Abstract
INTRODUCTION:
Inflammatory bowel disease (IBD) is associated with depression and anxiety in adults, but data are scarce on risk of psychiatric diseases in children with IBD. We aimed to estimate the risk of anxiety, depression, or attention-deficit/hyperactivity disorder (ADHD) in patients with pediatric-onset IBD.
METHODS:
We performed a nationwide, register-based cohort study including all patients with pediatric-onset IBD diagnosed in Denmark during 1998–2018, resulting in 3,559 patients matched 1:5 on age, sex, municipality of residence, and time period, resulting in 17,795 reference individuals. We used Cox regression to calculate hazard ratios for each outcome after a diagnosis with IBD.
RESULTS:
Patients with pediatric-onset IBD had an increased risk of depression (hazard ratio [HR] 1.50; 95% confidence interval [CI] 1.26–1.80) and of using antidepressants (HR, 1.54; 95% CI, 1.39–1.71) and, surprisingly, a reduced risk of using methylphenidate (HR, 0.75; 95% CI, 0.58–0.98). Patients with both IBD subtypes (Crohn's disease and ulcerative colitis) had an increased risk of using antidepressants and developing depression, which was particularly high in patients with Crohn's disease (HR, 1.73; 95% CI, 1.35–2.22). Patients with ulcerative colitis had reduced risk of using methylphenidate (HR, 0.63; 95% CI, 0.43–0.93) and a reduced—although not statistically significant—risk of being diagnosed with ADHD compared with the background population.
DISCUSSION:
Patients with pediatric-onset IBD have a 50% increased risk of developing depression, which is important for healthcare providers to be aware of and manage. Remarkably, we found a reduced risk of receiving methylphenidate and being diagnosed with ADHD, which merits further investigation.
KEYWORDS: inflammatory bowel disease, gut-brain axis, depression, anxiety, ADHD
INTRODUCTION
Inflammatory bowel disease (IBD) consists of 2 main subtypes: Crohn's disease (CD) and ulcerative colitis (UC). The disease is characterized by chronic inflammation of the gastrointestinal tract, and the symptoms vary depending on the subtype but typically present as abdominal pain, diarrhea, and rectal bleeding. Both CD and UC are not curable and carry high morbidity as well as risk of colorectal cancer and extraintestinal manifestations in many organ systems. IBD affects patients' work and school life (1,2) and social interactions and, hence, has a major impact on quality of life (3). The incidence of IBD peaks between the ages of 20 and 40 years (4), but around 25% of patients with IBD are younger than 20 years at the time of diagnosis (5).
A range of studies have suggested a link between neuropsychiatric disorders and IBD, particularly with strong evidence of an increased risk of depression and anxiety in patients with IBD (6–8). However, evidence in patients with pediatric-onset IBD is scarce. A systematic review with meta-analysis of 28 studies found that 16.4% of children with IBD present symptoms of anxiety and 15% experience symptoms of depression (9), although the authors noted a large heterogeneity because included studies varied widely in design and outcome definitions. Another recent systematic review with meta-analysis found just 3 studies based on unselected population-based cohorts estimating risk of depression or anxiety in pediatric patients with IBD compared with the general population (10). The studies found increased risk of depression after an IBD diagnosis (pooled hazard ratio [HR] 1.57, 95% confidence interval [CI] 1.39–1.78) but conflicting results on risk of anxiety (pooled HR, 1.47; 95% CI, 0.66–3.27). Other neuropsychiatric diseases have received little attention in the context of IBD, but 1 study has suggested an increased risk of attention-deficit/hyperactivity disorder (ADHD) in pediatric patients with IBD (HR, 1.20; 95% CI, 1.10–1.40) (11). To our knowledge, this finding has not yet been replicated in other populations.
The mechanisms underlying the co-occurrence of IBD and psychiatric diseases are not yet fully understood. The connection could partly be explained by an interplay of the gut microbiota and gut-brain axis, which is a network of bidirectional communication between the enteric and central nervous systems, the endocrine system, and immunological pathways (12). The vagus nerve is an important communication pathway for the gut microbiota to influence the brain because it can be activated by the gut microbiota (13). The gut-brain axis is well known to influence psychiatric diseases, such as anxiety and depression (14), and studies have suggested that the gut microbiota in combination with diet highly influences the development and symptoms of ADHD (15).
Although it is established that IBD is strongly associated with psychiatric comorbidities in adult populations, we lack knowledge of the extent to which these comorbidities occur in children with IBD. We aimed to estimate the risk of developing new anxiety or depression or being diagnosed with ADHD in patients diagnosed with IBD in childhood and adolescence in a population-based nationwide pediatric patient cohort.
MATERIAL AND METHODS
Study population
Through the Danish Civil Registration System, we identified a source population of individuals 0–17 years with an address in Denmark during 1998–2018. The register contains vital data on all persons born in or immigrated to Denmark and can be linked to the other nationwide registers through the unique 10-digit personal identification number given to all citizens at birth (16).
Case definition and matching
We identified IBD cases through the Danish National Patient Register (DNPR), which has recorded somatic inpatient contacts since 1977 and both somatic and psychiatric inpatient and outpatient contacts and emergency department contacts since 1995 (17). IBD cases were included if they had at least 2 IBD hospital contacts (ICD-8 codes: CD: 563.01, 563.02, 563.08, 563.09 UC: 563.19, 569.04, ICD-10 codes: CD: K50, UC: K51) in the DNPR within a 2-year period in the study period and before the age of 18 years. The 2 IBD contacts had to be the first contacts for IBD and could be 2 inpatient contacts, 2 outpatient visits, or 2 contacts as a mix of inpatient contacts or outpatient visit. This case definition was chosen to increase the likelihood of only including patients with a true IBD diagnosis. The case definition has a positive predictive value for IBD of 95% (18). Only patients with IBD with no history of anxiety, depression, or ADHD or use of antidepressants or methylphenidate in the 5 years before the date of the second IBD contact were included. Patients with IBD were required to have an address in a municipality in Denmark, which had to be maintained for at least 1 year before and within the period between the 2 IBD contacts. IBD subtype (CD or UC) was determined based on the ICD codes associated with the 2 IBD contacts. If both CD and UC were documented, the IBD subtype was classified as CD. For each 6-month interval within the study period, all newly diagnosed IBD cases were matched 1:5 on age, sex, and municipality of residence to individuals from the general population who did not have IBD using frequency matching. We used the second of the 2 IBD contacts as the matching time and the last day of the 6-month interval as the matching date for the general population. Only individuals who had never had a contact for IBD; who had been in Denmark for 1 year before the 6-month interval; and who had not had hospital contact anxiety, depression, or ADHD or a prescription for antidepressants or methylphenidate before the matching date were eligible as matches. An index date was assigned to each reference individual from the general population, which corresponded to the first of the 2 IBD contacts for the corresponding IBD case.
Outcomes
Based on the knowledge from previous studies, primarily in adult patients with IBD, we chose to investigate the risk of developing depression or anxiety and the risk of being diagnosed with ADHD. In Denmark, ADHD is diagnosed only by child psychiatrists in childhood and by psychiatrists in adulthood. Most patients are diagnosed in out-hospital clinics, but because of wait times, some are diagnosed by privately practicing psychiatrists/child psychiatrists. The wait times vary but can delay diagnoses for up to a year. Depression and anxiety can be diagnosed and treated both by psychiatrists in hospitals and also by privately practicing psychiatrists or by general practitioners (mild-moderate cases). Only contacts to hospitals—not to privately practicing psychiatrists or general practitioners—will be recorded in the Danish registers. Therefore, we chose to also investigate the risk of receiving antidepressants or methylphenidate, which are the most commonly used therapeutics for depression/anxiety and ADHD, respectively. We did not break down the analyses by type of antidepressant or formulation of methylphenidate because we considered the medication outcomes proxy measures for disease. Prescriptions for medication are registered regardless of the workplace of the prescriber.
Data on hospital contact outcomes (A- or B-diagnosis, inpatient/outpatient/emergency department) were drawn from DNPR, and data on medication use were drawn from the Danish National Prescription Register, which has recorded all dispensed prescriptions from Danish retail pharmacies since 1994 (19). An outcome was defined as at least 1 contact in the main DNPR for anxiety (ICD-10 code F41), depression (ICD-10 codes F32 and F33), or ADHD (ICD-10 code F90) or at least 1 dispensed prescription for antidepressants (ATC code N06A, except for N06AX12) or methylphenidate (ATC code N06BA04).
Statistical analysis
We created Kaplan-Meier curves for each outcome for the IBD cases and matched references, and we used Cox regression to analyze the risk of each outcome after IBD diagnosis/index date and to estimate a HR with a 95% CI. The analyses were adjusted for age at diagnosis, sex, and year of diagnosis. Time to first diagnosis or first prescription started at the date of first IBD diagnosis or index date for reference individuals. We stratified the analyses by IBD subtype, age at IBD diagnosis, and sex. The statistical analyses were performed using SAS 9.4 TS Level 1M7.
Patient and public involvement statement
There was no patient or public involvement in this study.
Register-based studies in Denmark do not require ethical approval or informed consent. The Danish Protection Agency has approved this study.
RESULTS
Cohort characteristics
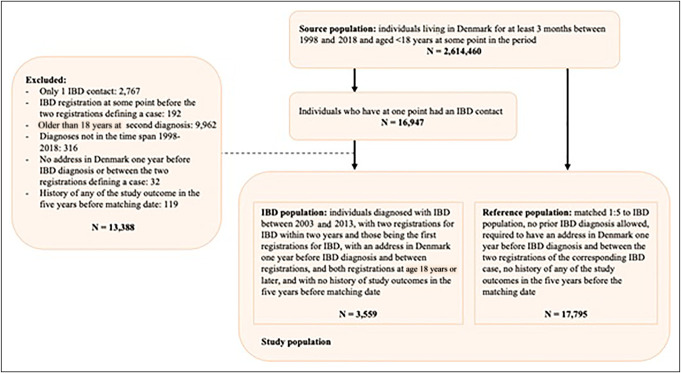
Within the source population of 2,614,228 people, we identified 3,559 patients with pediatric-onset IBD and 17,795 matched reference individuals (Table 1 and Figure 1). The reference group was selected to have the same distribution of age, sex, and municipality of residence in the same period as their corresponding IBD case. The IBD cohort consisted of 49.1% female patients and 50.9% male patients, with slightly more male patients having CD and slightly more female patients having UC (Table 1). The mean age at diagnosis of IBD was 13.3 years, and the most common age group of diagnosis in our study was 10–14 years overall and for Crohn's disease, whereas the most frequent occurrence of UC was observed in the 15–17 years age group. The mean length of follow-up varied between 8.8 and 9.3 years, depending on the frequency of the outcome.
Table 1.
Baseline characteristics for patients diagnosed with IBD in Denmark between 1998 and 2018 and matched reference individuals
| IBD (n = 3,559) | Crohn's disease (n = 1,813) | Ulcerative colitis (n = 1,746) | References (n = 17,795) | |
| Mean age at IBD diagnosis/index date | 13.3 (3.6) | 13.5 (3.3) | 13.2 (3.9) | 13.3 (3.6) |
| Age at diagnosis or index date | ||||
| <10 yr | 458 (16.5%) | 210 (14.9%) | 248 (18.2%) | 2,290 (16.5%) |
| 10–14 yr | 1,226 (44.2%) | 669 (47.7%) | 557 (40.8%) | 6,130 (44.2%) |
| 15–17 yr | 1,091 (39.3%) | 532 (37.7%) | 559 (41.0%) | 5,455 (39.3%) |
| Sex | ||||
| Female | 1,749 (49.1%) | 854 (47.1%) | 895 (51.3%) | 8,745 (49.1%) |
| Male | 1,810 (50.9%) | 959 (52.9%) | 851 (48.7%) | 9,050 (50.9%) |
| Year of IBD diagnosis or index date | ||||
| 1998–2004 | 924 (26.0%) | 409 (22.6%) | 515 (29.5%) | 4,620 (26.0%) |
| 2005–2011 | 1,223 (34.4%) | 603 (33.3%) | 620 (35.5%) | 6,115 (34.4%) |
| 2012–2018 | 1,412 (39.7%) | 801 (44.2%) | 611 (35.0%) | 7,060 (39.7%) |
IBD, inflammatory bowel disease.
Figure 1.
Flowchart for patient and reference inclusion. IBD, inflammatory bowel disease.
Risk of outcomes after IBD diagnosis
Overall, patients with IBD had an increased risk of developing depression (HR, 1.50; 95% CI, 1.26–1.80) and using antidepressants (HR, 1.54; 95% CI, 1.39–1.71) (Table 2). Kaplan-Meier curves show that the risk remained constantly increased over time with no point in time representing a particularly increased risk (Figure 2). Conversely, we found a decreased risk of using methylphenidate (HR, 0.75; 95% CI, 0.58–0.98) and a slightly reduced, but not statistically significant, risk of being diagnosed with ADHD (HR, 0.77; 95% CI, 0.56–1.06) (Table 2), both of which remained reduced over time (Figure 2). The risk of anxiety was similar in patients with IBD compared with the reference population (HR, 1.14; 95% CI, 0.88–1.49) (Table 2 and Figure 2).
Table 2.
Frequency, incidence rate, and hazard ratio for having a hospital contact for anxiety, ADHD, or depression or having a dispensed prescription for antidepressants or methylphenidate in the years after IBD diagnosis or index date
| IBD | Crohn's disease | Ulcerative colitis | ||||
| IR/1,000 PY | HR (95% CI) | IR/1,000 PY | HR (95% CI) | IR/1,000 PY | HR (95% CI) | |
| Depression | ||||||
| References | 3.18 | 1 (ref) | 3.10 | 1 (ref) | 3.25 | 1 (ref) |
| IBD | 4.76 | 1.50 (1.26–1.80) | 5.35 | 1.73 (1.35–2.22) | 4.22 | 1.30 (1.01–1.69) |
| Anxiety | ||||||
| References | 1.79 | 1 (ref) | 1.78 | 1 (ref) | 1.81 | 1 (ref) |
| IBD | 2.05 | 1.14 (0.88–1.49) | 2.08 | 1.17 (0.80–1.71) | 2.02 | 1.12 (0.77–1.61) |
| ADHD | ||||||
| References | 1.67 | 1 (ref) | 1.72 | 1 (ref) | 1.64 | 1 (ref) |
| IBD | 1.29 | 0.77 (0.56–1.06) | 1.57 | 0.92 (0.60–1.40) | 1.03 | 0.63 (0.39–1.03) |
| Antidepressants | ||||||
| References | 10.29 | 1 (ref) | 10.07 | 1 (ref) | 10.49 | 1 (ref) |
| IBD | 15.71 | 1.54 (1.39–1.71) | 15.85 | 1.59 (1.37–1.84) | 15.58 | 1.50 (1.30–1.73) |
| Methylphenidate | ||||||
| References | 2.49 | 1 (ref) | 2.29 | 1 (ref) | 2.64 | 1 (ref) |
| IBD | 1.87 | 0.75 (0.58–0.98) | 2.08 | 0.90 (0.62–1.31) | 1.67 | 0.63 (0.43–0.93) |
See Supplementary Table 1, http://links.lww.com/CTG/B37 for event numbers and total numbers of person years.
ADHD, attention-deficit/hyperactivity disorder; CI, confidence interval; HR, hazard ratio; IBD, inflammatory bowel disease; IR, incidence rate; PY, person years.
Figure 2.
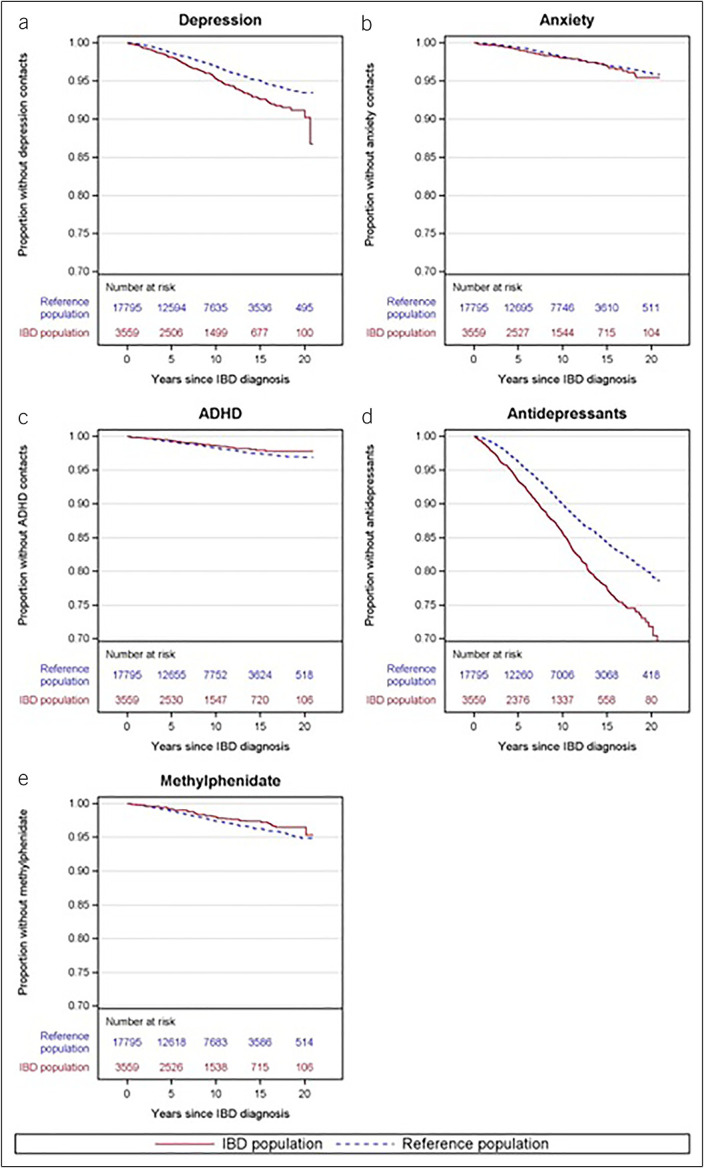
Kaplan-Meier curves for cumulative incidence of depression (a), anxiety (b), ADHD (c), use of antidepressants (d), and use of methylphenidate (e) in patients with IBD (red full line) and matched references (blue dotted line). ADHD, attention-deficit/hyperactivity disorder; IBD, inflammatory bowel disease.
Risk by IBD subtype
Patients with CD had an increased risk of depression (HR, 1.73; 95% CI, 1.35–2.22) and of using antidepressants (HR, 1.59; 95% CI, 1.37–1.84) compared with the reference group. The risk of depression and of using antidepressants remained persistently increased over time in the follow-up period (see Supplementary Figure 1, http://links.lww.com/CTG/B37). We found no association between CD and ADHD (HR, 0.92; 95% CI, 0.60–1.40), anxiety (HR, 1.17; 95% CI, 0.80–1.71), or using methylphenidate (HR, 0.90; 95% CI, 0.62–1.31), respectively (Table 2).
Patients with UC had a decreased risk of using methylphenidate compared with the reference group (HR, 0.63; 95% CI, 0.43–0.93), and a tendency toward reduced risk of being diagnosed with ADHD (HR, 0.63; 95% CI, 0.39–1.03) (Table 2). The reduced risk of both outcomes was quite persistent over time (see Supplementary Figure 2, http://links.lww.com/CTG/B37). The risk of depression (HR, 1.30; 95% CI, 1.01–1.69) and of use of antidepressants (HR, 1.50; 95% CI, 1.30–1.73) was persistently increased in patients with UC, although lower than in patients with CD (Table 2 and see Supplementary Figure 2, http://links.lww.com/CTG/B37). There was no association between UC and anxiety (HR, 1.12; 95% CI, 0.77–1.61) (Table 2).
Risk by sex and age
In Table 3, the risk of each outcome is stratified by age at IBD diagnosis and sex. Overall, most results were not dependent on age at diagnosis or sex. However, patients with IBD diagnosed between 15 and 17 years had a slightly higher risk of depression (HR, 2.0; 95% CI, 1.5–2.6) compared with those diagnosed before 14 years (HR, 1.3; 95% CI, 1.0–1.7) (P = 0.04). The difference by age at diagnosis was not seen for use of antidepressants, but male patients with IBD had a higher risk of receiving antidepressants (HR, 1.8; 95% CI, 1.5–2.1) compared with female patients (HR, 1.4; 95% CI, 1.2–1.6) (P = 0.02), although overall, female patients both with and without IBD had higher incidence rates of antidepressant use than male patients.
Table 3.
Hazard ratios divided by age at diagnosis and sex for having a hospital contact for anxiety, depression, or ADHD or having a dispensed prescription for antidepressants or methylphenidate after IBD diagnosis/index date in patients with IBD and matched reference individuals
| Age group/sex | IBD (n = 3,359) | References (n = 1,795) | HR (95% CI) | P value | ||
| Cases | IR/1,000 PY | Cases | IR/1,000 PY | |||
| Depression | ||||||
| <14 yr | 63 | 3.59 | 247 | 2.79 | 1.3 (1.0–1.7) | 0.04 |
| 15–17 yr | 65 | 6.66 | 169 | 3.40 | 2.0 (1.5–2.6) | |
| Female | 101 | 6.26 | 357 | 4.37 | 1.4 (1.2–1.8) | 0.48 |
| Male | 54 | 3.30 | 167 | 2.01 | 1.6 (1.2–2.2) | |
| Anxiety | ||||||
| <14 yr | 34 | 1.91 | 132 | 1.48 | 1.3 (0.9–1.9) | 0.26 |
| 15–17 yr | 21 | 2.10 | 115 | 2.29 | 0.9 (0.6–1.5) | |
| Female | 41 | 2.48 | 198 | 2.39 | 1.0 (0.7–1.5) | 0.34 |
| Male | 27 | 1.63 | 101 | 1.21 | 1.3 (0.9–2.1) | |
| ADHD | ||||||
| <14 yr | 21 | 1.18 | 170 | 1.91 | 0.6 (0.4–1.0) | 0.09 |
| 15–17 yr | 16 | 1.60 | 70 | 1.39 | 1.1 (0.7–2.0) | |
| Female | 19 | 1.14 | 121 | 1.46 | 0.8 (0.5–1.3) | 0.94 |
| Male | 24 | 1.45 | 158 | 1.90 | 0.8 (0.5–1.2) | |
| Antidepressants | ||||||
| <14 yr | 209 | 12.58 | 688 | 8.03 | 1.6 (1.4–1.9) | 0.54 |
| 15–17 yr | 167 | 18.61 | 595 | 12.74 | 1.5 (1.2–1.8) | |
| Female | 279 | 18.93 | 1,046 | 13.66 | 1.4 (1.2–1.6) | 0.02 |
| Male | 197 | 12.66 | 572 | 7.10 | 1.8 (1.5–2.1) | |
| Methylphenidate | ||||||
| <14 yr | 35 | 1.98 | 238 | 2.69 | 0.7 (0.5–1.0) | 0.92 |
| 15–17 yr | 18 | 1.80 | 119 | 2.37 | 0.8 (0.5–1.2) | |
| Female | 24 | 1.44 | 159 | 1.92 | 0.8 (0.5–1.2) | 1.00 |
| Male | 38 | 2.31 | 253 | 3.06 | 0.8 (0.5–1.1) | |
The P value represents the test for including the interaction term in the Cox regression model.
ADHD, attention-deficit/hyperactivity disorder; CI, confidence interval; HR, hazard ratio; IBD, inflammatory bowel disease; IR, incidence rate; PY, person-years.
DISCUSSION
This Danish nationwide cohort study included 3,359 patients with pediatric-onset IBD and 17,795 matched reference individuals. We examined the psychiatric comorbidity for almost a decade after an IBD diagnosis in childhood to reach a greater level of understanding of the burden of these diseases. We found that patients suffering from pediatric-onset IBD have a 50% higher risk of depression and 54% higher risk of using antidepressants, and the risk was persistently increased for up to 20 years after IBD diagnosis. Surprisingly, we found that patients with pediatric-onset UC had a 25% reduced risk of using methylphenidate, the most common therapeutic for treating ADHD (20), as well as a reduced, although not statistically significant, risk of being diagnosed with ADHD.
Few studies have investigated the incidence and prevalence of anxiety and depression in patients with pediatric-onset IBD. The increased risk of depression but not of anxiety found in our study aligns with the results from a British study, limited to patients from primary care, which found an increased risk of depression in patients diagnosed with IBD between 10 and 18 years (incidence rate ratio, 1.53; 95% CI, 1.25–1.87) but no association with anxiety (0.96; 95% CI, 0.72–1.25) (21). This contrasts with an insurance-based US study of pediatric patients with CD suggesting an increased risk of both depression (1.74; 95% CI, 1.35–2.25) and anxiety (2.28; 95% CI, 1.65–2.17) (22). A population-based large-scale study from Sweden suggested that patients with pediatric-onset IBD not only had an increased risk of mood disorders (HR, 1.60; 95% CI, 1.40–1.70) and anxiety (HR, 1.90; 95% CI, 1.70–2.00) but also were diagnosed with ADHD (HR, 1.20; 95% CI, 1.10–1.40) (11), which was not confirmed in the present study. The increased risk of depression seems robust across several populations, whereas the risk of anxiety and ADHD differs markedly across previous studies. A contributing factor to the contrasting results in the mentioned studies could be surveillance bias because it is generally assumed that patients diagnosed with IBD have a closer relation with the healthcare system and thereby have a logically higher risk of discovering psychiatric comorbidity. This bias might vary in importance in different populations, but it is unlikely to be the only explanation, and especially, it cannot explain the observation of a decreased risk of ADHD among patients with UC in this study, which was confirmed by analyses of prescription for methylphenidate. A plausible explanation for the lower use of methylphenidate in patients with IBD could lie in the life adjustments toward a more structured daily life that often follow a diagnosis with IBD. Having IBD might lead to parents ensuring a more balanced diet, to a greater need for routines around toilet accessibility, and to more time away from environments where symptoms of ADHD might worsen, such as school. Hence, having IBD might provide children who also have ADHD with a more supportive environment that could lead them to not being formally diagnosed or—if they are diagnosed—to having medical therapy prescribed less often compared with patients with ADHD who did not have IBD.
On performing subgroup analysis, we found that both patients with CD and UC have an increased risk of depression and of using antidepressants, although the risk was highest for patients with CD, which aligns with several studies in adult-onset IBD (6,7,23). Interestingly, only patients with UC had a lower risk of using methylphenidate and a lower risk of being diagnosed with ADHD, although that association did not reach statistical significance. Still, the association seems robust because the 2 outcomes support and internally validate each other.
The stratified analysis showed only few significant differences by age and sex. We did find a higher increased risk of having a hospital contact for depression in the patients diagnosed with IBD between 15 and 17 years compared with those diagnosed at 14 years or younger. This could reflect a possible higher vulnerability during the teenage years. However, we found no significant difference by age on risk of having a dispensed prescription for antidepressants, which is puzzling because we presume that clinicians would be more reluctant to use antidepressants in small children compared with teenagers, so these results should be interpreted with some caution. The same holds true for the observed higher increased risk of antidepressant use in male compared with female patients, which is not found for the outcome of depression.
A major strength of this study lies in the use of nationwide registries covering a unified hospital care system, hence allowing the establishment and longitudinal study of a large, unselected population of patients suffering from IBD diagnosed in childhood in Denmark. The data in the registers are collected prospectively, thus eliminating the risk of recall bias usually associated with retrospective analyses. This population is representative of pediatric patients with IBD in Denmark and presumably generalizable to other populations. The use of time-dependent matching increased the ability to account for period effects and thereby the validity of the results. To ensure valid IBD diagnoses, cases were only included if they had at least 2 hospital contacts for IBD within a 2-year period, ensuring a positive predictive value of 95% (18). Patients were followed from the time of IBD diagnosis to the event or censoring, and no individuals were lost to follow-up. By using both hospital contacts and dispensed prescriptions, we were able to capture a broad spectrum of outcome severities, particularly of depression and anxiety. Generally, for someone to be treated in hospital for depression or anxiety, they will likely have a severe presentation of the diseases while someone with more moderate depression or anxiety is more often treated by a general practitioner or a psychiatrist in private practice, which would not be recorded in the DNPR. However, any prescription dispensed at a retail pharmacy in Denmark is registered in the prescription register regardless of the workplace of the prescriber. Thus, the prescriptions for antidepressants and methylphenidate capture all patients, whether treated in hospital, in general practice, or in a private psychiatrist practice.
Potential limitations are also present in this cohort study. Although the national registers contain a large amount of data, granular information on disease activity, symptoms, and severity are not contained in the registers. These data could provide an intel of potential flare-ups in relation to psychiatric comorbidity. Another potential limitation is our interpretation of dispensed prescriptions for antidepressants as a proxy measure for moderate-to-severe depression, although antidepressants are approved to treat other conditions, such as obsessive compulsive disorder and pain. However, we have previously shown that the majority of prescribed antidepressants in Denmark are used to treat depression (6).
In this nationwide population-based cohort study of >3,000 patients with pediatric-onset IBD, we demonstrate an increased risk of depression, particularly after CD, whereas we could not confirm an increased risk of anxiety. Importantly, we found that patients with pediatric-onset UC had decreased risk of being diagnosed with ADHD and receiving methylphenidate, which is the preferred and most widely used ADHD medication. Unselected, and hence generalizable, data on psychiatric comorbidity in pediatric-onset IBD are limited, and further research is needed to understand the underlying mechanisms of these comorbidities. It is evident from the consistent findings around depression in pediatric-onset IBD that awareness of this comorbidity should be incorporated in clinical care. Identification and management of depression is crucial to enhance overall well-being among these chronically ill young individuals.
CONFLICTS OF INTEREST
Guarantor of the article: Tine Jess, DMSci.
Specific author contributions: All authors conceived of and designed the study and collected and analyzed the data. R.K. and T.B. drafted the manuscript. All authors had access to and interpreted the data, revised the manuscript, and approved the final manuscript.
Financial support: The Danish National Research Foundation [DNRF148], the Lundbeck Foundation [R313-2019-857], and Aage og Johanne Louis-Hansens Fond [9688-3374 TJS]. The funding sources had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. The researchers were independent from the funders, and all authors had full access to all the data in the study and can take full responsibility for the integrity of the data and accuracy of the data analysis.
Potential competing interests: T.J. has been paid a consulting fee from Ferring Pharmaceuticals. All other authors: none declared.
Data sharing statement: The Danish National Registers provided the data for this study, which cannot be made publicly available as they are protected by the Danish Act on Processing of Personal Data. Researchers can access the data by applying to and getting approval from The Danish Data Protection Agency and the Danish Health Data Authority https://sundhedsdatastyrelsen.dk.
Study Highlights.
WHAT IS KNOWN
✓ Inflammatory bowel disease (IBD) is associated with increased risk of anxiety and depression in adults.
✓ Data on psychiatric comorbidity are scarce in patients with pediatric-onset IBD.
WHAT IS NEW HERE
✓ Danish patients with pediatric-onset IBD have increased risk of depression.
✓ The risk of depression is particularly high in children with Crohn's disease.
✓ Remarkably, children with ulcerative colitis had a decreased risk of attention-deficit/hyperactivity disorder and of using methylphenidate.
Supplementary Material
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at http://links.lww.com/CTG/B37
Rebecca Kristine Kappel, Tania Hviid Bisgaard contributed equally to this work.
Contributor Information
Rebecca Kristine Kappel, Email: rkappe20@student.aau.dk.
Gry Poulsen, Email: Gryjp@dcm.aau.dk.
Tine Jess, Email: Jess@dcm.aau.dk.
REFERENCES
- 1.Høivik ML, Moum B, Solberg IC, et al. Work disability in inflammatory bowel disease patients 10 years after disease onset: Results from the IBSEN Study. Gut 2013;62(3):368–75. [DOI] [PubMed] [Google Scholar]
- 2.Dubinsky MC, Dotan I, Rubin DT, et al. Burden of comorbid anxiety and depression in patients with inflammatory bowel disease: A systematic literature review. Expert Rev Gastroenterol Hepatol 2021;15(9):985–97. [DOI] [PubMed] [Google Scholar]
- 3.Knowles SR, Graff LA, Wilding H, et al. Quality of life in inflammatory bowel disease: A systematic review and meta-analyses–part I. Inflamm Bowel Dis 2018;24(4):742–51. [DOI] [PubMed] [Google Scholar]
- 4.Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;142(1):46–54.e42; quiz e30. [DOI] [PubMed] [Google Scholar]
- 5.Seyedian SS, Nokhostin F, Malamir MD. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. J Med Life 2019;12(2):113–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bisgaard TH, Poulsen G, Allin KH, et al. Longitudinal trajectories of anxiety, depression, and bipolar disorder in inflammatory bowel disease: A population-based cohort study. eClinicalMedicine 2023;59:101986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ludvigsson JF, Olén O, Larsson H, et al. Association between inflammatory bowel disease and psychiatric morbidity and suicide: A Swedish nationwide population-based cohort study with sibling comparisons. J Crohns Colitis 2021;15(11):1824–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barberio B, Zamani M, Black CJ, et al. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: A systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2021;6(5):359–70. [DOI] [PubMed] [Google Scholar]
- 9.Stapersma L, van den Brink G, Szigethy EM, et al. Systematic review with meta-analysis: Anxiety and depression in children and adolescents with inflammatory bowel disease. Aliment Pharmacol Ther 2018;48(5):496–506. [DOI] [PubMed] [Google Scholar]
- 10.Bisgaard TH, Allin KH, Elmahdi R, et al. The bidirectional risk of inflammatory bowel disease and anxiety or depression: A systematic review and meta-analysis. Gen Hosp Psychiatry 2023;83:109–16. [DOI] [PubMed] [Google Scholar]
- 11.Butwicka A, Olén O, Larsson H, et al. Association of childhood-onset inflammatory bowel disease with risk of psychiatric disorders and suicide attempt. JAMA Pediatr 2019;173(10):969–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bisgaard TH, Allin KH, Keefer L, et al. Depression and anxiety in inflammatory bowel disease: Epidemiology, mechanisms and treatment. Nat Rev Gastroenterol Hepatol 2022;19(11):717–26. [DOI] [PubMed] [Google Scholar]
- 13.Fülling C, Dinan TG, Cryan JF. Gut microbe to brain signaling: What happens in vagus…. Neuron 2019;101(6):998–1002. [DOI] [PubMed] [Google Scholar]
- 14.Clapp M, Aurora N, Herrera L, et al. Gut microbiota's effect on mental health: The gut-brain axis. Clin Pract 2017;7(4):987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dam SA, Mostert JC, Szopinska-Tokov JW, et al. The role of the gut-brain axis in attention-deficit/hyperactivity disorder. Gastroenterol Clin North Am 2019;48(3):407–31. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt M, Pedersen L, Sørensen HT. The Danish Civil registration system as a tool in epidemiology. Eur J Epidemiol 2014;29(8):541–9. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt M, Schmidt SAJ, Sandegaard JL, et al. The Danish national patient registry: A review of content, data quality, and research potential. Clin Epidemiol 2015;7:449–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Albaek Jacobsen H, Jess T, Larsen L. Validity of inflammatory bowel disease diagnoses in the Danish national patient registry: A population-based study from the north Denmark region. Clin Epidemiol 2022;14:1099–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wallach Kildemoes H, Toft Sørensen H, Hallas J. The Danish national prescription registry. Scand J Public Health 2011;39(7 Suppl l):38–41. [DOI] [PubMed] [Google Scholar]
- 20.Drechsler R, Brem S, Brandeis D, et al. ADHD: Current concepts and treatments in children and adolescents. Neuropediatrics 2020;51(5):315–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Umar N, King D, Chandan JS, et al. The association between inflammatory bowel disease and mental ill health: A retrospective cohort study using data from UK primary care. Aliment Pharmacol Ther 2022;56(5):814–22. [DOI] [PubMed] [Google Scholar]
- 22.Loftus EV, Guérin A, Yu AP, et al. Increased risks of developing anxiety and depression in young patients with Crohn's disease. Am J Gastroenterol 2011;106(9):1670–7. [DOI] [PubMed] [Google Scholar]
- 23.Choi K, Chun J, Han K, et al. Risk of anxiety and depression in patients with inflammatory bowel disease: A nationwide, population-based study. J Clin Med 2019;8(5):654. [DOI] [PMC free article] [PubMed] [Google Scholar]