Abstract
Introduction
Retained shrapnel from gunshots is a common occurrence; however, retained shrapnel within the spinal canal is exceedingly uncommon. Guidelines for removal and treatment of these cases are a difficult topic, as surgical removal is not necessarily without consequence, and retention can lead to possible further injury or a secondary disease process of plumbism, which can be difficult to diagnose in this population.
Case presentation
This case report provides a unique example of a young patient with retained shrapnel from a gunshot. This patient suffered an initial spinal cord injury due to a gunshot and secondarily presented with abdominal pain, fatigue, elevated blood lead levels, and was diagnosed with plumbism. This was addressed with operative removal of shrapnel and posterior instrumented spinal fusion, resulting in decreased lead levels and symptom resolution postoperatively.
Discussion
Lead toxicity risk in patients with retained shrapnel, particularly in the spine, warrants vigilant monitoring. While management guidelines lack consensus, symptomatic lead toxicity may necessitate intervention. Residual neurological deficits complicate evaluation, emphasizing individualized management decisions.
Subject terms: Neurosurgery, Pathology
Introduction
Gunshot injuries continue to be an ongoing issue in the United States, with rates of gunshot-related injuries at an estimated 132,767 requiring emergency care in 2019 [1]. Of these, however, there are far fewer with retained shrapnel and with this the concern for possible lead toxicity [2]. With these retained foreign bodies with extra-articular involvement, there is far less concern for individuals to develop lead toxicity [3]. This is believed to be due to a current theory that fibrous encapsulations form and effectively wall off the lead fragments preventing an immune response and breakdown of the lead, thus stopping lead dissemination to the blood in high levels [3]. However, if these are not walled off these can form fluid filled cysts that are broken down by macrophages, introducing larger quantities of lead into the body [3]. This has been noted to be rare and often bullet fragments can be retained with little or no monitoring of lead levels unless the patient demonstrates symptoms [3]. This theory does not apply to intra-articular spaces or spaces bathed in CSF as these encapsulations can be restricted from forming [4].
Specifically, joints are lined with synovium and have a constant exchange with the rest of the body which can lead to increased absorption of lead ions [4]. Also, fragments can become abrasive to the surrounding joint surfaces causing cartilage damage. Bullet fragment retention within the spinal canal and vertebral column has a paucity of data. Overall, lead toxicity or plumbism are recorded at very low rates around 8% [5, 6]. The low rate despite being directly adjacent to cerebral spinal fluid is thought that there is an encapsulation that can occur with fibrous tissue similar to other extra-articular soft tissue injuries due to these spaces being relatively avascular [6].
Plumbism itself is defined as elevated blood lead levels >5 μg/dl, in addition to symptoms of fatigue, headache, anemia, abdominal pain, nausea, renal failure, encephalopathy, or peripheral neuropathy; however, most patients are symptomatic generally when levels are higher than 24 μg/dl [7, 8]. These symptoms can often not present initially as some patients become symptomatic many years later [3, 7, 8]. This delayed presentation has been attributed to firstly to the extended half-life of lead being 1–2 months in soft tissues and up to a decade within bone, and secondly the encapsulations having a delayed immune response with macrophages that absorb and transport this stored lead to the bloodstream [3, 7, 9]. Although exact triggers of these late immune responses are not well known, it is possible that episodes of increased metabolic stress can contribute [8]. In spinal injury patients these symptoms can also be superimposed by neurologic compromise due to residual neurologic deficits.
The general management of gunshot wound patients varies based on location of the retained bullet. Operative removal is indicated in cases of intra-articular retention, bullets in the globe of the eye, bullets impinging on a nerve or nerve root, bullets in the lumen of a vessel causing ischemia, and finally, in cases of lead poisoning. However, there is no unified opinion on the removal of bullets in patients with spinal cord injury. Although a perfect consensus has not been reached at this time, current school of thought in patients who have lead within their bodies is to test for venous lead levels if they become symptomatic [3, 8].
To add to this literature, this case study presents a patient who suffered a gunshot wound to the spine, with noted retained bullet fragments within the canal. He became symptomatic, with confirmed elevated blood lead levels that required interventional treatment.
Case presentation
This patient was a 10-year-old male with a history of ASIA A T11 paraplegia secondary to a gunshot wound to his thoracic spine. The patient was shot in the back and right knee and underwent exploratory laparotomy (Ex-lap) and decompression laminectomy of T11-12 in Mexico. The bullet fragments in his spinal canal and knee were not removed by his surgery team in Mexico at that time. He presented to our institution with additional symptoms: abdominal pain, decreased appetite, decreased frequency of bowel movements, somnolence, headaches, and fatigue. Upon further evaluation, he was found to have pyelonephritis (likely a sequela of his neurogenic bladder), but given the patient’s known secondary retained bullet fragment and nonspecific symptoms of abdominal pain, headaches, fatigue his serum lead levels were measured and found to be elevated at 16.4 μg/dl (nl <4 μg/dl). It is important to note that his neurologic deficits made it more difficult to determine whether he was suffering from these symptoms as a result of elevated lead levels, or whether they were secondary to his spinal cord injury; additionally, his injury may mask certain lead poisoning symptoms. In general lead poisoning can present with symptoms of joint pain, anemia, peripheral paresthesias, abdominal pain, constipation, headache, fatigue, signs of encephalopathy, and attention deficit and behavioral alterations [5]. In this patient lacking sensation or motor function below T11, it is hard to ascertain new neurologic findings below the injury such as weakness or decreased coordination in his lower extremities as this preexisting deficit is a significant limiter of the exam. Additionally, symptoms such as his abdominal pain and decreased bowel movement frequency could be attributed to his neurogenic bladder and bowel secondary to his spinal trauma or alternatively constipation secondary to his elevated lead levels. Thus, to most accurately assess for new neurologic findings in patients with plumbism superimposed with spinal trauma, it is best to evaluate symptoms that are independent of preexisting deficits, as evaluating below these insults can be difficult.
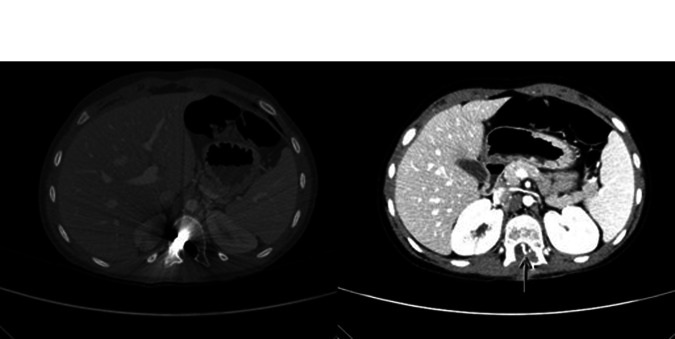
Further, radiographs (Fig. 1) and computed tomography (CT) scans demonstrate retained bullet fragment in the T11 vertebral body and intra-dural shrapnel fragments, as well as post laminectomy kyphosis at T11-T12 (Fig. 2). CT scans also demonstrated retained extra-articular bullet fragment in patient’s right knee. The physical exam revealed neurological deficits, including absent strength and reflexes in the patient’s lower extremities, as well as neurogenic bladder and bowel. Because of this, patient is wheelchair and catheter dependent.
Fig. 1. Pre-operative full spine X-rays.

AP (left) and lateral (right) scoliosis radiographs displaying retained bullet fragment.
Fig. 2. Pre-operative advanced imaging.
(Left) Pre-operative computed tomography (CT) scan displaying metallic bullet in the right vertebral body of T11. (Right) Magnetic resonance imaging displaying metallic and bony fragments in the spinal canal around the T12 level.
The patient was referred to be seen at an outpatient pediatric spine clinic, and a multidisciplinary team determined that due to the potential of the shrapnel fragments to leach lead into the patient’s blood stream, that it was the best course of action to proceed with an operative removal of the bullet fragments from within the patient’s spinal canal and intra-discal space [2]. It was also determined that because the bullet fragment in the patient’s right knee is extra-articular and thus of low concern for leeching lead into his blood stream removal would only be necessary for the fragments within the patient’s spine [3]. Additionally, a spinal fusion was determined to be necessary to treat the patient’s post-laminectomy kyphosis due to the patient’s significant growth potential and the high risk of progressive deformity.
Operative procedure
Surgical intervention utilized his previous posterior approach. The previously decompressed thoracic dura was exposed. The T11 pedicle transverse process and part of the rib were removed. The previous durotomy site was encountered and utilized to enter the dura. Using O-arm guidance, the shrapnel was identified and extracted from within the intra-dural space with addition of partial corpectomy of T11 to provide safe access to the remaining intra-discal shrapnel for removal. followed and interbody arthrodesis of T11-T12 and T10-T11. Additionally, a shard of bone was found longitudinally splitting the spinal cord at the T11-T12 level. Posterior spinal fusion was performed from T7-L3 (Fig. 3). The primary bullet fragment was lodged in the posterior aspect of the T11 vertebral body.
Fig. 3. Post op full spine X-rays.
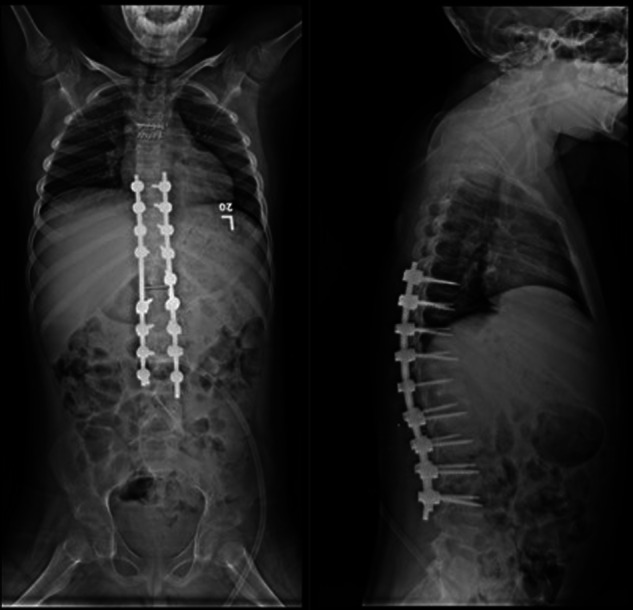
AP (Left) and lateral (Right) views displaying successful bullet fragment removal, and rods and screws from successful T7-L3 spinal fusion.
Postoperative course
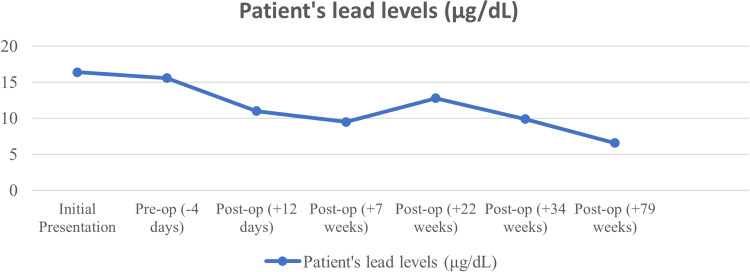
The patient was discharged after 13 days of inpatient care, during which he underwent inpatient rehabilitation to maximize his mobility following spinal fusion and to work on bowel and bladder continence. In the following months, his lead levels were closely monitored and found to have decreased from his most recent preoperative levels. Lead levels decreased from 15.6 μg/dl (4 days preop) to 11.0 μg/dl (12 days postop) to 9.5 μg/dl (7 weeks postop). However, at 22 weeks postop, lead levels unexpectedly rose to 12.8 μg/dl (Fig. 4). His symptoms of abdominal pain, decreased frequency of bowel movements, somnolence, and fatigue had reportedly resolved at this time and did not return with his mild elevation in lead levels. At 26 and 34 weeks postop, the patient continued to be asymptomatic. He reported only mild back pain but also noted the return of sensation to his left thigh at this time. By 34 weeks postop, his lead levels subsequently decreased to 9.9 μg/dl. His most updated lead levels are 6.6 μg/dl at 1.5 years postop (Fig. 4). Although the exact etiology for his unexpected increase in lead levels at 22 weeks post-op was not determined, it could be secondary to the mobilization of lead from various body compartments as a result of increased physiological or psychological stressors [6]. He may have mobilized lead particle remnants as a result of increased physiological stress from a UTI that was reported prior to his 22-week post op spike.
Fig. 4. Patient’s lead levels over time.
Relationship of patient’s systemic lead levels with respect to surgical intervention for bullet fragment extraction.
Discussion
Lead toxicity can be a concern in patients with retained gunshot shrapnel [2]. Current recommendations call for venous lead levels to be measured in patients with retained lead and symptoms of lead toxicity. Symptomatic lead toxicity can occur late, even years after the initial injury [3, 7, 8]. This case demonstrates that prevailing theories that allow for fragment retention and minimal lead level monitoring do not necessarily extend to situations with spinal canal/intradiscal involvement [4].
While it is generally agreed that in cases of bullet retention within a joint, in the globe of the eye, impinging on nerves/nerve roots, in lumens of vessels, or those actively causing lead poisoning management should be removal, there is no current consensus on the management of patients with retained bullet fragments within the spinal canal and intradiscal space [10]. Previous recommendations state that there is not enough evidence to recommend routine removal of retained lead missile to mitigate the risk of lead toxicity [5, 6]. These studies are based on a very limited number of patients, as only five case reports regarding lead toxicity secondary to retained intradiscal bullets have been published. Additionally, spinal injury in these patients can complicate their evaluation, as residual neurological deficits can be superimposed on symptoms of lead toxicity. It is our opinion that determinations regarding the management of these patients should be made on a case-by-case basis, with operative removal being considered in the instances of symptomatically elevated lead levels.
In this case, in which the patient became symptomatic for lead toxicity and had elevated blood lead levels, we felt that operative removal of the retained lead missile from the patient’s spine was necessary to mitigate the risk of worsening lead toxicity.
Conclusion
This case report presents the unique challenges associated with evaluating spinal cord injuries that involve retained foreign bodies and highlights the importance of ruling out lead toxicity from the differential diagnosis, given the potential for this to be overlooked as there can be many other distracting factors clouding the clinical evaluation.
It is our opinion that it is beneficial to surgically remove bullet fragments from the spinal canal/intradiscal space in the setting of elevated serum lead levels in a patient, to prevent worsening of lead toxicity.
Author contributions
Ezekial J Koslosky MD—Conceptualization, Investigation, Writing—Original Draft, Writing Review and Editing, Project Administration. Samuel Oshoba BA—Writing—Original Draft, Writing Review and Editing. Connor Armstrong MD—Investigation, Writing Review, and Editing. Christopher Chaput MD—Conceptualization, Supervision. Matthew Landrum MD—Conceptualization, Writing Review and Editing, Supervision.
Data availability
The data generated or analyzed during this study was made up of several single data points recording this patient’s lead levels over time can be found within the published article and its supplementary files.
Competing interests
The authors declare no competing interests.
Ethics approval
Ethical approval was not required for this case report as it involved the retrospective analysis of de-identified patient data and did not involve any interventions or procedures beyond routine clinical care. Furthermore, the study did not involve any identifiable information, and strict adherence to patient confidentiality was maintained throughout the data collection and reporting process. Thus, no formal ethical approval was sought or obtained for this case report.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
4/29/2024
The last word of the article title has been corrected.
References
- 1.Zwald ML, Holland KM, Bowen DA, Simon TR, Dahlberg LL, Stein Z, et al. Using the centers for disease control and prevention’s national syndromic surveillance program data to monitor trends in us emergency department visits for firearm injuries, 2018 to 2019. Ann Emerg Med. 2022;79:465–73. doi: 10.1016/j.annemergmed.2022.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaufman EJ, Wiebe DJ, Xiong RA, Morrison CN, Seamon MJ, Delgado MK. Epidemiologic trends in fatal and nonfatal firearm injuries in the US, 2009-2017. JAMA Intern Med. 2021;181:237–44. doi: 10.1001/jamainternmed.2020.6696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nickel WN, Steelman TJ, Sabath ZR, Potter BK. Extra-articular retained missiles; is surveillance of lead levels needed? Mil Med. 2018;183:e107–e113. doi: 10.1093/milmed/usx076. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen MP, Reich MS, OʼDonnell JA. Infection and complications after low-velocity intra-articular gunshot injuries. J Orthop Trauma. 2017;31:330–3. doi: 10.1097/bot.0000000000000823. [DOI] [PubMed] [Google Scholar]
- 5.Rentfrow RV, Elia C, Sethi A. Lead toxicity and management of gunshot wounds in the lumbar spine. Eur Spine J. 2013;22:2353–7. doi: 10.1007/s00586-013-2805-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Towner JE, Pieters TA, Maurer PK. Lead toxicity from intradiscal retained bullet fragment: management considerations and recommendations. World Neurosurg. 2020;141:377–82. doi: 10.1016/j.wneu.2020.05.112. [DOI] [PubMed] [Google Scholar]
- 7.Shefa ST, Héroux P. Both physiology and epidemiology support zero tolerable blood lead levels. Toxicol Lett. 2017;280:232–7. doi: 10.1016/j.toxlet.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 8.de Araújo GC, Mourão NT, Pinheiro IN, Xavier AR, Gameiro VS. Lead toxicity risks in gunshot victims. PLoS ONE. 2015;10:e0140220. doi: 10.1371/journal.pone.0140220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitra P, Sharma S, Purohit P, Sharma P. Clinical and molecular aspects of lead toxicity: an update. Crit Rev Clin Lab Sci. 2017;54:506–28. doi: 10.1080/10408363.2017.1408562. [DOI] [PubMed] [Google Scholar]
- 10.Dienstknecht T, Horst K, Sellei RM, Berner A, Nerlich M, HardCastle TC. Indications for bullet removal: overview of the literature, and clinical practice guidelines for European trauma surgeons. Eur J Trauma Emerg Surg. 2012;38:89–93. doi: 10.1007/s00068-011-0170-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated or analyzed during this study was made up of several single data points recording this patient’s lead levels over time can be found within the published article and its supplementary files.