Abstract
Background
Cervical myelopathy (CM) causes several symptoms such as clumsiness of the hands and often requires surgery. Screening and early diagnosis of CM are important because some patients are unaware of their early symptoms and consult a surgeon only after their condition has become severe. The 10-second hand grip and release test is commonly used to check for the presence of CM. The test is simple but would be more useful for screening if it could objectively evaluate the changes in movement specific to CM. A previous study analyzed finger movements in the 10-second hand grip and release test using the Leap Motion, a noncontact sensor, and a system was developed that can diagnose CM with high sensitivity and specificity using machine learning. However, the previous study had limitations in that the system recorded few parameters and did not differentiate CM from other hand disorders.
Objective
This study aims to develop a system that can diagnose CM with higher sensitivity and specificity, and distinguish CM from carpal tunnel syndrome (CTS), a common hand disorder. We then validated the system with a modified Leap Motion that can record the joints of each finger.
Methods
In total, 31, 27, and 29 participants were recruited into the CM, CTS, and control groups, respectively. We developed a system using Leap Motion that recorded 229 parameters of finger movements while participants gripped and released their fingers as rapidly as possible. A support vector machine was used for machine learning to develop the binary classification model and calculated the sensitivity, specificity, and area under the curve (AUC). We developed two models, one to diagnose CM among the CM and control groups (CM/control model), and the other to diagnose CM among the CM and non-CM groups (CM/non-CM model).
Results
The CM/control model indexes were as follows: sensitivity 74.2%, specificity 89.7%, and AUC 0.82. The CM/non-CM model indexes were as follows: sensitivity 71%, specificity 72.87%, and AUC 0.74.
Conclusions
We developed a screening system capable of diagnosing CM with higher sensitivity and specificity. This system can differentiate patients with CM from patients with CTS as well as healthy patients and has the potential to screen for CM in a variety of patients.
Keywords: cervical myelopathy, myelopathy, spinal cord disease, spinal cord disorder, nervous system disorder, nervous system disease, clumsiness, screening, 10-second hand grip and release test, machine learning, carpal tunnel syndrome, Leap Motion, clinical informatics, system validation, screening system, sensor, model, diagnosis, diagnostic, high-dimensional analysis, motion sensor, motion detection, high-dimensional data analysis, high-dimensional statistics
Introduction
Cervical myelopathy (CM) occurs in patients with cervical spondylotic myelopathy, ossification of the posterior longitudinal ligament, or cervical disk herniation [1-3]. CM causes symptoms such as clumsiness of the hands, numbness of the extremities and trunk, and gait disturbance, and often requires surgery. The longer the duration and the more severe the disease, the worse the postoperative outcome [4-6]. However, some patients with CM are unaware of their early symptoms and consult a spine surgeon only after their condition has become severe [7]. Therefore, screening and early diagnosis of CM are important for symptom monitoring and to determine the optimum time for surgery [8].
Clumsiness of hands is a characteristic and important symptom of CM and is referred to as myelopathy hand [9]. The 10-second hand grip and release (10-s) test is commonly used to check for the presence of myelopathy hand [9,10]. In the 10-s test, patients repeatedly grip and release their hand as fast as possible for 10 seconds; if the number of repetitions is less than 20, a myelopathy hand is suspected. The 10-s test is simple but would be more useful for screening if it could objectively evaluate not only the number of repetitions but also the changes in movement specific to myelopathy hand.
Nowadays, the latest commercial sensors and devices using virtual reality have been developed and are being used in the medical field [11]. Some studies have reported using smartphones and stylus pens to analyze hand movements and diagnose diseases [12-14]. In the field of cervical spine, there have been reports of diagnosis, surgery, and rehabilitation using virtual reality [15-17]. Several studies have also been conducted to analyze the movement of the myelopathy hand using sensors [18-22]. Most of these studies used wearable sensors such as motion capture systems, strain sensors, gyro sensors, and bend sensors, which are complicated.
For a simpler test, we analyzed hand and finger movements in the 10-s test using Leap Motion (Leap Motion) in a previous study [23]. Leap Motion is a noncontact sensor consisting of infrared cameras and LEDs, and captures hand and finger movements in real time [24,25]. Furthermore, we applied a machine learning algorithm to the obtained data to create a binary classification model to classify CM with 84% sensitivity, 60.7% specificity, and 0.85 area under the curve (AUC). However, because of the limitations of the system, only fingertip movements, not all joint movements, were recorded. Moreover, because only patients with CM and healthy participants were compared, it was not clear whether our model could differentiate CM from other hand disorders such as carpal tunnel syndrome (CTS).
To solve these problems, we improved the system so that the joints of each finger can also be recorded by Leap Motion and aimed to develop a system capable of diagnosing CM with higher sensitivity and specificity. Furthermore, we included patients with CTS, a common hand disorder, to verify if it is possible to distinguish CM from CTS.
Methods
Ethics Approval
This study was approved by the Institutional Review Board of Tokyo Medical and Dental University (M2019-047). Written informed consent was provided by all participants.
Recruitment
We included preoperative patients with CM (CM group), preoperative patients with CTS (CTS group), and volunteers (control group) between February 2020 and July 2021. Experienced spine surgeons diagnosed CM based on symptoms, physical and neurological findings, and magnetic resonance imaging (MRI) or computed tomography myelogram. Experienced hand surgeons diagnosed CTS based on symptoms, physical findings such as the Tinel sign and Phalen test, and nerve conduction studies (NCSs) measured by Neuropack X1 (Nihon Kohden). Volunteers were recruited from patients who had undergone total hip arthroplasty.
In all groups, participants with a history of other upper extremity disease, injury, or surgery; those with neurological diseases such as stroke, brain tumor, and traumatic brain injury; those with inflammatory diseases such as rheumatoid arthritis; those with dementia or psychiatric disease; and those who refused to participate were excluded. Moreover, spine surgeons also examined participants in the CTS and control groups, and excluded those with symptoms or physical findings suggestive of CM from the CTS and control groups. Similarly, hand surgeons examined participants in the CM and control groups, and excluded those with symptoms or physical findings suggestive of CTS from the CM and control groups.
In the CM group, primary diseases causing CM were recorded. The maximally compressed levels of the spinal cord were also recorded from the sagittal and axial images of the preoperative T2-weighted MRI. In the CTS group, Bland classifications were recorded as severity based on NCSs [26]. Finally, the CTS and control groups were combined to create a non-CM group.
Measurements With Leap Motion
Before the measurement, the procedure and a short demonstration were provided to the participants. The protocol of the measurement with Leap Motion was based on a previous study and was performed as follows: participants sat in front of Leap Motion placed in front of a laptop computer and connected by USB, extended the elbow on the side to be measured, placed the hand 10 cm above Leap Motion in a pronated position, and gripped and released the fingers as rapidly and as fully as possible 20 times after seeing the sign to start the examination (Figure 1) [23]. During the measurement, we confirmed that the system could correctly capture participant hand movements by watching the 3D hand model displayed on the screen in real time. All participants completed both hand measurements twice. A total of 229 parameters, listed in Table 1, were measured as waveform data (60 frames per second).
Figure 1.
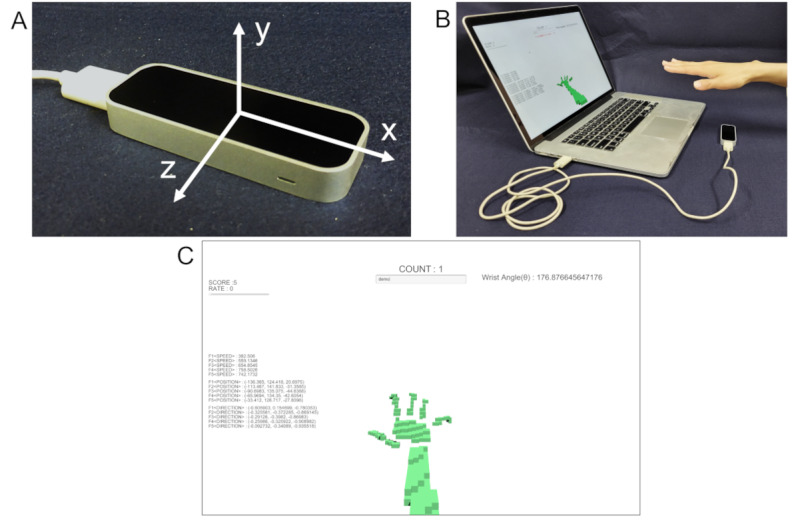
Images of the measurement with Leap Motion. Leap Motion and the three axes measured by Leap Motion (A). Participants placed their hand above Leap Motion, connected to a laptop computer via USB (B). During the measurement, a 3D hand model was displayed in real time on the screen of the laptop computer (C).
Table 1.
Parameters measured by Leap Motion.
| Parameters | Values, n | Total (N=229), n |
| Extended fingers (n) | 1 | 1 |
| Position of palm | 3 dimensionsa | 3 |
| Direction of palm | 3 dimensions | 3 |
| Angle of wrist extension | 1 | 1 |
| Position of wrist | 3 dimensions | 3 |
| Direction of forearm | 3 dimensions | 3 |
| Speed of fingertip | 5 fingers | 5 |
| Position of fingertip | 5 fingers × 3 dimensions | 15 |
| Direction of fingertip | 5 fingers × 3 dimensions | 15 |
| Position of distal end of bone | 5 fingers × 4 bonesb × 3 dimensions | 60 |
| Position of center of bone | 5 fingers × 4 bones × 3 dimensions | 60 |
| Direction of bone | 5 fingers × 4 bones × 3 dimensions | 60 |
aDimensions consist of x, y, and z coordinates.
bBones consist of distal phalanx, middle phalanx, proximal phalanx, and metacarpus. For convenience, bones of the thumb were assumed to consist of distal phalanx, proximal phalanx, metacarpus, and carpal bones.
Statistical Analysis
Characteristics of Participants
The characteristics of participants were assessed using Student t test for age, chi-square test for sex and measured side of the hand, and Fisher exact test for hand dominance. A P value <.05 was considered statistically significant.
Binary Classification Model
We aimed to create two models, one to diagnose CM among the CM and control groups (CM/control model), and the other to diagnose CM among the CM and non-CM groups (CM/non-CM model).
Preprocessing of the data was performed prior to the application of machine learning. First, each waveform data was divided into 15 segments of 64 frames each while allowing for overlap because each participant took different frames to perform 20 grips and releases. These segments (64 frames) were linearly detrended and multiplied by the Hanning window function [27]. The processed segments were converted to frequency domain data using fast Fourier transform. The subwaveforms (64 frames) were converted into frequency domain data, selecting only the lower 16 frequencies. Finally, a 54,960-dimensional data set (229 parameters × 16 frequency domain data × 15 segments) was obtained for each trial. Data from two trials on each hand were combined and used to create the CM/control model. Alternatively, since CTS can occur on only one hand, data from only two trials on one hand (either the right or left) were combined and used to create the CM/non-CM model.
A support vector machine (SVM) was used to create the binary classification models [28]. SVM is one of the common machine learning algorithms used for classification and has performed well in previous studies. After the learning phase, the SVM shows a predicted label of CM with a probability score. We set a threshold and created a binary classification model to classify whether a data set was CM or not. Data from the CM and control groups were used for the CM/control model, and data from all groups were used for the CM/non-CM model. In the validation phase, 10-fold cross-validation was performed [29]. We generated a receiver operating characteristic (ROC) curve by adjusting the threshold and calculating the AUC. The point on the ROC curve closest to the upper-left corner of the graph was set as the optimal cutoff value.
Furthermore, to investigate which parts of the hand contribute to the diagnosis of CM, we also generated modified CM/control models using data from only one of the 20 bones and then similarly calculated the AUC.
Results
Comparison of Characteristics of Participants
In total, 31 participants (62 hands), 27 participants (38 hands), and 29 participants (58 hands) were recruited to the CM, CTS, and control groups, respectively. Patient demographics and characteristics are summarized in Table 2. There was no significant difference between the groups in terms of age, sex, or hand dominance.
Table 2.
Characteristics of participants in the CM, CTS, and control groups.
| Characteristic | Non-CMa | CM | P value | ||||||||||
|
|
Control | CTSb |
|
CM/control | CM/non-CM | ||||||||
| Participants, n | 29 | 25 | 31 | N/Ac | N/A | ||||||||
| Age (years), mean (SD) | 63.6 (52.1-75.0) | 62.0 (49.2-74.7) | 67.0 (57.0-77.0) | .23 | .11 | ||||||||
| Sex (male), n | 12 | 5 | 16 | .59 | .11 | ||||||||
| Hand dominance (right), n | 29 | 25 | 30 | >.99 | .36 | ||||||||
| Hands, n | 58 | 34 | 62 | N/A | N/A | ||||||||
| Side (right), n | 29 | 20 | 31 | >.99 | .83 | ||||||||
| Bland classification, n | N/A |
|
N/A | N/A | N/A | ||||||||
|
|
Grade 1 |
|
3 |
|
|
|
|||||||
|
|
Grade 2 |
|
0 |
|
|
|
|||||||
|
|
Grade 3 |
|
17 |
|
|
|
|||||||
|
|
Grade 4 |
|
0 |
|
|
|
|||||||
|
|
Grade 5 |
|
14 |
|
|
|
|||||||
|
|
Grade 6 |
|
4 |
|
|
|
|||||||
| Primary disease, n | N/A | N/A |
|
N/A | N/A | ||||||||
|
|
CSMd |
|
|
13 |
|
|
|||||||
|
|
OPLLe |
|
|
16 |
|
|
|||||||
|
|
CDHf |
|
|
2 |
|
|
|||||||
| Maximally compressed level, n | N/A | N/A |
|
N/A | N/A | ||||||||
|
|
C1/2 |
|
|
1 |
|
|
|||||||
|
|
C2/3 |
|
|
0 |
|
|
|||||||
|
|
C3/4 |
|
|
12 |
|
|
|||||||
|
|
C4/5 |
|
|
8 |
|
|
|||||||
|
|
C5/6 |
|
|
9 |
|
|
|||||||
|
|
C6/7 |
|
|
1 |
|
|
|||||||
aCM: cervical myelopathy.
bCTS: carpal tunnel syndrome.
cN/A: not applicable.
dCSM: cervical spondylotic myelopathy.
eOPLL: ossification of the posterior longitudinal ligament.
fCDH: cervical disk herniation.
Binary Classification Model
The indexes of the binary classification models are listed in Table 3. The ROC curve of the control and CM/non-CM model are shown in Figure 2.
Table 3.
Index of binary classification models.
|
|
Sensitivity (%) | Specificity (%) | AUCa | |
| CMb/control model | 74.2 | 89.7 | 0.82 | |
| CM/non-CM model | ||||
|
|
Total | 71.0 | 72.8 | 0.74 |
|
|
Right hand | 71.0 | 75.5 | 0.77 |
|
|
Left hand | 74.2 | 79.1 | 0.76 |
aAUC: area under the curve.
bCM: cervical myelopathy.
Figure 2.
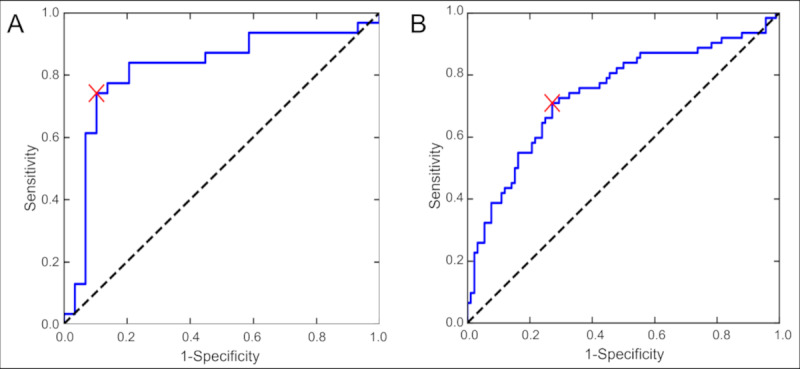
Receiver operating characteristic (ROC) curve of the cervical myelopathy (CM)/control model (A) and CM/non-CM model (B). The area under the ROC curve was 0.82 and 0.74 in the CM/control model and CM/non-CM model, respectively. The red cross indicates the optimal cutoff value.
The AUC of models limited to the parameters of each bone are listed in Table 4. The AUC of the model using the parameters of the proximal phalanx of the thumb was the highest (0.86).
Table 4.
Area under the curve of models limited to the parameters of each bone
|
|
Thumba | Index finger | Middle finger | Ring finger | Little finger |
| Distal phalanx | 0.83 | 0.82 | 0.80 | 0.78 | 0.78 |
| Middle phalanx | 0.86 | 0.83 | 0.81 | 0.80 | 0.79 |
| Proximal phalanx | 0.84 | 0.82 | 0.84 | 0.83 | 0.83 |
| Metacarpus | 0.82 | 0.82 | 0.83 | 0.83 | 0.82 |
aOnly in the thumb, middle phalanx means proximal phalanx, proximal phalanx means metacarpus, and metacarpus means carpal bones.
Discussion
Principal Results
We developed a classification model with high sensitivity and specificity to diagnose CM. However, despite increasing the parameters, major improvements in diagnostic performance of the CM/control model were not obtained in this study (74.2% sensitivity, 89.7% specificity, and 0.82 AUC) compared to the previous study (84% sensitivity, 60.7% specificity, and 0.85 AUC) [23]. Increasing only the number of parameters will result in improved diagnostic performance; therefore, it is necessary to increase the number of samples. Nevertheless, the classification model in this study is still effective as a screening method since it has a sufficiently high diagnostic performance when compared to classic tests. For example, the 10-s test showed 61%-74% sensitivity, 52%-66% specificity, and 0.71-0.77 AUC [10,30,31]; the finger escape sign showed 48%-55% sensitivity [30,31]; the deep tendon reflex change showed 15%-56% sensitivity and 96%-98% specificity [31-33]. In another previous study, the analysis and diagnoses of myelopathy hand was performed by wearing a glove with a sensor, with 87% sensitivity, 86% specificity, and 0.93 AUC [21]. Although the result of this study is inferior to the previous study, our method is superior in that it is easier to test many patients with the noncontact sensor, making it suitable for screening.
In the models limited to the parameters of each bone, the AUC of the model using the parameters of the proximal phalanx of the thumb was the highest. In addition, overall, the models using the parameters of bones of the thumb tended to have higher AUCs. This result is contrary to the finger escape sign, which indicates that the ulnar finger is more likely to be affected in CM [9]. The cause of this discrepancy may be due to the position of the sensor in this method. Because Leap Motion captures hand movement from the palmar side, the bones of the fingers other than the thumb are temporarily hidden by other bones during the grip and release movements, and occasionally not accurately captured. Alternatively, thumb movement is always tracked by Leap Motion. Moreover, another study reported that patients with CM exhibit specific changes in pinching movements with the thumb and index finger [20]. This result means that, in patients with CM, not only ulnar but also radial finger movements are significantly altered. These factors would contribute to the higher AUCs of the model using the parameters of the proximal phalanx of the thumb.
In this study, we attempted to differentiate the CM group from not only the control group, as in the previous study [23], but also the CTS (non-CM) group, and we achieved high diagnostic performance. The peak onset of CM is between the years of 40 and 60 years [1,3], but other hand disorders are also prevalent during that time. Because CTS is a common hand disorder, with a predilection for people 40 years or older [34,35], we included these patients in our study. Our system can distinguish myelopathy hand from motor disorders of the thumb that can occur in CTS [36]. While further trials are required to differentiate CM from other hand disorders, this result suggests the possibility of accurately screening for CM among a variety of hand disorders.
Several studies have also been conducted to analyze the movement of the myelopathy hand using sensors, but Leap Motion has the major advantage of simplicity. For example, motion captures can provide a detailed motion analysis, but the installation of the sensors requires skill and time of the examiners, and it is impossible to test a large number of patients in a short period of time. Alternatively, Leap Motion can be used for our test simply by connecting it to a computer if the program can be shared. Furthermore, the test can be performed by a single patient with only a simple test procedure guide. Leap Motion is also a less expensive commercial sensor, which is an advantage in that it is readily available. These advantages of Leap Motion are useful for screening large numbers of patients in a short period of time.
Limitations
This study had some limitations. First, it is possible that there were participants with potential CM in the CTS and control groups because participants in these groups did not undergo an MRI. Similarly, it is possible that there were participants with potential CTS in the CM and control groups because participants in these groups did not undergo an NCS.
Second, we did not compare subgroups by anatomical level of myelopathy and by severity of CM and CTS. There may be variation among subgroups within the same group. Third, only internal validation by 10-fold cross validation was performed and external validation was not. In future work, we will collect more samples to solve these problems.
Conclusions
We developed a screening system capable of diagnosing CM with higher sensitivity and specificity by high-dimensional analysis of finger motion and machine learning. This system can differentiate patients with CM from patients with CTS as well as healthy patients and has the potential to screen for CM in a variety of patients.
Acknowledgments
This research was supported by JST AIP-PRISM JPMJCR18Y2 and JST PRESTO JPMJPR17J4. We would like to thank Editage for English language editing.
Abbreviations
- 10-s
10-second hand grip and release
- AUC
area under the curve
- CM
cervical myelopathy
- CTS
carpal tunnel syndrome
- MRI
magnetic resonance imaging
- NCS
nerve conduction study
- ROC
receiver operating characteristic
- SVM
support vector machine
Footnotes
Conflicts of Interest: None declared.
References
- 1.Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine (Phila Pa 1976) 2015 Jun 15;40(12):E675–93. doi: 10.1097/BRS.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 2.Rao R. Neck pain, cervical radiculopathy, and cervical myelopathy: pathophysiology, natural history, and clinical evaluation. J Bone Joint Surg Am. 2002 Oct;84(10):1872–81. doi: 10.2106/00004623-200210000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Theodore N. Degenerative cervical spondylosis. N Engl J Med. 2020 Jul 09;383(2):159–168. doi: 10.1056/NEJMra2003558. [DOI] [PubMed] [Google Scholar]
- 4.Tanaka J, Seki N, Tokimura F, Doi K, Inoue S. Operative results of canal-expansive laminoplasty for cervical spondylotic myelopathy in elderly patients. Spine (Phila Pa 1976) 1999 Nov 15;24(22):2308–12. doi: 10.1097/00007632-199911150-00004. [DOI] [PubMed] [Google Scholar]
- 5.Tetreault L, Kopjar B, Côté P, Arnold P, Fehlings MG. A clinical prediction rule for functional outcomes in patients undergoing surgery for degenerative cervical myelopathy: analysis of an international prospective multicenter data set of 757 subjects. J Bone Joint Surg Am. 2015 Dec 16;97(24):2038–46. doi: 10.2106/JBJS.O.00189.97/24/2038 [DOI] [PubMed] [Google Scholar]
- 6.Tetreault LA, Kopjar B, Vaccaro A, Yoon ST, Arnold PM, Massicotte EM, Fehlings MG. A clinical prediction model to determine outcomes in patients with cervical spondylotic myelopathy undergoing surgical treatment: data from the prospective, multi-center AOSpine North America study. J Bone Joint Surg Am. 2013 Sep 18;95(18):1659–66. doi: 10.2106/JBJS.L.01323.1734761 [DOI] [PubMed] [Google Scholar]
- 7.Sadasivan KK, Reddy RP, Albright JA. The natural history of cervical spondylotic myelopathy. Yale J Biol Med. 1993;66(3):235–42. [PMC free article] [PubMed] [Google Scholar]
- 8.Kobayashi H, Kikuchi S, Otani K, Sekiguchi M, Sekiguchi Y, Konno S. Development of a self-administered questionnaire to screen patients for cervical myelopathy. BMC Musculoskelet Disord. 2010 Nov 22;11:268. doi: 10.1186/1471-2474-11-268. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-11-268 .1471-2474-11-268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ono K, Ebara S, Fuji T, Yonenobu K, Fujiwara K, Yamashita K. Myelopathy hand. New clinical signs of cervical cord damage. J Bone Joint Surg Br. 1987 Mar;69(2):215–9. doi: 10.1302/0301-620X.69B2.3818752. [DOI] [PubMed] [Google Scholar]
- 10.Machino M, Ando K, Kobayashi K, Morozumi M, Tanaka S, Ito K, Kato F, Ishiguro N, Imagama S. Cut off value in each gender and decade of 10-s grip and release and 10-s step test: a comparative study between 454 patients with cervical spondylotic myelopathy and 818 healthy subjects. Clin Neurol Neurosurg. 2019 Sep;184:105414. doi: 10.1016/j.clineuro.2019.105414.S0303-8467(19)30210-0 [DOI] [PubMed] [Google Scholar]
- 11.Patel V, Chesmore A, Legner CM, Pandey S. Trends in workplace wearable technologies and connected‐worker solutions for next‐generation occupational safety, health, and productivity. Adv Intelligent Syst. 2021 Sep 23;4(1):2100099. doi: 10.1002/aisy.202100099. [DOI] [Google Scholar]
- 12.Koyama T, Sato S, Toriumi M, Watanabe T, Nimura A, Okawa A, Sugiura Y, Fujita K. A screening method using anomaly detection on a smartphone for patients with carpal tunnel syndrome: diagnostic case-control study. JMIR Mhealth Uhealth. 2021 Mar 14;9(3):e26320. doi: 10.2196/26320. https://mhealth.jmir.org/2021/3/e26320/ v9i3e26320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pan D, Dhall R, Lieberman A, Petitti DB. A mobile cloud-based Parkinson's disease assessment system for home-based monitoring. JMIR Mhealth Uhealth. 2015 Mar 26;3(1):e29. doi: 10.2196/mhealth.3956. https://mhealth.jmir.org/2015/1/e29/ v3i1e29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watanabe T, Koyama T, Yamada E, Nimura A, Fujita K, Sugiura Y. The accuracy of a screening system for carpal tunnel syndrome using hand drawing. J Clin Med. 2021 Sep 27;10(19):4437. doi: 10.3390/jcm10194437. https://www.mdpi.com/resolver?pii=jcm10194437 .jcm10194437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burström G, Nachabe R, Persson O, Edström E, Elmi Terander A. Augmented and virtual reality instrument tracking for minimally invasive spine surgery: a feasibility and accuracy study. Spine (Phila Pa 1976) 2019 Aug 01;44(15):1097–1104. doi: 10.1097/BRS.0000000000003006.00007632-201908010-00016 [DOI] [PubMed] [Google Scholar]
- 16.Sarig Bahat H, Croft K, Carter C, Hoddinott A, Sprecher E, Treleaven J. Remote kinematic training for patients with chronic neck pain: a randomised controlled trial. Eur Spine J. 2018 Jun;27(6):1309–1323. doi: 10.1007/s00586-017-5323-0.10.1007/s00586-017-5323-0 [DOI] [PubMed] [Google Scholar]
- 17.Sarig-Bahat H, Weiss PL, Laufer Y. Cervical motion assessment using virtual reality. Spine (Phila Pa 1976) 2009 May 01;34(10):1018–24. doi: 10.1097/BRS.0b013e31819b3254.00007632-200905010-00007 [DOI] [PubMed] [Google Scholar]
- 18.Oess NP, Wanek J, Curt A. Design and evaluation of a low-cost instrumented glove for hand function assessment. J Neuroeng Rehabil. 2012 Jan 17;9:2. doi: 10.1186/1743-0003-9-2. https://jneuroengrehab.biomedcentral.com/articles/10.1186/1743-0003-9-2 .1743-0003-9-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Omori M, Shibuya S, Nakajima T, Endoh T, Suzuki S, Irie S, Ariyasu R, Unenaka S, Sano H, Igarashi K, Ichimura S, Ohki Y. Hand dexterity impairment in patients with cervical myelopathy: a new quantitative assessment using a natural prehension movement. Behav Neurol. 2018;2018:5138234. doi: 10.1155/2018/5138234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sakai N. Finger motion analysis of the patients with cervical myelopathy. Spine (Phila Pa 1976) 2005 Dec 15;30(24):2777–82. doi: 10.1097/01.brs.0000190452.33258.72.00007632-200512150-00012 [DOI] [PubMed] [Google Scholar]
- 21.Su X, Hou C, Shen B, Zhang W, Wu D, Li Q, Shen H. Clinical application of a new assessment tool for myelopathy hand using virtual reality. Spine (Phila Pa 1976) 2020 Dec 15;45(24):E1645–E1652. doi: 10.1097/BRS.0000000000003696.00007632-202012150-00006 [DOI] [PubMed] [Google Scholar]
- 22.Date S, Nakanishi K, Fujiwara Y, Yamada K, Kamei N, Kurumadani H, Yoshimura M, Ueda A, Ishii Y, Ohta R, Kotaka S, Tsuchikawa Y, Nakamae T, Ishikawa M, Hirao K, Fujimoto Y, Adachi N, Sunagawa T. Quantitative evaluation of abnormal finger movements in myelopathy hand during the grip and release test using gyro sensors. PLoS One. 2021;16(10):e0258808. doi: 10.1371/journal.pone.0258808. https://dx.plos.org/10.1371/journal.pone.0258808 .PONE-D-21-15086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koyama T, Fujita K, Watanabe M, Kato K, Sasaki T, Yoshii T, Nimura A, Sugiura Y, Saito H, Okawa A. Cervical myelopathy screening with machine learning algorithm focusing on finger motion using noncontact sensor. Spine (Phila Pa 1976) 2022 Jan 15;47(2):163–171. doi: 10.1097/BRS.0000000000004243.00007632-202201150-00013 [DOI] [PubMed] [Google Scholar]
- 24.Guna J, Jakus G, Pogačnik M, Tomažič S, Sodnik J. An analysis of the precision and reliability of the leap motion sensor and its suitability for static and dynamic tracking. Sensors (Basel) 2014 Feb 21;14(2):3702–20. doi: 10.3390/s140203702. https://www.mdpi.com/resolver?pii=s140203702 .s140203702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weichert F, Bachmann D, Rudak B, Fisseler D. Analysis of the accuracy and robustness of the leap motion controller. Sensors (Basel) 2013 May 14;13(5):6380–93. doi: 10.3390/s130506380. https://www.mdpi.com/resolver?pii=s130506380 .s130506380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bland JD. A neurophysiological grading scale for carpal tunnel syndrome. Muscle Nerve. 2000 Aug;23(8):1280–3. doi: 10.1002/1097-4598(200008)23:8<1280::aid-mus20>3.0.co;2-y.10.1002/1097-4598(200008)23:8<1280::AID-MUS20>3.0.CO;2-Y [DOI] [PubMed] [Google Scholar]
- 27.Harris F. On the use of windows for harmonic analysis with the discrete Fourier transform. Proc IEEE. 1978 Jan;66(1):51–83. doi: 10.1109/proc.1978.10837. [DOI] [Google Scholar]
- 28.Noble WS. What is a support vector machine? Nat Biotechnol. 2006 Dec;24(12):1565–7. doi: 10.1038/nbt1206-1565.nbt1206-1565 [DOI] [PubMed] [Google Scholar]
- 29.Cawley GC, Talbot NL. Efficient leave-one-out cross-validation of kernel fisher discriminant classifiers. Pattern Recognition. 2003 Nov;36(11):2585–2592. doi: 10.1016/S0031-3203(03)00136-5. [DOI] [Google Scholar]
- 30.Findlay GFG, Balain B, Trivedi JM, Jaffray DC. Does walking change the Romberg sign? Eur Spine J. 2009 Oct;18(10):1528–31. doi: 10.1007/s00586-009-1008-7. https://europepmc.org/abstract/MED/19387702 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong TM, Leung HB, Wong WC. Correlation between magnetic resonance imaging and radiographic measurement of cervical spine in cervical myelopathic patients. J Orthop Surg (Hong Kong) 2004 Dec;12(2):239–42. doi: 10.1177/230949900401200220. https://journals.sagepub.com/doi/10.1177/230949900401200220?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 32.Cook C, Brown C, Isaacs R, Roman M, Davis S, Richardson W. Clustered clinical findings for diagnosis of cervical spine myelopathy. J Man Manip Ther. 2010 Dec;18(4):175–80. doi: 10.1179/106698110X12804993427045. https://europepmc.org/abstract/MED/22131790 .18.4_Cook [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cook C, Roman M, Stewart KM, Leithe LG, Isaacs R. Reliability and diagnostic accuracy of clinical special tests for myelopathy in patients seen for cervical dysfunction. J Orthop Sports Phys Ther. 2009 Mar;39(3):172–8. doi: 10.2519/jospt.2009.2938.2278 [DOI] [PubMed] [Google Scholar]
- 34.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999 Jul 14;282(2):153–8. doi: 10.1001/jama.282.2.153.joc81321 [DOI] [PubMed] [Google Scholar]
- 35.Bland JDP, Rudolfer SM. Clinical surveillance of carpal tunnel syndrome in two areas of the United Kingdom, 1991-2001. J Neurol Neurosurg Psychiatry. 2003 Dec;74(12):1674–9. doi: 10.1136/jnnp.74.12.1674. https://jnnp.bmj.com/lookup/pmidlookup?view=long&pmid=14638888 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuroiwa T, Fujita K, Nimura A, Miyamoto T, Sasaki T, Okawa A. A new method of measuring the thumb pronation and palmar abduction angles during opposition movement using a three-axis gyroscope. J Orthop Surg Res. 2018 Nov 16;13(1):288. doi: 10.1186/s13018-018-0999-3. https://josr-online.biomedcentral.com/articles/10.1186/s13018-018-0999-3 .10.1186/s13018-018-0999-3 [DOI] [PMC free article] [PubMed] [Google Scholar]


