Abstract
Practical relevance:
Information crucial to the diagnosis and treatment of feline oral diseases can be ascertained using dental radiography and the inclusion of this technology has been shown to be the best way to improve a dental practice. Becoming familar with the techniques required for dental radiology and radiography can, therefore, be greatly beneficial.
Clinical challenges:
Novices to dental radiography may need some time to adjust and become comfortable with the techniques. If using dental radiographic film, the generally recommended ‘E’ or ‘F’ speeds may be frustrating at first, due to their more specific exposure and image development requirements. Although interpreting dental radiographs is similar to interpreting a standard bony radiograph, there are pathologic states that are unique to the oral cavity and several normal anatomic structures that may mimic pathologic changes. Determining which teeth have been imaged also requires a firm knowledge of oral anatomy as well as the architecture of dental films/digital systems.
Evidence base:
This article draws on a range of dental radiography and radiology resources, and the benefit of the author’s own experience, to review the basics of taking and interpreting intraoral dental radiographs. A simplified method for positioning the tubehead is explained and classic examples of some common oral pathologies are provided.
Getting started
Intraoral dental radiography is quickly becoming the standard of care in small animal dentistry. it has been shown that there is no better way to improve a dental practice than by adding this technology. Furthermore, dental radiology provides crucial information for the diagnosis and treatment of feline oral diseases. For these reasons, a firm grasp on the subject is strongly recommended. 1
Getting started in dental radiography can seem a daunting task. However, with a little training and practice, radiography becomes fun and surprisingly easy. For example, instead of measuring the bisecting angle for every radiograph, there is a simplified technique (discussed later) that can provide a quick approximation. Furthermore, given that the majority of dental radiographic findings are rarelysubtle, interpretation is often less challenging than it might at first sight seem.
Dental radiography equipment
Dental radiograph units2,3
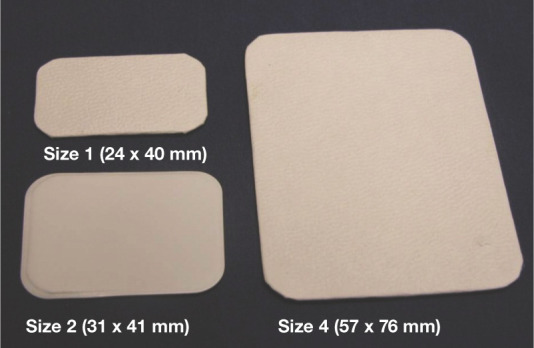
Radiographic exposure is controlled by three components: kilovolt peak (kVp), milliamperage (mA) and exposure time (see box). Since radiographically there is not a significant amount of variation in oral tissues, the kVp and mA are set constant on dental radiog- raphy units (Figure 1). The only variable factor is time. This is typically measured in seconds (or fractions of). Most dental radiography units have a digital control for the exposure and it is set by the operator. Recently, however, veterinary- specific machines have become available which have a computer that sets the exposure based on the size of the patient, the speed of dental film used (or type of digital system) and the particular object tooth. This can take a lot of the guesswork out of the exposure set- ting. Nonetheless, with a little experience and practice, it is easy to figure out a setting.
Figure 1.

Veterinary dental unit control pad.
One decision that a veterinary clinic will need to make when adding this technology is whether to have the generator wall mounted or to elect for a mobile stand. in general, wall mounted is preferable if the physical plant/dental area will support it. This is because it takes up less floor space, does not need to be moved into the dental area and, in general, is more stable.
Dental radiographic film2–4
Dental film is non-screen film. This means that it is directly exposed by the x-ray and does not require an intensifying screen, pro- viding much more detail than standard radio- graphic film. it is packaged in its own paper or plastic sleeve to protect it from light and the oral environment.
There are three types of dental film commonly used in dental radiography – ‘d’, ‘E’ and ‘F’ speeds. They differ in the size of the silver halide crystals and consequently the amount of exposure required to produce an image. ‘E’ speed film requires approximately half the amount of radiation for exposure than ‘d’ speed film, and ‘F’ speed even less. This reduces exposure to the patient and staff, as well as wear and tear on the x-ray unit. There is a slight decrease in resolution with faster films due to the larger crystal size but, accord- ing to most experts, the difference is negligi- ble. Therefore, it is recommended in human dentistry to use ‘E’ or ‘F’ speed to decrease exposure time. They are more technique sensi- tive, however, both in terms of exposure and development of the image. This may be frus- trating for the novice and so it is generally rec- ommended that practitioners start with ‘d’ speed film and advance to ‘E’ or ‘F’ speed when they are more comfortable with the set- tings and positioning of the tubehead.
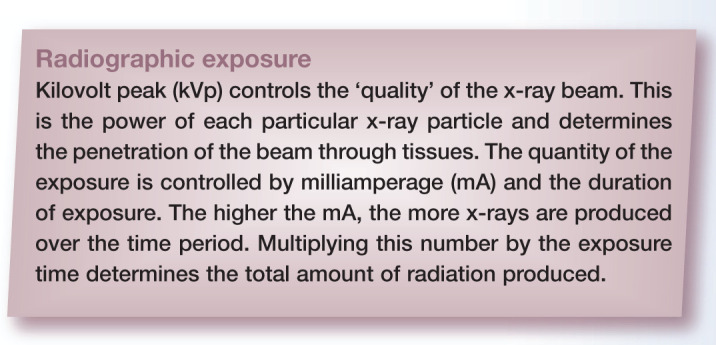
There are several different sizes of dental film available (4, 3, 2, 1 and 0). The most com- monly used in veterinary medicine are sizes 4, 2 and 1 (Figure 2). Size 4 film (57 x 76 mm) is the largest available and is used mostly for taking extraoral views. For maxillary and ros- tral mandibular views, size 2 (31 x 41 mm) is commonly used. Mandibular premolars and the first molar can be imaged with size 2, but size 1 (24 x 40 mm) or 0 (22 x 35 mm) may be easier for small cats.
Figure 2.
Dental radiographic film
Digital dental radiography 5
There are numerous veterinary digital sys- tems, both digital radiography (dR) using a sensor and computed radiography (CR) using photostimulable phosphor (PSP) plates (Figure 3). CR systems have the complete range of plate sizes available (0–4), while for dR systems the largest sensor size is 2. Since cats rarely require a size 4, sensor systems (size 1 or 2) are generally recommended. These are excellent means of obtaining dental radiographs. The major advantages of these systems are the decrease in radiation exposure (exposure times are generally much shorter), speed of acquisition of the image and ease of correction of projection errors. images from dR systems are available almost immediately, whereas CR systems require removing the film from the patient’s mouth and scanning.
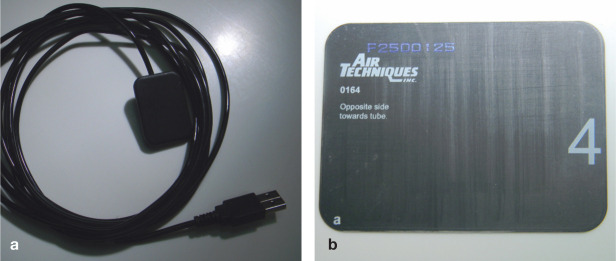
Figure 3.
Digital dental systems. (a) Direct digital sensor (DR). (b) Indirect phosphor plate (CR)
Digital dental radiography is quickly becoming the standard of practice in small animal hospitals. Exposure techniques for digital systems are very similar to those used for standard dental radiographs.
Taking a dental radiograph3,4,6–10
Step 1: Patient positioning
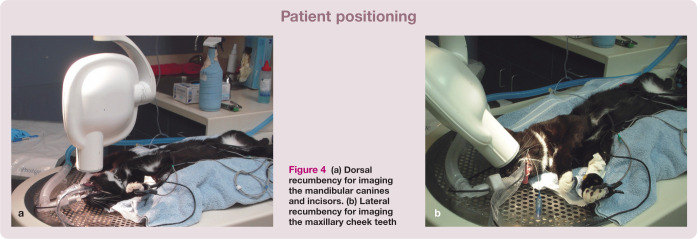
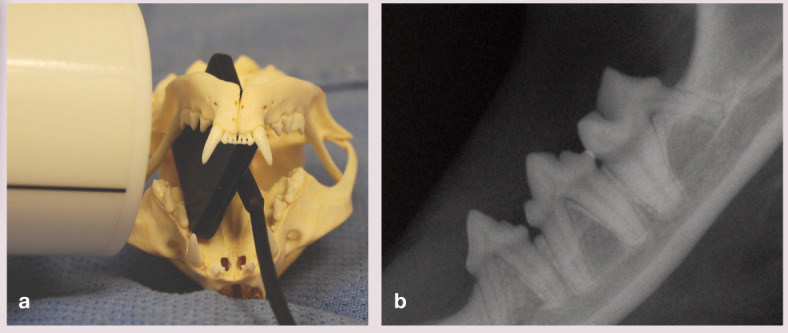
The cat is positioned so that the area of interest is convenient to the radiographic beam. in general the arcade to be imaged is ‘up’. When imaging the mandibular canines and incisors the patient should be in dorsal recumbency (Figure 4a). For mandibular cheek teeth the patient should be in lateral recumbency with the affected side up. opinion is divided over the best positioning for imaging the maxillary cheek teeth, with some dentists recommending ventral and others lateral recumbency (Figure 4b). it is easier to visualize angles in ventral recumbency and so this may be of benefit for the initial survey. However, in the author’s practice virtually all radiographs are exposed in lateral recumbency. This takes getting used to, but decreases the number of times a patient must be rolled when doing surgical (ie, post- extraction) or endodontic procedures.
Figure 4.
(a) Dorsal recumbency for imaging the mandibular canines and incisors. (b) Lateral arecumbency for imaging the maxillary cheek teeth
Step 2: Film placement within the patient’s mouth
Standard film has an embossed dot on a corner on one side, the convex aspect of which should be placed towards the x-ray beam. in most films, this side is pure white and the opposite or ‘back’ side of the film will usually be colored. When using a sensor, the cord will exit on the ‘back’ side of the sensor and this side faces away from the tubehead. The film/sensor is positioned in the mouth so that it covers the entire tooth (crown and full extent of the root). Placing the film/sensor as near as possible to (ideally touch- ing) the tooth and gingiva will minimize distor- tion. it should be ensured the film is straight, as any bending will result in image distortion.
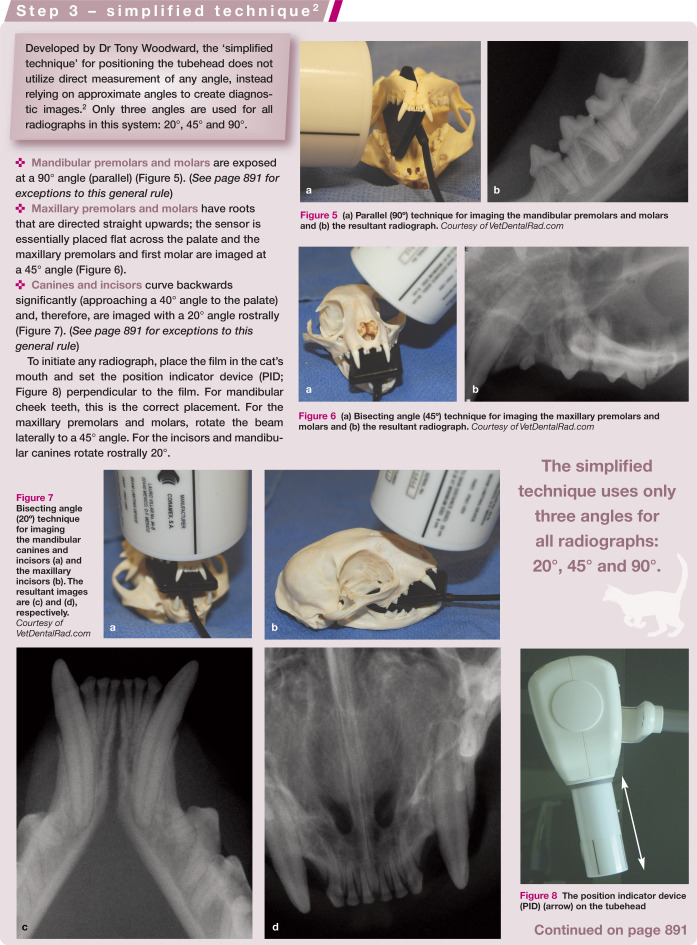
Step 3: Positioning the tubehead
There are two major techniques for positioning the tubehead in veterinary patients, both of which are used daily in practice. 10
Parallel technique The film/sensor is placed parallel to the tooth/root (object) being radiographed and the beam is directed perpendicular to both the film/sensor and the object. This is how the majority of standard (large) films are taken and produces the most accurate image. Unfortunately this is only useful for the mandibular cheek teeth – and not even all of them! The maxillary cheek teeth cannot be imaged in this manner due to the lack of an arched palate, nor the rostral mandibular cheek teeth due to the symphysis.
Bisecting angle technique The most common type of dental radiograph taken in veterinary patients uses the theory of equilateral triangles to create an image that accurately represents the tooth and roots. To utilize this technique, the film/sensor is placed as parallel as possible to the tooth root. The angle between the tooth root and film/sensor is then measured. This angle is cut in half (bisected) and the beam directed perpendicular to this angle. This gives the most accurate representation of the root. However, if this angle is incorrect, the radiographic image will be distorted. This is because the x-ray beam will create an image that is longer or shorter than the object (see box below).
Figure 5.
(a) Parallel (90º) technique for imaging the mandibular premolars and molars and (b) the resultant radiograph. Courtesy of VetDentalRad.com
Figure 6.
(a) Bisecting angle (45º) technique for imaging the maxillary premolars and molars and (b) the resultant radiograph. Courtesy of VetDentalRad.com
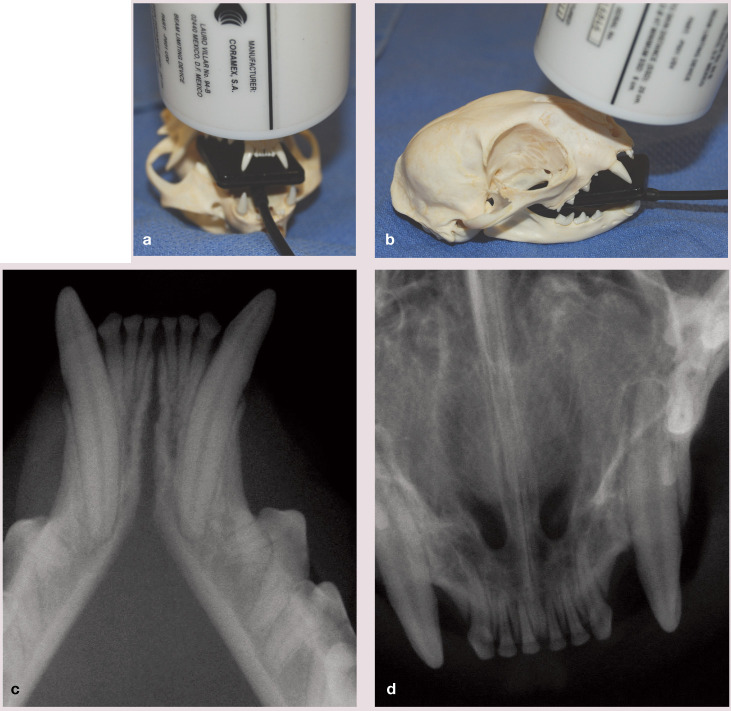
Figure 7.
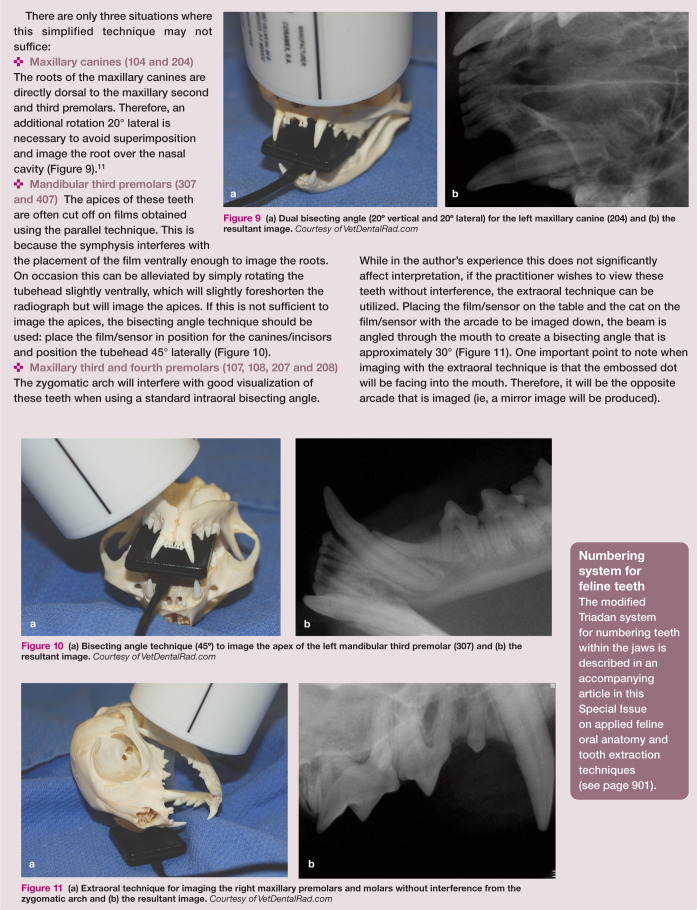
Bisecting angle (20º) technique for imaging the mandibular canines and incisors (a) and the maxillary incisors (b). The resultant images are (c) and (d), respectively. Courtesy of VetDentalRad.com
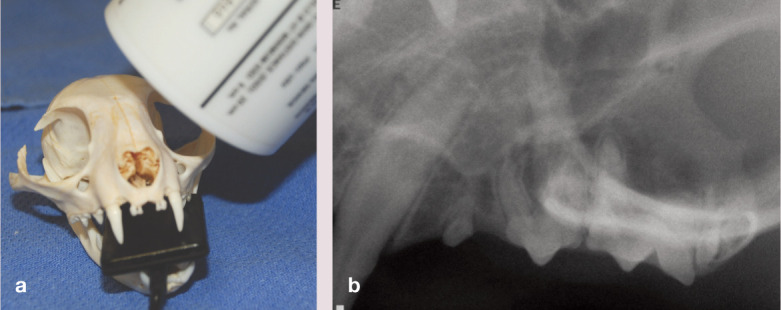
Figure 8.
The position indicator device (PID) (arrow) on the tubehead
Figure 9.
(a) Dual bisecting angle (20º vertical and 20º lateral) for the left maxillary canine (204) and (b) the resultant image. Courtesy of VetDentalRad.com
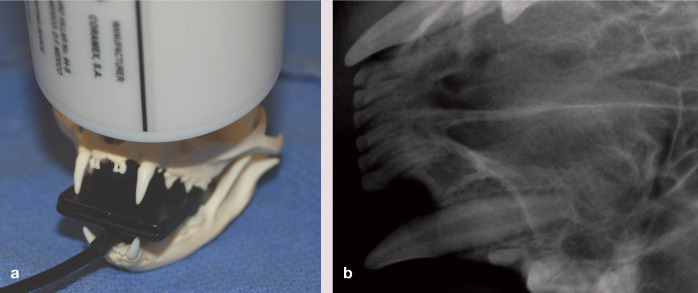
Figure 10.
(a) Bisecting angle technique (45º) to image the apex of the left mandibular third premolar (307) and (b) the resultant image. Courtesy of VetDentalRad.com
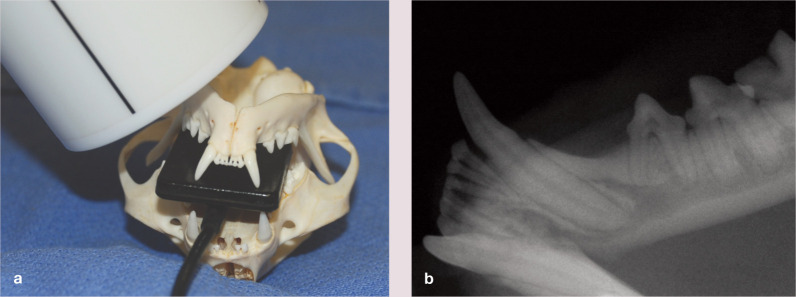
Figure 11.
(a) Extraoral technique for imaging the right maxillary premolars and molars without interference from the zygomatic arch and (b) the resultant image. Courtesy of VetDentalRad.com
Step 4: Setting the exposure
If using a machine where the exposure is set manually, the correct setting will need to be determined. Generally for cats there is one set- ting for the maxilla and one for the mandible that is easily established. if utilizing a com- puter-controlled system, the buttons are set for the species, film/digital system and tooth to be imaged.
Step 5: Exposing the radiograph
Dental radiograph machines have a handheld device to expose the radiograph. if possible, the operator should leave the room prior to exposing the radiograph. if not, it is important to stand at least 6 feet (1.8 m) away at a 90–130° angle to the primary beam. The device comprises a ‘dead man’s’ switch, which means that if the operator lets go dur- ing the exposure, it will stop the production of x-ray beams and give an error message; to avoid having to restart an exposure it should be ensured that the button is held down until the machine stops beeping.
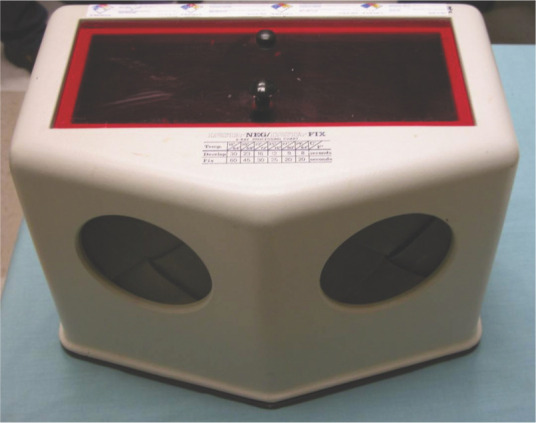
Step 6: Developing the radiograph4,6,12
Radiographs need to be developed away from ambient light. The most economical way is with cupfuls of dental developing solutions in a darkroom. (Using chemicals other than products for dental radiography will result in inferior film quality; Figure 12.) However, although a dark- room technique can produce quality films, the use of a chairside developer is recommended (Figure 13).
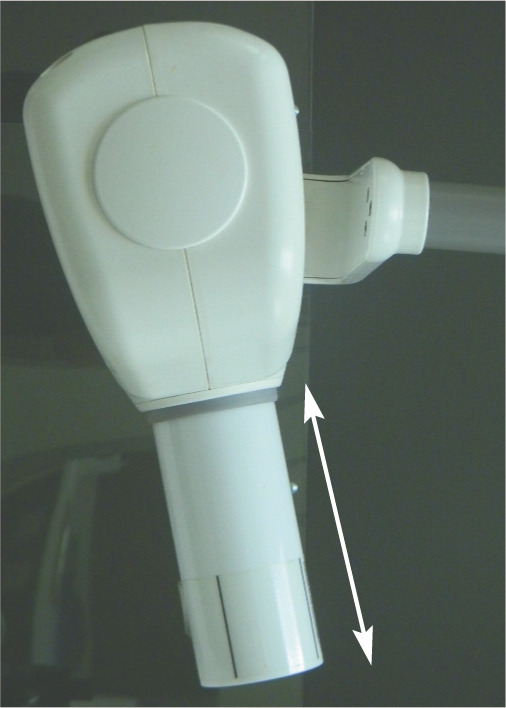
Figure 12.
Poor film quality due to use of a developing solution not specific for dental radiography
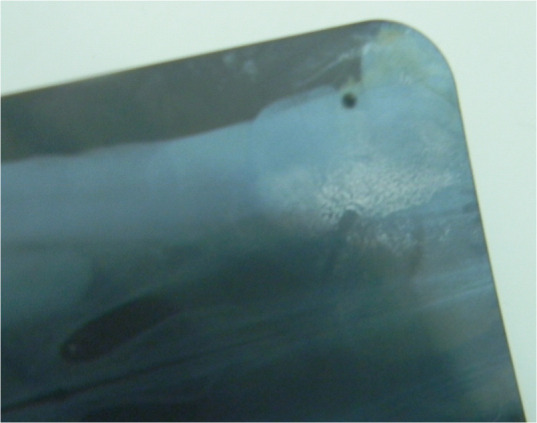
Figure 13.
Chairside developer
The process of developing a radio- graph is begun by peeling back the cov- ering layers from the film, taking care to handle the film only by the edges. A film clip is used to grasp the corner of the film, which is first immersed in water to hydrolyse the gela- tin layer covering the film before being placed in the developer (Figure 14). once an image is just visible (sight developing), the film is rinsed briefly in a water bath and placed in fixer for 30–60 s (following manufacturers’ rec- ommendations) until partially fixed. The film may be evaluated at this stage, but should be placed back in the fixer for an additional 10 mins to ensure complete fixation. When com- pletely fixed, the film becomes clear and will lose all traces of a greenish color. The film should then be thoroughly rinsed in running water, or placed in a clean water bath for 10–15 mins followed by a final rinse. it is important to remove all traces of fixer (any fixer remain- ing on a dental film will give it a characteristic ‘slick’ feel). The film is then placed in drying clips overnight to dry (films that are not com- pletely dry risk sticking together).
Figure 14.
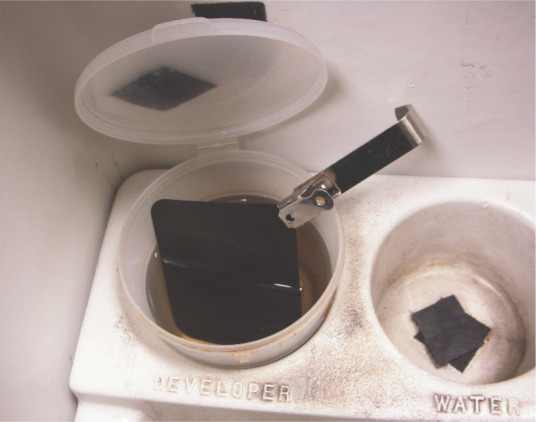
Film clip on the edge of an analog film
Solutions should be changed whenever developing and fixation times seem to be slowing down. This will occur after around 20 smaller (size 0 or 2) films or 10–15 larger (size 4) films have been developed and fixed. Use of exhausted chemistry results in poor image quality and hazy images.
Interpretation of dental radiographs
Interpreting dental radiographs can be daunting, but is very similar in principle to interpreting any standard bony radiograph.
The first step in radiographic interpretation – before attempting to decipher abnormal from normal – is determining which teeth have been imaged. This requires a firm knowledge of oral anatomy as well as the architecture of dental films/digital systems. digital systems with veterinary templates do not require this step as long as the images have been properly placed within the template (it should not be assumed that this is necessarily the case!).
Determining which teeth have been imaged13–15
Key to identifying the imaged teeth on stan- dard film is the embossed dot on one corner of the film. (When exposing a radiograph, if the film is properly positioned, the convex surface will point towards the radiographic tubehead. it is generally not possible to expose a radio- graph with the film in backwards, due to the lead sheet on the ‘back’ side of the film. This is the same with digital systems, as the cord needs to be on the side opposite the tubehead.)
Ensure the dot is facing towards you (this is done automatically on most digital systems), as this will mean you are looking at the teeth as if your eyes are the tubehead. You can then determine whether you are looking at a max- illary or mandibular view:
Maxillary view These films will have nasal turbinates visible, may have a three-rooted tooth (108/208), and will have a radiodense white line running across the canine just dorsal to the premolars (Figure 15).
-
Mandibular view These films will have a large two-rooted molar, and may have a mandibular symphysis, canal or ventral cortex visible (Figure 16).
Next, rotate (don’t flip!) the film so that the roots are in their natural position (upwards on a maxillary view, downwards on a mandibular view). This will orient the image as if the cat was standing in front of you.
Molars and premolars Ascertain mesial from distal (teeth generally get larger going distally). if the mesial side is on the left side of the film, the radiograph is of the left side of the patient; vice versa for the right (Figure 17).
Canines and incisors The film is oriented such that the right side of the mouth is on the left, and left side is on the right (similar to a ventrodorsal abdominal radiograph; Figure 18).
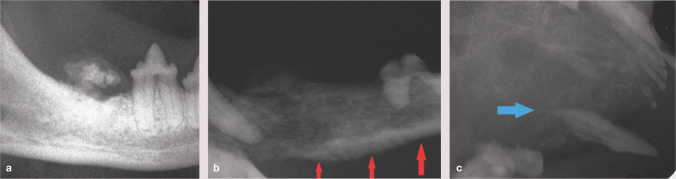
Figure 15.
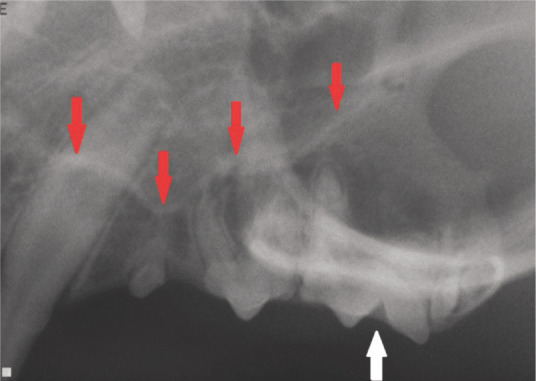
Dental radiograph of the left maxilla of a cat. Note the three-rooted fourth premolar (208; white arrow) and radiodense line (red arrows)
Figure 16.
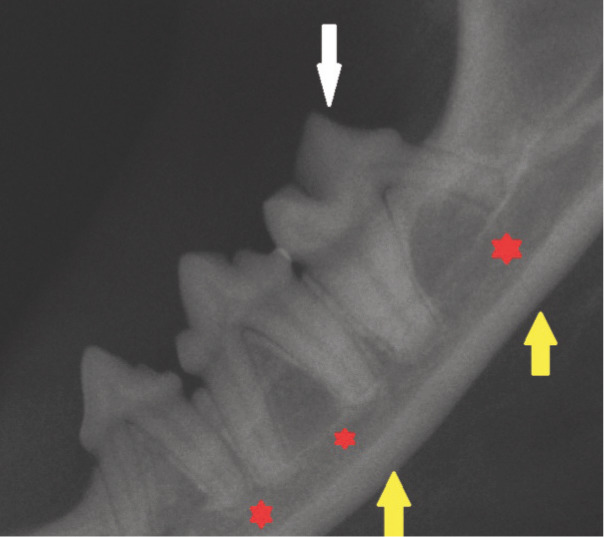
Dental radiograph of the left mandible of a cat. A large two-rooted molar (309; white arrow), the mandibular canal (red stars) and ventral cortex (yellow arrows) can be seen
Figure 17.
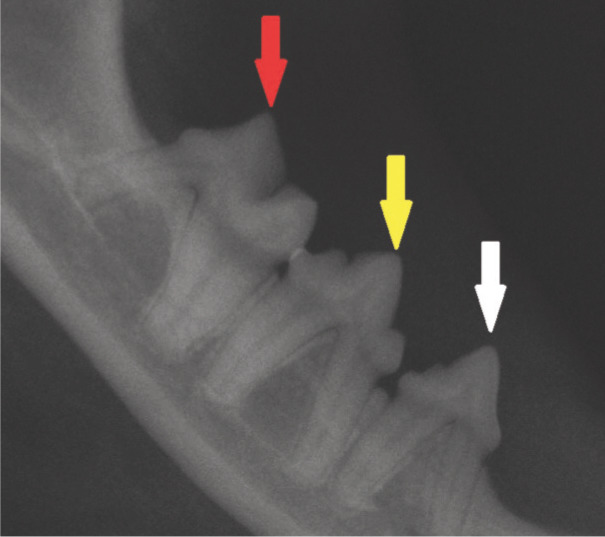
Dental radiograph of the right mandible of a cat. The teeth get larger the further distal they are; white arrow = third premolar (407), yellow arrow = fourth premolar (408), red arrow = first molar (409)
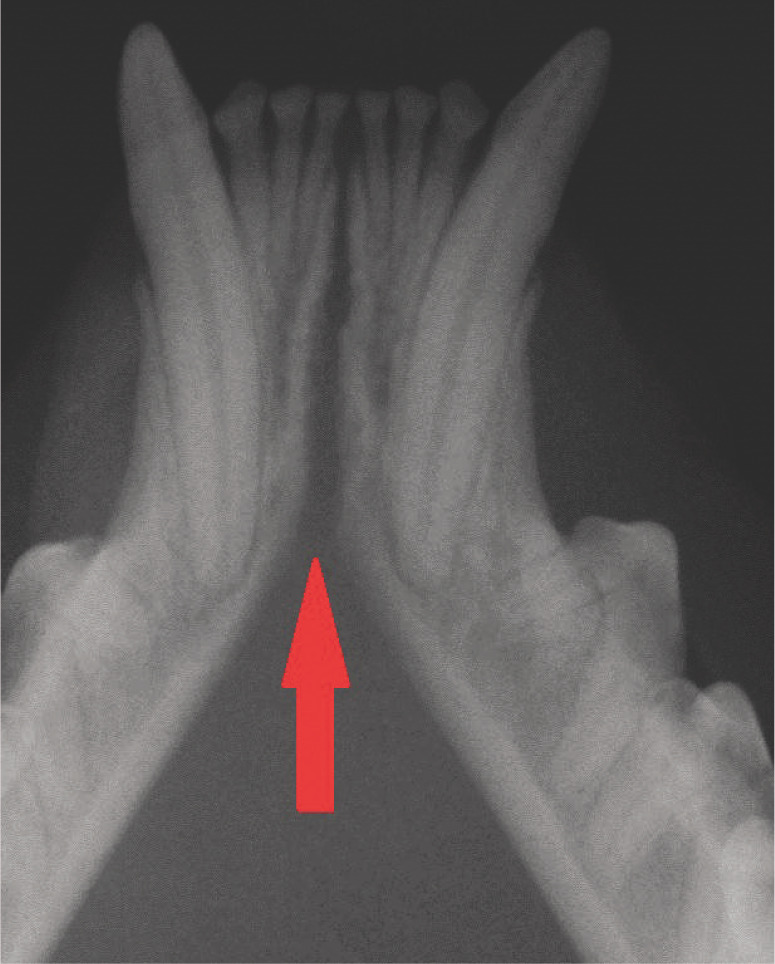
Figure 18.

Dental radiograph of the maxillary incisors of a cat. The red arrow points to the right third incisor (103)
Normal or abnormal?
Most dental pathologies are pretty obvious radiographically. However, there are patholog- ic entities that are unique to the oral cavity and several normal anatomic structures that may mimic pathologic changes (see page 894).
The discussion on pages 895–898 concen- trates on the most common pathologies, which are illustrated by classic examples. in practice, the clinician may be confronted by more ques- tionable cases. Continuing education meetings are invaluable for furthering expertise in radiographic interpretation. in addition, VetdentalRad.com is an excellent resource.
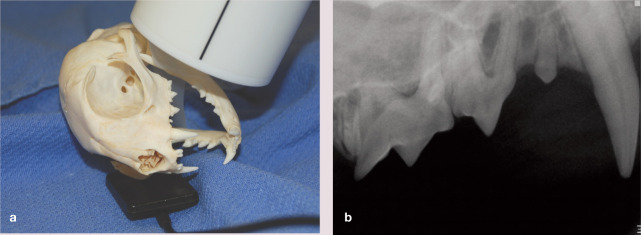
Figure 19.
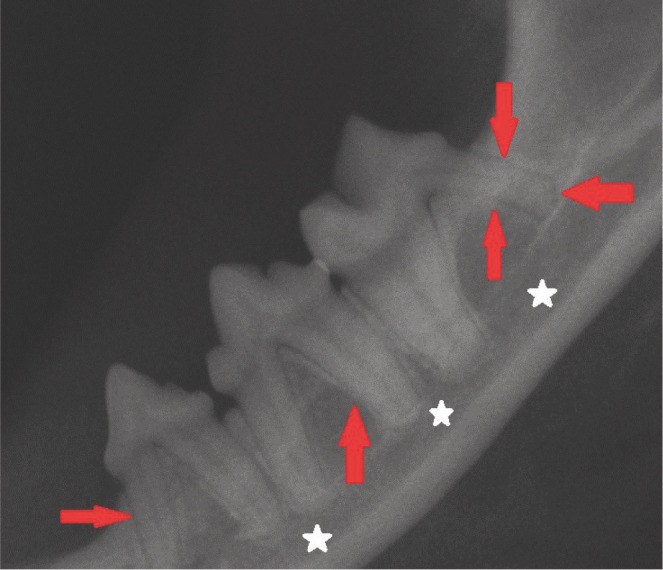
Normal mandibular dental radiograph. The periodontal ligaments appear as thin black lines around all the teeth (red arrows). The mandibular canal is demonstrated by the white stars
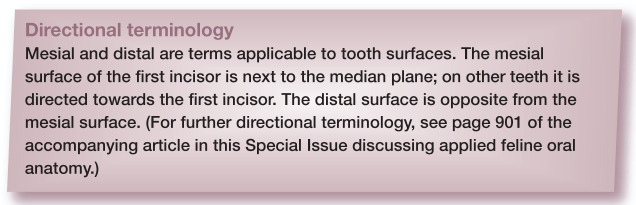
Figure 20.
Normal dental radiograph of the rostral mandible. The central black line (red arrow) is the fibrocartilaginous mandibular symphysis
Figure 21.
Normal dental radiograph of the rostral maxilla. The paired radiolucent areas distal to the intermediate incisors are the palatine fissures (red arrows)
Radiographic appearance of common pathologies
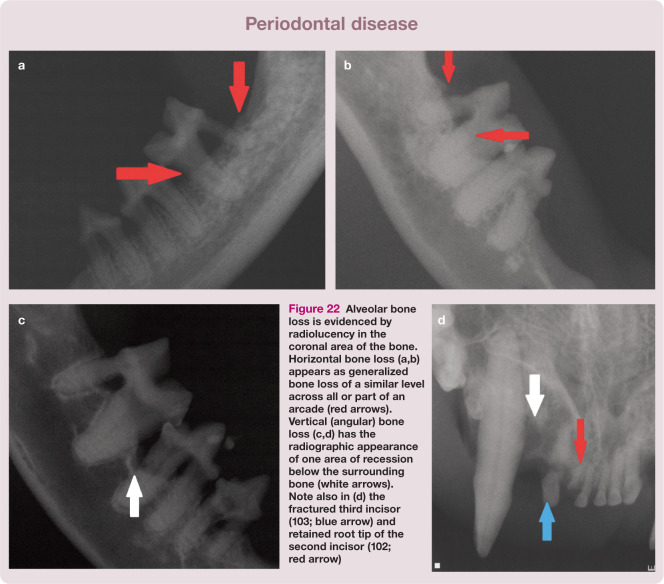
Periodontal disease13,17,18
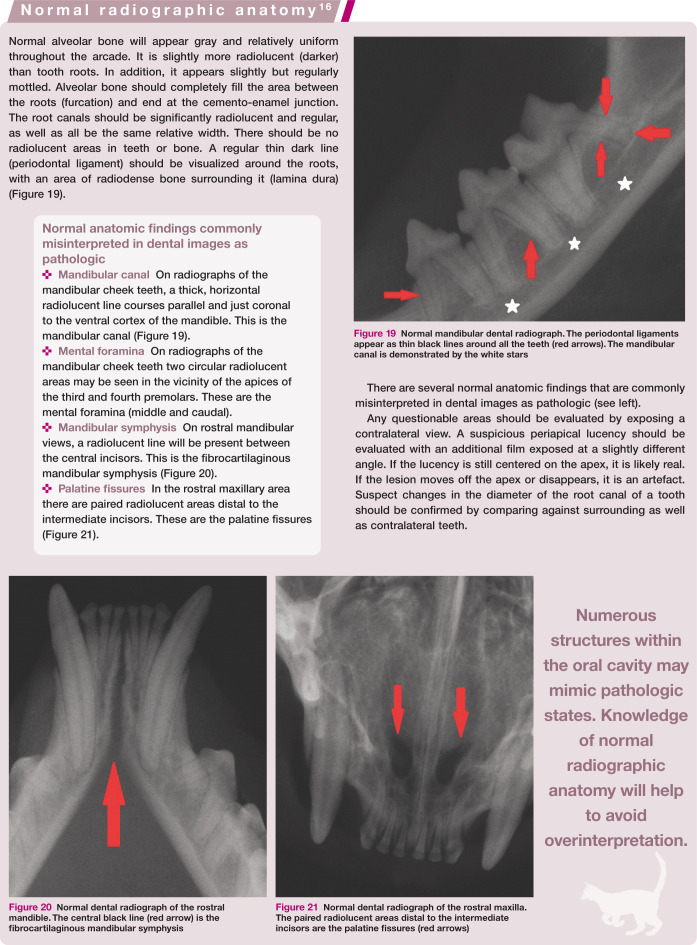
Horizontal bone loss is the most common pattern in veterinary patients with periodon- tal disease. This appears as generalized bone loss of a similar level across all or part of an arcade (Figure 22a,b). The other pattern is angular (vertical) bone loss, whereby one area of recession is visible below the surrounding bone; this is most common on the distal aspect of the mandibular first molar and palatal aspect of the maxillary canine (Figure 22c,d). it is common to have a combination of the two types of bone loss in the same arcade.
Figure 22.
Alveolar bone loss is evidenced by radiolucency in the coronal area of the bone. Horizontal bone loss (a,b) appears as generalized bone loss of a similar level across all or part of an arcade (red arrows). Vertical (angular) bone loss (c,d) has the radiographic appearance of one area of recession below the surrounding bone (white arrows). Note also in (d) the fractured third incisor (103; blue arrow) and retained root tip of the second incisor (102; red arrow)
Bone loss does not become radiographically evident until 30–50% of mineralization is lost. Therefore, radiographic findings will always underestimate bone loss. in addition, bone loss on one surface only (ie, lingual, palatal or facial) may be hidden by superimposition of bone or tooth. This may result in a non- diagnosed bony pocket, and underlines the importance of always interpreting radiographs in the light of the findings of a complete oral examination (see accompanying article in this Special issue on oral examination in the cat).
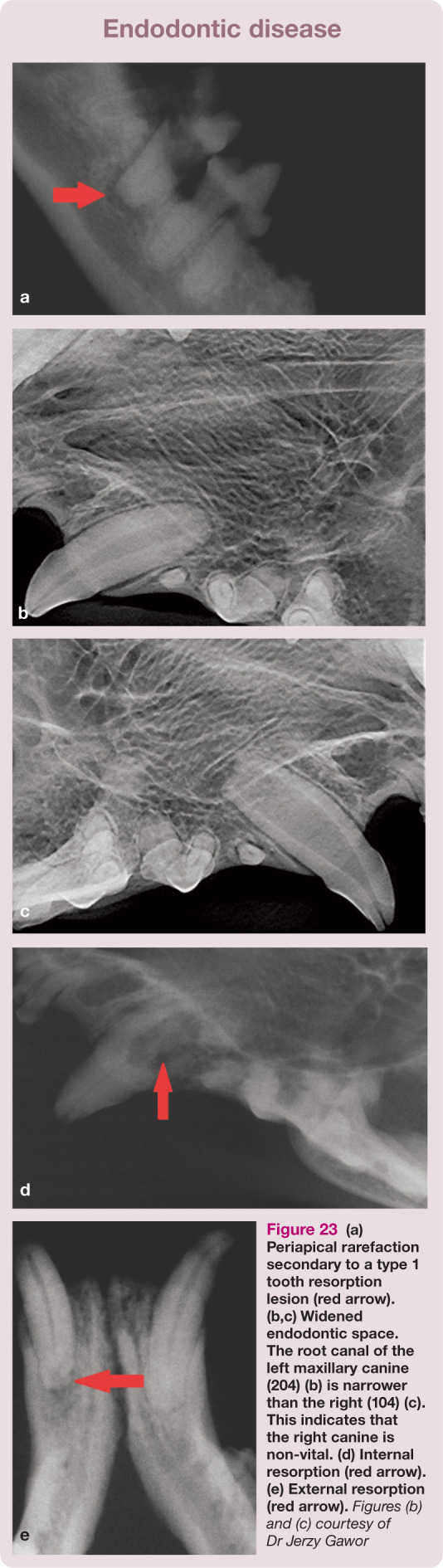
Endodontic disease13,19–22
Endodontic disease refers to any pathology that affects the endodontic system (ie, the root canal or pulp of a tooth). in general, when discussing endodontic disease radiographi- cally it means that the tooth is non-vital and infected. An individual tooth may show one, some or all of the different radiographic changes discussed below. Note, however, that only one of these need be present to establish a presumptive diagnosis of endo- dontic disease.
Radiographic changes can be grouped into two major classifications: changes in the sur- rounding bone, and changes within the tooth itself.
Bony changes The classic and most obvious finding is periapical rarefaction or lucency (Figure 23a). This appears as a radiolucent area surrounding the apex of a root. other, more subtle changes include a widened periodontal ligament, a thickened or discontinuous lamina dura or even periradicular opacities. if any area is in question, it is best to expose an additional film at a slightly different angle. if a periradicular lucency is still centered over the apex, it is more likely to be pathologic.
Tooth changes The most common change in endodontic disease within the tooth itself is a root canal with an altered diameter (Figure 23b,c). As a tooth matures, secondary dentin results in a radiographically visible narrowing of the pulp canal. When a tooth’s pulp becomes non-vital, dentin production stops. Consequently, non-vital teeth have wider root canals than the surrounding vital teeth. Width discrepancy can be gauged by comparing with any tooth (taking the size of tooth into consideration) but is most accurately determined by comparing with the contralateral tooth. Endodontic disease may also manifest radiographically as internal resorption (Figure 23d). This results from osteoclastic activity within the root canal system due to pulpitis. These changes create an irregular, enlarged region within an area of the root canal system. Finally, external root resorption can be seen with endodontic disease (Figure 23e). it will appear as a defect in the external surface of the root, generally accompanied by a loss of bone in the area. External resorption most commonly occurs at the root apex and is actually quite common in cats with chronic endodontic disease.
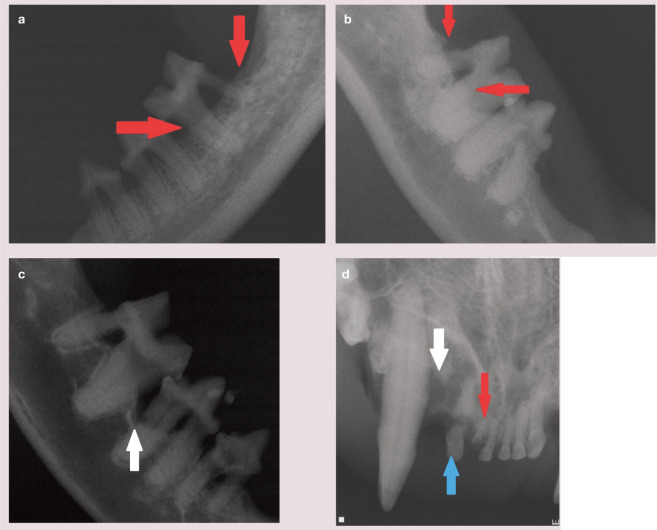
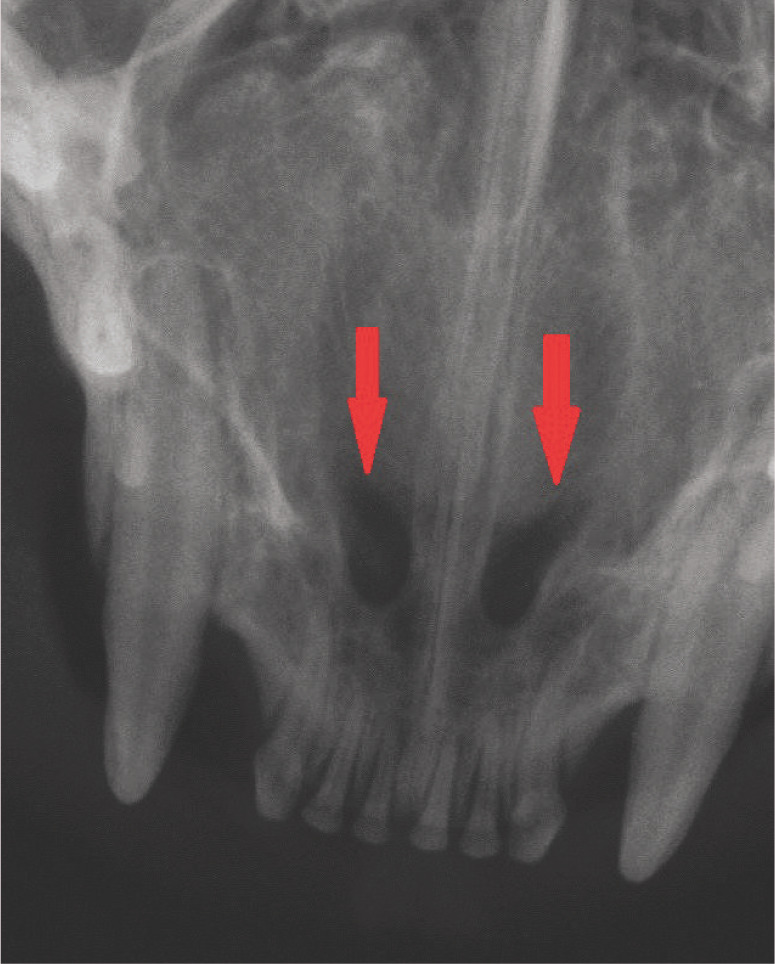
Figure 23.
(a) Periapical rarefaction secondary to a type 1 tooth resorption lesion (red arrow). (b,c) Widened endodontic space. The root canal of the left maxillary canine (204) (b) is narrower than the right (104) (c). This indicates that the right canine is non-vital. (d) Internal resorption (red arrow). (e) External resorption (red arrow). Figures (b) and (c) courtesy of Dr Jerzy Gawor
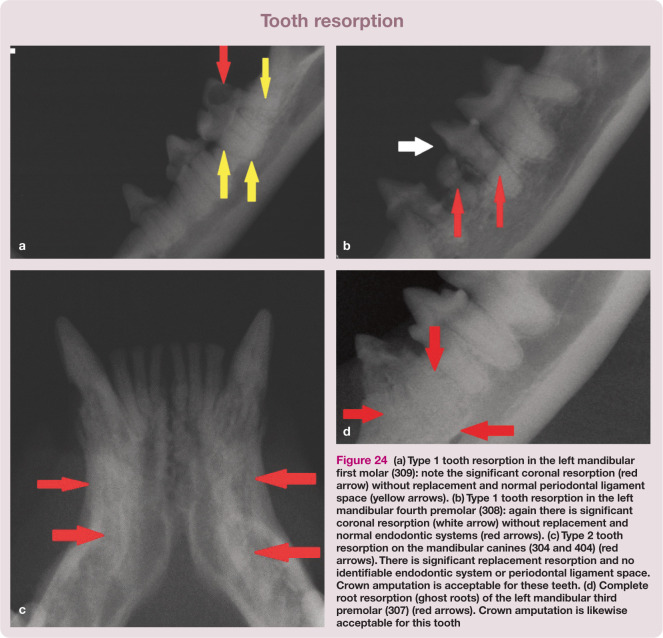
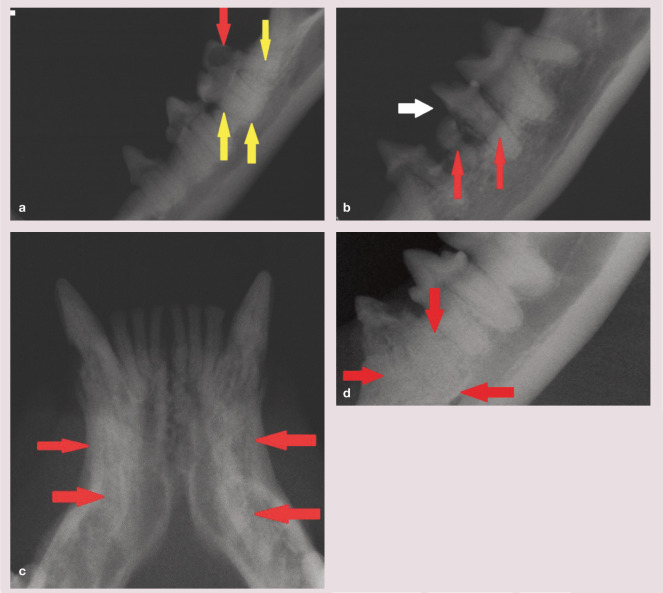
Tooth resorption6,13,18,22–25
Previously known as neck lesions, cervical line lesions, resorptive lesions and feline odonto- clastic resorptive lesions (FoRLs), tooth resorptions are the result of odontoclastic destruction of feline teeth. They are classified as type 1 or type 2; in type 1 resorption there is no replacement by bone, whereas in type 2 there is replacement of the lost root structure by bone. Where both types of lesion occur in the same tooth, this is referred to as type 3 tooth resorption. determining type 1 from type 2 tooth resorption is critical for proper treatment. Complete extraction is always the ideal treatment; however, crown amputation has been proposed as an acceptable treatment for advanced type 2 resorption.24,25
Radiographically type 1 tooth resorptions will show normal root density in some areas and a well defined periodontal space (Figure 24a). in addition, there is often a definable root canal in the intact part of the tooth (Figure 24b). Cats with this type will have significant resorption of the teeth and tooth roots that are not replaced by bone. These teeth must be completely extracted.
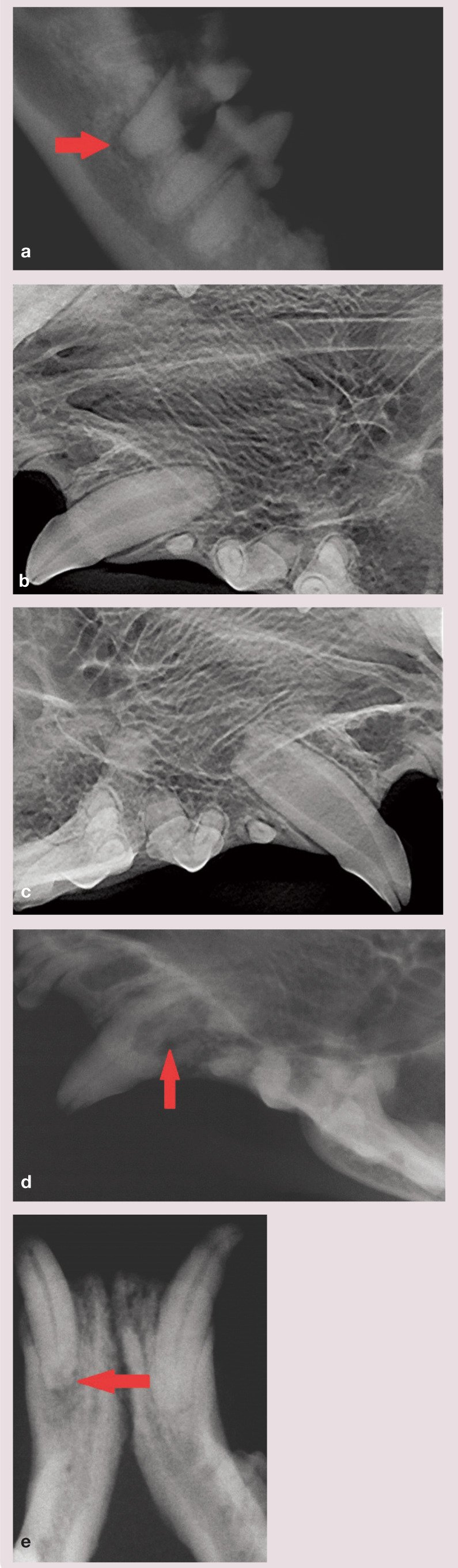
Figure 24.
(a) Type 1 tooth resorption in the left mandibular first molar (309): note the significant coronal resorption (red arrow) without replacement and normal periodontal ligament space (yellow arrows). (b) Type 1 tooth resorption in the left mandibular fourth premolar (308): again there is significant coronal resorption (white arrow) without replacement and normal endodontic systems (red arrows). (c) Type 2 tooth resorption on the mandibular canines (304 and 404) (red arrows). There is significant replacement resorption and no identifiable endodontic system or periodontal ligament space. Crown amputation is acceptable for these teeth. (d) Complete root resorption (ghost roots) of the left mandibular third premolar (307) (red arrows). Crown amputation is likewise acceptable for this tooth.
The radiographic appearance of type 2 tooth resorptions is that of teeth which have a differ- ent radiographic density as compared with normal teeth, as they have undergone signifi- cant replacement resorption (Figure 24c). Findings will include areas with no discernible periodontal ligament space (dentoalveolar ankylosis) or root canal. in the late stages, there will be little or no discernible root structure (ghost roots; Figure 24d). In these cases, the lost root structure will be replaced by bone. Crown amputation is a valid treatment option for these teeth. However, teeth that have evidence of infection (endodontic or periodontal), or have intact root canals or periodontal ligament spaces, should not undergo crown amputation.
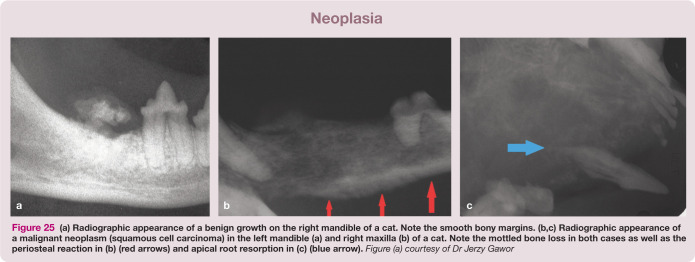
Neoplasia6,26–28
Benign masses Benign neoplastic growths are very rare in cats. If present, most benign growths will have no bony radiographic involvement. If bone involvement does occur it will typically be expansive, resulting in the bone ‘pulling away’ from the advancing tumor leaving a decalcified soft tissue filled space in the tumor site (Figure 25a). Bony margins are usually distinct and there will typically be tooth movement.
Malignant neoplasia Malignant oral neoplasms usually invade bone early in the course of disease, resulting in irregular, ragged bone destruction (Figure 25b). initially, the bone will have a mottled ‘moth-eaten’ appearance, but radiographs obtained late in the disease course (Figure 25c) will reveal a complete loss of bone (the teeth will appear to float in space). if the cortex is involved, an irregular periosteal reaction will be seen (Figure 25b).
Figure 25.
(a) Radiographic appearance of a benign growth on the right mandible of a cat. Note the smooth bony margins. (b,c) Radiographic appearance of a malignant neoplasm (squamous cell carcinoma) in the left mandible (a) and right maxilla (b) of a cat. Note the mottled bone loss in both cases as well as the periosteal reaction in (b) (red arrows) and apical root resorption in (c) (blue arrow). Figure (a) courtesy of Dr Jerzy Gawor.
Histopathologic testing is always necessary for accurate diagnosis of oral masses since a variety of benign and malignant tumors appear radiographically similar and aggres- sive tumors will show no bone involvement early in the course of disease.
Key Points
The information gained from dental radiography is critical for proper diagnosis and therapy in feline dentistry.
Dental radiographs should, however, be considered an adjunct to, and not a substitute for, a thorough oral examination.
Digital systems, while initially more expensive, will be more efficient and will save money over time.
Almost all dental radiographs can be made using only three angles: 20º, 45º and 90º.
Never ‘flip’ digital radiographs as this will create a mirror image and confuse the interpretation of the arcade imaged.
Dental radiographs always underestimate the level of bone loss.
Only advanced type 2 tooth resorptions can be treated with crown amputation
Malignant neoplasms tend to eat the bone away around the teeth and leave them in place.
Footnotes
Funding: The author received no specific grant from any funding agency in the public, commercial or not- for-profit sectors for the preparation of this article.
The author declares that there is no conflict of interest.
- Woodward TM and Niemiec BA. Dental radiology simplified. An instructional video. www.vetdentalrad.com/products/dvd (2007)
- Niemiec BA and Woodward TM. The importance of dental radiographs. Client educational poster. www.vetdentalrad.com/products/poster/ (2008)
- Niemiec BA. Veterinary dental radiography. in: Niemiec BA (ed). Small animal dental, oral and maxillofacial disease, a color handbook. London: Manson, 2010, pp 63–87.
- Dupont GG and debowes LJ. Atlas of dental radiography in dogs and cats. St Louis, Mo: Elsevier, 2009.
References
- 1. Niemiec BA. Case based dental radiology. Top Companion Anim Med 2009; 24: 4–19. [DOI] [PubMed] [Google Scholar]
- 2. Woodward TM. Dental radiology. Top Companion Anim Med 2009; 24: 20–36. [DOI] [PubMed] [Google Scholar]
- 3. Niemiec BA, Sabitino d, Gilbert T. Equipment and basic geometry of dental radiography. J Vet Dent 2004; 21: 48–52. [PubMed] [Google Scholar]
- 4. Mulligan TW, Aller MS, Williams CA. Atlas of canine and feline dental radiology. Trenton: Veterinary Learning Systems, 1998. [Google Scholar]
- 5. Niemiec BA. Digital dental radiography. J Vet Dent 2007; 24: 192–197. [DOI] [PubMed] [Google Scholar]
- 6. Niemiec BA. Veterinary dental radiology. In: Niemiec BA. (ed). Small animal dental, oral and maxillofacial disease, a color handbook. London: Manson, 2010, pp 63–77. [Google Scholar]
- 7. Holmstrom SE, Frost P, Eisner ER. Veterinary dental techniques. 2nd ed. Philadelphia; WB Saunders, 1998. [Google Scholar]
- 8. Wiggs RB, Lobprise HB. Veterinary dentistry: principles and practice. Philadelphia; Lippincott– Raven, 1997. [Google Scholar]
- 9. oakes A. Introduction: radiology techniques. In: Deforge DH, Colmery BH. (eds). An atlas of veterinary dental radiology. Ames; Iowa State University Press, 2000. [Google Scholar]
- 10. Niemiec BA, Furman R. Feline dental radiology. J Vet Dent 2004; 21: 252–257. [PubMed] [Google Scholar]
- 11. Gracis M. Radiographic study of the maxillary canine tooth of four mesaticephalic cats. J Vet Dent 1999; 16: 115–128. [DOI] [PubMed] [Google Scholar]
- 12. Niemiec BA, Sabitino d, Gilbert T. Developing dental radiographs. J Vet Dent 2004; 21: 116–121. [PubMed] [Google Scholar]
- 13. Niemiec BA. Dental radiographic interpretation. J Vet Dent 2005; 22: 53–59. [PubMed] [Google Scholar]
- 14. Verstraete FJ. Self-assessment color review of veterinary dentistry. Ames; Iowa State University Press, 1999. [Google Scholar]
- 15. Woodward TM. Interpretation of dental radiographs. Top Companion Anim Med 2009; 24: 37–43. [DOI] [PubMed] [Google Scholar]
- 16. Aller MS. Normal feline radiographic anatomy. In: deforge dH, Colmery BH. (eds). An atlas of veterinary dental radiology. Ames: Iowa State University Press, 2000, pp 117–134. [Google Scholar]
- 17. Gawor J. Dental radiology for periodontal disease. In: Niemiec BA. (ed). Veterinary periodon- tology. Ames: Wiley-Blackwell, 2013, pp 107–128. [Google Scholar]
- 18. Lyon KF, Visser CJ, okuda A, et al. Feline stom- atitis syndrome, periodontal disease, and feline odontoclastic resorptive lesions. In: Deforge DH, Colmery BH. (eds). An atlas of veterinary dental radiology. Ames; Iowa State University Press, 2000, pp 177–198. [Google Scholar]
- 19. Niemiec BA. Fundamentals of endodontics. Vet Clin North Am Small Anim Pract 2005; 35: 837– 868. [DOI] [PubMed] [Google Scholar]
- 20. Glickman GN, Pileggi R. Preparation for treatment. In: Cohen S, Burns RC. (eds). Pathways of the pulp. 8th ed. St Louis, Mo: Mosby, 2002, pp 103–145. [Google Scholar]
- 21. Anthony JMG, Marretta SM, okuda A. Feline endodontics. in: deforge dH, Colmery BH. (eds). An atlas of veterinary dental radiology. Ames: Iowa State University Press, 2000, pp 149–158. [Google Scholar]
- 22. dupont G. Pathologies of the dental hard tissues. In: Niemiec BA. (ed). Small animal dental, oral and maxillofacial disease, a color handbook. London: Manson, 2010, pp 128–159. [Google Scholar]
- 23. DuPont GA. Radiographic evaluation and treatment of feline dental resorptive lesions. Vet Clin North Am Small Anim Pract 2005; 35: 943–962. [DOI] [PubMed] [Google Scholar]
- 24. DuPont G. Crown amputation with intentional root retention for advanced feline resorptive lesions – a clinical study. J Vet Dent 1995; 12: 9–13. [PubMed] [Google Scholar]
- 25. DuPont GA. Crown amputation with intentional root retention for dental resorptive lesions in cats. J Vet Dent 2002; 19: 107–110. [PubMed] [Google Scholar]
- 26. Sarkiala-Kessel AM, Revenaugh AF. Feline oral neoplasia. In: Deforge DH, Colmery BH. (eds). An atlas of veterinary dental radiology. Ames: Iowa State University Press, 2000, pp 159–170. [Google Scholar]
- 27. Niemiec BA. Oral pathology. Top Companion Anim Med 2008; 23: 59–71. [DOI] [PubMed] [Google Scholar]
- 28. Dhaliwal R. Malignant oral neoplasia. In: Niemiec BA. (ed). Small animal dental, oral and maxillofacial disease, a color handbook. London: Manson, 2010, pp 225–235. [Google Scholar]