Introduction: Genetic Therapies Are Burgeoning
Rare diseases are not cumulatively rare, given that approximately 1 in 20 people is affected by one of over 7000 known rare diseases.1 Many of these disorders have a genetic basis, and the list of Food and Drug Administration (FDA) approved orphan drugs for rare disease is growing.2 However, therapies are still not available for the majority of rare genetic diseases. This commentary focuses on the growing list of nucleic acid-based technologies being explored for therapeutics, including viral-and nonviral-based gene transfer, gene editing, mRNA and antisense oligonucleotide therapies, which cumulatively lead to growing optimism and require specific knowledge and considerations in the area of rare disease therapeutics. We are referring to these technologies by the term “genetic therapies” throughout this document. New time-sensitive genetic therapies are continuously being developed and in particular could benefit affected babies detected through universal newborn screening. The rapidly growing list of new drugs and gene-based therapies has significant implications for newborn screening, since effective treatment is often the main impediment to adding a condition.3 As of December 2022, 5 gene therapy products have already been granted FDA marketing approval for rare Mendelian diseases in the USA, and several others have been approved outside of the USA. In the coming years, this list is expected to grow substantially given the number of products under development.4
Genetic Therapies Hold Unique Challenges That Require Genetics Expertise
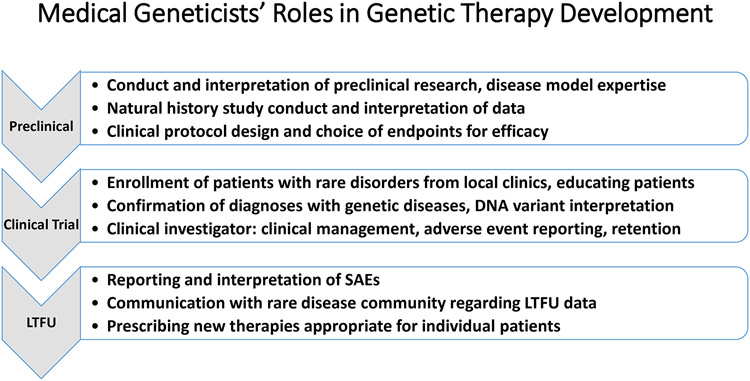
The field of medical genetics is focused on understanding genetic disease, from identification to management and treatment, all of which are critical to the design of therapeutic clinical trials. Clinical trials of genetic therapies for rare Mendelian disorders are fraught with challenges and present a valuable opportunity for enhancing trainee education and faculty development. In particular, data on the natural history of the condition and biomarkers that can be used as therapy endpoints may be limited. Moreover, enrollment may be challenging, given that ~30% of trials involving rare diseases in clinicaltrials.gov were not completed due to difficulties with patient accrual.5 Problems with participant accrual highlight the need for early conversations with relevant stakeholders to ensure realistic and achievable goals for the overall program. Furthermore, diagnosis may require accurate interpretation of genetic variants for diagnosis, and many providers report difficulty with genetic test interpretation.6 As medical geneticists have expertise in the diagnosis of rare disease and genetic test interpretation, knowledge about the natural history of rare genetic disorders, and relationships with patients with rare genetic diseases, partnership with medical geneticists are crucial to genetic therapy development and execution, from an early stage of program development (Figure 1).
Figure 1. Medical geneticists’ roles in genetic therapy development.
Medical geneticists have expertise that supports unique roles in the development of new genetic therapies, prior to study initiation (Preclinical), during clinical development (Clinical Trial), and following marketing approval (LTFU).
LTFU, long term follow-up; SAE, serious adverse events.
Though there are many variables at play, the success of a clinical study program is fundamentally dependent upon establishing appropriate efficacy endpoints, which requires knowledge of the natural history of the relevant disorder. In the realm of rare disorders, development of a body of information that informs the disorder’s natural history frequently requires collaborative studies that enroll large numbers of patients scattered across many institutions. One example of such an initiative is the NIH-sponsored Rare Diseases Clinical Research Networks, which have studied urea cycle disorders, mitochondrial disorders, lysosomal disorders, among others.7 Industry may also play a role in registry programs and clinical trials, and typically geneticists act as advisors and academic partners. Industry-sponsored initiatives have included patient registries for lysosomal storage disorders.8 The above-mentioned programs have largely been initiated and maintained through contributions by medical geneticists in collaboration with a care team that sees patients with genetic diseases. Broad recruitment in longitudinal studies is of particular importance to establish genotype-phenotype correlations that could also inform trial endpoints for specific cohorts of patients within the larger group of one disorder. Medical geneticists are at a particular vantage point to lead natural history studies and inform the greater community of opportunities for further study within one disorder.
Medical geneticists are important stakeholders who can inform the translational aspects of the preclinical work. For example, medical geneticists have led the development of adeno-associated viral (AAV) vector-mediated gene therapy for inherited metabolic disorders currently managed using liver transplantation (for example, methylmalonic acidemia (MMA) due to MUT gene defect). However, AAV vectors have inherent limitations including transgene loss and genotoxicity. A recent study evaluated an AAV vector with a promoterless transgene that integrated into the albumin locus in a neonatal mouse model of MMA to achieve a stable benefit.9 Furthermore, this strategy avoided the known risk for the development of AAV-related hepatocellular carcinoma (HCC), because HCC has been linked to promoter insertion to drive oncogenes in newborn-treated mice. Whereas HCC formation has not been observed during recombinant AAV vector clinical trials, recent studies have demonstrated that wild-type (WT) AAV can be associated with HCC in humans.10,11 Advances such as this one are possible through knowledge of the pathogenesis, relevant clinical endpoints, technology, and unmet needs for each disease, all of which medical geneticists are positioned to understand. However, there is great demand for medical geneticists to be involved in patient care, and the expectations for productivity frequently take precedence to research activities. Involvement in clinical trials can provide an academic activity that can lead to much career satisfaction as a leader in a research program and as a mentor that educates new generations of clinical investigators.
There Is a Critical Need for Variant Interpretation With Regard to Eligibility
It is important to consider sensitivity, specificity, and accuracy when performing DNA diagnostic testing for a genetic condition in patients considered for enrollment in a genetic therapy trial. Treating an inappropriately enrolled patient with therapies that have unknown toxicities and prolonged effects must be avoided. Identifying patients who are truly affected is complicated by heterogeneity: genetic disorders are often heterogeneous in their presentation, and a clinical phenotype can be associated with defects in multiple different genes (genetic heterogeneity). In turn, the concepts of incomplete penetrance and variable phenotypic expression may raise questions about the clinical findings of a particular genetic variant among members of the same family. One example is transthyretin (TTR) cardiac amyloidosis where it is difficult to determine which p.Val142Ile carriers will progress to heart failure and at what age. This example of variability is especially relevant in light of a recent clinical trial using CRISPR-Cas9 in vivo gene-editing for targeted TTR knockout to reduce serum TTR protein levels with therapeutic benefits.12 Expertise regarding the natural history and genotype-phenotype relationship for genetic diseases is needed to appropriately recommend new therapies to individual patients.
The appropriate selection of genetic therapies depends upon a reliable genetic diagnosis. Making genetic diagnoses relies upon accurate interpretation of variants, which require an assessment of phenotypic fit, functional significance, and segregation based on the family history, and generate much confusion outside of clinical genetics.13 Without known disease mechanisms, or functional studies that support the damaging effect of a DNA variant, and without segregation analysis (from family-based study), it may be very challenging for DNA laboratory directors and geneticists to classify ultra-rare or novel variants found in known disease genes as pathogenic or likely pathogenic based on ACMG criteria.14 However, clinical laboratory geneticists are not only trained in the analysis and interpretation of DNA variants,14,15 but also work closely with clinical geneticists in communicating DNA test results and advising on genotype-phenotype variability. Considering inclusion of patients in clinical trials for Mendelian disorders should also take into account demographic differences, the prevalence of a condition in diverse populations (often it is known only for well-studied population(s)), and differences in the frequency of certain founder variants (for example the p.Val142Ile, c.424G>A variant in TTR) in individuals with different ancestry or ethnicity. Effective genetic testing also depends on the number of genes tested. Although large gene panels may be the best strategy to maximize diagnostic yield in genetically heterogeneous diseases (and there may be a desire to increase enrollment under some circumstances), they will often prioritize incorrectly classified variants potentially requiring additional clinical follow-up.13 A recent study suggests that selecting variants that are not known to be pathogenic or likely pathogenic (ie, variants with reduced specificity, variants of uncertain significance) results in an increase in the selection of incorrectly classified variants.16 When employing panels containing >500 monogenic disease genes, most individuals tested will have at least one rare nonsynonymous variant. Geneticists are experienced in the interpretation of candidate variants found in the absence of relevant phenotypes to avoid falsely diagnosing a patient, who then might seek to enroll in a clinical trial. As our understanding of genotype-phenotype correlations grows for a particular disorder, trial design may be refined to stratify populations based on the severity of the condition, described progression, or a specific phenotype in a subset of affected individuals, the expected effect size of the investigational agent, and other specific parameters.
Medical Geneticists Have a Unique Role in Patient Assessment and Recruitment
Medical geneticists can play a key role in clinical trial enrollment. It is often challenging to measure the treatment benefits of genetic therapies accurately,17 due to the complexities of genetic disease. Changes in the expression and levels of transgene proteins (eg, enzymes, blood clotting factors) following the administration of a gene therapy may not be predictive of clinical benefits. Medical geneticists have an understanding of pathogenicity, disease progression, and biomarkers, which can be important for quantifying the clinical effectiveness of a gene therapy, which better equips them to evaluate efficacy from a genetic therapy. This information provides the knowledge base needed to effectively design clinical trials for genetic therapies in partnership with basic science investigators, and benefits pre-clinical study planning and discussions with regulatory agencies regarding study design. Such a team is better equipped to address the translational, clinical, and ethical issues of clinical trial design, including determining an optimal dosage, delivering the product effectively, determining sample size needed, and monitoring safety (Figure 1).
Successful recruitment and retention are paramount to the clinical trials’ success,17 both of which rely upon open communication and partnership between prospective participants and clinicians. Such communication is critical, given the inherent uncertainty about potentially long-lasting effects and effectiveness, and unpredictability of the future use of other therapeutic options, including different gene therapies.17 Medical geneticists are uniquely equipped to advise their patients regarding clinical trial participation. This decision is influenced both by motivations and by barriers for participation in clinical trials. Patient-centered approaches to study design and execution are likely to yield more successful trials,18 and have been identified as a priority by the National Academies of Sciences, Engineering, and Medicine.19 This includes discussions with knowledgeable persons regarding potential risks and benefits of participation, and identification of priorities from the patient’s perspective. A survey study among patients with a primary mitochondrial disorder,20 recorded motivating trial design factors that included: a self-administered study drug; agent (vitamin, antioxidant, natural or plant-derivative); formulation (pills vs infusions); daily treatment; guaranteed treatment access during and after study; short travel distances; and late-stage (Phase 3) participation with greater likelihood of benefits. Relative trial participation barriers included a new study drug; discontinuation of current medications; disease progression; daily phlebotomy; and requiring participant payment. It has been shown that partnering of medical geneticists with rare disease patient communities can achieve the robust design of clinical trials that engage patients and enable meaningful evaluation of emerging treatment interventions.20 Another recent study surveyed the attitude of patients with progressive ataxias towards clinical trials and highlights the importance of input from the patient community to the overall success of the program.21 The authors concluded that knowledge of motivations for and barriers to trial participation as well as the acceptability of investigations, time commitments and routes of drug administration should inform better, more patient focused trial design. This in turn may improve recruitment and retention of participants to future trials. Participation requires an informed decision that can be facilitated by discussions with a medical geneticist who understands the causative variant(s) and the approach/mechanism that the trial is aiming to treat/cure.
Our Understanding Regarding the Safety of Genetic Therapies Continues
Medical geneticists are involved with the diagnosis and management of patients with genetic diseases, and therefore have an interest in the development of genetic therapies. Drug development has a critical focus on determining both efficacy and safety of an investigational product, and genetic therapies are currently in clinical trials from early to later phases of development. Due to their novelty, the knowledge of the long term effects of these interventions is limited. The risks and benefits of genetic therapies can be clearly communicated by medical geneticists, because geneticists are integrally involved in the development and prescribing processes for these therapies. Therefore, sponsors should engage with the medical genetics community to disseminate new safety data. Furthermore, the reporting and long term follow-up (LTFU) of therapy-related adverse events, adverse events of special interest, or serious adverse events (SAEs), experienced during a clinical trial or in the post-approval period, is a primary concern for medical geneticists with regard to patients’ safety. Once a new therapy is approved, ongoing surveillance is of paramount importance, as new safety signals may become apparent during LTFU, once a greater number of affected individuals receive the treatment. While post-marketing surveillance is required by the regulatory agencies, it is less intensive in comparison with monitoring during Phase 1 to 3 clinical trials. Although genetic therapies may optimistically be regarded as curative, ongoing LTFU is critical to the understanding of post-treatment phenotypes, complications, and side effects.
Long lasting or permanent human gene delivery, editing, and modification reagents may introduce an increased risk of unexpected adverse events, including SAEs. The FDA has recognized the need for LTFU studies on permanent or long-acting human gene therapy products to mitigate this risk.22 Knowledge of disease progression from the medical genetics community is essential to address these new challenges. Long-term safety, as well as benefits, must be considered when prescribing these new therapies. This information is unique to the agent; for example, the most common SAEs observed in clinical trials of nusinersen were related to lumbar puncture and not the drug itself; however, the drug administration is part of the treatment and must be considered when prescribing a therapy. Patient’s concerns about SAEs influence clinical trials enrollment, and treatment decisions following marketing approval.23,24 One survey of participants in clinical trials of gene therapy for hemophilia revealed that participation was generally a positive experience, although participants were unprepared for adverse events related to immunosuppression and some felt a loss of control during their participation.25 Given these risks, medical geneticists and the medical community must advocate for transparency in the reporting of adverse events, especially SAEs, related to genetic therapies.
Recent events have emphasized the need for rapid dissemination of SAEs related to gene therapy for neuromuscular disorders.26 Despite promising preclinical data that supported safety, SAEs have emerged recently that raise the importance of timely and comprehensive communication to the provider community. This includes communication with sites that are administering the same investigational agent across different clinical trials that are enrolling simultaneously, and administration of the therapy in the post-marketing approval period. In the early phase clinical trials, which are focused on safety, SAEs may lead to FDA placing a clinical hold on the trial to allow investigation on the cause, such as in the ASPIRO clinical trial in X-linked myotubular myopathy.27 Similarly, unexpected adverse events have occurred in clinical trials of AAV vectors in Duchenne muscular dystrophy (DMD), ranging from immune responses associated with toxicity26 to a patient death.28 Although the latter event led to a clinical hold on the study involved, similar studies remain open. Ongoing surveillance is paramount after approval, with onasemnogene abeparvovec-xioi (Zolgensma) as one example of a post-marketing change in the product label to reflect the risk of acute liver failure.29 Until the chain of events that led to death is clarified, it is unclear whether the event represents a potential risk for similar gene therapy agents.
One concept for promoting transparency around SAEs is the involvement of patient advocacy groups in publicizing these events. Sharing of accurate information related to new developments will allow patients to enroll with enhanced knowledge of risks and will support informed consent. An example of such advocacy is the Parent Project for Muscular Dystrophy, a nonprofit focused on DMD, and the study sponsor involved that group directly about the patient death from gene therapy.28 The Parent Project was founded by the parent of a boy with muscular dystrophy, and has advocated for and supported the development of gene therapy for muscular dystrophy, engaging with sponsors including industry and the National Institutes of Health to promote research. Other patient organizations have played similar roles, but many rare diseases lack this active dialogue with the patient community to facilitate communication with sponsors and regulators.
Conclusion
Given the expansion of genetic therapies that looms in the coming years, the input of medical geneticists in the development and implementation of these products for the rare, genetic disease population is warranted. Expertise in medical genetics can provide added value with regards to clinical trial design, execution, recruitment, and medical geneticists will be needed to appropriately prescribe new genetic therapies, once available. Recognition of disease related factors is needed to accurately interpret potential benefits. As the specialists seeing many of the rare disease patients, medical geneticists will be responsible for monitoring safety of genetic therapies. Given the unknown risks of these therapies, special consideration to the transparency of reporting drug related toxicities is needed. The success of this burgeoning field will depend upon engagement with medical geneticists to address the unmet need for new therapies for genetic diseases, and highlights the need for protected time and education to foster continued involvement of the medical genetics community.
Acknowledgements
We wish to thank the following individuals for assistance with drafting and editing this manuscript: Sandor Roberts and Jennifer Malinowski.
Footnotes
Conflict of Interest
Funding and support listed here did not support development of this document unless included in the acknowledgements section. L.D.M.P. has received compensation for sponsored travel (Sanofi US), advisory board participation (ModernaTx, Sanofi US, Ultragenyx, AveXis, Inc., Orphazyme, BioMarin), and research support (ModernaTx, CycloTherapeutics, Inc., Takeda, Mallinkrodt, Orphazyme) in the past four years. G.M.E. has served as a consultant to AllStripes, Codexis, Glycomine, Hemoshear, Homology Medicines, Horizon Therapeutics, M6P Therapeutics, Moderna Therapeutics, Travere Therapeutics, and Ultragenyx and is the co-founder of Evvia Therapeutics; and serves on the Data Monitoring Committees for clinical trials for Abliva, Amicus Therapeutics, Audentes Therapeutics, BioMarin, Modis Therapeutics, Paradigm Biopharma, Passage Bio, and RegenxBio. E.D.E. is a salaried employee and stockholder of Invitae Corporation and a scientific advisory board member and stockholder at Taproot Health. T.Y. has served as a consultant for BioMarin Pharmaceutical. D.D.K. has served as a consultant for Sangamo Therapeutics, Genzyme Sanofi, Amicus Therapeutics, Takeda, and Vertex; has received grant support from Viking Therapeutics, Genzyme Sanofi, Roivant Rare Diseases, and Amicus; and has equity in Askbio, which is developing gene therapy for Pompe disease. The other authors declare no competing interests.
The Board of Directors of the American College of Medical Genetics and Genomics approved this statement on 23 January 2023.
Disclaimer
This statement is designed primarily as an educational resource for medical geneticists and other clinicians to help them provide quality medical services. Adherence to this statement is completely voluntary and does not necessarily assure a successful medical outcome. This statement should not be considered inclusive of all proper procedures and tests or exclusive of other procedures and tests that are reasonably directed to obtaining the same results. In determining the propriety of any specific procedure or test, clinicians should apply their own professional judgment to the specific clinical circumstances presented by the individual patient or specimen.
Clinicians are encouraged to document the reasons for the use of a particular procedure or test, whether or not it is in conformance with this statement. Clinicians also are advised to take notice of the date this statement was adopted, and to consider other medical and scientific information that becomes available after that date. It also would be prudent to consider whether intellectual property interests may restrict the performance of certain tests and other procedures. Where individual authors are listed, the views expressed may not reflect those of authors’ employers or affiliated institutions.
References
- 1.Nguengang Wakap S, Lambert DM, Olry A, et al. Estimating cumulative point prevalence of rare diseases: analysis of the Orphanet database. Eur J Hum Genet. 2020;28(2):165–173. 10.1038/s41431-019-0508-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tambuyzer E, Vandendriessche B, Austin CP, et al. Therapies for rare diseases: therapeutic modalities, progress and challenges ahead. Nat Rev Drug Discov. 2020;19(2):93–111. 10.1038/s41573-019-0049-9 [DOI] [PubMed] [Google Scholar]
- 3.Watson MS, Lloyd-Puryear MA, Howell RR. The progress and future of US newborn screening. Int J Neonatal Screen. 2022;8(3):41. 10.3390/ijns8030041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.FDA approves first haemophilia B gene therapy. Accessed January 3, 2023, from https://www.nature.com/articles/d41573-022-00199-8. [DOI] [PubMed]
- 5.Owusu Obeng A, Fei K, Levy KD, et al. Physician-reported benefits and barriers to clinical implementation of genomic medicine: A multi-site IGNITE-Network survey. J Pers Med. 2018;8(3):24. 10.3390/jpm8030024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schaibley VM, Ramos IN, Woosley RL, Curry S, Hays S, Ramos KS. Limited genomics training among physicians remains a barrier to genomics-based implementation of precision medicine. Front Med (Lausanne). 2022;9:757212. 10.3389/fmed.2022.757212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rare diseases clinical research network. Accessed September 20, 2022, from https://www.rarediseasesnetwork.org/index.php/.
- 8.Pastores GM, Gupta P. Orphan drug development. Pediatr Endocrinol Rev. 2013;11 Suppl 1:64–67. [PubMed] [Google Scholar]
- 9.Chandler RJ, Venturoni LE, Liao J, et al. Promoterless, nuclease-free genome editing confers a growth advantage for corrected hepatocytes in mice with methylmalonic acidemia. Hepatology. 2021;73(6):2223–2237. 10.1002/hep.31570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nault JC, Datta S, Imbeaud S, et al. Recurrent AAV2-related insertional mutagenesis in human hepatocellular carcinomas. Nat Genet. 2015;47(10):1187–1193. 10.1038/ng.3389 [DOI] [PubMed] [Google Scholar]
- 11.La Bella T, Imbeaud S, Peneau C, et al. Adeno-associated virus in the liver: natural history and consequences in tumour development. Gut. 2020;69(4):737–747. 10.1136/gutjnl-2019-318281 [DOI] [PubMed] [Google Scholar]
- 12.Gillmore JD, Gane E, Taubel J, et al. CRISPR-Cas9 in vivo gene editing for transthyretin amyloidosis. N Engl J Med. 2021;385(6):493–502. 10.1056/NEJMoa2107454 [DOI] [PubMed] [Google Scholar]
- 13.Newey PJ. Approach to the patient with a variant of uncertain significance on genetic testing. Clin Endocrinol (Oxf). 2022;97(4):400–408. 10.1111/cen.14818 [DOI] [PubMed] [Google Scholar]
- 14.Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405–424. 10.1038/gim.2015.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller DT, Lee K, Abul-Husn NS, et al. ACMG SF v3.1 list for reporting of secondary findings in clinical exome and genome sequencing: A policy statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2022;24(7):1407–1414. 10.1016/j.gim.2022.04.006 [DOI] [PubMed] [Google Scholar]
- 16.Beaumont RN, Wright CF. Estimating diagnostic noise in panel-based genomic analysis. Genet Med. 2022;24(10):2042–2059. 10.1016/j.gim.2022.06.008 [DOI] [PubMed] [Google Scholar]
- 17.Beachy SH, Alper J, Hackmann M, Addie S. Exploring Novel Clinical Trial Designs for Gene-Based Therapies: Proceedings of a Workshop. National Academies Press, 2020. [PubMed] [Google Scholar]
- 18.Mullins CD, Abdulhalim AM, Lavallee DC. Continuous patient engagement in comparative effectiveness research. JAMA. 2012;307(15):1587–1588. 10.1001/jama.2012.442 [DOI] [PubMed] [Google Scholar]
- 19.Shore C, Gee AW, Wizemann T. Envisioning a Transformed Clinical Trials Enterprise for 2030: Proceedings of a Workshop. National Academies Press, 2021. [PubMed] [Google Scholar]
- 20.Zolkipli-Cunningham Z, Xiao R, Stoddart A, et al. Mitochondrial disease patient motivations and barriers to participate in clinical trials. PLoS One. 2018;13(5):e0197513. 10.1371/journal.pone.0197513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomas-Black G, Dumitrascu A, Garcia-Moreno H, et al. The attitude of patients with progressive ataxias towards clinical trials. Orphanet J Rare Dis. 2022;17(1):1. 10.1186/s13023-021-02091-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ledley FD, Brody B, Kozinetz CA, Mize SG. The challenge of follow-up for clinical trials of somatic gene therapy. Hum Gene Ther. 1992;3(6):657–663. 10.1089/hum.1992.3.6-657 [DOI] [PubMed] [Google Scholar]
- 23.Moshe-Lilie O, Visser A, Chahin N, Ragole T, Dimitrova D, Karam C. Nusinersen in adult patients with spinal muscular atrophy: Observations from a single center. Neurology. 2020;95(4):e413–e416. 10.1212/WNL.0000000000009914 [DOI] [PubMed] [Google Scholar]
- 24.Elsheikh B, Severyn S, Zhao S, et al. Safety, tolerability, and effect of nusinersen treatment in ambulatory adults with 5q-SMA. Front Neurol. 2021;12:650535. 10.3389/fneur.2021.650535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fletcher S, Jenner K, Pembroke L, Holland M, Khair K. The experiences of people with haemophilia and their families of gene therapy in a clinical trial setting: regaining control, the Exigency study. Orphanet J Rare Dis. 2022;17(1):155. 10.1186/s13023-022-02256-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buscara L, Gross DA, Daniele N. Of rAAV and men: From genetic neuromuscular disorder efficacy and toxicity preclinical studies to clinical trials and back. J Pers Med. 2020;10(4):258. 10.3390/jpm10040258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Privolizzi R, Chu WS, Tijani M, Ng J. Viral gene therapy for paediatric neurological diseases: progress to clinical reality. Dev Med Child Neurol. 2021;63(9):1019–1029. 10.1111/dmcn.14885 [DOI] [PubMed] [Google Scholar]
- 28.Philippidis A. After patient death, FDA places hold on Pfizer Duchenne Muscular Dystrophy gene therapy trial. Hum Gene Ther. 2022;33(3–4):111–115. 10.1089/hum.2022.29198.bfs [DOI] [PubMed] [Google Scholar]
- 29.U.S. Food and Drug Administration. Zolgensma Package Insert. Accessed September 13, 2022, from https://www.fda.gov/media/126109/download.