Abstract
Background
Periprosthetic fracture is a rare complication of arthroplasty but can have devastating consequences for the patient and presents a complex surgical challenge. Locking compression plate and retrograde intramedullary nail are both widely accepted surgical fixation techniques for distal femoral periprosthetic fractures around a total knee arthroplasty. Although there is still a need for further high-quality research into both techniques, there is even less literature concerning the use of distal femoral replacement to treat distal femoral periprosthetic fractures. Interest has been piqued in distal femoral replacements for the treatment of distal femoral periprosthetic fractures due to the theoretical advantages of immediate post-operative weight-bearing and lack of dependence on fracture union, but there are still understandably reservations about performing such an extensive and invasive procedure when an accepted alternative is available. This meta-analysis aims to evaluate the current literature to compare the complication rates and return to pre-operative ambulatory status of distal femoral replacement and locking compression plate.
Method
A literature search was performed to identify articles related to the management of distal femoral periprosthetic fractures around a total knee arthroplasty in adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. Methodological quality was assessed using the methodological index for non-randomized studies (MINORS) criteria. Articles were reviewed, and data extracted for analysis.
Results
Five articles met the inclusion criteria, reporting on 345 periprosthetic fractures. The overall rates of complications for distal femoral replacement and locking compression plate were: re-operation (6.1% vs 12.1%), infection (3.0% vs 5.3%), mortality (19.7% vs 19.3%), and return to pre-operative ambulatory status (60.9% vs 71.8%) (respectively).
Conclusion
This meta-analysis shows no statistically significant difference in the rates of re-operation, infection, mortality or return to pre-operative ambulatory status when comparing distal femoral replacement to locking compression plate.
Keywords: Periprosthetic fracture, locking compression plating, distal femoral replacement, knee replacement, arthroplasty, knee
Introduction
As of its 2022 annual report, the United Kingdom (UK) National Joint Registry (NJR) has recorded over 1.4 million primary knee replacements since its inception in 2002. From these primary procedures, 92,919 knee revision procedures have been recorded in the UK NJR since 2002, 3,746 (4%) of which were for periprosthetic fracture (PPF).1 This would represent an incidence of 0.26% according to the UK NJR, but other large joint registries estimate the rates of PPF around a total knee arthroplasty (TKA) to be just over 1%.2–4
Whilst PPF is a rare complication of arthroplasty, it can have devastating consequences for the patient and presents a complex surgical challenge.5–8 Mortality has been reported as up to 17% at one year post-operatively by Streubel et al. and similar to that after a hip fracture by Bhattacharyya et al.5,6 Beyond mortality, there is significant morbidity after PPF from surgical complications and post-operative decline in knee function. A recent meta-analysis by Shin et al., comparing outcomes after locking compression plate (LCP) against retrograde intramedullary nail (RIMN), reported 24% of patients requiring revision surgery whilst Mardian et al. described only 20% of patients being able to mobilise post-operatively without assistance.9,10
Unfortunately, the surgical challenge of managing distal femoral PPFs is multi-factorial and not easily solved. Central to this clinical conundrum lies the advanced age of this patient cohort, as PPFs are often low-energy fragility fractures in elderly patients, and achieving stable fixation in elderly patients with poor bone stock and fragile bone quality is surgically challenging.4,11–14 Furthermore, with increasing age comes the unavoidable increased likelihood of underlying medical co-morbidities and predisposition to post-operative complications.12–15
LCP and RIMN are both widely accepted surgical fixation techniques for distal femoral PPFs around a TKA, with equivocal complication rates on recent meta-analyses.9,16 Although there is still a need for further high-quality research into both of these techniques, there is even less literature concerning the use of DFR to treat distal femoral PPFs. Interest has been piqued in DFR for the treatment of distal femoral PPFs due to the theoretical advantages of immediate post-operative weight-bearing and lack of dependence on fracture union.17 However, DFR is a far more invasive and extensive operation, with less salvage options should a major complication occur. Wyles et al. reported all-cause revision and any re-operation rates of 27.5% and 46.3% respectively at 10 years post-operatively, when using DFR as either a primary or revision prosthesis for a variety of indications.18 In cases where the femoral component is loose and bone stock is poor, DFR is recommended due to the necessity for revision arthroplasty and the likelihood of non-union with LCP or RIMN. However, in less clinically clear-cut cases, there exists a delicate management equipoise weighing the theoretical advantages and disadvantages of DFR compared to LCP or RIMN. This meta-analysis aims to evaluate the current literature to compare the complication rates and return to pre-operative ambulatory status of DFR and LCP.
Methods
Literature search strategy
This systematic review and meta-analysis was conducted in adherence to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist.19 Searches were conducted on PubMed/Medline looking at literature published between January 2012 and December 2022. The search terms were as follows: Total knee arthroplasty (All Fields) OR Total knee replacement (MeSH Terms) AND Periprosthetic Fracture (All Fields) OR Peri-prosthetic Fracture (MeSH Terms)’. Articles generated were then screened and excluded in accordance with outlined eligibility criteria by two authors independently.
Eligibility
Inclusion criteria: articles published between 1st January 2012 and 31st December 2022, primary procedures (revision procedures of failed fracture treatment not included), articles of evidence levels I-III and English language texts only. Procedures included were LCP and DFR.
Exclusion criteria: native distal femoral fractures, non-traumatic indications for arthroplasty, case series, reports, letters, conference articles and abstracts, repeated studies and data, cadaveric and animal studies and studies deemed poorly designed and of evidence levels IV-V. Procedures excluded were revision arthroplasty, RIMN, combination fixation strategies (LCP and RIMN hybrids), external fixation and conventional non-locked plating.
Data extraction and analysis
Two of the authors independently extracted data from the included articles and discussions were held for any data disputes. Study details were collated onto a Microsoft Excel 16.64 spreadsheet.
Review Manager 5.3 was used for data analysis. Mean difference and unpaired T-test were used to compare continuous data. Risk difference was used to analyse discrete data. Statistical significance was defined as P < 0.05, with confidence intervals of 95%. Chi squared was used to assess for heterogeneity in the pooled studies, with results represented through I2 . I2 cut offs for defining heterogeneity were as outlined in the Cochrane Handbook for Systematic Reviews of Interventions, 0-40% = low, 30- 60% = moderate, 50-90% = substantial 75%-100 = considerable.20 Results were presented as forest plots.
Outcome measures
The primary outcome measures of this review were post-operative rates of re-operation, infection, mortality and return to pre-operative ambulatory status. Data reporting length of post-operative hospital stay, mean operation duration and patient reported outcome measures (PROMs) were also collected.
Methodological Quality
The methodological index for non-randomized studies (MINORS) criteria was used to score the methodological quality of each study.21
Results
Literature Search
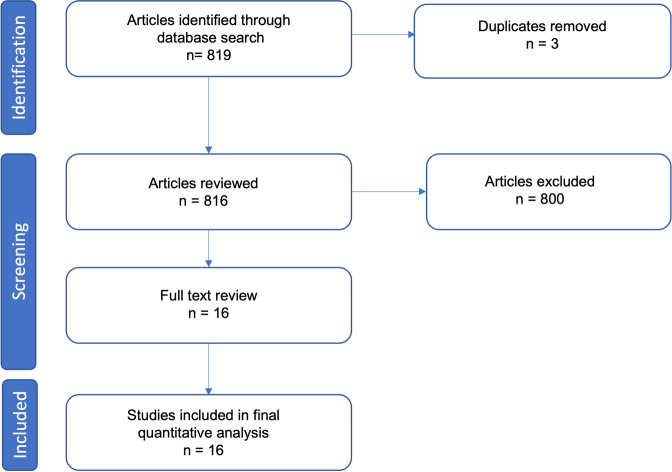
The literature search initially produced 969 articles, which were all screened by reviewing their title and abstract. Exclusions were made in accordance with aforementioned eligibility criteria. 5 articles were included for full text review and subsequently final quantitative analysis. The PRISMA flow diagram is shown below (see Fig. 1). All 5 of the final articles were retrospective cohort studies.
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram outlining study inclusion.
Quality Assessment
All included studies were deemed to meet the quality studies as assessed by the MINORS criteria (see Table 1).21–26
Table 1. MINORS criteria for each of the five included studies.
| Methodological Items for Non-Randomized Studies (MINORS) | Darrith et al., 201922 | Gan et al., 201823 | Hoellwarth et al., 201724 | Ross et al., 202125 | Ruder et al., 201626 |
|---|---|---|---|---|---|
| 1. A clearly stated aim | 2 | 2 | 2 | 2 | 2 |
| 2. Inclusion of consecutive patients | 2 | 2 | 2 | 2 | 1 |
| 3. Prospective collection of data | 0 | 0 | 0 | 0 | 0 |
| 4. Endpoints appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 |
| 5. Unbiased assessment of the study endpoint | 0 | 0 | 0 | 0 | 0 |
| 6. Follow-up period appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 |
| 7. Loss to follow-up <5% | 2 | 2 | 2 | 2 | 2 |
| 8. Prospective calculation of the study size | 0 | 0 | 0 | 0 | 0 |
| 9. An adequate control group | 2 | 2 | 2 | 2 | 2 |
| 10. Contemporary groups | 2 | 2 | 2 | 2 | 2 |
| 11. Baseline equivalence of groups | 1 | 2 | 2 | 2 | 1 |
| 12. Adequate statistical analysis | 2 | 2 | 2 | 2 | 2 |
Study Characteristics
The five included studies reported a total of 345 PPFs. 207 were treated with LCP, 132 with DFR, 5 with RIMN and 1 with a non-locking plate. The latter two treatment modalities (RIMN and non-locking plate) were not included in this meta-analysis leading to a total of 339 PPFs reported in this study. The characteristics of the five included studies (see Table 2), and outcome measures (see Table 3) are shown below.22–26
Table 2. Overview of study characteristics.
| Study | n (by sex) | n (LCP vs DFR) | Mean age, years ± standard deviation (range in parenthesis) | Classification |
|---|---|---|---|---|
| Darrith et al., 201922 | n: 72 63 female |
44 LCP 22 DFR 5 RIMN 1 non-locking plate |
ORIF: 71.8 ± 10.6 DFR: 75.8 ± 8.4 |
72 Lewis and Rorabeck II |
| Gan et al., 201823 | n: 15 15 female |
8 LCP 7 DFR |
LCP: 67.9 ± 8.37 (56-78) DFR: 76.7 ± 7.78 (63-86) |
12 Lewis and Rorabeck II - 8 treated by LCP 3 Lewis and Rorabeck III |
| Hoellwarth et al., 201724 | n: 140 | 87 LCP 53 DFR |
LCP: 80.0 ± 9.9 DFR: 80.1 ± 7.8 |
140 OTA-33 |
| Ross et al., 202125 | n: 60 48 female |
33 LCP 27 DFR |
Total: 80.6 ± 9.2 (60-101) LCP: 81.3 ± 10.5 DFR: 78.8 ± 8.3 |
40 Su et al. II - 25 treated by LCP 20 Su et al. III - 8 treated by LCP |
| Ruder et al., 201626 | n: 58 46 female |
35 LCP 23 DFR |
Total: 80 (61-95) LCP: 78 (61-95) DFR: 83 (69-94) |
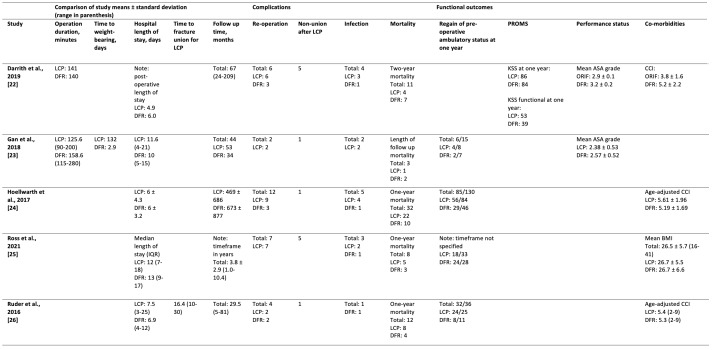
Table 3. Outcome measures by each study.
Indications and contraindications for DFR for treatment of distal femoral PPF
Each of the five studies described similar indications for DFR as a treatment of distal femoral PPF, most commonly significant fracture comminution and insufficient distal bone stock for adequate fixation by LCP.22–26 The indications for DFR as described in each individual study can be found in Table 4. Contraindications for DFR as reported by manufacturers include joint infection, sepsis, osteomyelitis, inadequate soft tissue coverage, osteoporosis, metabolic disorders which may impair bone formation, osteomalacia, distant foci of infections which may spread to the implant site, vascular insufficiency, muscular atrophy, and neuromuscular disease.27,28
Table 4. Reported indications for DFR in distal femoral PPF by study.
| Study | Reported indications for DFR |
|---|---|
| Darrith et al., 201922 | Severe fracture comminution Poor distal femoral bone quality Need for immediate post-op weight-bearing Contralateral lower extremity fracture requiring protected weight-bearing Patient preference |
| Gan et al., 201823 | Rorabeck and Taylor classification: Type 3 Or Type 2 and severe comminution or bone loss precluding fixation |
| Hoellwarth et al., 201724 | Significant fracture comminution Distal fractures with insufficient bone stock |
| Ross et al., 202125 | Insufficient distal bone stock for adequate fixation |
| Ruder et al., 201626 | Inadequate bone stock Incompetent collateral ligaments |
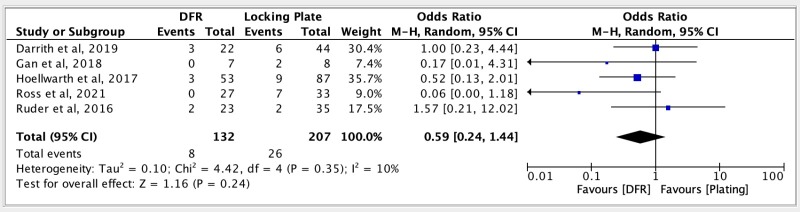
Re-operation
34 cases (10.0%) of re-operation were reported in a total of 339 patients across five studies comparing DFR and LCP, with low heterogeneity (I2 = 10%). Comparative analysis found no statistically significant difference (see Fig. 2).22–26
Figure 2. Forest Plot showing comparison of re-operation rate between DFR and LCP.
M-H = Mantel-Haenszel, CI = Confidence Interval
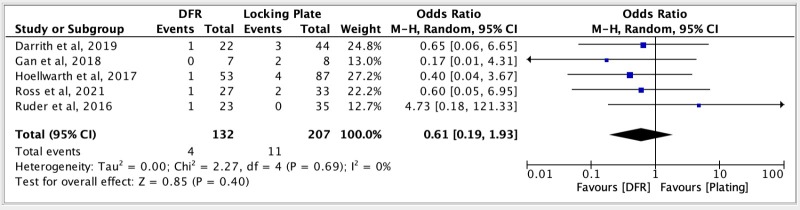
Infection
15 cases (4.4%) of infection were reported in a total of 339 patients across five studies comparing DFR and LCP, with low heterogeneity (I2 = 0%). Comparative analysis found no statistically significant difference (see Fig. 3).22–26
Figure 3. Forest Plot showing comparison of infection rate between DFR and LCP.
M-H = Mantel-Haenszel, CI = Confidence Interval
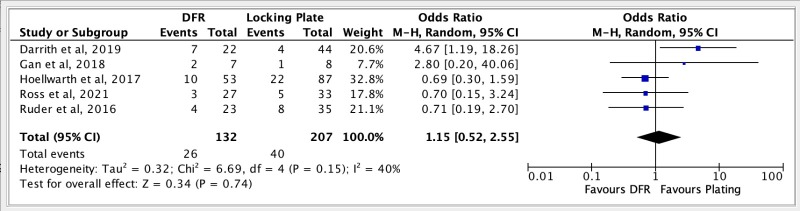
Mortality
66 mortalities (19.5%) were reported in a total of 339 patients across five studies comparing DFR and LCP, with moderate heterogeneity (I2 = 40%). Comparative analysis found no statistically significant difference (see Fig. 4).22–26
Figure 4. Forest Plot showing comparison of mortality rate between DFR and LCP.
M-H = Mantel-Haenszel, CI = Confidence Interval
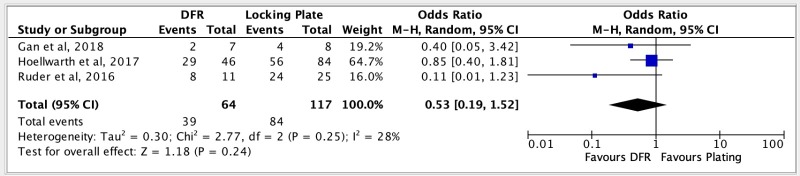
Return to pre-operative ambulatory status
123 patients (63%) out of a total of 181 patients across three studies, were reported to have returned to their pre-operative ambulatory status post-operatively. These studies demonstrated low heterogeneity (I2 = 28%) and comparative analysis showed no statistically significant difference when comparing DFR and LCP (see Fig. 5).23,24,26
Figure 5. Forest Plot showing comparison of return to pre-operative ambulatory status between DFR and LCP.
M-H = Mantel-Haenszel, CI = Confidence Interval
Discussion
The aim of this meta-analysis was to review the current literature for the role of DFRs in the treatment of distal femoral PPFs over the last decade, particularly comparing the rates of complications to LCP; a more established treatment modality for distal femoral PPFs. This study suggests that the rates of complications following DFR and LCP for distal femoral PPFs, are comparable. This meta-analysis found no statistically significant difference between DFR and LCP in rates of re-operation (6.1% vs 12.1%), infection (3.0% vs 5.3%), mortality (19.7% vs 19/3%), and return to pre-operative ambulatory status (60.9% vs 71.8%) (respectively). These findings are summarised below in Table 4.
Table 4. Incidence of complications for DFR, LCP, and overall cohort.
| DFR | LCP | Overall | |
|---|---|---|---|
| Re-operation | 8/132 (6.1%) | 26/207 (12.6%) | 34/339 (10.0%) |
| Infection | 4/132 (3.0%) | 11/207 (5.3%) | 15/339 (4.4%) |
| Mortality | 26/132 (19.7%) | 40/207 (19.3%) | 66/339 (19.5%) |
| Return to pre-operative ambulatory status | 39/64 (60.9%) | 84/117 (71.8%) | 123/181 (68.0%) |
The results of this meta-analysis support the findings of recent meta-analyses by Quinzi et al. and Wadhwa et al., both of which also reported no significant difference in the complication and re-operation rates of LCP and DFR.29,30 Our analyses showed weak trends towards DFR resulting in fewer re-operations and infections but, perhaps counter-intuitively, more patients returning to their pre-operative ambulatory status post-LCP. Without significant statistical power, no conclusions can be drawn on these faint trends and more quality research is required to elucidate any meaningful results.
The indication and operative strategy for cases requiring re-operation was described in all five studies. Darrith et al. reported six cases requiring re-operation after LCP: three for infection and three for non-union. The three cases of infection were all managed differently: one with two stage LCP exchange; one with two stage revision to DFR; and one with debridement, antibiotics, and implant retention (DAIR) which was unsuccessful, and the infection spread to the ipsilateral total hip replacement causing sepsis and requiring hip disarticulation for source control. One of the cases of aseptic non-union after LCP was caused by plate breakage and required revision arthroplasty whilst the other two cases were managed successfully with revision LCP. Darrith et al. reported three patients requiring re-operation post-DFR: one for infection that was successfully treated with DAIR; and two for patella mal-tracking, one of which was treated with liner exchange and soft tissue release whilst the other required femoral component revision due to malrotation.22
Gan et al. described two cases requiring re-operation after surgery, both of which were after LCP. Both cases required intervention for surgical site infection: one for a deep surgical infection treated with debridement and plate removal and eventually resulting in a malunion; and the other for a septic non-union which was managed with two stage knee fusion.23
Hoellwarth et al. reported twelve cases requiring re-operation: nine after LCP and three after DFR. Of the nine re-operations post-LCP, three were due to surgical infection. Of these three cases, one was managed by revision with blade plate, one by DAIR, and one with knee fusion, the latter of whom eventually died during that admission. The indications for the six non-infected re-operations after LCP were: two for removal of prominent screws, one for fasciotomy due to compartment syndrome, one for evacuation of a haematoma that then became infected and required conversion to DFR, one for post-operative tibial fracture and one for non-union that was subsequently converted to DFR. The three re-operations post-DFR were all for different indications: one for “wound drainage”, one for soft tissue rebalancing to address a fixed flexion deformity, and one for revision of the tibial component due to impending fracture seen on post-operative imaging.24
Ross et al. described seven patients requiring re-operation, all of whom were treated initially with LCP. Five of these re-operations were due to non-union from plate failure; two of which were managed by conversion to DFR and the other three by re-fixation (one with RIMN and two with dual LCPs). The other two causes of re-operation were one case of re-fracture managed by conversion to DFR and one case of deep infection managed by revision TKA.25
Ruder et al. reported four patients requiring re-operation: two following LCP and two after DFR. The two cases of re-operation post-LCP were for malunion and non-union, both of which were revised to DFR. Both cases of re-operation after DFR were for non-healing wounds that were both managed with local muscle flaps and skin grafting.26 Across all five studies, 7 (3.4%) out of the 207 LCPs were eventually revised to DFRs, either for infection or non-/mal-union.22–26
Infection was a relatively rarely reported complication following both DFR and LCP but is associated with significant morbidity, with all reported deep surgical site infections managed surgically, as described above. Apart from the morbidity of re-operation, Darrith et al. reported one case eventually requiring hip disarticulation, Gan et al. described one case of infection resulting in malunion and Hoellwarth et al. reported one case of infection requiring knee fusion and culminating in the death of this patient in the same admission.22–24 Ross et al. and Ruder et al. also each described one case of superficial wound infection, both of which were successfully managed with antibiotics.25,26
Beyond the aforementioned post-operative morbidity, femoral PPFs are also associated with significant mortality.5,6 All five studies reported a mortality rate numerically, but only Gan et al. described all the causes of death in their cohort: one death from end stage renal failure at 18 months post-operatively post-DFR, one unrelated cause of death at 16 months post-operatively post-DFR, and one death from urosepsis at 46 months post-operatively post-LCP.23 Darrith et al. reported two deaths on the day of surgery in their DFR cohort from cardiopulmonary causes in patients with known cardiopulmonary disease, but did not report a cause of mortality for their other cases.22
Whilst analysis of the five included studies showed no statistically significant difference in mortality for patients treated with DFR compared to LCP, two of the studies found age, not treatment modality, to be the most strongly associated variable with poor outcomes.24,26 Hoellwarth et al. reported the mean age of one year survivors was 77 compared to 85 for patients who had died by one year post-operatively.24 Furthermore, Ruder et al. reported patients over the age of 85 to be more likely to lose the ability to ambulate and to live in a skilled nursing facility at one year post-operatively.26
Beyond the scope of the five studies included in this review, there are numerous articles reporting increasing age being a poor predictive factor for morbidity and mortality.31–34 Ricci et al. and Mortazavi et al. both also reported patients over the age of 85 being more likely to lose their ability to ambulate and lose their living independence at one year post-operatively.31,32 With regards to mortality, Mortazavi et al. and Rahman et al. both described younger patients having a lower one-year mortality rate.32,33 In a study by Drew et al., patients who died before final follow-up had a mean age of 84 years compared to 75 years for those still alive at final follow-up.34 Increasing age being associated with higher rates of morbidity and mortality is significant in the context of DFR for distal femoral PPF, as older patients are more likely to have poor bone stock, which (combined with an unstable femoral implant) is the indication for DFR compared to LCP in the treatment of distal femoral PPF. However, this theoretical selection bias has not produced any statistically significant results, as this meta-analysis shows no difference in complication rates when comparing DFR to LCP.
Only three of our five included studies reported on the return of patients to their pre-operative ambulatory status.23,24,26 As previously mentioned, there is a weak trend favouring return to pre-operative ambulatory status after LCP. However, this is the most weakly powered of our analyses and without a statistically significant result at this stage, no conclusion can be made without significant further research. Interestingly, the theoretical benefit of immediate post-operative weight bearing after DFR also did not translate to shorter length of hospital stay, with an overall weighted mean length of stay across all five studies being 6.6 days for DFR and 6.7 days for LCP (p=0.26).22–26
This meta-analysis has several limitations. As discussed above, there is a theoretical selection bias of DFR being more commonly used in older patients. Whilst only Ruder et al. reported patients treated with DFR to be significantly older compared to those treated with LCP, two of the other studies in this analysis did show non-significant trends of patients treated with DFR being older.22,23 Secondly, all five of the studies included in this meta-analysis were retrospective cohort studies and have relatively small numbers of cases, both of which reduce the statistical power of our analyses. Thirdly, we recognise that surgeon preference and local practice will influence choice of treatment modality and thus the number of each procedure performed. Fourthly, our five included studies measured mortality at three different endpoints, so caution should be taken when interpreting this amalgamated analysis. Finally, as mentioned above, data for return to pre-operative ambulatory status and functional outcomes was variably and inconsistently reported, allowing for no significant comparison to be made between DFR and LCP for these measures.
Conclusion
This meta-analysis shows no statistically significant difference in the rates of re-operation, infection, mortality or return to pre-operative ambulatory status when comparing DFR to LCP. At this early stage, the theoretical benefits of DFR over LCP have yet to be demonstrated, but more high-quality research with age and co-morbidity adjustment is necessary to fully evaluate the role of DFRs in the treatment of distal femoral PPFs in the elderly.
References
- National Joint Registry 19th Annual report of the UK NJR. https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2019th%20Annual%20Report%202022.pdf [PubMed]
- Pitta Michael, Esposito Christina I., Li Zhichang, Lee Yuo-yu, Wright Timothy M., Padgett Douglas E. The Journal of Arthroplasty. 2. Vol. 33. Elsevier BV; Failure After Modern Total Knee Arthroplasty: A Prospective Study of 18,065 Knees; pp. 407–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo Jae Doo, Kim Nam Ki. Knee Surgery & Related Research. 1. Vol. 27. Springer Science and Business Media LLC; Periprosthetic fractures following total knee arthroplasty; pp. 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh Jasvinder A, Jensen Matthew, Lewallen David. Acta Orthopaedica. 2. Vol. 84. Medical Journals Sweden AB; Predictors of periprosthetic fracture after total knee replacement: an analysis of 21,723 cases; pp. 170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Are extreme distal periprosthetic supracondylar fractures of the femur too distal to fix using a lateral locked plate? Streubel P.N.., et al. 2010J Bone Joint Surg Br. 92:527–34. doi: 10.1302/0301-620X.92B3.22996. [DOI] [PubMed] [Google Scholar]
- Bhattacharyya Timothy, Chang Denis, Meigs James B, Estok Daniel M, II, Malchau Henrik. The Journal of Bone and Joint Surgery-American Volume. 12. Vol. 89. Ovid Technologies (Wolters Kluwer Health); Mortality after periprosthetic fracture of the femur; pp. 2658–2662. [DOI] [PubMed] [Google Scholar]
- Streubel Philipp N., Ricci William M., Wong Ambrose, Gardner Michael J. Clin Orthop Relat Res. 4. Vol. 469. Ovid Technologies (Wolters Kluwer Health); Mortality after distal femur fractures in elderly patients; pp. 1188–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lizaur-Utrilla Alejandro, Miralles-Muñoz Francisco A., Sanz-Reig Javier. The Journal of Arthroplasty. 9. Vol. 28. Elsevier BV; Functional outcome of total knee arthroplasty after periprosthetic distal femoral fracture; pp. 1585–1588. [DOI] [PubMed] [Google Scholar]
- Shin Young-Soo, Kim Hyun-Jung, Lee Dae-Hee. Knee Surgery, Sports Traumatology, Arthroscopy. 9. Vol. 25. Wiley; Similar outcomes of locking compression plating and retrograde intramedullary nailing for periprosthetic supracondylar femoral fractures following total knee arthroplasty: a meta-analysis; pp. 2921–2928. [DOI] [PubMed] [Google Scholar]
- Märdian S., Schaser K.-D., Scheel F., Gruner J., Schwabe P. Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca. 2. Vol. 82. Galen, spol. s r.o.; Quality of life and functional outcome of periprosthetic fractures around the knee following knee arthroplasty; pp. 113–118. [DOI] [PubMed] [Google Scholar]
- One year after proximal or distal periprosthetic fracture of the femur -two conditions with divergent outcomes? Eschbach D.., et al. 2018Injury. 49:1176–1182. doi: 10.1016/j.injury.2018.04.025. [DOI] [PubMed] [Google Scholar]
- Elsoe Rasmus, Ceccotti Adriano Axel, Larsen Peter. International Orthopaedics. 1. Vol. 42. Springer Science and Business Media LLC; Population-based epidemiology and incidence of distal femur fractures; pp. 191–196. [DOI] [PubMed] [Google Scholar]
- Poole W. E. C., Wilson D. G. G., Guthrie H. C., Bellringer S. F., Freeman R., Guryel E., Nicol S. G. The Bone & Joint Journal. 7. 99-B. British Editorial Society of Bone & Joint Surgery; ‘Modern’ distal femoral locking plates allow safe, early weight-bearing with a high rate of union and low rate of failure: five-year experience from a United Kingdom major trauma centre; pp. 951–957. [DOI] [PubMed] [Google Scholar]
- Berend Keith R., Lombardi Adolph V. Clin Orthop Relat Res. 2. Vol. 467. Ovid Technologies (Wolters Kluwer Health); Distal femoral replacement in nontumor cases with severe bone loss and instability; pp. 485–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers Philip, Laboe Patrick, Johnson Kory J., Fredericks Peter D., Crichlow Renn J., Maar Dean C., Weber Timothy G. J Orthop Trauma. 3. Vol. 32. Ovid Technologies (Wolters Kluwer Health); Patient Mortality in Geriatric Distal Femur Fractures; pp. 111–115. [DOI] [PubMed] [Google Scholar]
- Magill Henry, Ponugoti Nikhil, Selim Amr, Platt James. Journal of Orthopaedic Surgery and Research. 1. Vol. 16. Springer Science and Business Media LLC; Locked compression plating versus retrograde intramedullary nailing in the treatment of periprosthetic supracondylar knee fractures: a systematic review and meta-analysis; p. 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordeiro EMILIO NOEL, Costa ROBERTO CAVALIERI, Carazzato JOAO GILBERTO, Silva JORGE DOS SANTOS. Clinical Orthopaedics and Related Research. Vol. 252. Ovid Technologies (Wolters Kluwer Health); Periprosthetic fractures in patients with total knee arthroplasties; pp. 182–189. [DOI] [PubMed] [Google Scholar]
- Wyles Cody C., Tibbo Meagan E., Yuan Brandon J., Trousdale Robert T., Berry Daniel J., Abdel Matthew P. Journal of Bone and Joint Surgery. 1. Vol. 102. Ovid Technologies (Wolters Kluwer Health); Long-Term Results of Total Knee Arthroplasty with Contemporary Distal Femoral Replacement; pp. 45–51. [DOI] [PubMed] [Google Scholar]
- The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Page M.J.., et al. 2021BMJ. 372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- www.training.cochrane.org/handbook Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023) updated August 2023).
- Slim Karem, Nini Emile, Forestier Damien, Kwiatkowski Fabrice, Panis Yves, Chipponi Jacques. ANZ Journal of Surgery. 9. Vol. 73. Wiley; Methodological index for non-randomized studies (minors): development and validation of a new instrument; pp. 712–716. [DOI] [PubMed] [Google Scholar]
- Periprosthetic Fractures of the Distal Femur: Is Open Reduction and Internal Fixation or Distal Femoral Replacement Superior? Darrith B.., et al. 2020J Arthroplasty. 35:1402–1406. doi: 10.1016/j.arth.2019.12.033. [DOI] [PubMed] [Google Scholar]
- Gan Gerrard, Teo Yee Hong, Kwek Ernest Beng Kee. Clinics in Orthopedic Surgery. 2. Vol. 10. The Korean Orthopaedic Association; Comparing Outcomes of Tumor Prosthesis Revision and Locking Plate Fixation in Supracondylar Femoral Periprosthetic Fractures; p. 174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoellwarth Jason S., Fourman Mitchell S., Crossett Lawrence, Goodman Mark, Siska Peter, Moloney Gele B., Tarkin Ivan S. Injury. 2. Vol. 49. Elsevier BV; Equivalent mortality and complication rates following periprosthetic distal femur fractures managed with either lateral locked plating or a distal femoral replacement; pp. 392–397. [DOI] [PubMed] [Google Scholar]
- Management of low periprosthetic distal femoral fractures. Ross L.A.., et al. 2021Bone Joint J. 103-B:635–643. doi: 10.1302/0301-620X.103B4.BJJ-2020-1710.R1. [DOI] [PubMed] [Google Scholar]
- Ruder John A., Hart Gavin P., Kneisl Jeffrey S., Springer Bryan D., Karunakar Madhav A. The Journal of Arthroplasty. 5. Vol. 32. Elsevier BV; Predictors of Functional Recovery Following Periprosthetic Distal Femur Fractures; pp. 1571–1575. [DOI] [PubMed] [Google Scholar]
- OSS Orthopaedic Salvage System Distal Femoral Replacement Surgical Technique. https://www.zimmerbiomet.com/content/dam/zb-corporate/en/products/specialties/LimbSalvage/oss-orthopedic-salvage-system/OSSOrthopedicSalvageSystemDistalFemoralReplacemetnSurgicalTechnique01452GLBLenREV0316.pdf
- ONKOS Surgery Minimally Invasive Grower Custom Distal Femoral Surgical Technique Passive Fixed Hinge Tibia. https://onkossurgical.com/wp-content/uploads/2023/07/Minimally-Invasive-Grower-Custom-Distal-Femoral-Surgical-Technique-Passive-Fixed-Hinge-Tibia.pdf
- Quinzi David A., Ramirez Gabriel, Kaplan Nathan B., Myers Thomas G., Thirukumaran Caroline P., Ricciardi Benjamin F. Archives of Orthopaedic and Trauma Surgery. 6. Vol. 141. Springer Science and Business Media LLC; Early complications and reoperation rates are similar amongst open reduction internal fixation, intramedullary nail, and distal femoral replacement for periprosthetic distal femur fractures: a systematic review and meta-analysis; pp. 997–1006. [DOI] [PubMed] [Google Scholar]
- Wadhwa Harsh, Salazar Brett P., Goodnough L. Henry, Van Rysselberghe Noelle L., DeBaun Malcolm R., Wong Hong-Nei, Gardner Michael J., Bishop Julius A. J Orthop Trauma. 1. Vol. 36. Ovid Technologies (Wolters Kluwer Health); Distal Femur Replacement Versus Open Reduction and Internal Fixation for Treatment of Periprosthetic Distal Femur Fractures: A Systematic Review and Meta-Analysis; pp. 1–6. [DOI] [PubMed] [Google Scholar]
- Operative management of periprosthetic femur fractures in the elderly using biological fracture reduction and fixation techniques. Ricci W.M., Borrelli J. 2007Injury. 38 Suppl 3:53–8. doi: 10.1016/j.injury.2007.08.012. [DOI] [PubMed] [Google Scholar]
- Mortazavi S.M. Javad, Kurd Mark F., Bender Benjamin, Post Zachary, Parvizi Javad, Purtill James J. The Journal of Arthroplasty. 5. Vol. 25. Elsevier BV; Distal femoral arthroplasty for the treatment of periprosthetic fractures after total knee arthroplasty; pp. 775–780. [DOI] [PubMed] [Google Scholar]
- Rahman Wael A., Vial Tomás A., Backstein David J. The Journal of Arthroplasty. 3. Vol. 31. Elsevier BV; Distal Femoral Arthroplasty for Management of Periprosthetic Supracondylar Fractures of the Femur; pp. 676–679. [DOI] [PubMed] [Google Scholar]
- Drew Jacob M., Griffin William L., Odum Susan M., Van Doren Bryce, Weston Brock T., Stryker Louis S. The Journal of Arthroplasty. 6. Vol. 31. Elsevier BV; Survivorship After Periprosthetic Femur Fracture: Factors Affecting Outcome; pp. 1283–1288. [DOI] [PubMed] [Google Scholar]