Abstract
Background and Objective:
Yogic breathing helps in reduction of stress and strain in the body. Right and left nostril breathings (RNB and LNB, respectively) have different effects on cardiorespiratory parameters. The study was performed to examine the effect of RNB exercise on cardiorespiratory parameters and reaction time in young, healthy human volunteers.
Materials and Methods:
In this prospective, interventional study, 110 young healthy volunteers underwent systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse rate (PR), respiratory rate (RR), vital capacity (VC), peak expiratory flow rate (PEFR), and reaction time (RT) examination before and after 2 weeks of performing 45 min of RNB exercise daily.
Results:
There was notable increment in SBP (113.39 ± 17.72 vs. 117.74 ± 10.83 mmHg, P = 0.002) and DBP (67.64 ± 10.32 vs. 71.27 ± 8.68 mmHg, P = 0.002). PR increased nonsignificantly (86.44 ± 12.65/min vs. 87.32 ± 13.43/min, P = 0.476). Significant decrease in RR (14.40 ± 2.48/min vs. 12.31 ± 2.23/min, P < 0.0001) was observed. VC (3.57 ± 0.57 vs. 3.82 ± 0.55 L/min, P < 0.0001) and PEFR (441.36 ± 50.22 vs. 468.91 ± 53.66 L/min, P < 0.0001) also increased significantly. Substantial reduction in auditory reaction time (ART) (165.58 ± 32.18 vs. 147.42 ± 23.39 ms, P < 0.0001) and visual reaction time (VRT) (191.04 ± 37.94 vs. 165.86 ± 28.74 ms, P < 0.0001) was seen. After engaging in cardiorespiratory exercise, the maximal heart rate (MHR) remained unchanged (P = 0.929).
Conclusion:
RNB results in increase in blood pressure, heart rate, VC, and PEFR and decrease in ART and VRT. Further studies in patients with cardiorespiratory diseases are necessary to understand its clinical utility.
Keywords: Cardiorespiratory functions, pranayama, reaction time, yogic breathing
INTRODUCTION
Yoga breathing, or pranayama, minimizes the negative effects of stress and pressure on the body, enhancing health.[1,2] Imbalance between sympathetic and parasympathetic functions can cause many disorders.[3] There has been increase in stress-related disorders all over world.[4] The modern human has been severely impacted by stress-related disorders and daily stress. Yogic techniques help a person to withstand stressful stimuli.[5] Yoga has been practiced for centuries in India to unite the mind, body, and spirit.[6]
Pranayama (control of breath) is one of the components of the Ashtanga yoga suggested by Indian philosopher Maharshi Patanjali.[7] In our modern materialistic society, practicing pranayama and asana is considered essential for maintaining good health and well-being. Many healthcare providers advise yoga for people with back pain, arthritis, depression, and other chronic disorders, as well as those who are at risk for heart disease.[8]
Improvement in cardiorespiratory functions occurs by practicing breathing and chest expansion exercise in pranayama.[9] Yoga provides a calming effect on the body by improving the heart, lungs, and brain functioning.[10,11] In the yogic system of breathing, sympathetic activation occurs by right nostril breathing (RNB), whose dominance is associated with opening yoga’s “Pingala” subtle energy channel, and in the yogic system of breathing, sympathetic activation occurs by right nostril breathing (RNB) and parasympathetic activation occurs by left nostril breathing (LNB) “Ida” svara.[12] Practicing yoga has numerous physical benefits in addition to spiritual growth. Pranayama has unique impacts on both respiratory processes and physiological and psychological aspects of the body.[13]
In our bodies, both nostrils do not work simultaneously. Even when the nasal passages are clear and unblocked by mucus, one nostril is always more clogged than the other. Throughout the day and night, this congestion shifts between the right and left nostrils.[12] The practice of yoga can increase melatonin secretion and serve as a stimulation for the mind and body, leading to feelings of well-being and a relaxing influence on the mind, which can aid in reducing stress.[14]
Sympathomimetic effects may result in an increase in metabolism, resting oxygen consumption, systolic blood pressure (SBP), and heart rate (HR). RNB, referred to as or surya anuloma viloma pranayama, is associated with stimulation of sympathetic effects.[15] By improving respiratory functioning, pranayama may be beneficial for treatment of respiratory conditions such as bronchial asthma and chronic obstructive pulmonary disease (COPD).[16]
The reaction time (RT) is the duration between the onset of a movement response and the arrival of a signal. It determines sensory–motor connections, attainment, and cortical arousal. RT is an indirect index of central neuronal processing. Reduction in RT after practicing pranayama has been reported,[17,18] indicating that it could be a quick and accurate measure of processing by central neurons. Limited evidence is available focusing on the effects of RNB on the characteristics of heart and lungs in wholesome people.
The present study was, therefore, undertaken to look into the impact of RNB on the characteristics of heart and lungs in young and healthy human volunteers.
MATERIALS AND METHODS
One hundred and ten healthy adults from a medical college were involved in this interventional study. After their informed consent was taken, demographic parameters including age, height, and weight were recorded. Participants with history of any severe or persistent medical disorders, smokers, and alcoholics were excluded. Similarly, participants who used any kind of medicine or regularly engaged in breathing exercises were also excluded.
After enrollment, volunteers were requested not to engage in any further physical activity or yoga asanas beyond what was required for the research.
RNB or surya anuloma viloma was performed in a calm and quiet room with a relaxed and steady stance, with the head, neck, and trunk being aligned and the eyes shut with the finger position in chin mudra. Inhalation and exhalation were done gradually and fully only through the right nostril. The left nostril was closed with the left thumb.[19] RNB was done (6 cycles/min) for a duration of 2 weeks, spending 45 min every day under guidance of a yoga expert, who was trained on the study protocol. Vital capacity (VC) was measured using windmill-type spirometer, whereas peak expiratory flow rate (PEFR) was obtained by a mini-Wright peak flow meter. SBP, diastolic blood pressure (DBP), and pulse rate (PR) were measured at the same time of the day. Auditory reaction time (ART), visual reaction time (VRT), and cardiorespiratory activity (CRA) were measured at the base level and 2 weeks later at the same time of the day. For the evaluation of results on CRA, we used a stationary recliner bicycle. Recliner seats of the bicycle were modified to match the participant’s height to achieve 90° knee flexion during pedaling. Participants were asked to do warmup for 5 min at a modest intensity before cycling for 10 min at a low to moderate intensity. Blood pressure (BP) and PR were recorded using Omron HEM 6181 (Omron Healthcare Manufacturing Vietnam Co. Ltd) fully automatic wrist monitor. Target heart rate (THR) for the study participants was calculated using the American College of Sports Medicine (ACSM)’s guideline[20] and Karvoneon formula: THR (bpm) = % intensity × [(220− age)− resting heart rate (RHR) + RHR].[21,22] ART and VRT were evaluated on RT machine.[23] The study procedure is summarized in Figure 1.
Figure 1.
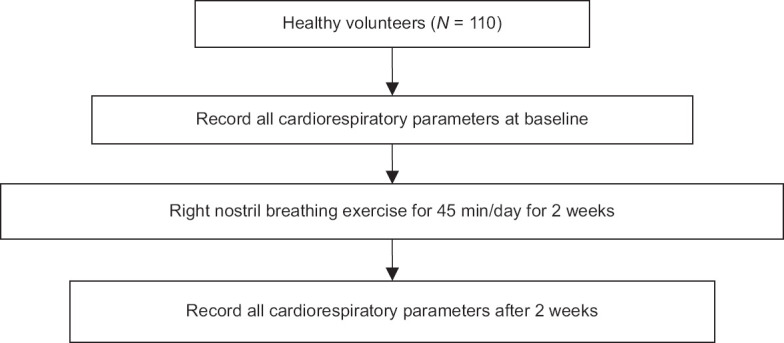
Study flow diagram
The research protocol was approved by the Institutional Ethics Committee for Biomedical and Health Research of Dr DY Patil Medical College and Hospital, Navi Mumbai (No.: IEC Ref. No. DYP/IECBH/2019/13). The study was conducted from January to April 2021.
Numbers and percentages are used for categorical data, while mean and standard deviation (SD) are used for continuous data. To examine the significance between the means of two groups, the paired “t”- test was used. Statistics were considered significant if the P-value was 0.05 or lower.
Sample size
Based on the major study outcome, which was the change in SBP following 2 weeks of breathing exercises, the sample size was determined. Considering the statistics provided by increase in SBP with RNB, a power of 80.52% was attained with 110 participants in each group.[23] This sample was adequate to a difference of -2.8 between two groups with a significance level (alpha) of 0.050 (95% confidence levels) using a two-sided t-test, assuming that the actual distribution is uniform. Samples were selected based on the sequential (nonprobability) sampling technique.
RESULTS
In this study, overall, 110 healthy volunteers with a mean (SD) age of 19.20 (1.80) years were included [Table 1]. The study included 55 (50%) male and female participants each. Mean height of the study participants was 157.89 cm. Mean weight and body mass index of the study participants was 59.14 kg and 22.47 kg/m2, respectively [Table 1].
Table 1.
Baseline parameters of study participants
| Parameters | Mean±SD |
|---|---|
| Age in years (mean±SD) | 19.20±1.80 |
| Male, n (%) | 55 (50%) |
| Female, n (%) | 55 (50%) |
| Height in centimeters (mean±SD) | 157.89±25.07 |
| Weight in kg (mean±SD) | 59.14±19.49 |
| Body mass index (kg/m2) (mean±SD) | 22.47±6.36 |
SD=standard deviation
Mean SBP increased from 113.39 to 117.74 mmHg. This change was statistically significant. Similarly, the rise in DBP was also statistically significant (67.64 vs. 71.27 mmHg, P = 0.002). Increase in PR was not statistically significant (86.44 vs. 87.32, P = 0.476).
Mean respiratory rate (RR) change decreased from 14.40 to 12.31 per minute. The change in mean RR showed statistical significance (P = 0.0001).
Mean VC increased from 3.57 to 3.82 L. The change in mean VC was also statistically significant (P = 0.0001). Similarly, mean PEFR increased significantly after 2 weeks of RNB exercise (441.36 vs. 468.91 L, P = 0.0001).
Mean ART (165.58 vs. 147.42 ms, P = 0.0001) as well as mean VRT (191.04 vs. 165.86 ms, P = 0.0001) decreased significantly compared to baseline.
Maximal heart rate (MHR) did not significantly change following 2 weeks of RNB exercise (148.13 vs. 148.23, P = 0.929) [Table 2].
Table 2.
Effect of RNB exercise on cardiorespiratory parameters, auditory reaction time, and visual reaction time in healthy, young individuals
| Parameter | Before Mean (SD) | After Mean (SD) | P |
|---|---|---|---|
| SBP (mmHg) | 113.39±17.72 | 117.74±10.83 | 0.002 |
| DBP (mmHg) | 67.64±10.32 | 71.27±8.68 | 0.002 |
| Pulse rate (/min) | 86.44±12.65 | 87.32±13.43 | 0.476 |
| Respiratory rate (/min) | 14.40±2.48 | 12.31±2.23 | 0.0001 |
| VC (L) | 3.57±0.57 | 3.82±0.55 | 0.0001 |
| PEFR (L) | 441.36±50.22 | 468.91±53.66 | 0.0001 |
| ART (ms) | 165.58±32.18 | 147.42±23.39 | 0.0001 |
| VRT (ms) | 191.04±37.94 | 165.86±28.74 | 0.0001 |
| MHR | 148.13±5.81 | 148.23±10.12 | 0.929 |
ART=auditory reaction time, DBP=diastolic blood pressure, MHR=maximum heart rate, PEFR=peak expiratory flow rate, PR=pulse rate, RNB=right nostril breathing, RR=respiratory rate, SBP=systolic blood pressure, SD=standard deviation, VC=vital capacity, VRT=visual reaction time
DISCUSSION
In this study, we observed substantial improvement in PEFR, VC, SBP, and DBP after 2 weeks of RNB. PR showed no significant increase compared to baseline. RR, ART, and VRT showed significant decrease; however, MHR did not alter significantly. The activation of the sympathetic nervous system may be responsible for changes in cardiorespiratory parameters following exposure to RNB. RNB has sympathetic effects and is also referred to as suryanadi pranayama or surya anuloma viloma pranayama.[15] Increment in SBP and DBP was consistent with the reports of Shannahoff-Khalsa and Kennedy,[24] Telles et al.,[25] and Dane et al.[26] These studies have demonstrated increment in SBP and HR along with substantial PR reduction. In contrast, some studies with RNB reported SBP or DBP did not change significantly in healthy male volunteers.[27] Another study reported substantial change in HR and notable decline in SBP and DBP in healthy male subjects, with no significant difference in healthy female participants.[28] In our study, HR was increased by RNB, which is in accordance with another study by Dane et al.,[26] in which participants exercised before examining the effect of nostril breathing on HR. They observed a rise in HR with both RNB and LNB, which was most likely brought on by the exercise’s overall impact on HR.
The autonomic nervous system can be brought into balance with the use of pranayama. By correcting incorrect breathing patterns and lowering respiratory muscle tone, pranayama may enable dilatation of the airways due to relaxing of the surrounding respiratory smooth muscles.[29,30] Breathing through both nostrils is said to have different effects on the human system as the right nostril corresponds to “pingala nadi,” which is a subtle energy channel and left to “ida. In yoga, special significance has been given for uninostril and alternate nostril breathing (ANB).[29,31,32]
Decrease in RR and increase in VC and PEFR observed in our study were in line with the findings of Yadav et al.,[33] Upadhyay et al.,[34] and Chanavirut et al.[30] Maximal expansion and compaction of lungs by consistently inhaling and exhaling for an extended period of time in yoga training may lead to increased endurance as well as improved strength of respiratory muscles.[35,36] In the course of pranayama, deep inspiration can stimulate the respiratory system to fill it with fresh air. Retention of air helps to increase oxygen absorption and internal temperature, whereas diaphragm returns to the original position by slow exhalation. Intercostal muscles contract and remove impure air filled with the toxins and impurities.[37,38] The primary function of pranayama is to exercise the abdominal muscles and strengthen the respiratory system.[37] Deep inhalation, air retention, and slow expiration all raise the lungs’ overall capacity, eventually enhancing the function of the lungs.[37]
In many respiratory diseases, PEFR and forced expiratory flow (FEF) 25%–75% are among the primary factors showing decrease. The development of COPD is expected to retard by any practice which increases PEFR and FEF 25%–75%.[39] Our result shows the positive impact of RNB exercise on PEFR. This result is consistent with the finding of Jain et al.[29] Eight years of age is considered as the ideal age to introduce pranayama because up to this age, the number of alveoli increases and afterward, the alveoli increase only in size.[38] Our findings, which show a rise in PEFR and VC, are in line with those of Sivapriya et al.[38]
There was no notable difference in MHR following RNB exercise. We feel 2 weeks of RNB exercise may not be enough to cause a change in CRA or increase Heart rate reserve (HRR).
In our body, RT for auditory and visual stimuli shortened remarkably following RNB exercise. According to our results, ART is faster than VRT, which is in accordance with the studies existing in the literature.[40] Another study reported a decrease in RT after doing both slow and quick pranayamas for 3 weeks.[18]
This is a single-center study among healthy adults, which is a limitation of our research. Further studies on patients with compromised cardiorespiratory function are necessary to understand the clinical significance of RNB. It would also be interesting to see if RNB is useful in improving physiological bradycardia. The function of sympathetic and parasympathetic systems can be better understood through additional testing, such as measuring galvanic skin resistance.
CONCLUSION
RNB technique has differential physiological effects. RNB leads to faster ART and VRT. ART is faster than VRT in healthy volunteers. Thus, we feel regular exercising should be promoted in students to improve their efficiency levels.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Singh S, Malhotra V, Singh KP, Madhu SV, Tandon OP. Role of yoga in modifying certain cardiovascular functions in type 2 diabetic patients. J Assoc Physicians India. 2004;52:203–6. [PubMed] [Google Scholar]
- 2.Brown RP, Gerbarg PL. Sudarshan kriya yogic breathing in the treatment of stress, anxiety and depression: Part 2- clinical applications and guidelines. J Altern Complement Med. 2005;11:711–7. doi: 10.1089/acm.2005.11.711. [DOI] [PubMed] [Google Scholar]
- 3.Thayer JF, Yamamoto SS, Brosschot JF. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factor. Int J cardiol. 2010;141:122–31. doi: 10.1016/j.ijcard.2009.09.543. [DOI] [PubMed] [Google Scholar]
- 4.Murray CJ, Lopez AD, Jamison DT. The global burden of disease in 1990: Summary results, sensitivity analysis and future directions. Bull World Health Organ. 1994;72:495–509. [PMC free article] [PubMed] [Google Scholar]
- 5.Nayak NN, Kamala S. Yoga: A therapeutic approach. Phys Med Rehabil Clin N Am. 2004;15:783–98. doi: 10.1016/j.pmr.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Bijlani RL. In: Yoga in Health and Disease Understanding Medical Physiology. 3rd ed. Bijlani RL, Manjunatha S, editors. Jaypee Publications; India: 2004. pp. 869–904. [Google Scholar]
- 7.Bryant EF. North Point Press; New York: 2015. The Yoga Sutras of Patanjali: A New Edition, Translation, and Commentary; p. 953. [Google Scholar]
- 8.Richmond B. The benefits of yoga. J Yoga. 2003;2:1. [Google Scholar]
- 9.Singh S, Gaurav V, Parkash V. Effects of a 6-week Nadi Shodhan Pranayama training on cardiopulmonary parameters. J Phys Educ Sports Manag. 2011;2:44–7. [Google Scholar]
- 10.Subbalakshmi NK, Saxena SK, Urmimala, D’ Souza UJA. Immediate effect of Nadishodhana Pranayama on selected parameters of cardiovascular, pulmonary, and higher functions of brain. Thai J Physiol Sci. 2005;18:10–6. [Google Scholar]
- 11.Shankarappa V, Prasanth P, Nachal Annamalai N, Malhotra V. The short term effect of pranayama on the lung parameters. JCDR. 2012;6:27–30. [Google Scholar]
- 12.Rama S. Pranayama: The Royal Path: Practical lessons on Yoga. Pennsylvania: The Himalayan Institute press Honesdale; 1979. pp. 55–70. [Google Scholar]
- 13.Parikh HN, Patel HM, Pathak NR, Chandwani S. Effect of yoga practices on respiratory parameters in healthy young adults. NJIRM. 2014;5:37–41. [Google Scholar]
- 14.Pal G K, Velkumary S, Madanmohan Effect of short-term breath exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120:115–21. [PubMed] [Google Scholar]
- 15.Telles S, Nagaratha R, Nagendra HR. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiology Parmacol. 1994;38:133–7. [PubMed] [Google Scholar]
- 16.Keerthi S, Bandi HK, Suresh M, Reddy MN. Immediate effect of suryanadi pranayama on pulmonary function (ventilator volumes and capacities) in healthy volunteers. Int J Med Res Helath Sci. 2013;2:724–9. [Google Scholar]
- 17.Madanmohan M, Thombre DP, Balakumar B, Nambinarayan TK, Thakur S, Krishnamurthy N. Effect of yoga training on reaction time, respiratory endurance and muscle strength. Indian J Physiol Pharmacol. 1992;36:229–33. [PubMed] [Google Scholar]
- 18.Madanmohan, Udupa K, Bhavanani AB, Vijayalakshmi P, Surendiran A. Effect of slow and fast Pranayamas on reaction time and cardiorespiratory variables. Indian J Physiol Pharmacol. 2005;49:313–8. [PubMed] [Google Scholar]
- 19.Garg R, Malhotra V, Tripathi Y, Agarawal R. Effect of left, right and alternate nostril breathing on verbal and Spatial memory. J Clin Diagn Res. 2016;10:CC01–3. doi: 10.7860/JCDR/2016/12361.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carol EG, Barry F, Bryan B, David CN, Michael RD, Michael JL, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adult: Guidance for prescribing exercise. Med Sci Sports Exer. 2011;43:1334–59. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 21.Maya I, Benny L, Shannon W, Saul I. The science of exercise prescription: Martti Karvonen and his contributions. B C Med J (BCMJ) 2017;59:38–41. [Google Scholar]
- 22.Daniel S, Bryndan L, Joel RM. Accuracy of commonly used age- predicted maximal heart rate equations. Int J Exerc Sci. 2020;13:1242–50. doi: 10.70252/XFSJ6815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhavanani AB, Ramanathan M, Balaji R, Pushpa D. Differential effects of uninostril and alternate nostril pranayamas on cardiovascular parameters and reaction time. Int J Yoga. 2014;7:60–5. doi: 10.4103/0973-6131.123489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shannahoff-Khalsa DS, Kennedy B. The effects of unilateral forced nostril breathing on the heart. Int J Neurosci. 1993;73:47–60. doi: 10.3109/00207459308987210. [DOI] [PubMed] [Google Scholar]
- 25.Telles S, Nagarathna R, Nagendra HR. Physiological measures of right nostril breathing. J Altern Complement Med. 1996;2:479–84. doi: 10.1089/acm.1996.2.479. [DOI] [PubMed] [Google Scholar]
- 26.Dane S, Caliskan E, Karasen M, Oztasan N. Effect of unilateral nostril breathing on blood pressure and heart rate in right- handed healthy subjects. Int J Neurosci. 2002;112:97–102. doi: 10.1080/00207450212019. [DOI] [PubMed] [Google Scholar]
- 27.Raghuraj P, Telles S. Immediate effect of specific nostril manipulating yoga breathing practices on autonomic and respiratory variables. Appl Psychophysiol Biofeedback. 2008;33:65–75. doi: 10.1007/s10484-008-9055-0. [DOI] [PubMed] [Google Scholar]
- 28.Jain N, Srivastava RD, Singhal A. The effects of right and left nostril breathing on cardiorespiratory and autonomic parameters. Indian J Physiol Pharmacol. 2005;49:469–74. [PubMed] [Google Scholar]
- 29.Jain N, Srivastav RD, Singhal A. The effect of right and left nostril breathing on cardiorespiratory and autonomic parameters. Indian J Physiol Pharmacol. 2005;49:469–74. [PubMed] [Google Scholar]
- 30.Chanavirut R, Khaidjapho K, Jaree P, Pongnaratorn P. Yoga exercise increases chest wall expansion and lung volumes. Thai J Physiol Sci. 2006;19:1–7. [Google Scholar]
- 31.Muktibodhananda S. Hatha Yoga Pradipika. Munger: Yoga Publication Trust; 2002. p. 654. [Google Scholar]
- 32.Saoji AA, Rghuvendra BR, Manjunath NK. Effect of yogic breath regulation: A narrative review of scientific evidence. J Ayurveda Integr Med. 2019;10:50–8. doi: 10.1016/j.jaim.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yadav A, Savita S, Singh KP. Role of the pranayama breathing exercise in the rehabilitation of coronary artery disease patients. Indian J Trad Knowledge. 2009;3:455–508. [Google Scholar]
- 34.Upadhyay DK, Malhotra V, Sarkar D, Prajapati R. Effect of alternate nostril breathing exercise on cardiorespiratory functions. Nepal Med Coll J. 2008;10:25–7. [PubMed] [Google Scholar]
- 35.Madanmohan, Lakshmi J, Udupa K, Bhavanani AB. Effect of yoga training on handgrip, respiratory pressures and pulmonary function. Indian J Physiol Pharmacol. 2003;47:387–92. [PubMed] [Google Scholar]
- 36.Raghuraj P, Telles S. Muscle power, dexterity skill and visual perception in community home girls who trained in yoga or sports and in regular school girls. Indian J Physiol Pharmacol. 1997;41:409–15. [PubMed] [Google Scholar]
- 37.Manaspure SP, Fadia A, Damodara Gowda KM. Effect of selected breathing technique on respiratory rate and breath holding time in healthy adults. IJABPT. 2011;2:225–9. [Google Scholar]
- 38.Sivapriya DV, Suba Malani S, Thirumeni S. Effect of Nadishodhana pranayama on respiratory parameters in school students. Rec Res Sci Tech. 2010;2:32–9. [Google Scholar]
- 39.Dullo P, Vedi N, Gupta U. Improvement in respiratory functions after alternate nostril breathing in healthy young adults. Pak J Physiol. 2008;4:15–6. [Google Scholar]
- 40.Pain MT, Hibbs A. Spirit starts and the minimum auditory reaction time. J Sports Sci. 2007;25:79–86. doi: 10.1080/02640410600718004. [DOI] [PubMed] [Google Scholar]


