SUMMARY
Accuracy of burn size estimation is critical in acute burn management because it directly affects the patient’s outcome and prognosis. This study aims to quantify the discrepancies of total body surface area (TBSA) burned between the burn unit (TBSAb) and the referring facilities (TBSAr). Data of all referred adult and paediatric patients admitted to the Hospital Universiti Sains Malaysia Burn Unit within 24 hours post burn were retrospectively reviewed from 2015 to 2019. %TBSA discrepancies were calculated by the differences between TBSAb and TBSAr. A total of 208 patients (111 adults and 97 paediatric patients) were recruited in this study. Of these, the TBSA was overestimated in 60.58% cases, underestimated in 13.46% cases, accurate in 7.69% cases, and in 18.27% cases the referrals had no TBSAr stated. The %TBSA discrepancy was the highest in severe burns (mean 10.80% in adults and 7.59 in paediatric patients; P<0.001). The time interval between referral and reassessment and patients’ body mass index (BMI) were not statistically significant for the magnitude of TBSA discrepancy. The number of burn areas involved correlated with the %TBSA discrepancies, with the highest recorded discrepancy being 21.50% in whole body involvement. There were significant discrepancies in TBSA estimations between the referring facilities and those of the Hospital Universiti Sains Malaysia (USM) burn unit, especially among the paediatric patients and those with severe burns. Implementation of educational programs by burn care experts and agreement on a universal method of TBSA assessment are necessary in reducing the discrepancies.
Keywords: total burn surface area, discrepancy, overestimation, underestimation
RÉSUMÉ
L’estimation précise de la surface brûlée est cruciale dans la prise en charge des patients. Cette étude a évalué les différences d’évaluation de SB selon sa réalisation en CTB (CTB) ou ailleurs (A). Les données de tous les patients (111 adultes et 97 enfants) hospitalisés entre 2015 et 2019, dans les 24h suivant leur brûlure, dans le CTB du CHU Universiti Sains Malaysia ont été revues rétrospectivement. L’estimation A n’était correcte que dans 7,69% des cas. Elle était exagérée dans 60,58% des cas, minorée dans 13,46% et absente dans 18,27%. L’erreur était plus nette (10,8% chez les adultes, 7,59% chez les enfants) en cas de brûlure grave. Le BMI et la durée entre les évaluations A et CTB n’entraient pas en ligne de compte. L’erreur augmentait avec le nombre de régions touchées, pour atteindre 21,5% si toutes comportaient une brûlure. Ces constatations nous amènent à proposer des actions d’éducation dispensées par des brûlologues et l’acceptation par tous d’une méthode unique de calcul de la SB.
Mots-clés: surface brûlée, différences, surestimation, sous-estimation
Introduction
Hospital Universiti Sains Malaysia (USM) is a tertiary center with a specialized burn unit. We receive burn referrals from the Kelantan state, with a population of 2 million spanning across 17,100 km2, and occasionally from neighboring states. A five-year retrospective study performed in the burn unit of Hospital USM showed 485 inpatient and outpatient burn cases.1
Harish and colleagues reported that TBSA is overestimated in burn injuries of all severities. Underestimations are less frequent, but the chance rises with an increase in the time interval after burn injury and with an increase in TBSA. However, severe burns of more than 20% TBSA are more accurately estimated. The inaccuracies in burn size assessment directly influence the treatment, which may cause over- or under-resuscitation fluid regime and inappropriate referral to specialized burn units.2
Overestimation of TBSA leads to undue fluid resuscitation and therefore results in pulmonary edema, compartment syndrome, and an increased need for escharotomy.3 “Fluid creep” caused by excess fluid resuscitation is associated with abdominal compartment syndrome.4 It can also result in inappropriate transfers to the burn unit, unnecessary consumption of healthcare resources, and psychological burden to the patients and their families.5 Conversely, underestimation of TBSA can lead to inadequate fluid resuscitation, which could result in circulatory collapse and renal failure, ultimately progressing to burn shock, apart from the progression of burn depth, increasing the need for escharotomy, fasciotomy and skin grafting.6
Several studies have emphasized inaccuracies in TBSA assessment by referring facilities; however, the trend for inaccuracy seems to be inconsistent. Some authors have found that smaller burns have a tendency to be overestimated and larger burns a tendency to be underestimated, while others have found a general tendency for overestimation in burn injuries of all severities.
Most previous studies, however, do not report a time frame or they only involved either adult or paediatric populations.6,7 Additionally, the correlation between body mass index (BMI) and areas of burn injuries with the accuracy of burn size estimation in both adult and paediatric burn patients has not been reported.
Following burn injury, evaluation of the %TBSA and burn depth assessment will determine appropriate fluid resuscitation and wound management. %TBSA estimation plays an important role in early burn management and is one of the criteria for the decision on hospitalization or outpatient care. According to the World Health Organization (WHO) 2004, criteria for burn injuries requiring hospitalization include %TBSA greater than 15% for adults; %TBSA greater than 10% for paediatrics; any burn in the very young, the elderly, or the infirm; full-thickness burn; burn involving special regions; circumferential burn; inhalational injury; and burn with associated trauma or underlying medical illness.8
Discrepancies in %TBSA between referring centers and specialized burn units have been reported.2,9,10 Minor burns tend to be overestimated whereas larger burns are underestimated.11 Errors in estimating %TBSA can be potentially fatal and can lead to unnecessary ambulance transfers and inconvenience for the patients.12
%TBSA determines the volume needed for early fluid resuscitation following acute burn injury. Burns over 15% TBSA in adults and 10% TBSA in paediatrics require fluid resuscitation as systemic inflammatory response syndrome (SIRS) is initiated and there is massive fluid shift resulting in burn oedema and burn shock if adequate volume is not given.13 In fact, the inflammatory response in burns can be worse than that of trauma and sepsis. Burn shock is a combination of distributive, cardiogenic, and hypovolemic shock. Therefore, it is imperative to replace the fluid in the intravascular compartment in order to preserve tissue perfusion of vital organs.14,15
The Parkland formula, which is commonly used in the determination of resuscitation fluid volume, carries the TBSA estimated by the clinician. The formula is as follows: 4 mL × %TBSA × patient’s weight (kg) = total fluid in the first 24 hours, with 50% of the total volume administered in the first 8 hours and the rest in the next 16 hours.16 Over the years, the accuracy of various guidelines has been questioned.17-19 Many other formulas have been reported to provide more precise fluid resuscitation volumes, such as the Brooke formula, the Evans formula, the Shriner’s Cincinnati formula for paediatrics, the Muir-Barclay formula, and the Monafo formula.20-23 In Hospital USM, the Parkland formula is used as a guideline to determine fluid requirement in the first 24 hours.
The difference in burn size assessment between adult and paediatric age groups can be seen when the paediatrics have a lower threshold for starting fluid resuscitation volume due to their different %BSA in their different developmental stages. Chan and colleagues have described a tendency for overestimation of %TBSA by a mean of 10.5% among the paediatric population.6 In another study, only 60% of paediatric patients referred to a burn unit with a TBSA of >10% were similarly assessed as having >10% TBSA by the burn unit, resulting in almost half of the children enduring unnecessary treatments and transfers.24 Reasons for the discrepancies are inclusion of simple erythema and the use of different calculation methods (Wallace Rule of Nine, Rule of Palm, and the Lund and Browder chart). The zone of hyperemia should not be included in the TBSA calculation since these are areas of vessel dilatation induced by inflammatory mediators.6
The most commonly used methods for %TBSA calculation are the Rule of Nine, Rule of Palm, and the Lund and Browder chart, all of which utilize the BSA with no variations made according to body weight. In obese patients, the Du Bois and Du Bois formula underestimates the BSA in obese patients by 20%.25 Furthermore, individuals with a higher muscle composition may mistakenly be classified as overweight or obese as the BMI does not distinguish between the weight of muscles and fat.26 Hand surface area reduces remarkedly as BMI increases, and this is found to be more evident in women, particularly those with a BMI greater than 31 kg/m2 in which the hand surface area represents only 0.64%.27
Larger areas of burn injuries also make it more difficult for healthcare providers to estimate the %TBSA, adding to calculation discrepancies. In both the Rule of Nine and the Lund and Browder chart, the area of the trunk lacks sufficient landmarks for precision calculation, whereas the hands, feet and head are too small to allow precise recording.28
The purpose of this study was to compare the estimation of TBSA by the referring hospital or the emergency departments (TBSAr) and that of the Hospital USM burn unit (TBSAb) in both adult and paediatric burn patients requiring treatment or transfer to a specialized burns unit. We hypothesize that BMI, time following burn injuries, and number of burn areas affect TBSA discrepancies.
Methods
Research design
We conducted a retrospective review of 208 inpatients referred to the burn unit of Hospital USM from January 2015 to December 2019. The case files of all adult and paediatric burn inpatients were analyzed, and the TBSAr was compared with the TBSAb.
All referrals within 24 hours of burn injury and patients who sought medical attention after the incident within 24 hours were included in this study. Additional data collected included the patients’demographic data (age, sex, residential address, height, weight, comorbidity, mechanism and area of burn injury, presence of inhalational injury, duration of hospitalization, time of burn injury, time of referral, time of reassessment at the burn unit, method of %TBSA assessment during referral, choice of fluid for resuscitation, depth of burn recorded during referral and reassessment, and whether surgical intervention was needed.
%TBSA discrepancy
The discrepancy in burn size estimated by the referring facilities (TBSAr) and the burn unit (TBSAb) was calculated by:
| %TBSA Discrepancy = TBSAr - TBSAb |
The %TBSA discrepancy was categorized into ‘overestimation,’ ‘underestimation,’ ‘perfect accuracy,’ and ‘TBSAr not stated.’ The categories ‘overestimation’and ‘underestimation’ were further grouped into 5%, 6-10%, 11-15%, 16-20%, and >20% for secondary variable analysis. TBSAb was used as a reference point of accuracy in all analyses.
Burn severity
Burn severity was categorized into three groups based on the TBSAb. According to the Burn Severity Grading System by the American Burn Association (ABA) for burn injury, paediatric patients have a lower threshold of %TBSA for major burn.29 In adults, the groups were minor burn (<10%), moderate burn (10-20%), and major burn (>20%). Paediatrics (to 12 years old) were divided into similar groups with different TBSAb values, namely minor burn (<5%), moderate burn (5-10%), and major burn (>10%). The mean and standard deviation (SD) for the %TBSA discrepancy in each burn severity group were calculated. The Pearson correlation test was used to assess the significance of discrepancy.
Time following burn injury
Time of burn injury, time of referral, and time of reassessment by the burn unit staff were recorded from the case files. The time elapsed between injury to referral and the time interval between referral and reassessment were further calculated in hours and minutes (hh:mm) using Microsoft Excel. Patients who presented more than 24 hours after the initial injuries were excluded from this study.
The time interval between referral and reassessment was further categorized into: <5 hours, 5-10 hours, and >10 hours. The significance between the time interval groups with the %TBSA discrepancy was calculated using one-way ANOVA. The mean time spent between burn injury to referral was calculated.
Body mass index (BMI)
For adults, the BMI (kg/m2) was calculated from height and weight, and the patients were categorized into four groups based on the BMI categories from the WHO Asian BMI cut points: <18.5 or underweight, 18.5-22.9 or normal weight, 23-27.4 or overweight, and ≥27.5 or obese.30 The mean and SD for %TBSA discrepancy in each category were calculated and correlated with results of the one-way ANOVA.
For paediatrics younger than 2 years, obesity was defined as ≥97th percentile, overweight as ≥85th percentile, underweight as ≤15th percentile, and severely underweight ≤3rd percentile for weight-for-age.31
The BMI for older patients in this group (≥2 years of age) was calculated using a standard equation: weight in kilograms divided by height in meters squared (kg/m2), with age- and gender-appropriate cut-offs applied according to the Centers for Disease Control algorithms.32
Number of burn areas
Areas of burn were divided into six categories: upper limbs, lower limbs, trunk (front), trunk (back), head and neck, and genitalia. For the upper and lower limbs, unilateral involvement and bilateral involvement were both considered as one area. The mean and SD for %TBSA discrepancy in each category were calculated and correlated with Spearman’s rho correlation test.
Statistical analysis
Data entry was done using Microsoft Excel Version 16.45 (21011103) and statistical analysis with IBM® SPSS® Statistics version 27. Descriptive statistics were used to summarize the socio-demographic characteristics of the patients. The data obtained are expressed as the mean with SD for numerical variables and frequency (n) with percentage (%) for categorical variables.
Categorical data included %TBSA discrepancy (overestimation, underestimation, perfect accuracy), burn severity (minor, moderate, major), time interval between referral and reassessment (<5 hours, 5-10 hours, >10 hours), BMI (underweight, normal weight, overweight, obese), number of burn areas (one, two, three, four, five, six), method of TBSAr assessment (Lund and Browder, Rule of 9, Palm method, sketch on 2D print stamp, hand drawn method, photo sharing, not stated), and length of hospitalization (<24hours, 1 to 10 days, 11 to 20 days, 21 to 30 days, >30 days). Statistical significance was defined as P < 0.05.
Pearson correlation test was utilized to compare TBSA discrepancies among the burn severity groups. One way ANOVA was used for correlations between both the BMI categories and the time interval between referral and reassessments. Spearman’s rho test was applied for correlation between the number of burn areas and the TBSA discrepancies.
Ethical approval
This study protocol has been reviewed and granted approval by The Human Research Ethics Committee of USM (JEPeM). The assigned study protocol code is USM/JEPeM/19120888.
Results
Demographic data
Over the five years, there were a total of 247 burn injuries referred and managed as inpatient cases in the Hospital USM burn unit. Of the included 208 burn inpatients, 97 (46.63%) patients were adults, and 111 (53.37%) patients were from the paediatric group (Table I). Two mortalities were reported in cases of inhalational injuries.
Table I.
Patients’ demographic data (n=208)
| Variables | Paeds, N=111 | Adults, N=97 | ||
|---|---|---|---|---|
| Mean (SD) | N (%) | Mean (SD) | N (%) | |
| Age | 3.88 (3.82) | 35.27 (16.83) | ||
| Height | 0.92 (0.27) | 1.63 (0.12) | ||
| Weight | 15.52 (9.04) | 63.89 (13.37) | ||
| BMI | - | 24.51 (8.16) | ||
| Mechanism of burn | ||||
| Contact | 9 (8.11) | 4 (4.12) | ||
| Electrical | 4 (3.60) | 4 (4.12) | ||
| Flame | 14 (12.61) | 29 (29.90) | ||
| Flash | 12 (10.81) | 32 (32.99) | ||
| Scald | 72 (64.86) | 25 (25.77) | ||
| Cold | 0 (0.00) | 0 (0.00) | ||
| Chemical | 0 (0.00) | 3 (3.09) | ||
| Radiation | 0 (0.00) | 0 (0.00) | ||
| Friction | 0 (0.00) | 0 (0.00) | ||
| TBSAb | 6.88 (6.70) | 11.25 (14. 51) | ||
A feature of bimodal peaks was observed in the age distribution of burn patients, with 98 (47.11%) out of 208 burn injury patients in the younger age group less than 11 years old. Another peak was seen in the age group of 61 to 70 years (Fig. 1).
Fig. 1.
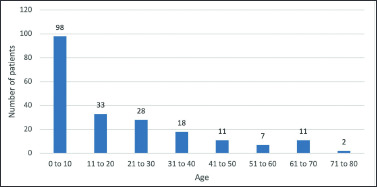
Age distribution of patients
In adults, minor burn injuries are those with TBSAb less than 10%; moderate burn injuries with TBSAb between 10 and 20%, and severe burn injury with TBSAb more than 20%. For adults, 67 (69.07%) patients had minor burn injuries, and 30 (30.93%) patients had moderate and severe burn injuries.
In paediatrics, minor burn injuries are those with TBSAb less than 5%, moderate burn injuries with TBSAb between 5 and 10%, and severe burn injuries with TBSAb more than 10%. For paediatrics, 54 (48.65%) patients had minor burn injuries, 34 (30.63%) patients had moderate burn injuries, and 23 (20.72%) patients had severe burn injuries. The mean TBSAb was 11.25% for adults and 6.88% for paediatrics.
The commonest mechanism of burn injury for paediatrics was scald injuries (64.86%), followed by flame injuries (12.61%), flash burn injuries (10.81%), contact burn (8.11%), and electrical burn (3.6%). For adults, the most prevalent mechanism of burn injuries was flash burn (32.99%), followed by flame burn (29.90%), scald injury (25.77%), electric and contact burn (4.12%), and chemical burn (3.09%). None of the patients had friction, cold or radiation burns (Table I).
%TBSA discrepancy between the referring centers and the burn unit in adult and paediatric patients
A total of 126 (60.58%) burn cases were overestimated by the referring centers, whereas 28 (13.46%) cases were underestimated. Up to 16 (7.69%) cases had the same agreed TBSA by the referring centers and the burn unit. As many as 38 (18.27%) referrals had no TBSAr stated (Fig. 2).
Fig. 2.
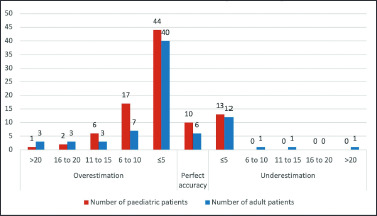
%TBSA discrepancy between referring centres and the burn unit in adult and paediatric patients
%TBSA discrepancy between minor, moderate and major burns
There were significant differences between minor, moderate and major burns in both adult and paediatric patients with %TBSA discrepancy (P < 0.001) (Table II). The mean %TBSA discrepancy was 3.30±3.21, 3.93±5.98, and 10.80±9.05 for minor, moderate, and major burns, respectively in adults, and 3.02±2.93, 3.39±3.57, and 7.59±6.81, respectively in paediatrics. The %TBSA discrepancy significantly increased with an increase in burn severity (P < 0.001) (Table II).
Table II.
Comparison %TBSA discrepancy with burn severity in adult and paediatric patients
| Variables | %TBSA discrepancy Mean (SD) | TBSAb Mean (SD) | P valuea |
|---|---|---|---|
| Burn severity for adults | |||
| <10% or minor burn | 3.30 (3.21) | 4.03 (2.71) | |
| 10-20% or moderate burn | 3.93 (5.98) | 14.33 (3.19) | < .001 |
| >20% or major burn | 10.80 (9.05) | 37.50 (18.33) | |
| Burn severity for paediatrics | |||
| <5% or minor burn | 3.02 (2.93) | 2.04 (1.15) | |
| 5-10% or moderate burn | 3.39 (3.57) | 7.38 (1.45) | < .001 |
| >10% or major burn | 7.59 (6.81) | 17.52 (6.50) |
a Pearson correlation test was applied
%TBSA discrepancy between different groups of BMI and time interval between referral and reassessment
There were no correlations between both BMI and time interval between referral and reassessment with %TBSA discrepancy, with P values of 0.508 and 0.887, respectively (Table III). Of the 208 burn patients, 174 (83.65%) sought medical attention within the first 5 hours of the incident (Table III).
Table III.
Comparison %TBSA discrepancy between different groups of BMI and time interval between referral and reassessment
| Variables | % TBSA discrepancy Mean (SD) | No. of patients (n=208) | P valuea |
|---|---|---|---|
| Adult BMI category | |||
| <18.5 or underweight | 4.87 | 10 | |
| 18.5-22.9 or normal weight | 5.19 | 33 | |
| 23-27.4 or overweight | 5.88 | 33 | 0.284 |
| ≥27.5 or obese | 3.18 | 21 | |
| Paediatric weight category | |||
| Severely underweight | 0.75 | 4 | |
| Underweight | 5.44 | 20 | |
| Normal weight | 4.82 | 58 | 0.280 |
| Overweight | 3.50 | 14 | |
| Obese | 2.13 | 15 | |
| Time interval between referral and reassessment (hours) | |||
| <5 | 4.71 (6.01) | 0.887 | |
| 5-10 | 5.57 (6.46) | ||
| >10 | 5.50 (0.00) |
a One way ANOVA was applied
%TBSA discrepancy and the number of burn areas
Areas of burn were allocated into six groups: upper limbs, lower limbs, trunk (front), trunk (back), head and neck, and genitalia. For each area involved, one point was assigned. Thus, whole body involvement yields the maximum score of six. Out of 208 patients, 94 (45.19%) patients had one burn injury area, 58 (27.88%) had two areas affected, 41 (19.71%) had three areas affected, 12 (5.77%) had four burn areas, two (0.96%) had five areas affected, and 1 (0.48%) patient had whole body involvement. There was a significant correlation between %TBSA discrepancy and the number of burn areas (P < 0.001) (Table IV). The %TBSA discrepancy also increased with an increase in the number of areas burned (Table IV).
Table IV.
Comparison %TBSA discrepancy number of burn areas.
| Variables | Number of patients N (%) | % TBSA discrepancy Mean (SD) | P valuea |
|---|---|---|---|
| Number of burn areas | < .001 | ||
| 1 | 94 (45.2) | 2.88 (3.69) | |
| 2 | 58 (27.9) | 4.04 (3.33) | |
| 3 | 41 (19.7) | 5.68 (6.81) | |
| 4 | 12 (5.8) | 10.25 (8.22) | |
| 5 | 2 (1.0) | 8.50 (4.95) | |
| 6 | 1 (0.5) | 21.50 (0.00) |
a Spearman’s rho correlation test was applied
Method of TBSA assessment
In both adult and paediatric patients, hand drawings on the referral letters were the most used method for TBSA assessment, which accounted for 29.90% and 33.33% cases, respectively. Only 20.62% of adult referrals and 15.32% of paediatric referrals utilized the Lund and Browder chart. Up to 24.74% of adult referrals and 18.92% of paediatric referrals did not state the method of TBSA assessment (Table V).
Table V.
Method of TBSA assessment in adult and pediatric burn patients
| Variables | Number of adult patients (n=97) N (%) | Number of paediatric patients (n=111) N (%) | TBSAr Mean |
|---|---|---|---|
| Method of %TBSA assessment | |||
| Lund and Browder | 20 (20.62) | 17 (15.32) | 19.67 |
| Rule of 9 | 8 (8.25) | 8 (7.21) | 16.8 |
| Palm method | 7 (7.22) | 11 (9.91) | 15.62 |
| Sketch on 2D print stamp | 8 (8.25) | 17 (15.32) | 13.18 |
| Draw | 29 (29.90) | 37 (33.33) | 8.97 |
| Photo sharing | 1 (1.03) | 0 (0.00) | Not stated |
| Not stated | 24 (24.74) | 21 (18.92) | 10.92 |
Duration of hospitalization
There were 24 (11.54%) burn patients admitted for less than 24 hours in the burn unit with a mean TBSAb of 1.45. A total of 147 (70.67%) patients were admitted for 1-10 days with a mean TBSAb of 6.93, and 3.37% of them required burn surgeries. Only 2.4% of the admitted patients required inpatient care for more than 30 days (Table VI).
Table VI.
Duration of hospitalization (days) and number of patients undergoing burn surgery
| Variables | Number of patients (n=208) N (%) | Number of patients with surgery done N (%) | TBSAb mean |
|---|---|---|---|
| Hospitalization (days) | |||
| <1 | 24 (11.54) | 0 (0.00) | 1.45 |
| 1 to 10 | 147 (70.67) | 7 (3.37) | 6.93 |
| 11 to 20 | 21 (10.10) | 14 (6.73) | 18.79 |
| 21 to 30 | 11 (5.29) | 8 (3.85) | 24.09 |
| > 30 | 5 (2.40) | 5 (2.40) | 25.9 |
Discussion
As a specialized burn centre on the east coast of Malaysia, the burn unit of Hospital USM receives referrals from district hospitals, emergency departments and neighboring states for acute burn management and burn reconstructions. Over the years, we noticed poor agreement in the estimation of TBSA between the referring facilities and the burn unit. Therefore, this study highlights the magnitude and trend of discrepancies and discusses their possible causes.
The aim of this study was to calculate the discrepancy between TBSAr and TBSAb among adult and paediatric burn patients. Factors such as burn severity, time following burn injuries to assessment, BMI, and number of burn areas were assessed. A standard referral from a referring center will include the total burn surface area (TBSAr) and depth of burn. Following transfer to Hospital USM, it is standard practice for the attending clinician from the burn unit to re-calculate the burn size (TBSAb) and ascertain if it has been determined accurately or is over- or underestimated. The burn area is plotted on the Lund and Browder chart, and fluid resuscitation, if required, is adjusted accordingly. The Parkland formula is used in the calculation and choice of fluids.
Cases of overestimation were significantly more frequent than cases of underestimation in both adult and paediatric burn patients by a ratio of 5:1, which is similar to the values reported in the literature.2,9,33 In paediatrics, the burn area was overestimated in 63.06% cases and underestimated in 11.71% cases. In adults, it was overestimated in 57.73% cases and underestimated in 15.46% cases. This shows that the tendency for overestimation was higher in paediatrics than in adults. This finding is consistent with the finding of a study from the United Kingdom, in which as high as 43% patients up to five years old had their TBSA overestimated, resulting in unnecessary transfers.9 TBSAr was not stated in 18.27% cases, and it was found that all of these patients had a TBSAb of less than 3%, with only three patients having a TBSAb of 8% and 9%. TBSAr overestimation caused unnecessary admissions that did not meet the ABA transfer criteria and resulted in potentially deleterious interventions.29 This explained the 11.54% of burn unit admissions for which the hospitalization duration was less than 24 hours, and 9.87% of these admissions were for paediatric patients. It is important to ensure the best use of healthcare resources while maintaining the best standard of care and optimization of the outcome.
The reasons for %TBSA discrepancies are diverse. We found that the %TBSA discrepancy rises with an increase in burn severity in both adult and paediatric groups. This is different from the finding of a study, conducted in Australia, that severe burns (≥20% TBSA) tend to have more accurate TBSAr.2 Referrals with a larger TBSA discrepancy were found to have included first degree burns or zone of hyperemia. This poses a great challenge to medical officers who are not familiar with burn care, as the gold standard of burn depth assessment is still clinical assessment.
Burn wounds undergo dynamic changes especially in the first three days.34 Although this study did not look into the assessment of burn depth, all included patients in this study were reassessed within 24 hours from the burn injuries to avoid another possible determinant of TBSA discrepancies. However, we did look into the time interval between assessment by the referring facilities and by the burn unit staff. The time interval between referral and reassessment was found to have no correlation with %TBSA discrepancy, as all admitted patients were reassessed after being transferred to Hospital USM (Table III).
Adult BMI and body weight of paediatrics did not correlate with the %TBSA discrepancy in this study (Table III), given that most of the studied patients had normal BMI or body weight. Variation in body habitus causes changes in the TBSA and the distribution of skin surfaces.35 In TBSA estimation, assessment methods that utilize the surface area are the patient’s palm in the palm method, the rule of nines, and the age-specific Lund and Browder chart. These methods depend on the distribution of the skin surface, although none of these methods consider differences in BMI.
In our centre, we have standardized all TBSAb assessment to be done via the Lund and Browder chart. Different methods of TBSAr estimation by the referring facilities were as stated in Table V. While numerous studies have discussed more accurate methods of TBSA assessment that considers body habitus and palm size, the Lund and Browder chart has remained the gold standard for TBSA estimation since 1944.36-43 There were six methods of TBSA assessment used by the referring healthcare providers. Illustrations documented on the referral letters were used to estimate TBSAr in 29.90% adults and 33.33% paediatric patients. This method of assessment is not recommended, and the mean TBSAb was only 8.97. It was found that 24.74% adult referrals and 18.92% paediatric referrals did not state the method of TBSAr assessment and, similarly, patients in this group were found to have a mean TBSAb of 10.92. Patients with a higher mean TBSAb were properly assessed via the palm method, the rule of nines, and the Lund and Browder chart (Table V). This could mean that untrained staff would find it difficult to use the latter mentioned methods in minor burns and small areas such as hands, feet, genitalia, and parts of the face.
The presence of multiple, patchy burn areas that are irregular in size at different regions of the body complicates TBSA estimation. TBSA estimation at different regions of the body also adds to cumulative discrepancies. Some areas may be missed during the assessment, which would lead to underestimation of the TBSA. In this study, the burn areas were allocated into six regions, namely the upper limbs, lower limbs, trunk (front), trunk (back), head and neck, and genitalia. The more burn areas involved, the larger were the TBSA discrepancies (P < 0.001). One patient with whole body involvement (all six regions) had a TBSA discrepancy of 21.5%, and despite being resuscitated, the patient died due to inhalational injury.
Early burn management is critical in determining outcome and prognosis. Careful TBSA estimation with clear documentation of the assessment method and the volume and type of fluids administered with ongoing monitoring is the most important step in the early management of burn patients. Officers who are unfamiliar with burn resuscitation often start intravenous full maintenance for adults and bolus fluids of 10 to 20 mL/kg for paediatrics. After administration of an adequate volume of fluids, the zone of hyperemia will heal if the region maintains perfusion and does not develop an infection.34
Study limitations
The expertise and experience of healthcare workers from the referring facilities were not taken into account here, which may have skewed the results. Burn severity was determined by TBSA. Burn depth was not considered.
Conclusion and recommendation
Addressing the issue of TBSA discrepancies has not been an easy task till now owing to the multiple factors involved. There were significant discrepancies in TBSA estimations between the referring facilities and those of the Hospital USM burn unit. Overestimation was noticeably more frequent than underestimation, especially in paediatric patients. The largest discrepancy in TBSA was seen in severe burns in both adults and paediatrics, which accounted for the positive correlation. The time interval between the TBSAr and TBSAb assessments did not correlate with the magnitude of %TBSA discrepancies. Patients’ BMI had no association with the %TBSA discrepancies. The %TBSA discrepancies increased with an increase in the number of burn areas.
Implementation of educational programs by the burn care experts and agreement on a universal method of TBSA assessment are necessary in reducing discrepancies. Accurate TBSA estimation serves as an important step for the development of a universal tool for fast and accurate TBSA estimation, even by inexperienced medical staff.
BIBLIOGRAPHY
- 1.Seow SN, Halim AS, Wan Sulaiman WA, Mat Saad AZ, Mat Johar SFN: The practice of first aid for burn injuries among the population of east coast of Peninsular Malaysia for 2012-2016. J Burn Care Res, 41(4): 905-7, 2020. [DOI] [PubMed] [Google Scholar]
- 2.Harish V, Raymond AP, Issler AC, Lajevardi SS, et al. : Accuracy of burn size estimation in patients transferred to adult burn units in Sydney, Australia: an audit of 698 patients. Burns, 41(1): 91-9, 2015. [DOI] [PubMed] [Google Scholar]
- 3.Berkebile BL, Goldfarb IW, Slater H: Comparison of burn size estimates between prehospital reports and burn centre evaluations. J Burn Care Rehabil, 7(5): 411-2, 1986. [DOI] [PubMed] [Google Scholar]
- 4.Pruitt Jr, Basil A: Protection from excessive resuscitation: “pushing the pendulum back”. J Trauma Acute Care Surg, 49(3): 567-8, 2000. [DOI] [PubMed] [Google Scholar]
- 5.Palmer JH, Sutherland AB: Problems associated with transfer of patients to a regional burns unit. Injury, 18(4): 250-7, 1987. [DOI] [PubMed] [Google Scholar]
- 6.Chan QE, Barzi F, Cheney L, Harvey JG, Holland AJ: Burn size estimation in children: still a problem. Emerg Med Australas, 24(2): 181-6, 2012. [DOI] [PubMed] [Google Scholar]
- 7.Goverman J, Bittner EA, Friedstat JS, Moore M, et al. : Discrepancy in initial paediatric burn estimates and its impact on fluid resuscitation. J Burn Care Res, 36(5): 574-9, 2015. [DOI] [PubMed] [Google Scholar]
- 8.WHO Expert Consultation: Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet, 363(9403): 157-63, 2004. [DOI] [PubMed] [Google Scholar]
- 9.Collis N, Smith G, Fenton OM: Accuracy of burn size estimation and subsequent fluid resuscitation prior to arrival at the Yorkshire Regional Burns Unit. A three year retrospective study. Burns, 25(4): 345-51, 1999. [DOI] [PubMed] [Google Scholar]
- 10.Parvizi D, Kamolz LP, Giretzlehner M, Haller HL, et al. : The potential impact of wrong TBSA estimations on fluid resuscitation in patients suffering from burns: things to keep in mind. Burns, 40(2): 241-5, 2014. [DOI] [PubMed] [Google Scholar]
- 11.Freiburg C, Igneri P, Sartorelli K, Rogers F: Effects of differences in percent total body surface area estimation on fluid resuscitation of transferred burn patients. J Burn Care Res, 28(1): 42-8, 2007. [DOI] [PubMed] [Google Scholar]
- 12.Klein MB, Nathens AB, Emerson D, Heimbach DM, Gibran NS: An analysis of the long-distance transport of burn patients to a regional burn center. J Burn Care Res, 28(1): 49-55, 2007. [DOI] [PubMed] [Google Scholar]
- 13.Cancio LC, Kramer GC, Hoskin SL: Gastrointestinal fluid resuscitation of thermally injured patients. J Burn Care Res, 27(5): 561-9, 2006. [DOI] [PubMed] [Google Scholar]
- 14.Pham TN, Cancio LC, Gibran NS: American Burn Association practice guidelines burn shock resuscitation. J Burn Care Res, 29(1): 257-66, 2008. [DOI] [PubMed] [Google Scholar]
- 15.Haberal M, Sakallioglu Abali AE, Karakayali H: Fluid management in major burn injuries. Indian J Plast Surg, 43(S 01): S29-36, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baxter CR: Guidelines for fluid resuscitation. J Trauma Acute Care Surg, 21(8): 687-9, 1981. [Google Scholar]
- 17.Cartotto RC, Innes M, Musgrave MA, Gomez M, Cooper AB: How well does the Parkland formula estimate actual fluid resuscitation volumes? J Burn Care Rehabil, 23(4): 258-65, 2002. [DOI] [PubMed] [Google Scholar]
- 18.Blumetti J, Hunt JL, Arnoldo BD, Parks JK, Purdue GF: The Parkland formula under fire: is the criticism justified? J Burn Care Res, 29(1): 180-6, 2008. [DOI] [PubMed] [Google Scholar]
- 19.Alvarado R, Chung KK, Cancio LC, Wolf SE: Burn resuscitation. Burns, 35(1): 4-14, 2009. [DOI] [PubMed] [Google Scholar]
- 20.Evans EI, Purnell OJ, Robinett PW, Batchelor A, Martin M: Fluid and electrolyte requirements in severe burns. Ann Surg, 135(6): 804-17, 1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Artz CP, Moncrief JA: The burn problem. In: Artz CP, Moncrief JA. (eds): “The treatment of burns”, 1-22, WB Saunders Co, Philadelphia, 1969. [Google Scholar]
- 22.Monafo WW: The treatment of burn shock by the intravenous and oral administration of hypertonic lactated saline solution. J Trauma, 10(7): 575-86, 1970. [DOI] [PubMed] [Google Scholar]
- 23.Muir IA, Barclay TL: “Burns and their treatment”, Year Book Medical Publishers, Chicago, 1974. [Google Scholar]
- 24.Face S, Dalton S: Consistency of total body surface area assessment in severe burns: implications for practice. Emerg Med Australas, 29(4): 429-32, 2017. [DOI] [PubMed] [Google Scholar]
- 25.Livingston EH, Lee D: Body surface area prediction in normal-weight and obese patients. Am J Physiol Endocrinol Metab, 281(3): E586-91, 2001. [DOI] [PubMed] [Google Scholar]
- 26.Borhani-Khomani K, Partoft S, Holmgaard R: Assessment of burn size in obese adults: a literature review. J Plast Surg Hand Surg, 51(6): 375-80, 2017. [DOI] [PubMed] [Google Scholar]
- 27.Berry MG, Evison D, Roberts AHN: The influence of body mass index on burn surface area estimated from the area of the hand. Burns, 27(6): 591-4, 2001. [DOI] [PubMed] [Google Scholar]
- 28.Wachtel TL, Berry CC, Wachtel EE, Frank HA: The inter-rater reliability of estimating the size of burns from various burn area chart drawings. Burns, 26(2): 156-70, 2000. [DOI] [PubMed] [Google Scholar]
- 29.Hartford CE, Kealey PG: Care of outpatient burns. In: Herndon DN. (ed): “Total burn care”, 67-80, Saunders, Philadelphia, 2012. [Google Scholar]
- 30.World Health Organization: Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet, 363(9403): 157-63, 2004. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization: Weight-for-age [https://www.who.int/docs/default-source/child-growth/child-growthstandards/indicators/weight-for-age/cht-wfa-boys-z-0-2.pdf?sfvrsn=e5bfbbee_6], 2021. Accessed March 8, 2021.
- 32.Centers for Disease Control and Prevention: BMI calculator for child and teen [https://www.cdc.gov/healthy-weight/bmi/calculator.html], 2021. Accessed March 8, 2021.
- 33.Armstrong J, Willand L, Gonzalez B, Sandhu J, Mosier M: Quantitative analysis of estimated burn size accuracy for transfer patients. J Burn Care Res, 38(1): e30-5, 2017. [DOI] [PubMed] [Google Scholar]
- 34.Herndon D: “Total Burn Care”, 5th ed, Elsevier, Philadelphia, 2017. [Google Scholar]
- 35.Hahn B, Roh SA, Price C, Fu W, et al. : Estimates of total burned surface area by emergency department clinicians and burn specialists. Cureus, 12(7): e9362, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rossiter ND, Chapman P, Haywood IA: How big is a hand? Burns, 22(3): 230-1, 1996. [DOI] [PubMed] [Google Scholar]
- 37.Neuwalder JM, Sampson C, Breuing KH, Orgill DP: A review of computer-aided body surface area determination: SAGE II and EPRI’s 3D Burn Vision. J Burn Care Res, 23(1): 55-9, 2002. [DOI] [PubMed] [Google Scholar]
- 38.Goldberg H, Klaff J, Spjut A, Milner S: A mobile app for measuring the surface area of a burn in three dimensions. J Burn Care Res, 35(6): 480-3, 2014. [DOI] [PubMed] [Google Scholar]
- 39.Sheng W, Zeng D, Wan Y, Yao L, et al. : BurnCalc assessment study of computer-aided individual three-dimensional burn area calculation. J Transl Med, 12(1): 1-12, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wurzer P, Parvizi D, Lumenta D, Giretzlehner M, et al. : Smartphone applications in burns. Burns, 41(5): 977-89, 2015. [DOI] [PubMed] [Google Scholar]
- 41.Thom D: Appraising current methods for preclinical calculation of burn size - a pre-hospital perspective. Burns, 43(1): 127-36, 2017. [DOI] [PubMed] [Google Scholar]
- 42.Cheah A, Kangkorn T, Tan E, Loo M, Chong S: The validation study on a three-dimensional burn estimation smart-phone application: accurate, free and fast? Burns Trauma, 6: 7, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith K, Poterlowicz K, Southern S, Mahajan AL, Jivan S: The effect of a known object in a static image of a burn to improve the burn size estimation. Burn, 47(6): 1295-9, 2021. [DOI] [PubMed] [Google Scholar]


