Abstract
Background
Mental disorders are currently a global public health concern, particularly after the coronavirus disease 2019 (COVID-19) pandemic. Mental health services gradually transitioned to teleservices, employing various methods like texting and videoconferencing. This meta-analysis aimed mainly to quantify the acceptability of tele-mental health services among both beneficiaries and providers. Secondary objectives included quantifying the usability of and satisfaction with these services.
Methods
We conducted a systematic search of the following databases PubMed Central, SAGE, Google Scholar, Scopus, Web of Science, PubMed Medline, and EBSCO according to Preferred Reporting Items of the Systematic Reviews and Meta-Analysis (PRISMA) guidelines until December 2022.
Results
Out of 3366 search results, 39 studies fully met the inclusion criteria. The pooled acceptability of tele-mental health services among beneficiaries was [71.0% with a 95% confidence interval (CI) of 63.0 − 78.5%, I2 = 98%]. Using meta-regression, four key factors contributed to this heterogeneity (R2 = 99.75%), namely, year of publication, type of mental disorder, participant category, and the quality of included studies. While acceptability among providers was [66.0% (95%CI, 52.0 − 78.0%), I2 = 95%]. The pooled usability of tele-mental health services among participants was [66.0% (95%CI, 50.0 − 80.0%), I2 = 83%]. Subgroup analysis revealed statistically significant results (p = 0.003), indicating that usability was higher among beneficiaries compared to providers.
Conclusions
The study highlighted a high acceptability of tele-mental health services. These findings suggest a promising outlook for the integration and adoption of tele-mental health services and emphasize the importance of considering user perspectives and addressing provider-specific challenges to enhance overall service delivery and effectiveness.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-18436-7.
Keywords: Internet based, Mental health, Tele-mental health, Health service users, Acceptability, Telehealth, Telemedicine
Introduction
According to the World Health Organization (WHO), there is a remarkable global increase in mental disorders [1]. Approximately, 12.5% of the global population is affected by mental disorders, which can have deleterious effects on physical health, quality of life, social relationships, and occupational functioning. The prevalence of mental disorders is rising among adolescents and young adults worldwide [2]. It is worth noting that anxiety and depression are the leading causes of disability and premature mortality [3, 4]. Globally, suicide has become the fourth leading cause of death among the population aged 15–29 years, it accounts for over 700,000 deaths annually [5]. While many mental disorders can be effectively treated at a relatively low cost, there still exists a gap between the demand for care and its accessibility. This is because the effective coverage of mental health services remains very low. The WHO Special Initiative on Mental Health was launched (2019–2023), to ensure adequate access of patients with mental conditions to quality and affordable services [6].
Due to the coronavirus disease 2019 (COVID-19) pandemic, the delivery of healthcare services has remarkably changed globally [7]. To combat healthcare-associated infections, access to face-to-face or traditional consultations has been significantly limited, and the healthcare systems have resorted to remote service delivery techniques such as telehealth [8, 9]. The telehealth trend, with its potential to address many key challenges in healthcare, has been emerging worldwide. It enhanced health services accessibility, and timeliness in managing patients with physical and mental disorders. This is crucial particularly in public health crises such as epidemics and natural disasters [9, 10], in remote and rural areas, especially in countries with a large population [11]. Also, it can be used on a large scale to serve patients in isolated regions and even reach them across borders [12]. Furthermore, telehealth addresses disparities in mental health services stemming from shortages of professionals, brief visit durations, and the increasing prevalence of mental disorders [13].
Apart from diagnosis and treatment, tele-mental health also provides mental health education, psychotherapy and monitoring symptoms and adverse events. For example, changes in sleep and appetite, metabolic indicators in schizophrenic patients, and mood fluctuations in patients with bipolar disorder, which are hard to capture during short mental health professionals’ visits. This will pave the way to personalized mental health services, which in turn would enhance patients’ outcome and improve the quality of the delivered services [14].
In an Australian survey of parents, over one third of participants expressed a readiness to utilize therapist-guided and self-guided digital mental interventions, particularly to support their children [15]. A study in Mexico found that approximately half of its participants, including mental health professionals, patients, and the general population, viewed mental health services delivered via mobile phones as highly acceptable and recommended [13]. Moreover, 78.5% of Jamaican adolescents expressed interest in mobile phone-based digital interventions (mHealth) [16]. Furthermore, over 70% of African American women indicated convenience and willingness to use video calls to connect with professionals for managing anxiety and depression [17].
With growing interest in transformation of mental health services, particularly after the pandemic and among vulnerable group of beneficiaries from face to face to tele-services, it is crucial to have a comprehensive view towards user acceptability which establishes a prerequisite for usage and satisfaction, which are fundamental requirements for successful implementation of tele-mental health services. Through this meta-analysis, we aimed to cast light on the acceptance of implementing tele-mental health services (online, web-based interventions) among users. Additionally, it evaluated the usability and satisfaction of these services. The study findings would give the decision makers and other stakeholders a big hand in planning and executing more strategies to assure both availability and accessibility to tele-mental health services.
Methods
We performed this systematic review in strict compliance with the preferred reporting items of the systematic review and metanalysis (PRISMA) checklist. All steps were conducted in concordance with the Cochrane Handbook of systematic review and metanalysis [18].
Operational case definitions
Acceptance of healthcare interventions, which is “a multi-faceted construct that reflects the extent to which people delivering or receiving a healthcare intervention consider it to be appropriate, based on anticipated or experienced cognitive and emotional responses to the intervention” [19].
Usability is “the effectiveness, efficiency, and satisfaction with which users achieve goals in a specific environment” []. In healthcare, the “particular environment” mentioned in the definition can be: care settings, medical devices, software, workflows, and related processes [20]. The Healthcare Information and Management Systems Society [21] stated the main principals of usability of medical software are: simplicity, naturalness, consistency, minimizing cognitive load, efficient interactions, forgiveness and feedback, effective use of language, effective information presentation, and preservation of context [21].
Satisfaction is one of the key metrics used to assess service quality and usability [22]. Patient satisfaction embodies the patient's perceived need, expectations from the health system, and experience of health care. This multidimensional concept includes both medical and non-medical aspects of health care [23]. The acceptability of tele-mental health services among users denotes their willingness and openness to employ these services for their mental health care and treatment. In contrast, usability evaluates the ease of use and interaction design of the telehealth systems. Both acceptability and usability impact user satisfaction with their experience and outcomes when utilizing tele-mental health services.
The study outcomes
Primary outcome: Quantifying acceptance of tele-mental health services among its users either patients, providers, payors, or healthcare policy makers.
-
Secondary outcomes of the study include:
- Assessment of the usability of tele-mental health services.
- Evaluation of satisfaction levels with tele-mental health services.
Inclusion and exclusion criteria
The inclusion criteria for articles in the study encompassed a broad spectrum: all articles had to address the acceptance of tele-mental health services, characterized by mental health services provided when the patient and provider are not physically co-located, facilitated through web-based or mobile-based tools. The scope of mental disorders was inclusive, and any target population, comprising users of tele-mental health services including patients, providers, payors, and policy makers was considered eligible. Additionally, studies of any design, whether observational or interventional, were included, provided that they measured the acceptance of the service. There was no specified time limit for the search period.
The exclusion criteria for articles in the study were defined as follows: Short Message Service (SMS) based services were excluded as it isn't aligning with the definition of tele-mental health services. Articles written in languages other than English were also excluded. Additionally, case report, case series, editorial, letter to editor, conference abstract papers, paper can’t be accessed, and data can’t be extracted were excluded.
Search strategy
We searched EMBASE, Scopus, EBSCO, MEDLINE central/PubMed, SAGE, Web of Science, and Google Scholar databases for articles without timeframe or geographical restrictions till December 20, 2022. (Table S1).
Data organization, extraction, and quality assessment
All records were exported to an Endnote library to detect and remove duplicates using the “remove duplicate function”. All references that had the same title and author and were published in the same year or the same journal were removed. References remaining after this step were exported to a Microsoft Excel file with essential information for screening.
The title and abstract screening were done by two independent reviewers to select papers based on the inclusion criteria.
During the full-text screening phase, all selected articles were downloaded, and the full text was reviewed by two independent reviewers. If any disagreement was noticed, the senior author (RMG) was asked to make his decision.
Interrater agreement for both title and abstract screening, and full text screening were calculated and displayed as Cohen’s Kappa.
We applied backward and forward search methods to do manual searching. Backward search enclosed searching the reference lists of all included articles. Forward search involved citation tracking in which the reviewers tracked all the articles that cite each one of the included articles, and all ‘related to’ or ‘similar’ articles. All excluded records were given exclusion reasons.
The data extraction was then thoroughly conducted by five reviewers (RMA, EE, EAH, DHE & AG) and checked by RA. Data were synthesized using Microsoft Office 2016 Excel spread sheet as well as narrative format to extract (First author last name, year, study setting, type of study either face-to-face or online survey, sample size and demographics, type of population either patients, healthcare providers, payors, or policy makers). As a primary objective, mean or proportion of acceptance of tele-mental health services, tool used for assessment of acceptance and the method of its delivery, either online or face to face, were extracted. Also, type on mental health disorder targeted by the tele- services including mood and/or anxiety disorders, psychotic, personality, and substance related and addictive disorders, and severe mental disorders. Additionally, the type of tele-mental health service delivery either mobile application, mobile game, video conferencing, video consultation, social media plateform or others were also extracted. Type of intervention either diagnostic or therapeutic or both was also retrieved.
As additional objectives, mean and/or proportion of both usability and satisfaction and their data collection tools. Moreover, data regarding the type of remote intervention either diagnostic or therapeutic and the tool used either, video-based calls, mobile application or others were extracted whenever possible.
The quality of each study was examined based on a set of methodological criteria for such studies previously suggested by Newcastle-Ottawa Scale by two different reviewers and Interrater agreement was also calculated and displayed [24].
Statistical analysis
Publication bias: was assessed by visual inspection of the funnel plot. Publication bias was explored by Begg’s test, a p-value < 0.05 was defined, a priori, to indicate the possible presence of publication bias.
Quantitative data synthesis: Data extracted from the selected studies for each category were pooled in metanalyses by use of R software version 4.2 (meta and metafore packages). Data were reported as proportion, hence they were pooled using pooled prevalence, with the perspective of a 95% confidence interval (CI) in the meta-analysis model. In the case of zero frequency, the correction value of 0.1 was used. Random effect models were used if the test of heterogeneity for a group of study results was significant (defined conservatively as p < 0.20).
Forest plots were presented to visualize the degree of variation of effect size between studies.
-
Assessment of heterogeneity:
- Visual inspection of the forest plot.
- Cochrane I-Square test (I2), following Cochrane Handbook for Systematic Reviews of Interventions (I2), and it was interpreted as follows: “0–40%: might not be important; 30–60%: may represent moderate heterogeneity; 50–90%: may represent substantial heterogeneity; 75–100%: considerable heterogeneity. The importance of the observed value depends on the magnitude and direction of effects, and strength of evidence for heterogeneity.
- Meta-regression analysis was used to assess how the inclusion of predictors namely, year of publication, mental disorder type, participant category (patients, caregivers, general population, refugees) influenced the effect size of the studies, thereby explaining the significant heterogeneity observed.
- Leave one out sensitivity analysis. We conducted a leave-one-out sensitivity analysis using the metafor R tool. This involved recalculating the meta-analysis results K times while excluding one study each time. To identify influential studies, we used the influence () function, which includes a series of leave-one-out diagnostic tests. We categorized what we considered to be influential and sorted the studies in the plot using I2.
- Remove outlier function: If a study’s confidence interval does not align with that of the pooled effect, it’s identified as an outlier. These outliers significantly impact the overall effect and deviate notably from the aggregate result. Studies with high sampling error often diverge substantially from the pooled outcome. However, due to their wide confidence intervals, there’s a higher likelihood of overlap with one of the pooled effects. This fundamental technique for outlier detection is implemented using the “find outliers” function. It identifies and removes outlier studies within a meta-analysis, subsequently recalculating the result.
- Subgroup analysis: we categorized the usability of tele mental health services according to the type of user, either beneficiary or provider.
Results
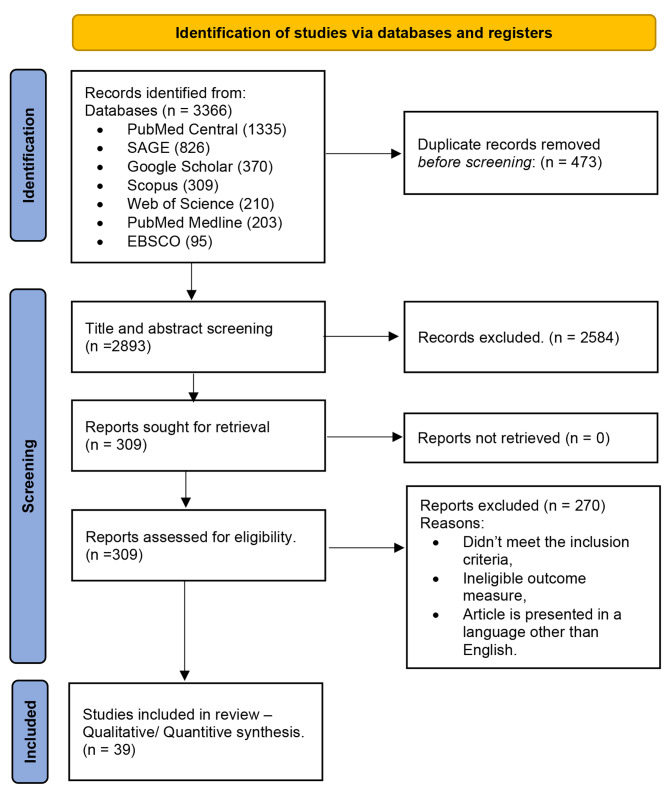
The PRISMA flow diagram summarized the study selection process. The included database’s search yielded a total of 3366 articles, before screening, 473 articles were removed for being duplicates. The screening phase involved 2893 articles proceeded to title and abstract screening, out of them, 2584 were removed as irrelevant and not coincident with inclusion criteria. Overall, 309 articles were eligible for full text screening and all of them were retrieved. Two hundreds and seventy articles were removed as they didn’t meet the inclusion criteria, ineligible outcome measure, article is presented in a language other than English. No new studies were encountered through the manual backward and forward search Fig. 1. The agreement between reviewers in title and abstract screening, full text screening, and quality assessment were substantial (k = 0.80, 0.88, 0.85), respectively.
Fig. 1.
PRISMA flow diagram for new studies which included searches of databases
A total of 39 studies published between 2004 and 2022 were included in the review, covering wide geographical locations and different types of mental disorders. Nine studies were conducted in the United States of America (USA) [17, 25–32], seven studies were conducted in Germany [33–40], three studies were conducted in the United Kingdom (UK) [41–43] and Australia [15, 16, 44], two studies were conducted in Netherlands [45, 46], France [47, 48] and China [49, 50], one study in Canada [51], Austria [33], Sweden [52], New Zealand [16], Portugal [53], and Estonia [54]. Studies from Africa included Egypt [40], Nigeria [55], Mozambique [56], and Kenya [57]. Additional one study was conducted in India [58] and in Mexico [13]. The studies’ populations were further classified as either healthcare beneficiaries, providers, or both. Studies enclosed different types of healthcare beneficiaries [13, 15, 17, 25, 27–30, 32–36, 38–41, 43–47, 50, 53–55, 57, 59] namely, general population, students, refugees, patients, pregnant women, parents of children who completed cancer treatment and other caregivers. Providers were represented either as healthcare workers (HCWs) or caregivers [16, 31, 37, 38, 51, 56, 58]. Some studies included both populations of providers and beneficiaries [26, 42, 48]. Studies covered many types of mental disorders, such as anxiety [13, 15, 17, 32, 35, 37, 44–46], mood changes [13, 15, 17, 25, 27, 30, 37, 39, 44–46, 53, 55, 59], psychotic disorders [27, 28, 33, 43, 50], neurocognitive disorders [26, 48], personality disorders [31], substance-related and addiction [29, 56, 57], severe mental illness [29, 58], and other non-specified mental disorders [16, 34, 36, 38, 40–42, 47, 49, 51, 52, 54]. Acceptability of tele-mental health services was studied for either educational [55], therapeutic [13, 15–17, 25, 28, 29, 31, 33–39, 42, 44–49, 52, 54, 56, 58], or diagnostic [26, 30, 41, 43, 59] services or both [27, 32, 40, 50, 51, 53, 57], Table 1.
Table 1.
All published studies that reported acceptability of tele-mental health services
| Study | Year | Participants | Age category | Mental disorder | Acceptance rate or Mean ± SD | Tool used | Method of application | Usability rate | Type of intervention | Quality |
|---|---|---|---|---|---|---|---|---|---|---|
| Country | Classified as; | Classified as; | Type of delivery | |||||||
| Design | Satisfaction | |||||||||
| Dietvorst [45] |
2022, Netherlands, Cross-sectional |
Students | Adolescences | Anxiety and depression | 72.60% | Questionnaire | Mobile application | Therapeutic | Satisfactory | |
| Dietvorst [45] | 75.60% | |||||||||
| Dietvorst [45] | Beneficiary | Mood Disorders; anxiety disorders | 7.1 ± 1.5 (from total score 10) | Online | ||||||
| Ericze´n [25] | 2012 | Pregnant | Adults | Maternal depression | 97.00% | Questionnaire | E-mental health interventions | Therapeutic | Satisfactory | |
| USA | Beneficiary | Mood disorders | Mixed | |||||||
| Cross-sectional | ||||||||||
| Mccall [17] | 2019 | Patients | Adults | Anxiety and depression | 70.00% | Questionnaire | Mobile phone | Therapeutic | Satisfactory | |
| USA | Beneficiary | Mood disorders; anxiety disorders | Online | |||||||
| Cross-sectional | ||||||||||
| Eichenberg [33] | 2016 | Patients | Adults | Psychological condition needs further investigation | 61.90% | Questionnaire | Serious game application | Therapeutic | Good | |
| Austria and Germany | Beneficiary | Psychotic disorders | Online | |||||||
| Cross-sectional | ||||||||||
| Woodford [52] | 2018 | Parents of children who had completed cancer treatment. | Adults | Mental health disorders | 74.10% | Questionnaire | Psychological interventions by internet | Therapeutic | Good | |
| Sweden | Beneficiary | Non specified | Online | |||||||
| Cross-sectional | ||||||||||
| Lincke [34] | 2022 | General population | All | Mental health disorders | 20.00% | Questionnaire | E-mental health interventions | Therapeutic | Good | |
| Germany | Beneficiary | Non specified | Online | |||||||
| Cross-sectional | ||||||||||
| Proudfoot [44] | 2010 | General population | Adults | Anxiety and depression | 76.00% | Questionnaire | Mobile phone | Therapeutic | Satisfactory | |
| Australia | Beneficiary | Mood disorders; anxiety disorders | Online | |||||||
| Cross-sectional | ||||||||||
| Damerau [35] | 2021 | Patients | Adults | Generalized anxiety disorder | 3.02 ± 1.14 | Questionnaire | E-mental health interventions | Therapeutic | Good | |
| Germany | Beneficiary | Anxiety disorders | Online | |||||||
| Cross-sectional | ||||||||||
| Greenwood [59] | 2004 | Patients | Adults | Overwhelmingly mood disorders | 80.00% | Questionnaire | Telepsychiatry | (12) 60% | Diagnostic | Unsatisfactory |
| -- | Beneficiary | Mood disorders | Mixed | |||||||
| Cross-sectional | (19) 95% | |||||||||
| Bruen [41] | 2020 | Patients | Adults | Mental health disorders | 86.00% | Data from app. | Swim App | 67 (84%) | Diagnostic | Good |
| UK | Beneficiary | Non- specified | ||||||||
| Cross-sectional | ||||||||||
| Hagen [36] | 2020 | Patients | Adults | Perceived stress, cognitive attitudes | 2.76 ± 1.16 | Questionnaire | Stress prevention programs | Therapeutic | Good | |
| Germany | Beneficiary | Non- specified | Mixed | |||||||
| Cross-sectional | ||||||||||
| Kenter [46] | 2013 | Patients | Adults | Anxiety and depression | 53.00% | Questionnaire | Problem solving treatment | Therapeutic | Satisfactory | |
| Netherlands | Beneficiary | Mood disorders; anxiety disorders | Online | |||||||
| Observation | ||||||||||
| Deb [58] | 2018 | Caregivers | Adults | Severe mental illness | 62.50% | Questionnaire | Mobile application | 16/34 (47.1%) | Therapeutic | Satisfactory |
| India | Provider | Face to Face | ||||||||
| Cross-sectional | ||||||||||
| Cloutier [51] | 2008 | HCWs | Adults | Mental health disorders | 92.00% | Questionnaire | Video conferencing | Diagnostic and Therapeutic | Satisfactory | |
| Canda | Provider | Non- specified | Online | |||||||
| Cross-sectional | ||||||||||
| Kiburi [57] | 2022 | Patients | Adults | Opioid use disorders | 95.00% | Questionnaire | Digital interventions | Diagnostic and Therapeutic | Satisfactory | |
| Kenya | Beneficiary | Substance-related and addictive disorders | Face to Face | |||||||
| Cross-sectional | ||||||||||
| Kola [55] | 2021 | Pregnant | Adolescences | Maternal depression | 96.20% | Questionnaire | Mobile application/ text messages | Educational | Satisfactory | |
| Nigeria | Beneficiary | Mood disorders | Face to Face | |||||||
| Cross-sectional | ||||||||||
| A. O’Grady [56] | 2021 | HCWs | Adults | Substance use (alcohol) | 4.33(± 0.45) | Questionnaire | Smartphone | Therapeutic | Satisfactory | |
| Mozambique | Provider | Substance-related and addictive disorders | Online | |||||||
| Cross-sectional | ||||||||||
| Linardon [15] | 2021 | Caregivers | Adults | Anxiety and depression | 30.00% | Questionnaire | Mobile phone | Therapeutic | Good | |
| Australia | Beneficiary | Mood disorders; anxiety disorders | Online | |||||||
| Cross-sectional | ||||||||||
| Sander [37] | 2021 | HCWs | Adults | Anxiety and depression | 36.00% | Questionnaire | Online platform | Therapeutic | Good | |
| Germany | Provider | Mood disorders; anxiety disorders | Face to Face | |||||||
| Cross-sectional | ||||||||||
| Tan [49] | 2020 | Patients– HCWs - General population | All | Mental health disorders | 50.00% | Questionnaire | Social media, Smartphone apps, Websites | Therapeutic | Satisfactory | |
| China | Beneficiary & Provider | Non-specified | Online | |||||||
| Cross-sectional | ||||||||||
| Hendrikof [38] | 2018 | Patients | Adults | Mental health disorders | 49.00% | Questionnaire | Video consultation | Therapeutic | Satisfactory | |
| Germany | Beneficiary | Non-specified | Mixed | |||||||
| Cross-sectional | ||||||||||
| Hendrikof [38] | 2018 | HCWs | Adults | Mental health disorders | 56.20% | Questionnaire | Video consultation | Therapeutic | ||
| Germany | Provider | Non-specified | Mixed | |||||||
| Cross-sectional | ||||||||||
| Landes [31] | 2021 | HCWs | Adults | Personality disorder | 73.00% | Questionnaire | Non-specified | Therapeutic | Unsatisfactory | |
| USA | Provider | Online | ||||||||
| Cross-sectional | ||||||||||
| Farrer [16] | 2022 |
HCWs (80.1% psychologist- 9.7% social workers- 5.3% counsellor) |
Adults | Mental health disorders | 73.00% | Questionnaire | Non-specified | 57.7% | Therapeutic | Satisfactory |
| Australia and New Zealand | Provider | Non-specified | Online | |||||||
| Cross-sectional | ||||||||||
| Harrell [26] | 2013 | Patients and caregivers | Geriatrics | Cognitive & psychological problems | 100.00% | Questionnaire | Videoconferencing | Diagnostic | Satisfactory | |
| USA | Beneficiary & Provider | Neurocognitive disorders | Face to Face | |||||||
| Cross-sectional | ||||||||||
| Cormi [47] | 2021 | HCWs | Adults | Mental health disorders | 38.00% | Questionnaire | Non-specified | Therapeutic | Good | |
| France | Beneficiary | Non-Specified | Online | |||||||
| Cross-sectional | ||||||||||
| Li [27] | 2022 | Patients | Adults | Anxiety and psychotic disorders | 87.00% | Questionnaire | Videoconferencing | Diagnostic and Therapeutic | Satisfactory | |
| USA | Beneficiary | Mood disorders; psychotic disorders | Telephone- based | |||||||
| Cross-sectional | ||||||||||
| Lynch [28] | 2020 | Patients | Adults | Complex psychosis | 89.00% | Questionnaire | Non-specified | Therapeutic | Satisfactory | |
| USA | Beneficiary | Psychotic disorders | Mixed | |||||||
| Cross-sectional | ||||||||||
| Mehrabian [48] | 2014 | Patients and caregivers. | Geriatrics | Cognitive impairment and Alzheimer’s disease | 65.00% | Questionnaire | Non-specified | Therapeutic | Satisfactory | |
| France | Beneficiary & Provider | Neurocognitive disorders | Face to Face | |||||||
| Cross-sectional | ||||||||||
| Benjet [13] | 2020 | Students | Adolescences | Anxiety and depression | 48.00% | Questionnaire | Mobile applications | Therapeutic | Good | |
| Mexico | Beneficiary | Mood disorders; anxiety disorders | Web Based | |||||||
| Cross-sectional | ||||||||||
| Painter [42] | 2021 | Patients and HCWs | Adults | Mental health disorders | 84.00% | Questionnaire | Video consultation | Therapeutic | Unsatisfactory | |
| UK | Beneficiary & Provider | Non-specified | Telephone- based | |||||||
| Cross-sectional | ||||||||||
| Gowarty [29] | 2021 | Patients | Adults | Severe mental illness, smoking cessation | 58.80% | Questionnaire | Mobile applications | Moderate to high satisfaction | Therapeutic | Unsatisfactory |
| USA | Beneficiary | Severe mental illness; Substance-related and addictive disorders | Face to Face | |||||||
| Mixed Methods | ||||||||||
| Tark [54] | 2019 | Patients | Paediatrics | Mental health disorders | 78.00% | Questionnaire | Mobile game | Therapeutic | Unsatisfactory | |
| Estonia | Beneficiary | Non-Specified | Face to Face | |||||||
| Cross-sectional | ||||||||||
| Guarino [32] | 2021 | Patients and healthy population | Adults | Anxiety and depression | 5.90 (± 0.4). | Questionnaire | Web-based program | Diagnostic and Therapeutic | Satisfactory | |
| USA | Beneficiary | Mood disorders; anxiety disorders | Online | |||||||
| Cross-sectional | ||||||||||
| Mayer [39] | 2022 | Patients | Adults | Depression | 0.25 ± (1.04) | Mixed | Mobile applications | Therapeutic | Good | |
| Germany | Beneficiary | Mood disorders | Face to face | |||||||
| Cross-sectional | ||||||||||
| Burchert [40] | 2019 | Refugees | Adults | Mental health disorders | Questionnaire | Web-based program | Diagnostic and Therapeutic | Satisfactory | ||
|
Germany, Sweden And Egypt |
Beneficiary | Non specified | Face to Face | |||||||
| Cross-sectional | ||||||||||
| Cella [43] | 2017 | Patients and healthy population | Adults | Schizophrenia | 80.000% | Questionnaire | Web-based program | Diagnostic | Satisfactory | |
| UK | Beneficiary | Psychotic disorder | Face to Face | |||||||
| Cross-sectional | ||||||||||
| Williams [30] | 2014 | Students | Adolescences | Depression | 93.80% | Questionnaire | Web-based program | Diagnostic | Unsatisfactory | |
| USA | Beneficiary | Mood disorders | Online | |||||||
| Cross-sectional | ||||||||||
| Xiao [50] | 2020 | Patients | Adults | Schizophrenia | 43.00% | Questionnaire | Web-based program | Diagnostic and Therapeutic | Satisfactory | |
| China | Beneficiary | Psychotic disorder | Face to Face | |||||||
| Cross-sectional | ||||||||||
| Fonseca [53] | 2016 | Pregnant women | Adults | Depression | Mean 2.73 (0.63) | Questionnaire | Web-based program | Diagnostic and Therapeutic | Satisfactory | |
| Portugal | Beneficiary | Mood disorders | Online | |||||||
| Cross-sectional |
Abbreviation list: App; Application, e; Electronic, HCWs; Healthcareworkers, UK: United Kingdom, USA: United States of America
Usability values are shown in bold
Acceptance of tele-mental health services
Acceptance of tele-mental health services among beneficiaries
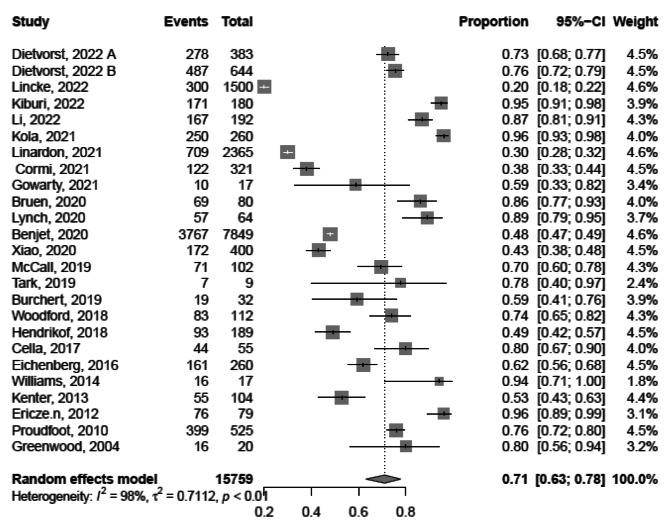
Based on the findings of 24 studies conducted from 2004 to 2022 [10, 13, 15, 28–30, 33, 34, 38, 40, 41, 43, 45–47, 50, 52, 54, 55, 57, 59–62], the pooled acceptance of tele-mental health services among beneficiaries was 71.0% with a 95% confidence interval (CI) of 63.0 − 78.5%, I2 = 98%. Acceptance of tele-mental health services ranged widely across the studies, from as low as 20% (95%CI, 18.0 − 22.0%) to as high as 96% (95%CI, 89.0 − 99.0%). Thus, a meta-regression was performed to explain this heterogeneity including year of publication, mental disorder type, participant category (patients, caregivers, general population, refugee) and the quality of included studies contributes (R2 = 99.75%), Fig. 2.
Fig. 2.
Forest plot showing acceptance of tele-mental health services among beneficiaries
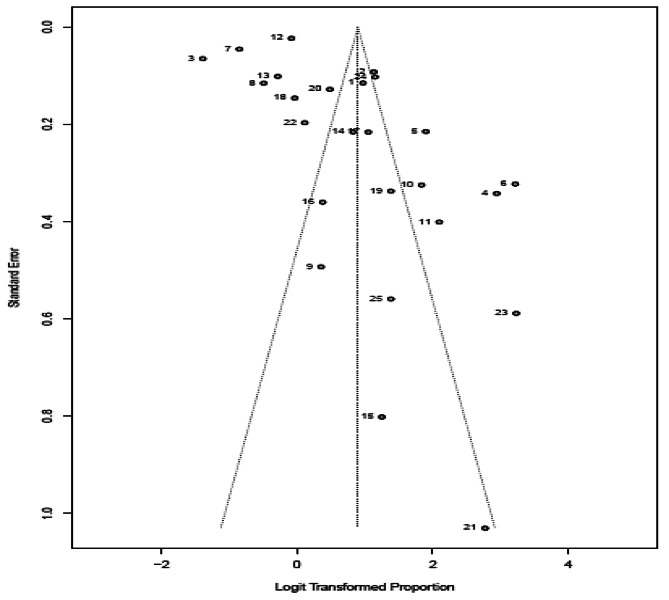
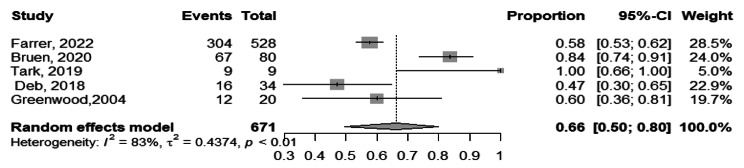
Visual inspection of funnel plot showed that studies with higher effect size are concentrated at the top of the pot. The Egger’s test result shows a value of 3.4 and a p-value of 0.002 indicating the presence of funnel plot asymmetry. This asymmetry may have implications for the interpretation of the studies and their associated evidence, indicating the possibility of publication bias or other sources of systematic bias, Fig. 3.
Fig. 3.
Funnel plot showing acceptance of tele-mental health services among beneficiaries
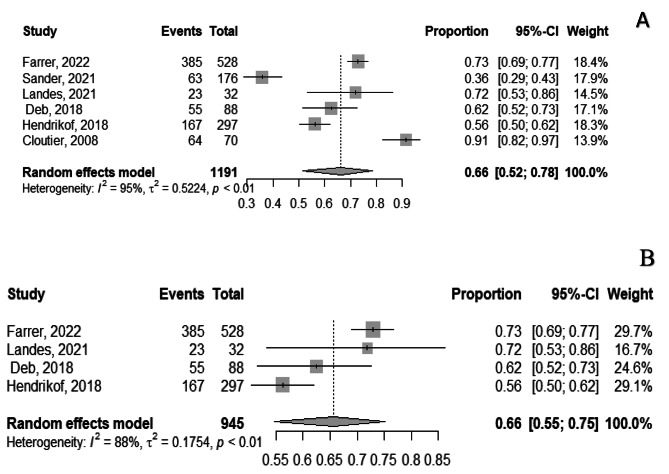
Acceptance of tele-mental health services among providers
Based on the findings of the 6 studies conducted from 2008 to 2022 [16, 31, 37, 38, 51, 58], the pooled acceptance of tele- mental health services among providers was 66.0%, (95%CI, 52.0 − 78.0%), I2 = 95%. The wide range of acceptance rates across the studies is evident, with the lowest acceptance reported at 36.0% (95%CI, 29.0- 43.0%) [37], and the highest acceptance at 91.0% (95%CI, 82.0 − 97.0%) [51], Fig. 4-A. After removal of outliers’ studies, Sander 2021, and Cloutier, 2008 the pooled acceptance was 66.0% (95%CI, 55.0 − 75.0%), and heterogeneity dropped to I2 = 88.0%, Fig. 4-B.
Fig. 4.
Forest plot showing acceptance of tele-mental health services among providers, after removal of two outlier studies (Sander, 2021, Cloutier 2008)
Visual inspection of the funnel plot revealed absence of publication bias. The Egger’s test result showed a (p-value = 0.838) that there is no evidence of funnel plot asymmetry, Fig. 5.
Fig. 5.
Funnel plot showing acceptance of tele-mental health services among providers
Acceptance of tele-mental health services among both (providers & beneficiaries)
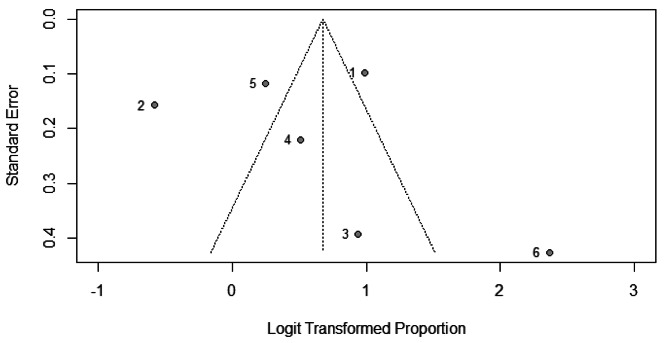
Concerning the acceptance of tele- mental health services in studies involving both providers and beneficiaries, there were a total of four studies conducted in 2013–2021 [26, 42, 48, 49], encompassing 734 participants. The pooled acceptance rate was 71.0% (95%CI, 51.0 − 85.0%), I2 = 87%, Fig. 6. However, after conducting a leave-one-out sensitivity analysis and excluding the study of Tan 2021 [49], the heterogeneity decreased to 77.0% and pooled acceptance raised to 83.0% (95%CI, 55.0 − 95.0%).
Fig. 6.
Forest plot showing acceptance of tele-mental health services among both providers and beneficiaries
Usability of tele-mental health services
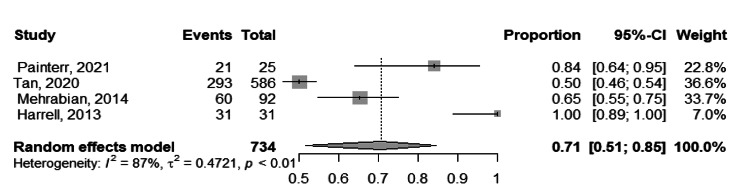
Based on the findings of the 5 studies [16, 41, 54, 58, 59], the pooled usability of tele-mental health services among the participants was 66.0% ranging from 47.0%, 100.0% with (95%CI, 50.0 − 80.0%), I2 = 83.0%, Fig. 7.
Fig. 7.
Forest plot showing usability of tele-mental health services among participants
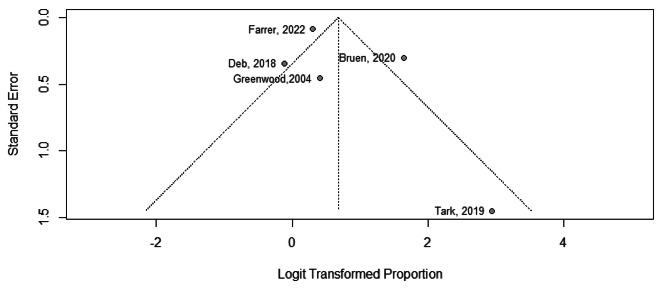
The visual inspection of the funnel plot, combined with Egger’s test result (p-value of 0.401), suggest that there is no evidence of publication bias, Fig. 8.
Fig. 8.
Funnel plot showing usability of tele-mental health services among participants
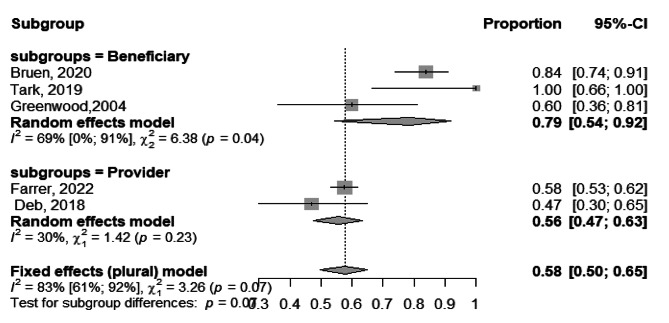
The subgroup analysis of usability of tele-mental health services among providers and beneficiaries yielded statistically significant results (p = 0.003), indicating that the subgrouping factor had a significant impact on the usability outcomes. Among beneficiaries [41, 54, 59], the pooled usability of telemedicine was found to be 79.0% (95%CI, 54.0 − 63.0%), I2 = 69.0%. On the other hand, among providers [16, 58], the pooled usability of telemedicine was 56.0% (95%CI, 47.0 − 53.0%), I2 = 30%, Fig. 9.
Fig. 9.
Forest plot showing usability of tele-mental health services among participants
Discussion
Tele-mental health has proven to be effective in managing common mental health disorders. Effectiveness of videoconferencing psychotherapy for the treatment of depression and anxiety disorder revealed a promising outcome in reducing depressive and improving anxiety symptoms [63, 64]. Also, mobile applications were effectively capable of well-assisting patients to reduce disease-related symptoms of mania, depression, and psychosis [65]. Hence, this review aimed mainly to quantify the acceptability of tele-mental health services among users namely, beneficiaries and providers, to enlighten health care decision at payor and policy makers levels about expanding the provision of these services on a broader scale. Secondary objectives included quantifying the usability of and satisfaction with these services. It assessed the acceptance of tele-mental health services for various mental disorders, including mood, anxiety, psychotic, personality, substance-related, and severe mental illness. The services were delivered through mobile applications, gaming, teleconferencing, video calls, and web-based programs. The multiple interfaces played by the tool or application make it more flexible as preventive, curative and it also provides a closer monitoring of the patient. This can be enhanced soon with inclusion of artificial intelligence in preventing risky behaviors or exacerbations of the mental health conditions. This review included 39 studies, over half of them were conducted after COVID-19 pandemic. Eleven studies revealed good quality, 22 studies were satisfactory, and only six studies were unsatisfactory. As pooled measure revealed high acceptability among the users, this would potentially encourage the delivery of interventional programs to deliver this type of services especially with the encountered proper usability and satisfaction.
Similar reviews were conducted to assess the acceptability of several forms of mental health services. Shek et al. [66], published a systematic review to assess acceptability and feasibility of technology-based interventions to support mental health after stroke revealed high acceptability, satisfaction, and adherence among these patients’ group. Additionally, Grist et al. [67], conducted a systematic review of studies involving children and adolescents less than 18 years to systematically appraise efficacy and acceptability of mobile apps for mental health They found that feasibility outcomes suggest high acceptability and moderate usage of this services. On the other hand, a scoping review was conducted by Apolinário-Hagen [68] to identify and evaluate the empirical evidence of public acceptability and attitudes towards e-mental health therapies, clarified that intentions to use this services was less than face-to-face services. An umbrella review was conducted to critically appraise the published reviews about Computerized Cognitive Behavioral Therapy revealed that this service must be individually tailored before being introduced to the users, to enhance its usability and adherence [69]. These reviews present a nuanced view of the acceptability of various mental health interventions, illustrating the opportunities and challenges in meeting the diverse needs of populations. Going forward, incorporating these insights into policy and practice has the potential to enhance the delivery and acceptance of mental health services. This integration can ultimately lead to improved outcomes for individuals in search of support and care.
Tele- health services were also used in other types of care. It yielded similar outcomes as face-to-face services in the management of heart failure, it could improve the control of blood glucose levels in patients with diabetes [70], and it improved the symptom management among rural palliative care population [71]. It is also acceptable and feasible in diagnosis and treatment of Human Immune Deficiency Viral infection among adults [72]. Compared to face-to face rehabilitation services, tele-rehabilitation yielded statistically significant improvements in quality of life, chronic respiratory disease and selfcare among community-dwelling patients with chronic diseases [73]. A survey for assessment of feasibility, acceptability, and usability of telehealth visits revealed that, vast majority of respondents (98%) were comfortable with this services [74].
Delivery of this tele-health services would undoubtedly improve accessibility especially with high acceptability among different categories of users, as this review clarified, among different age group or populations at risk e.g., care givers, pregnant women. Although clinical effectiveness was not studied in this review and it was claimed to be not improving over time [75], the growing penetration of this service and its intense use among adolescents and high acceptability among this age group is a good indicator of the potential growth of this service utilization over years.
Strengths & limitations
This review is one of the few studies that quantified perspectives of users regarding tele-mental health services acceptability, usability, and satisfaction. However, this review was limited to quantitative observational study designs with different tools which lead to high heterogeneity. Qualitative study designs are needed to provide in-depth insights regarding provision of these types of services particularly concerns related to safety and privacy. Also, this review didn`t investigate facilitators and barriers to acceptability and usability of tele-mental health services. A supporting review is needed to quantify the clinical effectiveness of this type of service before its full implementation in a healthcare system. In addition, articles written in language other than English were not included. Finally, we didn`t include grey literature and unpublished data, however, we performed a strict search of seven databases to get all the published data.
Conclusions
This systematic review and metanalysis addressed the global landscape of tele-mental health services, particularly in the post-COVID-19 period. Our findings suggest a promising perspective of the integration and adoption of tele-mental health services and underscore a distinction between beneficiaries and providers. Policy recommendations must encompass user directed interventions and training to facilitate the seamless integration of tele-mental health into healthcare systems. Further research should address concerns and barriers faced by providers in utilizing tele-mental health services.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We acknowledge the efforts introduced by our colleague Sally Waheed Elkhadry in database search, title and abstract screening and full text screening. Furthermore, we would like to express our gratitude to the Global Researcher Club for their invaluable consultation support, which has significantly expedited the advancement of this study.
Author contributions
The study was conceptualized and consensus on methodology was done by RMA, EE, RMG. Registration was done by RMA & EAH. Defining keywords for search was done by RMA & DHE. Database search was done by EAH & DHE. The first tier of title and abstract screening was done by RMA, EAH, DHE, SZ, second tier title and abstract screening was done by RMA, EAH, DHE, SZ. Full text screening and checking eligibility criteria was done by RMA, EAH, EE, DHE, RA, AG. Data extraction was done by RMA, EE, EAH, DHE & AG and reassessed by RA. Data analysis and results reporting was done by RA and reviewed by RMG. Introduction was drafted by SZ, methodology, discussion, and conclusion was drafted by RMA. RMA, EAH, EE, RA, RMG has reviewed the article, provided input. All coauthors approved the final form of the manuscript. EE was responsible for team management, articles management and work distribution.
Funding
This study received no funding.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Registration
Prospero registration was limited during the 2020 pandemic, to prioritize COVID-19 registrations.
Use of artificial intelligence (AI)
AI technologies were cautiously employed only to enhance the readability of this article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.(WHO) WHO. Mental health 2022 [ https://www.who.int/health-topics/mental-health#tab=tab_1.
- 2.Metrics, IoH. Evaluation. Global health data exchange (GHDx). Institute of Health Metrics and Evaluation Seattla, WA, USA; 2021.
- 3.Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):1517. doi: 10.1001/jama.2017.3826. [DOI] [PubMed] [Google Scholar]
- 4.WHO. Depression and other common mental disorders: global health estimates. World Health Organization; 2017.
- 5.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56(3):345–65. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 6.WHO. The WHO special initiative for mental health (2019–2023): universal health coverage for mental health. Geneva: World Health Organization. 2019 2019. Contract No.: WHO/MSD/19.1.
- 7.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18):1679–81. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 8.Bashshur R, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemedicine J e-health: Official J Am Telemedicine Association. 2020;26(5):571–3. doi: 10.1089/tmj.2020.29040.rb. [DOI] [PubMed] [Google Scholar]
- 9.Austin L, Sharp CA, van der Veer SN, Machin M, Humphreys J, Mellor P, et al. Providing ‘the bigger picture’: benefits and feasibility of integrating remote monitoring from smartphones into the electronic health record: findings from the remote monitoring of rheumatoid arthritis (REMORA) study. Rheumatology. 2020;59(2):367–78. doi: 10.1093/rheumatology/kez207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carneiro AC, de Pinho GS, Belo JV, Bolonhini S, Carneiro Neto MB, Mallet Toueg A et al. Outcomes of telemedicine care during the COVID-19 pandemic: experience from an intervention program designed for vulnerable population in Brazil. J Telemed Telecare. 2022:1357633X221089151. [DOI] [PMC free article] [PubMed]
- 11.Bradford NK, Caffery LJ, Smith AC. Telehealth services in rural and remote Australia: a systematic review of models of care and factors influencing success and sustainability. Rural Remote Health. 2016;16(4):1–23. [PubMed] [Google Scholar]
- 12.Wind TR, Rijkeboer M, Andersson G, Riper H. The COVID-19 pandemic: the ‘black swan’for mental health care and a turning point for e-health. Internet Interventions. 2020;20. [DOI] [PMC free article] [PubMed]
- 13.Benjet C, Wittenborn A, Gutierrez-García RA, Albor YC, Contreras EV, Hernández SC, et al. Treatment Delivery preferences Associated with type of Mental Disorder and Perceived Treatment barriers among Mexican University students. J Adolesc Health: Official Publication Soc Adolesc Med. 2020;67(2):232–8. doi: 10.1016/j.jadohealth.2020.01.025. [DOI] [PubMed] [Google Scholar]
- 14.Berrouiguet S, Perez-Rodriguez MM, Larsen M, Baca-García E, Courtet P, Oquendo M. From eHealth to iHealth: transition to participatory and personalized medicine in mental health. J Med Internet Res. 2018;20(1):e2. doi: 10.2196/jmir.7412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linardon J, Westrupp EM, Macdonald JA, Mikocka-Walus A, Stokes MA, Greenwood CJ, et al. Monitoring Australian parents’ shifting receptiveness to digital mental health interventions during the COVID-19 pandemic. Australian New Z J Psychiatry. 2022;56(11):1503–14. doi: 10.1177/00048674211065985. [DOI] [PubMed] [Google Scholar]
- 16.Farrer LM, Clough B, Bekker MJ, Calear AL, Werner-Seidler A, Newby JM, et al. Telehealth use by mental health professionals during COVID-19. Australian New Z J Psychiatry. 2023;57(2):230–40. doi: 10.1177/00048674221089229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCall T, Schwartz T, Khairat S. Acceptability of Telemedicine to help African American women manage anxiety and depression. Stud Health Technol Inform. 2019;264:699–703. doi: 10.3233/SHTI190313. [DOI] [PubMed] [Google Scholar]
- 18.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. 2008.
- 19.Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17(1):88. doi: 10.1186/s12913-017-2031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greene KK, Kelsey JM, Franklin JM. Measuring the usability and security of permuted passwords on mobile platforms. US Department of Commerce, National Institute of Standards and Technology; 2016.
- 21.Healthcare Information and Management Systems Society (HIMSS). Defining and Testing EMR Usability: Principles and Proposed Methods of EMR Usability Evaluation and Rating 2009.
- 22.Haron SN, Hamida MY, Talib A. Towards Healthcare Service Quality: an understanding of the Usability Concept in Healthcare Design. Procedia - Social Behav Sci. 2012;42:63–73. doi: 10.1016/j.sbspro.2012.04.167. [DOI] [Google Scholar]
- 23.De Silva A, Valentine N. A framework for measuring responsiveness: Citeseer; 2000.
- 24.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000.
- 25.Baker-Ericzén MJ, Connelly CD, Hazen AL, Dueñas C, Landsverk JA, Horwitz SM. A collaborative care telemedicine intervention to overcome treatment barriers for Latina women with depression during the perinatal period. Families Syst Health. 2012;30(3):224. doi: 10.1037/a0028750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harrell KM, Wilkins SS, Connor MK, Chodosh J. Telemedicine and the evaluation of cognitive impairment: the additive value of neuropsychological assessment. J Am Med Dir Assoc. 2014;15(8):600–6. doi: 10.1016/j.jamda.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 27.Li F, Mintz J, Sebastian V, Wang C, Kennedy C, Vyas S, et al. The acceptability of remotely delivered cognitive adaptation training. Schizophrenia Bull open. 2022;3(1):sgac062. doi: 10.1093/schizbullopen/sgac062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lynch DA, Medalia A, Saperstein A. The design, implementation, and acceptability of a telehealth comprehensive recovery service for people with complex psychosis living in NYC during the COVID-19 crisis. Front Psychiatry. 2020;11:581149. doi: 10.3389/fpsyt.2020.581149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gowarty MA, Longacre MR, Vilardaga R, Kung NJ, Gaughan-Maher AE, Brunette MF. Usability and acceptability of Two Smartphone Apps for Smoking Cessation among Young adults with Serious Mental illness: mixed methods study. JMIR Mental Health. 2021;8(7):e26873. doi: 10.2196/26873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams A, Larocca R, Chang T, Trinh NH, Fava M, Kvedar J, et al. Web-based depression screening and psychiatric consultation for college students: a feasibility and acceptability study. Int J Telemedicine Appl. 2014;2014:580786. doi: 10.1155/2014/580786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Landes SJ, Pitcock JA, Harned MS, Connolly SL, Meyers LL, Oliver CM. Provider perspectives on delivering dialectical behavior therapy via telehealth during COVID-19 in the Department of Veterans affairs. Psychol Serv. 2022;19(3):562. doi: 10.1037/ser0000571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guarino ID, Cowan DR, Fellows AM, Buckey JC. Use of a self-guided computerized cognitive behavioral tool during COVID-19: evaluation study. JMIR Formative Res. 2021;5(5):e26989. doi: 10.2196/26989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eichenberg C, Grabmayer G, Green N. Acceptance of Serious games in psychotherapy: an Inquiry into the stance of therapists and patients. Telemedicine J e-health: Official J Am Telemedicine Association. 2016;22(11):945–51. doi: 10.1089/tmj.2016.0001. [DOI] [PubMed] [Google Scholar]
- 34.Lincke L, Ulbrich L, Reis O, Wandinger E, Brähler E, Dück A, et al. Attitudes toward innovative mental health treatment approaches in Germany: E-mental health and home treatment. Front Psychiatry. 2022;13:889555. doi: 10.3389/fpsyt.2022.889555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Damerau M, Teufel M, Musche V, Dinse H, Schweda A, Beckord J, et al. Determining acceptance of e-mental health interventions in digital psychodiabetology using a quantitative web-based survey: cross-sectional study. JMIR Formative Res. 2021;5(7):e27436. doi: 10.2196/27436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Apolinário-Hagen J, Drüge M, Hennemann S, Breil B. Acceptance and commitment therapy for major depressive disorder: Insights into a new generation of face-to-face treatment and digital self-help approaches. Major Depressive Disorder: Rethinking and Understanding Recent Discoveries. 2021:311– 32. [DOI] [PubMed]
- 37.Sander J, Bolinski F, Diekmann S, Gaebel W, Günther K, Hauth I, et al. Online therapy: an added value for inpatient routine care? Perspectives from mental health care professionals. Eur Arch Psychiatry Clin NeuroSci. 2022;272(1):107–18. doi: 10.1007/s00406-021-01251-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hendrikoff L, Kambeitz-Ilankovic L, Pryss R, Senner F, Falkai P, Pogarell O, et al. Prospective acceptance of distinct mobile mental health features in psychiatric patients and mental health professionals. J Psychiatr Res. 2019;109:126–32. doi: 10.1016/j.jpsychires.2018.11.025. [DOI] [PubMed] [Google Scholar]
- 39.Mayer G, Hummel S, Oetjen N, Gronewold N, Bubolz S, Blankenhagel K, et al. User experience and acceptance of patients and healthy adults testing a personalized self-management app for depression: a non-randomized mixed-methods feasibility study. Digit Health. 2022;8:20552076221091353. doi: 10.1177/20552076221091353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burchert S, Alkneme MS, Bird M, Carswell K, Cuijpers P, Hansen P, et al. User-centered app adaptation of a Low-Intensity E-Mental Health Intervention for Syrian refugees. Front Psychiatry. 2018;9:663. doi: 10.3389/fpsyt.2018.00663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bruen AJ, Wall A, Haines-Delmont A, Perkins E. Exploring suicidal ideation using an innovative Mobile app-strength within me: the usability and acceptability of setting up a Trial Involving Mobile Technology and Mental Health Service users. JMIR Mental Health. 2020;7(9):e18407. doi: 10.2196/18407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Painter J, Turner J, Procter P. Understanding and accommodating patient and staff choice when implementing video consultations in Mental Health services. Computers Inf Nurs. 2021;39(10):578. doi: 10.1097/CIN.0000000000000804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cella M, Okruszek Ł, Lawrence M, Zarlenga V, He Z, Wykes T. Using wearable technology to detect the autonomic signature of illness severity in schizophrenia. Schizophr Res. 2018;195:537–42. doi: 10.1016/j.schres.2017.09.028. [DOI] [PubMed] [Google Scholar]
- 44.Proudfoot JG, Parker GB, Pavlovic DH, Manicavasagar V, Adler E, Whitton AE. Community attitudes to the appropriation of mobile phones for monitoring and managing depression, anxiety, and stress. J Med Internet Res. 2010;12(5):e1475. doi: 10.2196/jmir.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dietvorst E, Aukes MA, Legerstee JS, Vreeker A, Hrehovcsik MM, Keijsers L, et al. A Smartphone Serious game for adolescents (grow it! App): development, feasibility, and Acceptance Study. JMIR Formative Res. 2022;6(3):e29832. doi: 10.2196/29832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kenter R, Warmerdam L, Brouwer-Dudokdewit C, Cuijpers P, van Straten A. Guided online treatment in routine mental health care: an observational study on uptake, drop-out and effects. BMC Psychiatry. 2013;13(1):1–8. doi: 10.1186/1471-244X-13-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cormi C, Sanchez S, de l’Estoile V, Ollivier L, Letty A, Berrut G, et al. Telepsychiatry to provide Mental Health support to Healthcare professionals during the COVID-19 Crisis: a cross-sectional survey among 321 Healthcare professionals in France. Int J Environ Res Public Health. 2021;18:19. doi: 10.3390/ijerph181910146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mehrabian S, Extra J, Wu Y-H, Pino M, Traykov L, Rigaud A-S. The perceptions of cognitively impaired patients and their caregivers of a home telecare system. Med Devices: Evid Res. 2014:21–9. [DOI] [PMC free article] [PubMed]
- 49.Tan Y, Teng Z, Qiu Y, Tang H, Xiang H, Chen J. Potential of mobile technology to relieve the urgent mental health needs in China: web-based survey. JMIR mHealth uHealth. 2020;8(7):e16215. doi: 10.2196/16215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xiao S, Li T, Zhou W, Shen M, Yu Y. WeChat-based mHealth intention and preferences among people living with schizophrenia. PeerJ. 2020;8:e10550. doi: 10.7717/peerj.10550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cloutier P, Cappelli M, Glennie JE, Keresztes C. Mental health services for children and youth: a survey of physicians’ knowledge, attitudes and use of telehealth services. J Telemed Telecare. 2008;14(2):98–101. doi: 10.1258/jtt.2007.070815. [DOI] [PubMed] [Google Scholar]
- 52.Woodford J, Wikman A, Einhorn K, Cernvall M, Grönqvist H, Romppala A, et al. Attitudes and preferences toward a hypothetical trial of an internet-administered psychological intervention for parents of children treated for cancer: web-based survey. JMIR Mental Health. 2018;5(4):e10085. doi: 10.2196/10085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fonseca A, Gorayeb R, Canavarro MC. Women’s use of online resources and acceptance of e-mental health tools during the perinatal period. Int J Med Informatics. 2016;94:228–36. doi: 10.1016/j.ijmedinf.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 54.Tark R, Metelitsa M, Akkermann K, Saks K, Mikkel S, Haljas K, Usability Acceptability, feasibility, and effectiveness of a Gamified Mobile Health Intervention (triumf) for Pediatric patients: qualitative study. JMIR Serious Games. 2019;7(3):e13776. doi: 10.2196/13776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kola L, Abiona D, Adefolarin AO, Ben-Zeev D. Mobile phone use and acceptability for the delivery of mental health information among perinatal adolescents in Nigeria: survey study. JMIR Mental Health. 2021;8(1):e20314. doi: 10.2196/20314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.O’Grady MA, Mootz J, Suleman A, Sweetland A, Teodoro E, Anube A, et al. Mobile technology and task shifting to improve access to alcohol treatment services in Mozambique. J Subst Abuse Treat. 2022;134:108549. doi: 10.1016/j.jsat.2021.108549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kiburi SK, Paruk S, Chiliza B. Mobile phone ownership, digital technology use and acceptability of digital interventions among individuals on opioid use disorder treatment in Kenya. Front Digit Health. 2022;4:975168. doi: 10.3389/fdgth.2022.975168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sinha Deb K, Tuli A, Sood M, Chadda R, Verma R, Kumar S, et al. Is India ready for mental health apps (MHApps)? A quantitative-qualitative exploration of caregivers’ perspective on smartphone-based solutions for managing severe mental illnesses in low resource settings. PLoS ONE. 2018;13(9):e0203353. doi: 10.1371/journal.pone.0203353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Greenwood J, Chamberlain C, Parker G. Evaluation of a rural telepsychiatry service. Australasian Psychiatry. 2004;12(3):268–72. doi: 10.1080/j.1039-8562.2004.02097.x. [DOI] [PubMed] [Google Scholar]
- 60.Jones MD, Etherage JR, Harmon SC, Okiishi JC. Acceptability and cost-effectiveness of military telehealth mental health screening. Psychol Serv. 2012;9(2):132–43. doi: 10.1037/a0026709. [DOI] [PubMed] [Google Scholar]
- 61.McCall T, Schwartz T, Khairat S. Acceptability of telemedicine to help African American women manage anxiety and depression. MEDINFO 2019: health and wellbeing e. -Networks for All: IOS; 2019. pp. 699–703. [DOI] [PubMed] [Google Scholar]
- 62.Proudfoot J, Parker G, Hadzi Pavlovic D, Manicavasagar V, Adler E, Whitton A. Community attitudes to the appropriation of mobile phones for monitoring and managing depression, anxiety, and stress. J Med Internet Res. 2010;12(5):e64. doi: 10.2196/jmir.1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Berryhill MB, Culmer N, Williams N, Halli-Tierney A, Betancourt A, Roberts H, et al. Videoconferencing psychotherapy and depression: a systematic review. Telemedicine e-Health. 2019;25(6):435–46. doi: 10.1089/tmj.2018.0058. [DOI] [PubMed] [Google Scholar]
- 64.Batastini AB, Paprzycki P, Jones AC, MacLean N. Are videoconferenced mental and behavioral health services just as good as in-person? A meta-analysis of a fast-growing practice. Clinical psychology review. 2021;83:101944. [DOI] [PubMed]
- 65.Jørgensen SW, Lee K, Klausen SH, Petersen EN, Nørgaard B. Patients’ perspectives on telemedicine in the encounter between healthcare and patients with mental illness: a systematic review. Eur J Psychiatry. 2022.
- 66.Shek AC, Biondi A, Ballard D, Wykes T, Simblett SK. Technology-based interventions for mental health support after stroke: a systematic review of their acceptability and feasibility. Neuropsychological Rehabilitation. 2021;31(3):432–52. doi: 10.1080/09602011.2019.1701501. [DOI] [PubMed] [Google Scholar]
- 67.Grist R, Porter J, Stallard P. Mental health mobile apps for preadolescents and adolescents: a systematic review. J Med Internet Res. 2017;19(5):e176. doi: 10.2196/jmir.7332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Apolinário-Hagen J, Kemper J, Stürmer C. Public acceptability of e-mental health treatment services for psychological problems: a scoping review. JMIR Mental Health. 2017;4(2):e6186. doi: 10.2196/mental.6186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Treanor CJ, Kouvonen A, Lallukka T, Donnelly M. Acceptability of computerized cognitive behavioral therapy for adults: umbrella review. JMIR Mental Health. 2021;8(7):e23091. doi: 10.2196/23091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Reviews. 2015(9). [DOI] [PMC free article] [PubMed]
- 71.Bonsignore L, Bloom N, Steinhauser K, Nichols R, Allen T, Twaddle M, et al. Evaluating the feasibility and acceptability of a telehealth program in a rural palliative care population: TapCloud for palliative care. J Pain Symptom Manag. 2018;56(1):7–14. doi: 10.1016/j.jpainsymman.2018.03.013. [DOI] [PubMed] [Google Scholar]
- 72.Osingada CP, McMorris B, Piehler TF, Tracy MF, Porta CM. Acceptability, feasibility, and efficacy of telehealth interventions for HIV testing and treatment in adult populations. Telemedicine e-Health. 2023;29(7):1001–13. doi: 10.1089/tmj.2022.0424. [DOI] [PubMed] [Google Scholar]
- 73.Lee AYL, Wong AKC, Hung TTM, Yan J, Yang S. Nurse-led telehealth intervention for rehabilitation (telerehabilitation) among community-dwelling patients with chronic diseases: systematic review and meta-analysis. J Med Internet Res. 2022;24(11):e40364. doi: 10.2196/40364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gregory NS, Shukla AP, Noel JJ, Alonso LC, Moxley J, Crawford AJ et al. The feasibility, acceptability, and usability of telehealth visits. Front Med. 2023;10. [DOI] [PMC free article] [PubMed]
- 75.Stratton E, Lampit A, Choi I, Malmberg Gavelin H, Aji M, Taylor J, et al. Trends in effectiveness of organizational eHealth interventions in addressing employee mental health: systematic review and meta-analysis. J Med Internet Res. 2022;24(9):e37776. doi: 10.2196/37776. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.