Abstract
Background:
Tobacco smoking exacerbates diabetes-related complications; its prevalence is notwithstanding substantial. Persons with diabetes face a number of barriers and challenges to quitting such as multiple lifestyle restrictions; tailored interventions are required for smoking cessation.
Objective:
To identify research on behavioral interventions for smoking cessation in diabetes.
Methods:
Studies had to be randomized controlled trials, quasiexperimental or systematic reviews. The behavioral interventions included were: the 5As, Cognitive-Behavioral Therapy, Motivational Interviewing, Contingency Management, Health Coaching and Counselling, as compared to standard care. The outcomes were self-reported and/or biochemically verified smoking cessation. CINAHL Complete, MEDLINE Complete, the Cochrane databases of systematic reviews and randomized controlled trials, PsychInfo and PubMed Central were searched until July, 2023. Keywords used included diabetes, smoking cessation and each of the behavioral interventions included.
Results:
1615 papers were identified. Three studies on the 5As/brief advice, 4 on Motivational Intervention and 1 on counseling were retained. The results on the 5As and Motivational Interviewing were conflicting. More intensive interventions appear to be more successful in achieving smoking cessation in smokers with diabetes.
Conclusions:
Future research should focus on the continued development and evaluation of structured smoking cessation interventions based on the 5As, Motivational interviewing and Cognitive Behavioral Therapy.
Keywords: behavioral health, diabetes mellitus, smoking, lifestyle change, health promotion
Background
Introduction
Diabetes mellitus (DM) is a chronic metabolic disorder that poses significant challenges to individual health and public healthcare systems worldwide. This disease affects nearly 422 million people and is directly responsible for 1.5 million deaths, while indirectly contributing to another 17.5 million deaths globally each year. 1 Tobacco smoking is another leading cause of preventable morbidity, and mortality. Tobacco smoking is estimated to lead to the premature death of 6 million people worldwide. 2 Long-term smoking is linked to detrimental health effects, such as the development of cardiovascular disease, chronic respiratory disease and other conditions, that develop over time due to smoking habits. In the general population, individuals who continue to smoke beyond age 40 tend to experience higher levels of pain and disability than non-smokers. 3 Tobacco smoking is also 1 of the most important modifiable risk factors for pre-diabetes and DM. 4 It has also been demonstrated that smoking exacerbates diabetes-related complications and impedes effective self-management. 4 Smoking, for example, substantially increases the risk of cardiovascular disease in both the general population and patients with type 2 diabetes. 5 This increased risk is however more accentuated in persons living with diabetes, as these persons have a twofold additional hazard of cardiovascular disease compared to persons without diabetes 6 ; cardiovascular disease remains the most common cause of mortality among patients with diabetes.7,8
Despite the well-documented risks associated with smoking among individuals with diabetes, the prevalence of smoking in this population is still significant. Durlach et al, estimated the global prevalence of tobacco use amongst individuals with type 1 and type 2 diabetes at 30% and 20%, respectively. 4 Evidence suggests that when compared to other smokers, smokers with diabetes tend to be less motivated to stop smoking, possibly due to several diabetes-related barriers and challenges to quitting. 9 In addition to the commonly reported challenges and barriers to quitting, such as the smoking habit and addiction, individuals living with diabetes have reported that they believe smoking helps them to manage their diabetes, such as, in controlling their blood sugar levels, adhering to their diet and in managing their weight. 10 Living with diabetes and the accompanying required lifestyle changes, is in itself a stressor, and is known to be associated with distress and depression. 10 Persons with diabetes report that they use smoking to cope with boredom, anxiety, depression and stress. 11 All these elements make it additionally difficult for persons with diabetes to stop. 10 As a result, there is an urgent need for targeted interventions to support smoking cessation in people with diabetes.
Intensive smoking cessation support, including behavioral assistance such as counseling and pharmacological options such as nicotine replacement therapy (NRT), bupropion, or varenicline, has been shown to increase the success rate of smoking cessation in the general population. 12 A scoping review on smoking cessation interventions applied to individuals living with diabetes, and the associated specific challenges and barriers to smoking cessation, reported that this approach could also be beneficial for people with diabetes, helping them cope with the unique challenges associated with their condition. 10 However, given the scope of the review, the review authors did not identify specific behavioral interventions to guide clinical practice in this area. While a subsequent systematic review of stand-alone intensive smoking cessation interventions among individuals with diabetes recommends the use of intensive (long and frequent support sessions) interventions for use among this cohort, the limited number of studies and the inconsistent findings limited the ability to draw recommendations on the use of specific behavioral interventions for smoking cessation among individuals living with diabetes. 13 This scoping review, consequently, fills an important gap in the literature in that it seeks to identify which behavioral interventions have been researched to date and could be applied to assisting persons living with diabetes to quit smoking.
Objectives
The objective of this review was to map the research on behavioral interventions to assist smoking cessation in individuals with diabetes; the behavioral techniques which were the focus of this scoping review are the 5As framework for smoking cessation, Cognitive-Behavioral Therapy (CBT), Motivational Interviewing (MI), Contingency Management (CM), Health Coaching and Counselling.
More specifically this review seeks to explore
the extent of research on the above behavioral interventions for smoking cessation for individuals with diabetes,
identify gaps in the research to date and
make recommendations for the development of future research in this area
Methods
The methodological framework for scoping reviews developed by Arksey & O’Malley, as reviewed by Levac, Colquhoun, & O’Brien, was used in the conduct of this review.14,15 This framework includes 5 stages: identifying the research question, searching relevant studies, selecting studies, charting the data and collating it, summarizing and reporting the results. This scoping review is reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for scoping reviews checklist (PRISMA-ScR Checklist). 16
Review Question and Eligibility Criteria
The review question addressed in this review is “what is the current scope of research on behavioral interventions to assist smoking cessation in persons with diabetes?.”
Specifically, the behavioral interventions covered in this scoping review were:
The 5 As and brief advice
Cognitive Behavioral Therapy
Motivational Interviewing
Contingency Management
Health Coaching
Counseling
In light of this review question, papers were considered to be suitable for inclusion in this review if they met the criteria outlined in Table 1:
Table 1.
The Inclusion and Exclusion Criteria.
| PICOS elements | Inclusion | Exclusion |
|---|---|---|
| P: Persons living with diabetes who smoke | Study includes persons 18 years or over, with diabetes, who smoke tobacco products | Studies which include tobacco products other than smoked tobacco, such as smokeless tobacco products, heated tobacco products and nicotine-only products. |
| I: Behavioral therapies aimed at supporting smoking cessation | Behavioral interventions aimed at supporting smoking cessation which included: the 5As and brief advice Cognitive Behavioral Therapy Motivational Interviewing Contingency Management Health Coaching Counseling |
Behavioral intervention to promote self-management of diabetes, including diabetes stability Behavioral therapies not included in the list to the left |
| C: Standard care | Standard care in assisting persons to stop smoking, such as the provision of educational material, provision of pharmacotherapy in the absence of behavioral interventions. Standard diabetes management care |
No comparison included |
| O: Smoking cessation | Outcomes included smoking cessation measures: Self-reported smoking cessation Biochemically verified abstinence (such as exhaled carbon monoxide, cotinine in saliva, blood or urine verified abstinence) |
No verification of smoking cessation |
| S: Study design | Quasi experimental, experimental studies, systematic reviews and meta-analysis. | Cohort designs, surveys of participants’ views on smoking cessation, in vitro, ex vivo, and animal studies, narrative review articles, conference reports, short communications, and editorials. |
Only studies available in the English language were selected, without any time restriction.
Information Sources
The following databases were searched between the 1st and the 30th of July 2023: CINAHL Complete (EBSCO), MEDLINE Complete, the Cochrane database of systematic reviews, the Cochrane database central register of randomized controlled trials, APA PsychInfo and PubMed Central. The reference lists of retained papers were scanned to identify any additional relevant papers. Alerts were set to identify any additional papers published after July, 2023 until the end of October, 2023. A manual search of the bibliography of papers which were retained based on the title and abstract were scanned to assist with identification of any additional relevant studies.
Search Strategy
The following Boolean search strings were used for the databases search:
(diabetes OR diabetes mellitus OR type 1 diabetes OR type 2 diabetes) AND (smoking cessation OR smoking cessation interventions OR quit smoking OR stop smoking) AND (5As OR 3As OR 5A’s OR 3A’s OR brief advice OR brief intervention)
(diabetes OR diabetes mellitus OR type 1 diabetes OR type 2 diabetes) AND (smoking cessation OR smoking cessation interventions OR quit smoking OR stop smoking) AND (Cognitive Behavio?ral Therapy OR CBT)
(diabetes OR diabetes mellitus OR type 1 diabetes OR type 2 diabetes) AND (smoking cessation OR smoking cessation interventions OR quit smoking OR stop smoking) AND (motivational interviewing OR mi OR motivational interview)
(diabetes OR diabetes mellitus OR type 1 diabetes OR type 2 diabetes) AND (smoking cessation OR smoking cessation interventions OR quit smoking OR stop smoking) AND (contingency management)
(diabetes or diabetes mellitus OR type 1 diabetes OR type 2 diabetes) AND (smoking cessation OR smoking cessation interventions OR quit smoking OR stop smoking) AND (coaching OR health coaching)
(diabetes OR diabetes mellitus OR type 1 diabetes OR type 2 diabetes) AND (smoking cessation OR smoking cessation interventions OR quit smoking OR stop smoking) AND (health behavio?r counsel?ing OR individual behavio?r counsel?ing OR counsel?ing OR behavio?r counsel?ing OR health counsel?ing)
Selection of Sources of Evidence
The retrieved papers were initially compared to the inclusion criteria based on their title and abstract by 1 of the reviewers (R.S.); a second reviewer (J.G.) was responsible for checking the results of this initial screening. Those papers retained after this initial selection were independently rescreened on the basis of the full text by 2 of the reviewers (R.S. and J.G.) to ensure that these met the inclusion criteria. This process was facilitated by the use of a template which was developed to allow extraction of the study characteristics. The template included a section to explain the rationale behind each reviewer’s decision on whether the paper should be included in the review, excluded or if the reviewer was uncertain. The 2 reviewers subsequently compared their decisions for each paper and any disagreement was resolved by discussion with the third reviewer (P.C.) until consensus was achieved.
The review process was conducted by using RefWorks (2023) (ProQuest LLC).
Data Charting Process
Data extraction from the retained papers was performed using a data-charting form developed by 1 of the authors (R.S.). The process was iterative, involving 2 reviewers (R.S. and J.G.) who charted the data independently. Any disagreement was then discussed, and the information extracted from the studies was updated accordingly. To guarantee the effectiveness of data extraction, a trial run was carried out with a sample of 4 papers to check for any required amendments before the data were extracted from all the papers. No amendment was required.
Data Items
Data items included the author’s name, year, country, study design, population details, sample size, methods, intervention and control details, measured outcomes, time intervals at which outcomes were assessed and study results.
Synthesis of Results
Given the heterogeneity in behavioral therapies tested in the studies included in this scoping review, a narrative approach was used to synthesize the results for each behavioral therapy.
Results
Papers Included in the Review
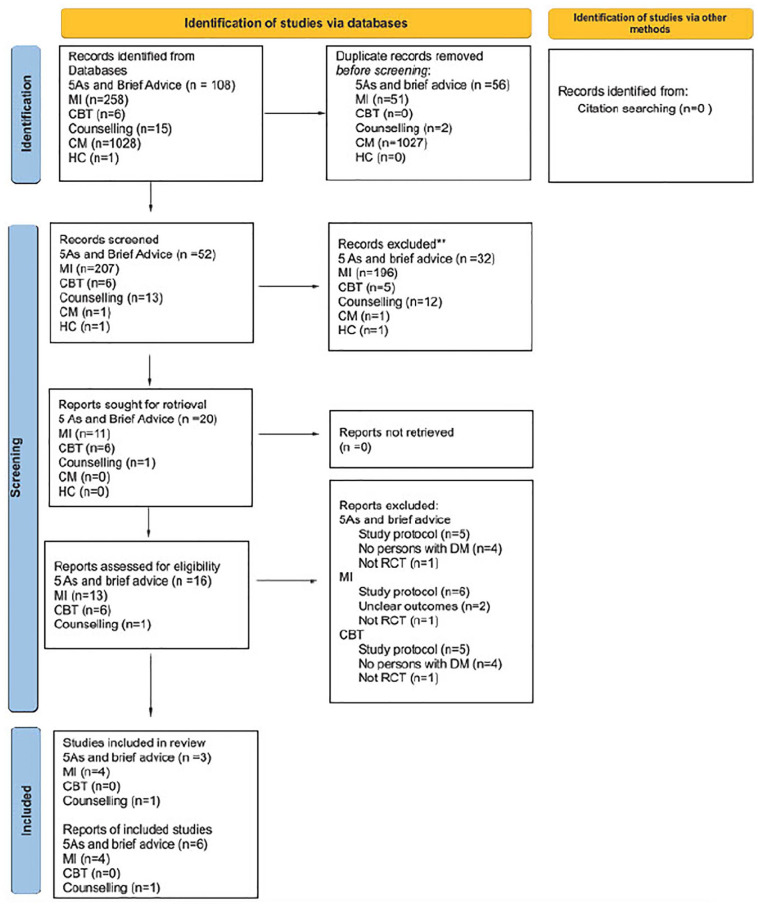
The PRISMA flow chart presented in Figure 1, provides a trail of the selection of studies on the behavioral therapies which were included in this review, that is the 5As model and brief advice, Cognitive Behavioral Therapy, Motivational Interviewing, Contingency Management, Health Coaching and Counselling. As seen in Figure 1, a total of 1615 papers were identified by the search strategy described in section 2.2 and 2.3.
Figure 1.
PRISMA 2020 flow diagram for scoping review of behavioral therapy to assist smoking cessation in persons with Diabetes Mellitus.
Source: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71.
Abbreviations: Ml, motivational interviewing; CBT, cognitive behavioral therapy; CM, contingency management; HC, health coaching.
Of these, 107 hits were related to papers on the 5As and brief advice. As seen in Figure 1, following removal of duplicates and scanning of the papers on the basis of their title and abstract, 16 papers were identified for retrieval. Following assessment of eligibility for inclusion on the basis of the full text, 11 papers were excluded as these were reports of study protocols, did not include persons with diabetes, did not include the 5As or brief advice in their intervention or did not use a randomized controlled design. The alerts set on the databases identified an additional relevant paper in November 2023, which was included in the review. In summary, 6 papers, reporting 3 studies, were retained.
There were a total of 258 hits for motivational interviewing. As seen in Figure 1, following removal of duplicates and scanning of the papers on the basis of their title and abstract, 13 papers were identified for retrieval. Following assessment of eligibility for inclusion on the basis of the full text, 9 papers were excluded as these were reports of study protocols, had unclear outcomes or did not use a randomized controlled design. Four papers reporting 4 studies on the use of Motivational Intervention were retained.
There were a total of 6 hits for Cognitive Behavioral Therapy. As seen in Figure 1, following removal of duplicates and scanning of the papers on the basis of their title and abstract, 1 paper was identified for retrieval. This was not eligible for inclusion in the review as it reported a study protocol. No studies on the use of Cognitive Behavioral Therapy were therefore included in this review.
There were a total of 147 hits for counseling. As seen in Figure 1, following removal of duplicates and scanning of the papers on the basis of their title and abstract, 11 papers were identified for retrieval. Following assessment of eligibility for inclusion on the basis of the full text, 10 papers were excluded as these were reports of study protocols, did not actually use counseling as an intervention, include a survey of nurses’ views on the use of counseling in smoking cessation with persons with diabetes, included both persons living with cardiac conditions and diabetes, but did not present results for the 2 cohorts separately. One study designed the use of counseling as a non-intensive comparison rather than an intervention. One paper reporting 1 study on the use of counseling to assist smoking cessation in persons living with diabetes was retained.
There were a total of 1028 hits for Contingency Management. As seen in Figure 1, following removal of duplicates and scanning of the papers on the basis of their title and abstract, 1 paper was identified for retrieval. This was not eligible for inclusion in the review as it reported a study protocol. No studies on the use of Contingency Management were therefore included in this review.
There were a total of 75 hits for Health Coaching. As seen in Figure 1, following removal of duplicates and scanning of the papers on the basis of their title and abstract, 1 paper was identified for retrieval. This paper was not deemed to be eligible for inclusion in the review in view of the concomitant use of Varenicline in the intervention group which made it difficult to separate the effects of pharmacotherapy from that of the behavioral therapy, in this case, health coaching. No studies on the use of Health Coaching were therefore included in this review.
The studies on the 5As and brief advice, motivational interviewing and counseling which are included in this scoping review are described and summarized in Table 2.
Table 2.
Studies on the Use of Behavioral Therapies to Promote Smoking Cessation in People With Diabetes.
| Authors (Country) | Design | Sample, Sample Size and Method | Intervention | Control | Outcome |
|---|---|---|---|---|---|
| 5 As and brief advice | |||||
| Albaroodi et al. (2023) Malaysia |
Randomized controlled trial | Patient with diabetes who smoked tobacco. Site: Outpatiets Clinic Intervetionn: n = 63 Control: n = 63 |
5 mintue physician-delivered brief counseling session using 5As. Usual care |
Usual care | Outcomes measured at baseline and at subsequent 3 and 6 months visits Quitting rate Mean number of cigarettes smoked Verified by breath CO test. |
| Lam et al 2017 Li et al 2017 Hong Kong |
Randomized controlled trial | Patients in nine major diabetes clinics, with t2D, smoking 2 cigarettes a day over the past 30 days; 18 years and over. n = 557 Intervention group n = 283 Control group n = 274 |
Brief (20- minute) individualized face-to-face counseling adapted from 5 As approach by trained nurses and a diabetes mellitus-specific leaflet. Telephone follow-up with intervention at 1 week, 1 month. |
Usual care and self-help pamphlet | Self-reported 7-day point-prevalence smoking abstinence at 12 months. Exhaled carbon monoxide test (≥4 ppm) Data collected at 3, 6, and 12 months. No significant difference in 7-day point-prevalence smoking abstinence (9.2% vs. 13.9%; P = .08). Biochemically validated quit rate, n (%) 12 months 9 (3.2) 14 (5.1) P = .25 |
| Thankappan et al. 2014 Thankappan et al 2013a Thankappan et al. 2013b India |
Randomized controlled trial | 224 adult male diabetic patients aged 18 years who smoked in the previous month from two dia-betes clinics Randomly assigned to intervention and control (n = 112 in each group) |
Asked and advised by a doctor to quit smoking and education materials on smoking-related complications. Diabetes specific 30-min smoking cessation counseling sessions using the five “As” (Ask, Assess, Advise, Assist, Arrange) and the five “Rs” (Relevance, Risks, Rewards, Roadblocks, Repetition) from a trained and certified health care professional. Reminder by doctor to quit smoking at 1, 3, and 6 months |
Asked and advised by a doctor to quit smoking and education materials on smoking-related complications. Reminder by doctor to quit smoking at 1, 3, and 6 months |
Self-reported abstinence for at least 7 days. harm reduction (reduction of smoking more than 50% of base-line use). Salivary cotinine tests after 1-year follow-up Odds of quitting significantly higher In intervention than control group (adjusted odds ratio [AOR] 3.35; 95% CI 1.82 to 6.18)Odds of quitting or harm reduction in the Intervention group were higher compared to the control (AOR 2.21; 95% CI 1.24-3.93). |
| Motivational Interviewing | |||||
| Perez-Tortosa et al. (2015) |
Perez-Tortosa et al. (2015) |
43 primary care teams from the province of Barcelona 722 people with diabetes who were smokers |
Motivational interview and therapies and medications adapted to the patient’s stage of change n = 345 |
No information on control n = 377 |
1 year follow up Continued abstinence was defined as at least 6 months without smoking and a carbon monoxide (CO) breath level of < 6 ppm measured by a cooximeter in standard conditions. |
| Intensive advice in diabetic patients in primary care (ITADI) study Spain |
Cluster Randomised Controlled Multicentre Study | T1 or T2, 14 years or older | Number of intervention visits varied according to the stage of the patient (five for precontemplation, seven for contemplation and eight for preparation/action). Patients could move from one stage to another with intervention adapted to change Patients in the intervention group attended a median (Q1–Q3) of 4 (2-6) visits, with a total cumulative time of all visits of 100 (48.8-183.3) min and a median time spent per visit of 22.1 (15-37.7) min. |
After 1 year, continued abstinence was recorded in 90 (26.1%) patients in the intervention group and in 67 (17.8%) controls ( P = .007). In patients with smoking abstinence, there was a higher percentage in the precontemplation and contemplation stages at baseline in the intervention group than in controls (21.2% vs. 13.7%, P = .024). When the precontemplation stage was taken as reference (OR = 1.0), preparation/action stage at baseline showed a protective effect, decreasing 3.41 times odds of continuing smoking (OR = 0.293 95% CI 0.179-0.479, |
|
| Rubak et al (2011) A sub-study of the ADDITION study Denmark |
Multi-centre randomized controlled trial | 40- to 69-year-old people with screen-detected type 2 diabetes. | Motivational interviewing n = 37 |
Control not described n = 43 |
1 year follow-up Self-reported smoking taken from the Summary of Diabetes Self-Care Activities questionnaire. No significant difference between the number of non-smokers in the control (71.2%) and intervention group (66.1%). |
| Heinrich et al. (2010) The Netherlands |
Cluster randomized controlled trial | All patients with T2D in practice of 33 nurses n = 1517 41% consented to participate (n = 618) Districts randomly assigned to intervention and control. Intervention: patients of 18 nurses in 2 districts Control: patients of 15 nurses in 2 districts |
Counseling intervention based on MI and health behavior change counseling lasting around 20 min Online educational program web-based education (www.diep.info) |
Online educational program web-based education (www.diep.info) | Outcomes measured at 12 and 24 months Smoking assessed using the Summary of Diabetes Self-Care Activities Scale: self report of smoking during the past 7 days (yes/no). No significant difference between the intervention and control group at 12 and 24 months follow-up |
| Hokanson et al. (2006) USA |
Randomized controlled trial | n = 114 (persons already registered in educational program) 21 to 80 years of age With type 2 diabetes Current or previous smokers: Had smoked at least 100 cigarettes in their lifetime Current: smoked daily or on most days Recent quitters: had stopped smoking in the previous 3 months. Random allocation to intervention and control |
n = 57 Face to face motivational interviewing of 20 min duration; additional 3 to 6 telephone counseling lasting an average of 10 min each. Offer of free medication to those willing to quit: Nicotine replacement therapy (transdermal patch or gum) or bupropion Offered as part of usual diabetes education |
n = 57 Standard care Information on local smoking cessation programs |
3 months and 6 months follow up Number of cigarettes smoked in last 7 days and % who smoked daily at 3 and 6 months Salivary cotinine levels at 6 months No significant difference between intervention and control group at 3 and 6 months |
| Counseling | |||||
| Canga et al. (2000) Spain |
Multi-centre randomized controlled trial | Smokers with diabetes: type 1 or type 2 aged between 17 and 84 years. Recruited from 15 primary care centres and 2 hospitals. n = 280 Randomized into: Intervention group (n = 147) Control group (n = 133) |
40-min nurse led counseling, education, and setting a negotiated cessation date. NRT offered to 105 patients (71% of the intervention group) for 3 months. 10 completed NRT therapy |
Usual care | Baseline and 6-month follow-up Self-reported smoking cessation Urine cotinine concentraion Mean number of cigarettes smoked per day Stage of change (Prochaska’s model of change). At 6-months 17.0% smoking cessation rate in the intervention group compared to 2.3%; difference of 14.7% (95% CI 8.2-21.3%). Those who continued smoking, a significant reduction in average cigarette consumption with mean number of cigarettes per day decreased from 20.0 at baseline to 15.5 at for the experimental group versus from 19.7 to 18.1 for the control group (P 0.01). |
The 5As and Brief Advice and Smoking Cessation in DM
The 3 studies (Table 2) which examined the effectiveness of the 5As and brief advice in supporting smoking cessation in DM present conflicting results with the results of 1 study17 -19 reporting a higher odds of quitting smoking in persons in the intervention group whilst the other 2 studies20 -22 reported no significant result.
These inconsistent results are likely due to the differences between the interventions used in the studies. The study by Thankappan et al included delivery of 30-minute counseling sessions which included the 5As together with the 5 Rs, that is relevance, risks, rewards, roadblocks and repetition.17 -19 The intervention delivered in the study reported by Li et al and Lam et al was less intensive, with one 20-minute counseling session which had been adapted from the 5As and telephone follow-ups after 1 week and 1 month.21,22 The intervention by Albaroodi et al was the least intensive, consisting of a 5-minute session utilizing the 5As. 20
The difference in results may therefore be due to the length of the counseling sessions and the number and length of follow-up, where smokers are reminded to quit smoking.
Motivational Interviewing and Smoking Cessation in DM
Similar to the results of the studies on the use of the 5As and brief advice, the results for the studies on the effectiveness of motivational interviewing in persons with DM to assist with smoking cessation are inconsistent. Of the 4 studies which explored the effectiveness of motivational interviewing, only Perez-Tortosa et al reported a positive significant difference in smoking cessation with the motivational interviewing intervention.23 -26
Once more, whilst all the studies utilized motivational interviewing there were substantial differences in the way in which the latter was delivered in the different studies. The main outstanding difference in the study by Perez-Tortosa et al when compared to the other studies, was the use of an intensive intervention which was also adapted to the individual participant according to their level of change. 25 This meant that the number of sessions each participant received varied between 5 and 7 sessions. The participants’ level of change was assessed regularly; the intervention received, therefore, was dynamic and based on the person’s current needs.
Counseling and Smoking Cessation in DM
One study explored the effectiveness of counseling in assisting persons living with diabetes to quit smoking. 27 The intervention delivered included a 40-min nurse-led counseling session combined with education, and the negotiated setting of a smoking cessation date with the participants. Nicotine Replacement Therapy was also offered for a period of 3 months to under half (n = 105) of the intervention group (n = 208), although only 10 participants utilized the Nicotine Replacement therapy for the whole prescribed period. The results of this study showed a positive statistically significant difference in smoking cessation with the use of the counseling intervention; for those who did not stop smoking in the intervention group, there was a significant decrease in the number of cigarettes smoked.
Discussion
The Current Scope of Research on Behavioural Interventions to Assist Smoking Cessation
The present review has explored various psychological interventions for smoking cessation in individuals with diabetes, including the 5As and brief advice, Cognitive Behavioral Therapy, Motivational Interviewing, Contingency Management, Health Coaching and Counseling. The results of this review show that a number of psychological interventions, particularly Cognitive Behavioral Interventions, which have been shown to be effective in supporting smoking cessation in the general population and has been extensively researched in the management of chronic diseases, have as yet not been researched in relation to persons living with diabetes.28 -30 This gap in the literature creates an excellent opportunity for the development of knowledge in relation to smoking cessation in persons with diabetes.
The behavioral therapies which have been researched amongst smokers with diabetes are the 5 As, Motivational Interviewing and Counseling. The results of the studies for the first 2 are contradictory. For both the 5 As and motivational interviewing, a possible explanation may be that intensive interventions are required with multiple sessions of at least 30 min each being required. The results of Perez-Tortosa et al suggest that a dynamic intervention with the proactive adaptation of the intervention to the person’s level of change is helpful in assisting with smoking cessation. 25 These results mirror those in a systematic review which sought to identify the components of successful smoking cessation interventions in persons living with DM. 13 This reported that in general, irrespective of the smoking cessation intervention, an intervention including 3 to 4 sessions, lasting more than 20 min each, was more likely to be associated with smoking cessation success. 13
Directions for Future Research on the Use of Behavioural Therapies to Assist Persons With DM to Quit Smoking
The results of this and previous reviews provide the basis for a framework for the development of behavioral support interventions for persons with diabetes who smoke. The intensive interventions identified as being effective to date could serve to build structured behavioral therapy programs for persons with diabetes. Structured programs need to be evidence-based, and suit the needs of the person, must have specific aims and objectives, and support the person and their family members and carers in developing attitudes, beliefs, knowledge and skills. 31 The structured program must stipulate and provide in written form the content to be delivered to persons with diabetes, the mode of delivery, the number of sessions to be included, the use of aides, such as written, audio-visual or technological materials. 31 The persons delivering the intervention must have received accredited training and certification and the program must be quality assured and must be regularly reviewed by independent assessors who also check for consistency in the delivery of the program. 31 The outcomes of the program must also be audited regularly. 31
Structured educational programs have been consistently found to be effective in improving self-management and glucose stability in persons with diabetes, when compared to unstructured approaches where the delivery of the intervention is left to the discretion of the different health care providers.32 -35 In view of the latter, it is recommended that the development and evaluation of a structured behavioral program on the basis of the 5As and motivational interviewing, which include the components of the interventions delivered by Thankappan et al, Thankappan et al and Perez-Tortosa et al should be the focus of future research.17,19,25 Other behavioral therapies including counseling need to be further researched to identify the intervention components which are effective, before structured programs are developed and tested.
Nicotine is a highly addictive chemical which results in physical and psychological withdrawal symptoms when a person seeks to stop smoking, making smoking cessation very difficult. 36 In view of this, the use of nicotine replacement therapy or other drug treatments such as varenicline or bupropion are likely to be required to assist with smoking cessation in persons receiving behavioral therapy to improve the outcomes of the latter. The 2 studies included in this review, which utilized nicotine replacement therapy, do not provide an indication if this assumption could be true, since the research design of these studies does not allow an assessment of the specific contribution of the behavioral therapy and nicotine replacement therapy to the outcomes, individually or in combination with each other.24,27 Future studies should include 3 arm randomized controlled trials which would allow the exploration of the added benefits of combining behavioral therapies with nicotine replacement therapy or other smoking cessation medications.
Strengths and Limitations of the Scoping Review
This scoping review sought to be comprehensive in terms of the search, included 2 reviewers throughout and sought to present the results transparently to allow evaluation of the conclusions reached and allow replicability of the review.
In view of the complexity of the interventions reviewed, the comparison and identification of the active components of the interventions as well as those components which were not effective in encouraging smoking cessation in persons with diabetes was problematic and this is a limitation in arriving at conclusions.
Conclusion
This scoping review has highlighted the limited research available in relation to the use of behavioral therapy to assist with smoking cessation in persons with DM. This therefore is a research area which should attract the attention of researchers with an interest in diabetes care and smoking cessation, particularly in view of the increased risk of complications as a result of smoking experienced by persons living with diabetes. This research should focus on the development of a structured behavioral therapy program using the 5As and Motivational Interviewing as well as more basic research in relation to other behavioral therapies, such as Cognitive Behavioral therapy, in view of continued unclear outcomes of these therapies. Also required is the use of 3 arm randomized controlled trials to evaluate the possible added benefits of accompanying behavioral interventions with nicotine replacement therapy or other drugs used to assist with smoking cessation.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Roberta Sammut  https://orcid.org/0000-0002-2354-8808
https://orcid.org/0000-0002-2354-8808
References
- 1. World Health Organisation. Diabetes. Updated 2023. Accessed June 27, 2023. https://www.who.int/news-room/fact-sheets/detail/diabetes.
- 2. Action on Smoking and Health, (ASH). Smoking statistics. Updated 2023. Accessed June 27, 2023. https://ash.org.uk/uploads/Smoking-Statistics-Fact-Sheet.pdf?v=1697728811.
- 3. West R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol Health. 2017;32(8):1018-1036. doi: 10.1080/08870446.2017.1325890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Durlach V, Vergès B, Al-Salameh A, et al. Smoking and diabetes interplay: a comprehensive review and joint statement. Diabetes Metab. 2022;48. 6. doi: 10.1016/j.diabet.2022.101370 [DOI] [PubMed] [Google Scholar]
- 5. Pan A, Wang Y, Talaei M, Hu FB. Relation of smoking with total mortality and cardiovascular events among patients with diabetes mellitus: a meta-analysis and systematic review. Circulation. 2015;132(19):1795-1804. doi: 10.1161/CIRCULATIONAHA.115.017926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88-98. doi: 10.1038/nrendo.2017.151 [DOI] [PubMed] [Google Scholar]
- 7. Baena-Díez JM, Peñafiel J, Subirana I, et al.; On behalf of the FRESCO Investigators. Risk of cause-specific death in individuals with diabetes: a competing risks analysis. Diabetes Care. 2016;39(11):1987-1995. doi: 10.2337/dc16-0614 [DOI] [PubMed] [Google Scholar]
- 8. Li S, Wang J, Zhang B, Li X, Liu Y. Diabetes mellitus and cause-specific mortality: a population-based study. Diabetes Metab J. 2019;43(3):319-341. doi: 10.4093/dmj.2018.0060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Campagna D, Alamo A, Di Pino A, et al. Smoking and diabetes: dangerous liaisons and confusing relationships. Diabetol Metab Syndr. 2019;11(1):85. doi: 10.1186/s13098-019-0482-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grech J, Norman IJ, Sammut R. Helping smokers with diabetes quit: a scoping review of the interventions utilised, and the challenges and barriers to smoking cessation. Prim Care Diabetes. 2023;17(2):119-128. doi: 10.1016/j.pcd.2023.01.005 [DOI] [PubMed] [Google Scholar]
- 11. Chau TK, Fong DY, Chan SS, et al. Misconceptions about smoking in patients with type 2 diabetes mellitus: a qualitative analysis. J Clin Nurs. 2015;24(17-18):2545-2553. doi: 10.1111/jocn.12854 [DOI] [PubMed] [Google Scholar]
- 12. Stead LF, Koilpillai P, Fanshawe TR, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst Rev. 2016;3(3):CD008286. doi: 10.1002/14651858.CD008286.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Grech J, Norman IJ, Sammut R. Effectiveness of intensive stand-alone smoking cessation interventions for individuals with diabetes: a systematic review and intervention component analysis. Tob Induc Dis. 2023;21:57. doi: 10.18332/tid/162329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19-32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 15. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. doi: 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467-473. doi: 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 17. Thankappan KR, Mini GK, Daivadanam M, et al. Pp034 feasibility of disease centered smoking cessation among diabetes patients. Respir Med. 2013;107:S16. https://www.sciencedirect.com/science/article/pii/S095461111370057X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Thankappan KR, Mini GK, Daivadanam M, et al. Smoking cessation among diabetes patients: results of a pilot randomized controlled trial in kerala, india. BMC Public Health. 2013;13(1):47. doi: 10.1186/1471-2458-13-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thankappan KR, Mini GK, Hariharan M, et al. Smoking cessation among diabetic patients in Kerala, India: 1-year follow-up results from a pilot randomized controlled trial. Diabetes Care. 2014;37(12):e256-e257. doi: 10.2337/dc14-1863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Albaroodi K, Sulaiman S, Awaisu A, Shafie A. Impact of brief smoking cessation intervention on abstinence rate and glycaemic control in patients with diabetes mellitus: A randomised controlled trial. 2021. ;51(10). doi: 10.21203/rs.3.rs-149819/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lam T, Li W, Wang M, et al. A brief, tailored smoking cessation intervention for smokers with diabetes mellitus in Hong Kong. Hong Kong Med J. 2017;23 Suppl 2(3):10-11. [PubMed] [Google Scholar]
- 22. Li WH, Wang MP, Lam TH, et al. Brief intervention to promote smoking cessation and improve glycemic control in smokers with type 2 diabetes: a randomized controlled trial. Sci Rep. 2017;7. doi: 10.1038/srep45902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Heinrich E, Candel MJ, Schaper NC, de Vries NK. Effect evaluation of a motivational interviewing based counselling strategy in diabetes care. Diabetes Res Clin Pract. 2010;90(3):270-278. doi: 10.1016/j.diabres.2010.09.012 [DOI] [PubMed] [Google Scholar]
- 24. Hokanson JM, Anderson RL, Hennrikus DJ, Lando HA, Kendall DM. Integrated tobacco cessation counseling in a diabetes self-management training program: a randomized trial of diabetes and reduction of tobacco. Diabetes Educ. 2006;32(4):562-570. doi: 10.1177/0145721706289914 [DOI] [PubMed] [Google Scholar]
- 25. Pérez-Tortosa S, Roig L, Manresa JM, et al.; ITADI Study Group. Continued smoking abstinence in diabetic patients in primary care: a cluster randomized controlled multicenter study. Diabetes Res Clin Pract. 2015;107(1):94-103. doi: 10.1016/j.diabres.2014.09.009 [DOI] [PubMed] [Google Scholar]
- 26. Rubak S, Sandbæk A, Lauritzen T, Borch-Johnsen K, Christensen B. Effect of “motivational interviewing” on quality of care measures in screen detected type 2 diabetes patients: a one-year follow-up of an RCT, ADDITION Denmark. Scand J Prim Health Care. 2011;29(2):92-98. doi: 10.3109/02813432.2011.554271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Canga N, De Irala J, Vara E, et al. Intervention study for smoking cessation in diabetic patients: a randomized controlled trial in both clinical and primary care settings. Diabetes Care. 2000;23(10):1455-1460. doi: 10.2337/diacare.23.10.1455 [DOI] [PubMed] [Google Scholar]
- 28. Vinci C. Cognitive behavioral and mindfulness-based interventions for smoking cessation: a review of the recent literature. Curr Oncol Rep. 2020;22(6):58-w. doi: 10.1007/s11912-020-00915-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Nalder E, Marziali E, Dawson DR, Murphy K. Delivering cognitive behavioural interventions in an internet-based healthcare delivery environment. Br J Occup Ther. 2018;81(10):591-600. doi: 10.1177/0308022618760786 [DOI] [Google Scholar]
- 30. Lukkatai N, Inouye J, Thomason D, et al. Integrative review on cognitive behavioral therapy in chronic diseases: the responses predictors. Iris Journal of Nursing and Care. 2019;1. doi: 10.33552/ijnc.2019.01.000525 [DOI] [Google Scholar]
- 31. National Institute for Clinical Excellence, (NICE). Quality statement 2: Structured education programme. In: Type 2 diabetes in adults; quality standard [QS209]. United Kingdom, 2023. Accessed November 2, 2023. [Google Scholar]
- 32. Wheatley SD, Arjomandkhah NC, Murdoch C, et al. Improved blood glucose control, cardiovascular health and empowerment in people attending X-PERT structured diabetes education. Pract Diabetes. 2021;38(6):31-35. doi: 10.1002/pdi.2368 [DOI] [Google Scholar]
- 33. Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the diabetes X-PERT programme makes a difference. Diabet Med. 2006;23(9):944-954. doi: 10.1111/j.1464-5491.2006.01906.x [DOI] [PubMed] [Google Scholar]
- 34. Elliott J, Jacques RM, Kruger J, et al. Substantial reductions in the number of diabetic ketoacidosis and severe hypoglycaemia episodes requiring emergency treatment lead to reduced costs after structured education in adults with type 1 diabetes. Diabet Med. 2014;31(7):847-853. doi: 10.1111/dme.12441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chatterjee S, Davies MJ, Heller S, et al. Diabetes structured self-management education programmes: a narrative review and current innovations. Lancet Diabetes Endocrinol. 2018;6(2):130-142. doi: 10.1016/S2213-8587(17)30239-5 [DOI] [PubMed] [Google Scholar]
- 36. National Institute on Drug Abuse, (NIDA). Is nicotine addictive? Updated 2021. Accessed Novemer 6, 2023. https://nida.nih.gov/publications/research-reports/tobacco-nicotine-e-cigarettes/nicotine-addictive.