Abstract
Background:
More than 700,000 people in the United States undergo total knee arthroplasty (TKA) each year. Chronic venous insufficiency (CVI) affects 5% to 30% of adults, sometimes resulting in leg ulceration. These CVI cases in TKAs have been associated with worse outcomes; however, we found no study differentiating CVI severity.
Methods:
This retrospective study analyzed TKA outcomes at one institution from 2011 to 2021 using patient-specific codes. Analyses included short-term complications (< 90 days postoperative), long-term complications (< 2 years), and CVI status (yes/no; simple/complex/unclassified). Complex CVI consisted of pain, ulceration, inflammation, and/or other complications. Revisions within 2 years and readmissions within 90 days post-TKA were assessed. Composite complications included short-term and long-term complications, revisions, and readmissions. Multivariable logistic regressions predicted complication (any/long/short) as a function of CVI status (yes/no; simple/complex) and potential confounding variables. Of 7,665 patients, 741 (9.7%) had CVI. Among CVI patients, 247 (33.3%) had simple CVI, 233 (31.4%) had complex CVI, and 261 (35.2%) had unclassified CVI.
Results:
There was no difference in CVI versus control in composite complications (P = .722), short-term complications (P = .786), long-term complications (P = .15), revisions (P = .964), or readmissions (P = .438) postadjustment. Composite complication rates were 14.0% without CVI, 16.7% with complex CVI, and 9.3% with simple CVI. Complication rates differed between simple and complex CVI (P = .035).
Conclusion:
Overall, CVI did not affect postoperative complications versus control. Patients who have complex CVI are at higher risk for post-TKA complications compared to those who have simple CVI.
Keywords: CVI, TKA, arthroplasty outcomes, arthroplasty complications, postoperative complications, readmission, severity
More than 700,000 people in the United States undergo total knee arthroplasty (TKA) each year [1]. Projections indicate that the utilization rate of this procedure will increase over the next few decades with a conservative model showing a 143% increase to 1.5 million cases per year by 2050 in the United States alone [1]. The increase in TKAs is shown to be correlated with improving economics, obesity, longer life expectancy, and higher rates of joint implants in younger patients [2].
Vascular complications arising from TKAs are well documented, occurring directly or via thromboembolic disease [3,4]. Specifically, patients who have venous thromboembolism (VTE) after TKA were shown to have 5 times higher mortality risk and increased healthcare costs than patients who do not have VTE [5]. However, effects of chronic venous insufficiency (CVI) diagnosis prior to TKA are not well documented. The CVI diagnosis affects an estimated 2.5 million adults in the United States, but the condition is often overlooked, or its effects underappreciated, potentially affecting outcomes postsurgery [6–8]. Estimates of CVI prevalence vary widely across populations, with a recent prospective cohort study of adults aged 40 to 80 years exhibiting a CVI prevalence of more than 40% [6,9,10]. It is often caused by abnormal venous flow due to valvular damage or obstruction, causing venous hypertension [7,11]. Venous leg ulcers commonly result from CVI due to irregular venous flow, affecting more than 600,000 patients in the United States alone [9]. These ulcers then heal slowly, have a high possibility of recurring, are open to infection, and are associated with high medical costs [9,11,12]. Since CVI commonly occurs in the lower extremity, surgeons may be more hesitant to perform TKAs in these patients.
There are limited data illustrating the impact of CVI in primary TKA outcomes. A meta-analysis in 2015 found that varicose veins are associated with higher incidence of VTE after TKA [13]. However, a separate study found that patients who have untreated varicose veins had no higher risk of DVT post-TKA compared to patients who did not have varicose veins or who had varicose veins treated prior to TKA [14]. A better understanding of postsurgical complications due to CVI is necessary to understand the associated risks to improve patient outcomes.
A retrospective review of patients diagnosed with CVI who underwent primary TKA was recently conducted within the PearlDiver (PearlDiver Technologies, Fort Wayne, Indiana) database of Medicare claims between 2005 and 2014 [15]. Results found that patients who had CVI are correlated with an increase in the following: lengths of hospital stay, healthcare costs, 90-day readmissions, periprosthetic joint infections, implant-related complications, and other medical complications [15]. To our knowledge, there is no recent study analyzing primary TKA outcomes while differentiating CVI diagnoses by severity. Severity of CVI is classified according to a clinical, etiological, anatomic, and pathophysiological score [16]. Although CVI has been shown to be highly prevalent, more severe forms that include ulceration are much less common [10].
Due to its broad diagnostic criteria, differentiating CVI by severity is crucial to understanding the true effect on TKA outcomes. The purpose of this study was to evaluate post-TKA outcomes of patients who have varying complexities of CVI in a database composed of recent public and private insurance claims.
Materials and Methods
This was an institutional review board–approved (IRB #1692) database study from Louisiana State University Health Sciences Center in New Orleans, Louisiana. This retrospective study obtained electronic health records within a healthcare system in the Southeast United States from January 1, 2011 to December 31, 2021. The dataset consists of patients who were treated with a primary TKA denoted by a Current Procedural Terminology (CPT) code 27447 and includes all healthcare information from visits within the healthcare system.
The CPT codes were used to analyze short-term complications (< 90 days of surgery), long-term complications (< 2 years), and CVI status (yes/no). Short-term complications included blood transfusion, cerebrovascular event, deep vein thrombosis, ileus, kidney injury, pancreatitis, periprosthetic joint infection, pneumonia, pulmonary embolism, respiratory failure, thrombocytopenia, urinary tract infection, and wound dehiscence. Long-term complications included extensor mechanism disruption, implant complication, implant loosening, medial collateral ligament injury, osteolysis, pain due to prosthetic, periprosthetic fracture, prosthetic breakdown, prosthetic instability, and stiffness. Complication codes were selected based on prior studies as well as the expert opinion of surgeons and researchers in the field of TKAs [3,15,17].
When CPT codes denoting CVI severity were available, we categorized CVI into simple, complex, and unclassified severities. Patients who had asymptomatic/uncomplicated varicose veins or chronic venous hypertension were grouped with simple CVI. Patients who had varicose veins or chronic venous hypertension with pain, ulceration, inflammation, and/or other complications were grouped with complex CVI. When CVI severity was not clear, these patients were grouped with unclassified CVI severity. Revision codes (CPT 27487, 27488) were assessed within 2 years of surgery. Readmissions were assessed if a patient had an emergency visit within 90 days of surgery following initial hospital discharge.
Statistical analyses were conducted using R statistical software version 4.0.2 (R Core Team 2023, Vienna, Austria). Categorical variables were summarized by reporting counts and percentages. Continuous variables were summarized by reporting means and standard deviations. Multivariable logistic regressions were performed to predict complication (any/long/short) as a function of CVI status (yes/no; simple/complex) and other potential confounding variables.
When comparing simple/complex CVI to no CVI, sensitivity analyses were performed by considering patients who have unclassified CVI as simple CVI, complex CVI, and removed from comparison. A follow-up analysis was done in the subset of CVI patients with classifiable CVI severity to determine if complex CVI was more likely to result in complication than simple CVI.
The study included 7,665 patients undergoing TKA between 2011 and 2021. Patient demographics included 68.3% White patients, 64.1% self-identifying as women, and 79.1% publicly insured patients (Appendix Table A). The average age of patients was 67 years (11 to 97 years), mean body mass index (BMI) was 37.15 (17 to 97), and adjusted Charlson Comorbidity Index (CCI) reference was 1.08. At the time of surgery, 741 of the TKA patients (9.7%) had CVI. In our population, patients who had CVI were older on average (CVI = 69 years, no CVI = 67 years; unadjusted P < .001), had a higher adjusted CCI (average with CVI = 1.84, average no CVI = 1.00; unadjusted P < .001), and had a higher BMI (average with CVI = 39.10, average no CVI = 36.94; unadjusted P < .001). Those with CVI were associated with having a TKA in recent years (average surgical year with CVI = 2018, average surgical year without CVI = 2017; unadjusted P < .001). Among the 741 CVI patients, 247 (33.3%) had simple CVI, 233 (31.4%) had complex CVI, and 261 (35.2%) had unclassified CVI.
The composite complication rate was 14.1%, encompassing short-term complications, long-term complications, revisions, and readmissions (Appendix Table B). In terms of specific complication occurrence, 7.1% had short-term complications, 1.2% had long-term complications, 1.4% had a TKA revision within 2 years post-operation, and 6.5% had a hospital readmission within 90 days of hospital discharge.
Results
Overall complication rates were 14.0% for patients who did not have a CVI, 16.7% for patients who had a complex CVI, 9.3% for patients who had a simple CVI, and 18.4% who had an unclassified CVI. Multivariable analyses demonstrated no statistical difference in composite complications and CVI status (adjusted odds ratio, aOR = 0.96; 95% Confidence Interval [CI] = 0.77 to 1.20; P = .722) (Appendix Figure A). A diagnosis of CVI was also not associated with a statistical difference in short-term complications (P = .786), long-term complications (P = .15), TKA revisions (P = .964), or readmissions (P = .438). In the set of patients who had classifiable CVI (n = 480), patients who had complex CVI were significantly more likely to have a composite complication than simple CVI patients (aOR = 1.91; 95% CI = 1.05 to 3.53; P = .035).
Patients who had simple CVI had significantly lower composite complication rates compared to all other CVI groups (all P < .040). Unclassified CVI complication rates were significantly higher than patients who did not have CVI (P = .047). However, there was no difference in composite complication rates between complex CVI patients and those who had unclassified CVI (P = .638) or no CVI (P = .249).
When unclassified CVI patients were removed from analysis or classified as complex CVI, patients who had simple CVI had a decreased risk of composite complications compared to those who did not have a CVI diagnosis (P = .023 and P = .022, respectively) (Appendix Table C). Patients who had a complex CVI were near significantly more likely to undergo TKA revision compared to those who did not have a CVI when unclassified CVI was removed from analysis (P = .05). Otherwise, there were no significant differences in complication risk for any type when comparing simple or complex CVI versus patients who did not have CVI when unclassified CVI severity was grouped as simple or complex or removed from analysis (all other P values > .05).
Other studied factors were associated with complication rates. Private insurance status was associated with a decreased risk of composite complications (P < .001), short-term complications (P = .001), and readmissions (P = .045). A more recent surgery year was associated with a decreased risk of composite complications (P < .001), short-term complications (P < .001), revisions (P < .001), and readmissions (P < .001). Increased age was associated with a decreased risk in composite complications (P = .038), long-term complications (P < .001), and revisions (P < .001). Black race was associated with an increased risk in short-term complications (P = .004). Smoking was associated with an increased risk in readmissions (P = .001). Increased CCI was associated with an increased risk of composite complications (P < .001), short-term complications (P < .001), revisions (P = .031), and readmissions (P < .001).
Discussion
With the expected rise in incidence of TKAs in the United States [1], it is important to study preoperative diagnoses that may lead to greater postoperative complications. CVI affects an estimated 5% to 30% of the adult population [6] and 741 (9.7%) in our cohort of TKA patients, indicating that CVI is likely to be seen as a preoperative diagnosis. Although chronic venous stasis theoretically could result in lower extremity procedure complications, there are little data on the postsurgical effect of CVI among those patients undergoing a TKA [15].
In this study, we found that CVI overall did not affect composite postoperative complications, short-term or long-term postoperative complications, 2-year revisions, or 90-day readmissions versus control postadjustment. To analyze the effect of CVI on post-TKA outcomes, patients were grouped into simple CVI, complex CVI, or unclassified CVI severity. There was no significant difference in complication rates between complex CVI compared to no CVI after multivariable adjustments. However, patients who had a complex CVI were found to be at a higher risk for post-TKA composite complications compared to simple CVI. Although, no individual complication rate was significant between simple and complex CVI. This is likely since the composite complication variable is a less specific variable. If a patient who has CVI presents for a preoperative TKA evaluation, stratification of CVI severity could help predict composite complication rates during informed consent.
In contrast to our results, prior literature found that CVI significantly influenced postoperative complications in patients undergoing TKA [15], but severity of CVI was not differentiated. Our study includes patient data from 2011 to 2021 and the use of both International Classification of Diseases (ICD) 9 and ICD-10 codes, which gives a current picture of medical practices. Interestingly, we found that a higher prevalence of CVI and lower composite complication rates in TKAs, independent of CVI status, occurred in recent years. Recent surgery year decreased short-term complications, revisions, and readmissions in analysis of all participants. A recent study found improvements in patient health in those undergoing TKA and improvements in TKA outcomes over a 10-year period [18]. In particular, TKA operative time and hospital length of stay decreased from 2008 to 2018, and 30-day readmission rates declined from 2011 to 2018 [18]. Therefore, our results over time are likely attributed to evolving medical practices and improved patient care.
Our study also stratified patients who had public and private insurances to obtain a patient sample representative of our population. We found that CVI was diagnosed more often in those with public insurance status. Patients who had private insurance had decreased rates of composite complications, short-term complications, and readmissions. These results are unsurprizing since public insurance has been previously associated with increased hospital length of stay and in-hospital complications after unilateral TKA compared to those with commercial insurance [19]. Therefore, CVI is associated with low socioeconomic status, which itself leads to poorer surgical outcomes, but may not compound these effects since CVI alone does not impact composite complication rates.
Another noteworthy population characteristic was present in our study. Approximately 83% of the study participants had a BMI indicative of obesity which could affect application across outside populations; however, other recent studies on TKA populations had obesity prevalence of 63% and 75% [20,21]. Low socioeconomic factors among the local patient population as well as the pathophysiological link between obesity and joint damage are likely explanatory.
A limitation in the study, due to its retrospective nature, is the inability to assess how surgeons may have altered their surgical plan or patient care when a patient is presented with CVI. Independent of TKAs, treatment for CVI typically ranges from leg elevation, exercise, compression therapy, and various surgical techniques [11,12]. Diagnostic consistency is also difficult to ensure in a retrospective study. Compared to patients who did not have CVI, simple CVI patients had lower adjusted composite complication rates. It is possible that prior treatment of the diagnosed and relatively benign simple CVI could have positively affected TKA outcomes. Additionally, our study is smaller than previous literature [15]. To our knowledge, only one other study evaluates CVI as a broad diagnosis and its effects on TKA outcomes [15]. These mixed results necessitate additional studies on CVI and its effects on TKA outcomes. With continued implementation of ICD-10 coding, more specific preoperative diagnoses of CVI severity can be better matched to surgical outcomes.
In conclusion, patients who have complex CVI are at a higher risk for post-TKA complications compared to those who have simple CVI. However, a general CVI diagnosis did not affect postoperative complications versus the control cohort. Stratifying CVI severity is crucial to determine a patient’s risk for post-TKA outcomes. Prevalence of CVI increased in TKAs, yet decreased composite complications may indicate improved surgical care over time.
Acknowledgments
We would like to thank the LA CaTs Grant, U54 GM104940, and the LA CaTS center support for help in compiling the database from medical records.
Appendix
Appendix Figure A.
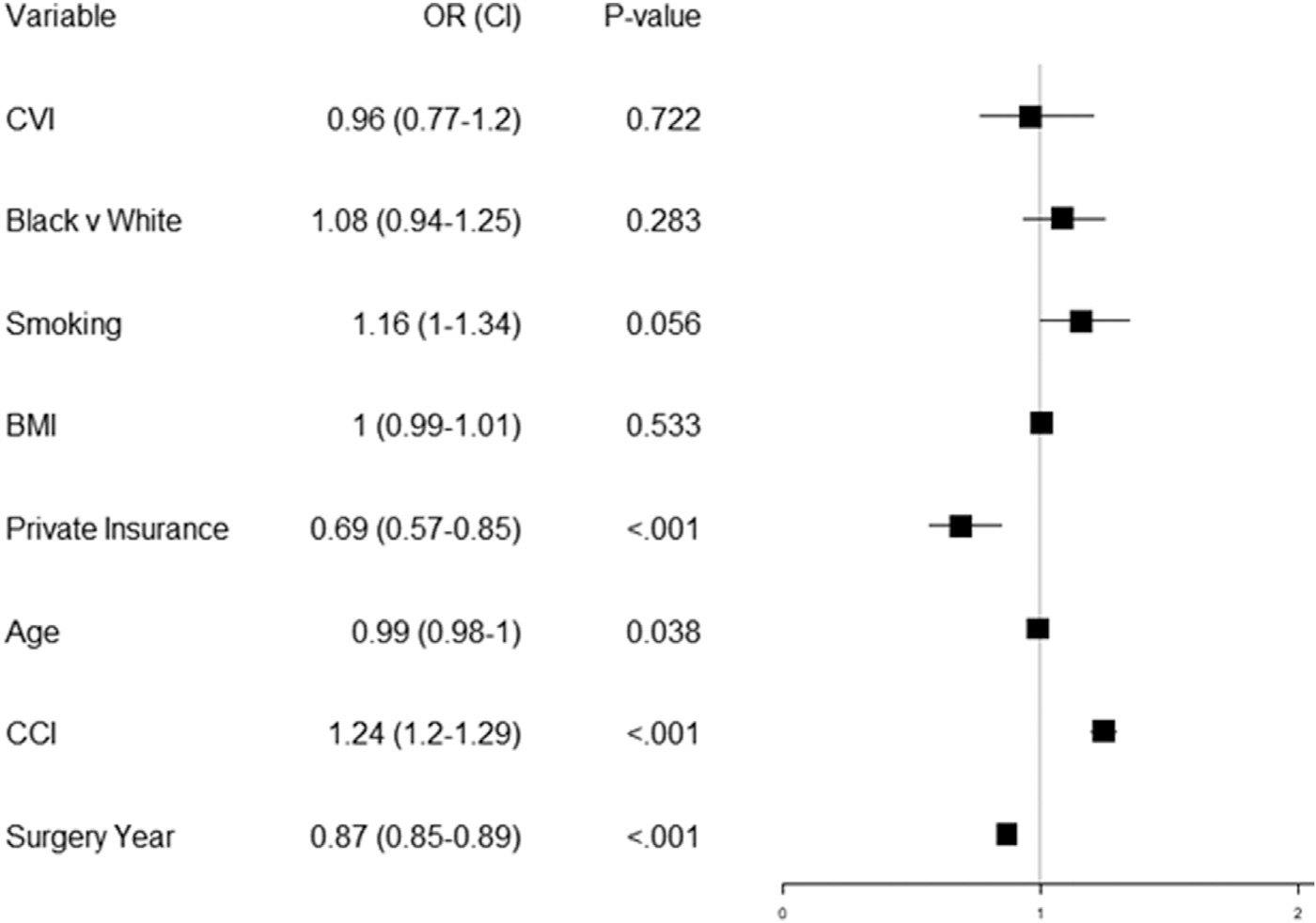
Multivariable logistic regression showing association to composite complication. (OR, odds ratio; CI, confidence interval; CVI, chronic venous insufficiency; BMI, body mass index; CCI, Charlson Comorbidity Index).
Appendix Table A.
Descriptive Characteristics by Chronic Venous Insufficiency Status.
| Variable | All (7,665) | Yes CVI (741) | No CVI (6,924) | P Value | % with CVI |
|---|---|---|---|---|---|
|
| |||||
| White Race | 5,239 (68.3) | 526 (71) | 4,713 (68.1) | .105 | 10 |
| Black Race | 2,426 (31.7) | 215 (29) | 2,211 (31.9) | 8.9 | |
| Men | 2,754 (35.9) | 241 (32.5) | 2,513 (36.3) | .044 | 8.8 |
| Women | 4,911 (64.1) | 500 (67.5) | 4,411 (63.7) | 10.2 | |
| Smoking | 1,837 (24) | 196 (26.5) | 1,641 (23.7) | .103 | 10.7 |
| No Smoking | 5,828 (76) | 545 (73.5) | 5,283 (76.3) | 9.4 | |
| Private Insurance | 1,603 (20.9) | 123 (16.6) | 1,480 (21.4) | .002 | 7.7 |
| Public Insurance | 6,062 (79.1) | 618 (83.4) | 5,444 (78.6) | 10.2 | |
| BMI ≥ 30 | 6,380 (83.2) | 654 (88.3) | 5,726 (82.7) | <.001 | 10.3 |
| BMI < 30 | 1,285 (16.8) | 87 (11.7) | 1,198 (17.3) | 6.8 | |
| Age ≥ 70 | 3,118 (40.7) | 376 (50.7) | 2,742 (39.6) | <.001 | 12.1 |
| Age < 70 | 4,547 (59.3) | 365 (49.3) | 4,182 (60.4) | 8.0 | |
| Composite Complication | 1,077 (14.1) | 110 (14.8) | 967 (14) | .505 | 10.2 |
| Short Complication | 545 (7.1) | 56 (7.6) | 489 (7.1) | .599 | 10.3 |
| Long Complication | 95 (1.2) | 4 (0.5) | 91 (1.3) | .079 | 4.2 |
| TKA Revision | 105 (1.4) | 10 (1.3) | 95 (1.4) | 1 | 9.5 |
| Hospital Readmission Continuous Variables | 496 (6.5) | 62 (8.4) | 434 (6.3) | .033 | 12.5 |
| Age | 66.98 (9.39) | 69.32 (8.97) | 66.72 (9.4) | <.001 | NA |
| CCI | 1.08 (1.6) | 1.84 (1.95) | 1 (1.53) | <.001 | NA |
| Year of TKA | 2,017.21 (2.85) | 2,017.77 (2.55) | 2,017.15 (2.88) | <.001 | NA |
| BMI | 37.15 (8.38) | 39.10 (9.21) | 36.94 (8.26) | <.001 | NA |
P < .05 Demonstrates Significance.
CVI, chronic venous insufficiency; BMI, body mass index; CCI, Charlson Comorbidity Index; TKA, total knee arthroplasty.
Appendix Table B.
Descriptive Characteristics by Composite Complication Status (SD).
| Variable | Complication (1,077) | No Complication (6,588) | P Value | % Complication |
|---|---|---|---|---|
|
| ||||
| CVI | 110 (10.2) | 631 (9.6) | .505 | 14.8 |
| No CVI | 967 (89.8) | 5,957 (90.4) | 14 | |
| Simple CVI | 23 (2.1) | 224 (3.4) | 9.3 | |
| Complex CVI | 39 (3.6) | 194 (2.9) | 16.7 | |
| Unclassified CVI | 48 (4.5) | 213 (3.2) | 18.4 | |
| White Race | 713 (66.2) | 4,526 (68.7) | .104 | 13.6 |
| Black Race | 364 (33.8) | 2,062 (31.3) | 15 | |
| Men | 411 (38.2) | 2,343 (35.6) | .1 | 14.9 |
| Women | 666 (61.8) | 4,245 (64.4) | 13.6 | |
| Smoking | 305 (28.3) | 1,532 (23.3) | <.001 | 16.6 |
| No Smoking | 772 (71.7) | 5,056 (76.7) | 13.2 | |
| Private Insurance | 171 (15.9) | 1,432 (21.7) | <.001 | 10.7 |
| Public Insurance | 906 (84.1) | 5,156 (78.3) | 14.9 | |
| Age | 67.32 (10.55) | 66.92 (9.19) | .023 | |
| CCI | 1.6 (1.91) | 1 (1.53) | <.001 | |
| Year of TKA | 2,016.35 (2.86) | 2,017.35 (2.83) | <.001 | |
| BMI | 37.76 (9.19) | 37.05 (8.24) | .081 | |
P value < .05.
CVI, chronic venous insufficiency; BMI, body mass index; CCI, Charlson Comorbidity Index; TKA, total knee arthroplasty.
Appendix Table C.
Multivariable Logistic Regressions for Each Complication Type and Chronic Venous Insufficiency (CVI) Grouping (Simple/Complex) versus No CVI.
| CVI Grouping versus No CVI | Composite Complication | Short Complication | Long Complication | Revision |
Readmission |
|---|---|---|---|---|---|
| <2 y | <90 d | ||||
|
| |||||
| Unclassified CVI patients removed from analysis | |||||
| Complex CVI versus none | 1.10 (0.75 to 1.56) | 1.04 (0.62 to 1.67) | 0.36 (0.02 to 1.66) | 2.24 (0.91 to 4.70) | 1.16 (0.70 to 1.83) |
| P = .617 | P = .868 | P = .315 | P = .05 | P = .532 | |
| Simple CVI versus none | 0.6 (0.37 to 0.91) | 0.58 (0.29 to 1.03) | 0.74 (0.12 to 2.36) | 0.35 (0.02 to 1.58) | 0.68 (0.36 to 1.19) |
| P = .023 | P = .085 | P = .669 | P = .296 | P = .212 | |
| Unclassified CVI patients classified as Simple | |||||
| Complex CVI versus none | 1.10 (0.76 to 1.57) | 1.06 (0.63 to 1.7) | 0.38 (0.02 to 1.75) | 2.13 (0.87 to 4.46) | 1.17 (0.71 to 1.84) |
| P = .594 | P = .812 | P = .34 | P = .066 | P = .52 | |
| Simple CVI versus none | 0.90 (0.68 to 1.17) | 0.91 (0.63 to 1.29) | 0.52 (0.13 to 1.40) | 0.44 (0.11 to 1.19) | 1.10 (0.77 to 1.53) |
| P = .431 | P = .626 | P = .267 | P = .168 | P = .59 | |
| Unclassified CVI patients classified as Complex | |||||
| Complex CVI versus none | 1.16 (0.89 to 1.48) | 1.15 (0.81 to 1.60) | 0.35 (0.06 to 1.13) | 1.25 (0.57 to 2.42) | 1.34 (0.96 to 1.83) |
| P = .262 | P = .414 | P = .145 | P = .54 | P = .078 | |
| Simple CVI versus none | 0.60 (0.37 to 0.91) | 0.58 (0.3 to 1.03) | 0.74 (0.12 to 2.36) | 0.35 (0.02 to 1.58) | 0.69 (0.36 to 1.19) |
| P = .022 | P = .088 | P = .672 | P = .296 | P = .214 | |
For Each Complication Type, the Adjusted Odds Ratio (95% Confidence Interval, P Value) is Reported. Confidence Intervals Greater Than (Less Than) 1 Indicate an Increased (Decreased) Risk of That Complication Type.
CVI, chronic venous insufficiency.
Appendix Table D.
Codes Used for Analysis.
| Category | ICD 9/10 and CPT Codes |
|---|---|
|
| |
| Unclassified CVI Codes | 459.81, 187.2 |
| Complex CVI | 454, 454.1, 454.2, 454.8, I83.001, I83.002, I83.003, I83.004, I83.005, I83.008, I83.009, I83.011, I83.012, I83.013, I83.014, I83.015, I83.018, I83.019, I83.021, I83.022, I83.023, I83.024, I83.025, I83.028, I83.029, I83.10, I83.11, I83.12, I83.201, I83.202, I83.203, I83.204, I83.205, I83.208, I83.209, I83.211, I83.212, I83.213, I83.214, I83.215, I83.218, I83.219, I83.221, I83.222, I83.223, I83.224, I83.225, I83.228, I83.229, I83.811, I83.812, I83.813, I83.819, I83.891, I83.892, I83.893, I83.899, 459.31, 459.32, 459.33, 459.39, I87.311, I87.312, I87.313, I87.319, I87.321, I87.322, I87.323, I87.329, I87.331, I87.332, I87.333, I87.339, I87.391, I87.392, I87.393, I87.399 |
| Simple CVI | |
| Short-term complication (< 90 d following surgery) | 454.9, I83.90, I83.91, I83.92, I83.93, 459.3, I87.301, I87.302, I87.303, I87.309 |
| Blood transfusion | 86999, 36430 |
| Cerebrovascular event | 430, 431, 432.1, 432.9, 433, 433.01, 433.1, 433.11, 433.2, 433.21, 433.3, 433.31, 433.8, 433.81, 433.9, 433.91, 434, 434.01, 434.1, 434.11, 434.9, 434.91, I60.00, I60.01, I60.02, I60.10, I60.11, I60.12, I60.2, I60.20, I60.21, I60.22, I60.31, I60.32, I60.4, I60.51, I60.52, I60.6, I60.7, I60.8, I60.9, I61.0, I61.1, I61.2, I61.3, I61.4, I61.5, I61.6, I61.8, I61.9, I62.00, I62.01, I62.02, I62.03, I62.9, I63.00, I63.011, I63.012, I63.013, I63.019, I63.02, I63.031, I63.032, I63.033, I63.039, I63.09, I63.10, I63.111, I63.112, I63.113, I63.119, I63.12, I63.131, I63.132, I63.133, I63.139, I63.19, I63.20, I63.211, I63.212, I63.213, I63.219, I63.22, I63.231, I63.232, I63.233, I63.239, I63.29, I63.30, I63.311, I63.312, I63.313, I63.319, I63.321, I63.322, I63.323, I63.329, I63.331, I63.332, I63.333, I63.339, I63.341, I63.342, I63.343, I63.349, I63.39, I63.40, I63.411, I63.412, I63.413, I63.419, I63.421, I63.422, I63.423, I63.429, I63.431, I63.432, I63.433, I63.439, I63.441, I63.442, I63.443, I63.449, I63.49, I63.50, I63.511, I63.512, I63.513, I63.519, I63.521, I63.522, I63.523, I63.529, I63.531, I63.532, I63.533, I63.539, I63.541, I63.542, I63.543, I63.549, I63.59, I63.6, I63.8, I63.81, I63.89, I63.9, I65.01, I65.02, I65.03, I65.09, I65.1, I65.21, I65.22, I65.23, I65.29, I65.8, I65.9, I66.01, I66.02, I66.03, I66.09, I66.11, I66.12, I66.13, I66.19, I66.21, I66.22, I66.23, I66.29, I66.3, I66.8, I66.9 |
| DVT | 451.11, 451.19, 453.4, 453.41, 453.42, 453.5, 453.51, 453.52, I82.401, I82.402, I82.403, I82.409, I82.411, I82.412, I82.413, I82.419, I82.421, I82.422, I82.423, I82.429, I82.431, I82.432, I82.433, I82.439, I82.441, I82.442, I82.443, I82.449, I82.451, I82.452, I82.453, I82.459, I82.461, I82.462, I82.463, I82.469, I82.491, I82.492, I82.493, I82.499, I82.4Y1, I82.4Y2, I82.4Y3, I82.4Y9, I82.4Z1, I82.4Z2, I82.4Z3, I82.4Z9, I82.501, I82.502, I82.503, I82.509, I82.511, I82.512, I82.513, I82.519, I82.521, I82.522, I82.523, I82.529, I82.531, I82.532, I82.533, I82.539, I82.541, I82.542, I82.543, I82.549, I82.551, I82.552, I82.553, I82.559, I82.561, I82.562, I82.563, I82.569, I82.591, I82.592, I82.593, I82.599, I82.5Y1, I82.5Y2, I82.5Y3, I82.5Y9, I82.5Z1, I82.5Z2, I82.5Z3, I82.5Z9 |
| Ileus | 560.1, NA, 560.1, K56.0, K56.7 |
| Kidney injury | 584.5, 584.6, 584.7, 584.8, 584.9, N17.0, N17.1, N17.2, N17.8, N17.9, N19, N99.0 |
| Pancreatitis | 577, K85.9, K85.90, K85.91, K85.92 |
| Periprosthetic joint infection | 996.66, 996.67, T84.53XA, T84.54XA |
| Pneumonia | 480, 480.1, 480.2, 480.3, 480.8, 480.9, 481, 482, 482.1, 482.2, 482.3, 482.31, 482.32, 482.39, 482.4, 482.41, 482.42, 482.49, 482.82, 482.83, 482.89, 482.9, 483, 483.1, 483.8, 484.1, 484.3, 484.6, 484.7, 484.8, 485, 486, 487, 997.31, J09.X1, J10.00, J10.01, J10.08, J11.00, J11.08, J12.0, J12.1, J12.2, J12.3, J12.81, J12.82, J12.89, J12.9, J13, J14, J15.0, J15.1, J15.20, J15.211, J15.212, J15.29, J15.3, J15.4, J15.5, J15.6, J15.7, J15.8, J15.9, J16.0, J16.8, J17, J18.0, J18.1, J18.2, J18.8, J18.9, J85.1, J95.851 |
| Pulmonary embolism | 415.11, 415.13, 415.19, 416.2, I26.09, I26.90, I26.92, I26.99, I27.82 |
| Respiratory failure | 518.51, 518.52, 518.53, 518.81, 518.82, 518.83, 518.84, J95.2, J95.3, J95.821, J95.822, J96.00, J96.01, J96.02, J96.10, J96.11, J96.12, J96.20, J96.21, J96.22, J96.90, J96.91, J96.92 |
| Thrombocytopenia | 287.3, 287.39, 287.5, D69.49, D69.59, D69.6 |
| UTI | 599, N39.0 |
| Wound dehiscence | 998.32, 998.83, T81.31XA |
| Long-term complication (< 2 y following surgery) | |
| Extensor mechanism disruption | 727.66, M66.261, M66.262, M66.269 |
| Implant complication | 996.47, T84.092A, T84.093A |
| Implant loosening | 996.41, T84.032A, T84.033A |
| MCL injury | 844.1, S83.411A, S83.412A, S83.419A |
| Osteolysis | 996.45, T84.052A, T84.053A |
| Pain due to prosthetic | 996.77, T84.84XA |
| Periprosthetic fracture | 996.44, M97.11XA, M97.12XA, T84.042A, T84.043A |
| Prosthetic breakdown | 996.43, T84.012A, T84.013A |
| Prosthetic instability | T84.022A, T84.023A |
| Stiffness | 719.56, M25.661, M25.662, M25.669 |
CVI, chronic venous insufficiency; ICD, international classification of diseases; CPT, current procedural terminology; DVT, deep vein thrombosis; UTI, urinary tract infection; MCL, medial collateral ligament.
Appendix Table E.
Individual Complication by Chronic Venous Insufficiency Status.
| Complications | All (7, 665) | CVI (741) | No CVI (6, 924) | P Value | % CVI |
|---|---|---|---|---|---|
|
| |||||
| Short term Complications | |||||
| Transfusion | 241 (3.1) | 21 (2.8) | 220 (3.2) | .739 | 8.7 |
| Cerebrovascular event | 44 (0.6) | 7 (0.9) | 37 (0.5) | .192 | 15.9 |
| DVT | 26 (0.3) | 3 (0.4) | 23 (0.3) | .735 | 11.5 |
| Ileus | 8 (0.1) | 1 (0.1) | 7 (0.1) | .509 | 14.3 |
| Kidney injury | 87 (1.1) | 9 (1.2) | 78 (1.1) | .854 | 10.3 |
| Pancreatitis | 2 (0) | 0 (0) | 2 (0) | 1 | 0 |
| Pneumonia | 9 (0.1) | 0 (0) | 9 (0.1) | 1 | 0 |
| Pulmonary embolism | 23 (0.3) | 2 (0.3) | 21 (0.3) | 1 | 8.7 |
| Respiratory failure | 55 (0.7) | 6 (0.8) | 49 (0.7) | .65 | 10.9 |
| Thrombocytopenia | 60 (0.8) | 9 (1.2) | 51 (0.7) | .182 | 15 |
| UTI | 22 (0.3) | 2 (0.3) | 20 (0.3) | 1 | 9.1 |
| Wound dehiscence | 0 (0) | 0 (0) | 0 (0) | NA | NA |
| Periprosthetic joint infection | 47 (0.6) | 4 (0.5) | 43 (0.6) | 1 | 8.5 |
| Long term Complications | |||||
| Extensor mechanism disruption | 1 (0) | 0 (0) | 1 (0) | 1 | 0 |
| Implant complication | 19 (0.2) | 0 (0) | 19 (0.3) | .249 | 0 |
| Implant loosening | 1 (0) | 0 (0) | 1 (0) | 1 | 0 |
| MCL injury | 6 (0.1) | 0 (0) | 6 (0.1) | 1 | 0 |
| Osteolysis | 0 (0) | 0 (0) | 0 (0) | NA | NA |
| Pain due to prosthetic | 38 (0.5) | 2 (0.3) | 36 (0.5) | .579 | 5.3 |
| Periprosthetic fracture | 1 (0) | 0 (0) | 1 (0) | 1 | 0 |
| Prosthetic breakdown | 3 (0) | 0 (0) | 3 (0) | 1 | 0 |
| Prosthetic instability | 2 (0) | 0 (0) | 2 (0) | 1 | 0 |
| Stiffness | 30 (0.4) | 2 (0.3) | 28 (0.4) | .764 | 6.7 |
CVI, chronic venous insufficiency; DVT, deep vein thrombosis; UTI, urinary tract infection; MCL, medial collateral ligament; NA, not applicable.
Appendix Table F.
Individual Complication by Chronic Venous Insufficiency Severity.
| Complications | Simple | None | Complex | Unclassified | P Value |
|---|---|---|---|---|---|
|
| |||||
| Composite Complication | 23 (9.3) | 967 (14) | 39 (16.7) | 48 (18.4) | .016 |
| Short Complication | 11 (4.5) | 489(7.1) | 19 (8.2) | 26(10) | .096 |
| Long Complication | 2 (0.8) | 91 (1.3) | 1 (0.4) | 1 (0.4) | .465 |
| TKA Revision | 1 (0.4) | 95 (1.4) | 7 (3) | 2 (0.8) | .099 |
| Hospital Readmission | 12 (4.9) | 434 (6.3) | 21 (9) | 29(11.1) | .007 |
| Short-term Complications | |||||
| Transfusion | 2 (0.8) | 220 (3.2) | 5(2.1) | 14 (5.4) | .021 |
| Cerebrovascular event | 1 (0.4) | 37 (0.5) | 3(1.3) | 3(1.1) | .169 |
| DVT | 1 (0.4) | 23 (0.3) | 1 (0.4) | 1 (0.4) | .555 |
| Ileus | 1 (0.4) | 7(0.1) | 0 (0) | 0 (0) | .38 |
| Kidney injury | 1 (0.4) | 78(1.1) | 1 (0.4) | 7 (2.7) | .083 |
| Pancreatitis | 0 (0) | 2 (0) | 0 (0) | 0 (0) | 1 |
| Pneumonia | 0 (0) | 9(0.1) | 0 (0) | 0 (0) | 1 |
| Pulmonary embolism | 0 (0) | 21 (0.3) | 1 (0.4) | 1 (0.4) | .601 |
| Respiratory failure | 2 (0.8) | 49 (0.7) | 4(1.7) | 0 (0) | .135 |
| Thrombocytopenia | 2 (0.8) | 51 (0.7) | 4(1.7) | 3(1.1) | .207 |
| UTI | 1 (0.4) | 20 (0.3) | 1 (0.4) | 0 (0) | .513 |
| Wound dehiscence | 0 (0) | 0 (0) | 0 (0) | 0 (0) | NA |
| Periprosthetic joint infection | 0 (0) | 43 (0.6) | 2 (0.9) | 2 (0.8) | .548 |
| Long-term Complications | |||||
| Extensor mechanism disruption | 0 (0) | 1 (0) | 0 (0) | 0 (0) | 1 |
| Implant complication | 0 (0) | 19 (0.3) | 0 (0) | 0 (0) | 1 |
| Implant loosening | 0 (0) | 1 (0) | 0 (0) | 0 (0) | 1 |
| MCL injury | 0 (0) | 6(0.1) | 0 (0) | 0 (0) | 1 |
| Osteolysis | 0 (0) | 0 (0) | 0 (0) | 0 (0) | NA |
| Pain due to prosthetic | 1 (0.4) | 36 (0.5) | 0 (0) | 1 (0.4) | .952 |
| Periprosthetic fracture | 0 (0) | 1 (0) | 0 (0) | 0 (0) | 1 |
| Prosthetic breakdown | 0 (0) | 3 (0) | 0 (0) | 0 (0) | 1 |
| Prosthetic instability | 0 (0) | 2 (0) | 0 (0) | 0 (0) | 1 |
| Stiffness | 1 (0.4) | 28 (0.4) | 1 (0.4) | 0 (0) | .736 |
TKA, total knee arthroplasty; DVT, deep vein thrombosis; UTI, urinary tract infection; MCL, medial collateral ligament; NA, not applicable.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.arth.2023.05.040.
References
- [1].Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S. Projected increase in total knee arthroplasty in the United States – an alternative projection model. Osteoarthr Cartil 2017;25:1797–803. 10.1016/j.joca.2017.07.022. [DOI] [PubMed] [Google Scholar]
- [2].Pabinger C, Lothaller H, Geissler A. Utilization rates of knee-arthroplasty in OECD countries. Osteoarthr Cartil 2015;23:1664–73. 10.1016/j.joca.2015.05.008. [DOI] [PubMed] [Google Scholar]
- [3].Healy WL, Della Valle CJ, Iorio R, Berend KR, Cushner FD, Dalury DF, et al. Complications of total knee arthroplasty: standardized list and definitions of the knee society knee. Clin Orthop Relat Res 2013;471:215–20. 10.1007/s11999-012-2489-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Harris WH, Sledge CB. Total hip and total knee replacement. N Engl J Med 1990;323:801–7. 10.1056/nejm199009203231206. [DOI] [PubMed] [Google Scholar]
- [5].Baser O, Supina D, Sengupta N, Wang L, Kwong L. Impact of postoperative venous thromboembolism on Medicare recipients undergoing total hip replacement or total knee replacement surgery. Am J Health Syst Pharm 2010;67:1438–45. 10.2146/ajhp090572. [DOI] [PubMed] [Google Scholar]
- [6].Prochaska JH, Arnold N, Falcke A, Kopp S, Schulz A, Buch G, et al. Chronic venous insufficiency, cardiovascular disease, and mortality: a population study. Eur Heart J 2021;42:4157–65. 10.1093/eurheartj/ehab495. [DOI] [PubMed] [Google Scholar]
- [7].Youn YJ, Lee J. Chronic venous insufficiency and varicose veins of the lower extremities. Korean J Intern Med 2019;34:269–83. 10.3904/kjim.2018.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Baliyan V, Tajmir S, Hedgire SS, Ganguli S, Prabhakar AM. Lower extremity venous reflux. Cardiovasc Diagn Ther 2016;6:533–43. 10.21037/cdt.2016.11.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lal BK. Venous ulcers of the lower extremity: definition, epidemiology, and economic and social burdens. Semin Vasc Surg 2015;28:3–5. 10.1053/j.semvascsurg.2015.05.002. [DOI] [PubMed] [Google Scholar]
- [10].Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation 2005;111:2398–409. 10.1161/01.CIR.0000164199.72440.08. [DOI] [PubMed] [Google Scholar]
- [11].Gould LJ, Dosi G, Couch K, Gibbons GW, Howell RS, Brem H, et al. Modalities to treat venous ulcers: compression, surgery, and bioengineered tissue. Plast Reconstr Surg 2016;138:199S–208S. 10.1097/PRS.0000000000002677. [DOI] [PubMed] [Google Scholar]
- [12].Millan SB, Gan R, Townsend PE. Venous ulcers: diagnosis and treatment. Am Fam Phys 2019;100:298–305. [PubMed] [Google Scholar]
- [13].Zhang J, Chen Z, Zheng J, Breusch SJ, Tian J. Risk factors for venous thromboembolism after total hip and total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg 2015;135:759–72. 10.1007/s00402-015-2208-8. [DOI] [PubMed] [Google Scholar]
- [14].Dua A, Neiva S, Sutherland A. Does previous varicose vein surgery alter deep vein thrombosis risk after lower limb arthroplasty? Orthop Surg 2012;4:222–6. 10.1111/os.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Summers S, Yakkanti R, Ocksrider J, Haziza S, Mannino A, Roche M, et al. Effects of venous insufficiency in patients undergoing primary total knee arthroplasty: an analysis of 12 million patients. J Knee Surg 2021;36:322–8. 10.1055/s-0041-1733901. [DOI] [PubMed] [Google Scholar]
- [16].Lurie F, Passman M, Meisner M, Dalsing M, Masuda E, Welch H, et al. The 2020 update of the CEAP classification system and reporting standards. J Vasc Surg Venous Lymphat Disord 2020;8:342–52. 10.1016/j.jvsv.2019.12.075. [DOI] [PubMed] [Google Scholar]
- [17].Ofa SA, Ross BJ, Flick TR, Patel AH, Sherman WF. Robotic total knee arthroplasty vs conventional total knee arthroplasty: a nationwide database study. Arthroplast Today 2020;6:1001–1008.e3. 10.1016/j.artd.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Siddiqi A, Warren JA, McLaughlin J, Kamath AF, Krebs VE, Molloy RM, et al. Demographic, comorbidity, and episode-of-care differences in primary total knee arthroplasty. J Bone Joint Surg Am 2021;103:227–34. 10.2106/JBJS.20.00597. [DOI] [PubMed] [Google Scholar]
- [19].Mehta B, Ho K, Bido J, Memtsoudis SG, Parks ML, Russell L, et al. Medicare/medicaid insurance status is associated with reduced lower bilateral knee arthroplasty utilization and higher complication rates. J Am Acad Orthop Surg Glob Res Rev 2022;6:1–11. 10.5435/jaaosglobal-d-21-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Brock JL, Kamath AF. Obesity and racial characteristics drive utilization of total joint arthroplasty at a younger age. J Clin Orthop Trauma 2019;10:334–9. 10.1016/j.jcot.2018.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].George J, Piuzzi NS, Ng M, Sodhi N, Khlopas AA, Mont MA. Association between body mass index and thirty-day complications after total knee arthroplasty. J Arthroplasty 2018;33:865–71. 10.1016/j.arth.2017.09.038. [DOI] [PubMed] [Google Scholar]


