Abstract
OBJECTIVES:
To address areas in which there is no consensus for the technologies, effort, and training necessary to integrate and interpret information from multimodality neuromonitoring (MNM).
DESIGN:
A three-round Delphi consensus process.
SETTING:
Electronic surveys and virtual meeting.
SUBJECTS:
Participants with broad MNM expertise from adult and pediatric intensive care backgrounds.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
Two rounds of surveys were completed followed by a virtual meeting to resolve areas without consensus and a final survey to conclude the Delphi process. With 35 participants consensus was achieved on 49% statements concerning MNM. Neurologic impairment and the potential for MNM to guide management were important clinical considerations. Experts reached consensus for the use of MNM—both invasive and noninvasive—for patients in coma with traumatic brain injury, aneurysmal subarachnoid hemorrhage, and intracranial hemorrhage. There was consensus that effort to integrate and interpret MNM requires time independent of daily clinical duties, along with specific skills and expertise. Consensus was reached that training and educational platforms are necessary to develop this expertise and to provide clinical correlation.
CONCLUSIONS:
We provide expert consensus in the clinical considerations, minimum necessary technologies, implementation, and training/education to provide practice standards for the use of MNM to individualize clinical care.
Keywords: Delphi consensus, multimodality monitoring, neurocritical care, precision medicine, secondary brain injury
Multimodality neuromonitoring (MNM) refers to the use of more than one source of physiologic measurement that can be integrated, displayed, and interpreted to guide the clinical management of patients with brain injuries (1–3) (Box 1). Monitoring cardiopulmonary function using electrocardiography (ECG), blood pressure, and plethysmography (Spo2) is standard in intensive care settings to identify and treat significant changes in a patient’s condition. Yet, brain-specific measurements have not been standardized in clinical practice and may variably include modalities focused on intracranial pressure (ICP) or cerebral blood flow, cerebral metabolism, or cortical function (4) depending on the institution, experience of clinicians, or clinical context. “Multimodality monitoring”, as typically abbreviated MMM, has been nearly synonymous with the use of invasive brain monitoring modalities in adult intensive care, whereas pediatric intensive care more often employs noninvasive modalities. Any monitor or device used for continuous or frequent serial bedside measurements may be considered to be part of what is referred to here as MNM.
Literature focused on practical use of MNM includes a consensus summary statement (1), expert opinion recommendations (3) and surveys from adult (5) and pediatric (2) brain monitoring practices in mostly U.S. centers. Disease-specific practice surveys from Europe and Latin America have focused on MNM for traumatic brain injury (TBI) (6–8). Narrative reviews of invasive and noninvasive MNM (9–15), or MNM for patients with TBI (16, 17), aneurysmal subarachnoid hemorrhage (aSAH) (18, 19), and cardiac arrest (20) also exist. Yet, there remains no consensus regarding: a) the minimum set of technologies required for MNM, b) which patients may benefit from care guided by MNM, c) the effort required to integrate MNM measurements and interpret the resulting data, and d) the training required to understand and accurately interpret MNM information. Only by addressing these gaps can we hope to provide consistency within clinical practice, enhance the clinical utility of MNM, and begin to systematically improve individualized intensive care management strategies to impact outcome.
Evidence-based guidelines are rare for emerging applications such as MNM and therefore expert opinion is required to provide standards for implementation. We conducted a three-round Delphi consensus process (21, 22) including clinicians with established expertise in the use of MNM to address these and other knowledge gaps.
MATERIALS AND METHODS
Expert Panel Selection
An international panel of adult and pediatric intensive care experts with established expertise in MNM was identified using mailing lists from the Neurocritical Care Society Informatics Section, involvement in MNM-based workshops, and peer recommendations. Practitioners from any primary specialty background with personal experience using MNM in an ICU setting were included. We excluded nonpracticing providers and trainees, those with experience limited to single technologies (e.g., continuous electroencephalography [cEEG]), and those working outside of the ICU setting. The Institutional Review Board (IRB) of the University of Cincinnati approved the study (No. 2021-0124 MMM Delphi; approval date: February 26, 2021) all procedures were followed in accordance with the ethical standards of the IRB and with the Helsinki Declaration of 1975. An email invitation and information sheet was sent to all potential participants who could then assent to participation or not.
Delphi Study Design
A three-round Delphi process design was used. Rounds 1 and 2 were survey-based (Microsoft Forms [Microsoft Corp, Redmond, WA]). Round 3 consisted of a virtual meeting and a final follow-up survey. All surveys were completed anonymously.
Round 1 consisted of a semi-structured survey including clinical considerations, case presentations, minimum necessary technologies, effort, and training standards. Structured statements used a Likert scale based on the Grading of Recommendations Assessment, Development, and Evaluation paradigm (23, 24). Participants could disagree (scores 1–3), remain neutral (scores 4–6), or agree (scores 7–9) with statements. Open-ended questions were included to generate ideas for new statements during round 2. All statements were developed by one of the authors (B.F.) and reviewed by 10 content experts.
Round 2 included the aggregate results from round 1 and a structured survey in which all statements required Likert scale responses. Experts could participate in round 2 regardless of participation in round 1. However, participation in round 2 was required for participation in round 3.
Round 3 was a virtual meeting to summarize areas of consensus and discuss statements that did not meet consensus criteria or did not exhibit between-round stability. Remaining statements were reevaluated for final consensus in a final survey. Input from round 3 participants following the completion of the discussion and survey was used to draft a practical framework for MNM.
Consensus Criteria and Statistical Analysis
The primary endpoint for concluding the Delphi process was consensus for half of statements. Consensus for a given statement was defined as greater than 70% within the lowest or highest tertile (21) and an interquartile range (IQR) of responses less than or equal to 1.75 (25). Agreement was separately defined as a median Likert score within the highest or lowest tertiles or selection of a multiselect item by more than two-thirds of participants. Between-round stability was assessed using the McNemar change test (26) for dichotomous variables. Permutation testing without replacement over 104 iterations was used to approximate normality assumptions for Likert items. A p value of 0.05 was considered significant. Analyses were conducted using R Version 4.2.0 (R Core Team, Vienna, Austria).
RESULTS
A total of 58 experts were invited to participate. Thirty participated in round 1 (52%) and thirty-five participated in round 2 (60%). Both rounds were completed by 29 participants (Fig. 1; and Supplemental Tables 1 and 2, http://links.lww.com/CCM/H385). Eighteen participants (51%) were neurology trained; the majority of participants (83%) primarily practiced neurocritical care. Six (17%) had a primarily pediatric practice. Half (51%) had greater than or equal to 11 years of clinical practice. A majority of experts had experience with 14 common MNM monitors and devices, although fewer pediatric specialists had experience with brain tissue oxygen (Pbto2) (33% vs 100%; p < 0.01) and regional cerebral blood flow (rCBF) monitors (0% vs 55% of adult specialists; p = 0.04).
Figure 1.
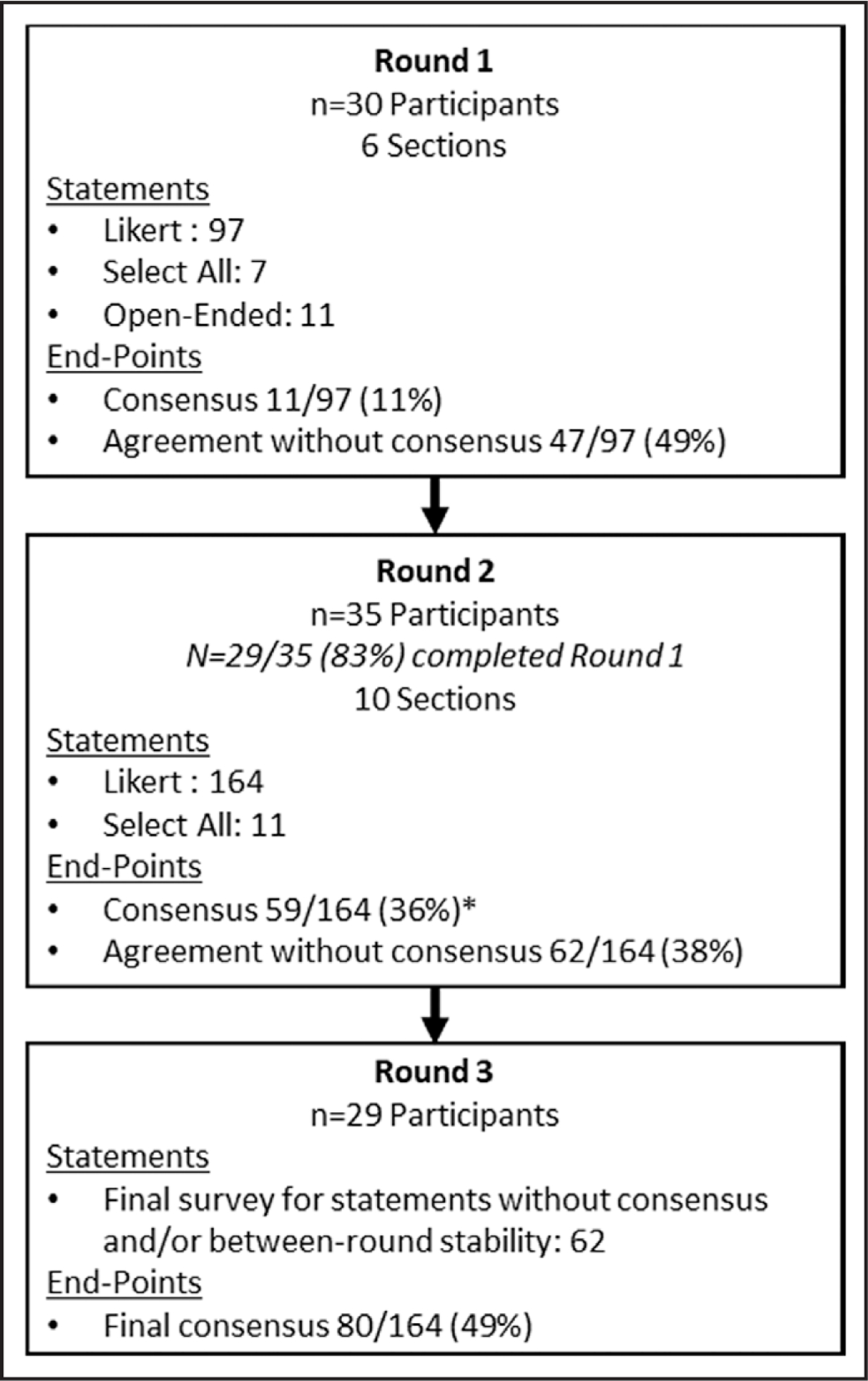
Delphi process flow diagram.
Delphi Round Performance
Round performance is shown in Figure 1. In response to open-ended questions in round 1, round 2 included additional sections regarding operationalization of MNM, reporting elements, core concepts, and educational formats. Eight statements failed to demonstrate between-round stability (Supplemental Materials 1 and 2, http://links.lww.com/CCM/H385). During round 3, discussion called for experts to differentiate between invasive or noninvasive monitoring modalities for case-based statements which were rephrased and addressed in a final survey. Case-based scenarios that had previously achieved consensus were reaffirmed for both invasive and noninvasive monitoring modalities. After round 3, 80 of 164 statements (49%) achieved consensus and all statements without between-round stability were affirmed. Table 1 summarizes areas of consensus; quantitative results are presented in Supplemental Table 3 (http://links.lww.com/CCM/H385). Supplemental Tables 4 and 5 (http://links.lww.com/CCM/H385) present areas of agreement without consensus and areas of neither agreement nor disagreement, respectively.
TABLE 1.
Areas of Consensus
| Clinical Considerations for the Utility of MNM | Contexts of Use: Case Presentations |
|---|---|
|
| |
| 1) Level of consciousness 2) Underlying disease or diagnosis 3) Potential risk for secondary brain injuries or neurodeterioration 4) Structural imaging findings 5) Confounding factors clouding the neurologic examination 6) Desire to understand pathophysiology underlying brain dysfunction 7) Guiding individualized management decisions 8) Informing goals or thresholds for targeted management 9) Abstaining from or de-escalating a therapy or treatment that might cause harm |
1) Nonsurgical TBI comatose (GCS 8 or less) after initial resuscitation 2) Surgical TBI comatose (GCS 8 or less) after evacuation and/or decompression 3) aSAH comatose (Hunt-Hess 4–5) after initial resuscitation and/or treatment of hydrocephalus 4) aSAH with vasospasm or vasospasm-associated delayed cerebral ischemia, comatose or ventilated on sedation 5) ICH without IVH comatose (GCS 8 or less) after initial resuscitation and/or treatment of hydrocephalus 6) ICH with IVH comatose (GCS 8 or less) after initial resuscitation and/or treatment of hydrocephalus |
|
| |
| Minimum Necessary Technology: Access | |
|
| |
| 1) Bedside visualization or display of… • single, current (live) measurement value • single measurement trended over time • multiple, current (live) measurement values together on the same screen • multiple measurements trended over time and aligned on the same screen • summary or aggregate data on a device visible in a patient care area 2) Access to data with high temporal resolution (≥ 1 data point/min) 3) Access to data at waveform resolution 4) EHR display (in a table or graph) of multiple different measurement values together on a single panel, tab, or screen |
5) Ability to… • annotate neuromonitoring data at bedside to indicate clinical events or context • display neuromonitoring data at bedside linked with annotations and/or with EHR information • manipulate visualization or display at bedside, e.g., zooming, scrolling, or selecting measurements • visualize or display neuromonitoring data in real-time remotely • manipulate and review displayed neuromonitoring data in real-time remotely • display neuromonitoring data remotely linked with bedside annotations and/or with EHR information • set alarms or thresholds to alert staff at bedside • access neuromonitoring data in real-time for use in data analytic tools either through a network interface or hardware connection |
|
| |
| Minimum Necessary Work of MNM | Operationalizing MNM |
|
| |
| 1) As part of daily clinical care, most intensivists staffing an ICU… • are not able to adequately integrate and interpret MNM data • do not have adequate time to fully review all available MNM data • do not have all the necessary technology to integrate and interpret MNM data • do not have technical knowledge sufficient to troubleshoot device errors and to identify artifactual or erroneous MNM data • would find regularly written reports summarizing MNM data and providing clinical interpretation/correlation to be helpful in making clinical decisions 2) The integration and interpretation of MNM requires… • access to raw data for data manipulation outside of source devices • review of a variety of time-scales—from hours to days of data—in order to make clinically meaningful inferences from the information • specific skill or expertise to synthesize multiple data trends over time • skill or expertise that is not routinely developed by existing fellowship training • integration with both brain-specific data and systemic data traditionally measured during critical care (e.g., hemodynamic information) • clinical context: clinical correlation is a central component of this process 3) MNM work that is time intensive independent of other clinical duties includes: •a pplication and maintenance of equipment and technologies • synthesis and interpretation of multiple neuromonitoring data trends 4) Existing billing codes for other neurophysiologic procedures such as continuous video electroencephalography monitoring (e.g., CPT 95720) or intraoperative monitoring (e.g., CPT 95941) do not adequately capture the work of MNM |
1) Provide bedside users (e.g., clinical care team) an interface that… • facilitates an understanding of multiple parameters in the context of specific disease processes • displays trend data on a single screen that can be used to manipulate and explore data 2) Enhance clinical confidence in monitoring data by using software tools to identify or remove artifacts within real-time monitoring data that limits clinical interpretation 3) Identify necessary Information Technology or Clinical Engineering personnel to overcome technological hurdles that limit access to monitoring data 4) Invest in education for bedside users (e.g., clinical care team) focused on… • understanding the parameters being measured and why • learning how to respond to monitoring data 5) Standardize who is monitored and by which technologies 6) Develop clinical management algorithms for bedside users (e.g., clinical care team) 7) Identify physiologic thresholds and other findings that would trigger clinical action or judgement 8) Access to a standardized lexicon of physiologic patterns with biological or clinical relevance 9) Enlist staff and/or trainees to provide technical and clinical expertise at any time 10) Staff member to act as a “clinical champion” to encourage the use of monitoring 11) Directly engage multiple stakeholders involved in day-today care 12) Schedule regularly held multidisciplinary case conferences to discuss monitoring cases |
|
| |
| Education Formats | Training Background and Expertise |
|
| |
| 1) Training and expertise necessary to understand and interpret MNM is best acquired through… • Hands-on workshops or seminars • Clinical practice or bedside teaching • Development of a core curriculum • Supervised performance and demonstration of procedural competency |
1) Specific training or expertise is required to adequately understand and interpret MNM information 2) Clinical training programs in emergency medicine (alone) do not provide adequate knowledge base 3) Clinical training programs in specialty nursing (alone) do not provide adequate knowledge base |
aSAH = aneurysmal subarachnoid hemorrhage, CPT = Current Procedural Terminology, EHR = electronic health record, GCS = Glasgow Coma Scale, ICH = intracerebral hemorrhage, IVH = intraventricular hemorrhage, MNM = multimodality neuromonitoring, TBI = traumatic brain injury.
Agreement was defined as a median Likert score of ≥ 7 or ≤ 3 while consensus was defined as > 70% within the lowest or highest tertile and an interquartile range difference ≤ 1.75. Items achieving consensus during discussion-based round 3 must have a) agreement during round 2 plus b) at least 70% voting strong agreement and < 10% voting strong disagreement.
Contexts of Use
Expert consensus was achieved for clinical factors that are important when considering the utility of MNM, including the patient’s level of consciousness, underlying disease state, and potential risk for secondary brain injuries. There was consensus that MNM is best used to guide individualized management, including abstention from harmful therapies. There was neither agreement nor disagreement about whether or not prognosis or age should impact the utility of MNM.
For both invasive and noninvasive monitoring strategies, there was consensus for the use of MNM in comatose patients with TBI, aSAH, or supratentorial intracerebral hemorrhage (ICH). For case-based scenarios involving patients with a Glasgow Coma Scale score of 9–12, experts could neither agree nor disagree on the utility of invasive and noninvasive MNM. No case-based scenarios achieved consensus for the use of noninvasive MNM alone. However, pediatric specialists differed from adult specialists in the utility of MNM for: a) patients with early status myoclonus postcardiac arrest (pediatric specialists median 7.5, IQR 7–8 vs adult specialists median 7, IQR 6–8; p = 0.03), b) patients requiring venoarterial extracorporeal membrane oxygenation (ECMO) (pediatric specialists median 7.5, IQR 7.5–8.0 vs adult specialists median 6, IQR 5–7; p < 0.01), and c) patients requiring venovenous ECMO (pediatric specialists median 7, IQR 7–7 vs adult specialists median 6, IQR 4–7; p = 0.02).
Minimum Necessary Monitors, Devices, and Technologies
There were 10 invasive and noninvasive monitors and devices considered important for MNM and many were also agreed upon as important across several specific clinical contexts of use (Table 2; and Supplemental Fig.1, http://links.lww.com/CCM/H385). There was agreement, but not consensus, that cerebrovascular autoregulatory indices (e.g., pressure reactivity index or tissue oxygenation index), optimum cerebral perfusion pressure (CPPopt), and quantitative electroencephalography are also important. Near-infrared spectroscopy (NIRS) and extended-duration transcranial Doppler (TCD) were agreed upon only by pediatric specialists.
TABLE 2.
Monitors and Devices for Secondary Brain Injuries
| Overall Consensus for Minimum Necessary Monitors and Devicesa | |
|---|---|
| ICP, CPP, PbtO2, cEEG, quantitative pupillometry, ABP, electrocardiography or cardiac telemetry, continuous core body temperature, ETCO2, plethysmography | |
| Monitors and Devices for Specific Contexts of Use b | |
| Brain tissue hypoxia | ICP, ABP, CPP, cerebral autoregulation, ETCO2, PbtO2 |
| Cerebral ischemia | ICP, ABP, CPP, cerebral autoregulation, CPPopt, ETCO2, PbtO2c |
| Autoregulatory dysfunction | ICP, CPP, cerebral autoregulationc, CPPopt |
| Acute coma or disorders of consciousness | ICP, ABP, CPP, cEEG, qEEG, quantitative pupillometry |
| Postcardiac arrest hypoxic-ischemic brain injury | ABP, cEEG, qEEG, ETCO2 |
| Metabolic crisis or mitochondrial dysfunction | cEEG, cerebral microdialysis |
| Seizures or ictal-interictal continuum patterns | cEEG, qEEG |
| Spreading depolarizations | Depth or strip electrocorticography |
| Intracranial hypertension | ICP, ABP, CPP, cerebral autoregulation, CPPopt, ETCO2, PbtO2, quantitative pupillometry |
ABP = arterial blood pressure, cEEG = continuous electroencephalography, CPP = cerebral perfusion pressure, CPPopt = optimum cerebral perfusion pressure, ETCO2 = end-tidal CO2, ICP = intracranial pressure, PbtO2 = brain tissue oxygen, qEEG = quantitative electroencephalography.
Consensus was defined as > 70% within the lowest or highest tertile and an interquartile range difference ≤ 1.75. Items achieving consensus during discussion-based round 3 had a) agreement during round 2 plus b) at least 70% voting strong agreement and < 10% voting strong disagreement.
Agreement on multiple selection items defined as selection of the item by at least two of three participants. These were not considered for consensus per se.
All adult specialists selected PbtO2 as useful to detect and guide management of cerebral ischemia in contrast to four of six pediatric specialists (67%) (p = 0.03). Similarly, 28 of 29 adult specialists (97%) selected cerebral autoregulatory measurements as useful for autoregulatory dysfunction compared with three of six pediatric specialists (50%) (p = 0.01).
Consensus-based technologies necessary for MNM include bedside displays of single and multiple values and trends over time displayed in time-locked fashion on a single visual display; access to high-resolution data; and the ability to manipulate data displays at bedside (i.e., scrolling or zooming in and out of different timescales). Bedside displays of summary data, an ability to set thresholds or alerts, and the capability to annotate MNM data in real-time to denote clinical events achieved consensus. The need for real-time remote review of MNM data alongside annotated clinical events, and an ability to access high-resolution data independent of bedside devices also reached consensus.
Minimum Necessary Clinical Effort
There was consensus that integration and interpretation of MNM data requires specific skill and expertise and that ICU providers (in general) do not have adequate time to integrate and interpret MNM during daily clinical care. Integration of both brain and cardiopulmonary measurements is essential along with the ability to manipulate, analyze, and interpret these data to provide clinical correlation. There was consensus that most ICU providers would find regularly written reports summarizing and interpreting MNM data helpful for decision-making during daily clinical care (Supplemental Fig. 2, http://links.lww.com/CCM/H385).
Operationalizing Neuromonitoring
Consensus addressing barriers to the implementation of MNM included the need for bedside interfaces to facilitate clinical understanding of MNM information and investment in the education of bedside users (e.g., the clinical care team) to better understand and respond to MNM information. There was agreement, but not consensus, that dedicated personnel with technical expertise (e.g., a neuromonitoring technologist) and a MNM “reader” could be helpful in implementing MNM. Experts reached consensus on the need for consistency in identifying which patients require invasive or noninvasive MNM and which specific technologies should be used. There was consensus that local practice standards should be developed by engaging a multidisciplinary group of stakeholders involved in the clinical care of patients undergoing MNM.
Training Background and Educational Opportunities
There was consensus that specific training is required to develop expertise in the interpretation of MNM data, although there was no consensus regarding the type of training programs that presently provide this foundation. Approaches to education include hands-on workshops, supervised performance, and clinical practice. Agreement was reached on nine core concepts critical for an adequate knowledge base to interpret MNM data (Fig. 2). Finally, there was agreement but not consensus that expertise should be recognized via certification, through either a working group or an established society.
Figure 2.
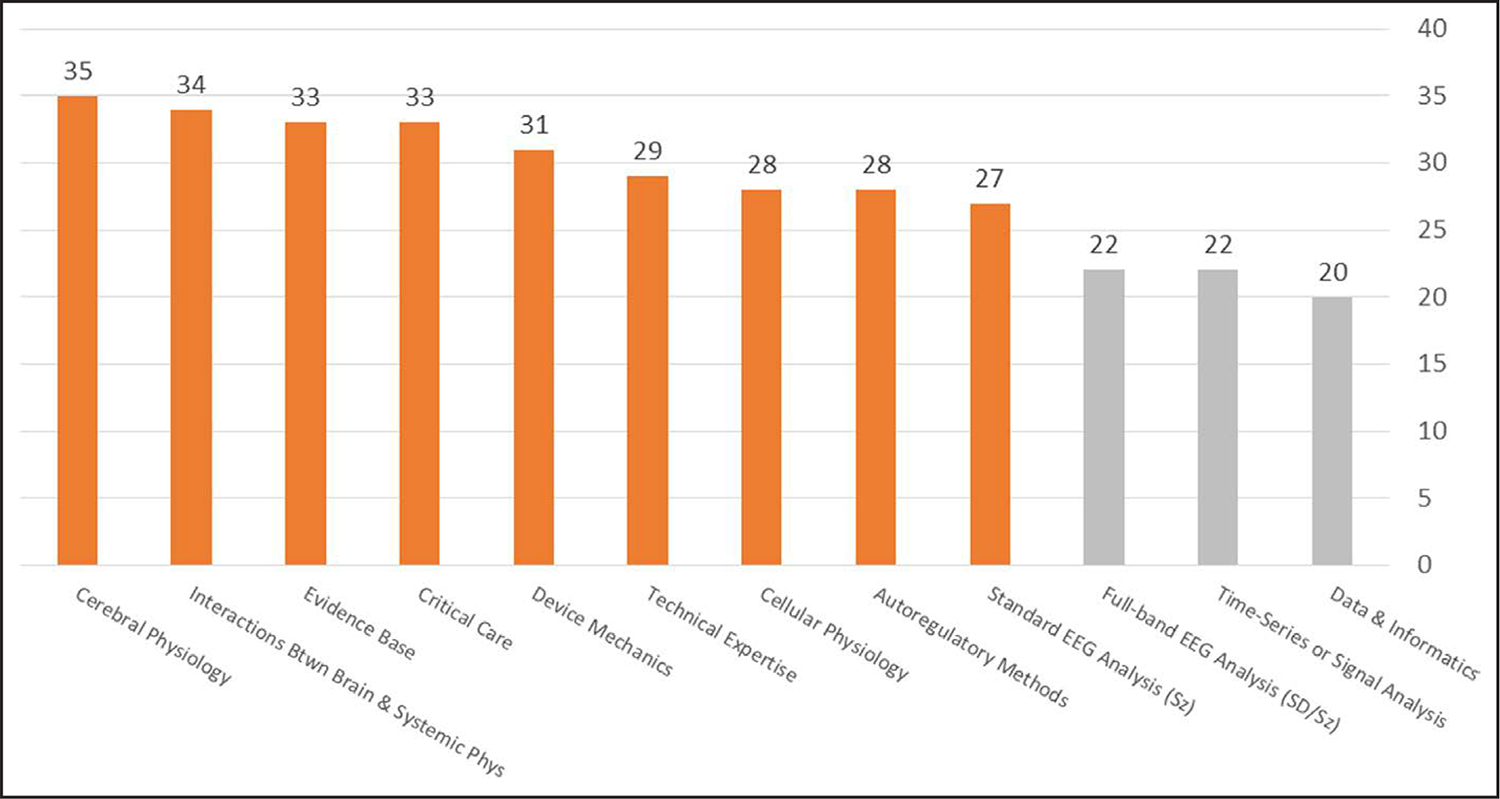
Core concepts necessary for clinical neuromonitoring. Participants were asked to select each core concept that was felt to be critically important for a clinician to have an adequate knowledge base for understanding and interpreting multimodality neuromonitoring information. Concepts in orange achieved agreement, defined as selection by greater than two of three participants; those in light gray did not meet the threshold for agreement. The y-axis reflects the number of participants that selected each concept out of a total of 35.
EEG = electroencephalography, sd = spreading depolarizations, Sz = seizures.
DISCUSSION
This Delphi process identified several broad areas of consensus concerning the practice of MNM. Consensus was achieved regarding the utility of MNM for clinical decision-making and the need for consistency in patient selection and the modalities used for clinical care. Our consensus process identified essential technologies for providing MNM. Experts agreed that MNM should be accompanied by the integration and interpretation of MNM information, which requires time and expertise independent of the work of daily clinical care. Our findings are summarized as a framework for MNM practice standards based on expert input (Table 3).
TABLE 3.
Multimodality Neuromonitoring: A Proposed Framework
| Indications for MNM |
|---|
|
|
| Indications for MNM include patients at-risk for secondary brain injuries, such as: |
| 1) Nonsurgical traumatic brain injury in patients who remain comatose after initial critical care resuscitation and management |
| 2) Surgical traumatic brain injury in patients who remain comatose after appropriate evacuation and/or decompression |
| 3) Aneurysmal subarachnoid hemorrhage in patients who remain comatose after initial critical care resuscitation and management or with signs or symptoms of delayed cerebral ischemia |
| 4) Supratentorial intracerebral hemorrhage with or without intraventricular hemorrhage who remain comatose after initial critical care resuscitation and management |
| Additional indications for MNM may be warranted based on the clinical scenario. |
| Minimum Necessary Technologies |
|
|
| 1) A minimum set of continuousa physiologic bedside measurements should be used for focused disease or clinical states (e.g., traumatic brain injury or coma). This must include: |
| a) At least two brain-focused measurements, either invasive or noninvasive, in any combination of the following: |
| i) Intracranial pressure and/or blood flow, including but not limited to: |
| 1) Parenchymal intracranial pressure monitors |
| 2) External ventricular drainage devices |
| 3) Regional cerebral blood flow |
| 4) Extended-duration (> 30 min) or frequent (> 1 daily) transcranial Doppler ultrasonography |
| ii) Oxygenation and/or metabolism, including but not limited to: |
| 1) Brain tissue oxygen monitors |
| 2) Jugular venous oxygen monitors |
| 3) Regional oxygen saturation or other optical imaging technology |
| 4) Cerebral microdialysis |
| iii) Electroencephalography over long-time scales (e.g., quantitative electroencephalography) or using full-band (DC or near-DC) amplifiers not routinely available via commercial epilepsy monitoring systems |
| iv) Quantitative pupillometry |
| plus, |
| b) At least one systemic cardiopulmonary physiologic measurement, either invasive or noninvasive: |
| i) Arterial blood pressure |
| ii) Continuous cardiac output monitoring |
| iii) End-tidal CO2 |
| iv) Tidal volume, inspiratory pressure, or minute ventilation |
| c) Additional measurements within each criterion or outside of these criteria may be included as part of MNM; there is no maximum set of measurements |
| 2) A minimum of two measurements, at least one from each category above, must be: |
| a) integrated within a single platform |
| b) time-synchronized |
| c) displayed together at bedside |
| d) user-accessible at maximum resolution, including waveforms as applicable |
| 3) Clinical data must be integrated with physiologic measurements, either though bedside annotations or information from the electronic health record |
| Indications for MNM |
|
|
| For example, the routine use or data capture of continuous physiologic bedside measurements in unselected groups of patients is not included in the criteria for minimum necessary technologies. These include: |
| a) Use of continuous video electroencephalography as deployed for patients across the hospital system |
| b) Continuous cardiac telemetry |
|
|
| Standards for interpretation and reporting |
| 1) MNM data defined above must be reviewed in its entirety by a provider with expertise and/or competency in cerebral physiology using bedside and/or remote data visualization platforms that include: |
| a) An ability to review data across multiple time scales |
| b) Processing and/or use of analytic tools not available from source devices |
| c) Access to time-synchronized clinical events, e.g., annotations indicating provocative bedside maneuvers or medication administration |
| 2) MNM reviewers must interpret data and provide a written summary including, but not limited to, the following: |
| a) Correlation between multiple related physiologic measurements |
| b) Identification of clinically relevant trends or changes over time |
| c) Synthesis of multiple measurements summarizing pathophysiologic state or condition of the patient during monitoring |
| 3) I ndividualized interpretation and/or clinical recommendations must be documented in a way that clinical care teams can access and act upon, e.g. within the electronic health record |
DC = direct current, MNM = multimodality neuromonitoring.
“Continuous” is defined by data sampled no less frequently than every 6 hr. The majority of devices that fulfill this criterion are sampled more frequently, and there should be a preference for waveform or second-to-second data where applicable.
We identified important clinical considerations regarding the utility of MNM. While some guidelines (27, 28) and an increasing number of clinical studies (29) highlight the utility of MNM to guide clinical management, experts in our Delphi process also considered MNM to be useful specifically to abstain from or de-escalate potentially harmful therapies. This consensus is supported by results from the Benchmark Evidence from South American Trials: Treatment of Intracranial Pressure study (30), which found that the use of invasive ICP monitoring allows for de-escalation or limitation of potentially harmful therapies, for example, paralytics or increased sedation. The Brain Oxygen Optimization in Severe Traumatic Brain Injury-II study (31) reported fewer interventions in the MNM ICP/Pbto2 arm (n = 867 interventions) versus ICP-only arm (n = 933 interventions).
Our consensus process also identified indications for MNM—using invasive or noninvasive modalities—reaffirming existing literature, focused on comatose patients with severe TBI (sTBI), aSAH, or ICH. However, experts did not reach consensus on any case-based scenario for which noninvasive modalities alone would be preferred. Prior consensus from an international group of mostly adult intensive care experts (1) viewed invasive ICP monitoring as a prerequisite for the interpretation of MNM, whereas a pediatric intensive care survey found noninvasive modalities were more commonly used (2). Broader indications for MNM have been described in pediatric intensive care including patients with hypoxic-ischemic injuries or undergoing ECMO. In our study, experts agreed MNM might be useful in these scenarios, but consensus was only achieved by pediatric specialists. Expanded indications for MNM in other ICU settings, including adult patients undergoing ECMO (32) or those with other critical care disorders for which patients are at-risk for secondary brain injury, are likely possible if noninvasive modalities are more frequently employed.
There was consensus that invasive (ICP, cerebral perfusion pressure, Pbto2) or noninvasive (cEEG, quantitative pupillometry) modalities were necessary for MNM in conjunction with cardiopulmonary measurements (arterial blood pressure [ABP], ECG, temperature, Spo2, and end-tidal co2 [ETco2]). There was agreement, but not consensus, that measures of cerebral autoregulation (both indices and calculation of CPPopt) were important. This may reflect the findings highlighted by a recent Delphi process, which found lack of expert consensus in whether and how to include these measures yet in clinical practice despite their importance in adults with sTBI (33). Rather, these and other specific measures such as electrocorticography and cerebral microdialysis (CMD) held agreement in several specific contexts. There is tremendous variability in the use and availability of brain-specific modalities. In a European multicenter TBI-focused practice survey, fewer than one-quarter of institutions considered invasive monitoring in patients with coma and negative CT or patients with abnormal CT who could not be assessed (7), scenarios for which we achieved consensus that MNM would be useful. In a survey of primarily academic centers mostly in North America (72%), 58% reported use of cEEG compared with fewer than 5% of European TBI centers (5, 7). The use of TCD has been reported by 38–49% of centers, Pbto2 by 15–26%, NIRS by 0–19%, rCBF by 4–5%, jugular venous oximetry by 3–9%, CMD by 2–13%, and autoregulatory indices by less than 5% (5–8). Practitioner-dependent variability also exists: neurointensivists are more likely than other intensivists to use TCD, Pbto2, or rCBF (5). However, there is consistency in the use of cardiopulmonary parameters, as most centers across surveys used ABP (77–93%), ETco2 (up to 90%), or cardiac output monitoring to guide management (26–53%) (5–7).
Experts in our study reached consensus that MNM data should be integrated and available in a single visual display both at bedside and remotely to facilitate review across multiple timescales. In a survey of pediatric intensive care centers, only eight of 52 centers (15%) used a platform to integrate multimodality information (2) suggesting this is an under-recognized need for the use of MNM. We also achieved consensus that integration of MNM information and its clinical interpretation requires specific skill and expertise. Prior Delphi statements focused on single devices supported standardization of implementation and interpretation by specially trained experts (22, 34). Prior consensus similarly endorsed interpretation of MNM by practitioners with rigorous training and expertise (1). Current use of MNM relies on limited evidence and conflicting conclusions regarding relationships between multiple measurements (35). There is risk to using inaccurately interpreted information for automated analytic algorithms and smart alarms recommended by prior expert consensus (1). Our experts reached consensus that a curriculum including identified core concepts would allow development of management algorithms, identification of physiologic thresholds, and creation of a standardized lexicon of patterns that occur within integrated MNM data. This idea of leveraging standardization and training paradigms to enable clinical correlation of novel observations has been successful in critical care electroencephalography, where standardized terminology (36) has led to multiple practice-changing studies.
Finally, there was consensus that the expertise employed to use and maintain necessary technologies, interpret MNM information, and report observations in clinic context requires effort independent of daily clinical care. A multicenter survey of international TBI centers reported the time and resource cost of MNM is often underestimated (37). Expert consensus agreed the daily work of intensive care precluded the time required to adequately interpret MNM information and that dedicated interpretation and reporting of MNM information to clinical teams was not captured by existing procedural codes. Experts agreed with development of a standardized framework for dedicated MNM interpretation and reporting to support multidisciplinary care teams (4, 38, 39). This paradigm was recently implemented in a pediatric intensive care population where MNM uniformly influenced care decisions, reducing the duration of invasive monitoring and mechanical ventilation (39).
There were several limitations to our study. First, there is no set of formal requirements for Delphi processes (22) in the era of remote teleconferencing. The response rate from invited experts was lower than the 90% (IQR, 80–100%) response rates reported in a systematic review of Delphi consensus processes in healthcare (21). However, the 35 participants in our study were double the median of 17 (IQR, 11–31) participants in other Delphi processes (21). We chose to exclude continuous, noninvasive ICP measurements insufficiently validated for clinical use (15) and other emerging technologies. Familiarity with existing devices may have influenced expert preferences, and the limited evidence base for MNM may have biased consensus regarding contexts of use. We had broad representation among experts but were limited in our ability to generalize areas of consensus to pediatric intensive care. We did not address emerging economies with unique needs and resources. Finally, we acknowledge that not all brain monitoring modalities are equivalent: different risk/benefit thresholds exist for the use of invasive versus noninvasive modalities, and some may be more helpful than others to evaluate specific pathology.
CONCLUSIONS
This Delphi process provides expert consensus supporting practice standards for the use of MNM to guide individualized intensive care for at-risk patients. We provide a framework informed by areas of consensus to guide the selection of technologies necessary for MNM and establish that the effort required to integrate and interpret MNM information is independent from daily clinical care. This consensus statement also provides avenues to enhance implementation of MNM and provide training and education for its broader use.
Supplementary Material
KEY POINTS.
Question:
What consensus exists for the use of multimodality neuromonitoring (MNM) in clinical care?
Findings:
MNM requires skill and expertise to integrate and interpret information consistently across clinical scenarios using a minimum set of technologies to guide and individualize management.
Meaning:
Practice standards are needed to best use MNM, and we provide expert consensus to support these standards.
DEFINITIONS USED FOR THE DELPHI PROCESS.
Multimodality neuromonitoring (MNM)
“Neuromonitoring” refers to the use of any frequent (ideally continuous) measure of brain physiology that can be obtained at the bedside to detect clinically important events in real-time. “Multimodality” refers to the use of more than one source of measurements for a more comprehensive assessment of the brain, implying a higher level of complexity reserved for selected at-risk patients, typically in an intensive care setting in patients with limited neurological examination. MNM is distinct from neurodiagnostic approaches such as radiological tests or tests ordered infrequently or as-needed, such as somatosensory evoked potentials or serum-based biomarkers.
Contexts of use
Broadly, contexts of use include the users, tasks, equipment, and both physical and social environments in which a system of service is used. In this case, contexts refer to the medical environment, including the type of problem that a patient may have for which MNM might be useful or helpful.
Data
The set of integrated measurements collected during the course of MNM which can be used for review, manipulation, or analysis.
Devices
Technologies, typically hardware, used to generate measurements used for brain monitoring by interfacing directly with the patient such as intraparenchymal strain gauge catheters, optical imaging pads, or electrodes and amplifiers.
Measurements
The quantifiable parameters that form one of a set of numerical data that defines and sets conditions for a system, in this case the brain and its neurophysiology.
Modalities
The strategies used to monitor the brain, including routine vital sign monitoring, noninvasive technologies such as scalp electroencephalography, and invasive approaches such as intracranial pressure monitoring.
Monitors
Hardware that records the output of devices locally, typically within a patient’s room. Examples include intracranial pressure monitors, electroencephalography systems, and bedside vital sign monitors.
Technologies
Any hardware or software that is applied for practical purposes to MNM.
ACKNOWLEDGMENTS
We wish to acknowledge each of the participants who provided their time and expertise for this Delphi consensus process.
Funding was provided by U.S. Department of Defense (W81XWH-18-DMRDP-PTCRA; to Drs. Foreman and Rosenthal) and by the National Institutes of Health (OD OT2OD032701; to Dr. Rosenthal).
Footnotes
Dr. Foreman’s institution received funding from the U.S. Department of Defense (DoD) (W81XWH-18-DMRDP-PTCRA); he received funding from Marinus Pharmaceuticals; he disclosed that he is on the Scientific Advisory Committee for the Neurocritical Care Society Curing Coma Campaign. Drs. Foreman and Appavu perform dedicated neuromonitoring services locally. Drs. Foreman and Rosenthal received Institutional support through U.S. Army W81XWH-18-DMRDP-PTCRA through parent award to Moberg Analytics. Drs. Foreman and Gilmore received funding from UCB Pharma. Drs. Foreman and Wainwright received funding from SAGE Therapeutics. Dr. Ngwenya’s institution received funding from Abbott and Biogen; she received funding from General Dynamics Information Technology/DoD. Dr. O’Phelan received funding from Bard Medical CEC. Dr. LaRovere disclosed that she has U.S. National Phase Applications (No.: 17/601,603, No.: US-2022–0181008-A1, Ref. No.: 21233 CMCC, Ref. No.: 3440 WGS, Ref. No.: M0437.70143US01 Patent—Issued). Dr. Appavu’s institution received funding from the U.S. DoD Congressionally Directed Medical Research Programs and the American Heart Association (AHA). Drs. Alkhachroum and Rosenthal received support for article research from the National Institutes of Health (NIH). Dr. Amorim received funding from the AHA (20CDA35310297, 83457), the CURE Epilepsy Foundation (Taking Flight Award), the NIH (1K23NS090900), the Hellman Fellows Fund, the Regents of the University of California (Resource Allocation Program), Cures Within Reach, and the Zoll Foundation. Dr. Gilmore received funding from the American Academy of Neurology and Caring Analytics Platform (CARPL.ai); she serves as Director of Neuromonitoring locally; co-founded Intracranial Bio Analytics; and holds NIH grant funding for development of a multimodal intracranial monitoring device and data visualization platform (UG3 NS123307). Dr. Rosenthal’s institution received funding from the NIH, the U.S. Army, Moberg Analytics, and Marinus Pharmaceuticals. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
REFERENCES
- 1.Le Roux P, Menon DK, Citerio G, et al. : Consensus summary statement of the International Multidisciplinary Consensus Conference on Multimodality Monitoring in Neurocritical Care: A statement for healthcare professionals from the Neurocritical Care Society and the European Society of Intensive Care Medicine. Neurocrit Care 2014; 21(Suppl 2):S1–S26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirschen MP, LaRovere K, Balakrishnan B, et al. ; Pediatric Neurocritical Care Research Group (PNCRG): A survey of neuromonitoring practices in North American Pediatric Intensive Care Units. Pediatr Neurol 2022; 126:125–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Citerio G, Oddo M, Taccone FS: Recommendations for the use of multimodal monitoring in the neurointensive care unit. Curr Opin Crit Care 2015; 21:113–119 [DOI] [PubMed] [Google Scholar]
- 4.Foreman B, Ngwenya LB: Sustainability of applied intracranial multimodality neuromonitoring after severe brain injury. World Neurosurg 2019; 124:378–380 [DOI] [PubMed] [Google Scholar]
- 5.Sivakumar S, Taccone FS, Rehman M, et al. : Hemodynamic and neuro-monitoring for neurocritically ill patients: An international survey of intensivists. J Crit Care 2017; 39:40–47 [DOI] [PubMed] [Google Scholar]
- 6.Wijayatilake DS, Talati C, Panchatsharam S: The monitoring and management of severe traumatic brain injury in the United Kingdom: Is there a consensus?: A national survey. J Neurosurg Anesthesiol 2015; 27:241–245 [DOI] [PubMed] [Google Scholar]
- 7.Cnossen MC, Huijben JA, van der Jagt M, et al. ; CENTER-TBI investigators: Variation in monitoring and treatment policies for intracranial hypertension in traumatic brain injury: A survey in 66 neurotrauma centers participating in the CENTER-TBI study. Crit Care 2017; 21:233–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Godoy DA, Carrizosa J, Aguilera S, et al. ; Latin America Brain Injury Consortium (LABIC) Members: Current practices for intracranial pressure and cerebral oxygenation monitoring in severe traumatic brain injury: A Latin American Survey. Neurocritical Care 2023; 38:171–177 [DOI] [PubMed] [Google Scholar]
- 9.Francoeur CL, Pain M, Mayer SA: Multimodality monitoring: Illuminating the comatose human brain. Semin Neurol 2016; 36:560–569 [DOI] [PubMed] [Google Scholar]
- 10.Roh D, Park S: Brain multimodality monitoring: Updated perspectives. Curr Neurol Neurosci Rep 2016; 16:56–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fan TH, Rosenthal ES: Physiological monitoring in patients with acute brain injury: A multimodal approach. Crit Care Clin 2023; 39:221–233 [DOI] [PubMed] [Google Scholar]
- 12.Sinha S, Hudgins E, Schuster J, et al. : Unraveling the complexities of invasive multimodality neuromonitoring. Neurosurg Focus 2017; 43:E4. [DOI] [PubMed] [Google Scholar]
- 13.Lindblad C, Raj R, Zeiler FA, et al. : Current state of high-fidelity multimodal monitoring in traumatic brain injury. Acta Neurochir (Wien) 2022; 164:3091–3100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rasulo FA, Togni T, Romagnoli S: Essential noninvasive multimodality neuromonitoring for the critically ill patient. Crit Care 2020; 24:100–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Mufti F, Smith B, Lander M, et al. : Novel minimally invasive multi-modality monitoring modalities in neurocritical care. J Neurol Sci 2018; 390:184–192 [DOI] [PubMed] [Google Scholar]
- 16.Foreman B, Lissak IA, Kamireddi N, et al. : Challenges and opportunities in multimodal monitoring and data analytics in traumatic brain injury. Curr Neurol Neurosci Rep 2021; 21:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCredie VA, Chavarria J, Baker AJ: How do we identify the crashing traumatic brain injury patient - the intensivist’s view. Curr Opin Crit Care 2021; 27:320–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Veldeman M, Albanna W, Weiss M, et al. : Invasive multimodal neuromonitoring in aneurysmal subarachnoid hemorrhage: A systematic review. Stroke 2021; 52:3624–3632 [DOI] [PubMed] [Google Scholar]
- 19.Roh DJ, Morris NA, Claassen J: Intracranial multimodality monitoring for delayed cerebral ischemia. J Clin Neurophysiol 2016; 33:241–249 [DOI] [PubMed] [Google Scholar]
- 20.Beekman R, Maciel CB, Balu R, et al. : Neuromonitoring after cardiac arrest: Can twenty-first century medicine personalize post cardiac arrest care? Neurol Clin 2021; 39:273–292 [DOI] [PubMed] [Google Scholar]
- 21.Boulkedid R, Abdoul H, Loustau M, et al. : Using and reporting the Delphi method for selecting healthcare quality indicators: A systematic review. PLoS One 2011; 6:e20476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Brien NF, Reuter-Rice K, Wainwright MS, et al. : Practice recommendations for transcranial Doppler ultrasonography in critically ill children in the pediatric intensive care unit: A multidisciplinary expert consensus statement. J Pediatr Intensive Care 2021; 10:133–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guyatt GH, Oxman AD, Kunz R, et al. ; GRADE Working Group: What is “quality of evidence” and why is it important to clinicians? BMJ 2008; 336:995–998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turnbull AE, Sepulveda KA, Dinglas VD, et al. : Core domains for clinical research in acute respiratory failure survivors: An international modified Delphi consensus study. Crit Care Med 2017; 45:1001–1010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trevelyan EG, Robinson N: Delphi methodology in health research: How to do it? Eur J Integr Med 2015; 7:423–428 [Google Scholar]
- 26.Kalaian SA, Kasim RM: Terminating sequential Delphi survey data collection. Pract Assess Res Eval 2012; 17:n5 [Google Scholar]
- 27.Chesnut R, Aguilera S, Buki A, et al. : A management algorithm for adult patients with both brain oxygen and intracranial pressure monitoring: The Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med 2020; 46:919–929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hawryluk GWJ, Aguilera S, Buki A, et al. : A management algorithm for patients with intracranial pressure monitoring: The Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC). Intensive Care Med 2019; 45:1783–1794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tas J, Czosnyka M, van der Horst ICC, et al. : Cerebral multimodality monitoring in adult neurocritical care patients with acute brain injury: A narrative review. Front Physiol 2022; 13:1071161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chesnut RM, Temkin N, Carney N, et al. ; Global Neurotrauma Research Group: A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med 2012; 367:2471–2481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okonkwo DO, Shutter LA, Moore C, et al. : Brain oxygen optimization in severe traumatic brain injury phase-II: A phase II randomized trial. Crit Care Med 2017; 45:1907–1914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park S, Robba C, Sonneville R: Neuromonitoring for prognostication under ECMO. Intensive Care Med 2023; 49:451–454 [DOI] [PubMed] [Google Scholar]
- 33.Depreitere B, Citerio G, Smith M, et al. : Cerebrovascular autoregulation monitoring in the management of adult severe traumatic brain injury: A Delphi consensus of clinicians. Neurocrit Care 2021; 34:731–738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rasulo FA, Hopkins P, Lobo FA, et al. : Processed electroencephalogram-based monitoring to guide sedation in critically ill adult patients: Recommendations from an international expert panel-based consensus. Neurocrit Care 2022; 38:296–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lazaridis C, Andrews CM: Brain tissue oxygenation, lactate-pyruvate ratio, and cerebrovascular pressure reactivity monitoring in severe traumatic brain injury: Systematic review and viewpoint. Neurocrit Care 2014; 21:345–355 [DOI] [PubMed] [Google Scholar]
- 36.Hirsch LJ, Fong MWK, Leitinger M, et al. : American Clinical Neurophysiology Society’s Standardized Critical Care EEG Terminology: 2021 Version. J Clin Neurophysiol 2021; 38:1–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rodriguez A, Smielewski P, Rosenthal E, et al. : Medical device connectivity challenges outline the technical requirements and standards for promoting big data research and personalized medicine in neurocritical care. Mil Med 2018; 183:99–104 [DOI] [PubMed] [Google Scholar]
- 38.Foreman B, Ngwenya LB, Stoddard E, et al. : Safety and reliability of bedside, single burr hole technique for intracranial multimodality monitoring in severe traumatic brain injury. Neurocrit Care 2018; 29:469–480 [DOI] [PubMed] [Google Scholar]
- 39.Appavu B, Burrows BT, Nickoles T, et al. : Implementation of multimodality neurologic monitoring reporting in pediatric traumatic brain injury management. Neurocrit Care 2021; 35:3–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


