Abstract
Significant inconsistencies in respiratory care provision for Duchenne muscular dystrophy (DMD) are reported across different specialist neuromuscular centres in the UK. The absence of robust clinical evidence and expert consensus is a barrier to the implementation of care recommendations in public healthcare systems as is the need to increase awareness of key aspects of care for those living with DMD. Here, we provide evidenced-based and/or consensus-based best practice for the respiratory care of children and adults living with DMD in the UK, both as part of routine care and in an emergency.
Methodology
Initiated by an expert working group of UK-based respiratory physicians (including British Thoracic Society (BTS) representatives), neuromuscular clinicians, physiotherapist and patient representatives, draft guidelines were created based on published evidence, current practice and expert opinion. After wider consultation with UK respiratory teams and neuromuscular services, consensus was achieved on these best practice recommendations for respiratory care in DMD.
Result
The resulting recommendations are presented in the form of a flow chart for assessment and monitoring, with additional guidance and a separate chart setting out key considerations for emergency management. The recommendations have been endorsed by the BTS.
Conclusions
These guidelines provide practical, reasoned recommendations for all those managing day-to-day and acute respiratory care in children and adults with DMD. The hope is that this will support patients and healthcare professionals in accessing high standards of care across the UK.
Keywords: respiratory measurement, critical care, emergency medicine, referral and consultation, respiratory muscles
Introduction and scope
This is a consensus summary from an expert respiratory working group (WG) of UK adult and paediatric respiratory and neuromuscular specialists and specialist physiotherapists from the UK’s NorthStar Network—all with experience in the management of patients with DMD as well as patient representatives. The work builds on the existing evidence and international expert opinion, including the international consensus statement on recommended standards of care (SoC) in DMD1 and the British Thoracic Society (BTS) guideline for respiratory management of children with neuromuscular weakness.2
The guidance is intended to give evidence-based and expert opinion-based recommendations for all clinicians involved with the monitoring, care and management of respiratory function and complications in people living with Duchenne muscular dystrophy (DMD). We add here to the current body of literature, by offering a practical and feasible approach to addressing both planned and acute respiratory care needs in the context of UK public healthcare systems. The guidance encompasses respiratory issues seen in children and adults across the various stages of DMD and seeks to address specific concerns raised by patients, their carers and clinicians in relation to access to appropriate, high standard respiratory care.
The guidelines referred to here have been endorsed by the British Thoracic Society, October 2022
Background: about DMD
DMD is a genetic condition caused by mutations in the DMD-gene, located on the X chromosome, which codes for the protein dystrophin.3 4 Depending on the specific mutation, these result in a more or less truncated (and non-functioning) form of the protein. Because of X-linkage, the vast majority of people diagnosed with DMD are male, although rarely female carriers may be ‘manifesting’ and also develop significant symptoms.5
Dystrophin is key to muscle fibre integrity and repair and without its functional form, skeletal muscles are progressively damaged over time, resulting in fibrosis and fat replacement.6 Although rare, DMD is the most common (and severe) form of muscular dystrophy in children and affects around 1:5000 live male births worldwide.7 In the UK today, there are approximately 2500 boys and men living with the disease.8
The average age of diagnosis in the UK is around 4 years.9 Skeletal muscles are the first to be noticeably affected and patients then experience progressive muscle weakness and wasting leading to gradual decline in motor function and tend to stop walking in their early teens.
The impact of DMD on respiratory function, largely as a result of intercostal and diaphragm muscle weakness,10 normally becomes noticeable after loss of ambulation (LOA), in adolescence and into adulthood, although there is significant heterogeneity in the onset of respiratory symptoms.11 Ventilatory support is frequently required at this stage of the disease—initially overnight but later it may be needed 24 hours/day.
Respiratory complications in DMD are related to inspiratory and expiratory muscle weakness. Inspiratory muscle weakness initially causes nocturnal hypoventilation and contributes to sleep-disordered breathing. Expiratory muscle weakness can cause a poor cough and inability to effectively manage respiratory secretions. The consequences of untreated respiratory muscle weakness include respiratory failure and pneumonia.
Respiratory complications are a major cause of morbidity, unplanned hospital admission and remain the second most frequent cause of death in DMD, after cardiac failure.12
DMD also affects the heart muscle and leads to a progressive dilated cardiomyopathy.13 Pro-active implementation of SoC including early introduction of cardiac medication can delay the onset and/or slow progression of cardiomyopathy in DMD.14 Cardiac involvement can impact respiratory function and in turn, respiratory failure can trigger cardiac arrhythmias or exacerbate cardiac failure.
There is currently no effective treatment for DMD. Corticosteroids are routinely recommended from a young age because they slow the rate of decline in muscle function and prolong ambulation.1 Corticosteroids have also been shown to delay respiratory decline and help to preserve ventilatory function for longer.15
Maintaining respiratory health is vital to prolonging survival and quality of life in DMD.16 With current SoC in the UK, median life expectancy for males with DMD is between 29 and 30 years of age.17
Background: drivers for new guidance
The international care standards for DMD include recommendations for respiratory management.1 There is, however, limited guidance about the emergency management of respiratory complications and the advice regarding monitoring and intervention has not been universally adopted across the UK, in part because of a lack of consensus among respiratory physicians in relation to some of the recommendations.
DMD Care UK is a collaborative initiative between expert clinicians and the patient community, led by Newcastle University and Duchenne UK—a prominent DMD charity in the UK (duchenneuk.org). DMD Care UK was formally established in 2020 to address gaps between UK DMD care-delivery and international recommendations and to harmonise care between centres across the UK—to ensure the best care for all and to better empower patients to be active participants in their own care.
During set-up, DMD Care UK conducted two surveys to gauge experiences of care provision for those living with DMD in the UK, and these were used to set priorities for the project as whole including highlighting gaps between international recommendations1 for management, including respiratory care, and the provision of care at different centres.
The first was a survey of clinicians working within the specialist paediatric neuromuscular centres of the UK NorthStar Network in 2019. Each centre was given a list of the key areas of the international care recommendations and asked to rate how well they were able to implement each one. Where there was not full implementation, centres were asked to state why this was (lack of evidence, lack of resource, lack of awareness or other).
This was followed by a survey of DMD families in 2021. Using Duchenne UK’s networks, families or individuals were asked to rate their understanding of, and satisfaction with, the key areas of care with open text options to comment on each.
Responses from 12 (of 24) paediatric NorthStar centres and 167 responses from parents/patients were received. The responses gave a broad picture and impression rather than offering statistical significance, and collated results have been presented with this caveat at Duchenne UK’s patient information days as well as at the NorthStar Network’s annual meetings.
One example shows that, in relation to the 2018 respiratory care recommendations, NorthStar centres reported 70% compliance with the recommended 6 monthly assessments for non-ambulant patients, while families reported these assessments were only done in 35%–67% of patients depending on the disease stage of the patient.
While only providing a snapshot of current provision, the surveys re-emphasised the need for more guidance around emergency and routine respiratory care. They highlighted the importance of empowering patients to make informed decisions and to advocate for their care, by providing appropriate information and facilitating discussion with relevant teams, including palliative care. While 75% of families reported a good/excellent understanding of the respiratory SoC, 23% reported a poor/very poor understanding, underlining the fact that any new guidance needs to be disseminated effectively and be readily accessible to families as well as to healthcare professionals who might have less experience with DMD. Those responding are likely to be the most engaged and informed within the patient community and thus the true national picture can be expected to be worse.
The clinician survey captured some of the reasons for non-compliance with published international SoC and these included: a lack of evidence to support individual recommendations, the need to make judgements based on multiple single factors, for example, in relation to timing and use of ventilatory support, lack of resources and issues with patient compliance.
Although the surveys may show selection bias given the specific sites and families who responded, and the effects of COVID-19 restrictions, the results highlight the need for clear and practical guidance with justified recommendations, based on evidence or expert opinion where evidence is lacking, to ensure best care is provided to all patients with DMD.
Methodology
The guideline presented and discussed in this paper has been produced by the Respiratory Care WG of DMD Care UK18 and has been endorsed by the BTS.
The Respiratory Care WG is formed of eight paediatric and adult respiratory clinicians with expertise in DMD, including two representatives from the BTS, three neuromuscular consultants, four respiratory specialist physiotherapists and two patient representatives. These group members were included after invitations to volunteer were targeted to lead specialists at UK NorthStar centres,19 and through Duchenne UK’s family networks. Professional expertise was the primary consideration in the setting-up of the group, but geographical spread was also considered to achieve as wide a representation as possible. Volunteers were also requested to join from the parallel physiotherapy WG of DMD Care UK to ensure good collaboration between the two WGs and alignment of guidelines. Once established, the WG reviewed current practice in the UK based on the surveys of clinicians and of families against international recommendations,1 further reporting from colleagues, wider published literature and expert clinical opinion.
Through a series of online meetings, a first draft guideline for recommended respiratory monitoring and care for people with DMD in the UK healthcare setting was agreed. This draft was circulated widely to respiratory clinicians, neuromuscular consultants and respiratory specialist physiotherapists working at each of the 24 neuromuscular NorthStar centres,19 to invite comment and input. Based on their feedback, revisions were agreed by the WG and additional input sought through repeated circulation, until consensus was reached by the WG. This agreed guideline was then submitted to the BTS for final review and their requested (minor) edits incorporated, to finally agree on the BTS-endorsed UK recommendation for respiratory care that we present in this paper.
These guidelines are aimed at all healthcare professionals involved in the care of patients with DMD, including those less familiar with the condition in accident and emergency, primary and secondary care settings.
Results
The BTS-endorsed, UK-consensus guideline for respiratory care in the DMD is presented for the first time in this paper. The guidelines should be followed for routine care (figure 1) and be referred to in circumstances where respiratory implications may be important, even if not the primary reason for medical care, for example, when preparing for a general anaesthetic, or during an unplanned admission to hospital (figure 2).
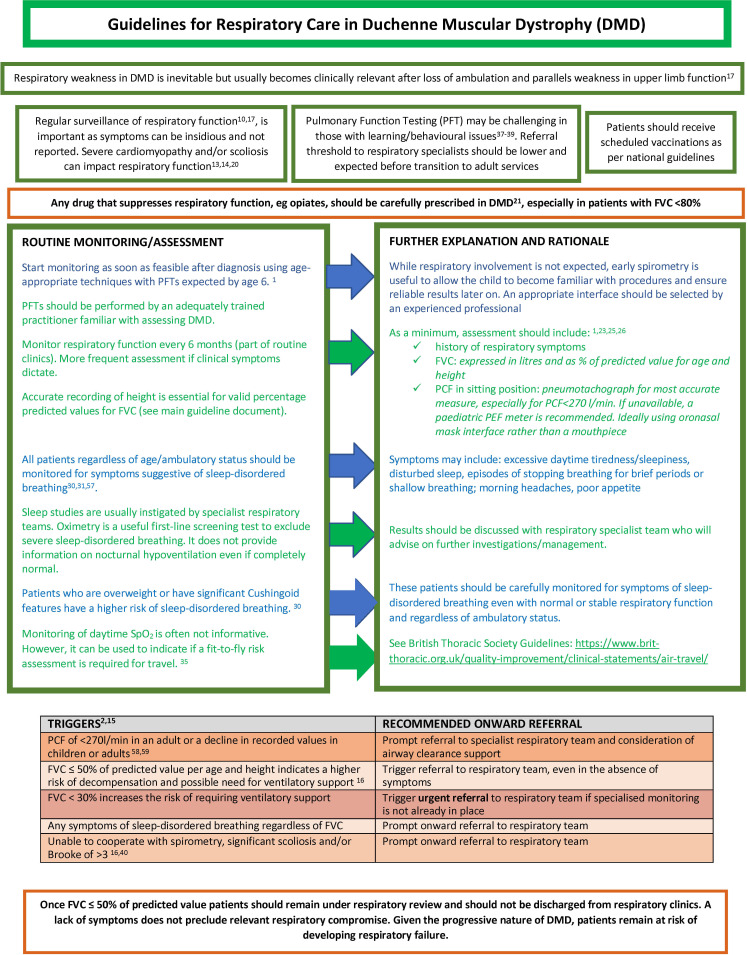
Figure 1.
Flow chart summary of respiratory routine standards of care for Duchenne muscular dystrophy (DMD). FVC, forced vital capacity; PCF, peak cough flow; PEF, peak expiratory flow.
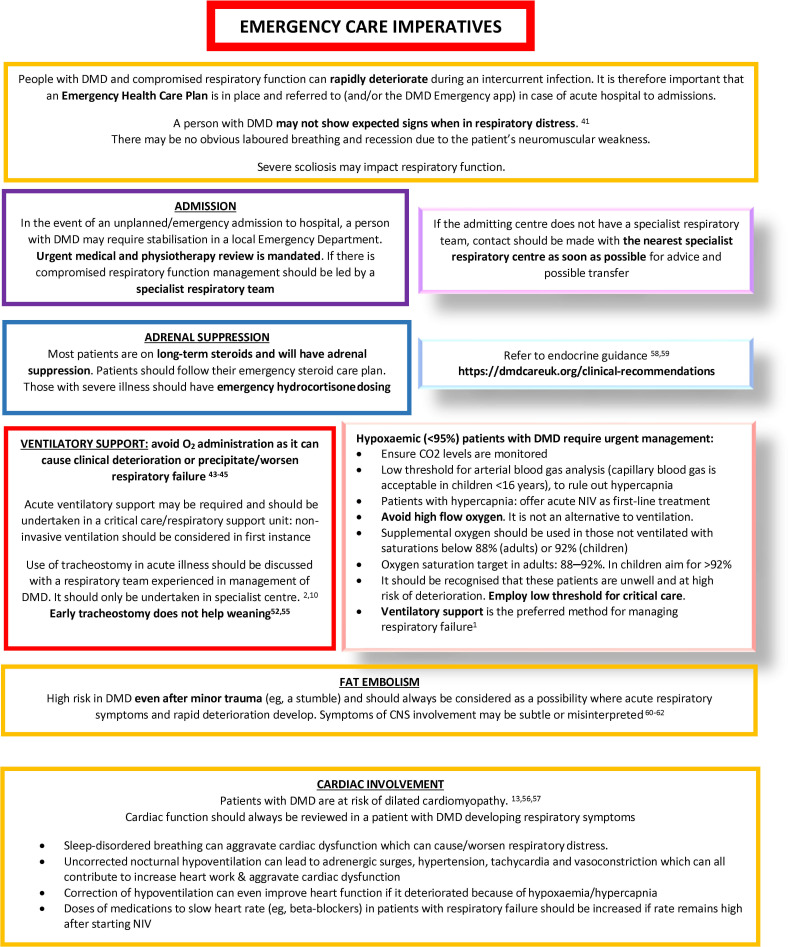
Figure 2.
Flow chart summary of respiratory care considerations for Duchenne muscular dystrophy (DMD) in an emergency or unplanned situation. CNS, central nervous system; NIV, non-invasive ventilation.
Figures 1 and 2 together present an accessible summary of this guideline.
Respiratory involvement in DMD
Respiratory weakness in DMD is inevitable but usually becomes clinically relevant after LOA and strongly correlates with progression of upper limb weakness.17
Patients and carers should be made aware that progressive weakness of respiratory muscles is part of the natural history of the disease and should be informed about early symptoms of sleep-disordered breathing and respiratory impairment.
Regular surveillance of respiratory function is critical as symptoms can be insidious and are often not reported by patients.10 17
The assessment of respiratory function in DMD needs to include a careful history to evaluate symptoms of sleep-disordered breathing, frequency of chest infections, ability to clear secretions, swallowing and ambulatory status in addition to measurement of lung function (pulmonary function tests (PFTs)).
As weakness and loss of function in a patient’s upper limbs develops and progresses, and a patient is no longer able to raise his or her hand to the mouth (Brooke score 3), respiratory impairment becomes more likely and closer respiratory monitoring should be initiated and possible interventions considered.16
Severe cardiomyopathy and/or significant scoliosis can impact respiratory function,13 14 20 dysphagia and poor oromotor function can result in aspiration,21 and therefore engagement with specialists to address these and other relevant comorbidities should always be considered.
Any drug that suppresses respiratory function (eg, opiates) should be carefully prescribed in DMD,22 especially in patients with respiratory impairment (forced vital capacity (FVC) <80%). Some ‘cough medications’ can temporarily reduce secretion clearance and should be used with caution, if at all.
All patients should receive scheduled vaccinations as per national guidelines (see box 1).
Box 1. Vaccination.
For scheduled vaccinations, refer to the Green Book:
https://www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book
-
Influenza jab:
Annual influenza jab is recommended from diagnosis.
Inactivated vaccine (subcutaneous) instead of live vaccine (nasal spray) must be used in patients on corticosteroids.
-
Pneumococcal polysaccharide conjugate vaccines (Prevenar13) should be given as per national guidance:
23 valent pneumococcal polysaccharide vaccine should be given prior to initiation of corticosteroid therapy and continued in line with national guidance.
National guidance: https://www.gov.uk/government/publications/pneumococcal-the-green-book-chapter-25
COVID-19 vaccinations should be given according to current recommendations for people with Duchenne muscular dystrophy and/or on long-term steroids (https://www.gov.uk/government/publications/covid-19-the-green-book-chapter-14a).
Live vaccine should be avoided in patients on corticosteroids.
Assessment and monitoring of respiratory function in DMD
A multidisciplinary team should be involved in the monitoring and delivery of respiratory care. The team should include respiratory physicians, physiotherapists and practitioners with experience in the management and assessment of patients with neuromuscular diseases or DMD.
Monitoring of respiratory function should start as soon as is feasible after diagnosis and would be expected to be done routinely by the age of 6 years.1 Testing should be performed by an adequately trained practitioner, familiar with assessing individuals with DMD and using an age-appropriate interface.23–25 Even before results of these assessments are reliable (in very young children), it is important to familiarise the patient with the test techniques in order to improve reliability once the test results do become clinically important.
Monitoring of respiratory function should occur every 6–12 months in ambulatory patients as part of routine clinical appointments, and every 6 months in non-ambulatory patients in view of their higher risk. More frequent assessments may be needed as dictated by clinical symptoms or in the face of specific comorbidities increasing risk of respiratory impairment.
As a minimum, assessment of respiratory function in DMD should include (see box 2)1 23 25 26:
Box 2. Forced vital capacity (FVC) and peak cough flow (PCF)26 .
FVC should be expressed in litres and as % of predicted value for age and height.
A pneumotachograph provides the most accurate measure of PCF. If unavailable, a paediatric peak expiratory flow metre is recommended.
PCF measurement should ideally be performed using an oronasal mask interface rather than a mouthpiece in a sitting position.
Accurate recording of a patient’s height is essential to provide valid percentage predicted values for FVC:
Standing height should be recorded for ambulant patients using a stadiometer.
For ambulant patients with ankle contractures beyond plantar grade, measure the standing height and deduct the measured distance from the floor to the base of the calcaneus.
Clinical judgement should be used to consider whether valid standing height can be recorded (in relation to significant compensations, asymmetries and/or contractures).
Consider ulnar length or arm span for those patients who have lost ambulation. A segmometer is required to perform valid ulnar length measure.
Efforts should be made to use the same measuring equipment and technique at each subsequent appointment.
medical history of respiratory symptoms, including recurrent chest infections;
FVC;
peak cough flow (PCF).
While comparative FVC measurements in lying and sitting can identify specific diaphragmatic weakness, it is often not practical to obtain these measurements in patients ith DMD with restricted mobility across all clinical settings.27–29 It is therefore recommended to record the position of the patient to allow better comparison and evaluation of serial measurements.
Moreover, all patients regardless of age or ambulatory status should be monitored for symptoms suggestive of sleep-disordered breathing (box 3).30 Patients who are overweight or have significant Cushingoid features are at higher risk even with apparently normal/stable pulmonary function tests and regardless of their ambulatory status.31
Box 3. Sleep-disordered breathing30 .
Sleep-disordered breathing in Duchenne muscular dystrophy can be due to respiratory muscle weakness leading to hypoventilation, or sleep apnoea.
Clinical suspicion of sleep-disordered breathing should prompt a referral to a specialist service with experience in sleep, management of patients with respiratory failure and delivery of home non-invasive ventilation.
Sleep apnoea is characterised by snoring/mouth breathing and breath holding. It may or may not be associated with nocturnal hypoventilation. However, due to sleep disruption, daytime symptoms can be very similar to those of hypoventilation.
Initial evaluation for sleep-disordered breathing should be determined by the specialist respiratory team and tailored to an individual patient. This will include clinical review and other investigations may include assessment of respiratory muscle strength (forced vital capacity; sniff nasal inspiratory pressure; maximal inspiratory pressure), home or in-hospital sleep studies (oximetry, respiratory polygraphy, combined oximetry/capnometry).
Symptoms that patients may report include excessive daytime tiredness/sleepiness (falling asleep or dozing off more frequently than normal or expected), disturbed sleep with frequent waking (possibly with symptoms of racing heart or breathlessness), witnessed episodes of stopping breathing for brief periods or shallow breathing; morning headaches (typically throbbing headache that settles by mid-day), poor appetite.
Children and young adults who are unable to report symptoms of sleep-disordered breathing due to communication difficulties and/or cognitive impairment may display changes to their daily routine and/or behaviour due to hypoventilation overnight. These indirect symptoms should be thoroughly explored with families and, if present, warrant further investigation.
Sleep studies are usually instigated by specialist respiratory teams. However, an overnight pulse oximetry can be useful to screen for sleep-disordered breathing32 and results should be discussed with the respiratory specialist team who will advise on further investigations and management.33–35
Monitoring of daytime SpO2 is often not informative in DMD—daytime saturations should not be relied on to diagnose or rule out ventilatory failure. For patients not on ventilatory support, it can be used to indicate whether a hypoxic challenge test is required prior to flying. All patients who are receiving ventilatory support will require a clinical assessment prior to flight which may include a hypoxic challenge test.2 36
Referral pathway and ongoing management
Patients with symptoms of sleep-disordered breathing, abnormal PFTs or recurrent chest infections require onward referral to a specialist respiratory service as summarised in box 4.
Box 4. Triggers for onward referral to specialist respiratory team with experience in Duchenne muscular dystrophy (DMD) management2 16 .
Symptoms of sleep-disordered breathing
Any symptom or suspicion of sleep-disordered breathing should prompt referral to a specialist respiratory team, regardless of forced vital capacity (FVC) values (see box 3).
Peak cough flow (PCF) values38 39
Absolute PCF values may be difficult to interpret. A PCF <270 L/min (in adults) or a decline in recorded value should prompt referral to a specialist respiratory team and consideration of airway clearance support (see box 5).
Decline in FVC16
FVC ≤50% of predicted value per age and height (box 2) indicates a higher risk of decompensation and potential need for ventilatory support*. This should trigger referral to a respiratory team, even in the absence of symptoms.
FVC <30% increases the risk of requiring ventilatory support and should trigger urgent referral to the respiratory team if specialised monitoring is not already in place.
Note that monitoring of daytime SpO2 is often not informative in DMD—daytime saturations should not be relied on to diagnose or rule out ventilatory failure.
*Once this FVC threshold is reached (FVC ≤50% of predicted value), subjects should remain under respiratory review and should not be discharged from respiratory clinics. Lack of symptoms does not preclude relevant respiratory compromise. Patients remain at risk of developing respiratory failure.
FVC ≤50% of predicted value corrected as per age and height (box 4) indicates weakness of respiratory muscles and is associated with a higher risk of sleep-disordered breathing/hypoventilation requiring ventilatory support. Patients might not report any symptoms at this stage, due to the slowly progressive nature of the respiratory involvement which means that patients can adapt and be unaware of the reduction in their respiratory function.2 Similarly, there are a number of patients with sleep-disordered breathing and higher FVC values. Therefore FVC ≤50% of predicted value should trigger referral to a respiratory team, even in the absence of symptoms37 and symptoms of sleep-disordered breathing should trigger a referral to specialist services even if FVC is >50%.
While a PCF <270 L/min for an adult indicates a compromised ability to clear secretions, normative data in children are missing and therefore it is more difficult to establish a reliable cut-off value to trigger referral.38 39 Moreover, the test requires compliance and the ability to follow instructions and so obtaining reliable values, especially in younger children, can be difficult. Therefore, clinicians should look at the absolute value and at any significant decline in PCF values when assessing the need for referral and consideration of airway clearance support.40 Guidance regarding management of secretions is provided in box 5.
Box 5. Cough augmentation40 49 .
Any concern about cough strength (as measured by peak cough flow), ability to manage chest secretions or frequent chest infections should lead to referral to a specialist respiratory service with a physiotherapist, for consideration of airway clearance support. These techniques can focus on inspiration, forced expiration or both.
For inspiration, consider:
Breath stacking
Lung volume recruitment (LVR)
For forced expiration, consider:
Manually assisted cough
For both inspiration and expiration, consider:
Mechanical insufflation-exsufflation devices (MI-E)
Breath stacking can be completed without the use of an LVR.
As patients progress, an LVR may be introduced
MI-E should be considered for patients with a significantly impaired cough.
MI-E settings should be individualised to each patient, set up by an expert in the area with a suitable interface and plan for review.
In the intensive care unit, MI-E maybe a useful technique to prevent re-intubation and to support extubation.
If dysphagia or gastro-oesophageal reflux is unmanaged, there may be risks caused by use of MI-E.
Recurrent lower respiratory chest infections (cough, increased amount of sputum, increased work of breathing), requiring antibiotic treatment, could indicate loss of respiratory muscle strength with decreased ventilation, ineffective cough or bulbar weakness resulting in aspiration. As a result of muscle weakness, this group may not be able to demonstrate the expected signs of severity, that is, weak cough, unable to increase work of breathing. Furthermore, patients with compromised respiratory function (FVC <80%) have a high risk of complications and rapid decompensation. A low threshold for antibiotic treatment should be considered. Those at high risk of respiratory decompensation should have an individual care plan to advise when antibiotics are indicated, type of antibiotic and length of course.
Children and adults who experience recurrent chest infections should have bulbar function assessed to exclude silent aspiration.21 Formal referral to speech and language therapist should be considered.
It is recognised that PFTs may be challenging in those with significant learning and behavioural issues.41–43 Therefore, the threshold for referral to respiratory specialists is likely to be lower in these patients and would be expected before transition to adult services. Difficulty performing reproducible PFTs does not preclude a young person from tolerating ventilatory support and other interventions. However, the risks and benefits of initiating treatment need to be considered on an individual basis and tolerating effective intervention is likely to require more time and support. Engagement with learning disability and palliative care teams is recommended.
Where formal spirometry cannot be reliably performed or in the presence of significant scoliosis, this should prompt onward referral.16 44
Decisions about initiation of ventilatory support are complex and depend on many factors, including patient wishes, and should be made by a specialist respiratory team after discussion with patient, carers and other relevant specialists including palliative care teams.
Emergency care considerations
Children and adults with DMD and compromised respiratory function can rapidly deteriorate during an intercurrent infection. Lack of awareness of DMD and its complications, including respiratory care requirements and considerations, can lead to inappropriate interventions.45
It is therefore important that an individualised emergency healthcare plan is in place and discussed with the patient and family and referred to in case of acute hospital admission. A DMD-specific ‘In case of emergency’ app46 is available for families to carry on their phones that includes key information about DMD, its complications and essential medical considerations for the management of a patients with DMD during acute medical events and hospital admissions.
Figure 2 provides emergency guidelines to support management during an unexpected medical event where there are respiratory considerations.
In the event of an unplanned/emergency admission to hospital, a child or adult with DMD may require stabilisation in a local emergency department. Due to the generalised weakness and reduced mobility, they may not display the laboured breathing and accessory muscle use seen typically in respiratory distress. Where there is a possibility of compromised respiratory function, management should be led by a specialist respiratory team. If the admitting centre does not have a specialist respiratory team, contact should be made with the nearest specialist respiratory centre as soon as possible for advice, guidance and possible transfer. Urgent assessment by a physiotherapist with experience in airway clearance is recommended.47
Whenever a patient with DMD is admitted acutely with a respiratory deterioration, the primary respiratory and neuromuscular teams looking after the patient in the long term should be contacted for advice as soon as is practicable.
Excessive oxygen administration in isolation should be avoided as it can worsen hypercapnia (see box 6).48–50 Low oxygen levels (saturations <95%) can indicate a need for ventilatory support and require urgent assessment, management and an increased frequency of observation. However, the use of oxygen in isolation without NIV is relatively contraindicated as even low flow oxygen administered to patients with diaphragmatic weakness can lead to worsening hypercapnia.51
Box 6. A patient with Duchenne muscular dystrophy (DMD) who is hypoxaemic (saturations <95%) requires urgent management:
Ensure CO2 levels are monitored.
There should be a low threshold for enhanced monitoring, critical care input and capillary/arterial blood gas analysis to rule out hypercapnia.
-
Consider non-invasive ventilation (NIV) if2
Hypoxaemia (saturations <95%).
Hypercapnia (>45 mm Hg/6 kPa).
Respiratory rate is above that recommended on local early warning score appropriate for age.
Patient is tiring.
Oxygen therapy is rarely required without additional ventilation, so oxygen therapy alone should not be provided without a check for hypercapnia. Supplementary oxygen should aim for target saturation range of 88%–92% in adults or above 92% for children. It should be recognised that patients with DMD with saturations above this range (but below 95%), while not requiring supplementary oxygen are unwell and at high risk of deterioration. A low threshold for critical care admission should be employed.2 47
High or increasing oxygen requirement should prompt urgent reassessment and consideration of NIV.51
Supplemental oxygen should be targeted to saturations and high flow oxygen should not be empirically administered.
Hypoxaemia should prompt an assessment of the adequacy of ventilation (eg, blood gases or transcutaneous CO2 measurement). If acute ventilatory support is required, this should be undertaken in a critical care or a respiratory support unit due to the risk of sudden deterioration and the requirement for increased frequency of observation. NIV is the initial treatment of choice in the setting of a chest infection and regular physiotherapy with use of mechanical insufflator-exsufflator (MI-E) is often required.
In the setting of single organ respiratory failure, the prospects of recovery are good and invasive ventilation should be considered as a treatment when non-invasive ventilation has been unsuccessful. If practicable, invasive ventilation should be discussed with the specialist respiratory team involved in the patient’s care. On recovery, extubation should be planned and undertaken in a specialist centre. NIV and MI-E use following extubation is strongly recommended.52–54
The use of tracheostomy in acute illness should be discussed with a respiratory team with experience in the management of DMD. Tracheostomy formation should only be undertaken following advice from a specialist centre.2 10 Note that early tracheostomy during weaning from mechanical ventilation in critical care has not been shown to improve mortality or length of critical care admission.52 55
During a critical care admission, especially if invasive ventilation is required, the goals and likely success of treatment should be regularly reassessed. If there is no improvement following intubation and other organ function deteriorates, this may indicate unsurvivable pathology. A change of focus from active, life-sustaining therapy to symptomatic treatment may need to be considered based on the deterioration in acute physiology and the background trajectory of disease and dependency. Patient wishes should be taken into account in addition to assessment of information from families and carers. Discussions about patient’s and carer’s wishes in the event of acute respiratory illness should take place when reduced respiratory reserve is first identified and not delayed until an acute crisis. Early engagement and close liaison with palliative care services is recommended to support parallel planning and the development of individual advanced care plans.
In view of the increased risk of dilated cardiomyopathy in DMD,13 56 57 cardiac function should always be reviewed in a patient with DMD developing acute respiratory symptoms (box 7).
Box 7. Cardiac involvement13 56 57 .
Uncorrected nocturnal hypoventilation can lead to adrenergic surges, hypertension, tachycardia and vasoconstriction, which can all contribute to increase heart work and aggravate cardiac dysfunction.
Correction of hypoventilation can improve heart function if it has deteriorated because of hypoxaemia/hypercapnia.
Respiratory inadequacy due to chronic hypoventilation, inspiration or acute infection can precipitate ventricular fibrillation in a patient with advanced cardiomyopathy.
Doses of medications to slow heart rate (eg, beta-blockers) in patients with respiratory failure should be increased if rate remains high after starting non-invasive ventilation.
Sleep-disordered breathing can aggravate cardiac dysfunction which can cause/worsen respiratory distress.
Most patients with DMD are on long-term treatment with corticosteroids (eg, prednisolone, deflazacort) and should be assumed to have adrenal suppression. All patients on corticosteroids should have an emergency steroid plan which includes stress dosing with oral steroid during mild-to-moderate illness.58 Hydrocortisone intramuscular or intravenous should always be considered at times of physiological stress such as illness, trauma or surgery or when adrenal crisis is suspected. The British Society of Paediatric Endocrinology and Diabetes national guidance for the management of adrenal insufficiency should be followed (https://www.bsped.org.uk/clinical-resources/bsped-adrenal-insufficiency-consensus-guidelines/).59
Fat embolism has been previously reported in DMD even after minor trauma and despite the absence of radiological evidence of a fracture. Symptoms of central nervous system involvement may be subtle or misinterpreted as agitation or panic.60–62 Fat embolism should always be considered as differential diagnosis in a patient with DMD who develops acute respiratory symptoms and rapid deterioration after trauma.
Discussion
The consensus guidelines reached through this work take international recommendations, incorporate additional clinical evidence and recent publications including adult consensus guidelines and reflect UK clinical experience and healthcare provision.
The guidelines highlight the importance of multiple factors, clinical experience and judgement, and patient/family circumstance in supporting optimal routine and emergency respiratory care for individual patients. The process of broad consultation across the UK network of NorthStar centres and their respiratory teams has already served to raise awareness among the clinical community and increase the ‘buy-in’ of colleagues as they have been part of the development of these guidelines. The parallel development of a patient-friendly user guide, accessible via support groups and neuromuscular clinics will serve to increase awareness among the patient community. Furthermore, this work makes a significant and important addition to the literature already published.
The international SoC promotes early initiation of ventilatory support when FVC drops below 50%. However, early intervention might not be tolerated by patients in the absence of clinical symptoms and could potentially affect their long-term compliance. Moreover, sleep-disordered breathing can also occur in patients with preserved respiratory function and therefore the FVC criteria alone could under-recognise patients requiring ventilatory support. This guidance provides clear, comprehensive criteria that should prompt referral to a specialised team with experience in the management of patients with DMD who can consider the whole picture and formulate an appropriate management plan with patients and carers.
The guidance emphasises the importance of specialist physiotherapy in the respiratory management of DMD and the anticipatory prescription of assisted cough devices. The DMD Care UK patient and clinician survey helped to highlight the variability in resources and access to equipment across various parts of the UK. It is hoped these guidelines will provide evidence to support benchmarking and service development in a more equitable manner.
The 2018 international guidance does not provide specific advice about the management of patients with DMD in the case of an acute medical event and/or unplanned hospital admission. The majority of patients requiring acute hospitalisation with DMD will have respiratory decompensation yet most clinical staff working in emergency departments will not be familiar with the disease, its treatment and complications. Therefore, these updated recommendations include a comprehensive and clear flow chart to guide the emergency respiratory management of a patient with DMD.
Conclusion
DMD remains a rare disease and therefore increased awareness of the condition and its implication is critical. It is hoped that more specific, practical guidance for the management and treatment of respiratory involvement in DMD will support the National Health Service in the UK to identify ways to optimise care and achieve the best clinical outcomes. By making these also accessible to emergency care providers and non-DMD specialists that are (or might be) involved in the care of those with DMD and by sharing with the patient community, these guidelines will enhance and support the highest standards of respiratory care in DMD for all those living with DMD in the UK.
Footnotes
Contributors: A-MC is the Chair of the respiratory working group who have authored this paper and has overall responsibility for its content and decision to publish. MG is co-chair and the clinical lead for the DMD Care UK project. RA, SB, LE, CE, JH, MJ, CM, BM, JMS, PBM, MS, AT and FT are the clinical members of the respiratory working group and have provided expert clinical input throughout the drafting and finalisation of this paper from the perspective of respiratory physiotherapy, neuromuscular and respiratory specialisms. JB has provided cardiac expert input to this manuscript as the chair of the cardiac working group in DMD Care UK. PF and VC have represented the patient community and given valuable insight into the patient and family experiences of respiratory care for DMD. CT has managed and coordinated the consensus building process as project manager and has worked on drafting and finalising of this manuscript.
Funding: This work has been supported by salary funding for CT from Duchenne UK, Duchenne Research Fund and Joining Jack (award number: NU-015572).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol 2018;17:347–61. 10.1016/S1474-4422(18)30025-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hull J, Aniapravan R, Chan E, et al. British thoracic society guideline for respiratory management of children with neuromuscular weakness. Thorax 2012;67 Suppl 1(Suppl 1):i1–40. 10.1136/thoraxjnl-2012-201964 [DOI] [PubMed] [Google Scholar]
- 3. Flanigan KM. Duchenne and becker muscular dystrophies. Neurol Clin 2014;32:671–88. 10.1016/j.ncl.2014.05.002 [DOI] [PubMed] [Google Scholar]
- 4. Aartsma-Rus A, Ginjaar IB, Bushby K. The importance of genetic diagnosis for Duchenne muscular dystrophy. J Med Genet 2016;53:145–51. 10.1136/jmedgenet-2015-103387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ishizaki M, Kobayashi M, Adachi K, et al. Female dystrophinopathy: review of current literature. Neuromuscul Disord 2018;28:572–81. 10.1016/j.nmd.2018.04.005 [DOI] [PubMed] [Google Scholar]
- 6. Veeger TTJ, van Zwet EW, Al Mohamad D, et al. Muscle architecture is associated with muscle fat replacement in Duchenne and becker muscular dystrophies. Muscle Nerve 2021;64:576–84. 10.1002/mus.27399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Crisafulli S, Sultana J, Fontana A, et al. Global epidemiology of Duchenne muscular dystrophy: an updated systematic review and meta-analysis. Orphanet J Rare Dis 2020;15:141. 10.1186/s13023-020-01430-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. NHS . Muscular dystrophy. 2023. Available: https://www.nhs.uk/conditions/muscular-dystrophy/
- 9. van Ruiten HJA, Straub V, Bushby K, et al. Improving recognition of Duchenne muscular dystrophy: a retrospective case NOTE review. Arch Dis Child 2014;99:1074–7. 10.1136/archdischild-2014-306366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sheehan DW, Birnkrant DJ, Benditt JO, et al. Respiratory management of the patient with Duchenne muscular dystrophy. Pediatrics 2018;142(Suppl 2):S62–71. 10.1542/peds.2018-0333H [DOI] [PubMed] [Google Scholar]
- 11. Trucco F, Ridout D, Domingos J, et al. Genotype-related respiratory progression in Duchenne muscular dystrophy-A multicenter international study. Muscle Nerve 2022;65:67–74. 10.1002/mus.27427 [DOI] [PubMed] [Google Scholar]
- 12. Van Ruiten HJA, Marini Bettolo C, Cheetham T, et al. Why are some patients with Duchenne muscular dystrophy dying young: an analysis of causes of death in North East England. Eur J Paediatr Neurol 2016;20:904–9. 10.1016/j.ejpn.2016.07.020 [DOI] [PubMed] [Google Scholar]
- 13. Nigro G, Comi LI, Politano L, et al. The incidence and evolution of cardiomyopathy in Duchenne muscular dystrophy. Int J Cardiol 1990;26:271–7. 10.1016/0167-5273(90)90082-g [DOI] [PubMed] [Google Scholar]
- 14. Bourke J, Turner C, Bradlow W, et al. Cardiac care of children with Dystrophinopathy and females carrying DMD-gene variations. Open Heart 2022;9:e001977. 10.1136/openhrt-2022-001977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Trucco F, Domingos JP, Tay CG, et al. Cardiorespiratory progression over 5 years and role of corticosteroids in Duchenne muscular dystrophy: a single-site retrospective longitudinal study. Chest 2020;158:1606–16. 10.1016/j.chest.2020.04.043 [DOI] [PubMed] [Google Scholar]
- 16. McDonald CM, Gordish-Dressman H, Henricson EK, et al. Longitudinal pulmonary function testing outcome measures in Duchenne muscular dystrophy: long-term natural history with and without glucocorticoids. Neuromuscul Disord 2018;28:897–909. 10.1016/j.nmd.2018.07.004 [DOI] [PubMed] [Google Scholar]
- 17. Broomfield J, Hill M, Guglieri M, et al. Life expectancy in Duchenne muscular dystrophy. Neurology 2021;97:e2304–14. 10.1212/WNL.0000000000012910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. DMD Care UK . 2023. Available: https://DmdcareukOrg/
- 19. NorthStar Network website. 2023. Available: https://WwwNorthstardmdCom/
- 20. Kurz LT, Mubarak SJ, Schultz P, et al. Correlation of Scoliosis and pulmonary function in Duchenne muscular dystrophy. J Pediatr Orthop 1983;3:347–53. 10.1097/01241398-198307000-00014 [DOI] [PubMed] [Google Scholar]
- 21. Toussaint M, Davidson Z, Bouvoie V, et al. Dysphagia in Duchenne muscular dystrophy: practical recommendations to guide management. Disabil Rehabil 2016;38:2052–62. 10.3109/09638288.2015.1111434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Marini Bettolo C, Guglieri M, van Ruiten H, et al. Cautionary tale in Duchenne muscular dystrophy – opioids in neuromuscular disorders. Neuromuscular Disorders 2015;25:S200. 10.1016/j.nmd.2015.06.060 [DOI] [Google Scholar]
- 23. Graham BL, Steenbruggen I, Miller MR, et al. Standardization of Spirometry 2019 update. an official American Thoracic society and European respiratory society technical statement. Am J Respir Crit Care Med 2019;200:e70–88. 10.1164/rccm.201908-1590ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for Spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J 2012;40:1324–43. 10.1183/09031936.00080312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sylvester KP, Clayton N, Cliff I, et al. ARTP statement on pulmonary function testing 2020. BMJ Open Respir Res 2020;7:e000575. 10.1136/bmjresp-2020-000575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chatwin M, Toussaint M, Gonçalves MR, et al. Airway clearance techniques in neuromuscular disorders: A state of the art review. Respir Med 2018;136:98–110. 10.1016/j.rmed.2018.01.012 [DOI] [PubMed] [Google Scholar]
- 27. Fromageot C, Lofaso F, Annane D, et al. Supine fall in lung volumes in the assessment of diaphragmatic weakness in neuromuscular disorders. Arch Phys Med Rehabil 2001;82:123–8. 10.1053/apmr.2001.18053 [DOI] [PubMed] [Google Scholar]
- 28. Lechtzin N, Wiener CM, Shade DM, et al. Spirometry in the supine position improves the detection of diaphragmatic weakness in patients with amyotrophic lateral sclerosis. Chest 2002;121:436–42. 10.1378/chest.121.2.436 [DOI] [PubMed] [Google Scholar]
- 29. Lo Mauro A, Aliverti A. Physiology of respiratory disturbances in muscular Dystrophies. Breathe (Sheff) 2016;12:318–27. 10.1183/20734735.012716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hoque R. Sleep-disordered breathing in Duchenne muscular dystrophy: an assessment of the literature. J Clin Sleep Med 2016;12:905–11. 10.5664/jcsm.5898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sawnani H, Thampratankul L, Szczesniak RD, et al. Sleep disordered breathing in young boys with Duchenne muscular dystrophy. J Pediatr 2015;166:640–5. 10.1016/j.jpeds.2014.12.006 [DOI] [PubMed] [Google Scholar]
- 32. Evans HJ, Gibson NA, Bennett J, et al. British Thoracic society guideline for diagnosing and monitoring Paediatric sleep-disordered breathing. Thorax 2023;78:1043–54. 10.1136/thorax-2022-219582 [DOI] [PubMed] [Google Scholar]
- 33. Bennet J, Chan S, Gavlak J, et al. BTS guideline for diagnosing and monitoring Paediatric sleep disordered breathing on behalf of the BTS Paediatric sleep disorders guideline development group; 2022.
- 34. McCallum M, Mayhew A, Moat D, et al. EP.52Overnight pulse oximetry for respiratory progression screening in a neuromuscular service. Neuromuscular Disorders 2019;29:S116. 10.1016/j.nmd.2019.06.284 Available: [DOI] [Google Scholar]
- 35. Pattipati M, Gudavalli G. Association between cushing’s syndrome and sleep apnea: results from the National inpatient sample. 2022. Available: 10.7759/cureus.22044 [DOI] [PMC free article] [PubMed]
- 36. Coker RK, Armstrong A, Church AC, et al. BTS clinical statement on air travel for passengers with respiratory disease. Thorax 2022;77:329–50. 10.1136/thoraxjnl-2021-218110 Available: 10.1136/thoraxjnl-2021-218110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hukins CA, Hillman DR. Daytime predictors of sleep hypoventilation in Duchenne muscular dystrophy. Am J Respir Crit Care Med 2000;161:166–70. 10.1164/ajrccm.161.1.9901057 Available: 10.1164/ajrccm.161.1.9901057 [DOI] [PubMed] [Google Scholar]
- 38. Kotwal N, Shukla PJ, Perez GF. Peak cough flow in children with neuromuscular disorders. Lung 2020;198:371–5. 10.1007/s00408-020-00340-7 Available: 10.1007/s00408-020-00340-7 [DOI] [PubMed] [Google Scholar]
- 39. Gauld LM, Boynton A. Relationship between peak cough flow and Spirometry in Duchenne muscular dystrophy. Pediatr Pulmonol 2005;39:457–60. 10.1002/ppul.20151 Available: 10.1002/ppul.20151 [DOI] [PubMed] [Google Scholar]
- 40. Camela F, Gallucci M, Ricci G. Cough and airway clearance in Duchenne muscular dystrophy. Paediatr Respir Rev 2019;31:35–9. 10.1016/j.prrv.2018.11.001 [DOI] [PubMed] [Google Scholar]
- 41. Gauld LM, Boynton A, Betts GA, et al. Spirometry is affected by intelligence and behavior in Duchenne muscular dystrophy. Pediatr Pulmonol 2005;40:408–13. 10.1002/ppul.20278 Available: 10.1002/ppul.20278 [DOI] [PubMed] [Google Scholar]
- 42. Cuvo AJ, Reagan AL, Ackerlund J, et al. Training children with autism spectrum disorders to be compliant with a physical exam. Research in Autism Spectrum Disorders 2010;4:168–85. 10.1016/j.rasd.2009.09.001 Available: [DOI] [Google Scholar]
- 43. Suglia SF, Wright RO, Schwartz J, et al. Association between lung function and cognition among children in a prospective birth cohort study. Psychosom Med 2008;70:356–62. 10.1097/PSY.0b013e3181656a5a Available: 10.1097/PSY.0b013e3181656a5a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. LoMauro A, Romei M, Gandossini S, et al. Evolution of respiratory function in Duchenne muscular dystrophy from childhood to adulthood. Eur Respir J 2018;51:1701418. 10.1183/13993003.01418-2017 Available: 10.1183/13993003.01418-2017 [DOI] [PubMed] [Google Scholar]
- 45. Bourke SC. Respiratory involvement in neuromuscular diseases. Clin Med 2014;14:72–5. 10.7861/clinmedicine.14-1-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. UK Duchenne . Available: https://www.duchenneuk.org/dmd-emergency-support n.d
- 47. Quinlivan R, Messer B, Murphy P, et al. Adult North star network (ANSN): consensus guideline for the standard of care of adults with Duchenne muscular dystrophy. J Neuromuscul Dis 2021;8:899–926. 10.3233/JND-200609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Gay PC, Edmonds LC. Severe hypercapnia after low-flow oxygen therapy in patients with neuromuscular disease and diaphragmatic dysfunction. Mayo Clin Proc 1995;70:327–30. 10.4065/70.4.327 [DOI] [PubMed] [Google Scholar]
- 49. Kravitz RM. Airway clearance in Duchenne muscular dystrophy. Pediatrics 2009;123 Suppl 4:S231–5.:2009. 10.1542/peds.2008-2952G [DOI] [PubMed] [Google Scholar]
- 50. Chiou M, Bach JR, Saporito LR, et al. Quantitation of oxygen-induced hypercapnia in respiratory pump failure. Rev Port Pneumol (2006) 2016;22:262–5. 10.1016/j.rppnen.2016.03.005 [DOI] [PubMed] [Google Scholar]
- 51. Comellini V, Pacilli AMG, Nava S. Benefits of non-invasive ventilation in acute Hypercapnic respiratory failure. Respirology 2019;24:308–17. 10.1111/resp.13469 Available: 10.1111/resp.13469 [DOI] [PubMed] [Google Scholar]
- 52. Bernardes Neto SCG, Torres-Castro R, Lima Í, et al. Weaning from mechanical ventilation in people with neuromuscular disease: A systematic review. BMJ Open 2021;11:e047449. 10.1136/bmjopen-2020-047449 Available: 10.1136/bmjopen-2020-047449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Davidson AC, Banham S, Elliott M, et al. BTS/ICS guideline for the ventilatory management of acute Hypercapnic respiratory failure in adults. Thorax 2016;71(Suppl 2):ii1–35. 10.1136/thoraxjnl-2015-208209 Available: 10.1136/thoraxjnl-2015-208209 [DOI] [PubMed] [Google Scholar]
- 54. Bach JR, Martinez D. Duchenne muscular dystrophy: continuous noninvasive ventilatory support prolongs survival. Respir Care 2011;56:744–50. 10.4187/respcare.00831 Available: 10.4187/respcare.00831 [DOI] [PubMed] [Google Scholar]
- 55. Young D, Harrison DA, Cuthbertson BH, et al. Tracman collaborators for the. effect of early vs late Tracheostomy placement on survival in patients receiving mechanical ventilation. JAMA 2013;309:2121–9. 10.1001/jama.2013.5154 Available: 10.1001/jama.2013.5154 [DOI] [PubMed] [Google Scholar]
- 56. Spurney C, Shimizu R, Morgenroth LP, et al. Cooperative International neuromuscular research group Duchenne natural history study demonstrates insufficient diagnosis and treatment of cardiomyopathy in Duchenne muscular dystrophy. Muscle Nerve 2014;50:250–6. 10.1002/mus.24163 Available: 10.1002/mus.24163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Fayssoil A, Abasse S, Silverston K. Cardiac involvement classification and therapeutic management in patients with Duchenne muscular dystrophy. J Neuromuscul Dis 2017;4:17–23. 10.3233/JND-160194 Available: 10.3233/JND-160194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Wong SC, et al. Available: https://dmdcareuk.org/clinical-recommendations [Accessed 29 Jun 2023].
- 59. British Society of Paediatric Endocrinology and Diabetes. 2023. Available: https://www.bsped.org.uk/clinical-resources/bsped-adrenal-insufficiency-consensus-guidelines/
- 60. McAdam LC, Rastogi A, Macleod K, et al. Fat embolism syndrome following minor trauma in Duchenne muscular dystrophy. Neuromuscul Disord 2012;22:1035–9. 10.1016/j.nmd.2012.07.010 [DOI] [PubMed] [Google Scholar]
- 61. Murphy LD, Yabrodi M, Lutfi R. Fat embolism syndrome in Duchenne muscular dystrophy patients: early recognition and aggressive therapy. Case Rep Crit Care 2018;2018:3686470. 10.1155/2018/3686470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Feder D, Koch ME, Palmieri B, et al. Fat embolism after fractures in Duchenne muscular dystrophy: an Underdiagnosed complication? A systematic review. Ther Clin Risk Manag 2017;13:1357–61. 10.2147/TCRM.S143317 [DOI] [PMC free article] [PubMed] [Google Scholar]