Abstract
Objective:
To quantify the frequency of use of selected fertility awareness indicators and to assess the influence on fecundability.
Design:
Web-based prospective cohort study.
Setting:
United States and Canada.
Participants:
Female pregnancy planners aged 21–45 years, attempting conception for ≤6 cycles at study entry.
Intervention(s):
None
Main Outcome Measure(s):
We ascertained time to pregnancy, in menstrual cycles, by bimonthly questionnaires. We estimated adjusted fecundability ratios (aFRs) and 95% confidence intervals (CIs) using proportional probabilities models, controlling for age, income, education, smoking, intercourse frequency, and other lifestyle and reproductive factors.
Results:
A total of 5,688 women were analyzed, with a mean age of 29.9 years and mean time trying of 2.1 cycles at baseline; 30% had ever been pregnant. At baseline, 75% were using one or more fertility indicators; specifically, counting days or charting menstrual cycles (71%), measuring basal body temperature (21%), monitoring cervical fluid (39%), using urine LH tests (32%), or feeling for changes in position of the cervix (12%). Women using any fertility indicator at baseline had higher subsequent fecundability (aFR 1.25, CI 1.16–1.35) than those not using any fertility indicators; for each individual indicator, aFRs ranged from 1.28 to 1.36, where 1.00 would indicate no relation with fecundability. The aFR for women using a combination of charting days, cervical fluid, and urine LH was 1.48 (CI 1.31–1.67) relative to women using no fertility indicators.
Conclusions:
In a North American preconception cohort study, use of fertility indicators indicating the fertile window was common, and was associated with greater fecundability.
Keywords: fertility awareness, fertility, time-to-pregnancy, preconception, cohort studies
Capsule:
We prospectively evaluated the association between fertility awareness indicators and fecundability among pregnancy planners. Use of fertility indicators to track the fertile window was associated with greater fecundability.
Introduction
Many couples desiring to conceive seek information to enhance their probability of conceiving, including information for optimal timing of intercourse (1). The most fecund days of the menstrual cycle (in terms of the probability of intercourse resulting in clinically-identified pregnancy) are the 2–3 days preceding the day of ovulation, while the full “fertile window” may be 6 or more days of the cycle (2–4). Among women with normal-length menstrual cycles, the fertile window in any particular cycle may start as early as day 6 or end as late as day 21 (5). Several biomarkers or self-observed indicators can be used to identify the fertile window (1, 6, 7).
Fertility indicators with a strong physiologic rationale for prospectively identifying the most fecund days of the menstrual cycle or the “fertile window” include changes in vaginal discharge from cervical fluid, self-palpation of the uterine cervix, home urine testing for increases in estrogen metabolites, and home urine testing for the surge in luteinizing hormone (LH), often called “ovulation predictor kits” (1, 6, 8). The fertile window can also be estimated by counting days since the start of the cycle, while determining which days are considered fertile based on previous cycle lengths (9, 10), possibly with the aid of adaptive computer algorithms (11). Another way that the fertile window can be estimated is based on the day of basal body temperature rise in previous cycles (12). Books, health organizations, instructors, and other educational resources have long existed to teach women how to monitor these indicators in different combinations either to avoid pregnancy or to conceive (13–15). Nonetheless, there is scant evidence comparing the different fertility indicators to ascertain which may be most effective for helping couples shorten time to pregnancy (16).
In the present report, we estimated the prevalence of fertility indicator use in an ongoing North American prospective cohort study of couples trying to conceive. We also assessed fecundability (the per-cycle probability of conception) for each of the aforementioned self-observed indicators of the fertile window.
Material and Methods
The Pregnancy Study Online (PRESTO) is a prospective web-based cohort study of preconception North American pregnancy planners. Study methods have been described in detail previously (17). Briefly, women aged 21–45 years living in the United States or Canada, in a stable relationship with a male partner, and not using contraception or fertility treatment at baseline, are eligible to participate. Female participants complete an online baseline questionnaire with items on demographic, behavioral, reproductive and medical history, and medication use. Females complete follow-up questionnaires to update exposure status, behavioral factors, and lifestyle factors that may have changed and ascertain pregnancy status every 8 weeks or until reported conception, initiation of fertility treatment, cessation of pregnancy attempt, withdrawal, loss to follow-up, or 12 months, whichever came first. Online informed consent was obtained from all participants and this study was approved by the Institutional Review Board at Boston Medical Center.
From June 2013 until May 2018, 7,259 eligible women completed the baseline questionnaire. Of those women, 100 were excluded because the start date of the last menstrual period (LMP) at baseline was >6 months before participants’ study entry, and 35 because they had insufficient or missing LMP data or were already pregnant at study entry. An additional 1,436 women were excluded because they had been attempting pregnancy for >6 cycles at baseline, yielding a final analytic sample of 5,688 women.
Use of Fertility Indicators
On the baseline and follow-up questionnaires, women were asked, “Are you or your partner doing anything to improve your chances of becoming pregnant?” If participants answered affirmatively, they were asked “Which methods are you using?” with the following response options: “check basal body temperature”, “monitor cervical fluid”, “urine LH ovulation testing kit or sticks”, “electronic fertility monitor” (with sub-options of “ClearBlue”, “OvaCue”, “Ovwatch”, “other”), “chart menstrual cycles”, “count for days since last menstrual period”, “feel for changes in position of cervix”, and “other,” with instruction to check all answers that applied. For analysis, “chart menstrual cycles” was combined with “count for days since last menstrual period” and called “charting days.” “Urine LH ovulation testing kit or sticks” was combined with “ClearBlue” (18). All “other” text responses were coded by a content expert (JBS) into the appropriate method, as applicable.
Outcome: Time to Pregnancy
Time to pregnancy (TTP) was estimated using data from the female baseline and follow-up questionnaires. On the baseline questionnaire, women reported their LMP, usual menstrual cycle length, and the number of cycles attempting pregnancy at study entry. On subsequent follow-up questionnaires, women reported their most recent LMP and whether they have conceived since the previous questionnaire. If women reported having irregular cycles, usual cycle length was estimated based on the baseline LMP data and consecutive LMP dates on follow-up questionnaires. TTP was estimated based on the total discrete cycles at risk of pregnancy, calculated as follows: cycles of attempt at study entry + [(LMP date from most recent follow-up questionnaire - date of baseline questionnaire completion)/usual cycle length] +1(19).
Covariates
Covariate information collected at baseline included age, height, weight, relationship duration, marital status, race/ethnicity, income, education, hours of sleep per night, parity, gravidity, multivitamin use, contraception history, intercourse frequency, menstrual regularity (defined through asking “within the past couple of years, has your menstrual period been regular (regular in a way so you can usually predict about when the next period will start)? Please think about those times you were not using hormonal contraceptives.”), history of infertility (defined as having tried to conceive for more than 12 months without success for any prior pregnancy attempt), smoking status, and alcohol use. Body mass index (BMI) was calculated as weight (kilograms) divided by height (meters) squared.
Analysis
We used proportional probabilities regression models to estimate fecundability ratios (FRs) and 95% confidence intervals (CI) for the association between each fertility indicator and fecundability. Couples contributed menstrual cycles until pregnancy, initiation of fertility treatment, cessation of pregnancy attempts, withdrawal, loss to follow-up, or completion of 12 cycles, whichever came first. We performed analyses based on: 1) fertility indicators reported at baseline only and 2) fertility indicators reported on each follow-up questionnaire (“time-varying”). In the time-varying analyses, we replaced the former values of exposure with the updated information in each bi-monthly period, ignoring previous values of that variable.
In addition, analyses were done for each possible combination of fertility indicators. The FR is the average per-cycle probability conception within each exposure category in comparison to the reference group. FRs of <1 indicate a longer TTP among exposed compared with unexposed participants. The model incorporates each observed cycle at risk, which accounts for the baseline decline in fecundability over time (20). The Anderson-Gill data structure outputs a single menstrual cycle per observation to accommodate time-varying variables and to account for left truncation from delayed entry into the cohort (21). Prevalence was calculated for the use of each fertility indicator at baseline and each of the follow-up questionnaires.
Potential confounders were assessed a priori based on a literature review and the consideration of directed acyclic graphs. Final models were adjusted for female age (<25, 25–29, 30–34, ≥35 years), race/ethnicity (White, non-Hispanic vs other race/ethnicity), prior pregnancy (yes vs no), BMI (<25, 25–29.9, 30–34.9, ≥35 kg/m2), income (<$50,000, $50–99,999, $100–149,999, $≥150,000 US dollars/year), current smoker (yes vs no), education (<college degree vs ≥college degree), partner education (<college degree vs ≥college degree), use of hormonal contraceptives as last method of contraception (yes vs no), hours of sleep per night (≤6 vs ≥7 hours), cycle regularity (regular vs irregular), use of prenatal supplements (yes vs no), marital status (married vs unmarried), intercourse frequency (<2 vs ≥2 times per week), history of benign gynecologic disorders including polycystic ovary syndrome (PCOS), endometriosis, or uterine leiomyomata (yes vs no), history of sexually transmitted infections including pelvic inflammatory disease (PID), chlamydia, herpes, or warts (yes vs no), history of infertility (yes, no, never attempted to conceive); and mother had difficulties getting pregnant (yes vs no). Caffeine was assessed as a potential confounder but was omitted from final models because it had no appreciable effect on the association (22). We conducted supplementary exploratory analyses stratified by cycle regularity, time trying at study entry, and history of subfertility (trying for 6 months or more to conceive in the past, before the current pregnancy attempt). In addition, we conducted sensitivity analyses restricted to those who had tried for <=1 cycle at entry and also restricted to two cycles of follow-up, to assess possible attenuation bias (23), as well as an analysis restricted to women without recent hormonal contraceptive use that can temporarily reduce fecundability (24).
Missing data
We imputed missing values for exposures, covariates, and pregnancy status using multiple imputation. We created five imputed datasets using a Markov chain Monte Carlo method, analyzing each dataset separately, and combining coefficient and standard error estimates across the imputed datasets. To reduce selection bias from differential loss to follow-up, we assigned one cycle of follow-up for the 10% of women with no follow-up data (N=564) and then imputed their pregnancy status (yes vs. no) by multiple imputation. Fewer than 0.2% of participants were missing data for using a method to improve chances of pregnancy. Missingness for covariates ranged from <0.1% (prior pregnancy, history of infertility, caffeine use, and history of anxiety) to 3.4% for income. There were no missing values for age.
Results
Overall, 5,688 female participants contributed 3,333 pregnancies and 22,612 menstrual cycles of attempt time. Table 1 shows demographic, reproductive, and behavioral characteristics of the participants at baseline, stratified by reported use of no fertility indicator (1,443 women; 25%) or any fertility indicator (4,245 women, 75%). Overall, the mean age of female participants was 29.9 years, with a mean time trying of 2.1 cycles at study entry; 30% had ever been pregnant. Use of the specific self-observed fertility indicators was reported as follows on the baseline questionnaire: basal body temperature 1,199 (21%), monitoring cervical fluid 2,239 (39%), self-palpation of cervix position 666 (12%), urine LH 1,837 (32%), charting or counting days 4,019 (71%); (Supplemental Table 1 reports the characteristics for each of these overlapping groups). The majority of women were married (91%), college-educated (74%) and had a household income >$50,000 per year (79%). Less than 20% reported a history of infertility. About two-thirds reported taking folic acid or multivitamin supplements.
Table 1.
Baseline characteristics* of 5,688 PRESTO participants by use of any fertility indicator
| All participants | No fertility indicator use | Any fertility indicator use | |
|---|---|---|---|
|
| |||
| 5,688 | 1,443 | 4,245 | |
| Age, years (mean) | 29.9 | 29.7 | 30.0 |
| Partner’s age, years (mean) | 31.9 | 31.9 | 31.9 |
| Body mass index (BMI), kg/m2 (mean) | 27.7 | 28.3 | 27.5 |
| Partner’s BMI, kg/m2 (mean) | 28.1 | 28.3 | 28.0 |
| Relationship duration, years (mean) | 5.4 | 5.2 | 5.5 |
| Attempt time at study entry, cycles (mean) | 2.1 | 1.6 | 2.3 |
| Married (%) | 91.4 | 89.0 | 92.3 |
| Non-Hispanic, White (%) | 83.5 | 79.6 | 84.7 |
| Income <$50,000 per year (%) | 20.6 | 24.3 | 19.4 |
| Education≥ college (%) | 73.5 | 72.7 | 73.7 |
| Partner education≥ college (%) | 56.4 | 52.4 | 57.7 |
| Sleep <7 hours (%) | 24.4 | 28.2 | 23.2 |
| Gravid (%) | 29.6 | 31.7 | 29.0 |
| Parous (%) | 48.7 | 46.1 | 49.5 |
| Took folic acid/multivitamin (%) | 75.1 | 62.6 | 79.3 |
| Most recent form of birth control was hormonal method (%) | 39.6 | 43.1 | 38.4 |
| Intercourse ≥2 times per week (%) | 61.4 | 56.2 | 63.2 |
| History of infertility (%)** | 13.4 | 15.0 | 13.0 |
| Irregular periods (%) | 17.1 | 22.2 | 15.5 |
| Current smoker (%) | 6.9 | 8.8 | 6.2 |
| Alcohol, drinks/week (mean) | 3.3 | 3.4 | 3.3 |
| Caffeine, mg/day (mean) | 124.0 | 126.6 | 122.9 |
| Benign Gynecologic Disorders (%) | |||
| Polycystic ovary syndrome | 7.9 | 9.4 | 7.4 |
| Endometriosis | 2.7 | 2.5 | 2.8 |
| Uterine leiomyomata | 2.3 | 2.2 | 2.3 |
| History of sexually transmitted infection (%) | |||
| Pelvic Inflammatory Disease | 1.1 | 1.4 | 1.0 |
| Chlamydia | 7.6 | 7.7 | 7.6 |
| Herpes | 4.1 | 4.5 | 3.9 |
| Genital warts | 3.3 | 4.0 | 3.0 |
| Participant’s mother had problems conceiving (%) | 20.2 | 18.9 | 20.7 |
All characteristics except age are standardized to age distribution of cohort at baseline
among those who had previously attempted pregnancy
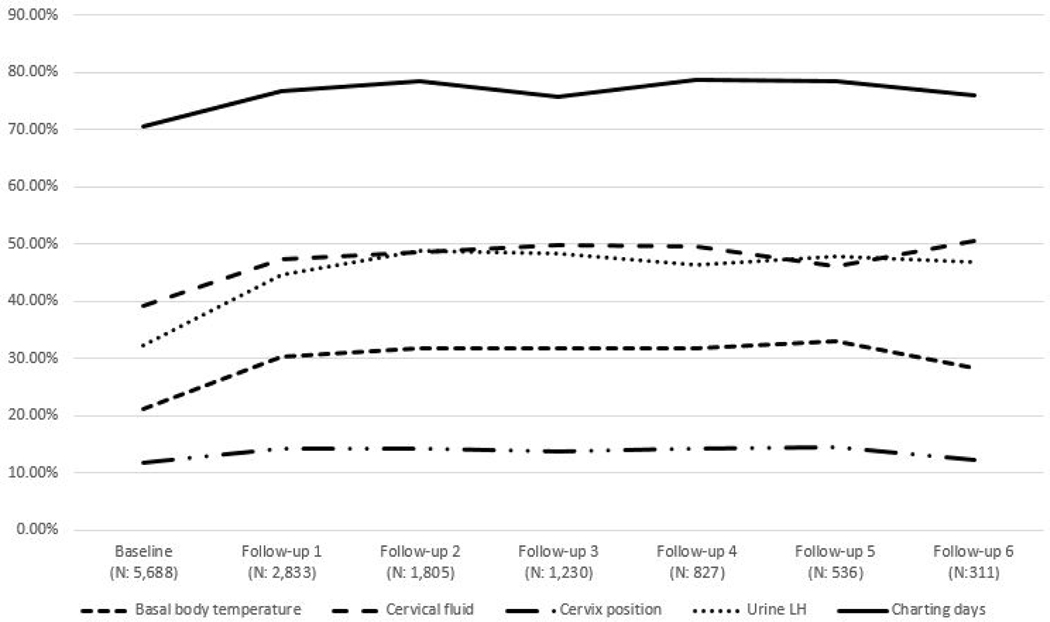
The prevalence for each indicator rose slightly after baseline among those women who were still trying to conceive and remained nearly flat through most of the remaining follow-up (Figure 1). At baseline, 25% of women used no indicators, 23% used only one indicator, 22% used two indicators, and 30% used three or more indicators.
Figure 1.
Prevalence of reported use of individual fertility indicators at baseline and bimonthly follow-up questionnaires.
Table 2 reports FRs for use of each specific fertility indicator, both unadjusted and adjusted for the multiple demographic, health, and lifestyle covariates described previously. Analyses using baseline and time-varying exposure classifications are included. Use of each of the fertility indicators was associated with higher fecundability, compared with non-use, with similar results observed for baseline and time-varying exposure classifications. The associations were attenuated slightly but remained positive after covariate adjustment. The adjusted effect estimates were similar across the various indicators, ranging from 1.28 to 1.36.
Table 2.
Association between fertility indicator use and fecundability
| Baseline assessment of fertility indicator use | Time varying assessment of fertility indicator use | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| No. of pregnancies | No. of cycles | Unadjusted | Adjusteda | No. of pregnancies | No. of cycles | Unadjusted | Adjusteda | |||||
|
| ||||||||||||
| FR | 95% CI | FR | 95% CI | FR | 95% CI | FR | 95% CI | |||||
| No fertility indicator use | 782 | 6,305 | 1.00 | Ref | 1.00 | Ref | 669 | 5,464 | 1.00 | Ref | 1.00 | Ref |
| Any fertility indicator use * | 2,551 | 16,307 | 1.34 | 1.24–1.45 | 1.25 | 1.16–1.35 | 2,664 | 17,148 | 1.41 | 1.30–1.53 | 1.31 | 1.21–1.42 |
| BBT | 737 | 4,640 | 1.34 | 1.22–1.47 | 1.22 | 1.11–1.35 | 833 | 5,466 | 1.41 | 1.28–1.55 | 1.28 | 1.16–1.42 |
| Cervical fluid | 1,391 | 8,543 | 1.40 | 1.28–1.52 | 1.29 | 1.18–1.40 | 1,506 | 9,467 | 1.47 | 1.35–1.60 | 1.35 | 1.23–1.47 |
| Cervix position | 429 | 2,386 | 1.49 | 1.33–1.67 | 1.32 | 1.17–1.49 | 458 | 2,690 | 1.53 | 1.36–1.71 | 1.36 | 1.21–1.53 |
| Urine LH | 1,062 | 6,961 | 1.33 | 1.21–1.45 | 1.21 | 1.11–1.33 | 1,244 | 8,155 | 1.44 | 1.31–1.58 | 1.31 | 1.20–1.44 |
| Charting cycles or counting days | 2,444 | 15,372 | 1.37 | 1.27–1.48 | 1.27 | 1.17–1.37 | 2,561 | 16,161 | 1.44 | 1.33–1.56 | 1.33 | 1.23–1.45 |
= Adjusted for female age, race/ethnicity, gravidity, BMI, income, current smoker, education, partner education, most recent method of birth control hormonal, hours of sleep per night, irregular cycles, history of infertility, prenatal supplement intake, marital status, intercourse frequency, history of benign gynecologic disorder, history of sexually transmitted infection, maternal problems getting pregnant
Fertility indicators are not mutually exclusive. Women could contribute cycles to one or more methods.
Abbreviations: BBT: Basal body temperature; Urine LH: Urine LH ovulation testing kit or stick
Table 3 indicates the number of pregnancies and cycles contributed by women in each combination of indicators used, and the associated FRs based on time-varying exposure; analyses for baseline exposure were also done for this table and were similar. Charting days used without other methods was the most common indicator (3,984 cycles, aFR 1.35, CI 1.23–1.49). Other indicators were rarely used alone. The most common combinations of indicators were charting days in combination with cervical fluid (2,934 cycles); charting days, urine LH (ovulation predictor kits), cervical fluid, and basal body temperature (2,752 cycles); charting days, urine LH (ovulation predictor kits), and cervical fluid (2,153 cycles), and charting days and urine LH (1,939 cycles). The strongest aFRs were observed for the combination of charting days, urine LH (ovulation predictor kits), and cervical fluid (aFR 1.48, CI 1.36–1.47), and charting days, urine LH, cervical fluid, and basal body temperature (aFR 1.42, CI 1.27–1.59).
Table 3.
Association between use of combinations of fertility indicators (time varying) and fecundability
| Time varying fertility indicator use | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| No. of pregnancies | No. of cycles | Unadjusted | Adjusteda | |||
|
| ||||||
| FR | 95% CI | FR | 95% CI | |||
| No fertility indicator use | 669 | 5,464 | 1.00 | Ref | 1.00 | Ref |
| Any fertility indicator use | 2,664 | 17,148 | 1.41 | 1.30–1.53 | 1.31 | 1.21–1.42 |
| BBT only | 7 | 44 | 1.37 | 0.70–2.67 | 1.39 | 0.71–2.70 |
| Urine LH only | 38 | 421 | 0.84 | 0.61–1.14 | 0.81 | 0.59–1.10 |
| Cervical fluid only | 10 | 147 | 0.63 | 0.33–1.21 | 0.61 | 0.32–1.16 |
| Charting days only | 675 | 3,984 | 1.44 | 1.30–1.59 | 1.35 | 1.23–1.49 |
| Charting days and BBT | 48 | 355 | 1.19 | 0.90–1.56 | 1.17 | 0.89–1.53 |
| Charting days and urine LH | 272 | 1,939 | 1.34 | 1.18–1.53 | 1.24 | 1.08–1.41 |
| Charting days and cervical fluid | 455 | 2,934 | 1.38 | 1.23–1.54 | 1.29 | 1.16–1.45 |
| Charting days, BBT, cervical fluid | 218 | 1,439 | 1.35 | 1.18–1.56 | 1.25 | 1.09–1.44 |
| Charting days, cervical fluid, urine LH | 363 | 2,153 | 1.61 | 1.42–1.82 | 1.48 | 1.31–1.67 |
| Charting days, BBT, urine LH | 77 | 605 | 1.25 | 0.99–1.57 | 1.12 | 0.89–1.41 |
| Charting days, BBT, cervical fluid, urine LH | 453 | 2,752 | 1.58 | 1.41–1.77 | 1.42 | 1.27–1.59 |
| Other methods | 48 | 375 | 1.09 | 0.81–1.47 | 1.07 | 0.80–1.43 |
= Adjusted for female age, race/ethnicity, gravidity, BMI, income, current smoker, education, partner education, most recent method of birth control hormonal, hours of sleep per night, irregular cycles, history of infertility, prenatal supplement intake, marital status, intercourse frequency, history of benign gynecologic disorder, history of sexually transmitted infection, maternal problems getting pregnant
Abbreviations: BBT: Basal body temperature; Urine LH: Urine LH ovulation testing kit or stick
There was no consistent difference in aFRs when stratifying by menstrual cycle regularity at baseline (Supplemental Table 2). There was a slightly stronger association between fertility indicator use and fecundability among women with a history of subfertility (aFR ranged from 1.30 to 1.54), than in women without a history of subfertility (aFR ranged from 1.29 to 1.35). Among women who had been trying to conceive for <3 cycles at study entry, there was a stronger association between fertility indicator use and fecundability among women (aFR ranged from 1.31 to 1.43) than among women who had been trying to conceive for 3–6 cycles at study entry (aFR for ranged from 1.07 to 1.10; Supplemental Table 4). Similar aFR were found when we restricted to women who had tried for <=1 cycle at study entry, with the analysis including only the first two cycles of follow-up (Supplemental Table 5). Finally, when we restricted the analysis to women whose last form of contraception was not hormonal contraception, the aFR were slightly stronger (Supplemental Table 6).
Discussion
In this large prospective cohort study of pregnancy planners, we found a consistently positive association between fecundability (shorter TTP) and use of fertility indicators, including basal body temperature, cervical fluid (mucus), cervix position, urine LH test (ovulation predictor kits), and charting cycles or counting days. The most commonly used indicator was charting days; it had consistently positive associations with fecundability. Most women used multiple fertility indicators. The combination of fertility indicators associated with the highest fecundability were charting days, urine LH and cervical fluid, with or without basal body temperature.
Although these associations could reflect a causal effect of using the fertility indicators to time intercourse during the fertile window, we do not have information about the actual timing of intercourse, since the questionnaire simply asked about average intercourse frequency per month. We cannot rule out the possibility that some or possibly all of the associations stem from residual confounding, whereby fertility charting is a marker for engagement, interest, or behavior that has not been fully controlled by measured covariates. We can state that these results add to a body of evidence that shows a positive association between fertility indicator use and fecundability, and that use of these indicators may increase fecundability, presumably by helping couples time intercourse during the most fertile days (25).
For the time-varying analysis of fertility indicators, we identified cycles of use retrospectively, i.e., from what women reported using in the two months before their most recently-completed follow-up questionnaire. Thus, we did not have precise information on use of fertility indicators during every menstrual cycle. Recall bias for indicator use based on conception status is not a concern, because participants reported their use of fertility indicators before pregnancy status became known. The design of PRESTO included random assignment (1:1) for access to a premium FertilityFriend membership, which allows users to record use of each of the indicators examined and graphically display their fertile window (17). This built-in randomized trial presumably encouraged the use of fertility indicators in some participants who continued in the trial. However, the results were similar for analyses that accounted for changes in fertility indicator use over time and those that relied on use reported at baseline only.
We combined the category of charting days from the two responses of “chart menstrual cycles” and “count for days since last menstrual period” because we considered these conceptually congruent a priori. Consistent with this, 82% of the participants who checked “count for days since the last menstrual period” also checked “chart menstrual cycles.” However, we also conducted analyses with the categories separated. In those analyses, the two categories each had similar results to the combined category.
Based on the normal variability of the timing of ovulation, we expected counting days to be more weakly associated with fecundability than presumably more accurate indicators of ovulation, such as cervical fluid, cervix position, urine LH test (ovulation predictor kits) (1). Nonetheless, overall associations were similar across all single indicators. It may be that counting cycle days is as robust as the other indicators for successful timing of intercourse to conceive, or that use of any fertility indicator is associated with an unmeasured indicator of intensity of trying that correlates positively with fecundability.
The association of fertility indicator use with higher fecundability was largely limited to women who had been trying to conceive for <3 cycles at study entry. This result is broadly concordant with results from a randomized trial, based on urine hormonal monitoring (estrogen and LH; the ClearBlue fertility monitor), that found a greater effect of the fertility indicators in women who had been trying to conceive for <6 months as compared with ≥6 months (26). There was also a suggestion of a stronger association between fertility indicator use and fecundability among women with a past history of subfertility, which may seem paradoxical. Perhaps the greater effect of using fertility indicators is in earlier cycles, and at the same time there may be greater effect in women with lower baseline fecundability. We did not find any difference in our results when we stratified by age (data not shown). In addition, we conducted analyses that adjusted for geographic region (including Canada); there were essentially no changes in any of the effect estimates (data not shown). In addition, there was no appreciable difference in FRs when the analysis was restricted to women who had <1 cycle of attempt time entering the study, and/or who had only 2 cycles of follow-up (data not shown).
Our results are consistent with several prior cohort studies that have found positive associations between fertility indicator use and fecundability, particularly studies examining the effects of monitoring cervical fluid combined with charting cycles (27–29). Randomized trials have produced mixed results, some positive and some null, which may reflect unique difficulties in conducting trials among women trying to conceive (16, 26, 30). It is clear from our study that use of fertility indicators is already highly prevalent among pregnancy planners. These challenges are likely greater when studying couples with subfertility (31).
Our study is the largest to date to examine the role of fertility indicators on trying to conceive. While it is a geographically diverse study of pregnancy planners, with assessment of a wide variety of relevant factors for fecundability, the majority of women in our cohort have a college education. Thus, the results of our study may not be generalizable to populations with less education as the efficacy and effectiveness of fertility indicator use are likely to be positively associated with education. All information in our study, including fertility indicator use, was self-reported on questionnaires, so we do not have information about consistency or accuracy of use. Subject to these limitations, our results indicate that charting or tracking of cycles is associated with higher fecundability for women at the beginning of their pregnancy attempts, and that use of a combination of fertility indicators might be helpful for women trying to conceive.
Supplementary Material
Acknowledgements:
This research was supported by NICHD grants R21HD072326 and R01HD086742. We acknowledge the contributions of PRESTO participants and staff. We thank Mr. Michael Bairos for technical support in developing the study’s web-based infrastructure. All authors made significant contributions to the manuscript in accordance with the Vancouver group guidelines.
Footnotes
Conflict of Interest Disclosures: Drs. Hatch, Wise, Rothman, and Stanford and Ms. Willis report grants from National Institutes of Health during the conduct of the study. Dr. Wise reports in-kind donations from FertilityFriend.com (fertility apps for PRESTO), Swiss Precision Diagnostics (home pregnancy tests for PRESTO), and Sandstone Diagnostics (semen test kits for PRESTO) during the conduct of the study. Dr. Stanford reports personal fees from Swiss Precision Diagnostics, outside the submitted work; and is an unpaid member of Boards for two organizations that educate health professionals about fertility awareness methods: the International Institute for Restorative Reproductive Medicine (Board of Directors), and the Fertility Appreciation Collaborative to Teach the Science (Advisory Board).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stanford JB, White GL, Hatasaka H. Timing intercourse to achieve pregnancy: current evidence. Obstet Gynecol 2002;100:1333–41. [DOI] [PubMed] [Google Scholar]
- 2.Dunson DB, Baird DD, Wilcox AJ, Weinberg CR. Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation. Hum Reprod 1999;14:1835–9. [DOI] [PubMed] [Google Scholar]
- 3.Colombo B, Masarotto G. Daily fecundability: first results from a new data base. Demographic research 2000;3. [PubMed] [Google Scholar]
- 4.Keulers MJ, Hamilton CJCM, Franx A, Evers JLH, Bots RSGM The length of the fertile window is associated with the chance of spontaneously conceiving an ongoing pregnancy in subfertile couples. Hum Reprod 2007;22:1652–6. [DOI] [PubMed] [Google Scholar]
- 5.Wilcox AJ, Dunson D, Baird DD. The timing of the “fertile window” in the menstrual cycle: day specific estimates from a prospective study. British medical journal 2000;321:1259–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ecochard R, Boehringer H, Rabilloud M, Marret H. Chronological aspects of ultrasonic, hormonal, and other indirect indices of ovulation. BJOG 2001;108:822–9. [DOI] [PubMed] [Google Scholar]
- 7.American Society for Reproductive Medicine. Optimizing natural fertility: a committee opinion. Fertil Steril 2013;100:631–7. [DOI] [PubMed] [Google Scholar]
- 8.Ecochard R, Duterque O, Leiva R, Bouchard T, Vigil P. Self-identification of the clinical fertile window and the ovulation period. Fertil Steril 2015;103:1319–25 e3. [DOI] [PubMed] [Google Scholar]
- 9.Arevalo M, Sinai I, Jennings V. A fixed formula to define the fertile window of the menstrual cycle as the basis of a simple method of natural family planning. Contraception 1999;60:357–60. [DOI] [PubMed] [Google Scholar]
- 10.Brayer FT, Chiazze L Jr., Duffy BJ Calendar rhythm and menstrual cycle range. Fertil Steril 1969;20:279–88. [DOI] [PubMed] [Google Scholar]
- 11.Li D, Heyer L, Jennings VH, Smith CA, Dunson DB. Personalised estimation of a woman’s most fertile days. The European journal of contraception & reproductive health care : the official journal of the European Society of Contraception 2016;21:323–8. [DOI] [PubMed] [Google Scholar]
- 12.Berglund Scherwitzl E, Linden Hirschberg A, Scherwitzl R. Identification and prediction of the fertile window using NaturalCycles. The European journal of contraception & reproductive health care : the official journal of the European Society of Contraception 2015;20:403–8. [DOI] [PubMed] [Google Scholar]
- 13.Brennan JJ, Klaus H. Terminology and core curricula in natural family planning. Fertil Steril 1982;38:117–8. [DOI] [PubMed] [Google Scholar]
- 14.Manhart MD, Duane M, Lind A, Sinai I, Golden-Tevald J. Fertility awareness-based methods of family planning: A review of effectiveness for avoiding pregnancy using SORT. Osteopathic Family Physician 2013;5:2–8. [Google Scholar]
- 15.Weschler T Taking Charge of Your Fertility, 10th Anniversary Edition: The Definitive Guide to Natural Birth Control, Pregnancy Achievement, and Reproductive Health 10/31/2006 ed: Collins, 2008. [Google Scholar]
- 16.Manders M, McLindon L, Schulze B, Beckmann MM, Kremer JA, Farquhar C. Timed intercourse for couples trying to conceive. Cochrane Database Syst Rev 2015;3:Cd011345. [DOI] [PubMed] [Google Scholar]
- 17.Wise LA, Rothman KJ, Mikkelsen EM, Stanford JB, Wesselink AK, McKinnon C et al. Design and Conduct of an Internet-Based Preconception Cohort Study in North America: Pregnancy Study Online. Paediatr Perinat Epidemiol 2015;29:360–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Behre HM, Kuhlage J, Gassner C, Sonntag B, Schem C, Schneider HP et al. Prediction of ovulation by urinary hormone measurements with the home use ClearPlan Fertility Monitor: comparison with transvaginal ultrasound scans and serum hormone measurements. Hum Reprod 2000;15:2478–82. [DOI] [PubMed] [Google Scholar]
- 19.Wise LA, Rothman KJ, Mikkelsen EM, Sorensen HT, Riis A, Hatch EE. An internet-based prospective study of body size and time-to-pregnancy. Human Reproduction 2010;25:253–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weinberg CR, Wilcox AJ, Baird DD. Reduced fecundability in women with prenatal exposure to cigarette smoking. American Journal of Epidemiology 1989;129:1072–8. [DOI] [PubMed] [Google Scholar]
- 21.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. New York City, New York: Springer Verlag, 2000. [Google Scholar]
- 22.Greenland S, Daniel R, Pearce N. Outcome modelling strategies in epidemiology: traditional methods and basic alternatives. Int J Epidemiol 2016;45:565–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eijkemans MJC, Leridon H, Keiding N, Slama R. A Systematic Comparison of Designs to Study Human Fecundity. Epidemiology 2019;30:120–9. [DOI] [PubMed] [Google Scholar]
- 24.Mikkelsen EM, Riis AH, Wise LA, Hatch EE, Rothman KJ, Sorensen HT. Pre-gravid oral contraceptive use and time to pregnancy: a Danish prospective cohort study. Hum Reprod 2013;28:1398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tiplady S, Jones G, Campbell M, Johnson S, Ledger W. Home ovulation tests and stress in women trying to conceive: a randomized controlled trial. Hum Reprod 2013;28:138–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robinson JE, Wakelin M, Ellis JE. Increased pregnancy rate with use of the Clearblue Easy Fertility Monitor. Fertil Steril 2007;87:329–34. [DOI] [PubMed] [Google Scholar]
- 27.Bigelow JL, Dunson DB, Stanford JB, Ecochard R, Gnoth C, Colombo B. Mucus observations in the fertile window: a better predictor of conception than timing of intercourse. Hum Reprod 2004;19:889–92. [DOI] [PubMed] [Google Scholar]
- 28.Mu Q, Fehring RJ. Efficacy of achieving pregnancy with fertility-focused intercourse. MCN The American journal of maternal child nursing 2014;39:35–40. [DOI] [PubMed] [Google Scholar]
- 29.Evans-Hoeker E, Pritchard DA, Long DL, Herring AH, Stanford JB, Steiner AZ. Cervical mucus monitoring prevalence and associated fecundability in women trying to conceive. Fertil Steril 2013;100:1033–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stanford JB, Smith KR, Varner MW. Impact of instruction in the Creighton Model FertilityCare System on time to pregnancy in couples of proven fecundity: results of a randomised trial. Paediatr Perinat Epidemiol 2014;28:391–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thijssen A, Meier A, Panis K, Ombelet W. ‘Fertility Awareness-Based Methods’ and subfertility: a systematic review. Facts Views Vis OBGYN 2014;6:113–23. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.