Abstract
Background
The distinctive features of the digital reality platforms, namely augmented reality (AR), virtual reality (VR), and mixed reality (MR) have extended to medical education, training, simulation, and patient care. Furthermore, this digital reality technology seamlessly merges with information and communication technology creating an enriched telehealth ecosystem. This review provides a composite overview of the prospects of telehealth delivered using the MR platform in clinical settings.
Objective
This review identifies various clinical applications of high-fidelity digital display technology, namely AR, VR, and MR, delivered using telehealth capabilities. Next, the review focuses on the technical characteristics, hardware, and software technologies used in the composition of AR, VR, and MR in telehealth.
Methods
We conducted a scoping review using the methodological framework and reporting design using the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) guidelines. Full-length articles in English were obtained from the Embase, PubMed, and Web of Science databases. The search protocol was based on the following keywords and Medical Subject Headings to obtain relevant results: “augmented reality,” “virtual reality,” “mixed-reality,” “telemedicine,” “telehealth,” and “digital health.” A predefined inclusion-exclusion criterion was developed in filtering the obtained results and the final selection of the articles, followed by data extraction and construction of the review.
Results
We identified 4407 articles, of which 320 were eligible for full-text screening. A total of 134 full-text articles were included in the review. Telerehabilitation, telementoring, teleconsultation, telemonitoring, telepsychiatry, telesurgery, and telediagnosis were the segments of the telehealth division that explored the use of AR, VR, and MR platforms. Telerehabilitation using VR was the most commonly recurring segment in the included studies. AR and MR has been mainly used for telementoring and teleconsultation. The most important technical features of digital reality technology to emerge with telehealth were virtual environment, exergaming, 3D avatars, telepresence, anchoring annotations, and first-person viewpoint. Different arrangements of technology—3D modeling and viewing tools, communication and streaming platforms, file transfer and sharing platforms, sensors, high-fidelity displays, and controllers—formed the basis of most systems.
Conclusions
This review constitutes a recent overview of the evolving digital AR and VR in various clinical applications using the telehealth setup. This combination of telehealth with AR, VR, and MR allows for remote facilitation of clinical expertise and further development of home-based treatment. This review explores the rapidly growing suite of technologies available to users within the digital health sector and examines the opportunities and challenges they present.
Keywords: augmented reality, virtual reality, mixed realities, telemedicine, eHealth, mobile health, mHealth
Introduction
Background
The term telemedicine refers to the provision of clinical health care services over a distance through information and communication technology (ICT) channels. Telemedicine overcomes geographical barriers in facilitating remote medical services. Building on this, the concept of telehealth extends to include continuing health education, research, and evaluation by medical professionals, all while promoting the health outcomes of individuals and communities [1]. Telehealth broadly encompasses the delivery of remote health-related services, including nonclinical services such as medical provider training; medical education; public health education; administrative meetings; and electronic exchange of clinical data enabling diagnosis, evaluation, consultation, treatment, and care management. The term telehealth has evolved as available technologies have improved, such that the term “digital health” is now often used as a more inclusive term reflecting the application of various different types of technologies and telecommunications systems in health care delivery. Digital health platforms can be either provider-to-provider or direct-to-consumer systems supported by the ICT infrastructure [2,3]. The telehealth sector has seen an effective increase in the past few years and has grown exponentially because of COVID-19 pandemic restrictions. According to the report published by Fortune Business Insights, the global telehealth market size was estimated at around US $144.38 billion in 2020 and is likely to reach US $636.38 billion by 2028 [4].
From the reality-virtuality continuum model, according to Milgram et al [5] (as seen in Figure 1), the real environment is that which is viewed without any overlay of the computer-generated entity, while at the opposite end of this continuum, immersive virtual reality (VR) is observed as completely enhanced computer-generated environments viewed through a head-mounted display unit. In the augmented reality (AR)–based display, digital information or entities are overlaid in the real environment, such that different aspects of reality are observed between the real and virtual environment. These augmentation-based realities can be discovered by optical see-through head-mounted displays (HMDs), mobile phones, tablets, or computer monitors [5].
Figure 1.
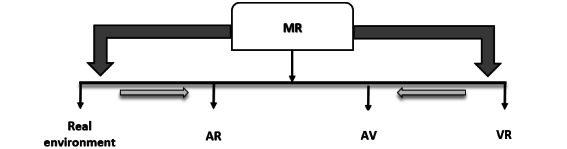
Representation of reality-virtuality continuum by Milgram et al [5]. AR: augmented reality; AV: augmented virtuality; MR: mixed reality; VR: virtual reality.
In AR technology, the digitally created data directly coincide with the user’s real-world environment, where the user can see the computer-generated 2D or 3D entities such as holograms. The virtual entities superimposed or mapped onto the real-world space are typically rendered using optical see-through display such as HMDs or mobile-based devices, also allowing for stereoscopic visualization. The next most advanced form of reality platform, the mixed reality (MR), follows the footstep of AR and allows interaction with these virtual entities by using hand gesture inputs, gaze recognition, or controllers. The VR platform is a completely enhanced digital representation featuring a 2D or 3D virtual environment or objects that can replicate real-life surroundings. VR provides engaging sensory perceptions for both visual and acoustic stimulation. Immersive VR relies on headsets or stand-alone VR devices, whereas nonimmersive VR relies on the monitor display [6].
The introduction of VR and AR technologies in medicine has been focused on clinical-related research. The key areas incorporating this digital reality are surgery, psychology, neurological condition, rehabilitation, and medical educational [7]. The 3D picturing capabilities of the VR- and AR-based platforms have been sought for applications in the visualization of scientific experimental imaging data, tools for surgical planning and studying anatomy, and other collaborative interfaces for education and telehealth [8]. Surgical simulation has distinctively used digital reality, while VR is principally used for visual and haptic rendering, whereas AR and MR were predominantly positioned for the tracking system and graphical rendering, with the latter being used in a real surgical setting [9]. The usefulness of VR education and training using simulation methods for nursing students was comparable with the standard models of education and training on the outcomes of skills, confidence, satisfaction, and performance time [10]. The current prospects of AR software applications in medical criteria are treatment and training based [11]. Surgical development using an MR platform has been linked as a predominant utilization tool for training and simulation technology, advanced imaging and navigation, and broadening the extent of clinical application. Recently, MR has been adapted to neurosurgery, otolaryngology, ophthalmology, urology, and dentistry [12]. Digital reality technology has been incorporated into the preoperative surgical planning for several cranial-based applications for the neurosurgical subspecialty [13]. VR-based exposure therapy is used for various psychiatric disorders such as anxiety, trauma and stress, neurocognitive disorders, and several mental disorders. The effects of VR have been studied to have long-lasting positive outcomes for the treatment [14]. VR-based training has been effective in the improvement of executive limb function and cognitive function in patients with stroke [15,16].
Objectives
Many published studies have reviewed the use of AR and VR capabilities in medical research and practice and have not detailed its implication in telehealth, thus addressing this research gap. This systematic scoping review provides an overview of the prospects of AR and VR applications delivered using telehealth platforms in clinical settings. This review offers end users and providers an update of the current use of AR, VR, and MR effectively in telehealth delivery and highlights the prospects of such technologies in the future. This review aims to explore the following research questions:
What clinical specialties have incorporated digital reality platforms such as AR, VR, or MR exclusively with telehealth?
What are the different hardware and software technology formats used in AR, VR, or MR within telehealth?
Which important technical features of AR and VR have been used in telehealth?
Methods
Overview
This scoping review used the framework of the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) guidelines [17]. Included studies from the database were solely concerned with the application of high-fidelity simulation technology such as AR, VR, or MR exclusively delivered via the telehealth platform. The study has no written or published protocol.
Database and Search Strategy
Articles from Embase, PubMed, and Web of Science were explored to obtain relative pieces of evidence. An exploded search strategy string was developed with the support of a university librarian. The search string included appropriate keywords and Medical Subject Headings terms—“augmented reality,” “virtual reality,” “mixed reality,” “extended reality,” “telemedicine,” “telehealth,” “m-Health,” “e-Health,” and “digital health.” The search strategy was initially developed on the Embase database and replicated across the other databases using predefined filtering techniques. The entire search strategy can be seen in Multimedia Appendix 1.
Eligibility Criteria
The studies included must satisfy the active component use of AR, VR, or MR delivered via telehealth approaches and should have been published between the years 2016 and 2021, since such devices with this technology format became commercially available, marked in reference to the release date for the first-generation Microsoft HoloLens [18]. The collaboration aspect of AR and MR technology into social or digital communication avenues could be observed during the same period [19]. Telemedicine or telehealth includes a broad spectrum of health care delivery, including education prospects; however, this review will focus on clinical aspects, including simulation. Only full-length text articles available on the web in the English language were included. Full-length text from peer-reviewed articles such as randomized controlled trials, feasibility studies, exploratory studies, narrative reviews, systematic reviews, case and cohort studies, book sections, and technical reports was considered eligible for inclusion. Any studies highlighting the mentioned technology for gaming, entertainment, or medical education were excluded. Correspondence papers, letters, conference abstracts (no full texts), editorial, commentary, poster presentations, and gray literature were also excluded from this review.
Study Selection and Data Extraction
The papers obtained from the applied search strategy from the information databases were imported to the reference manager EndNote 20 library, and duplicates were discarded [20]. Three researchers (HW, SC, and JK) performed initial screenings based on titles, abstracts, and keyword searches. Author HW conducted eligibility criteria and full-text screening. The selected studies were then reviewed based on the article type, study design, clinical condition addressed in the study, mode of telehealth communication, acceptance criteria, and the hardware and software used in the studies for the guidance for data synthesis. Finally, the relevant information from the studies was tabulated into an Excel (Microsoft Corp) spreadsheet, and a descriptive synthesis of the data was generated. In our review, we summarized and grouped the various telehealth branches using digital reality platforms for the various clinical condition based on descriptive statistical findings for the included studies. Different facets of the digital reality technology were detailed for its application in clinical research.
Results
Overview
Of the 4407 abstracts identified from the search protocol, 134 full-text articles fulfilled the inclusion criteria. A total of 1079 duplicate records were removed, 2598 records were discarded after title, abstract, and keyword search, and 410 records were deemed not fit after the initial screening as these articles were not about topic of interest having objectives that did not align with the outcomes of this review and did not satisfy the inclusion criteria. Of the 320 articles that were subjected to full-text review, 177 articles were deemed not relevant because they either included the digital reality technology or telehealth strategies but not delivered jointly, and 9 were excluded after recognizing multiple papers published on the same topic by the HW, SC, and JK (Figure 2).
Figure 2.
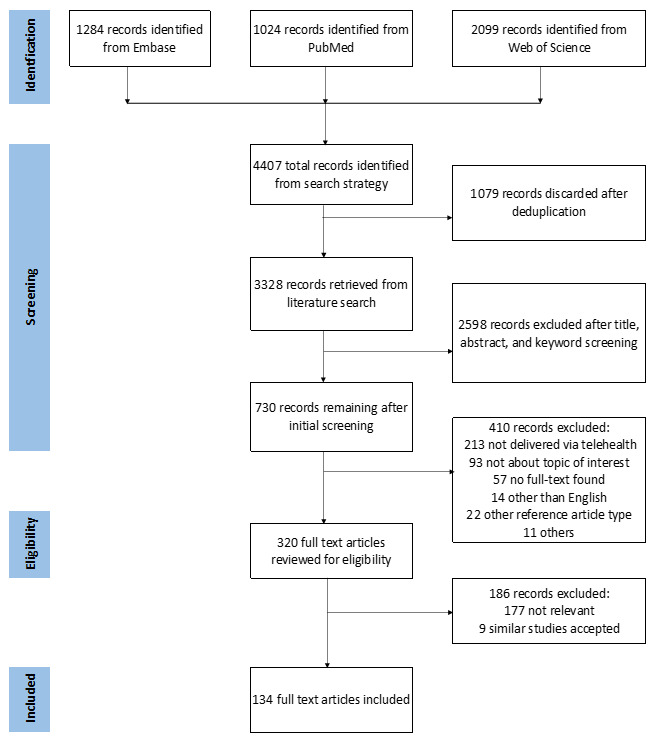
Flowchart for the structured literature search and selection.
Digital Reality Platform via Telehealth
As demonstrated in Figure 3, VR and AR cover most of the listed telehealth domains for the eligible studies. The most studied and researched area is telerehabilitation accomplished using VR. The other subareas involving VR use include telepsychiatry for evaluation and treatment, telediagnosis, and teleconsultation. In addition, AR and MR are prevalent modes of the reality technology platform for telementoring and teleconsultation. Finally, telesurgery and telemonitoring are the 2 subfields of telehealth where AR technology have seen an upward trend.
Figure 3.
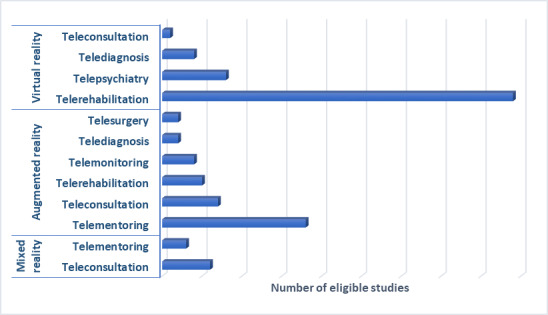
Collaboration between digital reality technology and telehealth for the included studies.
Clinically based digital health applications were considered for the review as various specific branches of the telehealth spectrum (Figure 4). Telerehabilitation is a postclinical care service delivered at home or remotely for recovery purposes and constitutes most of the included telehealth group from the included studies [21,22]. Evident from the included studies, stroke rehabilitation emerges as the leading medical condition that has seen an uptake of these services. Different aspects of rehabilitation, such as functional motor training, including upper-extremity training and fine motor skills, cognitive functional training, visuomotor tracking training, and balance and gait training are primarily used for treating poststroke survivors [23-41]. In turn, the patient groups who have used telehealth for the purposes of rehabilitation have reported improvements in their quality of life, increased daily activities, and improved levels of motivation [42]. From the multiple studies included, telerehabilitation has been experimented as a home-based treatment for various neurological and cognitive disorders or diseases such as Parkinson disease, acquired brain injuries, multiple sclerosis, cerebral palsy, mild cognitive impairment, Alzheimer disease, and dementia [43-58].
Figure 4.
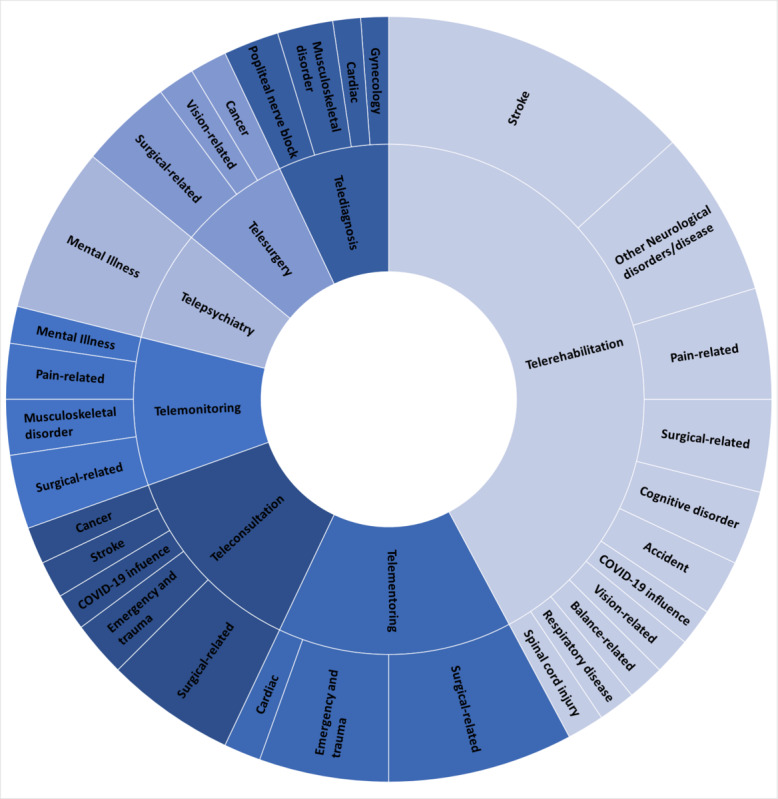
An overview of different clinical conditions and groups categorized within specific telehealth domains.
Conventional therapy programs in the form of physical therapy and behavioral therapy are the nonpharmacological treatments that have used this remote delivery platform. In a small number of studies, the home-based rehabilitation in the form of novel telerehabilitation have been used for patients undergoing surgical procedures, such as total hip replacement, total knee arthroplasty, and total knee replacement, as a postrecovery treatment measure [59-62]. Mirror therapy for patients with phantom limb pain and physiotherapy treatment for patients with chronic body pain have incorporated this model of remote teletherapy [63-68]. This field has also been applied in physical rehabilitation for musculoskeletal disorders, provision of vestibular rehabilitation therapy in patients with a balance disorder, and kinesiotherapy for older adults at risk of falls [2,69,70]. Physical therapy in the pediatric group and musical therapy in patients with spinal cord injury have explored this stream of technology [71,72]. Pulmonary rehabilitation therapy for respiratory disorders such as chronic pulmonary respiratory disorder, pulmonary fibrosis, and myocardial infarction; low vision rehabilitation in providing functional visual assistance; and the COVID-19 pandemic have been an influential factor in accelerating remote rehabilitation therapy [22,73-77].
Telementoring is a subset of telemedicine that reflects remote expert guidance such as training or telenavigation to medical and nonmedical personnel in performance of life-sustaining procedures [78]. The impact and usability of the telementoring technique in provision of cardiopulmonary resuscitation in treating cardiac arrest has been demonstrated by different authors in simulated environments, with the assistance of a remote mentor using an HMD or Google Glass [79,80]. Other authors have explored the use of telementoring guidance, in intraoperative telenavigation, and preoperative planning in simulated battlefield and emergency trauma. The telementoring approach for preoperative planning and telenavigation during the intraoperative process has been demonstrated in complex emergency hand reconstruction surgery [81,82]. Forward damage control procedure performed on a patient-simulator model depicting a right-sided femoral gunshot wound and simulated trauma injuries such as airway obstruction by conducting cricothyroidotomy have been carried out using remote instruction—as have, lung decompression, tracheostomy, or REBOA (resuscitative endovascular balloon occlusion of the aorta) catheter deployment to deal with specific trauma injuries with the aid of a remote medical expert [82-86]. The feasibility of telementoring applicability in the performance of chest thoracotomy, skin grafting, and fasciotomy has been evaluated using ex vivo animal models [78,87,88]. Telementoring has been used to great effect in different stages of surgical planning in various orthopedic, craniofacial, spinal cord, vascular, and cardiothoracic surgeries [6,89-100].
Teleconsultation is a primary segment of telehealth services, broadly consisting of remote consultation services using ICT. This remote consultation can be synchronous or asynchronous and between clinicians (provider-to-provider) for shared decision-making or between clinicians and their patients (provider-patient) [101]. This approach has been applied in patient assessment using the National Institute of Health Stroke Scale for patients with acute stroke and during remote clinical rounds in isolation wards for patients with COVID-19, thereby reducing direct exposure of the staff [102,103]. This technique has also been evaluated in trauma and emergency-related scenarios, such as remote consultation in reading and interpreting electrocardiogram reports related to drug intoxication or poisoning [104,105]. The effectiveness of provider-to-provider teleconsultation has been demonstrated in provision of support for ambulatory staff and first-responders in triage during simulation of major trauma [106]. The applications of teleconsultation in provision of surgical care are broad, allowing collaborative, contextual, and presurgical planning and visualization and intraoperative surgical navigation through high-fidelity immersive reality platforms and devices, as well as facilitating remote delivery of complex information to patients [107-115]. Teleconsultation via the reality platforms has been used to explore the feasibility of telepathology in carrying out an autopsy, image scanning, and transfer of serially sectioned cancer tissue from a mouse [116].
Telemonitoring is an advanced form of clinical care service that provides patient-centered care. This method allows health care providers to collect and track patient information and deliver remote care assistance [117]. This branch of telehealth has been evaluated in pediatric cohorts dealing with hospital-induced stress as a shared experience on a mobile-based AR game for play therapy. This aspect allows managing pediatric patient profiles, data collection, and further analysis for effective treatment [118]. Telemonitoring via holographic conversational agents; that is, a computer-generated character to deliver physiotherapy home exercises to patients with musculoskeletal disorders and chronic pain has been demonstrated to increase their treatment adherence [119]. Supervised AR-based home training has been used for patients with phantom limb pain by providing mirror therapy, thereby promoting visuomotor integration by reengaging the neural circuits related to lost limbs [120]. Telemonitoring has been used in postoperative care and wound assessment in orthopedic and neurosurgical cases and has also been applied for teleproctoring or remote monitoring in pilot simulation as training for fundamentals of laparoscopic surgery examination [121-123].
Telepsychiatry uses ICT to offer a range of clinical and nonclinical services such as psychiatric evaluation, therapy (individual or group-based), patient education, and management remotely [124]. Studies using this element of telehealth and computer-generated virtual environments have evaluated the feasibility of remote therapy such as Virtual Reality Exposure Therapy for patients with acrophobia and evaluation of the technical system in delivering specific phobia treatment for arachnophobia [125,126]. Remotely delivered psychological treatment by the mental health professional include behavioral intervention therapy, cognitive behavioral therapy, mindfulness therapy, and acceptance and commitment therapy for patients facing stress, anxiety, public speaking anxiety, and social anxiety disorder, among others [127-130]. In a simulation study, cognitive and affective assessment of astronauts has been carried out to characterize social isolation from space [131]. Evaluation of telepsychiatry using the reality platform such as VR versus the traditional videoconferencing platform, and the development of newer platforms such as social VR for older adults in urban areas has demonstrated such techniques could lead to improved quality of life by reducing social isolation [132]. Telepsychiatry assessment via VR as a home-based treatment delivered by mental health professionals, such as a psychiatrist, psychologist, licensed social worker, or a mental health counselor, has been demonstrated to mitigate clinician burnout [133,134].
Another exciting subsection of the telehealth sphere, telesurgery, enables teleoperation in an operating field executed over a distance. Telesurgery involves using various disciplines such as communication technology, imaging techniques, motor control systems, robotics, reality platforms, and digital signal processing [135,136]. For example, in an experimental setup, a VR-based teleoperative system consisting of a robotic catheter operating system can be used to imitate vascular interventional surgery for arterial aneurysms or other vascular diseases. This method allowed unskilled surgeons to train in essential catheter guidance skills and enabled experienced physicians to conduct surgeries cooperatively [137]. In addition, a telesurgical experiment was conducted with a tendon-driven continuum robot via telenavigation for endoscopic and minimally invasive surgical procedures by tracking coordinate trajectory registration [138]. Finally, in another simulation case, a magnetically driven endoscopic capsule enabled the teleoperator or user to receive visual feedback in VR to conduct capsule endoscopy for colorectal cancer [139].
Moreover, the reality platform is streamed as a functional stereoscopic display and navigates space during telesurgery. This aspect of telesurgery has been experimented with as a visualization opportunity using smartphone-delivered vision and VR headsets to perform microsurgery for cataract and phacoemulsification [140]. In addition, Stereoscopic AR Predictive Display using the da Vinci R Surgical System to perform laparoscopic surgery and AR-assisted robotic surgery for kidney transplant procedures are some of the current practical applications of telesurgery [141-143]. Telediagnosis refers to the detection or evaluation of a disease or condition using telematics technology. It is achieved remotely while the patient is at a local site with remote diagnostic tools and devices [144,145]. For instance, in experimental analysis, locating and evaluating tumor-bearing hysteromyoma coordinates during a 3D navigated gynecological operation facilitates telediagnosis when visualized on a 3D user interface of the medical record [146]. Another study proposes a framework based on bidirectional haptic feedback and tele immersion in the evaluation of range of motion and maximum isometric strength using the 10 arm movements method in the diagnosis of musculoskeletal disorders, poststroke rehabilitation, or postshoulder surgery [147]. Ultrasonography (USG) is a field in which telediagnosis using the high-fidelity visualization system has been used to great effect. Evaluation of 3D VR telenavigation in cardiac USG has been undertaken in simulated settings. The added benefits of AR enable real-time teleguidance on procedural performance and image registration for point-of-focus ultrasonography (POCUS) and foveated imaging pipeline in extending VR-based telediagnosis [148-150]. Another study mentions AR video communication projected by mobile-based AR guidance to conduct POCUS on popliteal nerve block and a subsequent diagnosis based on the availed health information [151].
Overview of the Hardware and Software Units for the Included Studies
To experience MR, high-simulation visualization hardware devices and some of the commercial ones included in the selected studies are listed in Multimedia Appendix 2. These include high-end AR and VR devices, smart glasses, mobile devices, standard LED (light emitting diode) and LCD (liquid crystal display) television or display screen, 3D television, and 3D projectors. The commonly included immersive reality-capable devices are mostly wearable technology such as smart glasses, VR or AR HMDs, and nonimmersive standard display units. However, these high-fidelity simulation display technologies form the final part of any system and are primarily used in combination with optical capturing and tracking devices and input devices. The optical capturing and tracking systems or devices incorporate 3D depth and color-sensing camera sensors. The input devices such as controllers, trackers, or customized input modules help navigate the immediate VR or any MR environment. Various studies have included the VR gaming element in their rehabilitation programs, with some having their own developed VR rehabilitation system. Most included studies have used biometric devices for specific medical parameter evaluation to draw analysis and simulation models to conduct various training. Other relative hardware devices and systems that have been used are listed in the Multimedia Appendix 3.
The graphical representation for any software harbors a visualization platform, and more specifically, the MR system incorporates contextual 3D figures and scenes. The various software applications and source platforms that were featured and used in the included studies are listed as a table in the Multimedia Appendix 4. These applications are grouped as 3D modeling and visualization software, communication and streaming software, file-sharing and transfer applications, and other specific and personalized software applications. The 3D composite images and environment for the MR technology are created using the computer graphic designing software and gaming engine platforms. Processing and accessing the 3D computer-generated environment or images needs specific and compatible visualization file applications supported by the device. The featured 3D modeling and viewing application allows for creating and editing static and interactive multidimensional models and VR scenes, animations, and games, conversion of the produced scanned images to computer-aided design models, and stereoscopic 3D display content. The telehealth domain explores the ICT for effective remote clinical services while using the streaming facilities offered by various low-bandwidth platforms. This domain allows offline or real-time interactive communication and collaboration for any dedicated clinical services. Many communication and streaming applications allow for remote one-to-one or group video calls and messaging, screen sharing, file sharing, hosting channels, and video broadcasting. Some of these platforms allow for direct AR and VR integration and acceptance. The file-sharing and other specific applications are synchronously and explicitly used as a sequential fragment of the entire system. The developed software from the studies mentioned in the table encapsulates the combination of AR and VR cooperatively with the remote telehealth applications.
Virtual Environment
A virtual environment (VE) recreates a coordinated appearance of sensory information representing that of a physical environment that can be unreal, interactive, or wholly imagined environment perceived when the user wears an appropriate gadget [152]. In addition, the term virtual worlds has been interchangeably used with a VE. Developing this state-of-the-art perceived environment is created using a subset of tools arising from computer game technology, specifically through commercial game engines. The scene can be a 2D or 3D illustration, which is a complex and time-consuming process for its creation [153]. This element of VE has been recreated in almost every aspect using the VR platform. For example, the study by Levy et al [125] demonstrated the use of virtual worlds such as a subway station and a 24-story high-rise building as background scenes to overcome acrophobia as a VR exposure therapy. Similarly, Cikajlo et al [127] developed a program called ReCoVR (Realizing Collaborative Virtual Reality for Well-being and Self-Healing). The participant attends a remote guided mindfulness program as part of a group. This mindfulness program was organized as 360° video scenes where they carried out different tasks and exercises. Initially, all the participants that joined were seated in the virtual fireplace room; upon the program’s progression, they were switched to other 3D VEs, such as the Dooney Rock, River Bonnet, or the mountain-view. Shao and Lee [132] have addressed a social VR platform that uses the 3D scenes in the VE for real-time face-to-face communication in different distant locations to learn about its value and urgency in the urban older adult population. Tamplin et al [72] developed a web-based music therapy telehealth platform using social VR, vTIME (vTime Limited), allowing group music therapy sessions in VE, such as singing around a campfire in a forest.
Gaming-Based VE
Moreover, many studies used VE in interactive game–based settings for rehabilitative exercise programs. In a program described by Meca-Lallana et al [53], patients were required to carry out specific tasks to accomplish a mission in 2 different scenes: a medieval fantasy world and a deserted island. Yet again, in another exercise setup, VR exercises depict a wooden church in Hrabova Roztoka. The patient explores this particular place using a VR headset, thereby facilitating lower-limb rehabilitation [36]. Telerehab VR, a custom-built application program that runs on either a mobile-based tablet or PC, was developed using the game engine Unity (Unity Technologies Inc). This system provides upper-limb rehabilitation for patients with multiple sclerosis. They perform various activities of daily living tasks happening in the VE in a realistic home setting. A leap motion controller (Ultraleap) was used to track and control the hand motion executed while performing the gaming tasks [48].
Telepresence
Telepresence describes the characteristic of directly interacting with the actual physical state, experienced from the first-person viewpoint of the user located remotely [154]. Tian et al [147] used the H-TIME (Haptic Enable Tele-Immersion Musculoskeletal Examination) set up at both the patient and doctor ends to conduct a remote diagnosis of musculoskeletal examination. At both sites, the doctor and patient could feel each other’s movements because of the bidirectional force feedback mechanism. They could view and communicate with each other in the VE, bringing them to the same examination room virtually. In another instance, in treating phobia, in particular, fear of spiders, the patients were allowed to interact in the VE, where the therapist gradually added the feared creature to the scene. This treatment is performed remotely via the tactile internet with VR headsets or standard computer screens using a hand-tracking and haptic device such as a glove [126].
Teleoperation refers to performing designated highly skilled manual tasks remotely, similar to a telerobotic medical system in minimally invasive surgery [155]. In a simulated study, an endoscopist performs a teleoperation process using a haptic device that controls the position of an external permanent magnet positioned at the end of a robotic arm. The user is wearing a VR headset and receives the corresponding visual information from the camera of the endoscopic capsule and then proceeds with the navigation process inside the colon [139]. Another simulated study used teleoperated ultrasonography that builds on the VE developed as a 3D representation of a real USG probe and a mannequin imitating a patient’s body highlighted with a geometric mesh for the purpose of following the examination. The user wears an Oculus Rift DK2 HMD (Oculus) to perform this simulation of tele-USG [148]. Syawaludin et al [150] introduced the use of 360° foveated pipeline imaging viewed via an HMD. The image or video capture is facilitated by the use of an omnidirectional pantilt-zoom camera module, and the remote physician can remotely diagnose the wound by zooming in and inspecting it in a 360◦ view over the HMD.
Exergaming and Serious Gaming via VR
In the context of virtual telerehabilitation, exergaming and serious games are the 2 most popular applications that emerge. Simply put, exergaming is an activity connected with playing video games that involve physical exercise [70]. In contrast, serious games follow the objective of games, implicitly focusing on increasing skills and abilities and gaining experience and knowledge [156]. The TELEKIN system, a beta edition, uses the interface of the serious game to rehabilitate cognitive and musculoskeletal disorders using a web-based framework [43]. The training sessions are conducted and played in a 3D VE that includes a number of games. Two of them involve physical actions—flexion and extension of wrist, hip, or shoulder as the doctor chooses to control the ball and platform in executing the game. Another game focuses on cognitive rehabilitation by featuring random words that the user must arrange them to form a sentence, which can be achieved using gesture-based controls [43]. Gandolfi et al [44] used the Tele Wii Lab platform as a home-based balance training, and Sheehy et al [28] and Allegue et al [30] used the Jintronix system (Jintronix, Inc) in upper-extremity rehabilitation of chronic poststroke patients, which used the exergaming platform. The study by Triandafilou et al [24] that developed a networked multiuser gaming format, Virtual Environment for Rehabilitative Gaming Exercise (VERGE), conducted a feasibility trial to determine the effectiveness of this developed system with other potential home treatments. The VERGE system features a set of 3 exercises, namely Ball Bump, where the users pass the ball back and forth across the table; Food Fight, where the users in multiplayer can pick up the food on the table and throw it at each other; and the Trajectory Trace game, where 1 player draws a trajectory path in the space while another player retraces the trajectory to erase it. Burdea et al [32] included a commercial rehabilitation system with a novel therapeutic game controller, BrightBrainer (Bright Cloud International Corp). This system offers a multitude of interactive games (Breakout 3D and Card Island Towers of Hanoi, among others), training motor, cognitive, and executive functions for chronic poststroke patients. Qiu et al [35] demonstrated the feasibility of a home-based VR system that features 12 developed games focusing on the elbow-shoulder, hand, wrist, and entire arm for upper-extremity rehabilitation in poststroke patients (finger games: car, bowling, and piano; hand games: piano and fruit picking; wrist games: Wakamole and wrist flying; and finally, the shoulder-elbow games: the Maze, Arm Flying, Brick Break, and soccer goalie)
Avatar Representations or Virtual Agents
The term avatar is a distinguishable digital characterization of a human form (either specific or random) [128]. Moreover, these avatars can be either in 2D or 3D illustration, representing a specific part of the body, usually arms or an entire body structure with particular facial expressions. 3D avatars have been a central representation in the scope of VR and AR. The study by Anton et al [59] implements the Kinect-based Telerehabilitation (ie, KiRES) interface, providing two 3D avatars to guide the patient during their physical therapy session. One of the avatars represents the remote therapist and represents the local user or the patient, colored red and blue, respectively, so the patient can follow and perform the exercises executed by the 3D remote therapist avatar (in red). The patient can see their movements reflected by their blue avatar changing their positions as per the scenes from the therapy. In the study trial conducted by Jung et al [74], in a telerehabilitation program—Pulmonary Rehabilitation in Virtual Reality (PR in VR) program—each patient was provided with a VR headset, pico G2 4k (Pico Immersive Pte Ltd), preloaded with the PR in VR application. This application contains education and rehabilitation modules, and the chronic obstructive pulmonary disorder rehabilitation module comprises several physical exercises directed by a virtual instructor in 3D avatar embodiment.
The REWIRE autonomous telerehabilitation platform offers home-based intensive rehabilitation as offline remote monitoring by hospital clinicians. This system features a virtual therapist with artificial intelligence implanted and provides real-time feedback to maintain correct posture. In addition, the exercises performed by the patients are showcased as a 3D avatar on the screen. This intelligent system highlights each body segment of the exercise in a different color, intense green for the proper posture and red color for the incorrect posture [23]. The VERGE system enables the use of avatars to control and manipulate objects in the virtual gaming environment, allowing the capability to include multiple avatars and different users to manipulate the same object [24]. In the social VR app, vTIME (vTime Limited), an avatar persona is used for self-characterization to communicate in an immersive VE [128]. Afyouni et al [65] describe the use of RehaBot, a virtual assistant that illustrates to the user how to perform the exercises correctly (both the therapist and patient can replay the session in a 3D avatar). The RehaBot embeds real-time pattern and gesture recognition together with a dynamic correction module that considers the game difficulty level and reading from the virtual assistant to produce a tailored set of exercises that are rather fitting to the patient’s native abilities.
Telestration and Annotations via AR and MR
Telestration enables the drawing of freehand representations, also known as annotations (such as lines, circles, or any other symbols or sketches) over any image or video feed. With the latest AR and MR technology, this telestration can be achieved in 2D and 3D and superimpose this annotation in the live video streaming during the video call [157]. The Virtual Interactive Presence and AR tool is a mobile or tablet-based augmented reality platform running on an iPad device (Apple). It incorporates the telestration feature, allowing the remote expert surgeon to freeze the screen and then draw an image using a 2D pen tool. This composite video feed, viewed on both the local and remote stations, enables intraoperative telecollaboration in real-time [90]. In the feasibility study by Wang et al [100], POCUS using the HoloLens was conducted by the trainee in a simulated teleconference session. The MR capture video from the trainee was broadcasted. Live guidance provided by the expert mentor facilitates the trainee to complete a right quadrant Focussed Assessment using Sonography in Trauma examination. The broadcasting was achieved using VSee, a proprietary low-bandwidth, group videoconferencing and screen-sharing application. To perform complex hand reconstruction of a patient after a bomb-blast injury, a telementoring network was established between an expert surgeon in Lebanon and a local surgeon in Gaza. This session was hosted using a cloud-based AR platform Proximie (Proximie Limited), allowing the remote surgeon to superimpose their own hands or range of annotations and drawing tools into the virtual surgical field [82].
Mitsuno et al [93] demonstrated telementoring in a simulation study to perform craniofacial surgery by using a teleconferencing setup, Skype (Microsoft Corp) for HoloLens, enabling the telestrated features and images overlaid on the receivers’ visual field. A POCUS examination was performed using a novel smartphone app Vuforia Chalk (PTC Inc), an AR video platform for remote AR assistance, anchoring the AR annotations in each other’s supposed visual environment [151]. In the study, Ritcher et al [141] proposed the first predictive display with AR registration and rendering using stereoscopic displays designed for teleoperated surgical robots known as Stereoscopic AR Predictive Display. The simulation study measured the effectiveness of Stereoscopic AR Predictive Display conducted on the da Vinci R Surgical System (Intuitive Surgical) to complete the peg transfer task. The System for Telementoring with AR (STAR) platform now combines optical see-through display, HoloLens AR HMD. Similarly, this system allows for telementoring guidance by overlaying 3D graphical annotations onto the mentee’s view of the surgical field, which remains anchored in the same place even after the mentee moves their head position [95].
The experiment by Zhang et al [110] aimed to enhance teleconsultation by using the AR technology ARkit (Apple) to create an immersive replica of the consultant. Using a Kinect sensor (Microsoft Corp) to capture the skeletal feature points of the consultant, the patient views a 3D dynamic virtual avatar doctor appearing in the patient’s telepresence environment on their iPad device. A qualitative study was conducted to gain the experience and perception of AR Glasses in patients with pulmonary disorders for home-based telerehabilitation. The web-based telerehabilitation system Optimov (Optimov) enabled via an AR Glasses device Laster WAVƎ headset (Laster Technologies) provides exercise coaching using a 3D virtual agent [73]. A holographic virtual therapist was deployed in the HOLOBALANCE, a novel health care platform for providing vestibular rehabilitation therapy for patients with balance disorders [158]. In the design and evaluation user study by Kowatsch et al [119], a hybrid ubiquitous coaching model relying on mobile and holographic conversation agents was introduced. The 3D virtual conversation agent demonstrated the squat exercise, engaging in real-time audio feedback for counting the repetition or providing automatic error detection for incorrectly or incompletely following the exercise. An innovative 3D point tracking module and unique AR system integrated with the HoloLens was used for surgical applications using telementoring. This module allowed for real-time 3D position tracking of the virtual scalpel handled by an experienced surgeon remotely. The inexperienced trainee wearing the HoloLens can see the surgical annotation superimposed with the actual surgical scene; the virtual path coregistered on the phantom arm model [78]. Next-generation mobile-based AR games for pediatric health care allow shared experiences with multiple other AR-supported devices to detect and interact using the same local area network. Several games were developed using the Unity game engine and ARCore Unity, a software development kit for Android operating software. Jungle Adventure, Map explorer, and Wakamole implemented AR interaction, whereas Map explorer and Wakamole particularly enabled the inclusion of a 2-player for a shared collaborative experience [118].
First-Person View for AR Capture Video Feed
Noorian et al [102] demonstrated smart reality glasses to conduct remote consultation using the National Institutes of Health Stroke Scale scores for stroke assessment. The onsite doctor wears the reality glass, Google glass. This Google glass is embedded with the Xpert Eye platform (AMA XpertEye), capable of assisted reality, allowing the person wearing this device to share their field of view in a 2-way real-time videoconferencing. Similarly, Nikouline et al [123] presented a feasibility study using the Google glass live video stream coming from the onsite proctor and the participant tasks related to fundamentals of Laparoscopy for scoring and evaluation done by the remote proctor. In their experiment, Lin et al [84] implement projective video texture-mapping that supplements a robust high-level stabilization video feed obtained from the mentee’s first-person view. This effective format provides the remote expert with an effective workspace visualization, allowing seamless integration of annotations in an effective AR surgical telementoring. The prospective observational study by Martin et al [103] uses HoloLens 2 MR device to conduct remote clinical consultation in a COVID-19 ward. A senior staff member would enter the COVID-19 ward to undertake clinical rounds, and the other staff members of the staff team would join virtually, thereby minimizing exposure and infection transmission. Dynamic 365 Remote Assist (Microsoft Corp) software allowed for bidirectional audio and video functionality through which the remote staff team could see the first-person view from the HoloLens 2 device. In addition, this platform allowed to place relevant imaging and electronic health record data in the user field of view, improving situational awareness and better clinical decision-making. Finally, it significantly reduced the risk of direct viral transmission.
Web- and Cloud-Based Telehealth Delivery Modes
As digital communication network and services evolve, these are rapidly being adopted in health care delivery. The web- and cloud-based applications have become prevalent in telehealth. Telehealth relies on the backbone of internet infrastructure supported using various broadband connections such as digital subscriber lines, fiber broadband, and wireless connection, including fixed wireless broadband, cellular network or mobile broadband, and satellite communication. Thus, ICT has become central to offering an array of digital health solutions such as real-time audio and videoconferencing, remote patient monitoring, store and forward technologies, and mobile health, among others [159,160]. A web-based application principally operates on the webserver. It is accessed through a web browser over an internet connection, whereas cloud-based applications operate similarly to web applications, operating on either or both the client and server sides [161]. The custom-developed systems KiRES [59] and STAR [85] rely on the WebRTC framework, an open-source application programing interface allowing for real-time audio-video and multimedia connection. In addition, the study by da Silva et al [55], included a web-based gaming application MoveHero, to evaluate the feasibility of home-based nonimmersive serious games in patients with cerebral palsy.
Interestingly, any virtual web-based application feeds on the information; thus, data storage and hosting become integral to all online services. The study by Kato et al [42], adopted the cloud-based storage and file hosting service Dropbox (Dropbox Inc) for collecting the spatial coordinate data for each joint using the 3D optical camera during the VR telerehabilitation. The proof-of-concept study by Sirilak et al [107], implemented an e-consultation system based on the AR and MR systems using the HoloLens device for remote consultancy services in the intensive care environment. This e-consultation platform depended on a cloud-based data center that performed as an information exchange and provided services for the end devices. It also consisted of body area network technology to integrate the vital physiological information from different client devices to the data center. Prvu Bettger et al [62], used a virtual telehealth system—virtual exercise rehabilitation assistant or virtual exercise rehabilitation assistant (Reflexion Health, Inc)—for posthospital care for total knee arthroplasty, Tsiouris et al [2] included a custom-developed platform HOLOBALANCE system in managing balance disorders, both using the technology-forward cloud-based platform.
Discussion
Principal Findings
This scoping review explores state-of-the-art extended reality platforms and telehealth solutions used in the clinical context. This review highlights the reported evidence-based practical and probable applications of the extended and MR platform with telehealth used in different clinical specialties. This review also addresses the technical characteristics of the AR and VR features used in telehealth services, including various hardware and software arrangements.
Stroke is the leading clinical condition incorporating telerehabilitation, a segment of the telehealth service and digital VR [23-41]. Approximately half of the included studies from the search strategy feature the use of telerehabilitation (Figure 4). Other clinical conditions such as neurological or cognitive disorders, musculoskeletal conditions, and postsurgical recovery have also adopted telerehabilitation facilities in the home or remote settings to continue treatment. Telerehabilitation used technical attributes of exergaming and serious gaming in improving the motor and cognitive functional skills [43-58].
Other divisions of telehealth, namely telementoring, teleconsultation, and telemonitoring, have been more frequently used for surgical-related procedures, emergencies and trauma, and in several disaster simulation for disaster response and preparedness [162]. The AR and MR technologies are more prevalent with telementoring, teleconsultation, and telesurgery (Figure 3). Exposure therapy under telepsychiatry has used VR to give the patient a photorealistic experience of overcoming their pathological response to their fear [126].
Telestrated AR features through anchoring of annotations in real-time and space, performed remotely via various communication channels: a useful aid in telesurgery [81]. The technical features from the digital reality technology of VE, digital avatars, telestration or the 3D rendering of annotations, and first-person viewpoint have demonstrated telemedical capabilities. The web- and cloud-based applications have various potential uses across the web-based clinical sphere [110]. Most of the included studies relied on existing commercial high-fidelity simulation technological hardware devices such as head-mounted AR and VR displays. The study and software designs for most of the included studies were codeveloped by the respective research teams by using multiple supportive platforms as a direct requirement for the project objectives.
These novel reality technologies of AR, VR, and MR enable 3D visualization, thereby creating a visual sense and experience of high ecological validity [163]. This technology has been extended as a remote, home-based solution for patients, thereby enabling patient empowerment [164]. This technology is highly engaging and motivating from the patient responses to telerehabilitation, consequently necessitating initial patient training needs may become an arduous task to the facilitator [42,165]. Network connectivity, internet and server security concerns, and technological constraints are some of the most common pitfalls across several studies included in this review [99,166]. The lack of interoperability between the hardware and software platforms poses a significant challenge in realizing the potential of this technology [2]. The need for improved network infrastructure and scalability poses a challenge and target for telehealth services; however, there is a risk of complete network failure, which can affect the use of such systems in critical care applications [83]. Patient confidentiality is integral at any stage during electronic exchange of health-related data; thus, network and data security protection are crucial factors for accessing telehealth services and should be robustly adhered to the governing regulations [66,149,167].
The exploded search strategy captures a broad array of important clinical applications of this high-fidelity reality technology and telehealth facilities. This review presents a current road map and the prospects of digital reality technology and telehealth in the clinical space. The determining factors presented allow the readers and researchers to evaluate the relevance of this technology and its subsequent uptake in the clinical health sector. The study protocol was not registered, the included studies were not classified for risk of bias assessment, and the general characterization for the included studies were not presented. In addition, the review only included studies available in the English language and no relevant additional pieces of information was considered from the gray literature. From the broad array of literature-based evidence, most of the included experimental studies were pilot feasibility studies with small sample sizes, leading to reporting bias.
Conclusions
This review uniquely details the current and potential applications of digital reality technologies such as VR and AR and telehealth solutions. The feasible and practical application of AR and VR in the digital clinical space has been explored, as well as the challenges this multiparty technology endures in effective implementation and adoption. This suite of technologies offers a collaborative experience among health care professionals and their patient community. The telehealth component with the high-fidelity digital reality allows for an immersive and integrative means for teleconsultation, telesurgical procedures, and telementoring among the medical peer-to-peer group allowing for effective decision-making and treatment approaches. The uptake of VR and exergaming in various telerehabilitation programs has opened new avenues to posttreatment measures. This essential application of telehealth enhances the traditional health care delivery approach by enabling remotely delivered clinical care and services and developing home-based treatment programs. Further validated studies are needed to evaluate the overall assessment of this trending technology, thereby leading to commercial pathways. A robust and secure communication infrastructure will improve the accessibility of telehealth capabilities and extend the interoperability of the digital reality platform allowing for a diverse digital health care ecosystem.
Acknowledgments
This review was supported by the Science Foundation Ireland under grants (13/RC/2073) and (13/RC/2094). The authors would like to thank the university librarian, Rosie Dunne, for providing feedback on the search strategy and helping in finding the appropriate databases to conduct the search in.
Abbreviations
- AR
augmented reality
- HMD
head-mounted display
- H-TIME
Haptic Enable Tele-Immersion Musculoskeletal Examination
- ICT
information and communication technology
- LCD
liquid crystal display
- LED
light emitting diode
- MR
mixed reality
- POCUS
point-of-focus ultrasonography
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews
- REBOA
resuscitative endovascular balloon occlusion of the aorta
- ReCoVR
Realizing Collaborative virtual reality for well-being and self-healing
- STAR
System for Telementoring with Augmented Reality
- USG
ultrasonography
- VE
virtual environment
- VERGE
Virtual Environment for Rehabilitative Gaming Exercise
- VR
virtual reality
Search strategy.
Augmented, virtual, and mixed reality hardware devices.
Other relative hardware devices.
List of software and source platforms.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Anthony Jr B. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020 Jun 15;44(7):132. doi: 10.1007/s10916-020-01596-5. https://europepmc.org/abstract/MED/32542571 .10.1007/s10916-020-01596-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsiouris KM, Gatsios D, Tsakanikas V, Pardalis AA, Kouris I, Androutsou T, Tarousi M, Vujnovic Sedlar N, Somarakis I, Mostajeran F, Filipovic N, op den Akker H, Koutsouris DD, Fotiadis DI. Designing interoperable telehealth platforms: bridging IoT devices with cloud infrastructures. Enterp Inf Syst. 2020 Apr 30;14(8):1194–218. doi: 10.1080/17517575.2020.1759146. [DOI] [Google Scholar]
- 3.Telehealth and Telemedicine. American Academy of Family Physicians. [2021-12-01]. https://www.aafp.org/about/policies/all/telehealth-telemedicine.html .
- 4.Telehealth market revenue, growth. Fortune Business Insights. [2022-07-25]. https://www.fortunebusinessinsights.com/industry-reports/toc/telehealth-market-101065# .
- 5.Milgram P, Takemura H, Utsumi A, Kishino F. Augmented reality: a class of displays on the reality-virtuality continuum. Proceedings of the 1994 SPIE Conference on Telemanipulator and Telepresence Technologies; SPIE '94; October 31-November 4, 1994; Boston, MA, USA. 1994. [DOI] [Google Scholar]
- 6.Verhey JT, Haglin JM, Verhey EM, Hartigan DE. Virtual, augmented, and mixed reality applications in orthopedic surgery. Int J Med Robot. 2020 Apr;16(2):e2067. doi: 10.1002/rcs.2067. [DOI] [PubMed] [Google Scholar]
- 7.Yeung AW, Tosevska A, Klager E, Eibensteiner F, Laxar D, Stoyanov J, Glisic M, Zeiner S, Kulnik ST, Crutzen R, Kimberger O, Kletecka-Pulker M, Atanasov AG, Willschke H. Virtual and augmented reality applications in medicine: analysis of the scientific literature. J Med Internet Res. 2021 Feb 10;23(2):e25499. doi: 10.2196/25499. https://boris.unibe.ch/id/eprint/152396 .v23i2e25499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Venkatesan M, Mohan H, Ryan JR, Schürch CM, Nolan GP, Frakes DH, Coskun AF. Virtual and augmented reality for biomedical applications. Cell Rep Med. 2021 Jul 20;2(7):100348. doi: 10.1016/j.xcrm.2021.100348. https://linkinghub.elsevier.com/retrieve/pii/S2666-3791(21)00197-X .S2666-3791(21)00197-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lungu AJ, Swinkels W, Claesen L, Tu P, Egger J, Chen X. A review on the applications of virtual reality, augmented reality and mixed reality in surgical simulation: an extension to different kinds of surgery. Expert Rev Med Devices. 2021 Jan;18(1):47–62. doi: 10.1080/17434440.2021.1860750. [DOI] [PubMed] [Google Scholar]
- 10.Chen FQ, Leng YF, Ge JF, Wang DW, Li C, Chen B, Sun ZL. Effectiveness of virtual reality in nursing education: meta-analysis. J Med Internet Res. 2020 Sep 15;22(9):e18290. doi: 10.2196/18290. https://www.jmir.org/2020/9/e18290/ v22i9e18290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eckert M, Volmerg JS, Friedrich CM. Augmented reality in medicine: systematic and bibliographic review. JMIR Mhealth Uhealth. 2019 Apr 26;7(4):e10967. doi: 10.2196/10967. https://mhealth.jmir.org/2019/4/e10967/ v7i4e10967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han J, Kang HJ, Kim M, Kwon GH. Mapping the intellectual structure of research on surgery with mixed reality: bibliometric network analysis (2000-2019) J Biomed Inform. 2020 Sep;109:103516. doi: 10.1016/j.jbi.2020.103516. https://linkinghub.elsevier.com/retrieve/pii/S1532-0464(20)30144-1 .S1532-0464(20)30144-1 [DOI] [PubMed] [Google Scholar]
- 13.Dadario NB, Quinoa T, Khatri D, Boockvar J, Langer D, D'Amico RS. Examining the benefits of extended reality in neurosurgery: a systematic review. J Clin Neurosci. 2021 Dec;94:41–53. doi: 10.1016/j.jocn.2021.09.037.S0967-5868(21)00493-8 [DOI] [PubMed] [Google Scholar]
- 14.Dellazizzo L, Potvin S, Luigi M, Dumais A. Evidence on virtual reality-based therapies for psychiatric disorders: meta-review of meta-analyses. J Med Internet Res. 2020 Aug 19;22(8):e20889. doi: 10.2196/20889. https://www.jmir.org/2020/8/e20889/ v22i8e20889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu J, Zeng A, Chen Z, Wei Y, Huang K, Chen J, Ren Z. Effects of virtual reality training on upper limb function and balance in stroke patients: systematic review and meta-meta-analysis. J Med Internet Res. 2021 Oct 12;23(10):e31051. doi: 10.2196/31051. https://www.jmir.org/2021/10/e31051/ v23i10e31051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Q, Fu Y, Lu Y, Zhang Y, Huang Q, Yang Y, Zhang K, Li M. Impact of virtual reality-based therapies on cognition and mental health of stroke patients: systematic review and meta-analysis. J Med Internet Res. 2021 Nov 17;23(11):e31007. doi: 10.2196/31007. https://www.jmir.org/2021/11/e31007/ v23i11e31007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018 Oct 02;169(7):467–73. doi: 10.7326/M18-0850. https://www.acpjournals.org/doi/abs/10.7326/M18-0850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .2700389 [DOI] [PubMed] [Google Scholar]
- 18.Gilbert B. Microsoft's ambitious HoloLens headset ships on March 30. Insider. 2016. Feb 29, [2022-10-30]. https://www.businessinsider.com/hololens-release-date-march-30-2016-2 .
- 19.Kim K, Billinghurst M, Bruder G, Duh HB, Welch GF. Revisiting trends in augmented reality research: a review of the 2nd decade of ISMAR (2008-2017) IEEE Trans Vis Comput Graph. 2018 Nov;24(11):2947–62. doi: 10.1109/TVCG.2018.2868591. [DOI] [PubMed] [Google Scholar]
- 20.Falconer J. Removing duplicates from an EndNote library. London School of Hygiene and Tropical Medicine. 2018. Dec 7, [2022-07-25]. https://blogs.lshtm.ac.uk/library/2018/12/07/removing-duplicates-from-an-endnote-library/
- 21.Kairy D, Veras M, Archambault P, Hernandez A, Higgins J, Levin MF, Poissant L, Raz A, Kaizer F. Maximizing post-stroke upper limb rehabilitation using a novel telerehabilitation interactive virtual reality system in the patient's home: study protocol of a randomized clinical trial. Contemp Clin Trials. 2016 Mar;47:49–53. doi: 10.1016/j.cct.2015.12.006.S1551-7144(15)30136-1 [DOI] [PubMed] [Google Scholar]
- 22.Aloyuni S, Alharbi R, Kashoo F, Alqahtani M, Alanazi A, Alzhrani M, Ahmad M. Knowledge, attitude, and barriers to telerehabilitation-based physical therapy practice in Saudi Arabia. Healthcare (Basel) 2020 Nov 04;8(4):460. doi: 10.3390/healthcare8040460. https://www.mdpi.com/resolver?pii=healthcare8040460 .healthcare8040460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Held JP, Ferrer B, Mainetti R, Steblin A, Hertler B, Moreno-Conde A, Dueñas A, Pajaro M, Parra-Calderón CL, Vargiu E, Josè Zarco M, Barrera M, Echevarria C, Jódar-Sánchez F, Luft AR, Borghese NA. Autonomous rehabilitation at stroke patients home for balance and gait: safety, usability and compliance of a virtual reality system. Eur J Phys Rehabil Med. 2018 Aug;54(4):545–53. doi: 10.23736/S1973-9087.17.04802-X. https://air.unimi.it/handle/2434/553392 .S1973-9087.17.04802-X [DOI] [PubMed] [Google Scholar]
- 24.Triandafilou KM, Tsoupikova D, Barry AJ, Thielbar KN, Stoykov N, Kamper DG. Development of a 3D, networked multi-user virtual reality environment for home therapy after stroke. J Neuroeng Rehabil. 2018 Oct 05;15(1):88. doi: 10.1186/s12984-018-0429-0. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-018-0429-0 .10.1186/s12984-018-0429-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou RJ, Hondori HM, Khademi M, Cassidy JM, Wu KM, Yang DZ, Kathuria N, Erani FR, Dodakian L, McKenzie A, Lopes CV, Scacchi W, Srinivasan R, Cramer SC. Predicting gains with visuospatial training after stroke using an EEG measure of frontoparietal circuit function. Front Neurol. 2018 Jul 24;9:597. doi: 10.3389/fneur.2018.00597. https://digitalcommons.chapman.edu/pt_articles/71/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fluet GG, Qiu Q, Patel J, Cronce A, Merians AS, Adamovich SV. Autonomous use of the home virtual rehabilitation system: a feasibility and pilot study. Games Health J. 2019 Dec;8(6):432–8. doi: 10.1089/g4h.2019.0012. https://europepmc.org/abstract/MED/31769724 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maresca G, Maggio MG, Latella D, Cannavò A, De Cola MC, Portaro S, Stagnitti MC, Silvestri G, Torrisi M, Bramanti A, De Luca R, Calabrò RS. Toward improving poststroke aphasia: a pilot study on the growing use of telerehabilitation for the continuity of care. J Stroke Cerebrovasc Dis. 2019 Oct;28(10):104303. doi: 10.1016/j.jstrokecerebrovasdis.2019.104303.S1052-3057(19)30344-1 [DOI] [PubMed] [Google Scholar]
- 28.Sheehy L, Taillon-Hobson A, Sveistrup H, Bilodeau M, Yang C, Welch V, Hossain A, Finestone H. Home-based virtual reality training after discharge from hospital-based stroke rehabilitation: a parallel randomized feasibility trial. Trials. 2019 Jun 07;20(1):333. doi: 10.1186/s13063-019-3438-9. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-019-3438-9 .10.1186/s13063-019-3438-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Torrisi M, Maresca G, De Cola MC, Cannavò A, Sciarrone F, Silvestri G, Bramanti A, De Luca R, Calabrò RS. Using telerehabilitation to improve cognitive function in post-stroke survivors: is this the time for the continuity of care? Int J Rehabil Res. 2019 Dec;42(4):344–51. doi: 10.1097/MRR.0000000000000369. [DOI] [PubMed] [Google Scholar]
- 30.Allegue DR, Kairy D, Higgins J, Archambault P, Michaud F, Miller W, Sweet SN, Tousignant M. Optimization of upper extremity rehabilitation by combining telerehabilitation with an exergame in people with chronic stroke: protocol for a mixed methods study. JMIR Res Protoc. 2020 May 21;9(5):e14629. doi: 10.2196/14629. https://www.researchprotocols.org/2020/5/e14629/ v9i5e14629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amorim P, Santos BS, Dias P, Silva S, Martins H. Serious games for stroke telerehabilitation of upper limb - a review for future research. Int J Telerehabil. 2020 Dec 08;12(2):65–76. doi: 10.5195/ijt.2020.6326. https://europepmc.org/abstract/MED/33520096 .ijt.2020.6326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Burdea GC, Grampurohit N, Kim N, Polistico K, Kadaru A, Pollack S, Oh-Park M, Barrett A, Kaplan E, Masmela J, Nori P. Feasibility of integrative games and novel therapeutic game controller for telerehabilitation of individuals chronic post-stroke living in the community. Top Stroke Rehabil. 2020 Jul;27(5):321–36. doi: 10.1080/10749357.2019.1701178. https://europepmc.org/abstract/MED/31875775 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim WS, Cho S, Ku J, Kim Y, Lee K, Hwang HJ, Paik NJ. Clinical application of virtual reality for upper limb motor rehabilitation in stroke: review of technologies and clinical evidence. J Clin Med. 2020 Oct 21;9(10):3369. doi: 10.3390/jcm9103369. https://www.mdpi.com/resolver?pii=jcm9103369 .jcm9103369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klaic M, Galea MP. Using the technology acceptance model to identify factors that predict likelihood to adopt tele-neurorehabilitation. Front Neurol. 2020 Dec 2;11:580832. doi: 10.3389/fneur.2020.580832. https://europepmc.org/abstract/MED/33343488 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Qiu Q, Cronce A, Patel J, Fluet GG, Mont AJ, Merians AS, Adamovich SV. Development of the Home based Virtual Rehabilitation System (HoVRS) to remotely deliver an intense and customized upper extremity training. J Neuroeng Rehabil. 2020 Nov 23;17(1):155. doi: 10.1186/s12984-020-00789-w. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-020-00789-w .10.1186/s12984-020-00789-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sramka M, Lacko J, Ruzicky E, Masan J. Combined methods of rehabilitation of patients after stroke: virtual reality and traditional approach. Neuro Endocrinol Lett. 2020 Sep;41(3):123–33.NEL410320A02 [PubMed] [Google Scholar]
- 37.Thielbar KO, Triandafilou KM, Barry AJ, Yuan N, Nishimoto A, Johnson J, Stoykov ME, Tsoupikova D, Kamper DG. Home-based upper extremity stroke therapy using a multiuser virtual reality environment: a randomized trial. Arch Phys Med Rehabil. 2020 Feb;101(2):196–203. doi: 10.1016/j.apmr.2019.10.182.S0003-9993(19)31365-6 [DOI] [PubMed] [Google Scholar]
- 38.Allegue DR, Kairy D, Higgins J, Archambault PS, Michaud F, Miller WC, Sweet SN, Tousignant M. A personalized home-based rehabilitation program using exergames combined with a telerehabilitation app in a chronic stroke survivor: mixed methods case study. JMIR Serious Games. 2021 Aug 31;9(3):e26153. doi: 10.2196/26153. https://games.jmir.org/2021/3/e26153/ v9i3e26153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jonsdottir J, Baglio F, Gindri P, Isernia S, Castiglioni C, Gramigna C, Palumbo G, Pagliari C, Di Tella S, Perini G, Bowman T, Salza M, Molteni F. Virtual reality for motor and cognitive rehabilitation from clinic to home: a pilot feasibility and efficacy study for persons with chronic stroke. Front Neurol. 2021 Apr 7;12:601131. doi: 10.3389/fneur.2021.601131. https://europepmc.org/abstract/MED/33897579 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ostrowska PM, Śliwiński M, Studnicki R, Hansdorfer-Korzon R. Telerehabilitation of post-stroke patients as a therapeutic solution in the era of the COVID-19 pandemic. Healthcare (Basel) 2021 May 31;9(6):654. doi: 10.3390/healthcare9060654. https://www.mdpi.com/resolver?pii=healthcare9060654 .healthcare9060654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferreira B, Menezes P. Gamifying motor rehabilitation therapies: challenges and opportunities of immersive technologies. Information. 2020 Feb 07;11(2):88. doi: 10.3390/info11020088. https://www.mdpi.com/2078-2489/11/2/88 . [DOI] [Google Scholar]
- 42.Kato N, Tanaka T, Sugihara S, Shimizu K, Kudo N. Trial operation of a cloud service-based three-dimensional virtual reality tele-rehabilitation system for stroke patients. Proceedings of the 11th International Conference on Computer Science & Education; ICCSE '16; August 23-25, 2016; Nagoya, Japan. 2016. pp. 285–90. [DOI] [Google Scholar]
- 43.Caminero RV, Méndez-Herrero LA, Diaz-Pernasl FJ, del Campo JC, Rodriguez MA, Martinez-Zarzuelal M. Telekin - tele-rehabilitation system for musculoskeletal and cognitive disorders using natural movement interface devices. Proceedings of the 3rd International Conference on Information and Communication Technologies for Ageing Well and e-Health; ICT4AWE '17; April 28-29, 2017; Porto, Portugal. 2017. pp. 198–203. [DOI] [Google Scholar]
- 44.Gandolfi M, Geroin C, Dimitrova E, Boldrini P, Waldner A, Bonadiman S, Picelli A, Regazzo S, Stirbu E, Primon D, Bosello C, Gravina AR, Peron L, Trevisan M, Garcia AC, Menel A, Bloccari L, Valè N, Saltuari L, Tinazzi M, Smania N. Virtual reality telerehabilitation for postural instability in Parkinson's disease: a multicenter, single-blind, randomized, controlled trial. Biomed Res Int. 2017;2017:7962826. doi: 10.1155/2017/7962826. doi: 10.1155/2017/7962826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O'Neil O, Fernandez MM, Herzog J, Beorchia M, Gower V, Gramatica F, Starrost K, Kiwull L. Virtual reality for neurorehabilitation: insights from 3 European clinics. PM R. 2018 Sep;10(9 Suppl 2):S198–206. doi: 10.1016/j.pmrj.2018.08.375.S1934-1482(18)30809-8 [DOI] [PubMed] [Google Scholar]
- 46.Keshner EA, Weiss PT, Geifman D, Raban D. Tracking the evolution of virtual reality applications to rehabilitation as a field of study. J Neuroeng Rehabil. 2019 Jun 21;16(1):76. doi: 10.1186/s12984-019-0552-6. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-019-0552-6 .10.1186/s12984-019-0552-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Isernia S, Di Tella S, Pagliari C, Jonsdottir J, Castiglioni C, Gindri P, Salza M, Gramigna C, Palumbo G, Molteni F, Baglio F. Effects of an innovative telerehabilitation intervention for people with Parkinson's disease on quality of life, motor, and non-motor abilities. Front Neurol. 2020 Aug 13;11:846. doi: 10.3389/fneur.2020.00846. https://europepmc.org/abstract/MED/32903506 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kalron A, Achiron A, Pau M, Cocco E. The effect of a telerehabilitation virtual reality intervention on functional upper limb activities in people with multiple sclerosis: a study protocol for the TEAMS pilot randomized controlled trial. Trials. 2020 Aug 12;21(1):713. doi: 10.1186/s13063-020-04650-2. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-04650-2 .10.1186/s13063-020-04650-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Manenti R, Gobbi E, Baglio F, Macis A, Ferrari C, Pagnoni I, Rossetto F, Di Tella S, Alemanno F, Cimino V, Binetti G, Iannaccone S, Bramanti P, Cappa SF, Cotelli M. Effectiveness of an innovative cognitive treatment and telerehabilitation on subjects with mild cognitive impairment: a multicenter, randomized, active-controlled study. Front Aging Neurosci. 2020 Nov 16;12:585988. doi: 10.3389/fnagi.2020.585988. https://europepmc.org/abstract/MED/33304267 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mantovani E, Zucchella C, Bottiroli S, Federico A, Giugno R, Sandrini G, Chiamulera C, Tamburin S. Telemedicine and virtual reality for cognitive rehabilitation: a roadmap for the COVID-19 pandemic. Front Neurol. 2020 Sep 15;11:926. doi: 10.3389/fneur.2020.00926. https://europepmc.org/abstract/MED/33041963 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maresca G, Maggio MG, De Luca R, Manuli A, Tonin P, Pignolo L, Calabrò RS. Tele-neuro-rehabilitation in Italy: state of the art and future perspectives. Front Neurol. 2020 Sep 30;11:563375. doi: 10.3389/fneur.2020.563375. https://europepmc.org/abstract/MED/33101176 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matamala-Gomez M, Maisto M, Montana JI, Mavrodiev PA, Baglio F, Rossetto F, Mantovani F, Riva G, Realdon O. The role of engagement in teleneurorehabilitation: a systematic review. Front Neurol. 2020 May 6;11:354. doi: 10.3389/fneur.2020.00354. https://europepmc.org/abstract/MED/32435227 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Meca-Lallana V, Prefasi D, Alabarcez W, Hernández T, García-Vaz F, Portaña A, Gomis D, Téllez N, García-Bernáldez C, Mauriño J, Medrano N, Vázquez-Doce A. A pilot study to explore patient satisfaction with a virtual rehabilitation program in multiple sclerosis: the RehabVR study protocol. Front Neurol. 2020 Aug 21;11:900. doi: 10.3389/fneur.2020.00900. https://europepmc.org/abstract/MED/33162924 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stasolla F, Matamala-Gomez M, Bernini S, Caffò AO, Bottiroli S. Virtual reality as a technological-aided solution to support communication in persons with neurodegenerative diseases and acquired brain injury during COVID-19 pandemic. Front Public Health. 2020 Feb 16;8:635426. doi: 10.3389/fpubh.2020.635426. https://europepmc.org/abstract/MED/33665181 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.da Silva TD, da Silva PL, de Jesus Valenzuela E, Dias ED, Simcsik AO, de Carvalho MG, Fontes AM, de Oliveira Alberissi CA, de Araújo LV, da Costa Brandão MV, Dawes H, de Mello Monteiro CB. Serious game platform as a possibility for home-based telerehabilitation for individuals with cerebral palsy during COVID-19 quarantine - a cross-sectional pilot study. Front Psychol. 2021 Feb 02;12:622678. doi: 10.3389/fpsyg.2021.622678. https://europepmc.org/abstract/MED/33633648 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Langer A, Gassner L, Flotz A, Hasenauer S, Gruber J, Wizany L, Pokan R, Maetzler W, Zach H. How COVID-19 will boost remote exercise-based treatment in Parkinson's disease: a narrative review. NPJ Parkinsons Dis. 2021 Mar 08;7(1):25. doi: 10.1038/s41531-021-00160-3. doi: 10.1038/s41531-021-00160-3.10.1038/s41531-021-00160-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lasaponara S, Marson F, Doricchi F, Cavallo M. A scoping review of cognitive training in neurodegenerative diseases via computerized and virtual reality tools: what we know so far. Brain Sci. 2021 Apr 21;11(5):528. doi: 10.3390/brainsci11050528. https://www.mdpi.com/resolver?pii=brainsci11050528 .brainsci11050528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Varela-Aldás J, Buele J, Ramos Lorente P, García-Magariño I, Palacios-Navarro G. A virtual reality-based cognitive telerehabilitation system for use in the COVID-19 pandemic. Sustainability. 2021 Feb 18;13(4):2183. doi: 10.3390/su13042183. https://www.mdpi.com/2071-1050/13/4/2183 . [DOI] [Google Scholar]
- 59.Anton D, Berges I, Bermúdez J, Goñi A, Illarramendi A. A telerehabilitation system for the selection, evaluation and remote management of therapies. Sensors (Basel) 2018 May 08;18(5):1459. doi: 10.3390/s18051459. https://www.mdpi.com/resolver?pii=s18051459 .s18051459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang X, Hunter DJ, Vesentini G, Pozzobon D, Ferreira ML. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019 Nov 03;20(1):506. doi: 10.1186/s12891-019-2900-x. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-019-2900-x .10.1186/s12891-019-2900-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Berton A, Longo UG, Candela V, Fioravanti S, Giannone L, Arcangeli V, Alciati V, Berton C, Facchinetti G, Marchetti A, Schena E, De Marinis MG, Denaro V. Virtual reality, augmented reality, gamification, and telerehabilitation: psychological impact on orthopedic patients' rehabilitation. J Clin Med. 2020 Aug 07;9(8):2567. doi: 10.3390/jcm9082567. https://www.mdpi.com/resolver?pii=jcm9082567 .jcm9082567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Prvu Bettger J, Green CL, Holmes DN, Chokshi A, Mather 3rd RC, Hoch BT, de Leon AJ, Aluisio F, Seyler TM, Del Gaizo DJ, Chiavetta J, Webb L, Miller V, Smith JM, Peterson ED. Effects of virtual exercise rehabilitation in-home therapy compared with traditional care after total knee arthroplasty: VERITAS, a randomized controlled trial. J Bone Joint Surg Am. 2020 Jan 15;102(2):101–9. doi: 10.2106/JBJS.19.00695.00004623-202001150-00002 [DOI] [PubMed] [Google Scholar]
- 63.Borresen A, Wolfe C, Lin CK, Tian Y, Raghuraman S, Nahrstedt K, Prabhakaran B, Annaswamy T. Usability of an immersive augmented reality based telerehabilitation system with haptics (ARTESH) for synchronous remote musculoskeletal examination. Int J Telerehabil. 2019 Jun 12;11(1):23–32. doi: 10.5195/ijt.2019.6275. https://europepmc.org/abstract/MED/31341544 .ijt-11-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rothgangel A, Braun S, Smeets R, Beurskens A. Feasibility of a traditional and teletreatment approach to mirror therapy in patients with phantom limb pain: a process evaluation performed alongside a randomized controlled trial. Clin Rehabil. 2019 Oct;33(10):1649–60. doi: 10.1177/0269215519846539. [DOI] [PubMed] [Google Scholar]
- 65.Afyouni I, Murad A, Einea A. Adaptive rehabilitation bots in serious games. Sensors (Basel) 2020 Dec 09;20(24):7037. doi: 10.3390/s20247037. https://www.mdpi.com/resolver?pii=s20247037 .s20247037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Birckhead B, Eberlein S, Alvarez G, Gale R, Dupuy T, Makaroff K, Fuller G, Liu X, Yu KS, Black JT, Ishimori M, Venuturupalli S, Tu J, Norris T, Tighiouart M, Ross L, McKelvey K, Vrahas M, Danovitch I, Spiegel B. Home-based virtual reality for chronic pain: protocol for an NIH-supported randomised-controlled trial. BMJ Open. 2021 Jun 15;11(6):e050545. doi: 10.1136/bmjopen-2021-050545. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=34130965 .bmjopen-2021-050545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Logan DE, Simons LE, Caruso TJ, Gold JI, Greenleaf W, Griffin A, King CD, Menendez M, Olbrecht VA, Rodriguez S, Silvia M, Stinson JN, Wang E, Williams SE, Wilson L. Leveraging virtual reality and augmented reality to combat chronic pain in youth: position paper from the interdisciplinary network on virtual and augmented technologies for pain management. J Med Internet Res. 2021 Apr 26;23(4):e25916. doi: 10.2196/25916. https://www.jmir.org/2021/4/e25916/ v23i4e25916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yeo SM, Lim JY, Do JG, Lim JY, In Lee J, Hwang JH. Effectiveness of interactive augmented reality-based telerehabilitation in patients with adhesive capsulitis: protocol for a multi-center randomized controlled trial. BMC Musculoskelet Disord. 2021 Apr 26;22(1):386. doi: 10.1186/s12891-021-04261-1. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-021-04261-1 .10.1186/s12891-021-04261-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Annaswamy TM, Pradhan GN, Chakka K, Khargonkar N, Borresen A, Prabhakaran B. Using biometric technology for telehealth and telerehabilitation. Phys Med Rehabil Clin N Am. 2021 May;32(2):437–49. doi: 10.1016/j.pmr.2020.12.007.S1047-9651(20)30111-X [DOI] [PubMed] [Google Scholar]
- 70.Piech J, Czernicki K. Virtual reality rehabilitation and exergames—physical and psychological impact on fall prevention among the elderly—a literature review. Appl Sci. 2021 Apr 30;11(9):4098. doi: 10.3390/app11094098. https://www.mdpi.com/2076-3417/11/9/4098 . [DOI] [Google Scholar]
- 71.Gmez-Portes C, Lacave C, Molina AI, Vallejo D. Home rehabilitation based on gamification and serious games for young people: a systematic mapping study. Appl Sci. 2020 Dec 10;10(24):8849. doi: 10.3390/app10248849. https://www.mdpi.com/2076-3417/10/24/8849 . [DOI] [Google Scholar]
- 72.Tamplin J, Loveridge B, Clarke K, Li Y, Berlowitz DJ. Development and feasibility testing of an online virtual reality platform for delivering therapeutic group singing interventions for people living with spinal cord injury. J Telemed Telecare. 2020 Jul;26(6):365–75. doi: 10.1177/1357633X19828463. [DOI] [PubMed] [Google Scholar]
- 73.Cerdán de Las Heras J, Tulppo M, Kiviniemi AM, Hilberg O, Løkke A, Ekholm S, Catalán-Matamoros D, Bendstrup E. Augmented reality glasses as a new tele-rehabilitation tool for home use: patients' perception and expectations. Disabil Rehabil Assist Technol. 2022 May;17(4):480–6. doi: 10.1080/17483107.2020.1800111. [DOI] [PubMed] [Google Scholar]
- 74.Jung T, Moorhouse N, Shi X, Amin MF. A virtual reality-supported intervention for pulmonary rehabilitation of patients with chronic obstructive pulmonary disease: mixed methods study. J Med Internet Res. 2020 Jul 07;22(7):e14178. doi: 10.2196/14178. https://www.jmir.org/2020/7/e14178/ v22i7e14178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lorenzini MC, Wittich W. Head-mounted visual assistive technology-related quality of life changes after telerehabilitation. Optom Vis Sci. 2021 Jun 01;98(6):582–91. doi: 10.1097/OPX.0000000000001705. https://europepmc.org/abstract/MED/34081648 .00006324-202106000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Matamala-Gomez M, Bottiroli S, Realdon O, Riva G, Galvagni L, Platz T, Sandrini G, De Icco R, Tassorelli C. Telemedicine and virtual reality at time of COVID-19 pandemic: an overview for future perspectives in neurorehabilitation. Front Neurol. 2021 Mar 25;12:646902. doi: 10.3389/fneur.2021.646902. https://europepmc.org/abstract/MED/33841313 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Asadzadeh A, Samad-Soltani T, Rezaei-Hachesu P. Applications of virtual and augmented reality in infectious disease epidemics with a focus on the COVID-19 outbreak. Inform Med Unlocked. 2021;24:100579. doi: 10.1016/j.imu.2021.100579. https://linkinghub.elsevier.com/retrieve/pii/S2352-9148(21)00069-1 .S2352-9148(21)00069-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Liu P, Li C, Xiao C, Zhang Z, Ma J, Gao J, Shao P, Valerio I, Pawlik TM, Ding C, Yilmaz A, Xu R. A wearable augmented reality navigation system for surgical telementoring based on Microsoft HoloLens. Ann Biomed Eng. 2021 Jan;49(1):287–98. doi: 10.1007/s10439-020-02538-5.10.1007/s10439-020-02538-5 [DOI] [PubMed] [Google Scholar]
- 79.Kutzin JM, Milligan Z, Chawla S. Using simulation to conduct a usability study of wearable technology. Clin Simul Nurs. 2017 Feb;13(2):64–70. doi: 10.1016/j.ecns.2016.12.003. [DOI] [Google Scholar]
- 80.Pérez Alonso N, Pardo Rios M, Juguera Rodriguez L, Vera Catalan T, Segura Melgarejo F, Lopez Ayuso B, Martí Nez Riquelme C, Lasheras Velasco J. Randomised clinical simulation designed to evaluate the effect of telemedicine using Google Glass on cardiopulmonary resuscitation (CPR) Emerg Med J. 2017 Nov;34(11):734–8. doi: 10.1136/emermed-2016-205998.emermed-2016-205998 [DOI] [PubMed] [Google Scholar]
- 81.Andersen D, Popescu V, Cabrera ME, Shanghavi A, Mullis B, Marley S, Gomez G, Wachs JP. An augmented reality-based approach for surgical telementoring in austere environments. Mil Med. 2017 Mar;182(S1):310–5. doi: 10.7205/MILMED-D-16-00051. [DOI] [PubMed] [Google Scholar]
- 82.Greenfield MJ, Luck J, Billingsley ML, Heyes R, Smith OJ, Mosahebi A, Khoussa A, Abu-Sittah G, Hachach-Haram N. Demonstration of the effectiveness of augmented reality telesurgery in complex hand reconstruction in Gaza. Plast Reconstr Surg Glob Open. 2018 Mar;6(3):e1708. doi: 10.1097/GOX.0000000000001708. https://europepmc.org/abstract/MED/29707463 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Harris TE, DeLellis SF, Heneghan JS, Buckman RF, Miller GT, Magee JH, Vasios WN, Nelson KJ, Kane SF, Choi YS. Augmented reality forward damage control procedures for nonsurgeons: a feasibility demonstration. Mil Med. 2020 Jan 07;185(Suppl 1):521–5. doi: 10.1093/milmed/usz298.5740711 [DOI] [PubMed] [Google Scholar]
- 84.Lin C, Rojas-Munoz E, Cabrera ME, Sanchez-Tamayo N, Andersen D, Popescu V, Noguera JA, Zarzaur B, Murphy P, Anderson K, Douglas T, Griffis C, Wachs J. How about the mentor? Effective workspace visualization in AR telementoring. Proceedings of the 2020 IEEE Conference on Virtual Reality and 3D User Interfaces; VR '20; March 22-26, 2020; Atlanta, GA, USA. 2020. pp. 212–20. [DOI] [Google Scholar]
- 85.Rojas-Muñoz E, Lin C, Sanchez-Tamayo N, Cabrera ME, Andersen D, Popescu V, Barragan JA, Zarzaur B, Murphy P, Anderson K, Douglas T, Griffis C, McKee J, Kirkpatrick AW, Wachs JP. Evaluation of an augmented reality platform for austere surgical telementoring: a randomized controlled crossover study in cricothyroidotomies. NPJ Digit Med. 2020 May 21;3:75. doi: 10.1038/s41746-020-0284-9. doi: 10.1038/s41746-020-0284-9.284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Weibel N, Gasques D, Johnson J, Sharkey T, Xu ZR, Zhang X, Zavala E, Yip M, Davis K. ARTEMIS: mixed-reality environment for immersive surgical telementoring. Extended Abstracts of the 2020 CHI Conference on Human Factors in Computing Systems; CHI EA '20; April 25-30, 2020; Honolulu, HI, USA. 2020. pp. 1–4. [DOI] [Google Scholar]
- 87.Rojas-Muñoz E, Cabrera ME, Lin C, Andersen D, Popescu V, Anderson K, Zarzaur BL, Mullis B, Wachs JP. The System for Telementoring with Augmented Reality (STAR): a head-mounted display to improve surgical coaching and confidence in remote areas. Surgery. 2020 Apr;167(4):724–31. doi: 10.1016/j.surg.2019.11.008.S0039-6060(19)30744-5 [DOI] [PubMed] [Google Scholar]
- 88.Glick Y, Avital B, Oppenheimer J, Nahman D, Wagnert-Avraham L, Eisenkraft A, Dym L, Levi D, Agur A, Gustus B, Furer A. Augmenting prehospital care. BMJ Mil Health. 2021 Jun;167(3):158–62. doi: 10.1136/jramc-2019-001320.jramc-2019-001320 [DOI] [PubMed] [Google Scholar]
- 89.Carbone M, Freschi C, Mascioli S, Ferrari V, Ferrari M. A wearable augmented reality platform for telemedicine. Proceedings of the 3rd International Conference on Augmented Reality, Virtual Reality, and Computer Graphics; AVR '16; June 15-18, 2016; Lecce, Italy. 2016. pp. 92–100. [DOI] [Google Scholar]
- 90.Davis MC, Can DD, Pindrik J, Rocque BG, Johnston JM. Virtual interactive presence in global surgical education: international collaboration through augmented reality. World Neurosurg. 2016 Feb;86:103–11. doi: 10.1016/j.wneu.2015.08.053. https://europepmc.org/abstract/MED/26342783 .S1878-8750(15)01069-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wei NJ, Dougherty B, Myers A, Badawy SM. Using Google Glass in surgical settings: systematic review. JMIR Mhealth Uhealth. 2018 Mar 06;6(3):e54. doi: 10.2196/mhealth.9409. https://mhealth.jmir.org/2018/3/e54/ v6i3e54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Andersen DS, Cabrera ME, Rojas-Muñoz EJ, Popescu VS, Gonzalez GT, Mullis B, Marley S, Zarzaur BL, Wachs JP. Augmented reality future step visualization for robust surgical telementoring. Simul Healthc. 2019 Feb;14(1):59–66. doi: 10.1097/SIH.0000000000000334. [DOI] [PubMed] [Google Scholar]
- 93.Mitsuno D, Hirota Y, Akamatsu J, Kino H, Okamoto T, Ueda K. Telementoring demonstration in craniofacial surgery with Hololens, Skype, and three-layer facial models. J Craniofac Surg. 2019 Jan;30(1):28–32. doi: 10.1097/SCS.0000000000004899. [DOI] [PubMed] [Google Scholar]
- 94.Rojas-Muñoz E, Andersen D, Cabrera ME, Popescu V, Marley S, Zarzaur B, Mullis B, Wachs JP. Augmented reality as a medium for improved telementoring. Mil Med. 2019 Mar 01;184(Suppl 1):57–64. doi: 10.1093/milmed/usy300.5418641 [DOI] [PubMed] [Google Scholar]
- 95.Rojas-Muñoz E, Cabrera ME, Andersen D, Popescu V, Marley S, Mullis B, Zarzaur B, Wachs J. Surgical telementoring without encumbrance: a comparative study of see-through augmented reality-based approaches. Ann Surg. 2019 Aug;270(2):384–9. doi: 10.1097/SLA.0000000000002764. [DOI] [PubMed] [Google Scholar]
- 96.Darrow DP, Spano A, Grande A. The potential for undue patient exposure during the use of telementoring technology. Cureus. 2020 Apr 08;12(4):e7594. doi: 10.7759/cureus.7594. https://europepmc.org/abstract/MED/32399328 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sadeghi AH, Mathari SE, Abjigitova D, Maat AP, Taverne YJ, Bogers AJ, Mahtab EA. Current and future applications of virtual, augmented, and mixed reality in cardiothoracic surgery. Ann Thorac Surg. 2022 Feb;113(2):681–91. doi: 10.1016/j.athoracsur.2020.11.030. https://linkinghub.elsevier.com/retrieve/pii/S0003-4975(20)32127-5 .S0003-4975(20)32127-5 [DOI] [PubMed] [Google Scholar]
- 98.Cofano F, Di Perna G, Bozzaro M, Longo A, Marengo N, Zenga F, Zullo N, Cavalieri M, Damiani L, Boges DJ, Agus M, Garbossa D, Calì C. Augmented reality in medical practice: from spine surgery to remote assistance. Front Surg. 2021 Mar 30;8:657901. doi: 10.3389/fsurg.2021.657901. http://hdl.handle.net/2318/1847163 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lareyre F, Chaudhuri A, Adam C, Carrier M, Mialhe C, Raffort J. Applications of head-mounted displays and smart glasses in vascular surgery. Ann Vasc Surg. 2021 Aug;75:497–512. doi: 10.1016/j.avsg.2021.02.033.S0890-5096(21)00252-1 [DOI] [PubMed] [Google Scholar]
- 100.Wang S, Parsons M, Stone-McLean J, Rogers P, Boyd S, Hoover K, Meruvia-Pastor O, Gong M, Smith A. Augmented reality as a telemedicine platform for remote procedural training. Sensors (Basel) 2017 Oct 10;17(10):2294. doi: 10.3390/s17102294. https://www.mdpi.com/resolver?pii=s17102294 .s17102294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Deldar K, Bahaadinbeigy K, Tara SM. Teleconsultation and clinical decision making: a systematic review. Acta Inform Med. 2016 Jul 16;24(4):286–92. doi: 10.5455/aim.2016.24.286-292. https://europepmc.org/abstract/MED/27708494 .AIM-24-286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Noorian AR, Bahr Hosseini M, Avila G, Gerardi R, Andrle A, Su M, Starkman S, Saver JL, Sharma LK. Use of wearable technology in remote evaluation of acute stroke patients: feasibility and reliability of a Google Glass-based device. J Stroke Cerebrovasc Dis. 2019 Oct;28(10):104258. doi: 10.1016/j.jstrokecerebrovasdis.2019.06.016.S1052-3057(19)30285-X [DOI] [PubMed] [Google Scholar]
- 103.Martin G, Koizia L, Kooner A, Cafferkey J, Ross C, Purkayastha S, Sivananthan A, Tanna A, Pratt P, Kinross J, PanSurg Collaborative Use of the HoloLens2 mixed reality headset for protecting health care workers during the COVID-19 pandemic: prospective, observational evaluation. J Med Internet Res. 2020 Aug 14;22(8):e21486. doi: 10.2196/21486. https://www.jmir.org/2020/8/e21486/ v22i8e21486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Skolnik AB, Chai PR, Dameff C, Gerkin R, Monas J, Padilla-Jones A, Curry S. Teletoxicology: patient assessment using wearable audiovisual streaming technology. J Med Toxicol. 2016 Dec;12(4):358–64. doi: 10.1007/s13181-016-0567-3. https://europepmc.org/abstract/MED/27381429 .10.1007/s13181-016-0567-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kaylor J, Hooper V, Wilson A, Burkert R, Lyda M, Fletcher K, Bowers E. Reliability testing of augmented reality glasses technology: establishing the evidence base for telewound care. J Wound Ostomy Continence Nurs. 2019;46(6):485–90. doi: 10.1097/WON.0000000000000585. [DOI] [PubMed] [Google Scholar]
- 106.Follmann A, Ohligs M, Hochhausen N, Beckers SK, Rossaint R, Czaplik M. Technical support by smart glasses during a mass casualty incident: a randomized controlled simulation trial on technically assisted triage and telemedical app use in disaster medicine. J Med Internet Res. 2019 Jan 03;21(1):e11939. doi: 10.2196/11939. https://www.jmir.org/2019/1/e11939/ v21i1e11939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sirilak S, Muneesawang P. A new procedure for advancing telemedicine using the HoloLens. IEEE Access. 2018 Oct 11;6:60224–33. doi: 10.1109/access.2018.2875558. [DOI] [Google Scholar]
- 108.Hu HZ, Feng XB, Shao ZW, Xie M, Xu S, Wu XH, Ye ZW. Application and prospect of mixed reality technology in medical field. Curr Med Sci. 2019 Feb;39(1):1–6. doi: 10.1007/s11596-019-1992-8.10.1007/s11596-019-1992-8 [DOI] [PubMed] [Google Scholar]
- 109.Venkata HS, Alsadoon A, Prasad PW, Alsadoon OH, Haddad S, Deva A, Hsu J. A novel mixed reality in breast and constructive jaw surgical tele-presence. Comput Methods Programs Biomed. 2019 Aug;177:253–68. doi: 10.1016/j.cmpb.2019.05.025.S0169-2607(19)30074-4 [DOI] [PubMed] [Google Scholar]
- 110.Zhang Q, Karunanithi M, Kang C. Immersive augmented reality (I am real) – remote clinical consultation. Proceedings of the 2019 IEEE EMBS International Conference on Biomedical & Health Informatics; BHI '19; May 19-22, 2019; Chicago, IL, USA. 2019. pp. 1–4. [DOI] [Google Scholar]
- 111.Dananjayan S, Raj GM. 5G in healthcare: how fast will be the transformation? Ir J Med Sci. 2021 May;190(2):497–501. doi: 10.1007/s11845-020-02329-w.10.1007/s11845-020-02329-w [DOI] [PubMed] [Google Scholar]
- 112.Desselle MR, Brown RA, James AR, Midwinter MJ, Powell SK, Woodruff MA. Augmented and virtual reality in surgery. Comput Sci Eng. 2020 May 1;22(3):18–26. doi: 10.1109/mcse.2020.2972822. [DOI] [Google Scholar]
- 113.Neupane A, Alsadoon A, Prasad PW, Ali RS, Haddad S. A novel modified chaotic simplified advanced encryption system (MCS-AES): mixed reality for a secure surgical tele-presence. Multimed Tools Appl. 2020 Aug 08;79(39-40):29043–67. doi: 10.1007/s11042-020-09478-1. [DOI] [Google Scholar]
- 114.Pinter C, Lasso A, Choueib S, Asselin M, Fillion-Robin JC, Vimort JB, Martin K, Jolley MA, Fichtinger G. SlicerVR for medical intervention training and planning in immersive virtual reality. IEEE Trans Med Robot Bionics. 2020 May;2(2):108–17. doi: 10.1109/tmrb.2020.2983199. https://europepmc.org/abstract/MED/33748693 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Higginbotham G. Virtual connections: improving global neurosurgery through immersive technologies. Front Surg. 2021 Feb 19;8:629963. doi: 10.3389/fsurg.2021.629963. https://europepmc.org/abstract/MED/33681283 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hanna MG, Ahmed I, Nine J, Prajapati S, Pantanowitz L. Augmented reality technology using Microsoft HoloLens in anatomic pathology. Arch Pathol Lab Med. 2018 May;142(5):638–44. doi: 10.5858/arpa.2017-0189-OA. https://meridian.allenpress.com/aplm/article-lookup/doi/10.5858/arpa.2017-0189-OA . [DOI] [PubMed] [Google Scholar]
- 117.Christensen JK. The emergence and unfolding of telemonitoring practices in different healthcare organizations. Int J Environ Res Public Health. 2018 Jan 03;15(1):61. doi: 10.3390/ijerph15010061. https://www.mdpi.com/resolver?pii=ijerph15010061 .ijerph15010061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Vidal-Balea A, Blanco-Novoa Ó, Fraga-Lamas P, Fernández-Caramés TM. Developing the next generation of augmented reality games for pediatric healthcare: an open-source collaborative framework based on ARCore for implementing teaching, training and monitoring applications. Sensors (Basel) 2021 Mar 07;21(5):1865. doi: 10.3390/s21051865. https://www.mdpi.com/resolver?pii=s21051865 .s21051865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kowatsch T, Lohse K, Erb V, Schittenhelm L, Galliker H, Lehner R, Huang EM. Hybrid ubiquitous coaching with a novel combination of mobile and holographic conversational agents targeting adherence to home exercises: four design and evaluation studies. J Med Internet Res. 2021 Feb 22;23(2):e23612. doi: 10.2196/23612. https://www.jmir.org/2021/2/e23612/ v23i2e23612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Thøgersen M, Andoh J, Milde C, Graven-Nielsen T, Flor H, Petrini L. Individualized augmented reality training reduces phantom pain and cortical reorganization in amputees: a proof of concept study. J Pain. 2020;21(11-12):1257–69. doi: 10.1016/j.jpain.2020.06.002.S1526-5900(20)30033-X [DOI] [PubMed] [Google Scholar]
- 121.Ponce BA, Brabston EW, Zu S, Watson SL, Baker D, Winn D, Guthrie BL, Shenai MB. Telemedicine with mobile devices and augmented reality for early postoperative care. Annu Int Conf IEEE Eng Med Biol Soc. 2016 Aug;2016:4411–4. doi: 10.1109/EMBC.2016.7591705. [DOI] [PubMed] [Google Scholar]
- 122.McKnight RR, Pean CA, Buck JS, Hwang JS, Hsu JR, Pierrie SN. Virtual reality and augmented reality-translating surgical training into surgical technique. Curr Rev Musculoskelet Med. 2020 Dec;13(6):663–74. doi: 10.1007/s12178-020-09667-3. https://europepmc.org/abstract/MED/32779019 .10.1007/s12178-020-09667-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nikouline A, Jimenez MC, Okrainec A. Feasibility of remote administration of the fundamentals of laparoscopic surgery (FLS) skills test using Google wearable device. Surg Endosc. 2020 Jan;34(1):443–9. doi: 10.1007/s00464-019-06788-w.10.1007/s00464-019-06788-w [DOI] [PubMed] [Google Scholar]
- 124.Chakrabarti S. Usefulness of telepsychiatry: a critical evaluation of videoconferencing-based approaches. World J Psychiatry. 2015 Sep 22;5(3):286–304. doi: 10.5498/wjp.v5.i3.286. https://www.wjgnet.com/2220-3206/full/v5/i3/286.htm . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Levy F, Leboucher P, Rautureau G, Jouvent R. E-virtual reality exposure therapy in acrophobia: a pilot study. J Telemed Telecare. 2016 Jun;22(4):215–20. doi: 10.1177/1357633X15598243.1357633X15598243 [DOI] [PubMed] [Google Scholar]
- 126.Jebbar Y, Belqasmi F, Glitho R, Alfandi O. A fog-based architecture for remote phobia treatment. Proceedings of the 2019 IEEE International Conference on Cloud Computing Technology and Science; CloudCom '19; December 11-13, 2019; Sydney, Australia. 2019. pp. 271–8. [DOI] [Google Scholar]
- 127.Cikajlo I, Cizman Staba U, Vrhovac S, Larkin F, Roddy M. A cloud-based virtual reality app for a novel telemindfulness service: rationale, design and feasibility evaluation. JMIR Res Protoc. 2017 Jun 05;6(6):e108. doi: 10.2196/resprot.6849. https://www.researchprotocols.org/2017/6/e108/ v6i6e108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Baccon LA, Chiarovano E, MacDougall HG. Virtual reality for teletherapy: avatars may combine the benefits of face-to-face communication with the anonymity of online text-based communication. Cyberpsychol Behav Soc Netw. 2019 Feb;22(2):158–65. doi: 10.1089/cyber.2018.0247. [DOI] [PubMed] [Google Scholar]
- 129.Yuen EK, Goetter EM, Stasio MJ, Ash P, Mansour B, McNally E, Sanchez M, Hobar E, Forte S, Zulaica K, Watkins J. A pilot of acceptance and commitment therapy for public speaking anxiety delivered with group videoconferencing and virtual reality exposure. J Contextual Behav Sci. 2019 Apr;12:47–54. doi: 10.1016/j.jcbs.2019.01.006. [DOI] [Google Scholar]
- 130.Pedram S, Palmisano S, Perez P, Mursic R, Farrelly M. Examining the potential of virtual reality to deliver remote rehabilitation. Comput Human Behav. 2020 Apr;105:106223. doi: 10.1016/j.chb.2019.106223. [DOI] [Google Scholar]
- 131.Galunder SS, Gottlieb JF, Ladwig J, Hamell J, Keller PK, Wu P. A VR ecosystem for telemedicine and non-intrusive cognitive and affective assessment. Proceedings of the IEEE 6th International Conference on Serious Games and Applications for Health; SeGAH '18; May 16-18, 2018; Vienna, Austria. 2018. pp. 1–6. [DOI] [Google Scholar]
- 132.Shao D, Lee IJ. Acceptance and influencing factors of social virtual reality in the urban elderly. Sustainability. 2020 Nov 10;12(22):9345. doi: 10.3390/su12229345. https://www.mdpi.com/2071-1050/12/22/9345 . [DOI] [Google Scholar]
- 133.Nakagawa K, Yellowlees PM. University of California Technology Wellness Index: a physician-centered framework to assess technologies' impact on physician well-being. Psychiatr Clin North Am. 2019 Dec;42(4):669–81. doi: 10.1016/j.psc.2019.08.005.S0193-953X(19)30075-9 [DOI] [PubMed] [Google Scholar]
- 134.Sampaio M, Haro MV, De Sousa B, Melo WV, Hoffman HG. Therapists make the switch to telepsychology to safely continue treating their patients during the COVID-19 pandemic. Virtual reality telepsychology may be next. Front Virtual Real. 2021 Jan;1:576421. doi: 10.3389/frvir.2020.576421. https://europepmc.org/abstract/MED/33585834 .576421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mohan A, Wara UU, Arshad Shaikh MT, Rahman RM, Zaidi ZA. Telesurgery and robotics: an improved and efficient era. Cureus. 2021 Mar 26;13(3):e14124. doi: 10.7759/cureus.14124. https://europepmc.org/abstract/MED/33927932 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Jiménez Moreno R, Espinosa Valcárcel FA, Amaya Hurtado D. Teleoperated systems: a perspective on telesurgery applications. Rev Ing Biomed. 2013;7(14):30–41. http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S1909-97622013000200004 . [Google Scholar]
- 137.Guo J, Guo S, Tamiya T, Hirata H, Ishihara H. A virtual reality-based method of decreasing transmission time of visual feedback for a tele-operative robotic catheter operating system. Int J Med Robot. 2016 Mar;12(1):32–45. doi: 10.1002/rcs.1642. [DOI] [PubMed] [Google Scholar]
- 138.Bhattacherjee S, Chattopadhayay S, Rao V, Seth S, Mukherjee S, Sengupta A, Bhaumik S. Kinematics and teleoperation of tendon driven continuum robot. Procedia Comput Sci. 2018;133:879–86. doi: 10.1016/j.procs.2018.07.106. [DOI] [Google Scholar]
- 139.Abu-Kheil Y, Al Trad O, Seneviratne L, Dias J. A proposed clinical evaluation of a simulation environment for magnetically-driven active endoscopic capsules. Adv Exp Med Biol. 2019;1170:87–94. doi: 10.1007/978-3-030-24230-5_4. [DOI] [PubMed] [Google Scholar]
- 140.Ho DK. Using smartphone-delivered stereoscopic vision in microsurgery: a feasibility study. Eye (Lond) 2019 Jun;33(6):953–6. doi: 10.1038/s41433-019-0356-8. https://europepmc.org/abstract/MED/30755728 .10.1038/s41433-019-0356-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Richter F, Zhang Y, Zhi Y, Orosco RK, Yip MC. Augmented reality predictive displays to help mitigate the effects of delayed telesurgery. Proceedings of the 2019 International Conference on Robotics and Automation; ICRA '19; May 20-24, 2019; Montreal, Canada. 2019. pp. 444–50. [DOI] [Google Scholar]
- 142.De Silva R, Siriwardhana Y, Samarasinghe T, Ylianttila M, Liyanage M. Local 5G operator architecture for delay critical telehealth applications. Proceedings of the IEEE 3rd 5G World Forum; 5GWF '20; September 10-12, 2020; Bangalore, India. 2020. pp. 257–62. [DOI] [Google Scholar]
- 143.Tuladhar S, AlSallami N, Alsadoon A, Prasad PW, Alsadoon OH, Haddad S, Alrubaie A. A recent review and a taxonomy for hard and soft tissue visualization-based mixed reality. Int J Med Robot. 2020 Oct;16(5):1–22. doi: 10.1002/rcs.2120. [DOI] [PubMed] [Google Scholar]
- 144.Piccolo D, Smolle J, Wolf IH, Peris K, Hofmann-Wellenhof R, Dell'Eva G, Burroni M, Chimenti S, Kerl H, Soyer HP. Face-to-face diagnosis vs telediagnosis of pigmented skin tumors: a teledermoscopic study. Arch Dermatol. 1999 Dec;135(12):1467–71. doi: 10.1001/archderm.135.12.1467. [DOI] [PubMed] [Google Scholar]
- 145.telediagnosis. Farlex. [2022-08-01]. https://medical-dictionary.thefreedictionary.com/telediagnosis .
- 146.Ji H, Wang J, Gao J, Liu X. Research on telemedicine technology and implement based on virtual reality. Proceedings of the 2016 IEEE Advanced Information Management, Communicates, Electronic and Automation Control Conference; IMCEC '16; October 3-5, 2016; Xi'an, China. 2016. pp. 1581–6. [DOI] [Google Scholar]
- 147.Tian Y, Raghuraman S, Annaswamy T, Borresen A, Nahrstedt K, Prabhakaran B. H-TIME: haptic-enabled tele-immersive musculoskeletal examination. Proceedings of the 25th ACM international conference on Multimedia; MM '17; October 23-27, 2017; Mountain View, CA, USA. 2017. pp. 137–45. [DOI] [Google Scholar]
- 148.Filippeschi A, Brizzi F, Ruffaldi E, Jacinto Villegas JM, Landolfi L, Avizzano CA. Evaluation of diagnostician user interface aspects in a virtual reality-based tele-ultrasonography simulation. Adv Robot. 2019 Jul 04;33(15-16):840–52. doi: 10.1080/01691864.2019.1635909. [DOI] [Google Scholar]
- 149.Baribeau Y, Sharkey A, Chaudhary O, Krumm S, Fatima H, Mahmood F, Matyal R. Handheld point-of-care ultrasound probes: the new generation of POCUS. J Cardiothorac Vasc Anesth. 2020 Nov;34(11):3139–45. doi: 10.1053/j.jvca.2020.07.004. https://europepmc.org/abstract/MED/32736998 .S1053-0770(20)30634-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Syawaludin MF, Lee M, Hwang JI. Foveation pipeline for 360° video-based telemedicine. Sensors (Basel) 2020 Apr 16;20(8):2264. doi: 10.3390/s20082264. https://www.mdpi.com/resolver?pii=s20082264 .s20082264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ramsingh D, Van Gorkom C, Holsclaw M, Nelson S, De La Huerta M, Hinson J, Selleck E. Use of a smartphone-based augmented reality video conference app to remotely guide a point of care ultrasound examination. Diagnostics (Basel) 2019 Oct 24;9(4):159. doi: 10.3390/diagnostics9040159. https://www.mdpi.com/resolver?pii=diagnostics9040159 .diagnostics9040159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wang GG. Definition and review of virtual prototyping. J Comput Inf Sci Eng. 2002;2(3):232–6. doi: 10.1115/1.1526508. [DOI] [Google Scholar]
- 153.Trenholme D, Smith SP. Computer game engines for developing first-person virtual environments. Virtual Real. 2008 Mar 28;12(3):181–7. doi: 10.1007/s10055-008-0092-z. [DOI] [Google Scholar]
- 154.Sherman WR, Craig AB. Interface to the virtual world–output. In: Sherman WR, Craig AB, editors. Understanding Virtual Reality: Interface, Application, and Design. Cambridge, MA, USA: Elsevier; 2003. pp. 114–203. [Google Scholar]
- 155.Cheng L, Tavakoli M. COVID-19 pandemic spurs medical telerobotic systems: a survey of applications requiring physiological organ motion compensation. Front Robot AI. 2020 Nov 9;7:594673. doi: 10.3389/frobt.2020.594673. https://europepmc.org/abstract/MED/33501355 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wattanasoontorn V, Boada I, García R, Sbert M. Serious games for health. Entertain Comput. 2013 Dec;4(4):231–47. doi: 10.1016/j.entcom.2013.09.002. [DOI] [Google Scholar]
- 157.Nickel F, Cizmic A, Chand M. Telestration and augmented reality in minimally invasive surgery: an invaluable tool in the age of COVID-19 for remote proctoring and telementoring. JAMA Surg. 2022 Feb 01;157(2):169–70. doi: 10.1001/jamasurg.2021.3604.2785412 [DOI] [PubMed] [Google Scholar]
- 158.Liston M, Genna G, Maurer C, Kikidis D, Gatsios D, Fotiadis D, Bamiou DE, Pavlou M. Investigating the feasibility and acceptability of the HOLOBalance system compared with standard care in older adults at risk for falls: study protocol for an assessor blinded pilot randomised controlled study. BMJ Open. 2021 Feb 12;11(2):e039254. doi: 10.1136/bmjopen-2020-039254. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=33579762 .bmjopen-2020-039254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Cassidy D. Broadband connection types explained. Bonkers Money. 2022. Feb 3, [2022-09-11]. https://www.bonkers.ie/guides/broadband-phone-tv/broadband-connection-types-explained/
- 160.What is telehealth? NEJM Catal Innov Care Deliv. 2018 Feb 1;4(1) doi: 10.1056/CAT.18.0268. [DOI] [Google Scholar]
- 161.Jay A. Cloud-based vs web-based applications: a comparison of features & key aspects. Finances Online. 2019. May 16, [2022-09-11]. https://financesonline.com/cloud-based-web-based-applications-a-comparison-of-features-key-aspects/
- 162.Gunshin M, Doi K, Morimura N. Use of high-fidelity simulation technology in disasters: an integrative literature review. Acute Med Surg. 2020 Dec 20;7(1):e596. doi: 10.1002/ams2.596. https://europepmc.org/abstract/MED/33364034 .AMS2596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Persky S. A virtual home for the virtual clinical trial. J Med Internet Res. 2020 Jan 03;22(1):e15582. doi: 10.2196/15582. https://www.jmir.org/2020/1/e15582/ v22i1e15582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Koledova E, Le Masne Q, Spataru A, Bagha M, Dixon D. Digital health in the management of pediatric growth hormone therapy - 10 years of developments. Stud Health Technol Inform. 2021 May 27;281:926–30. doi: 10.3233/SHTI210314.SHTI210314 [DOI] [PubMed] [Google Scholar]
- 165.Threapleton K, Drummond A, Standen P. Virtual rehabilitation: what are the practical barriers for home-based research? Digit Health. 2016 Apr 29;2:2055207616641302. doi: 10.1177/2055207616641302. https://journals.sagepub.com/doi/abs/10.1177/2055207616641302?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .10.1177_2055207616641302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Yu J, Ferniany W, Guthrie B, Parekh SG, Ponce B. Lessons learned from Google Glass: telemedical spark or unfulfilled promise? Surg Innov. 2016 Apr;23(2):156–65. doi: 10.1177/1553350615597085.1553350615597085 [DOI] [PubMed] [Google Scholar]
- 167.Vogiatzaki E, Krukowski A. Maintaining mental wellbeing of elderly at home. In: Ganchev I, Garcia NM, Dobre C, Mavromoustakis CX, Goleva R, editors. Enhanced Living Environments: Algorithms, Architectures, Platforms, and Systems. Cham, Switzerland: Springer; 2019. pp. 177–209. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy.
Augmented, virtual, and mixed reality hardware devices.
Other relative hardware devices.
List of software and source platforms.


