Abstract
Background and Aims:
Although most large nonpedunculated colorectal lesions can be safely and efficaciously removed using endoscopic mucosal resection (EMR), the use of colectomy for benign colorectal lesions appears to be increasing. The reason(s) is unclear. We aimed to determine the utilization and the adverse events of EMR in the United States.
Methods:
We used Optum’s de-identified Clinformatics Data Mart Database (2003–2016), a database from a large national insurance provider, to identify all colonoscopies performed with either EMR or simple polypectomy on adult patients from January 1, 2011, through December 31, 2015. We measured time trends, regional variation, and adverse event rates. We assessed risk factors for adverse events using multivariate logistic regression.
Results:
EMR is increasingly used in the United States, from 1.62% of all colonoscopies in 2011 to 2.48% of colonoscopies in 2015 (p<0.001). There were, however, significant regional differences in the utilization of EMRs, from 2.4% of colonoscopies in the western United States to 2.0% of colonoscopies in the southern United States. From 2011 to 2015, we found stable rates of perforation, gastrointestinal bleeding (GIB), infections, and cardiac adverse events, and decreasing rates of admissions after EMR. In our multivariate model, EMR was an independent risk factor for adverse events, albeit the rates of adverse events were low (1.35% GIB, 0.22% perforation).
Conclusion:
EMR is increasingly used in the United States, although there is significant regional variation. The rates of adverse events after EMR and polypectomies were low and stable, confirming the continuing safety of EMR procedures. A better understanding of the regional barriers and facilitators may improve the use of EMR as the standard management for benign colorectal lesions throughout the United States.
Keywords: Colorectal lesions, resection, colonoscopy, Endoscopic Mucosal Resection, Polypectomy, Outcomes
Introduction
Up to 3% of the 14 million patients undergoing annual colonoscopy will have a polyp ≥20 millimeter in size that will require removal using more sophisticated resection techniques, such as endoscopic mucosal resection (EMR)1. When used according to its indications, EMR provides safe and curative resection for large nonpedunculated colorectal lesions and obviates the higher morbidity, mortality, and cost associated with surgical resection2–4. Surgical resection of benign colon lesions, however, continues to be a common and increasing practice5, even though the vast majority of lesions referred for surgical resection are amenable to endoscopic resection.
Outcomes data show that endoscopic resection is associated with low morbidity and mortality. In a recent meta-analysis of 50 studies, endoscopic resection of large (>20 mm), complex colorectal lesions was associated with a 6.5% risk of bleeding, 1.5% risk of perforation, and 0.08% risk of death.6 In contrast, colectomies for benign lesions have been associated with a 14% risk of a major adverse event and a 0.7% risk of 30-day mortality.7 Recurrence after endoscopic resection was found in 13.8% of patients, but over 90% could be managed endoscopically.6 Endoscopic resection is also cost-effective compared with surgical resection.8,9 Despite these facts, surgical resection of benign colon lesions is rising in the United States,5 even though many lesions referred for surgical resection are, in fact, amenable to endoscopic resection.10,11
One potential way to gain insights into why EMR is not sufficiently used in the United States is to study its utilization and adverse events. Therefore, in this study, we aimed to quantify and examine the trends in the use of EMR and its outcomes for large benign nonpedunculated colorectal lesions in the United States.
Methods:
We used Optum©’s de-identified Clinformatics Data Mart Database (2003–2016), a database from a large national insurance provider, to identify a cohort of patients who underwent colonoscopy with polypectomy. This dataset has linked patient records containing demographics, inpatient, outpatient, and provider details of 12 to 14 million individuals annually enrolled in a large commercial insurance plan and Medicare Advantage.
Cohort Definitions
We identified all outpatient colonoscopies performed between January 1, 2011, and December 31, 2015, based on the Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS) and International Classification of Diseases codes, 9th and 10th revisions (ICD9, ICD10) codes. We distinguished polypectomies from other colonoscopies using CPT codes 44389, 44392, 44394, 44403, 44404, 45380, 45381, 45384, 45385 or 45390 with a simultaneous ICD9 or ICD10 code for benign colorectal lesion (211.3, 211.4, K63.5, D12.0-D12.8). We defined EMR cases as those with snare polypectomy (CPT codes 44394, 45385) and injection (CPT code 44404, 45381), or those labeled as EMR (CPT codes 44403, 45390). To ensure an EMR was performed for benign lesions, we excluded patients who developed colorectal cancer within 1 year of polypectomy (Supplementary Table 1A). All other polypectomies were classified as simple polypectomy.
Outcomes Definitions
Our primary outcome of interest was the volume of EMR use over time. Our secondary outcomes of interest were regional variation in EMR use, rates of gastrointestinal bleeding (GIB), perforation, cardiovascular adverse events (myocardial infarction [MI], cerebrovascular accident [CVA], and arrhythmia), infectious adverse events (sepsis and pneumonia), and admissions for any indication. We calculated the proportions of EMR use over time compared with all colonoscopies performed during the corresponding time period and the proportions of EMRs performed by region compared with all colonoscopies performed in that corresponding region. We used provider state to determine regional variation with regions (Northeast, Midwest, South, and West) as defined by the U.S. census.
We defined adverse events as an inpatient encounter for any of the indications (Supplementary Table 1A and B) listed above within 30 days of the index procedure.12
Statistical Analysis
We summarized descriptive statistics as medians and interquartile range (IQR) for continuous variables, and frequency, rates, and proportions for categorical variables. We tested statistical significance with the Chi-squared test for categorical variables and the Wilcoxon signed-rank test for continuous variables. We measured time-trends using linear regression to calculate the rate of change and P for trend. We assessed the risk of adverse outcomes using multivariate logistic regression. Our multivariate model was adjusted for patient age, gender, race, Charlson Comorbidity Index (CCI)13, provider state, procedure type (EMR versus simple polypectomy), and the year of the procedure.
Sensitivity Analysis
We assessed the risk factors for adverse events with EMR only and simple polypectomy only subgroups to determine the differential effect of EMR procedure as a risk factor compared with other covariates in the multivariate model.
Results
Trends and Regional Variation
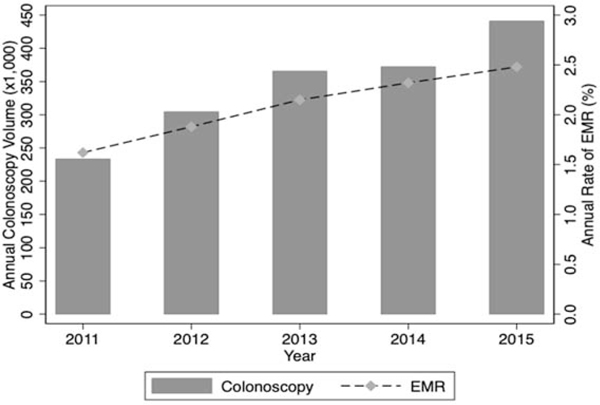
We identified 1,716,374 colonoscopies performed between January 1, 2011 to December 31, 2015, of which 709,513 (41.3%) included polypectomies and 36,979 (2.2%) included EMRs (Supplementary Figure 1). The frequency of colonoscopies steadily increased from 233,433 in 2011 to 440,981 in 2015 (p=0.004) (Figure 1). The frequency of EMRs also increased from 3,786 in 2011 to 10,937 in 2016. The increase was, however, proportionally more rapid, from 1.62% (95% CI, 1.57–1.67 ) to 2.48% (95% CI, 2.43–2.53) of all colonoscopies, respectively (p<0.001).
Figure 1.
Frequency of colonoscopies and proportions of EMR performed, by year. Frequency of colonoscopies has increased from 233,443 in 2011 to 440,981 in 2016 (p=0.004). Proportion of EMR have increased from 1.62% of colonoscopies in 2011 to 2.48% of colonoscopies in 2015, p<0.001.
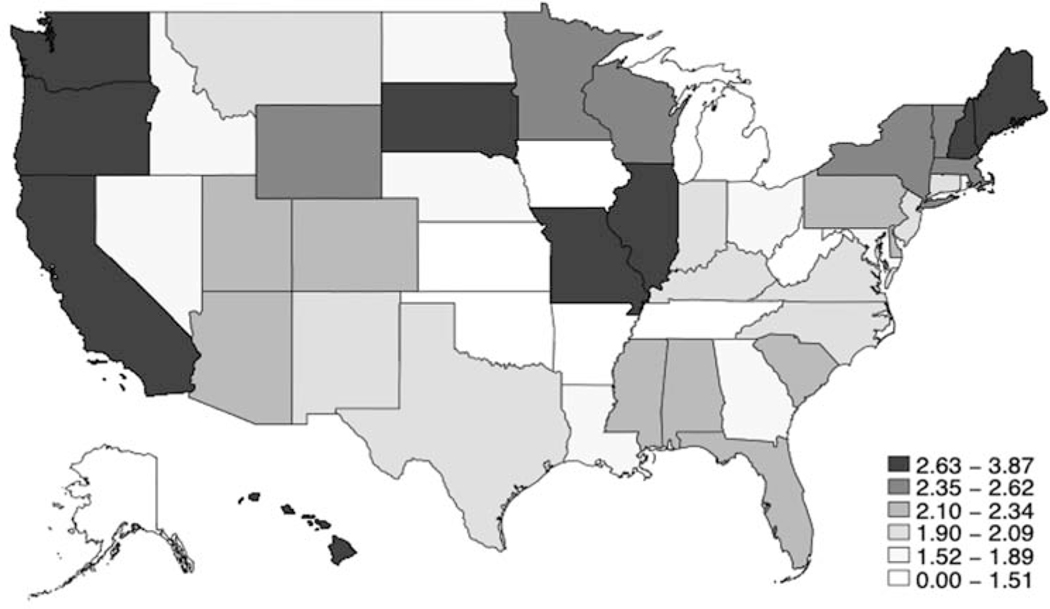
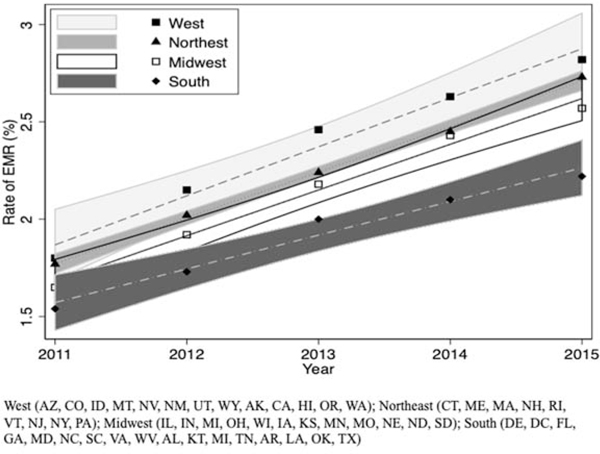
We found regional variation in EMR use in the United States. The Western region had the highest proportion of EMRs performed (2.4%; 95% CI, 2.4%−2.5%), followed by the Northeastern and Midwestern regions (2.3%; 95% CI, 2.3%−2.4% and 2.2%; 95% CI, 2.2%−2.3% respectively), and the Southern region (2.0%; 95% CI, 1.9–2.0%), p < 0.001. (Figure 2). Over time, the rates of use of EMR increased, but the regional variation remained, with the highest and lowest proportions of EMRs performed in the Western and Southern regions, respectively (Figure 3). The Western region had the highest rate of increase (0.25%; 95% CI, 0.18–0.33 per 100 colonoscopies) compared with the Southern region (0.17 %; 95% CI, 0.11–0.23 per 100 colonoscopies).
Figure 2.
Proportion of EMR performed per 100 colonoscopies, by state.
Figure 3.
Time trends of EMR use stratified by region1. Rate of increase with 95% CI differ by region (p<0.001).
EMR outcomes:
Table 1 summarizes the demographics of patients in our outcomes analysis. Patients who underwent EMR were older than patients who underwent simple polypectomy (median 65 years, IQR 56–71 years vs 63 years, IQR 54–69 years, p<0.001, respectively). Patients who underwent EMR were also more likely to be white (77.2% vs 75.4%, p< 0.001) and have CCI ≤2 (96.8% vs 95.4%, p< 0.001). There was no significant difference in gender between the two groups. Median patient age increased from 61 years (IQR 53–68 years) in 2011 to 63 years (IQR 55–70 years) in 2015 (p<0.001) and the proportion of patients with a CCI ≥ 2 increased from 1.86% to 4.04% (p<0.001).
Table 1.
Demographics of patients included in our outcomes analysis, stratified by EMR and simple polypectomy.
| EMR N=36,979 |
Simple polypectomy N=709,513 |
P value | |
|---|---|---|---|
| Age (years), median (IQR) | 65 (56–71) | 63 (54–69) | <0.001 |
| Gender | 0.43 | ||
| Male | 19,445 (52.6%) | 372603 (52.3%) | |
| Female | 17,534 (47.4%) | 336,879 (47.5%) | |
| Race | <0.001 | ||
| White | 27,130 (77.2%) | 510,432 (75.4%) | |
| Asian | 1032 (4.3%) | 23263 (95.8%) | |
| Black | 3434 (9.8%) | 685542 (10.1%) | |
| Hispanic | 2357 (6.7%) | 51592 (7.6%) | |
| Unknown | 1202 (3.4%) | 22,976 (3.4%) | |
| CCI | <0.001 | ||
| 0 | 17,322 (46.8%) | 361,626 (51.0%) | |
| 1 | 17,966 (48.6%) | 325,083 (45.8%) | |
| >=2 | 1,691 (4.6%) | 22,804 (3.2%) | |
| Median (IQR) | 1 (0–2) | 0 (0–2) | <0.001 |
CCI, Charlson comorbidity index; EMR, endoscopic mucosal resection IQR, interquartile range;
Time Variation in adverse event rates
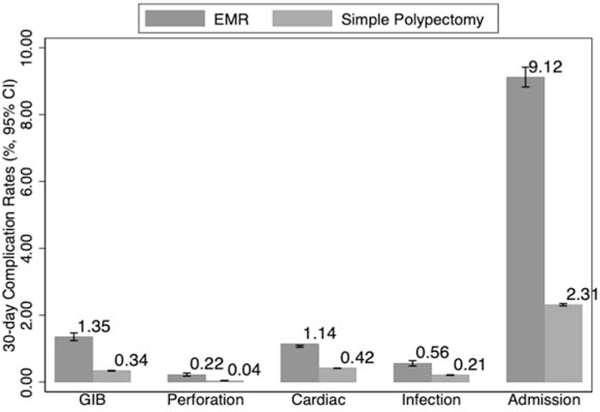
The adverse event rates after EMR were higher than those after simple polypectomy (p<0.001) (Figure 4). EMR procedures were associated with a 1.35% rate of GIB, 0.22% rate of perforation and 9.1% rate of admissions within 30 days compared with a 0.34% rate of GIB, 0.04% rate of perforation and 2.31% rate of 30-day admissions after simple polypectomies. The majority of procedure-related admissions, such as GIB (74%) and perforation (61%), occurred within the first 7 days, whereas only a minority of admissions for any indication (33%) occurred by the same time point. Median time to GIB was similar between EMR procedures and simple polypectomies (median 5 days, IQR 1–11 days vs median 6 days, IQR 1–12 days, p =0.19, respectively), though the median days to perforation and any admission was shorter with simple polypectomies than EMR procedures (perforation: median 1 day, IQR 0–7.5 days vs median 3 days, IQR 0–19, p=0.01, respectively; Admissions: median 11 days, IQR 4–21 vs median 14 days, IQR 6–22, p<0.001, respectively).
Figure 4.
30-day adverse event rates after EMR versus simple polypectomies.
We found that after EMR the rates of admissions decreased from 10.30% in 2011 to 8.38% in 2015 (p<0.001) (Table 2). After simple polypectomies, both the rates of perforation and admission for any indication decreased from 0.06% in 2011 to 0.03% in 2015 (p<0.001) and 2.46% in 2011 to 2.13% in 2015 (p<0.001), respectively. Rates of GIB, cardiac, or infectious adverse events have remained stable between 2011 to 2015 after both EMR and simple polypectomies.
Table 2.
Rate of 30-day adverse events after EMR or simple polypectomy, by year.
| EMR | 2011 N=3745 |
2012 N=5736 |
2013 N=7873 |
2014 N=8647 |
2015 N=10937 |
P value |
|---|---|---|---|---|---|---|
| GIB | 342 (1.11%) | 90 (1.57%) | 105 (1.33%) | 122 (1.41%) | 140 (1.28%) | 0.88 |
| Perforation | 4 (0.11%) | 18 (0.31%) | 18 (0.23%) | 18 (0.21%) | 25 (0.23%) | 0.78 |
| Admission | 290 (10.30%) | 585 (10.20%) | 746 (9.48%) | 736 (8.51%) | 917 (8.38%) | <0.001 |
| Infection | 28 (0.74%) | 38 (0.66%) | 31 (0.38%) | 44 (0.51%) | 65 (0.59%) | 0.41 |
| Cardiac | 41 (1.08%) | 63 (1.10%) | 87 (1.11%0 | 100 (1.16%) | 130 (1.19%) | 0.48 |
| Simple Polypectomies |
2011 N=89,251 |
2012 N=120,206 |
2013 N=150,081 |
2014 N=1156,662 |
2015 N=190,866 |
P value |
|
| ||||||
| GIB | 336 (0.38%) | 448 (0.3750 | 487 (0.32%) | 487 (0.31%) | 696 (0.36%) | 0.25 |
| Perforation | 58 (0.06%) | 63 (0.05%) | 73 (0.05%) | 58 (0.04%) | 56 (0.03%) | <0.0001 |
| Admission | 2207 (2.46%) | 3041 (2.53%) | 3544 (2.35%) | 3500 (2.23%) | 4078 (2.13%) | <0.001 |
| Infection | 176 (0.20%) | 274 (0.23%) | 329 (0.22%) | 348 (0.22%) | 389 (0.20%) | 0.80 |
| Cardiac | 364 (0.41%) | 524 (0.43%) | 651 (0.43%) | 645 (0.41%) | 763 (0.40%) | 0.28 |
EMR, endoscopic mucosal resection; GIB, gastrointestinal bleed
Risk Factors for adverse events after polypectomy
In our multivariate analysis, we found that EMR remained an independent risk factor for all adverse events (Table 3). Increasing age and CCI were associated with an increased risk of all post-polypectomy events. Black race was associated with increased risk of infection (OR, 1.21; 95% CI, 1.03–1.43) and admission (OR, 1.15; 95% CI, 1.09–1.21) for any indication, as compared with white race. Geographic region was also a significant risk factor for certain adverse events. Compared with the Western region, patients with polypectomies performed in other geographic regions were at a higher risk for GIB (Northeast OR, 1.27; 95% CI, 1.10–1.50; Midwest OR, 1.29; 95% CI, 1.14–1.47; South OR, 1.23; 95% CI, 1.09–1.40), cardiac adverse events (Northeast OR, 1.19; 95% CI, 1.04–1.36; Midwest OR, 1.35; 95% CI, 1.20–1.53; South OR, 1.27; 95% CI, 1.12–1.43) and any admissions (Northeast OR, 1.19; 95% CI, 1.12–1.26; Midwest OR, 1.33; 95% CI, 1.27–1.40; South OR, 1.27; 95% CI, 1.21–1.34).
Table 3.
Adjusted odds ratio of adverse events. Multivariate model is adjusted for procedure year, race, gender, CCI, and region.
| GIB | Perforation | Cardiac | Infection | Any Admission | |
|---|---|---|---|---|---|
| EMR | 3.23 (3.01–3.68) | 4.92 (3.83–6.32) | 2.21 (1.99–2.46) | 2.14 (1.84–2.49) | 3.93 (3.77–4.09) |
| Age (years) | 1.05 (1.05–1.06) | 1.04 (1.03–1.05) | 1.09 (1.08–1.09) | 1.06 (1.05–1.06) | 1.03 (1.03–1.04) |
| CCI | 1.22 (1.21–1.25) | 1.05 (1.00–1.12) | 1.26 (1.24–1.28) | 1.35 (1.32–1.37) | 1.25 (1.25–1.26) |
| Race (vs White) | |||||
| Asian | 0.81 (0.65–1.02) | 0.72 (0.37–1.41) | 0.48 (0.37–0.63) | 0.64 (0.45–0.90) | 0.66 (.059–0.73) |
| Black | 1.07 (0.95–1.20) | 0.85 (0.59–1.22) | 1.07 (0.95–1.19) | 1.16 (1.00–1.34) | 1.12 (1.07–1.17) |
| Hispanic | 0.80 (0.68–0.94) | 1.07 (0.72–1.60) | 0.89 (0.77–1.03) | 1.10 (0.92–1.32) | 1.00 (.095–1.06) |
| Female (vs Male) | 0.77 (0.72–0.83) | 1.28 (1.04–1.57) | 0.74 (0.69–1.05) | 0.97 (0.88–1.07) | 0.99 (0.96–1.02) |
| Procedure Year | 0.95 (0.92–0.97) | 0.85 (0.79–0.91) | 0.84 (0.92–0.97) | 0.94 (0.90–0.97) | 0.92 (0.91–0.93) |
| Region1 (vs West) | |||||
| Northeast | 1.27 (1.10–1.50) | 1.00 (0.69–1.45) | 1.19 (1.04–1.36) | 1.03 (0.86–1.23) | 1.19 (1.12–1.26) |
| Midwest | 1.29 (1.14–1.47) | 1.16 (0.84–1.61) | 1.35 (1.20–1.53) | 1.10 (0.93–1.31) | 1.33 (1.27–1.40) |
| South | 1.23 (1.09–1.40) | 0.97 (0.70–1.34) | 1.27 (1.12–1.43) | 1.13 (0.96–1.33) | 1.27 (1.21–1.34) |
West (AZ, CO, ID, MT, NV, NM, UT, WY, AK, CA, HI, OR, WA); Northeast (CT, ME, MA, NH, RI, VT, NJ, NY, PA); Midwest (IL, IN, MI, OH, WI, IA, KS, MN, MO, NE, ND, SD); South (DE, DC, FL, GA, MD, NC, SC, VA, WV, AL, KT, MI, TN, AR, LA, OK, TX)
CCI, Charlson comorbidity index; EMR, endoscopic mucosal resection; GIB, gastrointestinal bleed
Sensitivity analysis
In our multivariate analysis of the EMR and simple polypectomy subgroups, risk factors for adverse events were similar to the primary analysis in the simple polypectomy subgroup (Supplementary Tables 2 and 3). However, in the EMR-only subgroup, we found that a non-Western region was no longer an independent risk factor for adverse events. CCI was also not an independent risk factor for GIB but remained a risk factor for perforations, cardiac adverse events, infections, and admission for any indication.
Discussion:
Using a large U.S. administrative dataset, we provide important information on endoscopic management practices and outcomes of benign colon lesions. We found that the proportion of EMR procedures performed significantly increased from 1.62% of colonoscopies in 2011 to 2.48% of colonoscopies to 2015. We also found significant geographic regional variation, with the highest proportion of EMR in the Western region and lowest in the Southern region.
The rise in EMR use exceeds the rate of increase in all colonoscopy procedures. However, we found geographic regional variation in both the use and adoption of EMR. The Western region performed the highest proportion of EMR and had the fastest increase in EMR use whereas the Southern region performed the lowest proportion of EMRs and had the slowest increase (p<0.001). Our finding of the increase in EMR, however, does not correspond to a decrease in the trends of colectomy for benign colorectal lesions during this period. Rather, Peery et al5 reported increased rates of colectomy from 2000 to 2014 with the lowest rate increase in the Western region. Similarly, Bronzwaer et al14 found stable rates of colectomy in a Dutch cohort.
We are unclear of the reasons for both observed increases as, conceptually, the increase in EMR would correspond to a decrease in the number of surgeries for benign colorectal lesions. Although the rate of EMR is rising, the rate of increase may not be sufficient to overcome the increasing detection of complex benign colon polyps or current practice culture. Indeed, the flat colorectal neoplasm became widely recognized in the western countries in 2008 and its resection requires significant additional training15,16. It is also possible that surgical resection may be preferentially used for proximally located or larger polyps which are considered to be at higher risk for adverse events after endoscopic resection17,18. Bronzwaer et al found that 67% of polyps surgically resected were proximal lesions14.
Polypectomy is associated with an increased risk of adverse events compared with diagnostic colonoscopy19. In our study, we found a GIB rate of 0.34% and perforation rate of 0.04% after simple polypectomy, similar to previously reported rates,12,19,20 and a GIB rate of 1.35% and perforation rate of 0.24% after EMR. We found that EMR was an independent risk factor for an adverse event with a 2- to 5-fold increased odds of any specific adverse events that were either stable or decreased during our study period.
The most common adverse event was 30-day admissions, and importantly, it decreased during our study period. This may represent an increase in provider confidence with the management of more complex patients as we found that patient age and complexity increased over the same period. Furthermore, though rates of admission after EMR were high, they may not all be procedure-related. Procedure-related adverse events such as GIB and perforation occur sooner after polypectomy than non-procedure related adverse events.12 Similarly, we found that by 7 days, 74% of GIB and 61% of perforation occurred compared with only 33% of admissions for any indication.
Adverse event rates found in the current study are lower than those reported by a recent meta-analysis conducted by Hassan et al which found an estimated 0.08% risk of death, 1.5% risk of perforation, and 6.5% risk of bleeding6. This may be because Hassan et al6 included outcomes from older studies as well as endoscopic submucosal dissection (ESD) outcomes in their meta-analysis. It is also possible, that EMR may be used for smaller, less complex polyps whereas proximally-located or larger lesions are preferentially referred for surgical resection, contributing to the lower rates of adverse events observed in this study. We note, however, that the rate of adverse events after EMR remains much lower as compared with those after colectomy. In comparison, colectomies for benign colorectal lesions have been associated with a 14% risk of a major adverse event and a 0.7% risk of 30-day mortality7.
The reasons for the variation in the utilization of EMR nationwide remain unclear but may be due to differences in size and morphology of lesions diagnosed across the different regions. It is also possible that the differences reflect variations in access to providers with confidence in EMR techniques or local practice patterns. Our study was not designed to determine the cause of this variation.
Our study has some limitations. Although our dataset was large, it only encompasses data of a single commercial insurance and Medicare Advantage provider. Thus, patients covered under Medicare or other commercial insurance could not be captured. We were also limited as a specific CPT code (44403, 45390) for EMR was not introduced until 2016. This code is designated for use only with cap-assisted or band-assisted EMR. Therefore, we combined the CPT codes for the components of EMR (snare and injection) with a simultaneous diagnostic code for benign lesions to improve the identification of EMR procedures. To minimize misclassification, we excluded patients who were found to have a new diagnosis of cancer, as an injection may have been used for a tattoo, and we designated the end of the follow-up period for adverse events as December 31, 2015, to allow for the completion of any insurance adjudication. As no specific billing codes exist for ESD, we could also not distinguish between EMR and ESD procedures, albeit this would unlikely influence our findings as the practice of colorectal ESD in the United States remains rare. Additionally, we did not have access to colonoscopy or pathology reports, and thus we could not verify that the EMR was indicated based on lesion characteristics such as size, shape, or location.
In conclusion, we found that the EMR technique is used in an increasing proportion of procedures to endoscopically remove colorectal lesions in the United States. We show that the rates of EMR adverse events have been consistently low with a decrease in rates of admission. Thus, our study indicates the relative safety of EMR procedures when it is widely practiced. As expected, there is regional variation in its utilization. Used according to its indications, endoscopic resection can provide curative removal and obviate the higher morbidity, mortality, and cost associated with surgical treatment. Given the increase in the colectomy of benign lesions, we believe that future efforts should be directed at identifying the barriers and facilitators of EMR use in order to further its application as the first-line management strategy for benign complex colorectal lesions.
Supplementary Material
Supplementary Figure 1. Study consort diagram.
Funding support:
JXY: NIH 2T32 DK 00705642
AJK: NIH KL2 TR 001083
JL: NIH KL2 TR 001083 and NIH UL1 TR 001085
Financial Disclosures:
RS: Olympus – Consultant
TK: Olympus – Consultant; Aries Pharmaceutical – Consultant
Abbreviations:
- CCI
Charlson comorbidity index
- CI
confidence interval
- CPT
current procedural terminology
- CRC
colorectal cancer
- CVA
cerebrovascular accident
- EMR
endoscopic mucosal resection
- GIB
gastrointestinal bleeding
- ICD9
international classification of diseases codes, 9th revision
- ICD10
international classification of diseases codes, 10th revision
- IQR
interquartile range
- MI
myocardial infarction
- NDC
national drug code
- OR
odds ratio
- PAD
peripheral vascular disease
- SD
standard deviation
Footnotes
Data access for this project was provided by the Stanford Center for Population Health Sciences Data Core. The PHS Data Core is supported by a National Institutes of Health National Center for Advancing Translational Science Clinical and Translational Science Award (UL1 TR001085) and internal Stanford funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Ferlitsch M, Reinhart K, Pramhas S, et al. Sex-specific prevalence of adenomas, advanced adenomas, and colorectal cancer in individuals undergoing screening colonoscopy. JAMA. 2011;306:1352–1358. [DOI] [PubMed] [Google Scholar]
- 2.Keswani RN, Law R, Ciolino JD, et al. Adverse events after surgery for nonmalignant colon polyps are common and associated with increased length of stay and costs. Gastrointest Endosc. 2016;84:296–303 e291. [DOI] [PubMed] [Google Scholar]
- 3.Ahlenstiel G, Hourigan LF, Brown G, et al. Actual endoscopic versus predicted surgical mortality for treatment of advanced mucosal neoplasia of the colon. Gastrointest Endosc. 2014;80:668–676. [DOI] [PubMed] [Google Scholar]
- 4.SwaP, BourkJ, AlexandeS, MosA, Williams SJ. Large refractory colonic polyps: is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc. 2009;70:1128–1136. [DOI] [PubMed] [Google Scholar]
- 5.Peery AF, Cools KS, Strassle PD, et al. Increasing Rates of Surgery for Patients With Non-Malignant Colorectal Polyps in the United States. Gastroenterology. 2018. [DOI] [PMC free article] [PubMed]
- 6.Hassan C, Repici A, Sharma P, et al. Efficacy and safety of endoscopic resection of large colorectal polyps: a systematic review and meta-analysis. Gut. 2016;65:806–820. [DOI] [PubMed] [Google Scholar]
- 7.Peery AF, Shaheen NJ, Cools KS, et al. Morbidity and mortality after surgery for nonmalignant colorectal polyps. Gastrointest Endosc. 2018;87:243–250 e242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LaR, DaA, GregorD, et al. Endoscopic resection is cost-effective compared with laparoscopic resection in the management of complex colon polyps: an economic analysis. Gastrointest Endosc. 2016;83:1248–1257. [DOI] [PubMed] [Google Scholar]
- 9.Yu JX, Russell WA, Ching JH, et al. Cost Effectiveness of Endoscopic Resection vs Transanal Resection of Complex Benign Rectal Polyps. Clin Gastroenterol Hepatol. 2019. [DOI] [PubMed]
- 10.Raju GS, Lum PJ, Ross WA, et al. Outcome of EMR as an alternative to surgery in patients with complex colon polyps. Gastrointest Endosc. 2016;84:315–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friedland S, Banerjee S, Kochar R, Chen A, Shelton A. Outcomes of repeat colonoscopy in patients with polyps referred for surgery without biopsy-proven cancer. Gastrointest Endosc. 2014;79:101–107. [DOI] [PubMed] [Google Scholar]
- 12.Wang L, Mannalithara A, Singh G, Ladabaum U. Low Rates of Gastrointestinal and Non-gastrointestinal Complications for Screening or Surveillance Colonoscopies in a Population-based Study. Gastroenterology. 2017. [DOI] [PubMed]
- 13.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical care. 2005;43:1130–1139. [DOI] [PubMed] [Google Scholar]
- 14.Bronzwaer MES, Koens L, Bemelman WA, Dekker E, Fockens P, group Cs. Volume of surgery for benign colorectal polyps in the last 11 years. Gastrointest Endosc. 2018;87:552–561 e551. [DOI] [PubMed] [Google Scholar]
- 15.McGill SK, Soetikno R, Rouse RV, Lai H, Kaltenbach T. Patients With Nonpolypoid (Flat and Depressed) Colorectal Neoplasms at Increased Risk for Advanced Neoplasias, Compared With Patients With Polypoid Neoplasms. Clin Gastroenterol Hepatol. 2017;15:249–256.e241. [DOI] [PubMed] [Google Scholar]
- 16.Rao AK, Soetikno R, Raju GS, et al. Large Sessile Serrated Polyps Can Be Safely and Effectively Removed by Endoscopic Mucosal Resection. Clin Gastroenterol Hepatol. 2016;14:568–574. [DOI] [PubMed] [Google Scholar]
- 17.Kim HS, Kim TI, Kim WH, et al. Risk factors for immediate postpolypectomy bleeding of the colon: a multicenter study. Am J Gastroenterol. 2006;101:1333–1341. [DOI] [PubMed] [Google Scholar]
- 18.Buddingh KT, Herngreen T, Haringsma J, et al. Location in the right hemicolon is an independent risk factor for delayed post-polypectomy hemorrhage: a multi-center case-control study. Am J Gastroenterol. 2011;106:1119–1124. [DOI] [PubMed] [Google Scholar]
- 19.Warren JL, Klabunde CN, Mariotto AB, et al. Adverse events after outpatient colonoscopy in the Medicare population. Annals of internal medicine. 2009;150:849–857, W152. [DOI] [PubMed] [Google Scholar]
- 20.Arora G, Mannalithara A, Singh G, Gerson LB, Triadafilopoulos G. Risk of perforation from a colonoscopy in adults: a large population-based study. Gastrointestinal endoscopy. 2009;69(3 Pt 2):654–664. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1. Study consort diagram.