Abstract
Introduction
We investigated cognitive profiles among diverse, middle‐aged and older Hispanic/Latino adults in the Study of Latinos–Investigation of Neurocognitive Aging (SOL‐INCA) cohort using a cross‐sectional observational study design.
Methods
Based on weighted descriptive statistics, the average baseline age of the target population was 56.4 years, slightly more than half were women (54.6%), and 38.4% reported less than a high school education. We used latent profile analysis of demographically adjusted z scores on SOL‐INCA neurocognitive tests spanning domains of verbal memory, language, processing speed, and executive function.
Results
Statistical fit assessment indices combined with clinical interpretation suggested five profiles: (1) a Higher Global group performing in the average‐to‐high‐average range across all cognitive and instrumental activity of daily living (IADL) tests (13.8%); (2) a Higher Memory group with relatively high performance on memory tests but average performance across all other cognitive/IADL tests (24.6%); (3) a Lower Memory group with relatively low performance on memory tests but average performance across all other cognitive/IADL tests (32.8%); (4) a Lower Executive Function group with relatively low performance on executive function and processing speed tests but average‐to‐low‐average performance across all other cognitive/IADL tests (16.6%); and (5) a Lower Global group performing low‐average‐to‐mildly impaired across all cognitive/IADL tests (12.1%).
Discussion
Our results provide evidence of heterogeneity in the cognitive profiles of a representative, community‐dwelling sample of diverse Hispanic/Latino adults. Our analyses yielded cognitive profiles that may assist efforts to better understand the early cognitive changes that may portend Alzheimer's disease and related dementias among diverse Hispanics/Latinos.
Highlights
The present study characterized cognitive profiles among diverse middle‐aged and older Hispanic/Latino adults.
Latent profile analysis of neurocognitive test scores was the primary analysis conducted.
The target population consists of middle‐aged and older Hispanic/Latino adults enrolled in the Hispanic Community Health Study/Study of Latinos and ancillary Study of Latinos ‐ Investigation of Neurocognitive Aging.
Keywords: aging, Alzheimer's disease and related dementias, cognitive phenotyping, Hispanic/Latino, neuropsychology
1. BACKGROUND
The prevalence of Alzheimer's disease and related dementias (ADRD) in the United States is projected to rise exponentially as the aging population expands. 1 The US population is also increasingly diversifying, with Hispanic/Latino individuals comprising the second largest ethnic or racial group, projected to outpace the growth of all other ethnic and racial groups over the next few decades. 2 Consequently, ADRD prevalence among Hispanics/Latinos and other ethnoracially diverse groups is expected to double in the United States and other Western countries during this timeframe. Nevertheless, our understanding of the epidemiology of ADRD has been complicated by a limited, albeit growing, understanding of the extent to which commonly used methods for characterizing and diagnosing ADRD generalize to ethnoracially diverse groups, including diverse Hispanics/Latinos. 3 Further efforts to characterize cognitive aging among Hispanic/Latino adults will be imperative given current estimates and projections of ADRD in this population.
Examining the earliest neurocognitive changes associated with ADRD is critical for enhancing diagnostic accuracy for at‐risk individuals in early stages of ADRD. To that end, previous work has shown that using cluster‐analytic statistical techniques (e.g., hierarchical cluster analysis, latent class cluster analysis) considerably improves cognitive characterizations and diagnostic accuracy during the early stages of ADRD, including mild cognitive impairment (MCI). 4 , 5 , 6 , 7 Such tools have uncovered distinct, meaningful cognitive profiles (e.g., amnestic, dysnomic, and dysexecutive/mixed) of MCI that are not well captured by conventional diagnostic methods yet have been consistently observed in multiple study populations, in the context of both clinical samples as well as large‐scale, convenience sample cohort studies of cognitive aging (e.g., Alzheimer's Disease Neuroimaging Initiative [ADNI], Mayo Clinic Study of Aging 4 , 5 , 6 , 7 , 8 , 9 ). This body of research has shown that conventional methods can result in false‐positive diagnostic errors, 6 which could help to explain reports of high rates of reversion to cognitively normal and low rates of progression to dementia in those with MCI. 10 Additionally, previous studies suggest that empirically derived cognitive subtypes of MCI may have differential probabilities of progression toward different types of dementia (e.g., individuals with amnestic MCI profiles may be more likely to progress toward dementia with primary Alzheimer's disease [AD] pathology, whereas those with dysexecutive MCI profiles may be more likely to progress toward dementia with primary vascular contributions 9 ). However, these studies used ethnoracially homogeneous samples of primarily non‐Hispanic White, older adults and were therefore not adequately representative of the diverse population that is affected by ADRD, including Hispanic/Latino adults. Moreover, these studies focused largely on samples manifesting clear cognitive changes during more evident stages of ADRD. Whether similar cognitive profiles emerge when using the same cluster‐analytic statistical methods with a more diverse Hispanic/Latino sample in as early as middle age and during the earliest (e.g., preclinical) stages of ADRD has not been adequately investigated. Leveraging sensitive and reliable methods to improve our understanding of the earliest neurocognitive changes associated with ADRD among Hispanic/Latino adults, and to ultimately identify which cognitive subtypes may be more likely to develop into different types of dementia, is necessary to adequately prepare for the impending growth of the diverse aging population, and to meet our needs of accurately diagnosing and identifying at‐risk Hispanic/Latino adults.
We sought to characterize cognitive profiles among diverse, middle‐aged and older Hispanic/Latino adults using latent profile analysis of neurocognitive test scores collected through the Study of Latinos–Investigation of Neurocognitive Aging (SOL‐INCA), an ancillary study of the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). SOL‐INCA was designed to study the prevalence and determinants of neurocognitive decline and MCI in Hispanic/Latino adults. Thus, findings from the present study will assist in much‐needed efforts to improve our understanding of the earliest neurocognitive changes associated with ADRD in this population. Moreover, this work directly addresses our nation's identified priority of improving ADRD assessment tools and analytic methods to enhance the generalizability and equity of scientific research in AD/ADRD.
2. METHODS
2.1. Data
The HCHS/SOL is a prospective cohort study of community‐dwelling Hispanics/Latinos aged 18 to 74 years (n = 16,415) selected through a complex sampling design from households in four US field center locations (Chicago, IL; Miami, FL; Bronx, NY; San Diego, CA). Visit 1 of HCHS/SOL was completed between 2008 and 2011 and included assessment of neurocognitive function among adults ages 45 to 74 years (n = 9623). Details of the sampling design of HCHS/SOL, study scope, and cognitive tests included are published elsewhere. 11 , 12 Approximately 7 years after Visit 1 (2016–2018), a second neurocognitive assessment was obtained through the ancillary study of HCHS/SOL, SOL‐INCA (Visit 2). SOL‐INCA was designed to study the prevalence and determinants of neurocognitive decline and MCI prevalence in returning respondents ages ≥ 50 years.
RESEARCH IN CONTEXT
Systematic review: The authors reviewed the literature using traditional (e.g., PubMed) sources. Previous work has shown that using cluster‐analytic statistical techniques considerably improves cognitive characterizations and diagnostic accuracy during the early stages of Alzheimer's disease and related dementias (ADRD). These relevant studies are appropriately cited. Whether similar cognitive profiles emerge when using the same cluster‐analytic statistical methods with a more diverse Hispanic/Latino sample in as early as middle age and during the earliest stages of ADRD requires further investigation.
Interpretation: Findings provide evidence of heterogeneity in the cognitive profiles of a representative, community‐dwelling sample of diverse Hispanic/Latino adults, extending results from previous studies that used similar methods to characterize cognitive profiles among primarily non‐Hispanic White aging adults.
Future directions: Future directions for research include but are not limited to investigating how other longitudinal cognitive, functional, and clinical outcomes may differ across latent profile analysis–derived cognitive profiles in diverse Hispanic/Latino aging adults.
2.2. Neurocognitive function (SOL‐INCA Visit 2 only)
The neurocognitive battery was administered by trained bilingual staff in the participants’ preferred language (Spanish/English). The battery consisted of tests assessing (1) verbal memory (Brief Spanish‐English Verbal Learning Test [B‐SEVLT] Trials 1–3 and Recall), language (Word Fluency [WF] Letters F and A), processing speed (Digit Symbol Substitution [DSS] and Trail Making Test [TMT] Part A), and executive function (TMT Part B). The TMT was added to the Visit 2 neurocognitive battery; thus, the current study reflects a cross‐sectional analysis of neurocognitive data from Visit 2 only, in addition to baseline/Visit 1 demographic, sociocultural, and health‐related covariates. TMT Parts A and B were reverse coded so that higher values correspond with better performance and for ease of interpretation. Using a robust normative reference group (participants characterized as having typical physical and cognitive health per SOL‐INCA procedures 13 ), a regression model was fit for each Visit 2 cognitive test as a function of demographic variables (age, sex, educational status, language preference) and crystallized knowledge as measured by the National Institutes of Health Toolbox Picture Vocabulary Test. Regression coefficients (unstandardized coefficients [B]) and the standard error (SE) of the estimate values obtained from each regression model were used to generate predicted scores on each cognitive test, and residualized z scores were generated by subtracting predicted scores from observed scores and dividing by the model root mean square error.
2.3. Baseline/Visit 1 covariates
Primary latent profile analyses (LPAs) included the following covariates: (1) age (years); (2) sex (male, female); (3) education (less than high school, high school or equivalent, more than high school or equivalent); (4) Hispanic/Latino heritage (Central American, Cuban, Dominican, Mexican, Puerto Rican, South American, other/more than one); (5) acculturation, estimated using Short Acculturation Scale for Hispanics (SASH; language subscale) scores (with higher reported acculturation evidenced by higher SASH language scores); (6) cardiovascular risk, using 10‐year Framingham Cardiovascular Risk (FCR) scores (with higher cardiovascular risk evidenced by higher FCR scores); and (7) depression symptoms, using the Center for Epidemiologic Studies Depression Scale, 10‐item version (CESD‐10) scores (with higher self‐reported depression symptoms evidenced by higher CESD‐10 scores). Multiple demographic and sociocultural variables (age, sex, educational status, language preference) were accounted for in previous regressions conducted to generate residualized z scores on neurocognitive tests, which were subsequently entered as indicators in primary LPAs. To minimize potential circularity, LPAs included demographic/sociocultural variables as covariates relevant to the prediction, but not formal indicators, of latent profile membership.
We also accounted for contemporaneous limitations in daily function in primary LPAs. SOL‐INCA collected self‐reports of instrumental activities of daily living (IADLs) using seven component items probing ability to complete tasks related to telephone use, navigating within walking distance, shopping, meal preparation, housework, medication use, and finances. 14 , 15 Each probe was originally coded trichotomously (0 = without help, 1 = with some help, 2 = unable to perform at all). However, due to small sizes (e.g., fewer than 10 individuals in the target population [n = 6239] reported requiring some help or being unable to perform at all on four of the seven IADLs), “1” and “2” responses were recoded as “1” to indicate requiring any help on IADLs. Thus, IADLs were dichotomized (0 = without help; 1 = with any help), then a total score (range: 0–7) was generated for each individual, and the absence (total score = 0) versus presence (total score > 0) of limitations in IADLs was used as the IADL indicator in analyses.
2.4. Analytical subpopulation
SOL‐INCA enrolled 6377 eligible HCHS/SOL participants who had baseline/Visit 1 demographic, sociocultural, and other health data and were ≥ 50 years of age and completed neurocognitive assessments at Visit 2. We excluded 138 participants with missing values on any covariates of interest. The resulting analytical sample size was n = 6239.
2.5. Primary analyses
First, LPAs were fit to extract data‐driven classifications based on cognitive test performance and reported IADL functioning (Table 1). In line with standard practice, we iteratively fit a series of LPA models corresponding to two‐ to ten‐class solutions. For each derived class solution, we assessed absolute and relative model fit to the data using established indices (Akaike information criteria [AIC], Corrected Akaike information criteria [AICC], Bayesian information criteria [BIC], sample‐size‐adjusted BIC [aBIC]; Figure 1). Entropy values were also examined (values > 0.800 are generally accepted, and those < 0.600 are usually viewed as problematic). In addition to statistical fit assessment indices, consensus discussions (Graves, Tarraf, González) were used to decide on an acceptable number of, and labels for, clinically meaningful cognitive profiles. 16 , 17 We used full information maximum likelihood with robust standard errors to estimate all LPAs accounting for potential violations of normality assumptions in the measured cognitive tests and incorporating all available data. The distribution of cognitive tests across the best‐fitting solution are presented in Figure 2. Second, we generated weighted descriptive statistics to characterize the target population across the chosen latent profiles (Table 2). We used survey adjusted chi‐square tests for categorical variables, and survey adjusted F tests for continuous variables. Third, we fit multinomial logistic regressions to model the nominal latent profiles as a function of the covariates using the Higher Memory performance group (see section 3.1) as the referent group, given that memory is the domain typically affected earliest and most profoundly in AD. Relative risk ratios (RRs) and their 95% confidence intervals are presented in Table 3. We then estimated and plotted average marginal probabilities of classification into each of the latent cognitive profiles as a function of the model covariates (Figure 3). All analyses accounted for the complex design of SOL‐INCA and incorporated complex survey techniques to adjust for unequal probabilities of selection, clustering, and stratification. LPA models were fit in MPlus Version 8 and estimates were postprocessed using R. All other analyses were performed using survey functionalities in Stata 17.
TABLE 1.
Posterior probabilities of classification into latent cognitive profiles according to four‐, five‐, and six‐class solutions in the target population (n = 6239; participants who completed neurocognitive assessments at Visit 1 [HCHS/SOL; 2008–2011] and were ≥ 50 years of age at Visit 2 [SOL‐INCA; 2016–2018]).
| Four‐class solution | ||||||
|---|---|---|---|---|---|---|
| Column | ||||||
| 1 | 2 | 3 | 4 | |||
| 1 | 0.868 | 0.058 | 0.030 | 0.044 | ||
| 2 | 0.083 | 0.834 | 0.040 | 0.043 | ||
| 3 | 0.048 | 0.045 | 0.907 | 0.000 | ||
| 4 | 0.055 | 0.043 | 0.000 | 0.902 | ||
| Row | ||||||
| 1 | 2 | 3 | 4 | |||
| 1 | 0.871 | 0.055 | 0.025 | 0.049 | ||
| 2 | 0.086 | 0.824 | 0.034 | 0.057 | ||
| 3 | 0.057 | 0.051 | 0.892 | 0.000 | ||
| 4 | 0.050 | 0.033 | 0.000 | 0.917 | ||
| Five‐class solution | ||||||
| Column | ||||||
| 1 | 2 | 3 | 4 | 5 | ||
| 1 | 0.896 | 0.054 | 0.000 | 0.050 | 0.000 | |
| 2 | 0.024 | 0.862 | 0.044 | 0.046 | 0.025 | |
| 3 | 0.000 | 0.052 | 0.854 | 0.047 | 0.047 | |
| 4 | 0.038 | 0.086 | 0.055 | 0.821 | 0.000 | |
| 5 | 0.000 | 0.047 | 0.091 | 0.000 | 0.862 | |
| Row | ||||||
| 1 | 2 | 3 | 4 | 5 | ||
| 1 | 0.897 | 0.056 | 0.000 | 0.047 | 0.000 | |
| 2 | 0.024 | 0.874 | 0.037 | 0.046 | 0.019 | |
| 3 | 0.000 | 0.061 | 0.848 | 0.040 | 0.051 | |
| 4 | 0.040 | 0.087 | 0.063 | 0.810 | 0.000 | |
| 5 | 0.000 | 0.061 | 0.083 | 0.000 | 0.856 | |
| Six‐class solution | ||||||
| Column | ||||||
| 1 | 2 | 3 | 4 | 5 | 6 | |
| 1 | 0.847 | 0.040 | 0.074 | 0.036 | 0.000 | 0.004 |
| 2 | 0.068 | 0.871 | 0.002 | 0.058 | 0.001 | 0.000 |
| 3 | 0.058 | 0.002 | 0.805 | 0.051 | 0.047 | 0.037 |
| 4 | 0.041 | 0.025 | 0.071 | 0.825 | 0.038 | 0.000 |
| 5 | 0.000 | 0.000 | 0.060 | 0.037 | 0.858 | 0.045 |
| 6 | 0.002 | 0.000 | 0.058 | 0.001 | 0.076 | 0.863 |
| Row | ||||||
| 1 | 2 | 3 | 4 | 5 | 6 | |
| 1 | 0.822 | 0.034 | 0.097 | 0.046 | 0.000 | 0.001 |
| 2 | 0.077 | 0.861 | 0.006 | 0.056 | 0.000 | 0.000 |
| 3 | 0.044 | 0.000 | 0.837 | 0.048 | 0.043 | 0.026 |
| 4 | 0.031 | 0.026 | 0.078 | 0.825 | 0.040 | 0.001 |
| 5 | 0.000 | 0.000 | 0.067 | 0.035 | 0.850 | 0.047 |
| 6 | 0.005 | 0.000 | 0.082 | 0.000 | 0.070 | 0.843 |
FIGURE 1.
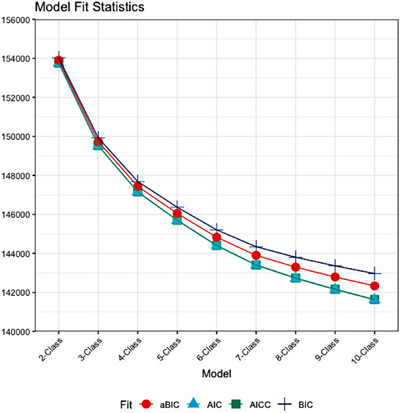
Standard fit assessment indices corresponding to two‐ to ten‐class estimated latent models fit to extract data‐driven phenotypes based on cognitive profiles and including a binary measure of IADL dysfunction. Study sample includes n = 6239 participants who completed neurocognitive assessments at Visit 1 (HCHS/SOL; 2008–2011) and were ≥ 50 years of age at Visit 2 (SOL‐INCA; 2016–2018). AIC, Akaike information criteria; AICC, finite sample corrected Akaike information criteria; aBIC, adjusted Bayesian information criteria; BIC, Bayesian information criteria; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; IADL, instrumental activities of daily living; SOL‐INCA, Study of Latinos–Investigation of Neurocognitive Aging
FIGURE 2.
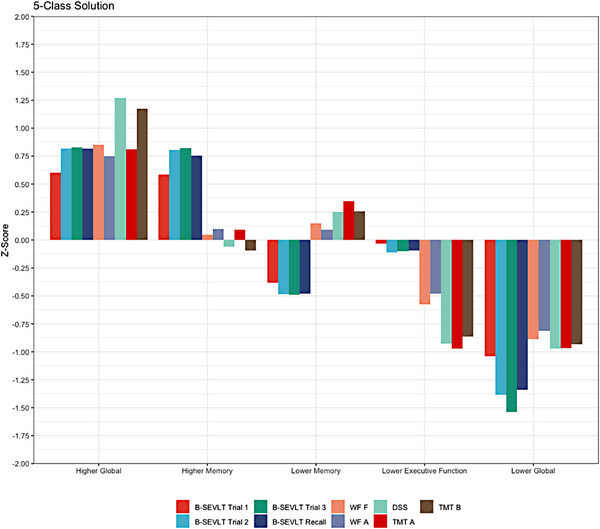
Average performance (demographically adjusted z scores) on cognitive tests across latent cognitive profiles (best‐fitting, five‐class solution derived from LPA: 1 Higher Global [13.8%]; 2 Higher Memory [24.6%]; 3 Lower Memory [32.8%]; 4 Lower Executive Function [16.6%]; and 5 Lower Global [12.1%]) in the study sample (n = 6239 participants who completed neurocognitive assessments at Visit 1 [HCHS/SOL; 2008–2011] and were ≥ 50 years of age at Visit 2 [SOL‐INCA; 2016–2018]). B‐SEVLT, Brief Spanish English verbal learning test; DSS, Digit Symbol Substitution; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; LPA, latent profile analysis; TMT, Trail Making Test; SOL‐INCA, Study of Latinos–Investigation of Neurocognitive Aging; WF, word fluency
TABLE 2.
Descriptive characteristics of target population (n = 6239 participants who completed neurocognitive assessments at Visit 1 [HCHS/SOL; 2008–2011] and were ≥ 50 years of age at Visit 2 [SOL‐INCA; 2016–2018]) across latent cognitive profiles (best‐fitting, five‐class solution derived from LPA: 1 Higher Global [13.8%]; 2 Higher Memory [24.6%]; 3 Lower Memory [32.8%]; 4 Lower Executive Function [16.6%]; and 5 Lower Global [12.1%]). Survey adjusted chi‐square tests were used for categorical variables, and survey adjusted F tests for continuous variables.
| Total (n = 6239) | Higher Global (n = 863) | Higher Memory (n = 1534) | Lower Memory (n = 2048) | Lower Executive Function (n = 1037) | Lower Global (n = 757) | P value | |
|---|---|---|---|---|---|---|---|
| Sex % (SE) | |||||||
| Female | 54.56 (0.84) | 57.71 (2.64) | 54.49 (1.75) | 52.37 (1.50) | 55.25 (2.31) | 55.96 (2.72) | P = 0.462 |
| Male | 45.44 (0.84) | 42.29 (2.64) | 45.51 (1.75) | 47.63 (1.50) | 44.75 (2.31) | 44.04 (2.72) | |
| Education % (SE) | |||||||
| Less than high school | 38.38 (1.07) | 41.26 (2.43) | 36.18 (2.05) | 35.45 (1.52) | 44.01 (2.60) | 39.34 (2.59) | P = 0.028 |
| High school | 21.12 (0.76) | 19.58 (1.76) | 20.33 (1.60) | 22.96 (1.29) | 21.72 (2.14) | 18.92 (1.94) | |
| More than high school | 40.50 (1.00) | 39.16 (2.27) | 43.49 (1.94) | 41.59 (1.62) | 34.28 (2.27) | 41.73 (2.79) | |
| Background % (SE) | |||||||
| Central American | 7.19 (0.56) | 3.55 (0.65) | 9.21 (1.05) | 4.95 (0.56) | 12.03 (1.47) | 6.61 (1.22) | <0.0001 |
| Cuban | 25.89 (1.89) | 17.67 (2.31) | 29.51 (2.74) | 23.02 (2.23) | 28.92 (2.68) | 30.79 (2.98) | |
| Dominican | 9.38 (0.77) | 2.55 (0.78) | 7.96 (1.03) | 7.67 (0.84) | 15.72 (1.74) | 14.72 (1.98) | |
| Mexican | 33.23 (1.68) | 42.42 (2.96) | 35.77 (2.53) | 36.11 (1.97) | 26.72 (2.65) | 21.08 (2.43) | |
| Puerto Rican | 15.38 (0.83) | 22.28 (2.01) | 6.97 (0.81) | 20.71 (1.35) | 9.00 (1.17) | 18.23 (1.87) | |
| South American | 5.18 (0.39) | 4.77 (0.90) | 7.31 (0.82) | 5.13 (0.62) | 3.52 (0.53) | 4.09 (0.92) | |
| Other/More than one | 3.76 (0.45) | 6.76 (1.58) | 3.27 (0.83) | 2.42 (0.51) | 4.09 (1.19) | 4.47 (1.47) | |
| IADL % (SE) | |||||||
| No IADL | 96.72 (0.38) | 98.54 (0.63) | 98.86 (0.52) | 98.85 (0.28) | 95.06 (0.90) | 88.25 (1.75) | <0.0001 |
| Any IADL | 3.28 (0.38) | 1.46 (0.63) | 1.14 (0.52) | 1.15 (0.28) | 4.94 (0.90) | 11.75 (1.75) | |
| Baseline age (mean [SD]) | 56.36 (8.09) | 55.50 (7.85) | 56.01 (8.04) | 55.73 (7.93) | 56.64 (8.19) | 58.93 (8.04) | <0.0001 |
| Baseline SASH (mean [SD]) | 1.72 (0.95) | 2.36 (1.25) | 1.53 (0.78) | 1.88 (1.02) | 1.37 (0.56) | 1.46 (0.66) | <0.0001 |
| Baseline FCR (mean [SD]) | 0.16 (0.14) | 0.14 (0.12) | 0.15 (0.12) | 0.15 (0.13) | 0.17 (0.14) | 0.21 (0.15) | <0.0001 |
| Baseline CESD‐10 (mean [SD]) | 7.38 (6.29) | 6.80 (6.06) | 6.82 (6.12) | 7.06 (6.12) | 7.98 (6.46) | 8.94 (6.52) | <0.0001 |
Abbreviations: CESD‐10, Center for Epidemiologic Studies Depression Scale, 10‐item version; FCR, Framingham Cardiovascular Risk; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; IADL, instrumental activities of daily living; LPA, latent profile analysis; SASH, Short Acculturation Scale for Hispanics (Language subscale); SD, standard deviation; SE, standard error; SOL‐INCA, Study of Latinos–Investigation of Neurocognitive Aging.
TABLE 3.
Adjusted associations of demographic, sociocultural, and health factors with latent cognitive profiles (best‐fitting, five‐class solution derived from LPA: 1 Higher Global [13.8%]; 2 Higher Memory [24.6%]; 3 Lower Memory [32.8%]; 4 Lower Executive Function [16.6%]; and 5 Lower Global [12.1%]) in the target population (n = 6239; participants who completed neurocognitive assessments at Visit 1 [HCHS/SOL; 2008–2011] and were ≥ 50 years of age at Visit 2 [SOL‐INCA; 2016–2018]). Results are based on survey multinomial logistic regression models using the LPA‐derived High Memory group as the referent group.
| RR [95% CI] | |||
|---|---|---|---|
| M1 | M2 | M3 | |
| Higher Global (ref: Higher Memory) | |||
| Age | 0.99 [0.98; 1.01] | 0.99 [0.97; 1.01] | 1.00 [0.98; 1.02] |
| Male (vs. female) | 0.88 [0.67; 1.16] | 0.66* [0.47; 0.93] | |
| High school (vs. LTHS) | 0.83 [0.57; 1.20] | 0.71 [0.48; 1.04] | |
| More than high school (vs. LTHS) | 0.78 [0.58; 1.04] | 0.51*** [0.38; 0.69] | |
| Central American | 0.39*** [0.24; 0.62] | ||
| Cuban (vs. Mexican) | 0.78 [0.53; 1.15] | ||
| Dominican (vs. Mexican) | 0.32*** [0.17; 0.63] | ||
| Puerto Rican (vs. Mexican) | 1.29 [0.86; 1.93] | ||
| South American (vs. Mexican) | 0.75 [0.46; 1.23] | ||
| Other/more than one (vs. Mexican) | 1.26 [0.53; 2.97] | ||
| Any IADL (vs. no IADL) | 1.18 [0.33; 4.22] | ||
| SASH | 2.31*** [1.95; 2.74] | ||
| FCR | 1.22 [0.27; 5.48] | ||
| CESD‐10 | 0.98* [0.95; 1.00] | ||
| Lower Memory (ref: Higher Memory) | |||
| Age | 1.00 [0.98; 1.01] | 1.00 [0.98; 1.01] | 0.99 [0.97; 1.01] |
| Male (vs. female) | 1.08 [0.90; 1.30] | 0.92 [0.73; 1.14] | |
| High school (vs. LTHS) | 1.13 [0.87; 1.48] | 1.10 [0.84; 1.44] | |
| More than high school (vs. LTHS) | 0.97 [0.76; 1.23] | 0.90 [0.70; 1.15] | |
| Central American | 0.56*** [0.39; 0.78] | ||
| Cuban (vs. Mexican) | 0.85 [0.64; 1.13] | ||
| Dominican (vs. Mexican) | 1.01 [0.72; 1.41] | ||
| Puerto Rican (vs. Mexican) | 2.15*** [1.54; 3.00] | ||
| South American (vs. Mexican) | 0.76 [0.54; 1.07] | ||
| Other/more than one (vs. Mexican) | 0.62 [0.32; 1.20] | ||
| Any IADL (vs. No IADL) | 0.96 [0.34; 2.69] | ||
| SASH | 1.42*** [1.22; 1.64] | ||
| FCR | 2.29 [0.69; 7.56] | ||
| CESD‐10 | 1.00 [0.98; 1.01] | ||
| Lower Executive Function (ref: Higher Memory) | |||
| Age | 1.01 [0.99; 1.03] | 1.01 [0.99; 1.03] | 0.99 [0.97; 1.01] |
| Male (vs. female) | 0.98 [0.78; 1.24] | 0.93 [0.71; 1.22] | |
| High school (vs. LTHS) | 0.90 [0.65; 1.25] | 0.99 [0.71; 1.38] | |
| More than high school (vs. LTHS) | 0.66** [0.51; 0.86] | 0.80 [0.62; 1.04] | |
| Central American | 1.67** [1.14; 2.44] | ||
| Cuban (vs. Mexican) | 1.15 [0.81; 1.64] | ||
| Dominican (vs. Mexican) | 2.55*** [1.70; 3.82] | ||
| Puerto Rican (vs. Mexican) | 2.06** [1.29; 3.30] | ||
| South American (vs. Mexican) | 0.69 [0.45; 1.06] | ||
| Other/More than one (vs. Mexican) | 1.86 [0.80;4.36] | ||
| Any IADL (vs. no IADL) | 3.58** [1.45; 8.80] | ||
| SASH | 0.68*** [0.55; 0.83] | ||
| FCR | 5.20** [1.76; 15.37] | ||
| CESD‐10 | 1.02* [1.00; 1.04] | ||
| Lower Global (ref: Higher Memory) | |||
| Age | 1.04*** [1.03; 1.06] | 1.04*** [1.03; 1.06] | 1.01 [0.99; 1.04] |
| Male (vs. gemale) | 0.97 [0.76; 1.24] | 0.87 [0.67; 1.12] | |
| High school (vs. LTHS) | 0.96 [0.68; 1.37] | 1.11 [0.76; 1.61] | |
| More than high school (vs. LTHS) | 0.96 [0.72; 1.28] | 1.29 [0.95; 1.75] | |
| Central American | 1.06 [0.67; 1.68] | ||
| Cuban (vs. Mexican) | 1.15 [0.79; 1.67] | ||
| Dominican (vs. Mexican) | 2.84*** [1.94; 4.17] | ||
| Puerto Rican (vs. Mexican) | 4.30*** [2.75; 6.71] | ||
| South American (vs. Mexican) | 0.87 [0.50; 1.53] | ||
| Other/More than one (vs. Mexican) | 2.02 [0.83; 4.93] | ||
| Any IADL (vs. no IADL) | 8.03*** [3.05;21.13] | ||
| SASH | 0.72** [0.58; 0.89] | ||
| FCR | 7.64*** [2.51; 23.24] | ||
| CESD‐10 | 1.04*** [1.02; 1.06] | ||
Abbreviations: CESD‐10, Center for Epidemiologic Studies Depression Scale, 10‐item version; CI, confidence interval; FCR, Framingham Cardiovascular Risk; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; LPA, latent profile analysis; LTHS, less than high school; IADL, instrumental activities of daily living; RR, relative risk ratio; SASH, Short Acculturation Scale for Hispanics (Language subscale); SOL‐INCA, Study of Latinos–Investigation of Neurocognitive Aging.
FIGURE 3.
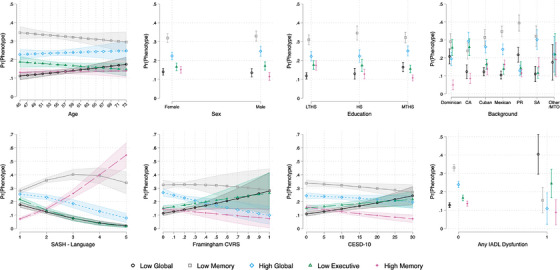
Average marginal probability estimates for the latent cognitive profiles (best‐fitting, five‐class solution derived from LPA: 1 Higher Global [13.8%]; 2 Higher Memory [24.6%]; 3 Lower Memory [32.8%]; 4 Lower Executive Function [16.6%]; and 5 Lower Global [12.1%]) as a function of demographic, sociocultural, and health‐related covariables in the study sample (n = 6239 participants who completed neurocognitive assessments at Visit 1 [HCHS/SOL; 2008–2011] and were ≥ 50 years of age at Visit 2 [SOL‐INCA; 2016–2018]). Post hoc estimates of marginal probabilities are derived from survey multinomial logistic regression models. CA, Central American; CESD‐10, Center for Epidemiologic Studies Depression Scale, 10‐item version; FCR, Framingham Cardiovascular Risk; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; HS, high school or equivalent; IADL, instrumental activities of daily living; LTHS, less than high school; MTHS, more than high school or equivalent; PR, Puerto Rican; SOL‐INCA, Study of Latinos–Investigation of Neurocognitive Aging; SA, South American; SASH, Short Acculturation Scale for Hispanics
3. RESULTS
Overall, the average baseline age in the target population was 56.4 years, slightly more than half were women (54.6%), and 38.4% reported less than a high school education. Mexican heritage had the most representation (33.2%). The baseline average SASH language score was 1.7 (standard deviation [SD] = 1.0), suggesting relatively lower acculturation overall; FCR score was 0.2 (SD = 0.1), suggesting relatively lower cardiovascular risk overall; CESD‐10 score was 7.4 (SD = 6.3), suggesting relatively lower depression symptoms overall; and 3.3% reported any IADL dysfunction.
3.1. Latent cognitive profiles
The five‐class solution provided optimal fit determined by the attenuation in relative and absolute fit criteria as well as clinical interpretability relative to other profile solutions (Figure 1). The five profiles were labeled as: (1) Higher Global (13.8%); (2) Higher Memory (24.6%); (3) Lower Memory (32.8%); (4) Lower Executive Function (16.6%); and (5) Lower Global (12.1%) performance groups (Figure 2). Descriptors were chosen to reflect observed scores or levels of performance within respective domains (high average = zs ≥ 0.5; average = zs −0.5 to 0.5; low average = zs −1.0 to −0.5; mildly impaired = zs ≤ −1.0), without necessarily implying the broader presence versus absence of “impairment” in these domains. 18 Relatedly, it is important to reiterate that the target population in this study consists largely of Hispanic/Latino adults who are cognitively unimpaired and/or in the preclinical or MCI stages of ADRD, and that “higher” and “lower” scores/performances are therefore relative to a robust normative reference group within the SOL‐INCA cohort that includes participants characterized as having typical physical and cognitive health per SOL‐INCA procedures.
The five‐class solution provided incremental utility over the four‐class solution by yielding an additional group that was clinically meaningful. Specifically, while the four‐class solution included a group of individuals who exhibited cognitively normal performance more broadly, the five‐class solution consisted of a Higher Memory performance group that was distinct from a Higher Global performance group. However, the six‐class solution did not appear to have incremental utility over the five‐class solution. Specifically, the six‐class solution consisted of a new group representing ≈ 27% of the target population and demonstrating cognitively normal performance broadly but with notable heterogeneity upon closer inspection. Entropy values for all examined class solutions were in the 0.75 to 0.80 range. Ultimately, the five‐class solution was retained and exhibited posterior probabilities values of ≥ 0.81 (Table 1).
The Higher Global group performed in the average‐to‐high‐average range (observed zs ≥ 0.5) across all cognitive and IADL tests, particularly those of executive function (TMT Part B) and processing speed (DSS). The Higher Memory group performed in the average range (observed zs = ≈ 0 to 1.0) across all cognitive/IADL tests, but exhibited relatively higher performance (observed zs = 0.5 to 1.0) on memory tests. The Lower Memory group performed in the average range (observed zs = −0.5 to 0.5) across all cognitive/IADL tests, but exhibited relatively lower performance (observed zs = ≈ −0.5) on memory tests (B‐SEVLT). The Lower Executive Function group performed in the average‐to‐low‐average range (observed zs = −1.0 to 0) across all cognitive/IADL tests, but exhibited relatively lower performance (observed zs = ≈ −1.0) on executive function and processing speed tests (DSS and TMT Parts A and B). Finally, the Lower Global group performed in the low‐average‐to‐mildly impaired range (observed zs = ≈ −1.5 to −1.0) across all cognitive/IADL tests.
3.2. Descriptive characteristics of the target population by latent cognitive profiles
In the Higher Global performance group, Cubans were underrepresented, and Mexicans and Puerto Ricans were overrepresented (P < 0.0001). Individuals in the Higher Global performance group were also slightly younger, reported higher acculturation, and had lower cardiovascular risk and self‐reported depression symptoms. The Lower Executive Function performance group had a higher proportion of individuals with less than high school education (P = 0.028). Finally, the Lower Global performance group had a higher representation of Cuban heritage, slightly higher average age, and higher cardiovascular risk, self‐reported depression symptoms, and reported IADL dysfunction.
3.3. Adjusted associations of target population characteristics with latent cognitive profiles (Higher Memory performance as referent group)
In the fully covaried multinomial logit model, and with the Higher Memory performance group as the referent group, the following was observed.
3.3.1. Higher global performance group
Individuals with higher reported acculturation had a higher RR for being in the Higher Global performance group. However, male (vs. female) individuals, those with more than a high school education (vs. less than a high school education), Central Americans and Dominicans (vs. Mexicans), and individuals with higher self‐reported depression symptoms had a lower RR for being in this group.
3.3.2. Lower Memory performance group
Puerto Ricans (vs. Mexicans) and individuals with higher reported acculturation had a higher RR for being in the Lower Memory performance group. However, Central Americans (vs. Mexicans) had a lower RR for being in this group.
3.3.3. Lower Executive Function performance group
Central Americans, Dominicans, and Puerto Ricans (vs. Mexicans), and individuals with higher cardiovascular risk, higher self‐reported depression symptoms, and reported IADL dysfunction had a higher RR for being in the Lower Executive Function performance group. However, individuals with higher reported acculturation had a lower RR for being in this group.
3.3.4. Lower Global performance group
Dominicans and Puerto Ricans (vs. Mexicans), and individuals with higher cardiovascular risk, higher self‐reported depression symptoms, and reported IADL dysfunction had a higher RR for being in the Lower Global performance group. However, individuals with higher reported acculturation had a lower RR for being in this group.
Table S1 in supporting information includes descriptive statistics for performance on neurocognitive tests by latent cognitive profile and Hispanic/Latino heritage.
4. DISCUSSION
Among middle‐aged and older Hispanic/Latino adults in the SOL‐INCA cohort, our analysis combined with clinical interpretation suggested five cognitive profiles: (1) a Higher Global group performing in the average‐to‐high‐average range across all cognitive and IADL tests (13.8%); (2) a Higher Memory group performing in the average range across all cognitive/IADL tests, but with relatively high performance on memory tests (24.6%); (3) a Lower Memory group performing in the average range across all cognitive/IADL tests, but with relatively low performance on memory tests (32.8%); (4) a Lower Executive Function group performing in the average‐to‐low‐average range across all cognitive/IADL tests, but with relatively low performance on executive function and processing speed tests (16.6%); and (5) a Lower Global group performing in the low‐average‐to‐mildly impaired range across all cognitive/IADL tests (12.1%). Our findings provide evidence of heterogeneity in the cognitive profiles of middle‐aged and older Hispanic/Latino adults, extending results from previous studies that also used cluster‐analytic statistical methods to characterize cognitive profiles among aging adults. Previous studies reported that empirically derived cognitive profiles may be useful for predicting incident AD among primarily non‐Hispanic White adults. 4 , 6 Our findings similarly provide important tools for predicting ADRD among diverse Hispanic/Latino adults and outline the relative strengths and weaknesses inherent in cognitive performance for aging Hispanics/Latinos.
Most prior studies (1) used convenience, non‐representative samples that were heavily represented by older, non‐Hispanic White individuals and (2) restricted analyses to participants preclassified as having MCI. However, it is difficult to directly compare the LPA‐derived cognitive profiles between those observed in previous studies and ours given differences not only in the demographic makeup across the study samples (based on age, ethnoracial background), whether preassigned MCI classifications were considered, and statistical methods used, but in neurocognitive test batteries used. The SOL‐INCA neurocognitive battery does not include a measure of naming; thus, our LPA is inherently unable to produce a dysnomic group. Moreover, the target population of the current study was not restricted to individuals meeting MCI criteria. Thus, the present results must be interpreted with the understanding that our study includes middle‐aged and older Hispanic/Latino adults with a more diverse range of neurocognitive function (largely cognitively healthy or mildly impaired) compared to samples used in previous studies. One prior study did investigate cognitive profiles of a diverse group of community‐dwelling older adults without dementia (only 40% non‐Hispanic White and only 15% Hispanic/Latino) using LPA; 9 it resulted in similar LPA‐derived cognitive profiles despite differing neurocognitive tests, suggesting that our results reflect important distinctions in cognitive characterizations for (largely) cognitively healthy older adults. Importantly, we suspect that a portion of our study sample, given its younger average age, includes some Hispanic/Latino adults in the preclinical stage of ADRD, and that the LPA‐derived cognitive profiles accordingly may depict some of the earliest changes that portend impending disease in this population.
Some qualitatively meaningful similarities between our class solution and those reported in previous large‐scale epidemiological studies are worth noting. First, our Lower Memory group aligns most closely with previously described amnestic groups. 6 , 7 , 8 However, our Lower Memory group exhibited a relative weakness in memory, not a substantial impairment or deficit based on conventional standards. Second, our LPA yielded a Lower Executive Function performance group perhaps most analogous to previously described dysexecutive groups, although our group had a relative weakness (not impairment) in executive function. Our Lower Global performance group also exhibited low average (but not impaired) executive function performance within the context of low‐average‐to‐mildly impaired memory performance. Some other notable distinctions between our results and those from the previous studies include the presence of Higher Memory and Higher Global performance groups. Together, our analysis describes a nuanced constellation of cognitive profiles that warrant close attention in efforts to better understand the early neurocognitive changes of ADRD in the aging Hispanic/Latino population. Given the emergence of two distinct, memory‐related (Lower Memory and Higher Memory) profiles, the present results extend previous findings showing that memory tests may be particularly useful for detecting neurocognitive changes in early stages of ADRD. 19 , 20
We also investigated adjusted associations of demographic, sociocultural, and health‐related factors with LPA‐derived cognitive profiles using the Higher Memory performance group as the referent group. Higher acculturation was generally associated with higher classification in higher performing groups and lower chances of classification in lower performing groups. In contrast, higher cardiovascular risk and depression symptoms were generally associated with higher chances of classification in lower performing groups. Taken together, higher acculturation may serve as a protective factor, while higher cardiovascular burden and depressive symptomatology may serve as risk factors, for cognitive profiles among diverse, aging Hispanic/Latino adults. However, these findings were based on examination of within‐group differences on demographic, sociocultural, and health‐related characteristics, although it is worth nothing that differences across latent cognitive profiles on age, education, acculturation, CVD risk, depression, and IADLs were observed (see Table 2). Future work by our group will directly and more comprehensively examine potential differences across latent cognitive profiles to further investigate and identify risk and protective factors for profiles associated with ADRD risk in diverse, aging Hispanics/Latinos.
Chances of classification in LPA‐derived cognitive groups also differed by Hispanic/Latino background. However, these findings are likely better explained by differences in other sociocultural or health‐related factors that were not fully captured in present analyses. Previous work suggests education influences some of the neurocognitive differences observed among Hispanic/Latino groups. 21 , 22 Neurocognitive differences were observed across Hispanic/Latino backgrounds in the present study even after statistical adjustment for educational status and other demographic/sociocultural covariates. However, there is high variability in educational quality among ethnoracial minority groups in the United States, and adjusting for educational status alone may be insufficient to control for education effects. Accounting for more precise measures of educational quality is needed in future work.
Our study has several strengths. It is the first to use LPA to characterize heterogeneous cognitive profiles in a large, representative, well‐characterized community‐dwelling sample of diverse middle‐aged and older Hispanic/Latino adults. Additional strengths include the availability and use of SOL‐INCA neurocognitive measures developed for Hispanic/Latino samples, and of regression‐based norming of cognitive test scores to adjust for demographic/sociocultural factors. However, the present study is not free of limitations. While the analysis accounted for acculturation, there was no direct examination of potential distinctions among LPA‐derived groups in preferred language of testing. Given that the LPA‐derived groups are cognitively based and the role of language in neurocognitive testing, this is a notable limitation and important focus of future investigation. Additionally, the underlying mechanisms that may be driving these cognitive profiles were not directly examined. Work within HCHS/SOL and elsewhere suggests that other acculturation‐related variables beyond language preference 23 , 24 and additional social determinants of health that are known to influence cognitive performance generally, 25 may also be influencing the observed cognitive profiles. Moreover, there was an average difference of 7 years between baseline and SOL‐INCA visits, and we acknowledge that demographic, sociocultural, and health‐related covariates may have changed during that time. Furthermore, it is important to note that to avoid confounding with other formally established preclinical or MCI criteria, our LPA classifications were based on objective cognitive performance only, with the goal of helping us to understand and characterize the cognitive vulnerabilities that exist within the aging Hispanic/Latino population. That said, the LPA‐derived profiles in the present study should not necessarily serve or be interpreted as proxies for clinically validated subtypes of MCI or preclinical ADRD. More work is needed to determine how the LPA‐derived cognitive profiles observed in the present study may portend risk for mild or major neurocognitive disorders due to ADRD in the Hispanic/Latino population. Additional future directions for research include examining the impact of various norming procedures on class solutions, assessing the stability of our LPA‐derived class solutions over time, and exploring whether empirically derived cognitive profiles have differential probabilities of progression toward different types of dementia.
In sum, our findings bolster ongoing efforts to improve our understanding of cognitive changes along the ADRD continuum for Hispanic/Latino adults. Notably, the present study and future, related investigations reflect important efforts to address our nation's identified priority of improving ADRD assessment tools and analytic methods to enhance the generalizability and equity of scientific research in AD/ADRD.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest. Author disclosures are available in the supporting information.
Supporting information
Supporting Information
Supporting Information
ACKNOWLEDGMENTS
The authors thank the staff and participants of the HCHS/SOL for their important contributions. A complete list of staff and investigators has been provided by Sorlie et al. 12 and is also available on the study website: http://www.cscc.unc.edu/hchs/. The HCHS/SOL was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01‐HC65233), University of Miami (N01‐HC65234), Albert Einstein College of Medicine (N01‐HC65235), Northwestern University (N01‐HC65236), and San Diego State University (N01‐HC65237). The SOL‐INCA received support from the National Institute on Aging (R01 AG075758). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: the National Center on Minority Health and Health Disparities, the National Institute of Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements.
Graves LV, Tarraf W, Gonzalez K, et al. Characterizing cognitive profiles in diverse middle‐aged and older Hispanics/Latinos: Study of Latinos‐Investigation of Neurocognitive Aging (HCHS/SOL). Alzheimer's Dement. 2024;16:e12592. 10.1002/dad2.12592
REFERENCES
- 1. Matthews KA, Xu W, Gaglioti AH, et al. Racial and ethnic estimates of Alzheimer's disease and related dementias in the United States (2015‐2060) in adults aged ≥65 years. Alzheimers Dement. 2019;15(1):17‐24. doi: 10.1016/j.jalz.2018.06.3063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Colby SandraL, Ortman JenniferM. Projections of the Size and Composition of the U.S. Population: 2014 to 2060. Current Population Reports. P25‐1143, U.S. Census Bureau; 2014. [Google Scholar]
- 3. Chin AL, Negash S, Hamilton R. Diversity and disparity in dementia. Alzheimer Dis Assoc Disord. 2011;25(3):187‐195. doi: 10.1097/wad.0b013e318211c6c9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clark LR, Delano‐Wood L, Libon DJ, et al. Are empirically‐derived subtypes of mild cognitive impairment consistent with conventional subtypes? J Int Neuropsychol Soc. 2013;19(6):635‐645. doi: 10.1017/s1355617713000313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Libon DJ, Xie SX, Eppig J, et al. The heterogeneity of mild cognitive impairment: a neuropsychological analysis. J Int Neuropsychol Soc. 2009;16(1):84‐93. doi: 10.1017/s1355617709990993 [DOI] [PubMed] [Google Scholar]
- 6. Edmonds EC, Delano‐Wood L, Clark LR, et al. Susceptibility of the conventional criteria for mild cognitive impairment to false‐positive diagnostic errors. Alzheimers Dement. 2014;11(4):415‐424. doi: 10.1016/j.jalz.2014.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Eppig JS, Edmonds EC, Campbell L, Sanderson‐Cimino M, Delano‐Wood L, Bondi MW. Statistically derived subtypes and associations with cerebrospinal fluid and genetic biomarkers in mild cognitive impairment: a latent profile analysis. J Int Neuropsychol Soc. 2017;23(7):564‐576. doi: 10.1017/s135561771700039x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Machulda MM, Lundt ES, Albertson SM, et al. Neuropsychological subtypes of incident mild cognitive impairment in the Mayo Clinic Study of Aging. Alzheimers Dement. 2019;15(7):878‐887. doi: 10.1016/j.jalz.2019.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lamar M, Drabick D, Boots EA, et al. Latent profile analysis of cognition in a non‐demented diverse cohort: a focus on modifiable cardiovascular and lifestyle factors. J Alzheimer's Dis. 2021;82(4):1833‐1846. doi: 10.3233/jad-210110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ganguli M, Snitz BE, Saxton JA, et al. Outcomes of mild cognitive impairment by definition: a population study. Arch Neurol. 2011;68(6):761‐767. doi: 10.1001/archneurol.2011.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. LaVange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the hispanic community health study/study of latinos. Ann Epidemiol. 2010;20(8):642‐649. doi: 10.1016/j.annepidem.2010.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sorlie PD, Avilés‐Santa LM, Wassertheil‐Smoller S, et al. Design and implementation of the hispanic community health study/study of latinos. Ann Epidemiol. 2010;20(8):629‐641. doi: 10.1016/j.annepidem.2010.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. González HM, Tarraf Wassim, Schneiderman N, et al. Prevalence and correlates of mild cognitive impairment among diverse Hispanics/Latinos: study of Latinos‐Investigation of Neurocognitive Aging results. Alzheimers Dement. 2019;15(12):1507‐1515. doi: 10.1016/j.jalz.2019.08.202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fillenbaum GG. Multidimensional Functional Assessment of Older Adults the Duke Older Americans Resources and Services Procedures. Psychology Press; 2013. [Google Scholar]
- 15. Lawton MP, Moss M, Fulcomer M, Kleban MH. A Research and service oriented multilevel assessment instrument. J Gerontol. 1982;37(1):91‐99. doi: 10.1093/geronj/37.1.91 [DOI] [PubMed] [Google Scholar]
- 16. Weller BE, Bowen NK, Faubert SJ. Latent class analysis: a guide to best practice. J Psychol. 2020;46(4):287‐311. doi: 10.1177/0095798420930932 [DOI] [Google Scholar]
- 17. Spurk D, Hirschi A, Wang M, Valero D, Kauffeld S. Latent profile analysis: a review and “how to” guide of its application within vocational behavior research. J Vocat Behav. 2020;120:103445. doi: 10.1016/j.jvb.2020.103445 [DOI] [Google Scholar]
- 18. Guilmette TJ, Sweet JJ, Hebben N, et al. American Academy of Clinical Neuropsychology consensus conference statement on uniform labeling of performance test scores. Clin Neuropsychol. 2020;34(3):437‐453. doi: 10.1080/13854046.2020.1722244 [DOI] [PubMed] [Google Scholar]
- 19. Thomas KR, Eppig J, Edmonds EC, et al. Word‐list intrusion errors predict progression to mild cognitive impairment. Neuropsychology. 2018;32(2):235‐245. doi: 10.1037/neu0000413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Thomas KR, Edmonds EC, Eppig J, Salmon DP, Bondi MW. Using neuropsychological process scores to identify subtle cognitive decline and predict progression to mild cognitive impairment. J Alzheimer's Dis. 2018;64(1):195‐204. doi: 10.3233/jad-180229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. González HM, Tarraf W, Gouskova N, et al. Neurocognitive function among middle‐aged and older Hispanic/Latinos: results from the Hispanic community health study/study of Latinos. Arch Clin Neuropsychol. 2014;30(1):68‐77. doi: 10.1093/arclin/acu066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tarraf W, Kaplan R, Daviglus M. Cardiovascular risk and cognitive function in middle‐aged and older Hispanics/Latinos: results from the Hispanic community health study/study of Latinos (HCHS/SOL). J Alzheimer's Dis. 2020;73(1):103‐116. doi: 10.3233/jad-190830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Muñoz E, Gallo LC, Hua S, et al. Stress is associated with neurocognitive function in Hispanic/Latino adults: results from HCHS/SOL Socio‐Cultural Ancillary Study. J Gerontol Ser B. 2019. doi: 10.1093/geronb/gbz144. Published online November 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vásquez PM, Tarraf W, Doza A, et al. The cross‐sectional association of cognitive stimulation factors and cognitive function among Latino adults in Hispanic Community Health Study/Study of Latinos (HCHS/SOL). TRCI. 2019;5(1):533‐541. doi: 10.1016/j.trci.2019.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lamar M, Barnes LL, Leurgans SE. Acculturation in context: the relationship between acculturation and socioenvironmental factors with level of and change in cognition in older latinos. J Gerontol Ser B. 2020;76(4):e129‐e139. doi: 10.1093/geronb/gbaa156 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information
Supporting Information


