house workshop was one of several specialties hosted during protected education time as part of a career exploration week for second-year medical students intended to address some of these shortcomings, while soliciting feedback using a mixed-survey method, which has not been reported in this space previously.
Our workshop included a didactic component to introduce students to the specialty (patients, procedures, anatomy, lifestyle), followed by hands-on procedure simulations. We dedicated nearly 50% of the workshop to hands-on training of basic urologic procedures, given that it has been shown that medical students had higher levels of interest in urology, as well as improved knowledge and confidence levels, after simulating basic urologic skills such as Foley catheter placement and digital rectal exams.15,16,18 Previous research by Head et al19 and Hicks et al20 on surgical exploration and early discovery (SEAD) programs support a combined didactic and hands-on format to jump start students’ interest in surgery. These workshops are structured similarly to the entire career exploration week at our institution. Head et al and Hicks et al found SEAD programs are effective in changing students’ perceptions of surgical fields and increasing an early and growing interest in surgical specialties. Unfortunately, we lack longitudinal data to assess the long-term effects of our program; for example, it would be worthwhile to track continued engagement in surgery or urology, including involvement in research projects, rotations via clerkships, and/or participation in the match.
The COVID -19 pandemic has certainly further reduced exposure to urology, as students’ clinical activities and exposure to different subspecialties has decreased. Manalo et al attempted to overcome this by organizing a week-long urology didactic curriculum administered virtually, which actively engaged students and faculty.14 This increased students’ objective knowledge in common urologic topics, as seen through score increases in preand post-course quizzes. Due to the virtual nature of the course, there was no hands-on practice involved in their curriculum. As indicated by the strong positive response to the hands-on simulation portion of our workshop, a mixed approach will most likely increase student’s knowledge and skill in the field of urology, and this type of mixed-methods workshop could serve as a model for other institutions hoping to similarly increase exposure to small specialties. Additionally, students who participated in our half-day workshop indicated increased gains in knowledge and interest, despite the short timeframe, indicating short-term exposure such as this may be useful.
Although not the critical component of our workshop, we also introduced an element of prospective mentorship with our faculty, fellows, and residents who helped run these sessions. This unmeasured mentorship (or point of contact) may additionally serve to increase interest or support in pursuing a career in urology, given reports that medical students who undergo their medical education at centers with strong residency programs with effective mentors are more likely to match into urology.10 Similarly, it has been reported in previous student survey studies that research and mentorship are commonly perceived by students to be important elements of a successful application and can represent a possible barrier for students interested in urology.1 In fact, a nationwide study to connect potential urology candidates to mentors received positive feedback and a match success rate in excess of 90%.21 Thus, although not a key objective of our workshop, this exposure to urology included potential mentors and points of contact, which may prove to be of particular benefit to students as they consider specialties in the coming years.
Urology remains a primarily male- and Caucasian-dominated specialty and lags other specialties in diversifying. 4,8,21–23 It can, therefore, be argued that urology has a “leaky pipeline,”24 as it does not catch certain demographics that are increasingly graduating from medical schools. For instance, there are increasing number of African American medical school graduates; however, the number of African American students applying to and getting accepted to urology has not only failed to increase but has slowly decreased.21
Similar patterns are seen with increasing numbers of female medical school graduates; while the number of female students applying and getting accepted to urology increased over 10-fold from 1978–2013, they remain under-represented in urology.23 It is promising, however, that over 40% of incoming urology residents per 2024 AUA match data identify as female. Linear and logistic regression modeling indicated that students’ ethnic and gender identity had no effect on their subjective gains in knowledge or skills following participation in our half-day course. In addition, the participating groups of students in our workshop included an over-representation of women (nearly 2/3 of participants were female), indicating a higher proportion compared to both our own medical school and national reports of females entering the field of urology (only 11.6% of practicing urologists in the 2022 American Urological Association Census were female).21 This provides initial evidence that this type of workshop or early introduction to specialties like urology can increase exposure to under-represented medical students, who may have not had opportunities for exposure to the field in the past.
Limitations
We do acknowledge some limitations to this study.
First was the half-day nature of the workshop. While participants reported benefits from the presented curriculum, it may be beneficial to expand the curriculum in future iterations. By increasing the length of the session or offering multiple sessions, we can potentially build upon knowledge and skillset to prepare very interested students for training in urology and to foster mentor/mentee relationships. For instance, future iterations of the session could include procedural training, such as cystoscopy and basic laparoscopy. It is worth noting that the incorporation of robotic/laparoscopic simulations should be done with care and at a level appropriate for the students’ skill and knowledge. While this is often a requested topic by medical students and is associated with high rates of satisfaction, it has not been shown to correlate with increased interest in pursuing surgical specialties, and is thought to be due to the complex nature of the techniques.25,26
Other limitations include the non-comparative nature of our workshop. Future studies could include multiple different workshops, such as didactic, simulation-only, combined as presented here, or other approaches to determine the most effective workshop methodology to increase students’ interest and understanding of a career in urology. On this note, our institution does have an entire career exploration week, where students can attend multiple sessions from other specialties; however, we only have evaluations and feedback from our single urology curriculum.
An additional limitation of this study is that our evaluation was only given at a single timepoint. Future studies could follow students long-term to see how many end up pursuing electives in surgery or urology, and how many end up applying to surgery or urology residency programs.
Finally, we acknowledge that there may be self-selection bias in this study, given that students voluntarily attended specialty sessions of interest.
CONCLUSIONS
Urology is often an under-represented topic in medical school curriculums, particularly during preclinical years of training. We developed a half-day curriculum that included a didactic overview and hands-on procedure simulation, which showed significant gains in participants’ self-reported understanding of the field of urology, urology as a specialty of choice, and in their own urologic knowledge and skill. This curriculum could serve as a model for further development or expansion of workshops or programming to increase knowledge of and exposure to the field of urology.
Supplementary Information
ACKNOWLDGEMENTS
The authors would like to acknowledge the contributions of their Clerkship Directors, Dr. Fara Bellows and Dr. Eric Springer, who assisted in the creation of previous versions of the slide deck used in the didactic presentation and specialty overview. They would like to thank the Ohio State University College of Medicine Clinical Skills Education and Assessment Center for providing the simulation equipment and space. And finally, they would like to thank the students who participated in this education session for their feedback and evaluations.
Footnotes
Appendix available at cuaj.ca
COMPETING INTERESTS: The authors do not report any competing personal or financial interests related to this work.
This paper has been peer-reviewed.
REFERENCES
- 1.Matloubieh JE, Eghbali M, Abraham N. Strategies to encourage medical student interest in urology. Curr Urol Rep. 2020;21:34. doi: 10.1007/s11934-020-00984-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Macdonald EJ, Gaines JM, Taubenfeld E, et al. Analysis of twitter engagement in a progressively more competitive urology match: A mixed methods study. Urology. 2022;167:30–5. doi: 10.1016/j.urology.2022.04.029. [DOI] [PubMed] [Google Scholar]
- 3.Patel SR, Mayer WA, Taylor JM. Urology match outcomes during the coronavirus pandemic. J Urol. 2021;206:194–6. doi: 10.1097/JU.0000000000001737. [DOI] [PubMed] [Google Scholar]
- 4.McKibben MJ, Kirby EW, Langston J, et al. Projecting the urology workforce over the next 20 years. Urology. 2016;98:21–6. doi: 10.1016/j.urology.2016.07.028. [DOI] [PubMed] [Google Scholar]
- 5.Hill Elspeth JR, et al. Can I cut it? Medical students’ perceptions of surgeons and surgical careers. Am J Surg. 2014;208:860–7. doi: 10.1016/j.amjsurg.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 6.Austin Ryan E, Wanzel Kyle R. Supply versus demand: A review of application trends to Canadian surgical training programs. Can J Surg. 2015;58:143–4. doi: 10.1503/cjs.006614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim Y, Kassam AF, McElroy IE, et al. The current status of the diversity pipeline in surgical training. Am J Surg. 2022;224:250–6. doi: 10.1016/j.amjsurg.2021.11.006. [DOI] [PubMed] [Google Scholar]
- 8.Ukeje C, Elmasri A, Kielb S. Improving gender diversity in urologic residency training. Curr Urol Rep. 2021;22:60. doi: 10.1007/s11934-021-01074-6. [DOI] [PubMed] [Google Scholar]
- 9.Beebe S, Payne N, Posid T, et al. The Lack of sexual health education in medical training leaves students and residents feeling unprepared. J Sex Med. 2021;18:1998–2004. doi: 10.1016/j.jsxm.2021.09.011. [DOI] [PubMed] [Google Scholar]
- 10.Kutikov A, Bonslaver J, Casey JT, et al. The gatekeeper disparity: Why do some medical schools send more medical students into urology? J Urol. 2011;185:647–52. doi: 10.1016/j.juro.2010.09.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loughlin KR. The current status of medical student urological education in the United States. J Urol. 2008;179:1087–91. doi: 10.1016/j.juro.2007.10.068. [DOI] [PubMed] [Google Scholar]
- 12.Slaughenhoupt B, Ogunyemi O, Giannopoulos M, et al. An update on the current status of medical student urology education in the United States. Urology. 2014;84:743–7. doi: 10.1016/j.urology.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 13.Mann U, Nayak JG. The potential impact of COVID-19 on the Canadian Resident Matching Service: Unique future challenges faced by urology residency programs and applicants. Can Urol Assoc J. 2020;14:E167–8. doi: 10.5489/cuaj.6616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manalo TA, Higgins MI, Pettitt-Schieber B, et al. A strategy for undergraduate medical education in urology during the COVID-19 pandemic. J Surg Educ. 2021;78:746–50. doi: 10.1016/j.jsurg.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodríguez-Díez MC, Díez N, Merino I, et al. La simulación mejora la confianza de los estudiantes para adquirir competencias en urología. Actas Urológicas Españolas. 2014;38:367–72. doi: 10.1016/j.acuro.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Cohen A, Nottingham C, Packiam V, et al. Attitudes and knowledge of urethral catheters: A targeted educational intervention. BJU Int. 2016;118:654–9. doi: 10.1111/bju.13506. [DOI] [PubMed] [Google Scholar]
- 17.Ingram A, Bellows F, McKisson E, et al. Implementation and assessment of a urology education curriculum for nursing residents. J Contin Educ Nurs. 2021;52:511–6. doi: 10.3928/00220124-20211008-06. [DOI] [PubMed] [Google Scholar]
- 18.Stout M, Posid T, Ballinger J, et al. Urology boot camp: A pilot medical student curriculum for common bedside urologic procedures. Urology. 2022;169:35–40. doi: 10.1016/j.urology.2022.06.050. [DOI] [PubMed] [Google Scholar]
- 19.Head, Linden K, et al. Harvesting the ‘SEAD’: Long-term followup of the surgical exploration and discovery program. J Surg Educ. 2020;77:96–103. doi: 10.1016/j.jsurg.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 20.Hicks, Katie E, et al. Surgical exploration and discovery program: Early exposure to surgical subspecialties and its influence on student perceptions of a surgical career. J Surg Educ. 2019;76:1248–57. doi: 10.1016/j.jsurg.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Shantharam G, Tran TY, McGee H, et al. Examining trends in underrepresented minorities in urology residency. Urology. 2019;127:36–41. doi: 10.1016/j.urology.2018.10.061. [DOI] [PubMed] [Google Scholar]
- 22.American Urological Association. The state of the urology workforce and practice in the United States. AUA; 2019. [Accessed Nov 20, 2023]. Available at: https://www.auanet.org/common/pdf/research/census/State-Urology-Work-force-Practice-US.pdf. [Google Scholar]
- 23.Halpern JA, Lee UJ, Wolff EM, et al. Women in urology residency, 1978–2013: A critical look at gender representation in our specialty. Urology. 2016;92:20–5. doi: 10.1016/j.urology.2015.12.092. [DOI] [PubMed] [Google Scholar]
- 24.Zheng MY, Overland M, Escobar D, et al. Formal mentorship as an opportunity to expand the urology pipeline: Under represented trainees entering residency (UReTER) program evaluation 2020–2021. Urology. 2022;162:108–13. doi: 10.1016/j.urology.2021.06.052. [DOI] [PubMed] [Google Scholar]
- 25.Madan AK, Frantzides CT, Quiros R, et al. Effects of a laparoscopic course on student interest in surgical residency. JSLS. 2005;9:134–7. [PMC free article] [PubMed] [Google Scholar]
- 26.Gjertson CK, Mohammadi Y, Lipke MC, et al. An innovative medical student clinical clerkship in advanced urologic laparoscopy: A preliminary experience. J Endourol. 2008;22:1345–50. doi: 10.1089/end.2008.0057. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


