To the Editor,
Defibrillation represents a crucial part of cardiopulmonary resuscitation and increases neurological outcome and overall survival if a shockable rhythm is detected.1, 2, 3 Correct and rapid ECG-interpretation is vital to perform correct treatment and to avoid prolonged hands-off times during rhythm analysis.4 Current European Resuscitation Guidelines underline the importance of education regarding BLS and ALS.5 As of now, limited data exist that elucidate the acquisition and development of emergency competencies during medical studies.
Therefore, this study investigates the manual defibrillation skills of an almost complete cohort of medical students at the beginning of clinical training (5th semester) by measuring correctness-of-decision (COD) and time-to-decision (TTD) regarding defibrillation of 7 typical emergency ECGs.
This study was ethically approved by the Ethics Committee of the University of Cologne (No: 23-1007_1). 202 medical students were individually asked to decide whether defibrillation is indicated regarding the following ECGs: asystole (ASY), fine ventricular fibrillation (fVF), pulseless ventricular tachycardia (pVT), normofrequent sinus rhythm (nSR), pulseless electrical activity (PEA), coarse ventricular fibrillation (cVF), sinus bradycardia (SB). Since it would be practically and ethically unfeasible to give defibrillation decisions in the hands of students, we simulated this scenario using TruMonitor (Laerdal Medical GmbH, Puchheim, Germany) software running on an iPad (Apple, Cupertino, CA, USA) in a randomized order. Primary endpoints were correctness of decision and time to decision. Group comparisons (gender, prior medical education, experience in resuscitation and defibrillation) were performed by Odds Ratios (OR), means and two-tailed-t-test. According to current guidelines, fine and coarse VF and pVT were defined as shockable rhythms, nSR, SB, AS and PEA were defined as non-shockable rhythms.
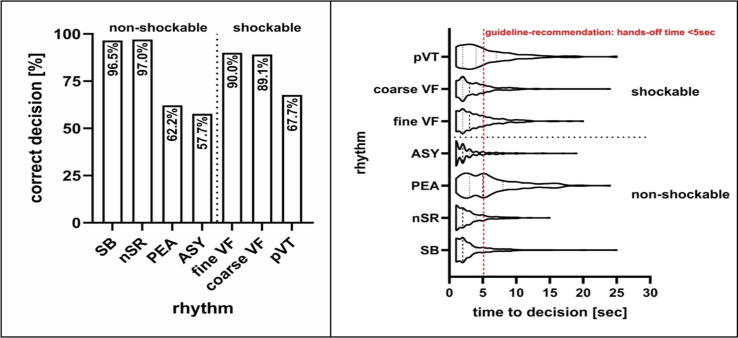
In February 2023 201 out of 202 students participated voluntarily (99,5%) and were presented individually with the 7 ECGs during objective structured clinical examination (OSCE) for a maximum of 25 sec. each. For shockable rhythms, mean correctness-of-decision (%) and time-to-decision (seconds) were (Fig. 1): pVT [68%|5.4s]; fVF [90%|4.1s]; cVF [89%|3.7s]. For non-shockable rhythms, mean COD (%) and TTD (seconds) were: ASY [58%|3.0s], PEA [62%|6.2s], nSR [97%|2.9s], SB: [97%|3.4s]. No gender-related differences were detected. Students with prior medical training (nurse or paramedic) had a higher probability of detecting asystole correctly (OR 2.93, 95%-CI 1.58–5.45). Students who had prior experience in resuscitation or defibrillation, had higher odds of detecting PEA and asystole correctly (PEA: 2.16 [1.04–4.47] and 3.37 [1.23–9.27], respectively, ASY: 6.09 [2.57–14.42] and 7.90 [2.30–27.08], respectively).
Fig. 1.
Correctness-of-decision and time-to-decision for each rhythm presented to the participants. The abbreviations utilized are delineated within the text. In the violin plot, the thickness of the respective area represents the distribution of values, the dotted lines represent the 25th and 75th percentile, the dashed line represents the median.
Medical students at this stage of training showed inconsistent treatment decisions for emergency ECGs. Particularly, treatment decisions for pVT, ASY and PEA were identified as inadequate. We therefore recommend that medical students at the beginning of clinical training (5th semester) use Automated External Defibrillators (AEDs), even if this might result in longer hands-off times for rhythm analysis.6 Our results indicate that acquiring proficiency in manual defibrillation is not a straightforward process and necessitates comprehensive education and specific training in ALS.7 In alignment with current ERC-Guidelines, we want to highlight the importance of (curricular) educational programs that integrate specialized components of ALS using high-fidelity and in-situ simulations.5, 8, 9, 10
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: [Bernd W. Böttiger is treasurer of the European Resuscitation Council (ERC), Founder of the ERC Research NET, Chairman of the German Resuscitation Council (GRC), Member of the „Advanced Life Support (ALS) Task Force of the International Liaison Committee on Resuscitation (ILCOR), Member of the Executive Committee of the German Interdisciplinary Association for Intensive Care and Emergency Medicine (DIVI), Founder of the “Deutsche Stiftung Wiederbelebung”, Federal Medical Advisor of the German Red Cross (DRK), Member of the Advisory Board of the “Deutsche Herzstiftung”, Co-Editor of “Resuscitation”, Editor of the Journal “Notfall + Rettungsmedizin”, Co-Editor of the Brazilian Journal of Anesthesiology. He received fees for lectures from the following companies: Forum für medizinische Fortbildung (FomF), Baxalta Deutschland GmbH, ZOLL Medical Deutschland GmbH, C.R. Bard GmbH, GS Elektromedizinische Geräte G. Stemple GmbH, Novartis Pharma GmbH, Philips GmbH Market DACH, Bioscience Valuation BSV GmbH. Niels-Benjamin Adams reports no competing interests regarding this study. Megan Mittag reports no competing interests regarding this study. Christoph Stosch reports no competing interests regarding this study. Sabine Bornemann reports no competing interests regarding this study. Jana Adams reports no competing interests regarding this study. Wolfgang A. Wetsch reports no competing interests regarding this study. Hendrik Drinhaus reports no competing interests regarding this study.].
References
- 1.Nakashima T., Noguchi T., Tahara Y., et al. Public-access defibrillation and neurological outcomes in patients with out-of-hospital cardiac arrest in Japan: a population-based cohort study. Lancet (London, England) 2019;394:2255–2262. doi: 10.1016/S0140-6736(19)32488-2. [DOI] [PubMed] [Google Scholar]
- 2.Pollack R.A., Brown S.P., Rea T., et al. Impact of bystander automated external defibrillator use on survival and functional outcomes in shockable observed public cardiac arrests. Circulation. 2018;137:2104–2113. doi: 10.1161/CIRCULATIONAHA.117.030700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gräsner J.T., Wnent J., Herlitz J., et al. Survival after out-of-hospital cardiac arrest in Europe - Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 4.Soar J., Böttiger B.W., Carli P., et al. European Resuscitation Council Guidelines 2021: adult advanced life support. Resuscitation. 2021;161:115–151. doi: 10.1016/j.resuscitation.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 5.Greif R., Lockey A., Breckwoldt J., et al. European Resuscitation Council Guidelines 2021: education for resuscitation. Resuscitation. 2021;161:388–407. doi: 10.1016/j.resuscitation.2021.02.016. [DOI] [PubMed] [Google Scholar]
- 6.Krammel M., Eichelter J., Gatterer C., et al. Differences in automated external defibrillator types in out-of-hospital cardiac arrest treated by police first responders. J Cardiovasc Dev Dis. 2023;10:196. doi: 10.3390/jcdd10050196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Derkenne C., Jost D., Roquet F., et al. Assessment of emergency physicians’ performance in identifying shockable rhythm in out-of-hospital cardiac arrest: an observational simulation study. Emerg Med J. 2022:1–6. doi: 10.1136/emermed-2021-211417. [DOI] [PubMed] [Google Scholar]
- 8.Chan P.S., Greif R., Anderson T., et al. Ten steps toward improving in-hospital cardiac arrest quality of Care and outcomes. Resuscitation. 2023;193 doi: 10.1016/j.resuscitation.2023.109996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stærk M., Lauridsen K.G., Støtt C.T., Riis D.N., Løfgren B., Krogh K. Inhospital cardiac arrest - the crucial first 5 min: a simulation study. Adv Simul (London, England) 2022;7:29. doi: 10.1186/s41077-022-00225-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stærk M., Lauridsen K.G., Johnsen J., Løfgren B., Krogh K. In-situ simulations to detect patient safety threats during in-hospital cardiac arrest. Resusc Plus. 2023;14 doi: 10.1016/J.RESPLU.2023.100410. [DOI] [PMC free article] [PubMed] [Google Scholar]