Abstract
Intro
Medical drones are an emerging technology which may facilitate rapid treatment in time-sensitive emergencies. However, drones rely on lay rescuers, whose interactions with multipurpose medical drones have not been studied, and the optimal drone design remains unclear.
Methods
We conducted 24 simulations of adult out-of-hospital cardiac arrest (OHCA) and pediatric anaphylaxis with a prototype drone equipped with spoken and visual cues and a multipurpose medical kit. 24 layperson volunteers encountered one of the two scenarios and were supported through administering treatment by a simulated 911 dispatcher. Bystander-drone interactions were evaluated via a convergent parallel mixed methods approach using surveys, video event review, and semi-structured interviews.
Results
83% (20/24) of participants voiced comfort interacting with the drone. 96% (23/24) were interested in future interaction. Participants appreciated the drone’s spoken instructions but found visual cues confusing. Participants retrieved the medical kit from the drone in a mean of 5 seconds (range 2–14) of drone contact; 79% (19/24) found this step easy or very easy. The medical kit’s layered design caused difficulty in retrieving appropriate equipment. Participants expressed a wide range of reactions to the unique drone design.
Conclusions
Laypeople can effectively and comfortably interact with a medical drone with a novel design. Feedback on design elements will result in further refinements and valuable insights for other drone designers. A multipurpose medical kit created more challenges and indicates the need for further refinement to facilitate use of the equipment.
Keywords: Emergency Medical Services, Drones, Bystander CPR, Out of Hospital Cardiac Arrest, Anaphylaxis
Introduction
Patient outcomes in prehospital emergencies rely on expedient treatment.1, 2 In life-threatening circumstances such as out-of-hospital cardiac arrest (OHCA) and anaphylaxis, patient survival declines with each minute treatment is delayed. As such, a major focus of prehospital medicine has been shortening times to medical intervention.3, 4, 5
Drones have the potential to hasten prehospital interventions by rapidly delivering medical supplies to the scene of an emergency. Prior studies demonstrate the feasibility of rotary-wing drones (RWDs) in this role, with significant time savings compared to ground ambulances.6, 7, 8, 9 With their greater range and speed, fixed-wing drones (FWDs) have theoretical advantages over RWDs, and are already in use delivering blood products to remote healthcare facilities.10
Upon arrival to an out-of-hospital emergency, medical drones rely on lay rescuers to retrieve and administer the treatments they carry. However, layperson response to medical FWDs is unknown. Furthermore, though previous studies have suggested the incorporation of aural and visual cues to assist bystanders, the optimal approach to facilitating bystander-drone interactions remains unclear.7, 10 Lastly, previous experimental drones have delivered a single medical device, limiting their utility to a single type of emergency.
The aim of this study was to evaluate the effectiveness of bystander interactions with a multipurpose medical kit delivered by a non-flying prototype of a novel, high-speed FWD. A FWD of this design could rapidly deliver treatments to a wide range of time-sensitive emergencies, more fully exploiting the rapid response capabilities offered by the FWD platform.
Methods
Participant selection, ethics, and characteristics
We screened potential participants through umhealthresearch.org, an institutional recruitment portal through which university-affiliated health researchers post studies and interested members of the public can communicate. Eligible participants had to be over the age of 18 years, able to travel to the testing site, and have the ability to ambulate independently for at least 100 meters. Individuals were excluded if they had formal medical or prehospital training, or if they had extensive knowledge of or experience with drones. A convenience sample of 24 participants based on time availability, finances, and project aims was decided on for this pilot study.. Participant demographics are in Table 1. Most participants had graduated college, and five had postgraduate degrees. Most had received CPR training in the past, although only 25% had received training on AED or epinephrine autoinjector use. No participants had ever used an AED or epinephrine autoinjector in a real-life scenario. Written consent of participants to participate was obtained by the investigative team. The institutional review board approved this study on April 1, 2022.
Table 1.
Participant demographics.
| Total (Epi & AED) | AED | Epi | |
|---|---|---|---|
| Participant Characteristics | (n = 24) | (n = 12) | (n = 12) |
| Gender | |||
| Female | 13 (54%) | 3 (25%) | 10 (83%) |
| Age, (yrs) (median) | 48 | 47 | 48 |
| Education | |||
| High School | 4 (17%) | 1 (8%) | 3 (25%) |
| Some College | 5 (21%) | 3 (25%) | 2 (17%) |
| College Graduate | 11 (46%) | 6 (50%) | 5 (42%) |
| Graduate/Professional | 4 (17%) | 2 (17%) | 2 (17%) |
| Training | |||
| Previous CPR training | 15 (63%) | 9 (75%) | 6 (50%) |
| AED training | 6 (25%) | 5 (42%) | 1 (8%) |
| Previous AED Use | 0 | 0 | 0 |
| Epi training | 6 (25%) | 5 (42%) | 1 (8%) |
| Previous Epi Use | 0 | 0 | 0 |
Drone and medical kit design
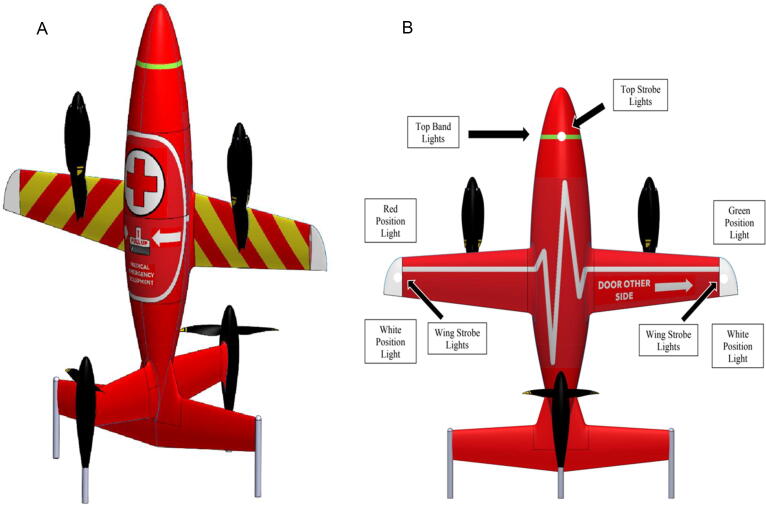
The study drone was a non-flying prototype of a FWD capable of vertical take-off and landing (VTOL) with a much higher cruising speed than most commercially-available drones currently being studied for prehospital use. The drone featured standard red and green aviation navigation lighting on the wingtips, along with extra safety lighting.. At the start of the simulated landing sequence, these lights turn red and a voice command directs bystanders to wait before approaching. After an interval of time to simulate the drone’s propellers coming to a halt, the lights turn green and another voice command provides directions on approaching the drone and retrieving the medical kit. The drone, along with descriptions of its design features, is shown in Fig. 1. The medical kit is housed within the fuselage, which features written instructions for access and removal. It contains a Samaritan Pad 350P AED training device (HeartSine, Redmond, WA), an epinephrine autoinjector training device (EPIPEN®, Mylan, Canonsburg, PA), and other medical supplies inside nested compartments (Fig. 1). Design, content, and organization of the medical kit were informed by literature review,11 stakeholder interviews, and expert opinion of authors.
Fig. 1.
Four part figure with the drone images and the two views of the medical kit. (A, B) 3D rendering of the drone model used in the simulations. Its height and wingspan are each about 1.25 meters. It features Federal Aviation Administration (FAA)-standard green and red navigation lighting on the wingtips, as well as extra safety lighting and an aural warning system. During landing, these lights flash and a voice command directs: “Landing. Stay Back.” When safe for bystander approach, the navigation lights turn white, and the voice command directs: “Medical emergency drone safe. Pull handle. Swing open door. Grab handle and remove medical kit.” (C, D) 3D rendering of the drone-portable medical kit in closed and open configurations. The kit contains personal protective equipment (gloves, surgical face mask); automated external defibrillator (AED); CPR breathing mask; epinephrine auto-injector; Intranasal (IN) naloxone; Tourniquet; Hemostatic gauze; gauze roll; albuterol inhaler; Intranasal glucagon; chewable aspirin; Pulse oximeter; Trauma shears; Razor; tape.
Simulation design
The study was conducted between May and July of 2022. Simulations were performed in an indoor space designed to resemble a residence. The mock drone landing site was situated approximately 30 meters away.
12 participants were randomized into each of the OHCA and pediatric anaphylaxis groups. Standardized scripts and simulation scenarios ensured consistency across all participants. Before each simulation, participants were introduced to the manikin (Resusci Anne or Resusci Junior, Laerdal, Stavanger, Norway), actors, and simulation environment. Participants were told that they would encounter a simulated medical emergency and call a simulated 911 dispatcher, and that a drone would deliver equipment for their use. No additional information regarding the simulated emergency, the drone, or its medical kit was provided. The scenarios are available in Appendix A.
Data collection and analysis
We video-recorded the simulations and measured time intervals for specific critical actions from the recordings. Two team members independently recorded time values. The median was used in data analysis. We then employed a convergent parallel mixed methods design in which we simultaneously collected quantitative and qualitative data on bystander-drone interactions.12 After independent analysis of each dataset, we integrated findings from the quantitative and qualitative parallel phases with specific attention to concordant and discordant elements.12, 13
The quantitative data consisted of a web-based survey (Qualtrics XM, Qualtrics, Provo, UT and Seattle, WA) completed immediately after the simulation. We evaluated participant’s views on their simulation experience and interactions with the drone and medical kit using Likert scale questions with a 5-point spectrum ranging from strongly disagree (1) to neutral (3) to strongly agree (5) (Appendix B). We utilized existing research on bystander-drone interactions to design the survey.7, 9, 14, 15 We pilot tested the instrument within the author group as well as an unrelated group with advanced training in survey research and iteratively refined the tool. We used IBM SPSS Statistics for Windows, version 28 (IBM Corp, Armonk, NY) for descriptive statistical analysis.
Qualitative data derived from semi-structured interviews focused on participant reactions (Appendix C) conducted immediately after the simulation by one of two members of the author team (NH, EM). The interview script was piloted and refined within the author group. Interviews were audio-recorded using Zoom™ (Zoom Video Communications Inc, San Jose, CA), and commercially transcribed (Rev, San Francisco, CA). Descriptive coding16 was conducted using Dedoose (Dedoose version 9.0.54, Los Angeles, CA: Socio Cultural Research Consultants, LLC.www.dedoose.com) and proceeded by consensus between the two coders (EM, LRH). Key themes were iteratively developed and refined through discussion with the research team. Saturation, as defined by the absence of new codes and themes, was achieved after coding half the transcripts with no significant new codes or themes identified in the full group of 24 transcripts.17
Results
Quantitative data
Participants noted a range of comfort with drones pre-simulation. Post-simulation, 20/24 (83%) indicated positive comfort levels with drones. Four participants (17%) felt somewhat or very uncomfortable with drones after the experience, including one individual whose comfort level increased during the simulations, one whose comfort level was unchanged, and two whose comfort level decreased. Most (87.5%, 21/24) felt somewhat or extremely safe around the drone, and almost all (96%, 23/24) were somewhat or extremely interested in interacting with a medical drone in the future. Participants found it somewhat or extremely easy to locate the drone (96%, 23/24), locate the medical kit on the drone (79%, 19/24), remove the medical kit from the drone (92%, 22/24), carry the medical kit back to the simulated patient (96%, 23/24), and locate the AED or epinephrine autoinjector in the medical kit (79%, 18/24). Participants did not report difficulty using the AED or autoinjector, with 83% (20/24) finding this somewhat or extremely easy (Appendix B).
Video review data
Participants retrieved the medical kit within a mean of five seconds (range 2–14) of drone contact. Participants in the OHCA group identified and turned on the AED within a mean of 21 seconds (range 15–36) after re-entering the room. Participants in the anaphylaxis group took slightly longer: a mean of 29 seconds (range 20–47) elapsed between participants re-entering the room and retrieving the autoinjector from the kit, of which a mean of 16 seconds (range 8–24) was spent searching for the autoinjector within the kit.
Qualitative Data
Appreciation and enthusiasm
Participants consistently expressed enthusiasm for the drone as a rapid response mechanism. One participant drew on a personal experience with OHCA in which “we called, and nobody came..so this would’ve been perfect.” (participant #3). Another participant indicated a hope that similar drones could be widely deployed in the near future. Overall, most participants expressed interest in future interactions with medical drones.
Initial drone design impressions and divergent expectations
Most participants were surprised by the drone’s appearance, and by the location of the medical kit. Participants expected a small RWD with medical equipment held below it or dropped to the ground. One participant stated: “The structure of the drone wasn't [what I was expecting] […] This was more like a little mini airplane” (#22). Some participants used terminology that seemed to imply a hostile or threatening appearance “like a missile” (#17) when describing the drone. However, these divergent expectations did not limit participants’ ability to approach the drone and retrieve the medical kit.
Participant comfort and drone safety
Participants expressed feelings of safety around the drone. One participant noted that the drone was “calming because…you weren’t just waiting for an ambulance…you were actively doing something to help the person” (#5).
Feedback regarding medical drone design
Participants provided detailed feedback regarding the design of the drone and medical kit. In general, the drone design was perceived positively. Many participants noted the importance of the drone’s voice commands. The volume and pace of the commands were adequate, as noted by a participant who stated “I liked the loud commands talking slowly” (#10). However, the voice commands sometimes competed with dispatcher instruction; multiple participants noted not fully registering the drone’s voice commands or having difficulty focusing on what the dispatcher was saying while the drone was also speaking. The content of the dispatcher’s instructions, as well as their interaction with the drone’s voice commands, are investigated in greater detail in a companion study by the same author group.
Participants found some design elements disconcerting or confusing. In particular, the drone’s landing and “cool-down” process was longer than many participants expected. One participant stated: “the longest part was the waiting when it kept saying it was landing… And I feel like it was in an emergency situation” (#19). In addition, the drone’s red and green safety and navigation lights caused some confusion. One participant stated that “I was confused […] because there are so many lights” (#3).
Feedback regarding multimodal medical kit design
Many participants noted that a strength of the kit was its compact design and ease of handling. Though the kit’s location within the drone fuselage surprised several participants, it was easily identifiable as medical equipment. However, the kit’s multi-layered configuration was consistently critiqued. Participants were frustrated at the need to search for components, noting that “there was a lot of stuff in it, and it was confusing…” (#7) and “it was hard to see the [epinephrine autoinjector] through that top layer” (#5). During video review, several participants resorted to dumping out the contents of the medical kit to locate items.
Discussion
Many prior works have examined the willingness of untrained bystanders to intervene in medical emergencies. This research has shown that bystanders are often hesitant to provide interventions such as dispatcher-assisted CPR because they fear for their personal safety, doubt their ability to intervene effectively, or are overwhelmed in the face of heavy cognitive load.18, 19, 20, 21 Our work augments this existing literature by showing that bystanders with no relevant expertise are able to overcome these barriers even while interacting with an unfamiliar piece of medical technology. Our simulations also strongly demonstrated the importance of anticipating and limiting the cognitive load placed on lay rescuers.
Bystander-drone interactions
The speed with which participants began interacting with the drone upon encountering it illustrates the feelings of comfort and safety voiced throughout the semi-structured interviews. Participants also expressed appreciation for the drone’s aural and visual cues; however, these same stimuli worsened cognitive overload in a stressful situation––a phenomenon which may have contributed to the minority of subjects who still felt uncomfortable interacting with drones after the simulation. Aural cues should be further developed in tandem with standardized dispatcher scripts, as the overlap of these spoken instructions was likely responsible for some participants ignoring drone-issued safety warnings. Similarly, instructional lighting should be clearly and obviously differentiated from Federal Aviation Administration-required navigation lights, such as by disabling navigation lights upon landing.
Participants’ relatively uniform expectations surrounding the drone’s appearance and the location of the medical kit should also be incorporated into future medical drone designs. Though participants were quick to remove the medical kit from the drone and consistently stated that this step was easy, future designs which adhere more closely to participants’ expectations by locating the medical kit beneath the drone or dropping it while hovering may simplify bystander-drone interactions. Widespread implementation of a similar drone design may require an educational campaign on deployment to promote familiarity and set expectations.
Bystander-medical kit interactions
Participants’ success and speed in identifying, retrieving, and using the AED and epinephrine autoinjector, as well as their stated positive feelings regarding the medical kit, demonstrate the feasibility of a multimodal drone-delivered medical kit utilized by lay rescuers. Though prior studies have focused primarily on the delivery of a single intervention by drone, our findings indicate that one drone may be equipped to respond to a variety of time-sensitive emergencies, albeit with significant refinement as suggested by the results of this study.
Though the nested, multi-layered design of the medical kit allowed a large number of items to be carried inside the drone’s payload bay, it likely worsened cognitive overload. When retrieving the epinephrine autoinjector, participants were confronted with a complex container system and numerous other items. This problem may be mitigated by simplifying the medical kit into a single layer of equipment that is immediately and entirely visible upon opening, as well as by introducing non-redundant color labeling on all items. The size and composition of the kit should also be refined in order to retain flexibility while limiting cognitive overload. Further study is needed to identify which specific interventions warrant inclusion in a drone-delivered medical kit, as well as the optimal design and layout of such a kit.
Concordance and discordance of results
The themes noted in the post-simulation surveys and semi-structured interviews were largely concordant, particularly with respect to participants’ comfort and safety around the drone and indicated ease of interaction. However, data regarding medical kit interactions, the use of the AED, and the use of epinephrine autoinjector reflected areas of discordance. This finding likely reflects greater ambivalence among participants regarding the medical kit compared to the drone itself. In addition, survey data may have failed to capture differences between the OHCA and anaphylaxis group, as the survey instrument lacked questions specific to the type of simulation. Future simulations involving lay rescuers should seek to better understand which specific emergencies cause the greatest stress, confusion, and/or cognitive overload among bystanders, and how these challenges can best be overcome through a combination of dispatcher instructions, automated safety and instructional cues, and medical kit design.
Impact on time-sensitive prehospital care
Bystanders have previously been shown to be capable of interacting with RWD delivered AEDs and appreciative of a drone delivery system.6, 7, 10, 11, 14 This study demonstrated similarly positive bystander experiences with a novel FWD. Given its ability to rapidly respond to a variety of time-sensitive prehospital emergencies, a prehospital system employing a high-speed, long range FWD and multimodal medical kit has may be the ideal prehospital drone delivery system. The possibility of leveraging FWDs’ much faster flight speeds to create a drone network that can arrive on scene within 5 minutes of a 911 call is tantalizing, but will obviously require future computer modeling to optimize high-speed FWD numbers and locations. This also depends on the take-off and landing times of VTOL FWDs, which were not addressed in this study given the non-flying prototype. A FWD that can hover in VTOL configuration and line-drop a multipurpose medical kit is intriguing given the relative safety benefits of hovering over landing, and is worth future development consideration. The success of bystander-drone interactions demonstrated in our simulations is a crucial step in realizing the potential of this emerging technology. Further research is needed regarding drone and medical kit design, particularly with respect to reducing bystander cognitive load while preserving the versatility of the drone and medical kit. Lastly, clinical trials are needed to establish the efficacy and impact of drone-delivered interventions on prehospital patient outcomes. The faster response times and expanded use cases of this VTOL FWD system may improve the financial feasibility of drone-delivered prehospital medical interventions; however, the development of clinical trials in this space is currently limited by aviation regulations, insurance uncertainty, logistical concerns, and financial barriers.
Limitations
The study’s small sample size reduces its generalizability. The simulation design itself possesses several noteworthy limitations. Because the drone was never in flight, participants did not have to interact with the drone during landing or while its propellers were rotating. This would likely have introduced additional safety hazards, noise, and cognitive load. Although we tried to create a high-fidelity environment, the simulations were performed in a controlled indoor situation without a live patient in distress, potentially compromising suspension of disbelief and eliminating unpredictable environmental factors. Participants were highly educated relative to the U.S. population and were not equally distributed by gender across the two scenarios; in addition, since saturation was reached within 12 participants, including a total of 24 subjects was potentially an unnecessary use of research time. Lastly, bystander interaction with other capabilities of the multipurpose medical kit beyond the AED and epinephrine autoinjector were not explored. Future studies should involve higher-fidelity simulations, carried out in a wider variety of environments and with a greater diversity of recruitment methods, participant educational backgrounds, and simulated emergencies.
Conclusion
In 24 simulations of OHCA and anaphylaxis, we found that bystanders with no medical training or experience with drones were able to effectively interact with a fixed-wing medical drone containing a multipurpose medical kit. Participants were generally enthusiastic about more widespread introduction of medical drones, and voiced interest in interacting with medical drones in the future. Participants also provided valuable feedback on the design of the drone and medical kit which should be incorporated into future iterations.
CRediT authorship contribution statement
Thomas Leith: Writing – review & editing, Writing – original draft, Validation, Methodology, Investigation, Data curation. Jason A. Correll: Writing – review & editing, Investigation. Emma E. Davidson: Writing – review & editing, Investigation. Adam L. Gottula: Writing – review & editing, Supervision, Methodology, Investigation, Conceptualization. Noor K. Majhail: Writing – review & editing, Investigation. Emily J. Mathias: Writing – review & editing, Validation, Supervision, Methodology. James Pribble: Writing – review & editing, Validation, Supervision, Methodology, Formal analysis. Nathan B. Roberts: Writing – review & editing, Visualization, Validation, Supervision, Methodology. Isabella G. Scott: Writing – review & editing, Investigation. James A. Cranford: Writing – review & editing, Validation, Supervision, Methodology, Formal analysis. Laura R. Hopson: Writing – review & editing, Validation, Supervision, Project administration, Methodology, Investigation, Data curation, Conceptualization. Nathaniel Hunt: Writing – review & editing, Validation, Supervision, Methodology, Investigation. Christine M. Brent: Writing – review & editing, Validation, Supervision, Project administration, Methodology, Investigation, Funding acquisition, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: ‘Dr. Brent, Dr. Hopson, Dr. Pribble, Dr. Mathias and Dr. Hunt report funding support from Toyota Motors North America Research and Development for this study. Ms. Davidson, Ms. Majhail and Ms. Scott report employment, during one or more phases of the study, with Huron Valley Ambulance of Emergent Health Partners, a licensed transporting advanced life support agency (ALS) that serves as a regional provider of BLS/ALS medical transport and 9–1-1 dispatched emergency response in southern Michigan. Dr. Brent and Dr. Hunt report a leadership role as co-deputy medical director for the Washtenaw/Livingston Medical Control Authority, a regional EMS oversight body. All other authors report no relevant interests.’.
Acknowledgements
The study team acknowledges Toyota Motors North America Research and Development for the simulation recording technology. The study team acknowledges Tyler Nix for assistance in the background research and literature review.
REDCap electronic data capture and participant registry tools (i.e., UMHealthResearch) used in the study were.
hosted at the Michigan Institution for Clinical & Health Research (grant support (CTSA: UL1TR002240)).
Author contributions
Christine M. Brent (CMB), Laura Hopson (LRH), Nathaniel Hunt (NH), Emily Mathias (EM) and James Pribble (JP) conceived of the study and collaboratively developed the study design. CMB, NH provided budget oversight throughout the project. CMB, Thomas Leith (TL), Nathan Roberts (NR), Emily Ager (EG) conducted background literature review. CMB managed regulatory approval of the study. CMB, LRH, EM, JP, Jason A. Correll (JAC) developed data collection and analysis protocols and associated documents. CMB developed and managed the electronic data capture tool and screening instruments. CMB, NH trained and coordinated project staff. Noor K. Majhail (NKM), Isabella G. Scott (IGS), Emma E. Davidson (EED), JAC, CMB, NH, TL conducted participant recruitment. NKM, IGS, JM, NH, EED, EM, JP, LRH, TL facilitated participant consenting and debriefing, simulation scenarios, automated data capture and manual abstraction. NH, LRH, EM, JP, JAC conducted data analysis. TL, EED, NH, CMB and JAC drafted the initial manuscript and all listed authors provided meaningful review on subsequent manuscript drafts in accordance with ICMJE guidelines.
Funding
This work was supported by Toyota Motor North America Research and Development. The study sponsors were not involved in the study design, collection of data, analysis, and interpretation of data, or in the writing or submission of the manuscript.
Footnotes
Supplementary material to this article can be found online at https://doi.org/10.1016/j.resplu.2024.100633.
Appendix A. Supplementary material
The following are the Supplementary material to this article:
References
- 1.Mell H.K., et al. Emergency medical services response times in rural, suburban, and urban areas. JAMA Surg. 2017;152:983–984. doi: 10.1001/jamasurg.2017.2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banerjee P., et al. Every one-minute delay in EMS on-scene resuscitation after out-of-hospital pediatric cardiac arrest lowers ROSC by 5. Resusc Plus. 2021;5 doi: 10.1016/j.resplu.2020.100062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cui E.R., et al. Disparities in emergency medical services time intervals for patients with suspected acute coronary syndrome: findings from the North Carolina prehospital medical information system. J Am Heart Assoc. 2021;10:e019305. doi: 10.1161/JAHA.120.019305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cui E.R., et al. Emergency medical services time intervals for acute chest pain in the United States, 2015-2016. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2020;24:557–565. doi: 10.1080/10903127.2019.1676346. [DOI] [PubMed] [Google Scholar]
- 5.Mueller L.R., et al. National characteristics of emergency medical services in frontier and remote areas. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2016;20:191–199. doi: 10.3109/10903127.2015.1086846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rees N., Howitt J., Breyley N., Geoghegan P., Powel C. A simulation study of drone delivery of Automated External Defibrillator (AED) in Out of Hospital Cardiac Arrest (OHCA) in the UK. PloS One. 2021;16:e0259555. doi: 10.1371/journal.pone.0259555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zegre-Hemsey J.K., et al. A feasibility study to assess delivery of automated external defibrillators via drones in simulated cardiac arrest-users’ experiences and the human-drone interaction. Circulation. 2019;140 doi: 10.1016/j.resuscitation.2020.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drennan I., et al. AED on the fly: A drone delivery feasibility study for rural and remote out-of-hospital cardiac arrest. Can J Emerg Med. 2020;22:S13–S14. [Google Scholar]
- 9.Ornato J.P., et al. Feasibility of bystander-administered naloxone delivered by drone to opioid overdose victims. Am J Emerg Med. 2020;38:1787–1791. doi: 10.1016/j.ajem.2020.05.103. [DOI] [PubMed] [Google Scholar]
- 10.Stephan F., Reinsperger N., Grünthal M., Paulicke D., Jahn P. Human drone interaction in delivery of medical supplies: A scoping review of experimental studies. PloS One. 2022;17:e0267664. doi: 10.1371/journal.pone.0267664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roberts N.B., et al. Current summary of the evidence in drone-based emergency medical services care. Resusc Plus. 2023;13 doi: 10.1016/j.resplu.2022.100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Creswell J.W., Plano Clark V.L. SAGE; 2018. Designing and conducting mixed methods research. [Google Scholar]
- 13.Onwuegbuzie AJ. Linking research questions to mixed methods data analysis procedures. vol. 11, 474–498.
- 14.Sanfridsson J., et al. Drone delivery of an automated external defibrillator – a mixed method simulation study of bystander experience. Scand J Trauma Resusc Emerg Med. 2019;27:40. doi: 10.1186/s13049-019-0622-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glei D.A., Goldman N., Ryff C.D., Weinstein M. Can we determine whether physical limitations are more prevalent in the US than in countries with comparable life expectancy? SSM – Popul Health. 2017;3:808–813. doi: 10.1016/j.ssmph.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 17.Saunders B., et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893–1907. doi: 10.1007/s11135-017-0574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghanbari S., Haghani F., Barekatain M., Jamali A. A systematized review of cognitive load theory in health sciences education and a perspective from cognitive neuroscience. J Educ Health Promot. 2020;9:176. doi: 10.4103/jehp.jehp_643_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greenberg K., Zheng R. Cognitive load theory and its measurement: a study of secondary tasks in relation to working memory. J Cogn Psychol. 2022;34:497–515. [Google Scholar]
- 20.Riou M., et al. Caller resistance to perform cardio-pulmonary resuscitation in emergency calls for cardiac arrest. Soc Sci Med 1982. 2020;256 doi: 10.1016/j.socscimed.2020.113045. [DOI] [PubMed] [Google Scholar]
- 21.Shida H., et al. Laypersons’ psychological barriers against rescue actions in emergency situations – A questionnaire survey. Circ J Off J Jpn Circ Soc. 2022;86:679–686. doi: 10.1253/circj.CJ-21-0341. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.