Abstract
Sensory behaviors are widely reported in autism spectrum disorder (ASD). However, the impact of these behaviors on families remains largely unknown. This study explored how caregivers of minimally verbal children with ASD responded to their child’s sensory behaviors. Using a mixed-methods approach, we examined two variables for each endorsed child behavior: (1) Did the caregiver respond/try to change the behavior? and (2) What response did they employ? Caregivers did not differ in the frequency of responses to hypo- or hyper-responsive behaviors but employed different responses. Caregivers responded to more social sensory behaviors and predominately changed their own behavior in response to their child’s. Our findings demonstrate how extensively caregivers adapt to their child’s behaviors and vary their response dependent on behavior exhibited.
Keywords: autism, sensory behaviors, caregivers, language
Background
Unusual interests in and/or reactions to sensory input (hereafter sensory behaviors) are widely reported in children with autism spectrum disorder (ASD; Baranek, 1999; Baranek, David, Poe, Stone, & Watson, 2006; Ben-Sasson, Soto, Martnez-Pedraza, Carter, 2013; Rogers, Hepburn, & Wehner, 2003; Tomchek & Dunn, 2007) and are now featured within the DSM-5 conceptualization of the disorder (American Psychiatric Association, 2013). These behaviors are characterized by self-stimulation, avoidance of stimuli, overreaction to stimuli, and failure to respond to input from sensory modalities (Rogers et al., 2003; Tomchek & Dunn, 2007). The goal of this study was to determine how sensory behaviors manifest in a well-defined sample of school-aged, minimally verbal children with a diagnosis of ASD. In addition, we sought to understand which child sensory behaviors caregivers reported responding and the strategies caregivers used in response.
Sensory Behaviors in ASD
Although reactions to sensory input are not unusual in typically developing children and children with other developmental disorders, they are reported as more common and interfering in children with ASD with less reduction in their intensity and/or frequency over time. Common examples in ASD include responding negatively to loud sounds, unusual need for touching surfaces/textures, mouthing objects, and seeking out movement. Atypical sensory behaviors are observed in the early development of ASD (Baranek, 1999; Freuler, Baranek, Watson, Boyd, & Bulluck, 2012) and are based on caregiver report; between 45% and 95% of children with ASD react to, or seek out, sensory stimuli from their environment (Baker, Lane, Angley, & Young, 2008; Baranek et al., 2006; Tomchek & Dunn, 2007).
Different profiles of sensory behaviors have been identified in children with ASD with differential associations to other child characteristics, such as language (Patten, Ausderau, Watson, & Baranek, 2013; Watson, et al, 2011), adaptive behavior (Lane, Young, Baker, & Angley, 2010), repetitive behaviors (Boyd, McBee, Holtzclaw, Baranek, & Bodfish, 2009) and social-communication behaviors (Watson et al., 2011). Boyd and colleagues (2009) reported that high rates of hypo-responsiveness being predictive of elevated rates of restricted and repetitive behaviors (RRBs). This relationship was independent of mental age. Hypo-responsiveness has also been reported to associate positively with severity of social communication impairment in children with ASD and other developmental disabilities. Sensory behaviors have predicted communication competence and maladaptive behavior (Lane et al., 2010) suggesting that these behaviors exert a major influence on a range of other aspects of functioning.
Research using caregiver report indicates increased rates and severity of sensory behaviors (particularly sensory seeking and hypo-responsiveness) in children with minimal verbal language skills compared to other children with ASD (Patten et al., 2013; Watson et al., 2011). Both Patten and colleagues (2013) and Watson and colleagues (2011) reported negative associations between sensory behaviors and language abilities, particularly with hypo-responsive behaviors. In this study, we specifically explore the sensory behaviors in school-aged minimally verbal children with ASD. This sub-group of children is often categorized as poorer responders to traditional ASD treatments and may require multiple treatments to achieve observable gains/behavioral change (Tager-Flusberg & Kasari, 2013). Minimally verbal children with ASD are typically defined as over 5 years of age, with few functional words used on a daily basis (Tager-Flusberg & Kasari, 2013).
The Impact of Sensory Behaviors in ASD on the Family
Although there is a sizeable body of research defining sensory behaviors in children with ASD, there has been very little research exploring how caregivers respond to the sensory behaviors displayed by their children with ASD. The literature indicates that children’s interests in or reactions to sensory stimuli can limit child and family participation in activities (Baranek, 2002; Ben-Sasson et al., 2013; Leekam, Nieto, Libby, Wing, & Gould, 2007; Little, Ausderau, Sideris, & Baranek, 2015; Rogers & Ozonoff, 2005) while also increasing caregiver stress (Ben-Sasson et al., 2013). Studies have not specifically focused on the impact of these behaviors in minimally verbal children with ASD or how their caregivers respond to them.
A handful of studies have used in-depth qualitative methodology to examine the impact of sensory behaviors on families of children with ASD. Dickie and colleagues (2009) found that parents rated child sensory behaviors associated with auditory stimuli (such as loud, sudden noises) as unpleasant whereas those involving tactile stimuli and movement were rated as more pleasant experiences (relative to other stimuli) for both the child and parent. Bagby, Dickie, and Baranek (2012) conducted interviews with 12 parents that were analyzed to generate a grounded theory examining how sensory behaviors impact family activities in children with and without ASD. Sensory behaviors shown by children with ASD not only affected the activities in which families participated, but the extent to which they had to prepare for activities and the degree to which experiences were shared. Families of children with ASD reported avoiding certain situations based on prior negative experiences and discussed extensive planning and preparation to cope with the sensory behaviors their child may display. Schaaf, Toth-Cohen, Johnson, Outten, and Benevides (2011) used semistructured interviews to explore the impact of child sensory behaviors on family routines. Parents reported using several strategies including changing their own behavior to accommodate their child’s sensory behaviors, implementing reward systems, and exerting environmental control.
The previous studies used in-depth qualitative methodology to provide examples of the strategies caregivers may employ in order to manage their child’s sensory behaviors. Although these studies provide rich detail, the number of participants is typically restricted. The current study employed a mixed-methods approach to first quantify how frequently caregivers responded to their child’s sensory behaviors. In the second stage of the study, the types of caregiver strategies were examined to understand whether caregiver responses varied as a function of the type of child sensory behavior reported (e.g., sensory modality, sensory processing pattern or social-non-social dimensions). This study is novel in that it couples both quantitative and qualitative data drawn from a large well-defined sample and its in-depth exploration of the types of responses caregivers employ.
Aims
This study aimed to (1) examine sensory behaviors in minimally verbal children with ASD and (2) understand how their caregivers responded to these behaviors and the techniques they employ. A unique aspect of our study is the focus on minimally verbal children with ASD. Nearly a third of children with ASD have not developed functional spoken language skills by the time they enter school (Anderson et al., 2007). Yet very few studies explicitly focus on these children (Tager-Flusberg & Kasari, 2013); and those studies that do, have understandably focused primarily on characterizing communication skills and interventions to target those skills (Goods, Ishijima, Chang, & Kasari, 2013; Kasari et al., 2014). Given prior reports of increased rates and severity of sensory behaviors in children with minimal verbal language skills compared to other children with ASD (Patten et al., 2013; Watson et al., 2011), we were interested in exploring the profile of sensory behaviors these children display and how their caregivers respond to these behaviors.
We had two specific aims. First, we explored patterns of caregiver-reported child sensory behaviors in a sample of minimally verbal children with ASD aged between 5 and 8 years. Secondly, we quantified how frequently caregivers responded to their child’s sensory behaviors and the responses they employed.
Methods
This research was approved by the Institutional Review Board at each of the three study sites. Caregivers gave written consent for their child to participate in the study.
Participants
This study included 56 children and their caregivers. Sixty-one children were recruited into the study; however, only 56 participants had complete data from the Sensory Experiences Questionnaire Version 2.1 (SEQ; (Baranek et al., 2006). Families were initially screened by phone and invited for screening assessments by the study coordinator. Inclusion criteria included (1) a previous clinical diagnosis of ASD confirmed by the administration of the Autism Diagnostic Observation Schedule (ADOS-Generic) Module 1; (2) chronological age between 5 and 8 years; (3) no diagnosis of a genetic disorder; (4) minimally verbal (defined as fewer than 20 spontaneous functional spoken words on a naturalistic language sample); (5) received at least 2 years of prior early intervention, and (6) a nonverbal developmental age of at least 24 months based on standardized cognitive assessments. Data for this study are from baseline assessments only.
Measures
In addition to caregivers completing a measure of child sensory behaviors, child participants completed a series of standardized assessments upon entry into the study to confirm both eligibility and provide sample characteristics (summarized in Table 1). ASD diagnosis (required for eligibility) was determined using the Autism Diagnostic Observation Schedule-Module 1 (Lord et al., 2000). The ADOS is a semi-structured assessment designed for individuals who may have ASD. The ADOS uses a hierarchy of presses to elicit behaviors relevant to ASD. The ADOS has internal consistencies ranging from 0.47 to 0.94 (Lord et al., 200). Test-retest indicates excellent stability for Social Interaction and Communication algorithm domains, with good stability for the Stereotyped Behaviors and Restricted Interests algorithm domain.
Table 1.
Participant Characteristics
| Gender (Boys:Girls) | 48:8 | |
| Chronological age (months) | 6.32 (1.16) | |
| Standardized Assessments | ||
| TELD-3 | Receptive AE | 1.99 (.54) |
| Expressive AE | 1.71 (.33) | |
| Leiter-R | Brief IQ | 67.07 (19.23) |
| AE | 3.95 (1.14) | |
| PPVT-4 | AE | 2.61 (.68) |
| ADOS | Social Affect | 14.16 (3.6) |
| RRB | 5.64 (1.76) | |
| RBS-R | Total | 32.06 (35.41) |
Note. Mean (SD) unless otherwise indicated. TELD-3 = Test for Early Language Development; Leiter-R = Leiter International Performance Scale-Revised; PPVT-4 = Peabody Picture Vocabulary Test; ADOS = Autism Diagnostic Observation Schedule-Generic; RBS-R: Repetitive Behavior Scale-Revised.
Participants completed the Leiter International Performance Scale-Revised (Leiter-R; Roid & Miller, 2002), a nonverbal cognitive assessment for ages 2 to 20. The Leiter-R is frequently used with children who are cognitively delayed and on the autism spectrum. The Leiter-R yields both a Brief IQ and a mental age equivalent score through the administration of game-like tasks across a number of scales. These include Attention, Memory, Sequencing and Matching. The Leiter-R has a test-retest ranging between 0.65 to 0.90 dependent on the scale and internal consistencies ranging from 0.88 to 0.93.
Participants also completed two language assessments. The Peabody Picture Vocabulary Test (PPVT-4; Dunn & Dunn, 2012) was administered as a measure of receptive vocabulary development. The PPVT-4 is a norm-referenced instrument for measuring receptive vocabulary in children and adults. Both internal consistency (0.95) and test-retest (0.93) are high, though construct validity is lower for children with ASD. Participants completed the Test for Early Language Development (TELD-3; Hresko, Reid, & Hammill, 1999), a standardized assessment of receptive and expressive language development in semantic, syntactic, morphologic, phonologic, and pragmatic domains. Test-retest reliability for the TELD-3 ranges from 0.82 to 0.95.
Child sensory behaviors: Sensory Experiences Questionnaire-2 (SEQ-2).
The SEQ-2 was used in this study to measure (1) child sensory behaviors and (2) caregiver responses to their child’s sensory behaviors. The SEQ-2 is a caregiver-completed questionnaire focusing on sensory responsiveness (and lack thereof) commonly observed in children with ASD and other developmental disabilities (Baranek et al., 2006); it requires about 20 min to complete. Caregivers answer 30 items (including distractor items) quantitatively using a 5-point Likert scale (1 = Almost Never through to 5 = Almost Always), then may complete a qualitative section to report specific information about intervention/coping strategies used by the caregiver to address their child’s behavior related to each of the 30 items. In addition, there are six additional items capturing child sensory seeking behaviors. The SEQ-2 has an internal consistency of 0.80 (Baranek et al., 2006). Nearly two thirds of children with ASD in the SEQ-2 standardization sample received scores one or two standard deviations above the overall SEQ-2 mean score with higher scores meaning more noticeable/interfering responses to sensory stimuli (Baranek et al., 2006).
The SEQ-2 categorizes child sensory behaviors in multiple ways. First, the SEQ-2 generates a total score based on items from all five sensory modality subscales (Auditory; Visual; Tactile; Gustatory/Olfactory, referred to here as Taste/Smell,; and vestibular/proprioceptive, referred to here as Movement); and a sensory seeking subscale. These categories are mutually exclusive and mean scores are generated for each of the five sensory modalities. SEQ-2 scores may be grouped by sensory processing patterns with two mutually exclusive scales of 13 items each (Hypo- and Hyper-responsiveness). Hypo-responsiveness describes the lack of, delayed or reduced response to sensory stimuli (e.g., Is your child slow to notice new objects or toys in the room?), whereas Hyper-responsiveness denotes an exaggerated response to stimuli such as aversion or avoidance (e.g., Does your child avoid touching certain textures or playing with messy materials?). The SEQ-2 items also may be grouped based on whether they are considered Social (e.g., Does your child dislike being tickled?) or Non-Social (e.g., Does your child put objects, toys or other non-food items in his/her mouth to lick, suck or explore?). For the purpose of our first aim (characterizing sensory behaviors in minimally verbal children with ASD), SEQ-2 mean scores served as dependent variables. These scores were based on the following groupings: total, sensory modalities, sensory processing pattern (Hypo- and Hyper-responsiveness) and the Social/Non-Social dimension.
Although the SEQ-2 has now been replaced with the SEQ-3 (Ausderau et al., 2014), this study was initiated prior to the development of the most recent edition. Moreover, a strength of the SEQ-2 is the inclusion of a free text section exploring how caregivers respond to their children’s sensory behaviors. We used these free text responses to categorize caregiver strategies using a coding scheme (see coding of caregiver strategies) developed in our lab.
Coding of caregiver strategies.
Coding of caregiver strategies was achieved through a two-step process. First, we identified categories of responses expected to arise per published qualitative studies examining caregiver responses to child sensory behaviors and the impact of these behaviors on family life (Bagby et al., 2012; Schaaf et al., 2011). We also drew from a recent study that examined how caregivers responded to their child’s RRBs (Harrop et al., 2016). This was due to the overlap between some RRBs and sensory behaviors (Boyd et al., 2010; Boyd et al., 2009). In addition, much less is known about sensory behaviors relative to RRBs. Therefore, this body of research is important to consider.
If a caregiver response could not be assigned to one of the previously identified categories (outlined next), the coders assigned a new code using content analysis. Content analysis is defined as “the subjective interpretation of the context of text data through the systematic classification process of coding and identifying themes or patterns” (Hsieh & Shannon, 2005, p. 1278). Content analysis is a form of data reduction which allows researchers to make sense of textual data and identify themes emerging from the data itself (Patton, 2002). In general, content analysis provides a way to quantify data that is qualitative in nature. Following this two-step coding process, the first and second author met to discuss the emerging categories. Including the prior identified categories, seven different types of caregiver response emerged from the data (Table 2).
Table 2.
Caregiver Responses/Strategies to Child Sensory Experiences
| Response Category | Example | |
|---|---|---|
| 1 | Reassurance/Explain |
Reassure him all is well
Talk about what he is hearing Talk about the process as we are doing it Explain that we don’t put things in our mouth |
| 2 | Prompting: Verbal or Physical |
Ask him to put his hands down
Ask him to respond Count 1,2,3…. Take hands off his ears Turn his face to look at mine |
| 3 | Caregiver changes own behavior |
Engage him at eye level and follow his gaze
We will try get his attention I will try and join in the experience with him We’ll spin with him |
| 4 | Physical change/adjustment to the environment |
Provide noise-cancelling headphones
I will reduce the noise Change to a room that doesn’t echo We changed his toothbrush as he didn’t like the texture of his old one |
| 5 | Exposure/Reinforcement |
Expose him to a variety of sounds
He does not like it when we sing, but we keep on singing I insist he completes brushing his teeth We reward him for finishing his dinner with preferred activities We pair the undesirable food with a favorite one |
| 6 | Redirection |
Redirect him to an different activity
Draw his attention to something else Show him a different way to engage with the object |
| 7 | Training/Professional Input |
We use strategies the ABA therapist taught us
We are seeing an OT |
ABA = Applied Behavior Analysis; OT = Occupational Therapist.
Babgy et al. (2012) and Schaaf et al. (2011) reported that caregivers avoided certain activities and planned extensively based on their child’s sensory behaviors. Caregivers also reported environmental manipulations (such as removing sounds or providing adaptations such as chew toys; Schaaf et al., 2011). Schaaf et al. (2011) reported reward systems for children when they completed an activity, as well as caregivers changing their own behavior to adapt to their child’s sensory behaviors. We expected three further categories (redirecting the behavior and verbal and/or physical prompting) based on the observational findings of Harrop et al. (2016. Redirections were also reported by Grahame and colleagues (2015) in a recent intervention study targeting child RRBs.
As previously identified from Bagby et al. (2012) and Harrop et al. (2016), verbal and physical prompting emerged as themes from the data and were grouped together into a single category of Prompting. Environmental Changes (drawn from Schaaf et al., 2011), such as removing items or adjusting the environment also emerged. In addition to the previously identified codes, caregivers frequently reported changing their own behavior in response to their child’s sensory behavior, such as moving in front of a child or persisting with an activity until the child responded. These responses were consistent with Schaaf and colleagues’ (2011) category of caregiver flexibility and grouped as Caregiver Changes Own Behavior. Redirections also emerged from the data (similar to Harrop et al., 2016, and Grahame et al., 2015).
Offering comfort and reassurance while also offering explanations emerged as a consistent response (Reassurance/Explain). Many caregivers reported exposing children to stimuli while also offering reinforcements (Exposure/Reinforcement), such as providing favorable rewards (as identified by Schaaf et al., 2011). Specific strategies gained through training or provided by professionals, such as Applied Behavior Analysis (ABA) or Occupational Therapy (OT), also emerged from the data and were not identified from previous literature (Training/Professional Input). All seven potential caregiver responses are reported in Table 2 with examples.
Following category generation, the first and second authors independently coded each reported caregiver response by selecting one of the response categories defined in stage one (reported previously and in Table 2). When multiple responses were reported, the raters selected all applicable categories. When a caregiver reported responding to the child’s sensory behavior (i.e., by checking yes to the question “Do you try and change this behavior”) but did not provide a free text response, this was noted in the database. If the caregiver simply reported a statement such as “Bath time is okay. Great with brushing teeth” this was noted as a comment and not included in the analysis of caregiver response type. If the caregiver reported not making a response (i.e., by ticking no to the question “Do you try and change this behavior?”) but then reported a qualitative response, this was not included. All free text responses were rated by both the first and second author. Cohen’s kappa was run to determine agreement between the raters for caregiver response type. High agreement was found overall (k = .96, p <. 001).
Procedures
All study procedures were approved by Institutional Review Boards at the three research sites. Assessments and caregiver questionnaires were completed at research clinics. The ADOS was completed by research-reliable administrators. The Leiter-R, PPVT-4, and TELD-3 were administered by graduate research assistants, doctoral students, postdoctoral researchers, or clinical researchers. All administrators had experience working with children with ASD. Graduate research assistants were supervised by a licensed psychologist or speech-language pathologist at each site. Caregivers typically completed the SEQ-2 while their child completed one of the language assessments. A research assistant explained the purpose of the questionnaire and was at hand to answer any questions. Procedures were adapted for children as needed; for example, caregiver questionnaires were sent home with the family if the caregiver was needed during the child’s assessments and returned when they visited the clinic for intervention sessions.
Analysis
To explore the different profiles of child sensory behaviors, we calculated total and mean scores from the SEQ-2. Mean scores were calculated for the five sensory modality subscales (Tactile, Auditory, Visual, Taste/Smell, and Movement) and the scale of Sensory Seeking. We also collapsed items to provide mean scores for the sensory processing patterns (Hypo- vs. Hyper-responsive) and the social-nonsocial dimensions of the SEQ-2.
Caregiver responses were explored in two ways. First, we examined how frequently caregivers reported responding to their child’s sensory behaviors (based on the response to the question “Do you try and change this behavior?”). Second, we examined whether the type of response reported varied as a function of child sensory behavior. Type of response was based on the free text responses caregivers reported.
For each different way of categorizing the data (sensory modality, sensory processing pattern, and social-non-social dimensions), we calculated the percentage of items endorsed by caregivers for their children. Although mean scores give a sense of the occurrence/interference of the child’s sensory behavior (on a scale from zero to two), caregiver endorsement of items related to whether or not the child demonstrated the item (yes vs. no). We conducted one way ANOVAs and independent t tests to explore whether caregivers endorsed items in their children differentially across the different sensory modalities, sensory processing patterns, and social-non-social dimensions. A Bonferonni adjusted significance level of 0.01 was employed to control for the multiple comparisons resulting from three different ways of categorizing the data (sensory category, processing pattern, and social-non-social).
To examine the caregiver data, we calculated the mean number of times caregivers reported responding (yes vs. no) to their child’s sensory behavior (in response to the subquestion “Do you try and change this behavior?”) and grouped responses by the three different ways of analyzing the data. Data were then descriptively analyzed to explore how the percentage of caregiver responses for each given type of categorization (sensory modality, sensory processing pattern, and social-non-social dimensions) related to the number of items they endorsed in their children. This was to examine whether certain types of behaviors were endorsed frequently by caregivers but caregivers did not report responding to these behaviors (and vice versa). We ran one-way ANOVAs to explore whether caregivers responded differentially across the different sensory modalities and independent t tests to answer this for sensory processing patterns and the social-non-social dimensions. A Bonferonni adjusted significance level of 0.01 was employed to control for the three different ways of categorizing the data.
We then categorized caregiver responses to their child’s sensory behaviors by type (Table 2) and used one-way ANOVAs to examine whether the type of response caregivers reported varied by the sensory modality, sensory processing pattern, and social-non-social dimension. A Bonferonni adjusted significance level of 0.005 was employed to control for the seven different types of caregiver response possible and the three different ways of categorizing the data (sensory category, processing pattern, and social-non-social). Only main effects and post hoc tests that met the adjusted significance levels are reported in the results. All results that reached the Bonferoni adjusted significance levels are denoted in the results with an asterisk.
Results
Sensory Behaviors in Minimally Verbal Children With ASD
Mean scores and caregiver endorsement by sensory modality.
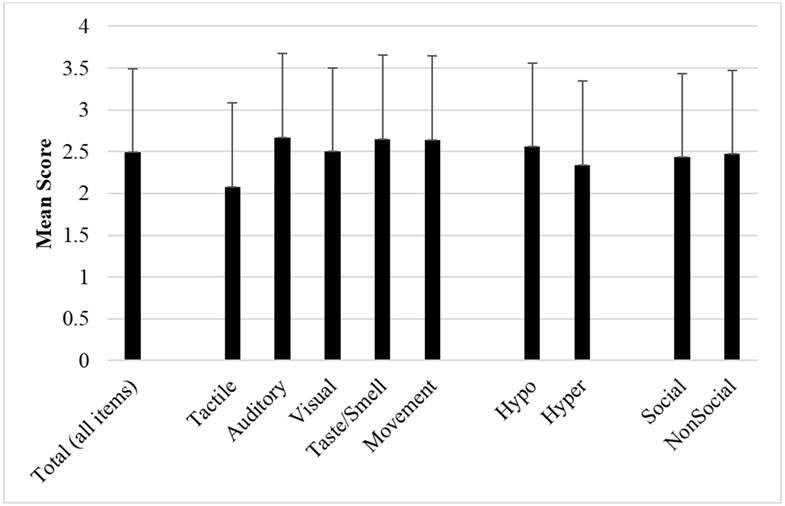
Mean scores varied by sensory modality, F (4, 220) = 10.16, p <.001*; Figure 1. Post-hoc comparisons revealed lower mean scores for Tactile items than items from all other scales (p < .001*; Figure 1), indicating caregivers rated these items as less severe/commonly occurring.
Figure 1.
Mean SEQ Scores by Sensory Modality, Sensory Processing Pattern and Social-Non-Social Dimension.
Note. Errors Bars = SD
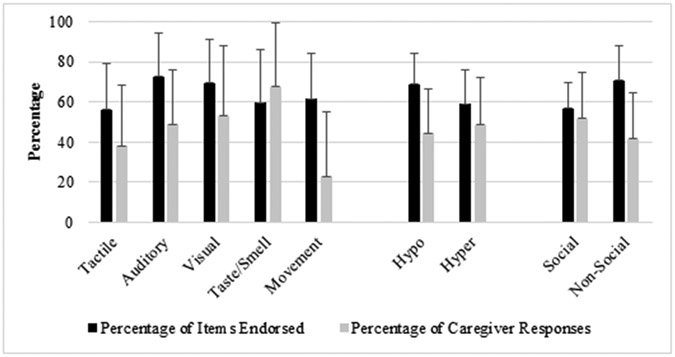
Caregiver endorsement of items (does the behavior occur: yes vs. no) also varied by sensory modality, F (4, 220) = 6.34, p <.001*; Figure 2. Post-hoc comparisons revealed that caregivers endorsed Auditory items more than all other sensory modality categories with the exception of Visual (Tactile: p < .001*; Taste/Smell: p = .01*; Movement: p = .05). Visual items were endorsed more than Tactile items (p < .001*).
Figure 2.
Percentage of Items Endorsed and Responses Reported by Sensory Modality, Sensory Processing Pattern and Social-Non-Social Dimension.
Note. Errors Bars = SD
Mean scores and caregiver endorsement by sensory processing pattern.
Mean scores and caregiver endorsement of items varied by sensory processing pattern (Figures 1 and 2). Caregivers reported more items categorized as Hypo-responsive compared to items categorized as Hyper-responsive, t (55) = 3.29, p = .002*; Figure 1, and endorsed a greater percentage of items from this scale, t (55) = 4.25, p <.001*; Figure 2.
Mean scores and caregiver endorsement by social-non-social dimension.
Mean scores across the Social and Non-Social items did not differ, t (55) = −.82, p = .41; Figure 1, however caregivers’ endorsement of items did differ, t (55) = −8.23, p <.001*; Figure 2. Caregivers endorsed more items classified as Non-Social than Social.
Caregiver Responses to Child Sensory Behaviors
Percentage of caregiver responses.
Percentage of caregiver responses by sensory modality.
The percentage of caregiver responses varied as a function of sensory modality, F (4, 220) = 23.43, p <.001*; Figure 2. Caregivers reported responding less frequently to behaviors involving Movement than Auditory, Visual and Taste/Smell (p <.001*). Caregivers responded more frequently to behaviors involving Taste/Smell compared to both Auditory (p = .002*) and Tactile behaviors (p < .001*). Caregivers reported responding to their children’s Visual sensory behaviors more than to Tactile behaviors (p = .005*).
Percentage of caregiver responses by sensory processing pattern.
Despite differences in caregiver endorsement of items by sensory processing pattern (Hypo- vs. Hyper-Responsiveness), there was no difference how frequently caregivers responded to these behaviors, t (55) = −1.78, p = .08; Figure 2.
Percentage of caregiver response by social-non-social dimension.
Although caregivers endorsed more Non-Social items in their children, caregivers reported employing responses more frequently to behaviors classed as social rather than Non-social, t (55) = 4.42, p <.001*; Figure 2.
Caregiver response type.
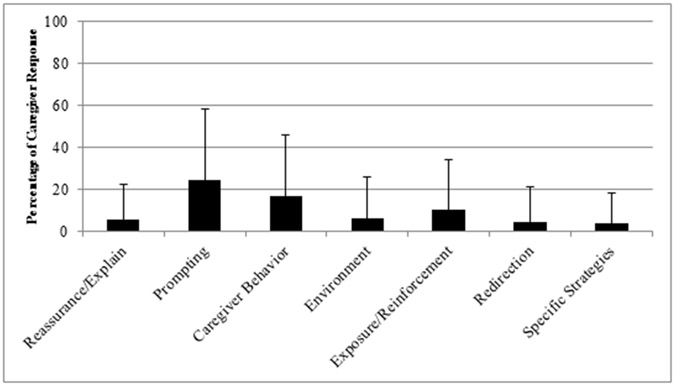
Across all items, the most common type of caregiver response was prompting followed by the caregiver changing their own behavior (Figure 3). Qualitative responses were missing for nearly 9% of items. In addition, 6% of items were unclassifiable. Nearly 15% of responses included multiple responses. No caregivers reported more than two different strategies to one item.
Figure 3:
Caregiver Response Type: Overall.a
Note: Errors Bars = SD.
a Percentage refers only to the caregivers who reported responding to a particular behavior. Caregivers who reported not responding to the behavior or did not endorse the behavior in their child were not included.
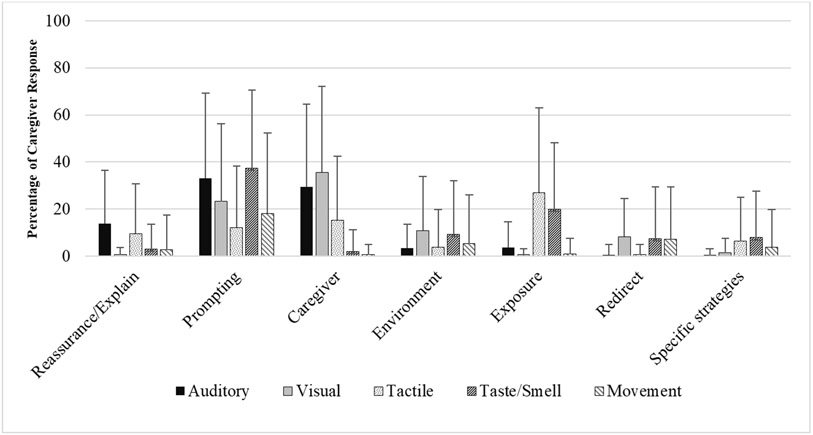
Caregiver response type by sensory modality.
The type of responses caregivers used varied as a function of sensory modality (Figure 4). Four main effects were found. Caregivers differed in the use of reassurance/explanations, F (4,275) = 6.60, p < .001*; Figure 4; they were more likely to employ this strategy in response to Auditory items than Visual (p <.001*), Taste/Smell (p =.005*) and Movement (p = .003*).
Figure 4.
Percentage of Caregiver Response Type by Sensory Modality.a
Note: Errors Bars = SD.
a Percentage refers only to the caregivers who reported responding to a particular behavior. Caregivers who reported not responding to the behavior or did not endorse the behavior in their child were not included.
Caregivers’ use of prompting also varied as a function of sensory modality, F (4,275) = 5.65, p < .001*; caregivers were more likely to use verbal or physical prompts for Auditory (p = .005*) and Taste/Smell items (p = .001*) compared to Tactile. Caregiver reports of adjusting their own behavior also varied, F (4, 275) = 20.65, p <.001*. They were more likely to modify their own behavior for child behaviors involving auditory stimuli compared to behaviors related to taste/smell (p <.001*) and movement (p <.001*). Caregivers also were more likely to modify their own behavior when their child sought out/reacted to visual stimuli compared to tactile (p <.001*), taste/smell (p <.001*) and movement (p <.001*).
Caregiver reports of exposure/reinforcement strategies varied by sensory modality, F (4, 275) = 18.96, p <.001*, with caregivers more likely to use these strategies for child behaviors involving tactile and taste/smell stimuli relative to all other modalities (all p <.001*). No differences were found in the use of specific strategies (such as ABA or OT), redirections or environmental changes.
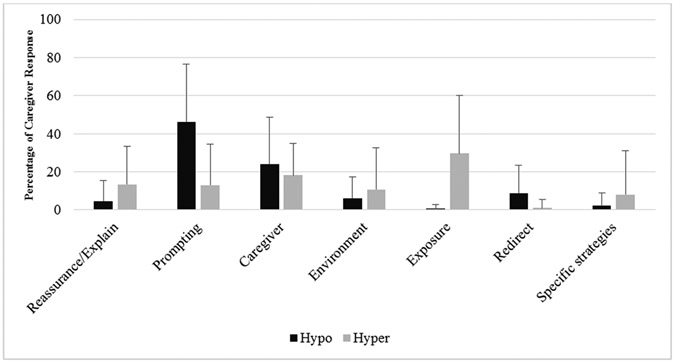
Caregiver response type by sensory processing pattern.
Caregiver response varied as a function of sensory processing pattern (Figure 5). The most common caregiver-reported response for items classed as Hypo-Responsive was prompting, t (110) = 6.64, p <.001*; Figure 5. Caregivers also reported using redirection strategies, t (110) = 3.92, p <.001*, in response to these behaviors. By contrast, the most common strategy for items classed as Hyper-responsive was exposure/reinforcement, t (110) = −7.17, p <.001*; Figure 5. Caregivers were also more like to offer reassurance and/or explanations to Hyper-responsive behaviors, t (110) = −2.9, p =.005*.
Figure 5.
Caregiver Response Type by Sensory Processing Pattern.a
Note: Errors Bars = SD.
a Percentage refers only to the caregivers who reported responding to a particular behavior. Caregivers who reported not responding to the behavior or did not endorse the behavior in their child were not included.
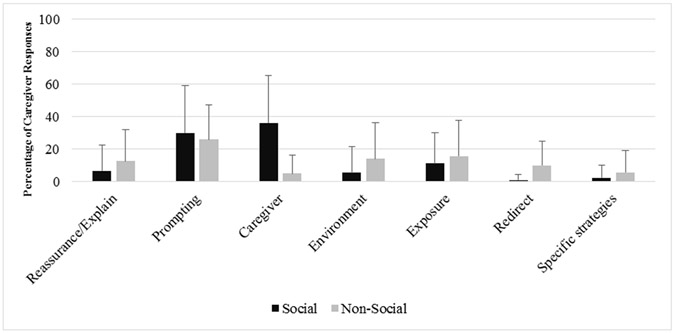
Caregiver response type by social-non-social dimension.
The most common response reported for items classed as Social was caregiver adjustment of their own behavior, t (110) = 7.43, p <.001*, followed by prompting, which did not differ between Social and Non-Social items. Caregivers showed a more distributed pattern of responses to Non-Social items (Figure 6). Caregivers were more likely to report redirecting behaviors, t (110) = −4.46, p <.001*, for non-social behaviors relative to social.
Figure 6.
Caregiver Response Type By Social-Non-Social Dimension.a
Note. Errors Bars = SD.
a Percentage refers only to the caregivers who reported responding to a particular behavior. Caregivers who reported not responding to the behavior or did not endorse the behavior in their child were not included.
Discussion
This study had two aims; (1) explore the patterns of caregiver reported child sensory behaviors in a sample of minimally verbal children with ASD; and (2) quantify the frequency and define the types of strategies caregivers employ in responding to their child’s sensory behaviors. The overall goal was to gain a deeper understanding of how child sensory behaviors affect caregiver behaviors.
Profile of Sensory Behaviors in Minimally Verbal Children With ASD
With regards to sensory modality, items from the Auditory and Visual scales were endorsed more frequently by caregivers. This suggests that behaviors involving auditory stimuli (such as avoidance of loud noises or seeking out certain sounds in the environment) occurred most frequently in our sample of minimally verbal children with ASD. In our sample, child behaviors related to tactile stimuli were endorsed less than all other sensory modalities and also rated as less severe suggesting that minimally verbal children with ASD may be less sensitive to stimuli involving touch and different textures. Although not a direct comparison, our findings differ from those of Rogers et al. (2003), who reported that toddlers with ASD had higher rates of behaviors relating to taste and smell than controls, suggestive of potential developmental change in profiles of sensory behaviors in ASD, or differences due to level of impairment. Caregivers endorsed more Hypo-responsive items in their children (characterized as a lack of, delayed or reduced response to stimuli) compared to items related to Hyper-responsive reactions. This is similar to the findings of Ben-Sasson et al. (2013) who found that toddlers with ASD had higher rates of underresponsiveness and avoidance behaviors relative to controls. Hypo-responsive behaviors were also rated as more severe by caregivers, suggesting that these behaviors were more common and more impacting for minimally verbal children with ASD. This aligns with the findings of Waston et al. (2011) that language was inversely related to hypo-responsive behaviors. Although there were no differences in how severely caregivers rated social and non-social items, caregivers endorsed more non-social items.
Caregiver Responses: Frequency and Type
Frequency and type of caregiver response varied as a function of sensory modality, sensory processing pattern and social versus. non-social contexts. Two additional categories of caregiver response were drawn from the data (Reassurance/Explain and Training/Professional Input) and the most commonly emerging categories overlapped with those reported by Bagby et al. (2012), Schaaf et al. (2011) and Harrop et al. (2016). Overall, the most common response reported by caregivers was verbal and/or physical prompting. This was followed by caregiver adaption of their own behavior to accommodate their child’s sensory behavior, a category similar to Schaaf and colleagues’ (2011) descriptions of adaptability and flexibility. Despite the overlap between certain sensory behaviors and RRBs, our findings differ from those of Harrop et al. (2016) who found that caregivers of toddlers used redirections most frequently when addressing their child’s RRBs. This suggests that caregivers may change their response type dependent on the age and functioning level of their child and the type of behavior displayed (sensory behaviors vs. RRBs). Together with previous qualitative studies, our findings suggest that caregivers use a range of responses dependent on the type of sensory behavior exhibited by their child.
Sensory modality.
Caregiver responses varied by sensory modality. For auditory stimuli, caregivers frequently reported using reassurance, prompting, and modifying their own behavior. Examples included removing auditory stimuli when possible or changing activities (such as vacuuming) in response to the child’s reaction. Prompting and exposure strategies were used commonly for behaviors concerning taste/smell. Caregivers frequently adjusted their own behavior for visual behaviors. A number of these items overlap with ASD core symptoms, such as not noticing when a person enters the room or not making eye contact during play and therefore caregivers likely place more emphasis on responding to the absence of these behaviors rather than the presence of others.
Caregivers in our sample reported infrequently responding to behaviors involving movement, supporting the observational findings of Harrop et al. (2016) that caregivers infrequently responded to motor RRBs and suggests that caregivers may respond to these behaviors in similar ways. Taken together, these findings suggest that although these behaviors are commonly occurring, motor behaviors (both sensory and RRBs) may not interfere with caregiver-child interactions and daily living activities or cause as much distress to families compared to other types of behavior. Conversely, caregivers may have learned over time to pick their battles, particularly with behaviors often seen as characteristic of ASD, and may not focus on these relative to other behaviors.
Sensory processing pattern.
Focusing on sensory processing pattern (hypo- vs. hyper-responsive), when children demonstrated a lack of response to sensory stimuli (hypo-responsiveness), caregivers commonly reported using prompting and redirections. This may reflect the caregivers’ drive to make children aware of stimuli around them – such as people entering a room. When children displayed overreaction to sensory stimuli (hyper-responsiveness), caregivers employed a wider range of responses including exposing children to the stimuli and offering reassurance/explanations. As shown in Figure 5, behaviors reflective of hyper-responsiveness may have a greater number of responses appropriate for them and caregivers may employ multiple in order to get the desired response from their child. Despite caregivers rating hypo-responsive behaviors as more severe, hyper-responsive behaviors may be viewed as more impacting on family daily living activities therefore the caregiver may employ different and/or multiple strategies in order to complete everyday tasks such as mealtimes and grooming.
Social-Non-Social Dimension.
Caregivers reported adapting their own behavior to child sensory behaviors that occurred within social contexts. These typically included the caregiver adapting their behavior in order to elicit a response from their child. Many of the items categorized as social in the SEQ-2 have significant overlap with ASD core deficits in social interaction and communication (e.g., a child not responding to their name being called), thus caregivers may not attribute these to a sensory processing style. Additionally, many of the social items represent an absence of typical behaviors rather than the presence of atypical behaviors (such as peering at items from an angle, or sniffing objects). Therefore, caregivers may employ different responses to these behaviors given their importance to other areas of development and status as core ASD deficits.
Implications for Future Research and Treatment
Our findings reveal a complex interplay between child sensory behaviors and how and when caregivers respond to them in a well-characterized sample of minimally verbal children with ASD. Currently we know very little about the effectiveness of caregiver-mediated interventions for this core deficit. A recent systematic review for interventions targeting sensory behaviors in ASD reported no caregiver-mediated interventions for these behaviors (Case-Smith, Weaver, & Fristad, 2015) despite success for other core ASD domains (social communication: Green et al. 2010; Kasari et al., 2014;. RRBs: Boyd, McDonough, Rupp, Khan, & Bodfish, 2011, Grahame et al., 2015).
Our results (and those of others) have implications for how professionals involve caregivers within interventions for sensory behaviors. Child sensory behaviors are known to limit activities in families (Bagby et al., 2012; Little et al., 2015; Schaaf et al., 2011) and cause significant caregiver strain (Kirby, White, & Baranek, 2015) therefore involving families within meaningful caregiver-mediated interventions has the potential to impact both caregiver and child behaviors. Not only may involvement of caregivers result in a greater reduction of sensory behaviors due to generalizations outside the clinic, it may also increase feelings of caregiver confidence and reduced stress.
Study Limitations
Although a strength of our study is the relatively large sample of well-defined minimally verbal children, further research is required to expand and compare to children across the autism spectrum and to understand whether similar patterns of both child and caregiver behaviors are found in younger children and those with greater language abilities. The average chronological age of the sample was 6.32 years and their nonverbal age 3.95, therefore a comparison to both younger children and those with greater language abilities will allow researchers to identify differential patterns of caregiver response by age and functioning level, and also inform intervention approaches to these behaviors. The age of our sample may also have rendered some items (and therefore how caregivers respond to them) inappropriate. For example, caregivers may not approach an 8-year old in the same way as a 2-year old (for example, using tickling).
All the children in this study had received at least two years of early intervention prior to entering the study. Therefore, it is likely that caregivers would have been exposed to a range of intervention styles prior to completing the SEQ-2. This may explain the low rates of caregivers reporting using specific strategies such as OT or ABA. It could be possible that, through parent training, caregivers do not attribute their strategies (such as verbal or physical prompting) to a specific intervention unless delivered by an interventionist.
Content analysis is commonly used to explore themes and we employed both deductive and inductive forms of category generation in this study. However, the categories generated were subjective based on the authors’ expectations and previous literature, therefore further work is required to establish how common these strategies are in a wider sample of children with ASD, both using quantitative and qualitative methodologies. Caregivers were not required to report whether their responses were successful (e.g., stopping the child’s behavior or resulting in the child completing an activity), therefore it was not possible to explore whether certain strategies are more successful than others.
As described in our Methods section, we excluded any comments that caregivers made that did not report specific strategies or responses (such as Bath time is okay. Great with brushing teeth.). Although comments such as these were infrequent, they demonstrate that caregivers (and their children) can perceive sensory experiences as positive and positively share in sensory aspects of their experiences (as discussed by Bagby et al., 2012). It is important to acknowledge that not all sensory behaviors are negative for the child and/or caregiver and may result in pleasant, shared experiences. Although it is easy to assume that a greater number of child sensory behaviors and caregivers reporting of responses automatically leads to greater stress in caregivers (Ben-Sasson et al., 2013) and limited community participation for the family (Little et al., 2015), we did not include independent measures of stress or activity participation. The inclusion of additional caregiver report measures focused on family stress and community participation in future research could further elucidate the associations between child sensory behaviors and family functioning.
Conclusions
In summary, this study represents a comprehensive examination of parent report of sensory behavior displayed by minimally verbal children with ASD and their responses to these behaviors. Our results indicate that caregivers employed different responses based on the behavior displayed by their child and have implications for caregiver-mediated interventions targeting sensory behaviors.
Acknowledgments
This study was funded by Autism Speaks #5666, Characterizing Cognition in Nonverbal Individuals with Autism, an initiative begun by Ms. Portia Iverson and Cure Autism Now. Grant support was also provided by the National Institute of Child Health and Human Development (NICHD) R01HD073975-02 (C.K., A.K.) and R01HD073975-03 (C.K., R.L).
We thank Themba Carr and Stephanie Shire for their discussion of the findings.
Footnotes
Sections of this data were presented at the 50th Gatlinburg Conference in San Diego, CA.
Contributor Information
Clare Harrop, University of North Carolina at Chapel Hill.
Nicole Tu, University of California Los Angeles.
Rebecca Landa, Kennedy Krieger Institute.
Ann Kasier, Vanderbilt University.
Connie Kasari, University of California Los Angeles.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC. [Google Scholar]
- Anderson DK, Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, ….. Pickles A (2007). Patterns of growth in verbal abilities among children with autism spectrum disorder. Journal of Consulting and Clinical Psychology, 75(4), 594. doi: 10.1037/0022-006X.75.4.594 [DOI] [PubMed] [Google Scholar]
- Ausderau K, Sideris J, Furlong M, Little LM, Bulluck J, & Baranek GT (2014). National survey of sensory features in children with ASD: Factor structure of the sensory experience questionnaire (3.0). Journal of Autism and Developmental Disorders, 44(4), 915–925. doi: 10.1007/s10803-013-1945-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagby MS, Dickie VA, & Baranek GT (2012). How sensory experiences of children with and without autism affect family occupations. The American Journal of Occupational Therapy, 66(1), 78–86. doi: 10.5014/ajot.2012.000604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker AEZ, Lane A, Angley MT, & Young RL (2008). The relationship between sensory processing patterns and behavioural responsiveness in autistic disorder: A pilot study. Journal of Autism and Developmental Disorders, 38(5), 867–875. doi: 10.1007/s10803-007-0459-0 [DOI] [PubMed] [Google Scholar]
- Baranek GT (1999). Autism during infancy: A retrospective video analysis of sensory-motor and social behaviors at 9–12 months of age. Journal of Autism and Developmental Disorders, 29(3), 213–224. doi: 10.1023/A:1023080005650 [DOI] [PubMed] [Google Scholar]
- Baranek GT (2002). Efficacy of sensory and motor interventions for children with autism. Journal of Autism and Developmental Disorders, 32(5), 397–422. doi: 10.1023/A:1020541906063 [DOI] [PubMed] [Google Scholar]
- Baranek GT, Boyd BA, Poe MD, David FJ, & Watson LR (2007). Hyperresponsive sensory patterns in young children with autism, developmental delay, and typical development. Journal Information, 112(4), 233–245. doi: 10.1352/0895-8017(2007)112[233:HSPIYC]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Baranek GT, David FJ, Poe MD, Stone WL, & Watson LR (2006). Sensory Experiences Questionnaire: Discriminating sensory features in young children with autism, developmental delays, and typical development. Journal of Child Psychology and Psychiatry, 47(6), 591–601. doi: 10.1111/j.1469-7610.2005.01546.x [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, & Gal E (2009). A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(1), 1–11. doi: 10.1007/s10803-008-0593-3 [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Soto TW, Martnez-Pedraza F, & Carter AS (2013). Early sensory over-responsivity in toddlers with autism spectrum disorders as a predictor of family impairment and parenting stress. Journal of Child Psychology and Psychiatry, 54(8), 846–853. doi: 10.1111/jcpp.12035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodfish JW, Symons FW, & Lewis MH (1999). The repetitive behavior scale. Western Carolina Center Research Reports. [Google Scholar]
- Boyd BA, Baranek GT, Sideris J, Poe MD, Watson LR, Patten E, & Miller H (2010). Sensory features and repetitive behaviors in children with autism and developmental delays. Autism Research, 3(2), 78–87. doi: 10.1002/aur.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd BA, McBee M, Holtzclaw T, Baranek GT, & Bodfish JW (2009). Relationships among repetitive behaviors, sensory features, and executive functions in high functioning autism. Research in Autism Spectrum Disorders, 3(4), 959–966. doi: 10.1016/j.rasd.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd BA, McDonough SG, Rupp B, Khan F, & Bodfish JW (2011). Effects of a family-implemented treatment on the repetitive behaviors of children with autism. Journal of Autism and Developmental Disabilities, 41(10), 1330–1341. doi: 10.1007/s10803-010-1156-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case-Smith J, Weaver LL, & Fristad MA (2015). A systematic review of sensory processing interventions for children with autism spectrums disorders. Autism, 19(2), 133–148. doi: 10.1177/1362361313517762 [DOI] [PubMed] [Google Scholar]
- Creswell JW (2007). Qualitative inquiry and research design: Choosing among five traditions. Thousand Oaks, CA: Sage. [Google Scholar]
- Dickie VA, Baranek GT, Schultz B, Watson LR, & McComish CS (2009). Parent reports of sensory experiences of preschool children with and without autism: A qualitative study. The American Journal of Occupational Therapy.: Official Publication of the American Occupational Therapy Association, 63(2), 172–181. doi: 10.5014/ajot.63.2.172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn LM, & Dunn DM (2012). Peabody Picture Vocabulary Test, (PPVT-4). Johannesburg, South Africa: Pearson Education. [Google Scholar]
- Freuler A, Baranek GT, Watson LR, Boyd BA, & Bulluck JC (2012). Precursors and trajectories of sensory features: Qualitative analysis of infant home videos. The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association, 66(5), e81. doi: 10.5014/ajot.2012.004465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grahame V, Brett D, Dixon L, McConachie H, Lowry J, Rodgers J, … LeCouteur A (2015). Managing repetitive behaviours in young children with autism spectrum disorder (ASD): Pilot randomised controlled trial of a new parent group intervention. Journal of Autism and Developmental Disabilities, 45(10), 3168–82. doi: 10.1007/s10803-015-2474-x [DOI] [PubMed] [Google Scholar]
- Green J, Charman T, McConachie H, Aldred C, Slomins V, Howlin P, ….. PACT Consortium (2010). Parent-mediated communication-focused treatment in children with autism (PACT): A randomised controlled trial. The Lancet, 375(9732), 2152–2160. doi: 10.1016/S0140-6736(10)60587-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goods KS, Ishijima E, Chang Y-C, & Kasari C (2013). Preschool based JASPER intervention in minimally verbal children with autism: Pilot RCT. Journal of Autism and Developmental Disorders, 43(5), 1050–1056. doi: 10.1007/s10803-012-1644-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrop C, Gulsrud A, Shih W, Hovsepyan L, & Kasari C (2016). Charcaterizing caregiver responses to restricted and repetitive behaviors in toddlers with autism spectrum disorder. Autism, 20(3), 330–342. doi: 10.1177/1362361315580443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hresko WP, Reid DK, & Hammill DD (1999). Test of Early Language Development (TELD). Third Edition. Austin: Texas. PRO-ED. [Google Scholar]
- Hsieh H, & Shannon SE (2005). Three Approaches to Qualitative Content Analysis. Qualitative Health Research, 15(9), 1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Kasari C, Kaiser A, Goods K, Nietfeld J, Mathy P, Landa R, ….Almirall D (2014). Communication interventions for minimally verbal children with autism: A sequential multiple assignment randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(6), 635–646. doi: 10.1016/j.jaac.2014.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby A, White T, & Baranek G (2015). Caregiver strain and sensory features in children with autism spectrum disorder and other developmental disabilities. American Journal of Intellectual and Developmental Disabilities, 120(1), 32–45. doi: 10.1352/1944-7558-120.1.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane AE, Young RL, Baker AEZ, & Angley MT (2010). Sensory processing subtypes in autism: Association with adaptive behavior. Journal of Autism and Developmental Disorders, 40(1), 112–122. doi: 10.1007/s10803-009-0840-2 [DOI] [PubMed] [Google Scholar]
- Leekam SR, Nieto C, Libby SJ, Wing L, & Gould J (2007). Describing the sensory abnormalities of children and adults with autism. Journal of autism and developmental disorders, 37(5), 894–910. doi: 10.1007/s10803-006-0218-7 [DOI] [PubMed] [Google Scholar]
- Little LM, Ausderau K, Sideris J, & Baranek GT (2015). Activity participation and sensory features among child with autism spectrum disorders. Journal of Autism and Developmental Disorders,45(9), 2981–2990. doi: 10.1007/s10803-015-2460-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH Jr., Leventhal BL, DiLavore PC, ….Rutter M (2000). The Autism Diagnostic Observation Schedule-Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. doi: 10.1023/A:1005592401947 [DOI] [PubMed] [Google Scholar]
- Patten E, Ausderau KK, Watson LR, & Baranek GT (2013). Sensory response patterns in nonverbal children with ASD. Autism Research and Treatment. Article ID 436286, 9 pages, 2013. doi: 10.1155/2013/436286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton MQ (2002). Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage. [Google Scholar]
- Rogers SJ, Hepburn S, & Wehner E (2003). Parent reports of sensory symptoms in toddlers with autism and those with other developmental disorders. Journal of Autism and Developmental Disorders, 33(6), 631–642. doi: 10.1023/B:JADD.0000006000.38991.a7 [DOI] [PubMed] [Google Scholar]
- Rogers SJ, & Ozonoff S (2005). Annotation: What do we know about sensory dysfunction in autism? A critical review of the empirical evidence. Journal of Child Psychology and Psychiatry, 46(12), 1255–1268. doi: 10.1111/j.1469-7610.2005.01431.x [DOI] [PubMed] [Google Scholar]
- Roid GH, & Miller LJ (2002). Leiter International Performance Scale-Revised (Leiter-R): Wood Dale, IL. [Google Scholar]
- Schaaf RC, Toth-Cohen S, Johnson SL, Outten G, & Benevides TW (2011). The everyday routines of families of children with autism: Examining the impact of sensory processing difficulties on the family. Autism, 15(3), 373–389. doi: 10.1177/1362361310386505 [DOI] [PubMed] [Google Scholar]
- Shire SY, Goods K, Shih W, Distefano C, Kaiser A, Wright C, …Kasari C (2014). Parents’ Adoption of Social Communication Intervention Strategies: Families Including Children with Autism Spectrum Disorder Who are Minimally Verbal. Journal of Autism and Developmental Disorders, 45(6), 1712–24. doi: 10.1007/s10803-014-2329-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tager-Flusberg H, & Kasari C (2013). Minimally verbal school – aged children with autism spectrum disorder: The neglected end of the spectrum. Autism Research, 6(6), 468–478. doi: 10.1002/aur.1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomchek SD, & Dunn W (2007). Sensory processing in children with and without autism: A comparative study using the short sensory profile. American Journal of Occupational Therapy, 61(2), 190–200. doi: 10.5014/ajot.61.2.190 [DOI] [PubMed] [Google Scholar]
- Watson LR, Patten E, Baranek GT, Poe M, Boyd BA, Freuler A, & Lorenzi J (2011). Differential associations between sensory response patterns and language, social, and communication measures in children with autism or other developmental disabilities. Journal of Speech, Language, and Hearing Research, 54(6), 1562–1576. doi: 10.1044/1092-4388(2011/10-0029) [DOI] [PMC free article] [PubMed] [Google Scholar]