Abstract
Background:
It has been hypothesized that post-stroke fatigue (PSF) is associated with reduced physical activity (PA) and impaired physical fitness (fitness). Understanding associations between PSF and PA, and/or fitness could help guide the development of targeted exercise interventions to treat PSF.
Aims:
Our systematic review and meta-analysis aimed to investigate PSF’s associations with PA and fitness.
Summary of review:
Following a registered protocol, we included studies with cross-sectional or prospective observational designs, published in English or a Scandinavian language, which reported an association of PSF with PA and/or fitness in adult stroke survivors. We searched MEDLINE, Embase, AMED, CINAHL, PsycINFO, ClinicalTrials.gov, and World Health Organization’s International Clinical Trials Registry Platform from inception to November 30, 2022. Risk of bias was assessed using Quality in Prognosis Studies. Thirty-two unique studies (total n = 4721 participants, 55% male), and three study protocols were included. We used random-effects meta-analysis to pool data for PA and fitness outcomes, and vote-counting of direction of association to synthesize data that could not be meta-analyzed. We found moderate-certainty evidence of a weak association between higher PSF and impaired fitness (meta r = –0.24; 95% confidence interval (CI) = –0.33, –0.15; n = 905, 7 studies), and very low-certainty evidence of no association between PSF and PA (meta r = –0.09; 95% CI = –0.34, 0.161; n = 430, 3 studies). Vote-counting showed a higher proportion of studies with associations between higher PSF and impaired fitness (pˆ = 0.83; 95% CI = 0.44, 0.97; p = 0.22, n = 298, 6 studies), and with associations between higher PSF and lower PA (pˆ = 0.75; 95% CI = 0.51, 0.90; p = 0.08, n = 2566, 16 studies). Very low- to moderate-certainty evidence reflects small study sample sizes, high risk of bias, and inconsistent results.
Conclusions:
The meta-analysis showed moderate-certainty evidence of an association between higher PSF and impaired fitness. These results indicate that fitness might protect against PSF. Larger prospective studies and randomized controlled trials evaluating the effect of exercise on PSF are needed to confirm these findings.
Keywords: Associations, meta-analysis, physical activity, physical fitness, post-stroke fatigue, systematic review
Introduction
Post-stroke fatigue (PSF) is a debilitating condition that affects rehabilitation outcomes, 1 quality of life, 2 and mortality. 1 The reported prevalence of PSF ranges from 25 to 85%. 3 PSF’s etiology is unknown, but is believed to be multifactorial and different types may exist. 4
The literature suggests that PSF could be associated with physical activity (PA) and physical fitness (fitness), 5 which are two distinct, yet related outcomes. PA is defined as “any bodily movement produced by skeletal muscles that results in energy expenditure,” 6 while fitness is “a set of attributes that people have or achieve that relates to the ability to perform PA.” 6 Components of fitness include, but are not restricted to, aerobic fitness, muscle endurance, muscle strength, and body composition. 6 PSF may lead to reduced PA and consequently to impaired fitness, but it is also possible that impaired fitness following a stroke may trigger PSF, leading to reduced PA and further impairments in fitness. 5 PA and fitness are both modifiable factors, so that, although causal relationships are difficult to establish, a better understanding of their associations with PSF could guide development of targeted exercise interventions to reduce PSF. 5 This would be an important step, as there are currently no established interventions for treating PSF, although exercise training interventions have been successful in decreasing fatigue in other conditions.7,8 A systematic review on associations between PSF and impaired fitness concluded that the three eligible studies yielded insufficient evidence about any such association. 5 As additional studies have since been published, we have updated and expanded this review using broader inclusion criteria.
Our primary aim was to conduct a systematic review and meta-analysis to determine whether PSF is associated with PA and/or fitness in patients with stroke. Our secondary aim was to explore PSF’s associations across different sub-domains of PA and fitness.
Methods
The study protocol was registered in the Prospective Register of Systematic Reviews (PROSPERO; CRD42021216435) and reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statement. 9
Eligibility criteria
Eligible studies had cross-sectional or prospective observational designs, were published in English or a Scandinavian language, included stroke survivors aged 18 years or older, and examined associations between PSF and PA and/or fitness. Studies that only measured balance, activities of daily living, or functional limitations were excluded. We included published study protocols/clinical trial registry records (TRRs)) if they met our inclusion criteria.
Search strategies and selection criteria
We performed a systematic search in AMED, CINAHL, Embase, MEDLINE, PsychINFO, ClinicalTrials.gov, and World Health Organization’s (WHO) International Clinical Trials Registry Platform (ICTRP) from inception to November 30, 2022. The search strategies are described in Figure S1.
We de-duplicated records in EndNote X9 10 and imported them into DistillerSR 11 or Rayyan. 12 Two authors (PL and EE) independently screened titles and abstracts, and full-text articles using a pre-piloted eligibility-criteria checklist. TRRs were screened in Rayyan or manually by one author (PL).
Data extraction
Two authors (PL and EE) independently extracted data from eligible studies using a customized data extraction form in DistillerSR. For the updated search, PL extracted the data and another author (MU or AL) cross-checked the extraction. If disagreements could not be resolved, a third author (JB) was consulted. Data included publication details, study and patient characteristics, PSF outcome, PA/fitness outcome, and measure of association (Table S1). We contacted study authors if additional information was needed. Data from multiple reports of the same study were linked together and treated as one. For each study, only one association per outcome (i.e. PA/fitness) was extracted. If a study reported more than one association per outcome, we chose the most relevant (Table S2).
Data synthesis
We performed a meta-analysis when two or more studies reported a correlational value between PSF and PA, or PSF and fitness. We used Comprehensive Meta-analysis software 13 to calculate meta correlation (meta r), 95% confidence intervals (CIs), and prediction intervals. We used random-effects models, which assume that study population or design differences may influence the data. 14 Heterogeneity was assessed by prediction intervals 15 and by visually inspecting the Forest plot. We could not perform sub-group and sensitivity analyses predefined in the PROSPERO protocol, due to an insufficient number of studies. Data that could not be pooled were synthesized by vote-counting of direction of association. We calculated the proportion of studies reporting a negative association (higher PSF and lower PA/fitness) along with 95% CIs (Wilson intervals) using an online calculator. 16 A two-sided p-value was obtained from the binomial probability test using Stata software. 17 Vote-counting does not consider statistical significance or magnitude of association. 14
Risk of bias assessment
Two authors (EE and PL) independently assessed risk of bias. If consensus was not reached, a third author (JB) was consulted. We used the Quality In Prognosis Studies (QUIPS) checklist, 18 modified for our study. QUIPS has six domains (Table S3), each rated as having low, moderate, or high risk of bias.
To detect outcome-reporting biases, we searched for existing protocols for the included studies. We compared the planned outcomes reported in the protocols with reported outcomes in the final publications.
Certainty of evidence
One author (PL) rated certainty of evidence and a second author (JB) cross-checked the rating using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) framework. 19 Quality of evidence was rated as very low, low, moderate, or high. We summarized the evidence in GRADEpro. 20
Results
Search results
The search identified 4125 records. One additional record was obtained from the reference list of a systematic review. 5 After duplicates were removed, 2298 records remained for screening. We excluded 2146 records based on titles and abstracts. We assessed 285 TRRs for eligibility in Rayyan, 40 TRRs manually, and 153 full-text documents in DistillerSR/Rayyan. Thirty-four published papers and two TRRs met the inclusion criteria (Figure S2).
Study characteristics
We included 32 unique studies (total n = 4721 participants, 55% males). Michael and colleagues published two articles21,22 on the same sample, both referred to as Michael 2007. 21 One published protocol and one TRR described included studies.23,24 The second TRR was ongoing. 25 Most studies were of cross-sectional design (n = 22), the others were longitudinal prospective studies (n = 7) or randomized controlled trials (RCTs; n = 2) (Table S4). All studies were published in English between 2006 and 2022. Table S5 describes the characteristics of each included study.
Outcomes
We extracted data for 34 PSF associations, 20 with PA21,23,26–43 and 14 with fitness.21,24,31,32,44–53 Two studies21,31 contributed an association for both outcomes and the rest for only one (n = 30). Three studies became eligible once the authors provided additional information regarding the regression coefficient 39 or direction of association.40,41 The nine-item Fatigue Severity Scale (FSS-9) (19 studies), step-count (six studies), and gait-speed (six studies) were the most frequently used outcome measures for PSF, PA, and fitness, respectively (Table S4). Meta-analyses were performed for PSF and PA (three studies)21,38,41 and for PSF and fitness (seven studies).46–49,51,52,54 There were not enough similar studies to perform meta-analyses for our secondary aim.
Associations between PSF and PA
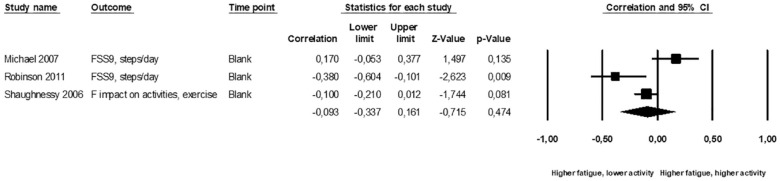
The three studies in the PA meta-analysis included 430 participants.21,38,41 PSF was measured with the FSS-921,38 or a single question about the impact of fatigue on daily activities. 41 PA was measured as steps-per-day21,38 and with a question about weekly exercise habits. 41 The pooled data (Figure 1) showed no correlation between PSF and PA (meta r = –0.09; 95% CI = –0.34, 0.16; p = 0.47; I2 = 79%; very low-certainty evidence). Prediction interval was not calculated because of few included studies.
Figure 1.
Standardized association between post-stroke fatigue and physical activity. Results are shown for individual studies reporting Pearson’s correlation.
The majority of studies reporting on the association between PSF and PA could not be pooled due to heterogeneity in the statistics used (17 studies, 2621 participants).23,26–37,39,40,42,43,55 These studies were synthesized using vote-counting based on direction of association. Table S5 summarizes each study’s statistical methods and association estimates. PSF was most frequently measured using the FSS-729,32 or FSS-9 questionaire.23,27,30,31,33,39,43 Eight studies measured PA with activity monitors and reported: step-counts,23,27,28,32 time in moderate-vigorous activity,39,42 walking time, 33 or time in activity. 34 Eight studies used self-reported PA26,30,31,35–37,40,43 and one used observational methods 29 (Table S4). Twelve studies26,28,30–32,34–37,39,40,43 found a negative direction of association (i.e. higher PSF-lower PA) and four studies23,29,33,42 found a positive association (i.e. higher PSF-higher PA) (Table S6). One study found no direction of association 27 and was excluded from the synthesis. Seventy-five percent of the studies reported an association between higher PSF and lower PA, but the proportion was not statistically significant (pˆ = 0.75; 95% CI = 0.51, 0.90; p = 0.08; very low-certainty evidence; n = 2566; 16 studies).
Combined, PA meta-analysis and vote-counting showed no association between PSF and reduced PA; very low-certainty evidence.
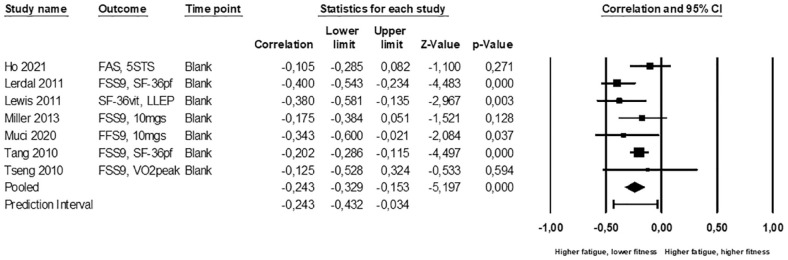
Associations between PSF and fitness
Seven studies with 878 participants contributed to the meta-analysis of fitness.46–49,51,52,54 PSF was measured with the FSS-9,47,49,51,52,54 Fatigue Assessment Scale, 46 or Short Form-36 Vitality subscale. 48 Fitness was measured by five sit-to-stand (5STS), 46 Short Form-36 Physical Functioning subscale (SF-36PF),47,51 lower-limb extensor-power (LLEP), 48 10-meter gait speed (10MGS),49,54 or peak oxygen uptake (VO2-peak). 52 We found a statistically significant correlation (Figure 2) between higher PSF and lower fitness (meta r = –0.24; 95% CI = –0.33, –0.15; p < 0.001; I2 = 31%; 95% prediction interval = –0.43, –0.03; moderate-certainty evidence).
Figure 2.
Standardized association between post-stroke fatigue and physical fitness. Results are shown for individual studies reporting Pearson’s correlation.
The remaining seven studies (330 participants) reporting on associations between PSF and fitness could not be pooled because of differing statistics.21,24,44–46,50,53 PSF was measured with FSS-9,21,24,44,45,50,53 or modified Fatigue Impact Scale. 50 Fitness was measured with 10MGS,21,31,45,50 community ambulation questionnaires,44,53 or VO2-peak. 24 Vote-counting showed 5 studies21,24,44,45,53 had a negative direction of association (higher PSF-lower fitness) and one study 50 had a positive direction (higher PSF-higher fitness) (Table S6). One study showed no association 31 and was excluded from the synthesis. Eighty-three percent of the studies reported an association between higher PSF and lower fitness, but the proportion was not statistically significant (pˆ = 0.83; 95% CI = 0.44, 0.97; p = 0.22, very low-certainty evidence; n = 298; 6 studies).
Combined, the fitness meta-analysis and vote-counting showed a weak association between higher PSF and impaired fitness; low-certainty evidence.
Risk of bias
For the 30 included studies, the QUIPS domains most frequently assessed as having low risk of bias were “Statistical analysis” (all studies) and “Measurement of prognostic factor, fatigue” (all but three studies).29,35,41 The domain most frequently assessed as high risk of bias was “Study confounding” (11 studies)21,32,33,38,40,41,44,45,49,50,54 (Table S7). Our GRADE judgments are shown in Tables S8 and S9. The most common reason for downgrading certainty of evidence was risk of bias, followed by inconsistency and imprecision.
Discussion
To our knowledge, this is the first systematic review including meta-analyses of PSF’s associations with PA and fitness. In contrast to the 2012 review, 5 there were sufficient studies to pool data and assess certainty of evidence.
Fitness vote-counting showed statistically non-significant, very low-evidence of a higher proportion of studies reporting a negative association between PSF and fitness. The analysis was underpowered 14 and should be interpreted with care. However, the meta-analysis showed moderate-certainty evidence of a weak association between PSF and impaired fitness. This finding could support the hypothesis of fitness as a protective factor against PSF. Since fitness is a modifiable factor that can be improved by exercise, 6 exercise training could be a viable intervention for PSF. Zedlitz et al. 56 reported that cognitive therapy combined with exercise training was better at reducing PSF than cognitive therapy alone and suggested that improving physical endurance may help reduce PSF. Their finding is consistent with studies showing that exercise can reduce fatigue associated with other diagnoses.7,8 The potential benefits of exercise training for preventing and treating PSF have been discussed for at least a decade, 57 but few advances have been made toward this goal. We found no studies designed to investigate the effect of exercise training on PSF. Nonetheless, there is now sufficient evidence of a connection between PSF and fitness to warrant RCTs on exercise interventions to relieve PSF.
We estimated no correlation between PSF and PA in the meta-analysis; very low-certainty evidence. Vote-counting showed very low-certainty evidence of a higher proportion of studies reporting a negative association between PSF and PA, but the test was not statistically significant. Our results are supported by a previous meta-analysis that reported no association between PSF and PA. 58 In theory, PSF may cause individuals to be less physically active, 5 but increased PA could also exacerbate PSF. 5 Causality is difficult to establish and may even vary between individuals. Our findings may reflect such variability. Intrapersonal factors affecting patients’ participation in PA may also play a role: some individuals may choose to avoid PA because of PSF, while others may choose to participate in PA despite PSF. 59 Because PSF and PA are complex concepts, with many dimensions and associated factors,4,58,60 a straightforward causal relationship between the two may not exist. Larger prospective studies, designed to investigate specific hypotheses about PSF’s relationship to PA, are warranted.
In prior meta-analyses, the most frequently-reported risk factors for PSF included female sex, depression, and disability.60,61 PA and fitness were not among the factors analyzed, but PA was highlighted as a candidate that could explain more of the variance in PSF. 60 Based on our meta-analyses, we propose fitness as a more likely candidate. However, the weak association of our estimate suggests there are additional factors involved. Previous research has found a non-linear relationship between PSF and age, with higher PSF among both younger and older individuals.60,62 A similar relationship could exist between PSF and fitness, but our study only evaluated linear relationships. Perhaps more likely, age and higher demands on younger individuals 60 may confound PSF’s relationship with fitness. In our clinical experience, younger patients often suffer from PSF despite being relatively fit. Thus, age-adjusted associations may be stronger, but some included studies did not adjust for age. Well-designed studies are needed to further update the evidence-base on both PSF risk factors and interventions to improve care for stroke survivors of all ages. 63
Limitations and strengths
There are several limitations of the included studies. The majority of the evidence came from studies with small sample sizes, using different outcome measures, measured at different time-points. Fatigue instruments are known to measure different dimensions (e.g. intensity, physical fatigue, mental fatigue, impact on activities), and there is a lack of content overlap between instruments. 64 This means that the fatigue instruments themselves may have varying degrees of associations with PA and fitness. The same applies to the different PA and fitness outcome measures. The included studies also measured associations at different time-points post-stroke, and associations between PSF, PA, and fitness may differ during the acute phase, rehabilitation, or a more stable phase. The extracted associations were reported as a secondary aim or finding in 15 studies,26,27,30,32,33,38,41,43,44,46,47,49,51–53 suggesting that these studies were designed and powered for other primary objectives.
As for limitations of our review, since most of the included studies did not have published protocols, we did not use protocols in conjunction with risk of bias assessment as we had planned. This decision did not affect the overall risk of bias in the two studies23,24 concerned, nor did it affect the GRADE confidence in certainty of evidence. The PA meta-analysis estimate should be interpreted with caution due to high heterogeneity. A very low certainty of evidence means that the actual estimate of association may differ in either direction. Finally, selection bias may exist, as we only included studies published in English or a Scandinavian language. Our study’s strengths include the multidisciplinary research team, adherence to systematic review guidelines, the extensive search (including TRRs), ability to pool data, and use of GRADE to appraise the certainty of evidence.
Clinical implications
Given the multiple benefits of PA and exercise for post-stroke recovery, 65 it is arguable that PA and exercise training should be recommended regardless of whether patients have PSF or not. As PSF can be a barrier to PA, 66 proper screening, assessment and individually-tailored management of PSF is essential.
Conclusion
The fitness meta-analysis showed moderate-certainty evidence of an association between PSF and fitness, indicating that being physically fit might protect against PSF. This result needs to be confirmed by RCTs evaluating exercise interventions, with PSF as the primary outcome. The PA meta-analysis showed very low-certainty evidence of no association between PSF and PA, highlighting the lack of large prospective observational studies in this field of research.
Supplemental Material
Supplemental material, sj-docx-1-wso-10.1177_17474930231152132 for Association of post-stroke fatigue with physical activity and physical fitness: A systematic review and meta-analysis by Petra Larsson, Julia Bidonde, Unni Olsen, Caryl L Gay, Anners Lerdal, Marie Ursin, Gillian Elizabeth Mead and Elisabeth Edvardsen in International Journal of Stroke
Acknowledgments
The authors thank health information specialist Hilde Flaaten of University of Oslo’s Library of Medicine and Science, who helped to develop and perform the literature search, and Professor Milada C. Småstuen at OsloMet for statistical advice in planning this review.
Footnotes
Author note: PROSPERO 2021 CRD42021216435.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Petra Larsson  https://orcid.org/0000-0003-3866-8287
https://orcid.org/0000-0003-3866-8287
Anners Lerdal  https://orcid.org/0000-0002-7144-5096
https://orcid.org/0000-0002-7144-5096
Gillian Mead  https://orcid.org/0000-0001-7494-2023
https://orcid.org/0000-0001-7494-2023
Supplemental material: Supplemental material for this article is available online.
References
- 1. Glader EL, Stegmayr B, Asplund K. Poststroke fatigue: a 2-year follow-up study of stroke patients in Sweden. Stroke 2002; 33: 1327–1333. [DOI] [PubMed] [Google Scholar]
- 2. Lerdal A, Gay CL. Fatigue in the acute phase after first stroke predicts poorer physical health 18 months later. Neurology 2013; 81: 1581–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cumming TB, Packer M, Kramer SF, et al. The prevalence of fatigue after stroke: a systematic review and meta-analysis. Int J Stroke 2016; 11: 968–977. [DOI] [PubMed] [Google Scholar]
- 4. Nadarajah M, Goh HT. Post-stroke fatigue: a review on prevalence, correlates, measurement, and management. Top Stroke Rehabil 2015; 22: 208–220. [DOI] [PubMed] [Google Scholar]
- 5. Duncan F, Kutlubaev MA, Dennis MS, Greig C, Mead GE. Fatigue after stroke: a systematic review of associations with impaired physical fitness. Int J Stroke 2012; 7: 157–162. [DOI] [PubMed] [Google Scholar]
- 6. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 1985; 100: 126–131. [PMC free article] [PubMed] [Google Scholar]
- 7. Belloni S, Arrigoni C, Caruso R. Effects from physical exercise on reduced cancer-related fatigue: a systematic review of systematic reviews and meta-analysis. Acta Oncol 2021; 60: 1678–1687. [DOI] [PubMed] [Google Scholar]
- 8. Razazian N, Kazeminia M, Moayedi H, et al. The impact of physical exercise on the fatigue symptoms in patients with multiple sclerosis: a systematic review and meta-analysis. BMC Neurol 2020; 20: 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 2021; 134: 178–189. [DOI] [PubMed] [Google Scholar]
- 10. The EndNote Team. EndNote, https://endnote.com/ (2013).
- 11. DistillerSR (Version 2.35), https://www.evidencepartners.com (accessed January 2021-April 2022).
- 12. Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-aweb and mobile app for systematic reviews. Syst Rev 2016; 5: 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Comprehensive meta-analysis (Version 4.0), http://www.Meta-Analysis.com (2022).
- 14. Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions (version 6.3). Cochrane, www.training.cochrane.org/handbook (2022).
- 15. Borenstein M, Higgins JP, Hedges LV, et al. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res Synth Methods 2017; 8: 5–18. [DOI] [PubMed] [Google Scholar]
- 16. Statistics Kingdom. Proportion confidence interval calculator, https://www.statskingdom.com/proportion-confidence-interval-calculator.html (accessed 12 September 2022).
- 17. StataCorp. Stata Statistical Software: Release 17. College Station, TX: StataCrop LLC, 2019. [Google Scholar]
- 18. Hayden JA, van der Windt DA, Cartwright JL, et al. Assessing bias in studies of prognostic factors. Ann Intern Med 2013; 158: 280–286. [DOI] [PubMed] [Google Scholar]
- 19. Schüneman H, Brozek J, Guyatt G, et al. GRADE handbook for grading of evidence and strength of recommendations. https://gdt.gradepro.org/app/handbook/handbook.html (2013, accessed 14 September 2022)
- 20. GRADEpro GDT, gradepro.org (2022, accessed September-December 2023). [Google Scholar]
- 21. Michael K, Macko RF. Ambulatory activity intensity profiles, fitness, and fatigue in chronic stroke. Top Stroke Rehabil 2007; 14: 5–12. [DOI] [PubMed] [Google Scholar]
- 22. Michael KM, Allen JK, Macko RF. Fatigue after stroke: relationship to mobility, fitness, ambulatory activity, social support, and falls efficacy. Rehabil Nurs 2006; 31: 210–217. [DOI] [PubMed] [Google Scholar]
- 23. Fini NA, Bernhardt J, Churilov L, et al. A 2-year longitudinal study of physical activity and cardiovascular risk in survivors of stroke. Phys Ther 2021; 101: 1–9. [DOI] [PubMed] [Google Scholar]
- 24. Oyake K, Baba Y, Suda Y, et al. Cardiorespiratory responses to exercise related to post-stroke fatigue severity. Sci Rep 2021; 11: 12780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lejeune T. Functional characterisation of post-stroke fatigue (study protocol). https://clinicaltrials.gov/ct2/history/NCT04277234 (2020)
- 26. Almhdawi KA, Jaber HB, Khalil HW, et al. Post-stroke fatigue level is significantly associated with mental health component of health-related quality of life: a cross-sectional study. Qual Life Res 2021; 30: 1165–1172. [DOI] [PubMed] [Google Scholar]
- 27. Danks KA, Pohlig RT, Roos M, et al. Relationship between walking capacity, biopsychosocial factors, self-efficacy, and walking activity in persons poststroke. J Neurol Phys Ther 2016; 40: 232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Duncan F, Lewis SJ, Greig CA, et al. Exploratory longitudinal cohort study of associations of fatigue after stroke. Stroke 2015; 46: 1052–1058. [DOI] [PubMed] [Google Scholar]
- 29. Egerton T, Hokstad A, Askim T, et al. Prevalence of fatigue in patients 3 months after stroke and association with early motor activity: a prospective study comparing stroke patients with a matched general population cohort. BMC Neurol 2015; 15: 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hamre C, Fure B, Helbostad JL, et al. Factors associated with level of physical activity after minor stroke. J Stroke Cerebrovasc Dis 2021; 30: 105628. [DOI] [PubMed] [Google Scholar]
- 31. Hoang CL, Salle JY, Mandigout S, Hamonet J, Macian-Montoro F, Daviet JC. Physical factors associated with fatigue after stroke: an exploratory study. Top Stroke Rehabil 2012; 19: 369–376. [DOI] [PubMed] [Google Scholar]
- 32. Mahendran N, Kuys SS, Brauer SG. Which impairments, activity limitations and personal factors at hospital discharge predict walking activity across the first 6 months poststroke? Disabil Rehabil 2020; 42: 763–769. [DOI] [PubMed] [Google Scholar]
- 33. Paul L, Brewster S, Wyke S, et al. Physical activity profiles and sedentary behaviour in people following stroke: a cross-sectional study. Disabil Rehabil 2016; 38: 362–367. [DOI] [PubMed] [Google Scholar]
- 34. Hei Chow C, Fraysse F, Hillier S. The relationship between sleep and physical activity in an in-patient rehabilitation stroke setting: a cross-sectional study. Top Stroke Rehabil 2021; 30: 1–10. [DOI] [PubMed] [Google Scholar]
- 35. Kirchberger I, Wallner F, Linseisen J, et al. Factors associated with early and late post-stroke fatigue in patients with mild impairment. Results from the stroke cohort study Augsburg. Front Neurol 2022; 13: 852486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pedersen A, Almkvist E, Holmegaard L, et al. Fatigue 7 years post-stroke: predictors and correlated features. Acta Neurol Scand 2022; 146: 295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sibbritt PD, Peng DW, Hosseini DM, Maguire PJ, Bayes J, Adams PJ. An examination of modifiable risk factors in stroke survivors, with a view to recurrent stroke prevention. J Stroke Cerebrovasc Dis 2022; 31: 106547. [DOI] [PubMed] [Google Scholar]
- 38. Robinson CA, Shumway-Cook A, Ciol MA, Kartin D. Participation in community walking following stroke: subjective versus objective measures and the impact of personal factors. Phys Ther 2011; 91: 1865–1876. [DOI] [PubMed] [Google Scholar]
- 39. Sanchez-Sanchez ML, Arnal-Gomez A, Cortes-Amador S, et al. Association of barriers, fear of falling and fatigue with objectively measured physical activity and sedentary behavior in chronic stroke. J Clin Med 2021; 10: 1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schüler J, Wolff W, Pfeifer J, et al. The role of perceived energy and self-beliefs for physical activity and sports activity of patients with multiple sclerosis and chronic stroke. Front Psychol 2020; 11: 570221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shaughnessy M, Resnick BM, Macko RF. Testing a model of post-stroke exercise behavior. Rehabil Nurs 2006; 31: 15–21. [DOI] [PubMed] [Google Scholar]
- 42. Shepherd AI, Pulsford R, Poltawski L, et al. Physical activity, sleep, and fatigue in community dwelling stroke survivors. Sci Rep 2018; 8: 7900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wang SS, Wang JJ, Wang PX, Chen R. Determinants of fatigue after first-ever ischemic stroke during acute phase. PLoS ONE 2014; 9: e110037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Durcan S, Flavin E, Horgan F. Factors associated with community ambulation in chronic stroke. Disabil Rehabil 2016; 38: 245–249. [DOI] [PubMed] [Google Scholar]
- 45. Goh HT, Stewart JC. Poststroke fatigue is related to motor and cognitive performance: a secondary analysis. J Neurol Phys Ther 2019; 43: 233–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ho LYW, Lai CKY, Ng SSM. Contribution of sleep quality to fatigue following a stroke: a cross-sectional study. BMC Neurol 2021; 21: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lerdal A, Bakken LN, Rasmussen EF, et al. Physical impairment, depressive symptoms and pre-stroke fatigue are related to fatigue in the acute phase after stroke. Disabil Rehabil 2011; 33: 334–342. [DOI] [PubMed] [Google Scholar]
- 48. Lewis SJ, Barugh AJ, Greig CA, et al. Is fatigue after stroke associated with physical deconditioning? a cross-sectional study in ambulatory stroke survivors. Arch Phys Med Rehabil 2011; 92: 295–298. [DOI] [PubMed] [Google Scholar]
- 49. Muci B, Keser I, Meric A, et al. What are the factors affecting dual-task gait performance in people after stroke? Physiother 2022; 38: 621–628. [DOI] [PubMed] [Google Scholar]
- 50. Obembe AO, Olalemi AE, Loto BO. Fatigue impact, gait and balance performance in chronic stroke survivors. Physiother Pract Res 2014; 35: 49–54. [Google Scholar]
- 51. Tang WK, Lu JY, Chen YK, Mok VC, Ungvari GS, Wong KS. Is fatigue associated with short-term health-related quality of life in stroke. Arch Phys Med Rehabil 2010; 91: 1511–1515. [DOI] [PubMed] [Google Scholar]
- 52. Tseng BY, Billinger SA, Gajewski BJ, et al. Exertion fatigue and chronic fatigue are two distinct constructs in people post-stroke. Stroke 2010; 41: 2908–2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. van de Port IG, Kwakkel G, Lindeman E. Community ambulation in patients with chronic stroke: how is it related to gait speed. J Rehabil Med 2008; 40: 23–27. [DOI] [PubMed] [Google Scholar]
- 54. Miller KK, Combs SA, Van Puymbroeck M, et al. Fatigue and pain: relationships with physical performance and patient beliefs after stroke. Top Stroke Rehabil 2013; 20: 347–355. [DOI] [PubMed] [Google Scholar]
- 55. Paul L, Brewster S, Wyke S, et al. Physical activity profiles and sedentary behaviour in people following stroke: a cross-sectional study. Disabil Rehabil 2016; 38: 362–367. [DOI] [PubMed] [Google Scholar]
- 56. Zedlitz AM, Rietveld TC, Geurts AC, Fasotti L. Cognitive and graded activity training can alleviate persistent fatigue after stroke: a randomized, controlled trial. Stroke 2012; 43: 1046–1051. [DOI] [PubMed] [Google Scholar]
- 57. Mead G, Bernhardt J, Kwakkel G. Stroke: physical fitness, exercise, and fatigue. Stroke Res Treat 2012; 2012: 632531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Thilarajah S, Mentiplay BF, Bower KJ, et al. Factors associated with post-stroke physical activity: a systematic review and meta-analysis. Arch Phys Med Rehabil 2018; 99: 1876–1889. [DOI] [PubMed] [Google Scholar]
- 59. Rietberg MB, van Wegen EE, Uitdehaag BM, Kwakkel G. The association between perceived fatigue and actual level of physical activity in multiple sclerosis. Mult Scler 2011; 17: 1231–1237. [DOI] [PubMed] [Google Scholar]
- 60. Cumming TB, Yeo AB, Marquez J, et al. Investigating post-stroke fatigue: an individual participant data meta-analysis. J Psychosom Res 2018; 113: 107–112. [DOI] [PubMed] [Google Scholar]
- 61. Zhang S, Cheng S, Zhang Z, Wang C, Wang A, Zhu W. Related risk factors associated with post-stroke fatigue: a systematic review and meta-analysis. Neurol Sci 2021; 42: 1463–1471. [DOI] [PubMed] [Google Scholar]
- 62. Lerdal A, Gay CL, Lee KA. Curvilinear relationship between age and post-stroke fatigue among patients in the acute phase following first-ever stroke. Int J Phys Med Rehabil 2013; 1: 1–7. [Google Scholar]
- 63. Aali G, Drummond A, das Nair R, et al. Post-stroke fatigue: a scoping review. F1000Res 2020; 9: 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Skogestad IJ, Kirkevold M, Indredavik B, Gay CL, Lerdal A. and NORFAST (Norwegian Study of Fatigue After Stroke) Group. Lack of content overlap and essential dimensions-a review of measures used for post-stroke fatigue. J Psychosom Res 2019; 124: 109759. [DOI] [PubMed] [Google Scholar]
- 65. Billinger SA, Arena R, Bernhardt J, et al. Physical activity and exercise recommendations for stroke survivors. Stroke 2014; 45: 2532–2553. [DOI] [PubMed] [Google Scholar]
- 66. Debora Pacheco B, Guimaraes Caetano LC, Amorim Samora G, et al. Perceived barriers to exercise reported by individuals with stroke, who are able to walk in the community. Disabil Rehabil 2021; 43: 331–337. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-wso-10.1177_17474930231152132 for Association of post-stroke fatigue with physical activity and physical fitness: A systematic review and meta-analysis by Petra Larsson, Julia Bidonde, Unni Olsen, Caryl L Gay, Anners Lerdal, Marie Ursin, Gillian Elizabeth Mead and Elisabeth Edvardsen in International Journal of Stroke