Abstract
BACKGROUND
Radicular pain after lumbar decompression surgery can result from epidural hematoma/seroma, recurrent disc herniation, incomplete decompression, or other rare complications. A less recognized complication is postoperative nerve root herniation, resulting from an initially unrecognized intraoperative or, more commonly, a spontaneous postoperative durotomy. Rarely, this nerve root herniation can become entrapped within local structures, including the facet joint. The aim of this study was to illustrate our experience with three cases of lumbosacral nerve root eventration into an adjacent facet joint and to describe our diagnostic and surgical approach to this rare complication.
OBSERVATIONS
Three patients who had undergone lumbar decompression surgery with or without fusion experienced postoperative radiculopathy. Exploratory revision surgery revealed all three had a durotomy with nerve root eventration into the facet joint. Significant symptom improvement was achieved in all patients following liberation of the neural elements from the facet joints.
LESSONS
Entrapment of herniated nerve roots into the facet joint may be a previously underappreciated complication and remains quite challenging to diagnose even with the highest-quality advanced imaging. Thus, clinicians must have a high index of suspicion to diagnose this issue and a low threshold for surgical exploration.
Keywords: nerve root herniation, dural tear, incidental durotomy, facet joint, FIESTA MRI, fast imaging employing steady-state acquisition
ABBREVIATIONS: CSF = cerebrospinal fluid, CT = computed tomography, FIESTA = fast imaging employing steady-state acquisition, MRI = magnetic resonance imaging, TE = echo time, TR = repetition time
The presence of radicular pain after lumbar decompression surgery can be attributed to various factors. Notable findings on postoperative imaging in symptomatic patients include epidural hematoma/seroma, recurrent disc herniation, or incomplete initial decompression.1 Another postoperative complication potentially contributing to a similar patient presentation is incidental durotomy, that is, occurring either spontaneously in the postoperative period or in an unrecognized manner at the index surgery.2 And while most incidental durotomies remain asymptomatic or present as a pseudomeningocele,3 a subsequent complication is nerve root entrapment, occurring by way of this durotomy.2 Once herniated through the dural defect, the neural elements can become entrapped, either strangulated by the dura or physically trapped within one of a few surrounding anatomical structures, such as the facet joint1 or the intervertebral disc.4 With this condition, patients will typically experience an initial period of pain relief postoperatively, followed by the acute onset of severe radicular pain into a unilateral lower extremity.5
Postoperative nerve root herniation is a rare condition and thus has been overlooked, as it remains quite challenging to diagnose even with the most sophisticated of advanced imaging techniques. The purpose of this study was to review the literature and illustrate the clinical course and surgical management of three patients with herniated nerve roots that subsequently eventrated into an adjacent lumbar facet joint. We also aimed to share our experience with the three-dimensional fast imaging employing steady-state acquisition (FIESTA) magnetic resonance imaging (MRI) to assist in the preoperative diagnosis of this condition.6
Illustrative Cases
Between April 2022 and October 2023, two surgeons at one academic medical center conducted lumbar spine surgeries in three different patients, all of whom subsequently developed early postoperative radicular pain. After the completion of advanced imaging, concern for spontaneous postoperative durotomy with nerve root herniation and eventration into the adjacent facet joint prompted returns to the operating room for exploration and, in all three cases, a reduction of the nerve root herniation and dural repair. In two of the three cases, fusion of the index operative segment was ultimately performed in the setting of wide facetectomy on revision decompression, as there was concern for postoperative segmental instability without fusion.
Case 1
Clinical Presentation, Imaging, and Primary Surgery
A 70-year-old male presented for surgical consultation with symptoms and examination findings suggesting neurogenic claudication. Preoperative imaging revealed a mild degenerative spondylolisthesis at L3–S1 without dynamic instability, along with severe lumbar spinal stenosis (Fig. 1A). After insufficient improvement with nonsurgical treatments, the patient underwent microsurgical decompressive laminectomy with bilateral medial facetectomies at L3–S1. Intraoperatively, satisfactory decompression of the neural elements was achieved, and at the end of the case, a Valsalva maneuver revealed no cerebrospinal fluid (CSF) leakage.
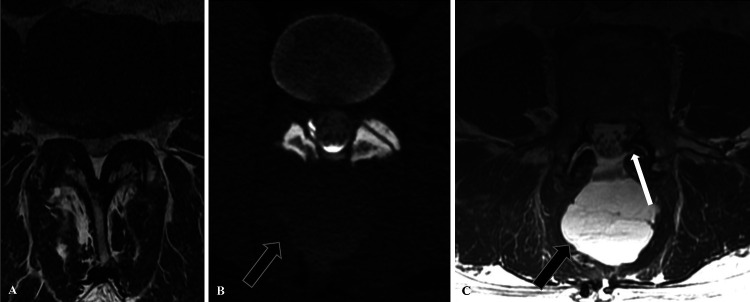
FIG. 1.
Case 1. A: Preoperative axial MRI at the L3–4 level demonstrated severe central and bilateral lateral recess stenosis. B: Postoperative CT myelogram with evidence of epidural contrast leakage into a large dorsal paraspinous fluid collection (arrow), suspicious for CSF leakage. C: Postoperative T2 FIESTA MRI highlights thickening and displacement of the lumbosacral nerve roots within the diastatic left L3–4 facet joint (white arrow), along with a large subfascial fluid collection (black arrow).
Initial Postoperative Course
The patient did very well immediately after surgery and was discharged home on postoperative day 2. He experienced complete resolution of his preoperative leg pain for almost 3 weeks, until postoperative day 20, when he spontaneously developed mild headaches, worsening back pain, and new-onset left lower-extremity radicular pain with any movement of the leg. On examination, he maintained full strength in all major myotomes and normal sensation, albeit with evidence of tension signs in the left lower extremity (positive straight leg raise and contralateral straight leg raise).
Postoperative Imaging
In the setting of postoperative spontaneous headache, a computed tomography (CT) myelogram demonstrated extradural contrast leakage into a large dorsal paraspinous fluid collection, suspicious for CSF leakage (Fig. 1B). MRI was subsequently performed, which redemonstrated a large dorsal fluid collection and also demonstrated diastasis of the L3–4 facet joints bilaterally, with concern for eventration of the neural elements into the left L3–4 facet joint (Fig. 1C). Notably, this MRI was obtained with the FIESTA sequence, which offers submillimeter spatial resolution and a high CSF to soft tissue contrast.7 The specific parameters for the FIESTA sequence are as follows: slice thickness, 1 mm; field of view, 160 mm; repetition time (TR), 5 msec; echo time (TE), 2.4 msec; matrix, 320 × 256; and flip angle, 35°.7
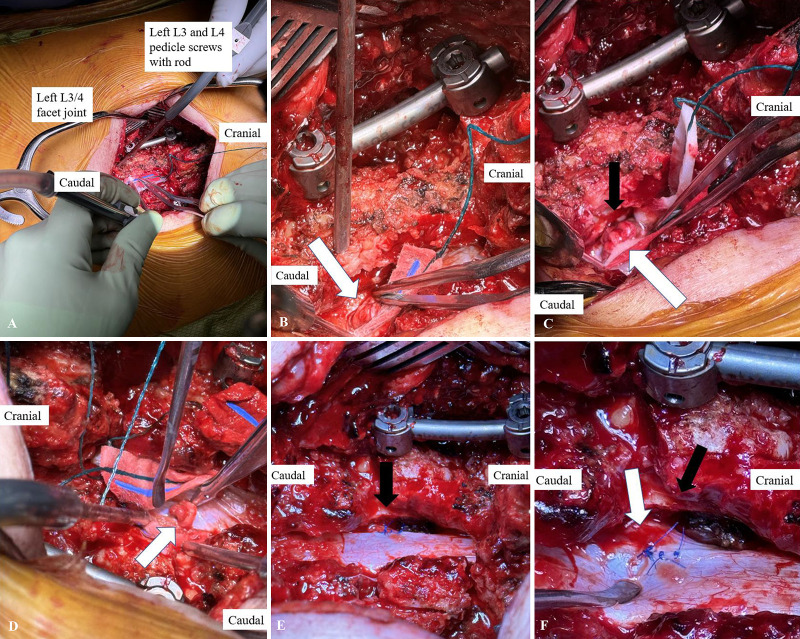
Revision Surgery
The patient returned to the operating room 21 days after his index operation. The surgical incision was reincised, and a subfascial hematoma/seroma was immediately encountered. Upon exposing the thecal sac, no frank CSF leakage, durotomy, or nerve root herniation was immediately identifiable (Fig. 2A). With gentle manipulation of the thecal sac, a durotomy with active CSF leakage became evident, and although the left L4 nerve root herniation was not initially visible, it became evident that, consistent with the postoperative MRI, the neural elements were entrapped within the L3–4 facet joint. It was determined that distraction of the left L3–4 facet joint would be required for safe retrieval of the left L4 nerve root. Pedicle screws were placed into the L3 and L4 pedicles bilaterally, and on the left side, a temporary rod was placed. Upon initiation of rod distraction, the herniated left L4 nerve root immediately became visible, having been successfully freed from the facet joint (Fig. 2B). Careful inspection of the herniated root highlighted its proximity to the ipsilateral L3–4 facet joint line (Fig. 2C). Although the nerve root exhibited swelling and erythema, it remained intact (Fig. 2D). The nerve root was subsequently neurolysed and carefully reduced back into the thecal sac through the durotomy. Subsequent primary repair of the dura was performed with four simple Prolene sutures (Fig. 2E). The primary repair was supplemented with the placement of fibrin glue. Of note, a wide medial facetectomy was required for access for the dural repair and to ensure adequate decompression of the nerve root (Fig. 2F).
FIG. 2.
Case 1. A: The thecal sac has been exposed. Note that the left L4 nerve root herniation is not immediately visible, because it remains entrapped in the L3–4 facet joint. On the patient’s left side, pedicle screws have been placed at L3 and L4, accompanied by a rod. B: After rod distraction, the left L4 nerve root herniation (arrow) is now visible and can be retrieved from the left L3–4 facet joint. C: Note the proximity of the herniated left L4 nerve root (white arrow) to the left L3–4 facet joint line (black arrow). D: Viewed from the patient’s left, one can appreciate the herniated left L4 nerve root (arrow), with a swollen and erythematous appearance. Also in this image are the right L3 and L4 pedicle screws, without a rod connecting at this point in the procedure, because no distraction was necessary on this side. E: View from the patient’s right after the left L4 nerve root has been reduced into the thecal sac and the durotomy repaired. Note the proximity of the left L4 nerve root shoulder (black arrow) to the left L3–4 facet joint in which it was previously entrapped. F: Note the dural repair at the medial-most aspect of the nerve root shoulder (white arrow) and the wide medial facetectomy performed to access the dura for repair and ensure adequate decompression of the neural elements.
Final Postoperative Course
After the repeat surgical intervention, the patient experienced an immediate, complete resolution of his left lower-extremity radicular symptoms, and his tension signs resolved. A subfascial surgical drain was placed to gravity and removed on postoperative day 2 without complication. The head of his bed remained flat until postoperative day 1 when bedrest restrictions were lifted. His subsequent clinical trajectory remained uneventful.
Case 2
Clinical Presentation, Imaging, and Primary Surgery
A 69-year-old male presented for surgical consultation with symptoms and examination findings suggesting neurogenic claudication. Preoperative imaging revealed severe spinal stenosis at the L4–5 level (Fig. 3A). After insufficient improvement with nonsurgical treatments, the patient underwent a minimally invasive (tubular) L4–5 decompression via a left-sided laminotomy, with an over-the-top decompression of the right side. Intraoperatively, satisfactory decompression of the neural elements was achieved, and at the end of the case, a Valsalva maneuver revealed no CSF leakage.
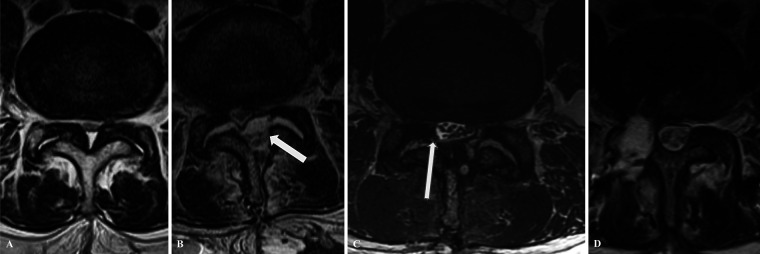
FIG. 3.
Case 2. A: Preoperative axial MRI at the L4–5 level showing severe central and lateral recess stenosis. B: Postoperative axial T2-weighted MRI demonstrates an over-the-top decompression extending from the left hemilamina to the right lateral recess, with a compressive fluid collection (arrow). C: MRI with the T2 FIESTA sequence highlights the right-sided lumbosacral nerve rootlets entrapped in the diastatic right L4–5 facet joint (arrow). D: Six-month postoperative axial T2-weightde MRI demonstrates dural repair with evidence of the maintained reduction of the previously herniated nerve roots. Also evident is a complete right-sided facetectomy.
Initial Postoperative Course
On the first postoperative day, the patient developed radiating left lower-extremity pain, which intensified during the following 2 days to the point where he was bedridden and unable to perform activities of daily living. MRI was performed on postoperative day 3 and demonstrated a postoperative epidural fluid collection largely on the patient’s left side (Fig. 3B).
Initial Revision Surgery
The patient returned to the operating room for exploration and evacuation of the compressive fluid collection. Intraoperatively, seromatous fluid within the laminotomy space was identified. The fluid was evacuated and the thecal sac reexpanded. There was no evidence of a durotomy of CSF leakage after irrigation; thus, the procedure was completed in a standard fashion.
Subsequent Postoperative Course
In the days after the initial revision surgery, the patient experienced new-onset, right greater than left, lower-extremity radicular pain. He exhibited progressively worsening tension signs, and any motion of the spine or right lower extremity severely exacerbated his right lower-extremity radicular pain.
Subsequent Postoperative Imaging
Repeat MRI was performed, which demonstrated a significant reduction in the size of the previous left-sided postoperative fluid collection but persistent diastasis of the bilateral L4–5 facet joints. Although difficult to definitively appreciate on the available imaging studies, there was concern for eventration of the right-sided lumbosacral nerve rootlets into the right L4–5 facet joint (Fig. 3C, Video 1). Thus, surgical exploration was recommended.
VIDEO 1. Case 2. Clip showing MRI with the T2 FIESTA sequence, which highlights the right-sided lumbosacral nerve rootlets entrapped in the diastatic right L4–5 facet joint (arrow). Click here to view.
Second Revision Surgery
Now 7 days after the index operation, the patient again returned to the operating room for repeat exploration, which revealed a durotomy at the L4–5 level on the right, with nerve root herniation through the dural defect and incarceration of the lumbosacral nerve rootlets within the L4–5 facet joint. Freeing the incarcerated nerve rootlets required a complete right-sided L4–5 facetectomy, ultimately leading to the decision to fuse the segment. After freeing the nerve roots, they were carefully reduced into the thecal sac, and a primary dural repair requiring only one suture along with an autologous muscle patch ensued.
Final Postoperative Course
Postoperatively, the patient did have residual right lateral leg pain; however, his strength was full, and his sensation was intact. A subfascial surgical drain was placed to gravity and removed on postoperative day 2 without complication. The head of his bed remained flat until postoperative day 1 when bedrest restrictions were lifted. By 4 weeks postoperatively, he had complete resolution of his right lower-extremity radicular pain, albeit with residual left-sided axial low-back pain. Repeat MRI at 6 months postoperatively was performed in the setting of this persistent axial low-back pain, which provided evidence of dural repair with reduction of the previously herniated nerve rootlets (Fig. 3D).
Case 3
Clinical Presentation, Imaging, and Primary Surgery
A 65-year-old male presented for surgical consultation with symptoms and examination findings suggesting neurogenic claudication. His preoperative imaging revealed severe spinal stenosis spanning L3–5 (Fig. 4A). After insufficient improvement with nonsurgical treatments, the patient underwent a minimally invasive (tubular) L3–4 decompression via a left-sided laminotomy, with an over-the-top decompression of the right side. At the L4–5 level, a grade I anterolisthesis was present; thus, at this level he underwent decompression via a similar approach, along with percutaneous posterior fusion. Intraoperatively, satisfactory decompression of the neural elements was achieved, and at the end of the case, a Valsalva maneuver revealed no CSF leakage.
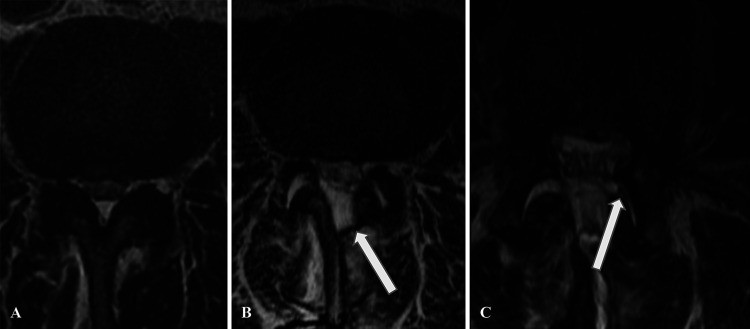
FIG. 4.
Case 3. A: Preoperative axial MRI at the L3–4 level demonstrates severe central and bilateral lateral recess stenosis. B: Postoperative MRI demonstrates a postoperative fluid collection (arrow) at the surgical site, along with diastasis of the bilateral L3–4 facet joints. C: Axial T2-weighted MRI after the evacuation surgery demonstrates eventration of the thecal sac contents into the left L3–4 facet joint (arrow).
Initial Postoperative Course
The initial postoperative period was uneventful. At 3 weeks postoperatively, he experienced the acute onset of severe left lower-extremity radicular pain into the thigh and lateral calf, rendering him reliant on a walker for ambulation. MRI demonstrated a left-sided epidural fluid collection (Fig. 4B).
Initial Revision Surgery
The patient returned to the operating room for exploration and evacuation of the compressive fluid collection. Intraoperatively, seromatous fluid within the laminotomy space was identified. The fluid was evacuated and the thecal sac reexpanded.
Subsequent Postoperative Course
Postevacuation, the patient’s left leg pain persisted, inhibiting any meaningful ambulation. Postoperative MRI with supplemental FIESTA sequences for improved spatial resolution, conducted on the first postoperative day after the evacuation surgery, now demonstrated concern for possible eventration of the lumbosacral nerve rootlets into the left L3–4 facet joint (Fig. 4C). Thus, with the lack of clinical improvement and these concerning findings on advanced imaging, repeat surgical exploration was recommended.
Second Revision Surgery
The patient returned to the operating room for a second time, and the wound was reexplored. A spontaneous durotomy at the L3–4 level on the left, with eventration of the lumbosacral nerve rootlets into the facet joint, was encountered. Extraction of the neural elements without the need for facet joint resection, followed by reduction into the thecal sac and dural repair with 5 independent sutures and an autologous muscle patch ensued. The primary dural repair was supplemented with fibrin glue.
Final Postoperative Course
Postoperatively, the patient had complete resolution of his left lower-extremity radicular pain, but he did note a persistent, dense sensory deficit in the left lateral leg. His strength remained full. A subfascial surgical drain was placed to gravity and removed on postoperative day two without complication. The head of his bed remained flat until postoperative day 1 when bedrest restrictions were lifted. For his persistent sensory deficit, he was initially treated with gabapentin. As the sensory deficit evolved, the region of paresthesia remained, albeit without any associated pain; thus, the gabapentin was eventually weaned entirely.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Incidental durotomy after spine surgery has been described in great detail.2 However, this clinical condition has a wide range of presentations, from being an asymptomatic radiological finding to precipitating symptomatic nerve root herniation and entrapment. This three-patient case series represents the first of its kind, with clinical, radiological, and confirmatory surgical evidence of postoperative nerve root herniation into the facet joint after an index lumbar decompression. Additionally, this case series marks the first report utilizing the FIESTA MRI sequence to enhance the sensitivity for detecting this rare complication.
Although postoperative nerve root herniation with entrapment remains a relatively infrequent complication after lumbar spine surgery, its presence has been reported and may become more frequently encountered, especially with the growing popularity of minimally invasive surgeries with smaller incisions, less muscle dissection, and questionably limited visualization.1,8,9 And although the majority of these complications have been described after decompression-type surgeries, an interesting case of nerve root incarceration after epidural block has also been recently reported.10 Whereas reports of these complications remain rare, it is prudent to diagnose them effectively and efficiently, because treatment of this mechanical entrapment is primarily surgical, and misdiagnosis could contribute to prolonged, suboptimal treatment.11
The first documented case of eventration of the nerve root into the adjacent facet joint dates from 1995, when an S1 nerve root herniated into the facet joint after a hemilaminectomy.12 At this time in medical history, no MRI was performed; thus, the diagnosis was confirmed only at the time of surgical exploration. A subsequent case report details a postoperative nerve root herniation into the adjacent facet joint after microsurgical decompression.1 Notably, because this case was described within the past few years, postoperative MRI demonstrated a facet joint effusion, with the herniated nerve root visible within this facet joint gap.1
Observations
In all three cases described, clinical evaluation (history and physical examination) proved paramount in diagnosing the lumbosacral nerve root herniation and facet joint entrapment. Although some postoperative conditions can be treated with a conservative watch-and-wait approach, physical entrapment of the neural elements needs freeing via surgical intervention, which likely requires revision decompression and possibly fusion. Although not clearly diagnostic, advanced techniques on postoperative MRI imaging (FIESTA sequence) read by an experienced, trained radiologist and/or surgeon can supplement the clinical suspicion with radiological data to suggest this rare diagnosis.
Although we aim to provide recommendations to improve diagnostic capabilities for this rare postoperative condition, it remains a challenging diagnosis and can be missed if not carefully considered. For instance, looking critically at cases 2 and 3, it is certainly possible that subtle dural defects (injuries to the dura with preservation of the arachnoid layer and thus with no gross detection of CSF or dural blebs) may have been missed at the index procedure or indeed the first exploratory revision surgery. Notably, in all cases, the surgical site was thoroughly explored, and although no dural defects were encountered, when considering that these cases were both completed in a minimally invasive fashion via tubular decompression, it remains possible that a durotomy may have been missed because of limitations in the field of view. That said, careful review of all postoperative MRI studies did not suggest any evidence of CSF leakage, nerve root herniation, or facet joint eventration, and both cases were more consistent with neurological compression from epidural fluid collections (although, notably, FIESTA MRI sequences were not obtained). Another important point to consider is that in all three cases, at the time that the dural defect was ultimately identified intraoperatively, the dural defect was plugged with the herniated nerve root, and only after reduction of the nerve root into the thecal sac was a gush of CSF noted. This, too, could potentially contribute to missed diagnoses even with careful inspection. Interestingly, in contrast, case 1 was completed from the index surgery in an open fashion, and the dural defect was discovered swiftly and addressed definitively on the first exploratory surgery. Clearly, this underscores the importance of thoroughly inspecting the surgical site for possible dural defects at the conclusion of all decompression operations and of always ensuring proper visualization of the surgical field.
Alternatively, rather than being missed by the operating surgeon, it was surmised in cases 2 and 3 that the inflammatory response of two surgical insults over a short time period contributed to inflammation of the thecal sac, and that ultimately via a residual bony spike or simply by means of continued motion through the partially resected facet joint (after a partial medial facetectomy), the inflamed, traumatized thecal sac was abraded and an incidental durotomy was created.
Lessons
When patients exhibit a sudden postoperative resurgence of unyielding radiating pain and postoperative MRI reveals the absence of another clear etiology, nerve root herniation should be considered as a potential diagnosis. The advanced, thin-cut FIESTA MRI sequence can provide supportive radiological data to help visualize root entrapment within the facet joint, which may prompt urgent exploratory revision surgery. Although routine spinal MRI studies are often limited by low spatial resolution as a result of CSF pulsation, balanced steady-state sequences (e.g., FIESTA) eliminate this pulsation artifact, allowing for a clearer image.7 The improved spatial resolution provides exquisite anatomical detail, even helping to delineate postoperative hematoma/seroma from CSF leakage, assisting in making a clear diagnosis.7 We suggest, if possible, using this MRI sequence when this complication remains on the differential.
Limitations of this study are inherent to the rarity of the investigated condition. The complication of postoperative nerve root herniation and entrapment in the adjacent facet joint has previously been reported only twice, in two separate case reports.1,12 Another limitation of this study is the generalizability of the lessons, as the FIESTA MRI sequence must be suggested at the time that the MRI scan is first obtained; that is, this must be considered, requested, and obtained if this diagnosis is considered. Although this sequence is not routinely obtained, we have worked at our home institution to add this sequence to the protocol for postoperative radiculopathy because of its clear advantages in providing clear images. Finally, at our institution, our radiologists have completed advanced training in musculoskeletal radiology or neuroradiology, which may not always be the case in all medical practices.
In conclusion, persistent, severe postoperative radicular pain should prompt further diagnostic evaluation, and the diagnosis of lumbosacral nerve root herniation with entrapment must always be considered. Using the FIESTA MRI sequence to enhance image quality has been shown to be effective in our series in improving diagnostic sensitivity in such cases. Prompt recognition of this rare postoperative condition is important, because this allows for appropriate surgical exploration, freeing of the entrapped neural elements, and symptomatic relief for the patient.
Author Contributions
Conception and design: Kelly, Altorfer, Burkhard, Huang, Chazen. Acquisition of data: Kelly, Chazen. Analysis and interpretation of data: Kelly, Burkhard, Cammisa, Chazen. Drafting the article: Kelly, Altorfer, Burkhard, Cammisa. Critically revising the article: all authors. Reviewed submitted version of manuscript: Kelly, Altorfer, Huang, Cammisa, Chazen. Approved the final version of the manuscript on behalf of all authors: Kelly. Statistical analysis: Kelly. Administrative/technical/material support: Kelly, Altorfer. Study supervision: Kelly, Burkhard, Chazen.
Supplemental Information
Videos
Video 1. https://vimeo.com/921152107.
References
- 1. Popadic B, Scheichel F, Themesl M, Decristoforo I, Sherif C, Marhold F. Nerve root herniation with entrapment in the facet joint gap after lumbar decompression surgery: a case presentation. BMC Musculoskelet Disord. 2021;22(1):736. doi: 10.1186/s12891-021-04601-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cammisa FP, Jr, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine (Phila Pa 1976) 2000;25(20):2663–2667. doi: 10.1097/00007632-200010150-00019. [DOI] [PubMed] [Google Scholar]
- 3. Weng YJ, Cheng CC, Li YY, Huang TJ, Hsu RW. Management of giant pseudomeningoceles after spinal surgery. BMC Musculoskelet Disord. 2010;11(1):53. doi: 10.1186/1471-2474-11-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Choi JH, Kim JS, Jang JS, Lee DY. Transdural nerve rootlet entrapment in the intervertebral disc space through minimal dural tear: report of 4 cases. J Korean Neurosurg Soc. 2013;53(1):52–56. doi: 10.3340/jkns.2013.53.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bae JS, Pee YH, Jang JS, Lee SH. Clinical and radiological findings of nerve root herniation after discectomy of lumbar disc herniation. J Korean Neurosurg Soc. 2012;52(1):62–66. doi: 10.3340/jkns.2012.52.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nemoto O, Fujikawa A, Tachibana A. Diagnostic value of 3D fast imaging employing steady-state acquisition MR imaging for lumbar foraminal nerve root entrapment. Eur Orthop Traumatol. 2014;5(1):43–47. doi: 10.1007/s00590-013-1377-9. [DOI] [PubMed] [Google Scholar]
- 7. Li Z, Chen YA, Chow D, Talbott J, Glastonbury C, Shah V. Practical applications of CISS MRI in spine imaging. Eur J Radiol Open. 2019;6:231–242. doi: 10.1016/j.ejro.2019.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shu W, Wang H, Zhu H, et al. Nerve root entrapment with pseudomeningocele after percutaneous endoscopic lumbar discectomy: A case report. J Spinal Cord Med. 2020;43(4):552–555. doi: 10.1080/10790268.2018.1507802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kamali R, Naderi Beni Z, Naderi Beni A, Forouzandeh M. Postlaminectomy lumbar pseudomeningocele with nerve root entrapment: a case report with review of literature. Eur J Orthop Surg Traumatol. 2012;22(suppl 1):57–61. doi: 10.1007/s00590-011-0934-3. [DOI] [PubMed] [Google Scholar]
- 10. Lim DJ, Kim HT. Delayed cauda equina syndrome by nerve root incarceration after caudal epidural block: A case report. Int J Surg Case Rep. 2022;99:107662. doi: 10.1016/j.ijscr.2022.107662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stuebe CM, Soto JM, Vance AZ. Delayed symptomatic entrapment and herniation of lumbar nerve root due to a prior durotomy defect initially misdiagnosed as arachnoiditis: a case report. Cureus. 2022;14(8):e28588. doi: 10.7759/cureus.28588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nishi S, Hashimoto N, Takagi Y, Tsukahara T. Herniation and entrapment of a nerve root secondary to an unrepaired small dural laceration at lumbar hemilaminectomies. Spine (Phila Pa 1976) 1995;20(23):2576–2579. doi: 10.1097/00007632-199512000-00020. [DOI] [PubMed] [Google Scholar]