Abstract
Women who exchange sex and use drugs (WESUD) are at high risk for HIV infection and partner violence. The few tested interventions at the intersection of HIV and IPV show mixed results. This analysis examined the impact of a combination HIV risk reduction (HIVRR) and microfinance (MF) intervention on reported paying and intimate partner violence against WESUD in Kazakhstan. This cluster randomized controlled trial enrolled 354 women from 2015 to 2018 and randomized them to either a combination of HIVRR and MF intervention or HIVRR alone. Outcomes were assessed at four time points over 15 months. Logistic regression within a Bayesian approach assessed change in odds ratio (OR) of recent physical, psychological, or sexual violence perpetrated by current or past intimate partners; and paying partners/clients by study arm over time. Compared to the control arm, the combination intervention decreased the odds of participants experiencing physical violence from past intimate partners by 14% (OR = 0.861, p = 0.049). Women in the intervention group reported significantly lower rates of sexual violence from paying partners (HIVRR + MF − HIVRR: 25.9%; OR = 0.741, p = 0.019) at 12-month follow-up. No significant differences in rates from current intimate partners were found. A combination HIVRR and microfinance intervention may reduce gender-based violence from paying and intimate partners among WESUD above and beyond HIVRR interventions alone. Future research should examine how microfinance reduces partner violence and how to implement combination interventions in diverse settings.
Keywords: Violence, Drug use, HIV Prevention Trials, Sex Workers, Economic Empowerment
Abstract
Las mujeres que intercambian sexo y consumen drogas (WESUD) tienen un alto riesgo de infección por VIH y violencia por parte de sus parejas. Las pocas intervenciones que se han probado en la intersección del VIH y la violencia de pareja muestran resultados mixtos. Este ensayo controlado aleatorio por grupos inscribió a 354 mujeres de 2015 a 2018 y las asignó al azar a una intervención combinada de HIVRR y MF o HIVRR sola. Los resultados se evaluaron en 4 puntos temporales durante 15 meses. La regresión logística dentro de un enfoque bayesiano evaluó el cambio en la violencia reciente perpetrada por las parejas que pagan y/o las parejas y ex-parejas (p.ej. esposos, novios) por brazo de estudio, a través del tiempo. En comparación con el grupo de control, la intervención combinada disminuyó las probabilidades de que los participantes sufrieran violencia física por parte de sus parejas íntimas anteriores en un 14% (OR = 0,861, p = 0,049). Las mujeres en el grupo de intervención informaron tasas significativamente más bajas de violencia sexual por parte de parejas que pagan (HIVRR + MF − HIVRR: 25,9%; OR = 0,741, p = 0,019) a los 12 meses de seguimiento. No se encontraron diferencias significativas en las tasas de parejas íntimas actuales. La combinación de HIVRR y microfinanzas puede ofrecer mayores reducciones en la violencia de las parejas que pagan y las ex-parejas en esta población.
Introduction
Globally, 26% of women have experienced physical or sexual violence from current or former intimate partners at least once in their lifetime [1]. Women engaged in sex work (WESW) are at exceptionally high risk for experiencing violence, with prevalence estimates ranging from 45–75% across the lifetime and 32–55% within the past year [2]. While we recognize that the term "female sex worker" or FSW is standard in publications, we would like to promote person-first language, “women engaged in sex work” or WESW, or “women who exchange sex” (WES) to be more accurate and culturally consonant, given that many women who engage in these behaviors do not necessarily identify as “sex workers.” The systemic nature of partner violence and its intersectionality with sex work is demonstrated by the broad range of perpetrators responsible for violence against WES: intimate partner violence (IPV) at the hands of spouses and current or past main sexual partners, in addition to clients, or paying partners or from pimps, police or others in the community due to high rates of stigma and criminalization of sex work [3]. Sex work further exacerbates the experience of violence for women who use drugs (WESUD), including those who inject drugs [4]. WESW who inject drugs face a 7-fold increase in the risk of client violence compared to WESW who do not inject, and frequent intoxication during sex work increases the risk of partner violence [5].
The overlap between sex work and drug use is especially prevalent in Eastern Europe and Central Asia since the collapse of the Soviet Union, which has resulted in dramatic declines in income and employment and has led to economic instability [6]. Population-level estimates of lifetime violence among WESUD from intimate partners and clients in Central Asia are estimated to be 23% and 7%, respectively. Central Asia is also among the regions with the least data available, and prevalence estimates may be underreported, especially among marginalized populations such as WESW or women who use drugs [1]. In Kazakhstan, over half (52%) and nearly one-third (30%) of women living with human immunodeficiency virus (HIV) experience intimate partner or client violence, respectively [7]. Modeling suggests that reducing physical and sexual violence has the potential to avert approximately 25% of incident HIV infections among WES and 6% in the general population, signaling the urgency of violence prevention interventions for WESUD [3].
The criminalization of sex work means sex workers are afforded little to no legal protection. This lack of legal protection translates to human rights violations and tolerance of violence against sex workers, exacerbated by gender and economic inequities and stigma [1, 4]. The direct and indirect consequences of partner violence include injury, depression, alcohol and other substance use disorders, unsafe sex practices which may result in STIs, including HIV/AIDS, or unplanned pregnancies, which may result in premature birth or low birth weight infants, and death from suicide or homicide [1]. Among WESUD, partner violence negates condom negotiation and engagement in healthcare, is associated with riskier sex and drug use behaviors, fear and avoidance of healthcare services, unwanted pregnancy, pregnancy loss, HIV and other STIs, and relapse to drug use [8–10].
Gender inequality, poverty, unemployment, and lack of economic opportunities are structural drivers of HIV and violence risk [11]. Economic strengthening interventions such as microfinance (MF) seek to empower women to achieve financial independence from their male partners and reduce financially driven decisions in sexual practices [12]. MF has been used as a development strategy to alleviate poverty by providing small-scale financial services for low-income households, particularly poor women living in rural areas who do not have access to traditional banking [13]. The field of MF has grown substantially from the microcredit model to include a wide range of programs to promote economic opportunities, such as vocational training, savings, and cash transfers [14].
Few interventions target HIV and partner violence risks among WESW [4, 15]. In South Asia, community empowerment approaches to HIV programming have led to higher uptake of HIV services and reduced violence from clients [16]. A multilevel intervention to reduce IPV and increase condom use among WESW in India found that despite a reduction in acceptance of IPV and increased awareness of self-protection strategies, there was no effect of the intervention on women’s experience of sexual and/or physical IPV or condom use [17]. A clinical trial in Mongolia examined the efficacy of an HIV/ sexually transmitted infections (STIs) prevention intervention bolstered with motivational interviewing sessions to reduce partner violence. Although no significant differences were observed between the three conditions (HIV risk reduction [HIVRR]), HIVRR and motivational interviewing, control condition with wellness promotion), women in all groups experienced reduced physical and sexual violence from paying and intimate partners combined [18].
A growing body of empirical studies has evaluated the impact of MF interventions for women at the intersections of HIV and IPV. However, a comprehensive review points to mixed results for the impact of MF on women’s experiences of violence and to a critical gap in our understanding of the efficacy of MF interventions among WESW [19]. An RCT conducted in Cote d’Ivoire among rural women found that those who attended intervention sessions with their male partners (gender dialogue plus group savings) reported significantly reduced physical IPV in the past year compared to women who attended the group savings alone [20]. Additionally, women in the treatment group were significantly less likely to report economic abuse. In South Africa, a community-mobilization intervention that offered microloans paired with gender and life skill sessions reduced physical or sexual IPV in the last 12 months in treatment villages compared with the age-matched random sample in control villages [21]. A hybrid microcredit and livestock asset transfer intervention in Congo found that women reported a reduction in all types of IPV at ten months post-baseline. However, there was no significant difference between the intervention and control groups [22]. Some MF studies that demonstrated increased IPV were possibly due to contextual factors such as conservative cultural values, economic status, or urban settings [23, 24]. However, adverse IPV impacts have been found in associational studies only, and there is a need for further longitudinal, causal evidence [19].
Despite global evidence for an overwhelming burden of HIV and violence, poverty, and gender inequality among WESW, few MF interventions focus on WESW [19]. Furthermore, there is less attention to the impact of asset-based approaches to MF, which may be less risky for WESW. Asset-based MF can foster economic independence through increased job opportunities and assets (e.g., savings, livestock) without the burden of high-interest rates or over-reliance on debt often associated with the microcredit model [24]. To our knowledge, only one study, Undarga, used a randomized control trial to evaluate the efficacy of an asset-based MF intervention in combination with HIVRR education among WESW in Mongolia [25]. The study found that the MF group reported significantly fewer acts of unprotected sex and a lower percentage of income from sex work at six months post-intervention compared to the control group. Additionally, participants from both study groups reported decreased client violence, with the intervention group reporting a larger decrease than the control group [26]. However, the Undarga study did not explore women’s experience with violence from current intimate partners and did not include WESUD.
A closer examination of the combined impact of MF and HIV risk reduction interventions on partner violence against WESUD is urgently needed. This study examined the impact of a combination HIVRR and MF intervention on reducing violence from paying and/or intimate partners among WESUD in Kazakhstan.
Methods
This study utilized a cluster-randomized controlled trial (cRCT) design to compare participants receiving HIVRR alone versus those receiving HIVRR + MF. The original study outcomes focused on HIV risk reduction are published elsewhere [27]. The current study focuses on a secondary outcome - the impact of the intervention (HIVRR + MF) on reducing paying and intimate partner violence compared to participants receiving the HIVRR alone. Recruitment and enrollment began in May 2015, and follow-up data collection ended in October 2018. All procedures received approval from the Institutional Review Board (IRB) at the investigators’ university and the Ethics Committee of the Kazakhstan School of Public Health.
Recruitment of Participants
The study took place in two Kazakhstan cities, Almaty and Temirtau. We recruited participants from partner NGOs, medical and social service organizations, and peer referrals. Research assistants distributed informational brochures and conducted outreach to provide study information to potential participants. Additional detail on recruitment is published elsewhere [28].
Screening for Eligibility
Research assistants administered an eligibility screening using a computer-based program to determine if participants met the following criteria for eligibility: (a) being over 18 years old; (b) illicit drug use within the past 12 months; (c) having provided sex in return for money, goods, drugs or services within the past 90 days; and (d) at least one incidence of unprotected sex (with either paying or non-paying partner) within the past 90 days. Participants were ineligible if they (a) could not communicate in Russian, (b) intended to move from the study site within the next year, or (c) were determined to have cognitive impairment that would affect their ability to provide consent or participate fully in the intervention. Participants received $1 for screening completion. To ensure retention, participants complete a comprehensive contact form in which they share names, addresses, and mobile phone contacts with family or friends they will allow to share their whereabouts with study team members over time. Additionally, the study team reached out to confirm contact information quarterly.
Study Procedures
Randomization
Eligible, interested participants completed an informed consent process at a field office, followed by a baseline assessment. Within two weeks, we randomized each cohort of 6–8 participants to either the treatment (HIVRR + MF) or control (HIVRR only) arm of the study using a random number generator conducted by the study biostatistician. Neither participants nor study staff were blind to study arm assignments. Outcomes were assessed at four time points over 15 months, encompassing three months of intervention activities and 12 months of follow-up (baseline prior to cohort assignment and randomization, then at 3-, 6- and 12-months post-intervention). Participants received 10 USD for baseline, 9 USD for 6-month, and 11 USD for 12-month follow-up completion.
Intervention
Detailed information on intervention components, selection, and adaptation is provided elsewhere [27, 28]. Participants in both arms received four HIVRR sessions over two weeks. Those assigned to the combination HIVRR + MF treatment arm received 30 sessions over three months. The study intervention consisted of three interventions components: (1) six sessions focused on financial literacy, (2) 24 sessions of vocational training in hairdressing, sewing, or manicurist professions, and (3) a matched savings program that incentivized participants to accumulate assets for small business development or job/vocational training. Participants received small financial incentives (12 USD per session) for each session attended and safer-sex kits of condoms and lubricants. Sessions included safety check-ins to assess whether participants experienced intimate partner or gender-based violence related to or unrelated to study participation. Facilitators referred participants who reported violence to the research team, who linked women to requested services [28].
Partner Violence Reduction Activities: HIVRR
The HIVRR intervention (received by all participants) contained two specific activities related to violence prevention and safety check-ins. The first activity aimed to reduce the stigma associated with discussing partner violence and to help women recognize, identify, describe, and avoid future abusive behaviors that they have witnessed or experienced. Participants were paired and given cards that describe various abusive behaviors (e.g., depriving women of their basic needs, following her to see where she is going, being forced to have sex) to identify the types of abuse. They also discussed how drug and alcohol use may precede or follow experiences of violence. Facilitators spoke about how violence and abuse are related to power and control, how violence fits within cultural norms and traditions in Kazakhstan and intimate relationships, and how violence may impede help-seeking. Participants were asked to tape each card onto a flipchart with the categories including physical, psychological, sexual, and economic abuse. A brief three-question partner violence screening was read aloud, and participants were asked if any of these experiences had happened to them. Any participants who answered yes were invited to meet with the project staff after the group for further confidential discussion and safety planning.
The second activity focused on safety planning with paying partners. Participants were asked to identify scenarios in which a woman’s safety can be threatened by paying partners, including alcohol and substance use, condom refusal, and police encounters. As a group, participants discussed and created a list of strategies they have used or believed they could use to protect themselves in such situations if/as they arise with paying partners.
Partner Violence Reduction Activities: Microfinance (MF)
In addition to HIVRR sessions, facilitators conducted safety check-ins at the six financial literacy training (FLT) sessions. At the beginning of each session, facilitators asked participants whether they were currently experiencing any aggression or violence at the hands of someone in their family or friends, including paying partners, or community members. If any women reported a lack of safety, they were asked to remain after the session to develop a safety plan.
Measures
Participants completed computer-assisted interviews at each of the four time points. Age was expressed in years; study sites corresponded to a categorical variable identifying participants living in Almaty or Temirtau. Age of initiating sex work was recoded into a binary variable to identify participants who started sex work before or after the age of 18; years of sex work consisted of a self-report continuous variable; marital status was measured categorically, composed of three levels; prior incarceration/detention/arrest consisted of a binary variable identifying participants who have been arrested, or detained or arrested (1 vs. 0); substance use consisted of a binary variable, corresponding to 1 if participants used any substance including marijuana, ecstasy, cocaine, heroin or 0 if participants used no substance in the past 90 days. Outcomes were measured using an adaptation of the Revised Conflict Tactics Scale. Items can be measured as a dichotomous variable representing the prevalence of each violent tactic and by summing the number of times the acts in the scale occurred to define the chronicity of violence [29]. We assessed Physical, Psychological, and Sexual partner violence using four items for each type. We dichotomized violence variables to determine whether participants experienced violence in the past 90 days. In other words, if a participant endorsed at least one of the items assessing physical violence, their corresponding score was 1. If participants did not endorse any items assessing physical violence, their score was 0. Each type of violence was assessed based on whether it was perpetuated by a current intimate partner(s), past intimate partner(s), or paying partners. Paying partners were defined as those partners with whom participants exchanged sex for money or drugs, or other goods in the past 90 days.
Data Analysis
To test the change in rates of IPV by study arm over time, we used logistic mixed effect models with Bernoulli distribution and logit link. The analysis was adjusted for repeated measures, with participant id as the clustering variable. All models included random intercepts, uninformative priors, and time was treated as a continuous variable. We used a Bayesian estimator coupled with an intent-to-treat approach to reduce the potential estimation bias from missing data (e.g., loss to follow-up). All regression models were adjusted for the following, a priori, theoretical covariates: Age, study site, education, age started sex work, years of sex work, and time-varying covariates, including current relationship status (i.e., whether married now or previously), prior incarceration/detention/arrest, and any recent illicit substance use. The estimates produced consist of odds ratios (OR). Analysis was completed using the brm function in the brms package in R [30].
Results
We screened 763 individuals, of whom 401 met eligibility criteria and completed the baseline assessment. Of these, 354 participants, for a total of 53 cohorts of 6–8 participants, were randomized into either the HIVRR + MF arm (n = 175) or the HIVRR arm (n = 179). There were no significant differences between study arms with respect to overall retention rates (p > 0.05) (HIVRR + MF = 92.7% vs. HIVRR = 92.7%; retention rates at each follow-up are provided in Fig. 1). Both arms had high HIVRR attendance (average of 3.5 of 4 sessions; 87.5%). HIVRR + MF participants had an average session attendance of 4.9 out of 6; 81.7%, and 19.6 out of 24; 81.7%, for FLT and VT, respectively. Over 75% (n = 133) of HIVRR + MF participants were eligible for the matched savings, but only 86 (49.1%) deposited money. The average deposit was US $149. Data Safety Monitoring Board (DSMB) members and investigators identified no safety concerns related to intervention participation. Table 1 describes sociodemographic characteristics at baseline assessment for 354 participants by intervention assignment. Sociodemographic characteristics did not differ significantly between the two arms.
Fig. 1.
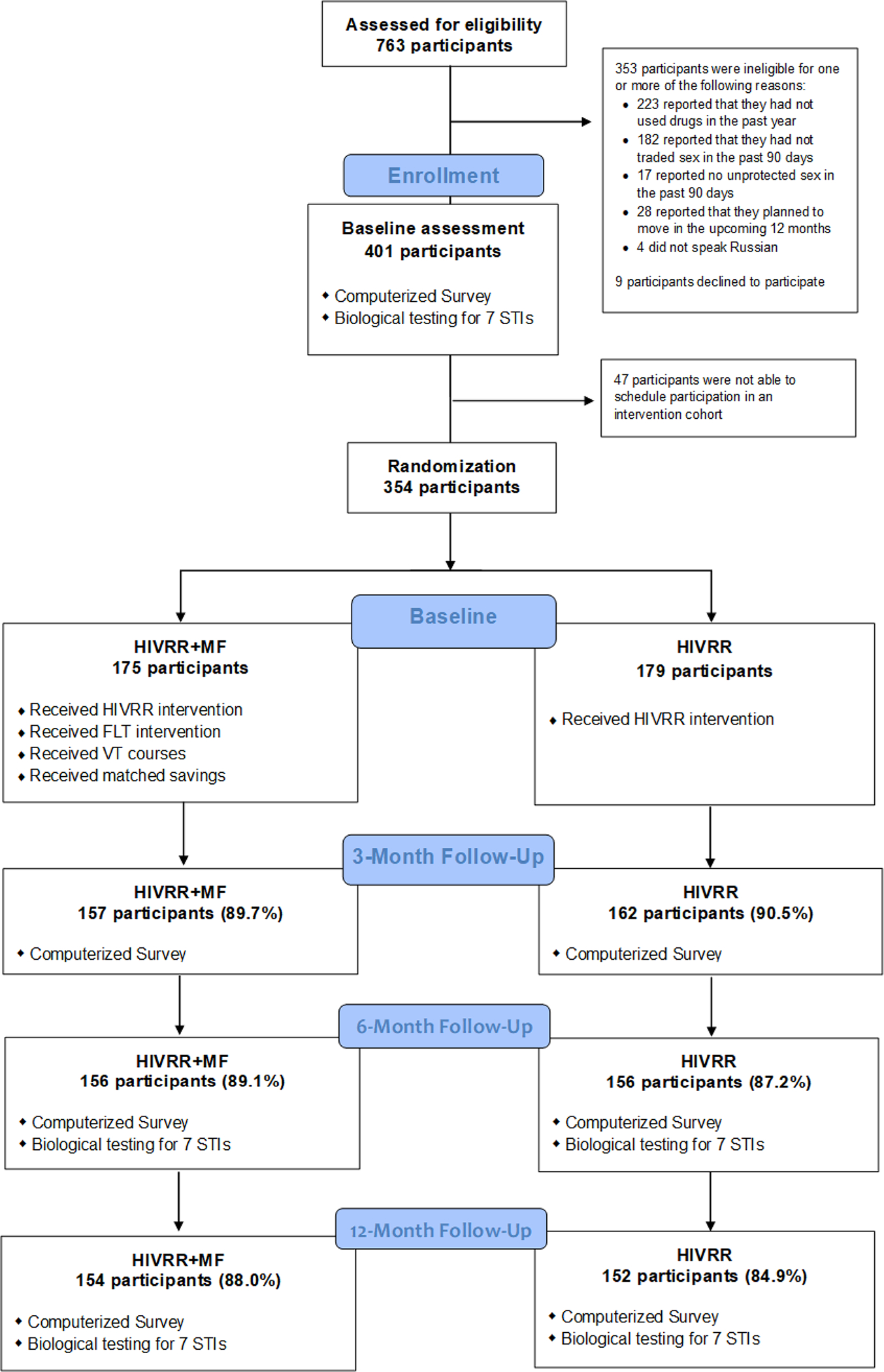
CONSORT Flow Diagram
Table 1.
Descriptive statistics of the sample reported at the baseline assessment
| Total (N = 354)a n (%) |
HIVRR (N = 179)a n (%) |
HIVRR + MF (N = 175) n (%) |
|
|---|---|---|---|
|
| |||
| Age, mean (SD) | 34.0 (8.4) | 34.0 (8.4) | 34.1 (8.4) |
| Almaty site | 222 (62.9%) | 109 (61.2%) | 113 (64.6%) |
| Russian | 238 (67.4%) | 119 (66.9%) | 119 (68.0%) |
| Completed high school and above | 239 (67.7%) | 120 (67.4%) | 119 (68.0%) |
| Single, never married | 110 (31.2%) | 55 (30.9%) | 55 (31.4%) |
| Married or common law marriage | 96 (27.2%) | 48 (27.0%) | 48 (27.4%) |
| Has a main partner | 194 (45.%) | 96 (53.9%) | 98 (56.0%) |
| Homeless in the past 90 day | 204 (57.8%) | 109 (61.2%) | 95 (54.3%) |
| Not enough money to buy food in the past 90 days | 319 (90.4%) | 162 (91.0%) | 157 (89.7%) |
| Years in sex work, mean (SD) | 9.8 (7.3) | 10.2 (7.2) | 9.3 (7.3) |
| Any drug use in the past 90 days | 288(81.6%) | 145(81.5%) | 143(81.7%) |
| Been arrested or detained in the past 90 days | 100 (28.3%) | 53 (29.8%) | 47 (26.9%) |
| Been in jail or prison in the past 90 days | 11 (3.1%) | 5 (2.8%) | 6 (3.4%) |
Abbreviations: HIVRR = HIV Risk Reduction; HIVRR + MF = HIV Risk Reduction and Microfinance
Note:
1 missing case
Table 2 illustrates the descriptive statistics of each IPV type by perpetrator. Statistics are stratified by study arm by time. Rates of abuse did not vary widely depending on partner type. Table 2 shows trends in reductions over time from baseline to 12-month follow-up.
Table 2.
Descriptive Statistics of current, past, and paying partner violence by time and study arm
| Baseline | 3-month | 6-month | 12-month | ||
|---|---|---|---|---|---|
|
| |||||
| Current partner | Sexual violence | ||||
| Control group, n (%) | 36 (20.2) | 18 (11.1) | 13 (8.3) | 13 (8.6) | |
| Intervention group, n (%) | 25 (14.3) | 14 (8.9) | 9 (5.8) | 4 (2.6) | |
| Physical violence | |||||
| Control group, n (%) | 39 (21.9) | 26 (16.0) | 15 (9.6) | 12 (7.9) | |
| Intervention group, n (%) | 42 (24.0) | 21 (13.4) | 19 (12.2) | 10 (6.5) | |
| Psychological violence | |||||
| Control group, n (%) | 35 (19.7) | 29 (17.9) | 29 (18.6) | 21 (13.8) | |
| Intervention group, n (%) | 40 (22.9) | 32 (20.4) | 28 (17.9) | 16 (10.4) | |
| Past partner | Sexual violence | ||||
| Control group, n (%) | 29 (16.3) | 9 (5.6) | 4 (2.6) | 4 (2.6) | |
| Intervention group, n (%) | 28 (16.0) | 9 (5.7) | 3 (1.9) | 0 (0.0) | |
| Physical violence | |||||
| Control group, n (%) | 42 (23.6) | 13 (8.0) | 7 (4.5) | 8 (5.3) | |
| Intervention group, n (%) | 39 (22.3) | 10 (6.4) | 1 (0.6) | 3 (1.9) | |
| Psychological violence | |||||
| Control group, n (%) | 45 (25.3) | 15 (9.3) | 10 (6.4) | 10 (6.6) | |
| Intervention group, n (%) | 47 (26.9) | 16 (10.2) | 7 (4.5) | 6 ( 3.9) | |
| Paying partner | Sexual violence | ||||
| Control group, n (%) | 38 (21.3) | 10 (6.2) | 5 (3.2) | 3 (2.0) | |
| Intervention group, n (%) | 38 (21.7) | 9 (5.7) | 2 (1.3) | 0 (0.0) | |
| Physical violence | |||||
| Control group, n (%) | 34 (19.1) | 8 (4.9) | 1 (0.6) | 2 (1.3) | |
| Intervention group, n (%) | 32 (18.3) | 8 (5.1) | 1 (0.6) | 3 (1.9) | |
| Psychological violence | |||||
| Control group, n (%) | 49 (27.5) | 14 (8.6) | 5 (3.2) | 2 (1.3) | |
| Intervention group, n (%) | 37 (21.1) | 12 (7.6) | 7 (4.5) | 3 (1.9) | |
In Table 3, we report the results of the regression analysis. Overall, physical, sexual, and psychological IPV decreased over time. There were no significant reductions in violence among women in the intervention group from their current intimate partners. However, Table 3 shows that compared to the control arm, the intervention decreased the odds of experiencing physical violence from past intimate partners by 14% (OR = 0.861, p = 0.049). Women in the intervention group reported significantly lower rates of sexual violence from paying partners (HIVRR + MF − HIVRR: 25.9%; OR = 0.741, p = 0.019).
Table 3.
Change in current, past, and paying partner IPV by arm over time: logistic Bayesian mixed model
| Sexual violence | Physical violence | Psychological violence | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Current partner | aOR | CIs | p | aOR | CIs | p | aOR | CIs | p | |
| Interv | 0.726 | (0.379–1.391) | 0.340 | 1.041 | (0.560–1.935) | 0.901 | 1.350 | (0.719–2.535) | 0.354 | |
| Time | 0.914 | (0.852–0.98) | 0.007 | 0.887 | (0.819–0.951) | 0.000 | 0.970 | (0.914–1.03) | 0.304 | |
| Time*Interv | 0.932 | (0.827–1.03) | 0.193 | 0.970 | (0.887–1.073) | 0.599 | 0.932 | (0.861–1.01) | 0.111 | |
| Past partner | Sexual violence | Physical violence | Psychological violence | |||||||
| aOR | CIs | p | aOR | CIs | p | aOR | CIs | p | ||
| Interv | 1.197 | (0.583–2.484) | 0.613 | 1.051 | (0.566–1.935) | 0.865 | 1.271 | (0.691–2.27) | 0.441 | |
| Time | 0.819 | (0.726–0.914) | 0.001 | 0.878 | (0.803–0.951) | 0.002 | 0.869 | (0.803–0.942) | 0.000 | |
| Time*Interv | 0.852 | (0.684–1.041) | 0.117 | 0.861 | (0.726–1.000) | 0.049 | 0.932 | (0.827–1.051) | 0.245 | |
| Paying partner | Sexual violence | Phy sical violence | Psychological violence | |||||||
| aOR | CIs | p | aOR | CIs | p | aOR | CIs | p | ||
| Interv | 1.221 | (0.571–2.638) | 0.604 | 0.896 | (0.415–1.896) | 0.771 | 0.651 | (0.353–1.174) | 0.152 | |
| Time | 0.763 | (0.670–0.869) | 0.000 | 0.726 | (0.600–0.844) | 0.000 | 0.733 | (0.644–0.827) | 0.000 | |
| Time*Interv | 0.741 | (0.560–0.951) | 0.019 | 1.073 | (0.869–1.336) | 0.499 | 1.116 | (0.951–1.31) | 0.159 | |
Interv = Intervention arm; aOR = Adjusted Odds-Ratio; CI = confidence interval; p = p-value; Analysis was adjusted for age, study site, education, age started sex work, years of sex work, marital status, prior incarceration/detention/arrest, recent substance use
Discussion
The current RCT contributes to building a rigorous evidence base for interventions targeting co-occurring issues of HIV and IPV among WESUD, who are at a heightened risk for both [4]. Findings show that adding asset-based microfinance components to a traditional HIVRR intervention demonstrates a significant and increased reduction in sexual violence from paying partners and physical violence from past intimate partners among WESUD over 12 months. Additionally, we did not see a significant increase in reported violence associated with the HIVRR + MF intervention, a concern related to the mixed findings of prior economic empowerment studies among financially vulnerable women [23, 31].
Results from this study were consistent with other savings-led interventions, finding positive effects in financial (e.g., savings accumulation and income), gender (e.g., women’s empowerment), and health (e.g., maternal and infant health) outcomes compared to other forms of microfinance programs [32]. There are several possible explanations for why the combination microfinance intervention yielded these findings. One reason may have been the opportunity to integrate violence risk reduction activities into goal-setting and to have a longer time frame - throughout the many weeks of additional participation in FL and VT -during which participants were building self-efficacy related to violence reduction. Women assigned to HIVRR + MF received an intervention sustained over more time, during which staff offered a safety check-in and support, including safety planning. Social cognitive theory suggests that integrating knowledge and skills over time using goal-setting and generalization of learning outside of interventive sessions to one’s real life strengthens the capacity to engage skills with sustained efficacy.
Adding financial literacy training and vocational training sessions may have offered women increased capacity for engaging in alternative forms of income, which may have reduced their exposure to clients due to reduced sex work. As women gained knowledge and skills in managing finances and learning vocational options for income, they were also engaged in savings behavior reinforced by a matched savings program, which may have built self-efficacy for savings. This economic empowerment may have made some women less tolerant of violence exposure. While some prior studies found increases in violence related to economic empowerment, this was among current intimate partners and not paying partners [31]. Had the study been conceptualized as an equivalence trial, comparing HIVRR to the combination HIVRR + MF to test whether economic empowerment increased violence reported by women, the steady decrease across groups may have signaled success in not increasing violence exposure. We recognize that findings related to past partners may either demonstrate the robust capacity for the intervention to reduce violence among former partners or a simple artifact of reduced proximity and exposure to that person as a former partner. However, randomization should account for reduced exposure across both intervention conditions.
In a mixed method review of cash transfers and IPV among women in LMICs, Buller et al. (2018) describe three pathways through which financial assets may impact IPV: (1) economic security and emotional well-being, (2) intrahousehold conflict, and (3) women’s empowerment. Their analysis does not consider the unique circumstances of WESUD, but these pathways may account for some of the findings in this study. Our interventions may have served to strengthen economic security and emotional well-being among participants, as well as to enhance empowerment through building self-efficacy and financial assets and strengthening the choice to reduce reliance on sex work for income. The question of intrahousehold conflict would only be relevant for those women reporting a main partner. We saw no changes within that group [33].
Prior work among WESW in Mongolia did not find that participation in an asset-based MF intervention influenced experiences of client violence among WESW over those in the control condition [26]. However, as with this study, it did show that women in both groups showed trends in violence reduction over time. We believe this may be related to the assets gained by group-based and social support built as a participant in a collective intervention. Peer networks have shown to be an essential source of emotional support and physical survival for women who exchange sex [34]. Since the exchange of sex for money is highly stigmatized in Kazakhstan, as in Mongolia, women engaged in sex work do not trust law enforcement to seek safety or justice. In addition, women exchanging sex feel isolated and too ashamed to tell others about their work [35]. Therefore, individual protection from violence is left to women who exchange sex and their clients. Hence, we speculate that the group format of each treatment arm may have strengthened the women’s peer networks, increasing their protection and safety around their commercial sexual activity and at other times. In addition, peer networks may have connected the women with other community resources to help prevent violence [18].
The sample of women in the current study differs in that they also use drugs, which may mean higher exposure to violence; hence more or greater violence reduction was possible over the follow-up period [15].
Findings strengthen the evidence that activities targeting violence reduction, sustained through, or combined with microfinance components, including FLT, vocational training, and matched savings, can be achieved in HIV prevention. However, these findings are only at the individual level, reflecting individual-level and interpersonal knowledge and skills acquisition. Violence against women is also a function of patriarchal cultural values deeply embedded in social structures that have yet to change.
This study has limited the generalizability of findings to other WESW populations, given that we used a convenience sample of women who used drugs recruited from specific venues and through peer networks in two cities in Kazakhstan. Self-reported outcome data opens the possibility of participant response bias, including social pressures to under-report experiences of violence. Computer-assisted self-interviewing mitigated this risk, as participants could provide their responses privately.
Conclusions
Findings show that a combination HIVRR and microfinance intervention reduces sexual violence from paying partners and physical violence from past intimate partners among WESW who use drugs compared to the HIVRR intervention. Given the strong evidence indicating that violence impedes women’s capacity and ability to engage in HIV prevention effectively, future research should replicate these findings in other regions while also examining the causal pathways through which components or mechanisms of microfinance may be associated with such reductions.
Acknowledgements
We thank our research assistants and intervention facilitators, as well as all the participants who gave their time to our study. We also thank our partners at the NGOs “Moi Dom” and “Doverie” for their support and cooperation.
Funding
This study was funded by the National Institute on Drug Abuse (NIDA) to Drs. Witte and El Bassel (R01DA036514). The funder was not involved in study design or analysis. Additionally, Trena I. Mukherjee is supported by the National Institute of Allergy and Infectious Diseases (T32AI114398); and Tara McCrimmon is supported by the National Institute on Drug Abuse (T32DA037801).
Footnotes
Competing interests The authors declare that they have no competing interests.
References
- 1.Organization WH. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. World Health Organization; 2013. [Google Scholar]
- 2.Deering KN, Amin A, Shoveller J, Nesbitt A, Garcia-Moreno C, Duff P, Argento E, Shannon K. A systematic review of the correlates of violence against sex workers. Am J Public Health. 2014;104:e42–e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Decker MR, Pearson E, Illangasekare SL, Clark E, Sherman SG. Violence against women in sex work and HIV risk implications differ qualitatively by perpetrator. BMC Public Health. 2013;13:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El-Bassel N, Mukherjee TI, Stoicescu C, Starbird LE, Stockman JK, Frye V, Gilbert L. Intertwined epidemics: progress, gaps, and opportunities to address intimate partner violence and HIV among key populations of women. The Lancet HIV 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leddy AM, Weiss E, Yam E, Pulerwitz J. Gender-based violence and engagement in biomedical HIV prevention, care and treatment: a scoping review. BMC Public Health. 2019;19:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeHovitz J, Uuskula A, El-Bassel N. The HIV epidemic in eastern Europe and central Asia. Curr HIV/AIDS Rep. 2014;11:168–76. [DOI] [PubMed] [Google Scholar]
- 7.Jiwatram-Negrón T, Michalopoulos LM, El-Bassel N. The syndemic effect of injection drug use, intimate partner violence, and HIV on mental health among drug-involved women in Kazakhstan. Global social welfare. 2018;5:71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Decker MR, Wirtz AL, Moguilnyi V, Peryshkina A, Ostrovskaya M, Nikita M, Kuznetzova J, Beyrer C. Female sex workers in three cities in Russia: HIV prevalence, risk factors and experience with targeted HIV prevention. AIDS Behav. 2014;18:562–72. [DOI] [PubMed] [Google Scholar]
- 9.Lang DL, Salazar LF, DiClemente RJ, Markosyan K. Gender based violence as a risk factor for HIV-associated risk behaviors among female sex workers in Armenia. AIDS Behav. 2013;17:551–8. [DOI] [PubMed] [Google Scholar]
- 10.Lyons CE, Grosso A, Drame FM, Ketende S, Diouf D, Ba I, Shannon K, Ezouatchi R, Bamba A, Kouame A. Physical and sexual violence affecting female sex workers in Abidjan, Côte d’Ivoire: prevalence, and the relationship with the work environment, HIV and access to health services. J Acquir Immune Defic Syndr. 2017;75:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shannon K, Crago A-L, Baral SD, Bekker L-G, Kerrigan D, Decker MR, Poteat T, Wirtz AL, Weir B, Boily M-C. The global response and unmet actions for HIV and sex workers. The Lancet. 2018;392:698–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swann M Economic strengthening for HIV prevention and risk reduction: a review of the evidence. AIDS Care. 2018;30:37–84. [DOI] [PubMed] [Google Scholar]
- 13.Dworkin SL, Blankenship K. Microfinance and HIV/AIDS prevention: assessing its promise and limitations. AIDS Behav. 2009;13:462–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reed LR, Marsden J, Ortega A, Rivera C, Rogers S. State of the microcredit summit campaign report 2011. Microcredit Summit Campaign Washington DC: 2011. [Google Scholar]
- 15.Decker MR, Lyons C, Guan K, Mosenge V, Fouda G, Levitt D, Abelson A, Nunez GT, Njindam IM, Kurani S. A systematic review of gender-based violence prevention and response interventions for HIV key populations: female sex workers, men who have sex with men, and people who inject drugs. Trauma Violence & Abuse. 2022;23:676–94. [DOI] [PubMed] [Google Scholar]
- 16.Blanchard AK, Nair SG, Bruce SG, Ramanaik S, Thalinja R, Murthy S, Javalkar P, Pillai P, Collumbien M, Heise L. A community-based qualitative study on the experience and understandings of intimate partner violence and HIV vulnerability from the perspectives of female sex workers and male intimate partners in North Karnataka state, India. BMC women’s health. 2018;18:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Javalkar P, Platt L, Prakash R, Beattie T, Bhattacharjee P, Thalinja R, Sangha CATM, Ramanaik S, Collumbien M, Davey C. What determines violence among female sex workers in an intimate partner relationship? Findings from North Karnataka, south India. BMC Public Health. 2019;19:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carlson CE, Chen J, Chang M, Batsukh A, Toivgoo A, Riedel M, Witte SS. Reducing intimate and paying partner violence against women who exchange sex in Mongolia: results from a randomized clinical trial. J interpers Violence. 2012;27:1911–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gibbs A, Jacobson J, Kerr Wilson A. A global comprehensive review of economic interventions to prevent intimate partner violence and HIV risk behaviours. Global health action. 2017;10:1290427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gupta J, Falb KL, Lehmann H, Kpebo D, Xuan Z, Hossain M, Zimmerman C, Watts C, Annan J. Gender norms and economic empowerment intervention to reduce intimate partner violence against women in rural Côte d’Ivoire: a randomized controlled pilot study. BMC Int health Hum rights. 2013;13:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pronyk PM, Hargreaves JR, Kim JC, Morison LA, Phetla G, Watts C, Busza J, Porter JD. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. The lancet. 2006;368:1973–83. [DOI] [PubMed] [Google Scholar]
- 22.Glass N, Perrin NA, Kohli A, Campbell J, Remy MM. Randomised controlled trial of a livestock productive asset transfer programme to improve economic and health outcomes and reduce intimate partner violence in a postconflict setting. BMJ Global Health. 2017;2:e000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murshid NS, Akincigil A, Zippay A. Microfinance participation and domestic violence in Bangladesh: results from a nationally representative survey. J interpers Violence. 2016;31:1579–96. [DOI] [PubMed] [Google Scholar]
- 24.Peterman A, Palermo TM, Ferrari G. Still a leap of faith: microfinance initiatives for reduction of violence against women and children in low-income and middle-income countries. BMJ global health 2018, 3, e001143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Witte SS, Aira T, Tsai LC, Riedel M, Offringa R, Chang M, El-Bassel N, Ssewamala F. Efficacy of a savings-led microfinance intervention to reduce sexual risk for HIV among women engaged in sex work: a randomized clinical trial. Am J Public Health. 2015;105:e95–e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tsai LC, Carlson CE, Aira T, Norcini Pala A, Riedel M, Witte SS. The impact of a microsavings intervention on reducing violence against women engaged in sex work: a randomized controlled study. BMC Int health Hum rights. 2016;16:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.El-Bassel N, McCrimmon T, Mergenova G, Chang M, Terlikbayeva A, Primbetova S, Kuskulov A, Baiserkin B, Denebayeva A, Kurmetova K. A cluster‐randomized controlled trial of a combination HIV risk reduction and microfinance intervention for female sex workers who use drugs in Kazakhstan. J Int AIDS Soc. 2021;24:e25682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCrimmon T, Witte S, Mergenova G, Terlikbayeva A, Primbetova S, Kuskulov A, Bellamy SL. El-Bassel N. Microfinance for women at high risk for HIV in Kazakhstan: study protocol for a cluster-randomized controlled trial. Trials. 2018;19:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. J Fam Issues. 1996;17:283–316. [Google Scholar]
- 30.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015. [Google Scholar]
- 31.Matjasko JL, D’Inverno AS, Marshall KJ, Kearns MC. Microfinance and violence prevention: a review of the evidence and adaptations for implementation in the US. Prev Med. 2020;133:106017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duvendack M, Mader P. Impact of financial inclusion in low-and middle‐income countries: a systematic review of reviews. J Economic Surveys. 2020;34:594–629. [Google Scholar]
- 33.Buller AM, Peterman A, Ranganathan M, Bleile A, Hidrobo M, Heise L. A mixed-method review of cash transfers and intimate partner violence in low-and middle-income countries. World Bank Res Obs. 2018;33:218–58. [Google Scholar]
- 34.Rodríguez DC, Krishnan A, Kumarasamy N, Krishnan G, Solomon D, Johnson S, Vasudevan C, Solomon R, Ekstrand ML. Two sides of the same story: alcohol use and HIV risk taking in South India. AIDS Behav. 2010;14:136–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Witte SS, Batsukh A, Chang M. Sexual risk behaviors, alcohol abuse, and intimate partner violence among sex workers in Mongolia: implications for HIV prevention intervention development. J Prev Interv Community. 2010;38:89–103. [DOI] [PMC free article] [PubMed] [Google Scholar]


