Abstract
Introduction
Poison is defined as any chemical that has the potential to affect or harm human physiology due to its chemical activity. Poisoning is becoming a major preventable public health issue in many countries, including Ethiopia. There is a variation in acute poisoning mortality among the existing evidence in Ethiopia. This study aims to determine the pooled mortality rate from acute poisoning and its predictors in Ethiopia.
Methods
We searched available evidence of acute poisoning mortality in databases such as PubMed, Hinari, Cochrane, ScienceDirect, and other search engines. Using the Microsoft Excel data extraction form, three authors independently extracted all relevant data. The Higgins I2 test statistics were used to examine heterogeneity among included studies A random-effects model was used to analyze the pooled estimates and predictors in Stata MP version 17.
Results
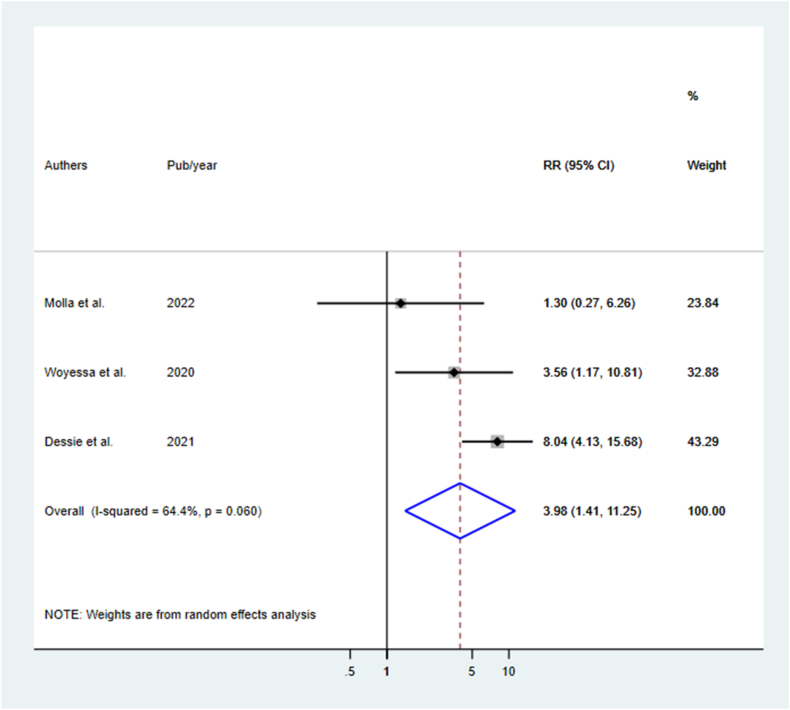
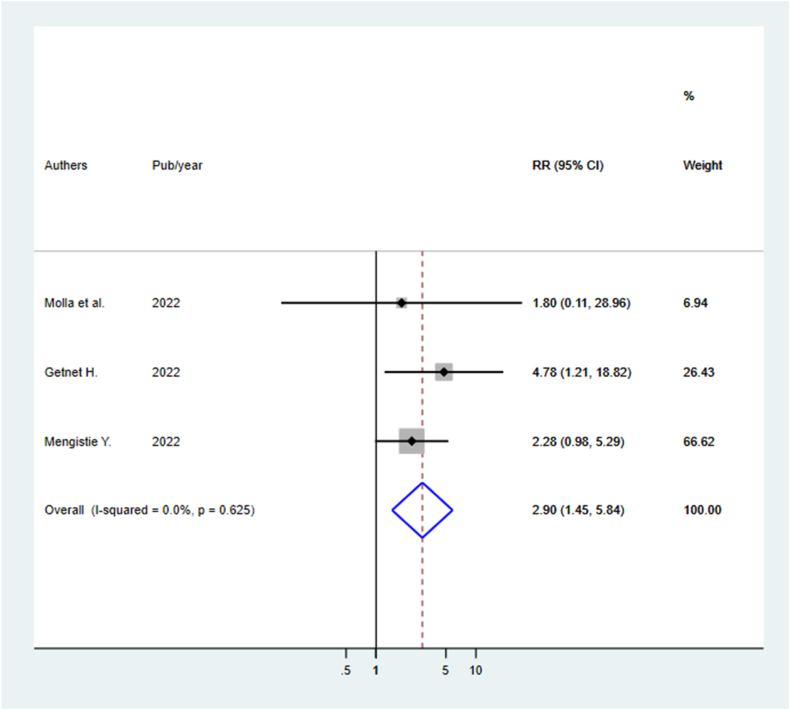
We retrieved 2685 relevant records from different database sources, and after screening, 21 studies (17 published and 4 unpublished) were included. The pooled mortality rate for acute poisoning was 4.69(95 % CI: 3.69, 5.69 I2 = 94.7 %). The most common poisoning agents are organophosphate (29.9 %), household cleansing agents (17.5 %), and pharmaceuticals/medications (9.3 %). The majority of poisoning cases were intentional poisoning committed suicide. Poisoning cases in rural areas [RR: 3.98(95 % CI: 1.41, 11.25)] and delayed arrival times [RR: 2.90(95 % CI: 1.45, 5.84)] were identified predictors of mortality.
Conclusions
In this study, the pooled mortality from acute poisoning was 4.69 %. Poisoned cases from rural areas and delayed arrival times to the hospital were predictors of mortality. To prevent mortality, healthcare professionals should give special attention to rural residents and delayed arrival of poison cases. To control this avoidable death, poison control centers should be strengthened, and other preventive measures implemented at the national level.
Keywords: Acute poisoning, Mortality, Predictors, Ethiopia
1. Introduction
Poison is defined as any chemical that can alter or harm humans’ normal physiology through general or local cell damage or death by its chemical activity [[1], [2], [3]]. Poisoning is becoming a major public health problem in many countries [[4], [5], [6]]. It is the most common reason for a visit to the emergency department, with severe consequences such as morbidity, hospitalization, mortality, and financial crisis [[1], [2], [3],[7], [8], [9]]. The incidence of poisoning is not accurately known due to a paucity of records and unreported cases [2,10,11]. Globally, around 370,000 and 193,469 deaths are recorded each year due to intentional and unintentional poisonings, respectively. Low and middle-income countries account for (84 %) of poisoning incidents [12,13]. Unintentional poisoning is the most common in children under 5 years, while intention poisoning increases between 13 and 19 years [[14], [15], [16]].
The poisoning mortality rate in India ranges from 0.99 % to 5 % [[16], [17], [18]], 5.35 % in South Korea [19], and 5.1 % in Nepal [20]. According to the World Health Organization (WHO), unintentional poisoning caused an estimated 16,500 deaths in sixteen African countries. It ranges from 0.3 in Mauritius to 8.1 in Mozambique per 100,000 people, but this is underestimated the actual figure due to unreported cases [5]. Poisoning mortality rates in Ethiopia were 27.6 % in Mettu [2], 5.8 % in Jimma [21], 7.1 % in Wollega [7], 0.3 % in Gondar [22], and 62 % in Bahir Dar [23]. Pesticide poisoning kills about 300,000 people per year around the world [2,24]. Pesticide self-poisoning accounts for approximately 20 % of all suicides worldwide and is mostly linked to growing widespread use in agricultural areas in low and middle-income countries [4,9,25,26].
The pattern of poisoning varies between countries and geographical areas; pesticides, kerosene, household cleaning products, traditional medicines, and natural toxins are the most common poisoning agents [3,5,12,13]. In countries with an agrarian economy, organophosphates are the most common farming insecticides, herbicides, and pesticide agents that remain as poisoning agents [12,27]. It also accounts for the majority of suicide attempts in many under-developing countries [27,28]. According to evidence, unmet expectations, changing or breaking down of local cultures, chronic disease states, business loss, love failure, illiteracy, younger age, gender, marital status, and living alone are the reasons for intentional poisoning [2,12,17,29]. However, weak regulatory activities, residence, sex, arrival time to the hospital, length of hospital stay, management type, mode of poisoning, and age were all identified as risk factors for poisoning mortality [1,3,7,[30], [31], [32]]. Poison control centers are important measures to reduce morbidity and mortality from poisoning because they facilitate poisoning diagnosis, treatment, and preventive measures [5,9,10,33]. Ethiopia lacks a well-organized poison control center, making it extremely difficult to obtain primary data on poisoning cases and mortalities before reaching the hospitals [8,33]. There is substantial variation in evidence of acute poisoning mortality between regions in Ethiopia [2,21,34]. Additionally, no systematic review and meta-analysis has been done to enhance the quality and consistency of the evidence. The purpose of this systematic review and meta-analysis was to determine the pooled mortality of acute poisoning and its predictors in Ethiopia using available evidence. This study will help health professionals, policymakers, programmers, and planners establish and enforce case management, and control strategies, as well as implement effective interventions, to reduce the preventable mortality burden in Ethiopia.
2. Materials and methods
2.1. Search strategy
Three authors (ATT, SDH, and BE) independently searched PubMed, Hinari, Cochrane, ScienceDirect, Google Scholar, and other search engines for articles reporting poisoning-related mortalities (S1 Table). Our search was extended by doing hand searches for gray literature and retrieving reference lists of eligible articles. The literature search was completed in March 2023. The Condition, Context, and Population (CoCoPop) criteria were employed to search the databases using a comprehensive searching strategy that included common Boolean words such as Mortality OR Outcome OR Acute poisoning OR poisoning OR epidemiology OR associated factors OR predictors AND Ethiopia OR Federal Democratic of Ethiopia AND all poisoned cases. We presented this systematic review and meta-analysis by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [35]. Publications with incomplete data will be rectified by contacting the corresponding author. It was then exported to EndNote version 20.4 software to manage duplicated articles.
2.2. Protocol registration
This systematic review and meta-analysis were registered under the PROSPERO 2023 ID: CRD42023404236. The protocol was published by the National Institute for Health Research University of York PROSPERO International Prospective Register of Systematic Reviews. Some amendments were made to the information provided at registration or in the protocol.
2.3. Eligibility criteria
Inclusion criteria: Before the search began, eligibility criteria were determined. We included all published and unpublished observational studies that reported acute poisoning mortality/death. This review included studies conducted in Ethiopia and published in English.
Exclusion criteria: Case reports/series, systematic reviews, books, and guidelines were all excluded. Articles reporting no mortality from acute poisoning were not included. Moreover, articles that were not fully accessible, despite at least two email contacts with the primary authors were removed due to the difficulties of assessing the quality of articles without full text.
2.4. Data extraction
Three different authors (ATT, SDH, and BE) searched articles, (ATT, MYB, and KW) independently screened the retrieved articles using their titles and abstract, and (ATT, TA, and GG) extracted data using a predetermined Microsoft Excel spreadsheet format. The data extraction format includes the first author, publication year (which was used as the study year for unpublished articles), study area, participant age, sample size, response rate, intentional poisoning rate, and mortality rate. Any disagreements among authors during the extraction were resolved by discussion and mutual agreement with the help of a fourth author (DT).
2.5. Outcome measurement
In this study, estimating mortality rates and identifying predictors are the outcomes reported from this systematic review and meta-analysis. The primary outcome is the pooled acute poisoning mortality rate. This is computed by the number of mortalities divided by the number of acute poisoning cases included in the studies (sample size) and multiplied by 100. The relative risk (RR) of predictor variables was calculated using the two-by-two tables with binary outcomes of residence (rural/urban), arrival time to the hospital (≤1 h/>1 h), length of hospital stay (≤48 h/>48 h), and sex (male/female).
2.6. Quality assessment
The Newcastle Ottawa Scale for cohort studies was used to assess the quality of the included studies. The tool has three main dimensions: the first dimension addresses the assessment of the selection of the exposed and non-exposed groups using the representativeness of the exposed group, the selection of the non-exposed cohort, ascertainment of exposure, and demonstration of the outcome of interest, which was not present at the beginning of the study. The second dimension assesses the comparability of the cohorts based on the design or analysis. The third dimension examines the quality of outcome addressing through assessment of the outcome, ways to follow-up long enough for the outcome to occur, and adequacy of follow-up of cohorts [36,37]. The study gets a score of ≥5 stars from a total of 9 scores considered as high quality (S2 and 3 Tables).
2.7. Statistical data analysis
The data were extracted using Microsoft Excel and then exported to Stata MP version 17 software meta-analysis package for analysis. We calculate the effect size for individual studies by generating incidence to each study using mortalities divided by sample size and multiplied by 100 (incidence = mortalities/sample size *100). Then the incidence is transformed to standard error using incidence multiplied by after (incidence subtracted from 100) and divided by sample size (standard error incidence = incidence*(100-incidence)/sample size). We used tables and forest plots to present the results. The pooled estimate of the meta-analysis, together with a 95 % confidence interval (CI), was presented using a forest plot. Heterogeneity between studies was assessed by the calculated p-value of Higgins I2-test statistics; values 25 %, 50 %, and 75 % indicated low, moderate, and high heterogeneity testing, respectively [38]. To assess publication bias, a funnel plot visual inspection and Egger's objectivity test were used with slope intercept p-value less than 0.05 [39,40]. A random-effect model was used as a method of analysis to test results in the presence of heterogeneity [41,42]. In addition, to execute the heterogeneity among the included studies, subgroup analysis was done based on the group's regions of country, age, follow-up period, sample size, publication year, proportion of participants' response, and intentional poisoning.
3. Results
3.1. Description of selection procedure eligible articles
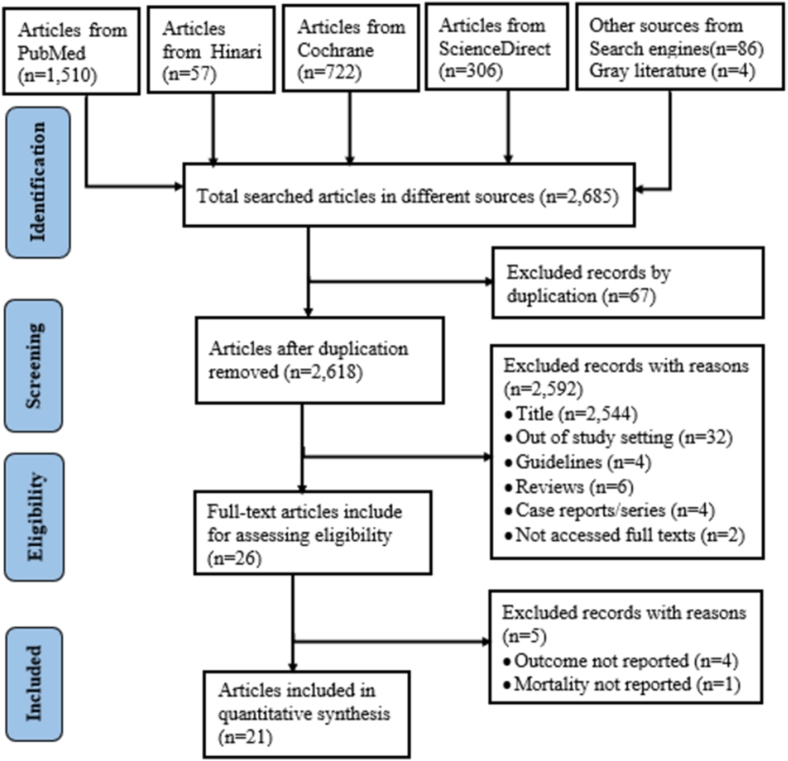
We retrieved 2685 relevant records from databases PubMed, Hinari, Cochrane, ScienceDirect, and other search engine sources. After excluding duplications, 2618 articles were screened. Finally, 21 articles (17 published and 4 unpublished) were included in this systematic review and meta-analysis (Fig. 1).
Fig. 1.
Flow diagram to show the article selection procedure for systematic review and meta-analysis.
3.2. Characteristics of the included studies
In this study, 21 studies met the inclusion criteria and included in systematic review and meta-analysis among those only four studies [31,32,43,44] were unpublished. All of the studies were conducted in four regions: nine in Amhara [3,22,23,30,31,43,[45], [46], [47]], five in Addis Ababa [13,32,44,48,49], six in Oromia [1,2,7,21,50,51], and the last one study in Harar [52], with a total of 4196 respondents. The included studies’ follow-up period ranges from 1.8 months in Dessie [3] to 6 years in Jimma [51]. The smallest and largest estimated sample sizes were 76 in Mettu [2] and 998 in Addis Ababa [49], respectively. The lowest response rate in the included study was 59.3 % [49]. The mortality rate in the included studies ranges from 0.3 % in Gondar [22] to 62 % in Bahir Dar [23]. The proportion of intentional poisoning ranges from 31 % in Gondar [22] to 100 % in Bahir Dar [43,46] (Table 1). The majority of the included studies do not provide distinct arrival timings and lengths of hospital stays. Despite this, four studies reported hospital arrival times of less than 30 min [21,32,43,46], with only one study reporting an arrival time of 96 h following poisoning exposure [32]. Similarly, only 9 studies reported the length of hospital stay; of these, the minimum length of stay was one day [13], and the maximum was 11 days [46].
Table 1.
Characteristics of 21 studies reported the mortality of acute poisoning in Ethiopia.
| Authors | Pub/year | Region (area) | Ages | Follow-up period in months | Samples | Response rate (%) | Intentional poisoning (%) | Mortality rate (%) |
|---|---|---|---|---|---|---|---|---|
| Adinew et al. [22] | 2017 | Amhara (NGZ) | All ages | 52 | 543 | 63.4 | 31 | 0.3 |
| Bereda et al. [2] | 2021 | Oromia (Mettu) | All ages | 13 | 76 | 100 | 64.5 | 27.6 |
| Bogale et al. [46] | 2021 | Amhara (BDR) | All ages | 30 | 141 | 89 | 100 | 31.2 |
| Chala et al. [50] | 2015 | Oromia (Adama) | All ages | 24 | 292 | 100 | 36.6 | 1.37 |
| Desalew et al. [48] | 2011 | Addis Ababa | Adults | 24 | 116 | 100 | 96.6 | 8.6 |
| Eyasu et al. [49] | 2017 | Addis Ababa | Adults | 60 | 998 | 59.3 | 85.5 | 1.2 |
| Getie et al. [3] | 2020 | Amhara (Dessie) | All ages | 1.8 | 147 | 81.6 | 64.2 | 6.6 |
| Molla et al. [30] | 2022 | Amhara (Gondar) | Children | 48 | 103 | 79.6 | 24.4 | 8.5 |
| Nigussie et al. [52] | 2022 | Harar | All ages | 60 | 175 | 85.2 | 51.3 | 16.7 |
| Shumet et al. [23] | 2022 | Amhara (BDR) | All ages | 12 | 121 | 100 | 98.3 | 62 |
| Tefera et al. [1] | 2020 | Oromia (Ambo) | All ages | 14.5 | 134 | 100 | 76.9 | 1.5 |
| Teklemariam et al. [21] | 2016 | Oromia (Jimma) | All ages | 24 | 110 | 93.6 | 50.5 | 5.8 |
| Woyessa et al. [7] | 2020 | Oromia (Wollega) | All ages | 10 | 211 | 100 | 46.45 | 7.1 |
| Zemedie et al. [13] | 2021 | Addis Ababa | All ages | 12 | 98 | 100 | 98 | 10.2 |
| Adinew et al. [45] | 2016 | Amhara (Gondar) | All ages | 52 | 233 | 100 | 57.5 | 0.43 |
| Dessie et al. [32] | 2021 | Addis Ababa | Adults | 36 | 218 | 83.9 | 92.3 | 13.7 |
| Melese et al. [44] | 2018 | Addis Ababa | All ages | 12 | 306 | 93.2 | 88.5 | 8.4 |
| Getnet H [43] | 2022 | Amhara (BDR) | Adults | 12 | 268 | 100 | 100 | 20.9 |
| Endayehu et al. [47] | 2019 | Amhara (DT) | All ages | 36 | 102 | 100 | 91.2 | 18.6 |
| Ahmed et al. [51] | 2018 | Oromia (Jimma) | All ages | 72 | 236 | 100 | 76.7 | 6.4 |
| Mengistie Y [31] | 2022 | Amhara (BDR) | Adults | 24 | 304 | 100 | 88.2 | 30.6 |
*Note: NGZ: North Gondar Zone; BDR: Bahir Dar; DT: Debre Tabor.
3.3. The magnitude of poisoned cases by type of poisoning agent
In the 21 studies that were included, 15 types of known poisoning agents were reported. Three most common poisoning agents reported were organophosphate 1255(29.9 %), bleach/household cleaning agents 735(17.5 %), and pharmaceuticals/medications 390(9.3 %). Hydrogen peroxide, snake venom, and herbal/traditional medicines account for the least poisoning cases (Table 2).
Table 2.
Number of poisoned cases by type of poisoning agents in Ethiopia.
| S/no | Types of poisoning agents | Number of poisoned cases (N) | Percent (%) |
|---|---|---|---|
| 1 | Organophosphates | 1255 | 29.9 |
| 2 | Bleach/household cleaning agent | 735 | 17.5 |
| 3 | Pharmaceuticals/medications | 390 | 9.3 |
| 4 | Other/unknown chemicals | 285 | 6.8 |
| 5 | Rodenticides | 262 | 6.2 |
| 6 | Aluminum phosphate | 224 | 5.3 |
| 7 | Alcohol | 200 | 4.8 |
| 8 | Organ chemicals/pesticides | 197 | 4.7 |
| 9 | Rate poison | 187 | 4.5 |
| 10 | Carbon monoxide | 176 | 4.2 |
| 11 | Food poisoning | 114 | 2.7 |
| 12 | Kerosene/Benzine | 65 | 1.5 |
| 13 | Herbal/Traditional medication | 58 | 1.4 |
| 14 | Snake Venom | 39 | 0.9 |
| 15 | Hydrogen peroxide | 9 | 0.2 |
3.4. Meta-analysis
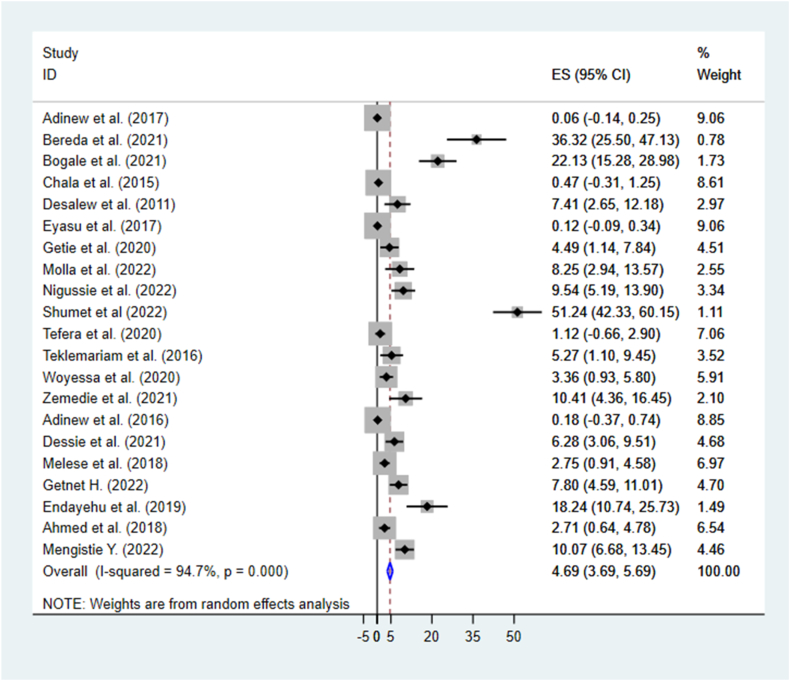
The pooled mortality rate from acute poisoning in this systematic review and meta-analysis was 4.69(95 % CI: 3.69, 5.69, I2 = 94.7 %). The I2 test revealed high heterogeneity among included studies; the model used random effect (I2 = 94.7 %, P =<0.001) (Fig. 2).
Fig. 2.
The pooled mortality rate of acute poisoning in Ethiopia.
3.5. Subgroup analysis
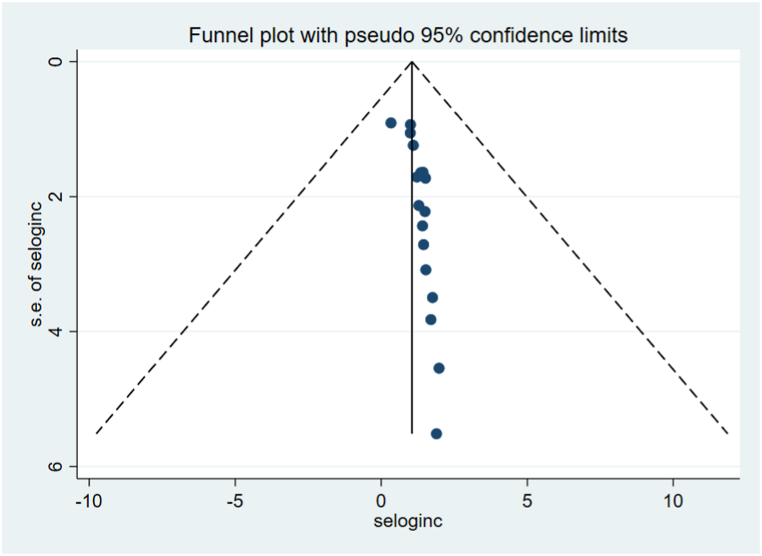
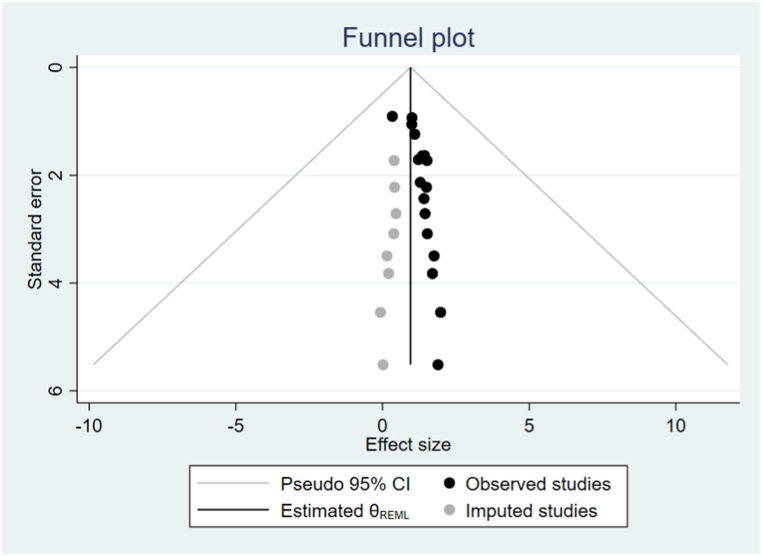
In this systematic review and meta-analysis, we investigated study heterogeneity used subgroup analysis. The highest mortality rate was observed in Amhara 9.30(95 % CI: 6.78, 11.82), followed by Addis Ababa 4.61(95 % CI: 1.37, 7.84). Similarly, the mortality rate was higher in the last 5 years of publication 11.24(95 % CI: 7.79, 14.69), and above 72.3 % of intentional poisoning cases 9.87(95 % CI: 6.52, 13.21) (Table 3). To examine publication bias between included studies, funnel plot visual inspection, and it appears asymmetric distribution of studies shows the presence of publication bias (Fig. 3) This was also checked by performing the Eggers objectivity test, which indicates the presence of publication bias (p < 0.001). Hence, trim and fill analysis was used to alter the pooled mortality rates of acute poisoning (Fig. 4).
Table 3.
Subgroup analysis of mortality rate of acute poisoning in Ethiopia.
| Variable | Characteristics | No. studies | Study participants | Mortality rate at (95 % CI) | I2 tests (%) |
|---|---|---|---|---|---|
| Region | Amhara | 9 | 1699 | 9.30(6.78, 11.82) | 96.9 |
| Oromia | 6 | 1052 | 4.23(1.34, 7.12) | 90.5 | |
| Addis Ababa | 5 | 1295 | 4.61(1.37, 7.84) | 90.3 | |
| Harar | 1 | 150 | 9.54 (5.19, 13.90) | – | |
| Age groups | All ages | 15 | 2651 | 5.93(4.31, 7.56) | 95.2 |
| Adults only | 5 | 1463 | 6.20(1.21, 11.18) | 94.8 | |
| Children only | 1 | 82 | 8.25(2.94, 13.57) | – | |
| Follow-up period | ≤30 months | 13 | 2274 | 10.36(6.91, 13.82) | 95.3 |
| >30 months | 8 | 1922 | 1.29(0.51, 2.08) | 90.0 | |
| Sample size | ≤234 | 14 | 1854 | 11.44(7.72, 15.17) | 95.5 |
| >234 | 7 | 2342 | 1.50(0.72, 2.29) | 91.4 | |
| Publication year | 2018–2022a | 15 | 2516 | 11.24(7.79, 14.69) | 93.7 |
| 2017 and before | 6 | 1680 | 0.24(0.12, 0.60) | 68.9 | |
| Response rate | <100 % | 9 | 2005 | 2.70(1.67, 3.73) | 92.1 |
| 100 % | 12 | 2191 | 8.85 (6.13, 11.57) | 95.8 | |
| Intentional poisoning | ≤72.3 % | 9 | 2090 | 2.85(1.51, 4.20) | 91.1 |
| >72.3 % | 12 | 2994 | 9.87(6.52, 13.21) | 96.2 |
Note.
Used publication year as study year for unpublished articles.
Fig. 3.
Funnel plot analysis of included studies for mortality of acute poisoning in Ethiopia.
Fig. 4.
Fill and trim funnel plot analysis for mortality of acute poisoning in Ethiopia.
3.6. Predictors of mortality acute poisoning
In this systematic review and meta-analysis, participants’ residence and arrival time at the hospital were identified as predictors of acute poisoning mortality. Three studies with a sample size of 532 reported the association between residence and mortality from acute poisoning [7,30,32]. Poisoned cases from rural residents were 4 times more at risk of mortality compared to counterparts of urban residents [RR: 3.98(95 % CI: 1.41, 11.25)] (Fig. 5). Similarly, delayed arrival time to the hospital after poison exposure was a statistical predictor of mortality reported in three studies with the sum of sample sizes 675 [30,31,43]. Poisoned cases who arrived at the hospital after 1 h of poisoning exposure to the hospital were nearly three times more at risk of mortality compared who arrived within 1 h of exposure [RR: 2.90(95 % CI: 1.45, 5.84)] (Fig. 6). However, length of hospital stay from three studies [1,30,43] and sex from two studies [1,31] were not statistically significant predictors of mortality.
Fig. 5.
Predictors of mortality of acute poisoning in Ethiopia by the residence of the participants.
Fig. 6.
Predictors of mortality of acute poisoning in Ethiopia by arrival time after poisoning exposure.
4. Discussion
Acute poisoning is becoming a public health problem and the major cause of emergency department hospitalization, morbidity, and mortality globally [[4], [5], [6],11,12,53,54]. The majority of them are deliberate self-poisoning committed to suicide, which is the most preventable mortality [4,5,28,33,54,55]. This systematic review and meta-analysis tried to assess the pooled acute poisoning mortality rate in Ethiopia. In this study, the pooled mortality rate of acute poisoning was 4.69 (95 % CI: 3.69, 5.69, I2 = 94.7 %). This finding is consistent with previous evidence reported 4 % in Southern and 5 % in South-Eastern India [16,18], and 5.1 % in Nepal [20]. This study was higher than the systematic review and meta-analysis study conducted 0.8 % in Iran [56]. The previous study's inclusion of a different study population in pediatrics may have the possible reason for to decrease in mortality rates. This finding is higher in the single studies reported: 1.1 % in Saudi Arabia [57], 0.99 % in Karnataka and 2.4 % in Bengaluru India [17,58], and 2.6 % in Taiwan [59]. The difference might be attributed to the study setting, design, and sample size. Previous studies were carried out with a high level of knowledge, awareness, and use of technology, large sample sizes, and the presence of well-functioning poison control strategies.
This finding is lower than those reported in systematic reviews and meta-analyses: 7 % in Thailand [55], 27 % [60] in Iran, and 13.7 % in pesticide poisoning globally [61]. This variation might be due to differences in the study setting, which resulted in strengthened poison information and control centers for early tracking mortalities, the availability of new poisoning agents, and increased accessibility to pharmaceuticals in the previous studies. The study population's awareness level and usage of technology have also played a pivotal role in reporting poisoning cases and associated health outcomes in Thailand and Iran [55,62]. In Ethiopia, there is weak regulatory activity, and the increased utilization of agricultural chemicals such as herbicides, pesticides, and rodenticides has boosted poisoning incidents recently [25,26,33,[63], [64], [65]]. However, the current study lacks the ability to track unreported poisoning cases and mortality rates, which may underestimate the national incidence of acute poisoning mortality. Furthermore, this is also lower single studies reported ranges from 6.4 % to 16.5 % [27,[66], [67], [68], [69], [70]] in different regions, including poison information centers in India, 8.3 % in Bangladesh [71], and 20.8 % in Korea [19]. This might be due to differences in study settings and incomparability of single study mortality with the pooled effect size resulting from the mortality of multiple studies.
Organophosphates 1255(29.9 %), bleach/household cleaning agents 735(7.5 %), pharmaceuticals/medications 390(9.3 %), other/unknown chemicals 285(6.8 %), and rodenticides 262(6.2 %) were the most common five poisoning agents reported in this study. This is supported by previous systematic reviews in Ethiopia, Iran, and the multi-country developing world [56,[72], [73], [74]]. There are also no significant variations between the single studies' reported in Iran, which found that pharmaceutical drugs, pesticides, and insecticides are the leading causes of poisoning [62,75]. Pesticides followed by household agents, and pharmaceutical products are the major causes of poisoning in Thailand [55]. Similarly, other studies’ findings are consistent with this finding reported in India, Bangladesh, and multicounty studies [18,58,[69], [70], [71],[76], [77], [78]].
The majority of the studies included in this systematic review and meta-analysis study reported that the reason for poisoning was intentional poisoning for self-suicidal attempts, ranging from 24.4 % [30] to 100 % [43,46]. This is consistent with the previous evidence conducted in Ethiopia, South Africa, Thailand, India, Korea, and Nepal [19,20,55,67,[72], [73], [74],76,78,79].
The predictors of acute poisoning mortality are not well addressed in published articles (most of the existing evidence is descriptive studies). In this systematic review and meta-analysis study, rural residents’ acute poisoning cases were identified as predictors of mortality compared to urban residents. This finding is consistent with the study conducted in Sira Lanka and Zambia [80,81]. Rural dwellers are illiterate, have low health-seeking behaviors, are inaccessible to health facilities due to transportation problems, and have poor availability of health resources in the nearby health facilities. This might be the possible reason for the delay in seeking poisoned treatment, increasing the likelihood of severe complications and major organ failures that lead to mortality. Hospital arrival time following poisoning exposure was a statistical predictor of acute poisoning mortality. This is consistent with previous evidence reported in different studies in India and Nepal [18,20,67]. The clinical management of poisoning and the outcome of treatment are determined by the timing of arrival after exposure. Delayed arrival time to the hospital may increase mild to severe health conditions including headache, vomiting, tachypnea, tachycardia, altered consciousness, comma, abdominal pain, bleeding, epigastric pain, and major organ failure, which can lead to mortality [24,54,67,82,83]. Nevertheless, length of hospital stay and sex were not statistical predictors for acute poisoning mortality in this systematic review and meta-analysis. This evidence is not in line with previous findings in Ethiopia and Sri Lanka [73,84]. This might be due to the small sample size of individual studies, as well as the small number of articles that reported predictors of mortality, which could obscure the association when the effect size of multiple studies is pooled.
In subgroup analysis revealed that Amhara region, adults, follow-up period 2.5 years and less, small sample size, high response rate, and intentionally poisoned groups had higher mortalities. This is attributable to the region's huge number of studies, the higher likelihood of suicide attempts in adults, the fact that deliberate self-poisoning cases are self-suicidal, and the traceability of current patient charts. All of these reasons may increase acute poisoning mortality rates compared to counterparts in this study. In general, hospital arrival time, residence, and length of hospital stay are clinically relevant variables for preventing acute poisoning mortality and require great attention in clinical settings and the community as a whole.
5. Limitations of the study
Due to a lack of available evidence, this study was unable to cover all parts of the country.
6. Conclusions
In this systematic review and meta-analysis, preventable acute poisoning mortality was 4.69 %. Rural dwellers and delayed arrival times to the hospital were identified as predictors of acute poisoning mortality. Health promotion and education activities are encouraged to prevent this looming public health problem. Healthcare professionals devote special attention to acute poisoning cases from rural areas and those with delayed hospital arrival times. All higher-level official bodies should have well-functioning and strengthened poison information and control centers. Implement immediate interventions and other national-level initiatives to prevent such preventable mortalities. Moreover, further multicenter prospective studies with large sample sizes should be conducted to address unreported cases, chart incompleteness, regions with no prior evidence, and potential predictors of acute poisoning mortality.
Ethics approval and consent to participate
Not applicable.
Consent to publication
Not applicable.
Availability of data and materials
Not applicable or all data used in this study was presented in this document.
Funding statement
This research has not received specific funding.
CRediT authorship contribution statement
Animut Takele Telayneh: Writing – review & editing, Writing – original draft, Visualization, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Samuel Derbie Habtegiorgis: Writing – review & editing, Writing – original draft, Validation, Software, Methodology, Investigation, Formal analysis, Data curation. Molla Yigzaw Birhanu: Writing – review & editing, Writing – original draft, Validation, Supervision, Software, Investigation, Data curation. Bickes Wube Sume: Writing – review & editing, Writing – original draft, Supervision, Software, Methodology, Investigation, Formal analysis. Temesgen Ayenew: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Resources, Methodology, Investigation. Getnet Gedif: Writing – review & editing, Writing – original draft, Validation, Supervision, Methodology, Investigation, Formal analysis, Data curation. Bekalu Endalew: Writing – review & editing, Writing – original draft, Visualization, Validation, Methodology, Investigation, Formal analysis, Data curation. Dejenu Tsegaye: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Methodology, Formal analysis, Data curation. Getasew Yirdaw: Writing – review & editing, Writing – original draft, Software, Methodology, Investigation, Formal analysis, Data curation. Kalkidan Worku Mitiku: Writing – review & editing, Writing – original draft, Supervision, Software, Methodology, Formal analysis, Data curation. Frehiwot Molla: Writing – review & editing, Visualization, Validation, Software, Methodology, Formal analysis, Data curation. Nurilign Abebe Moges: Writing – review & editing, Writing – original draft, Software, Methodology, Formal analysis, Data curation. Getachew Mullu Kassa: Writing – review & editing, Writing – original draft, Software, Methodology, Formal analysis, Data curation.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:Animut Takele reports administrative support was provided by Debre Markos University. Animut Takele reports a relationship with Debre Markos University that includes: employment. Animut Takele has patent pending to no. No If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would like to acknowledge the authors of the included articles.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e29741.
Contributor Information
Animut Takele Telayneh, Email: animuttakele@gmail.com.
Samuel Derbie Habtegiorgis, Email: kasadr21@gmail.com.
Molla Yigzaw Birhanu, Email: mollayigzaw33@gmail.com.
Bickes Wube Sume, Email: bkswbe123@gmail.com.
Temesgen Ayenew, Email: teme31722@gmail.com.
Getnet Gedif, Email: Get4ged@gmail.com.
Bekalu Endalew, Email: bekiehsm@gmail.com.
Dejenu Tsegaye, Email: dejenetsegaye8@gmail.com.
Getasew Yirdaw, Email: gech23man@gmail.com.
Kalkidan Worku Mitiku, Email: promisegold07@gmail.com.
Frehiwot Molla, Email: mollafrehiwot@gmail.com.
Nurilign Abebe Moges, Email: nure113@gmail.com.
Getachew Mullu Kassa, Email: gechm2005@gmail.com.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Tefera G.M., Teferi L.G. Prevalence, predictors and treatment outcome of acute poisoning in Western Ethiopia. Open Access Emerg. Med.: OAEM. 2020;12:365. doi: 10.2147/OAEM.S277269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bereda G., Bereda G. Incidence, circumstances, and predictors of acute poisoning in the emergency department of Mettu Karl Referral Hospital, South Western, Ethiopia: a retrospective cross-sectional study. International Journal of Advanced Research in Biological Sciences. 2021;8(7):81–89. [Google Scholar]
- 3.Getie A., Belayneh Y.M. A retrospective study of acute poisoning cases and their management at the emergency department of Dessie Referral Hospital, Northeast Ethiopia. Drug Healthc. Patient Saf. 2020;12:41. doi: 10.2147/DHPS.S241413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . Geneva World Health Organization; 2020. Guidelines for Establishing a Poison Center. [Google Scholar]
- 5.World Health Organization . World Health Organization; Geneva: 2015. Improving the Availability of Poisons Center Services in Eastern Africa: Highlights from a Feasibility Study for a Subregional Poison Center in the Eastern Africa Subregion, Including a Toolkit on Setting up a Poisons Information Service. [Google Scholar]
- 6.Yuan X., Kou C., Zhang M., Ma W., Tang Z., Sun H., Li W. Injury and poisoning mortality trends in urban and rural China from 2006 to 2020 based on age-period-cohort analysis. Int. J. Environ. Res. Publ. Health. 2022;19(12):7172. doi: 10.3390/ijerph19127172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woyessa A.H., Palanichamy T. Patterns, associated factors, and clinical outcomes of poisoning among poisoning cases presented to selected hospitals in Western Ethiopia: a hospital-based study. Emergency Medicine International. 2020;2020 doi: 10.1155/2020/5741692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gebremariam E., Gelaw B. Global epidemiology of acute poisoning with an emphasis on Ethiopia: a systematic review. International Journal of Pharma Sciences and Scientific Research. 2016;2(4):120–130. [Google Scholar]
- 9.World Health Organization . 2020. Guidelines for Establishing a Poison Center. [Google Scholar]
- 10.World Health Organization . Geneva World Health Organization; 1997. Guidelines for Poison Control. [Google Scholar]
- 11.Bacha T., Tilahun B. A cross-sectional study of children with acute poisoning: a three-year retrospective analysis. World Journal of Emergency Medicine. 2015;6(4):265. doi: 10.5847/wjem.j.1920-8642.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nadeem M.N., Maqdoom M., Akif M.E. A Prospective observational study on pattern of poisoning cases reported to the emergency department of a teaching hospital in South India. Biomedical and Pharmacology Journal. 2020;13(4):1863–1869. [Google Scholar]
- 13.Zemedie B., Sultan M., Zewdie A. Acute poisoning cases presented to the Addis Ababa burn, emergency, and trauma hospital emergency department, Addis Ababa, Ethiopia: a cross-sectional study. Emergency Medicine International. 2021;2021 doi: 10.1155/2021/6028123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silver E., Oller L.K., White K., Coons D.M., Thornton S.L. 2019 annual report of the Kansas poison control center at the university of Kansas health system. Kansas Journal of Medicine. 2021;14:87. doi: 10.17161/kjm.vol1414886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gummin D.D., Mowry J.B., Beuhler M.C., Spyker D.A., Brooks D.E., Dibert K.W., Rivers L.J., Pham N.P., Ryan M.L. 2019 Annual report of the American Association of poison control centers' National Poison Data System (NPDS): 37th annual report. Clin. Toxicol. 2020;58(12):1360–1541. doi: 10.1080/15563650.2020.1834219. [DOI] [PubMed] [Google Scholar]
- 16.Lavanya J., Sivaranjani V., Arshiya B. A retrospective analysis of patterns, severity and clinical outcome of different poisoning cases in a tertiary care teaching hospital. IOSR J. Pharm. Biol. Sci. 2018;13(1):9–15. [Google Scholar]
- 17.Maheswari E., Abraham L., Chacko C.S., Saraswathy G.R., Ramesh A.C. Assessment of pattern, severity, and outcome of poisoning in the emergency care unit. J. Appl. Pharmaceut. Sci. 2016;6(12):178–183. [Google Scholar]
- 18.Jesslin J., Adepu R., Churi S. Assessment of prevalence and mortality incidences due to poisoning in a South Indian tertiary care teaching hospital. Indian J. Pharmaceut. Sci. 2010;72(5):587. doi: 10.4103/0250-474X.78525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cha E.S., Khang Y.-H., Lee W.J. Mortality from and incidence of pesticide poisoning in South Korea: findings from national death and health utilization data between 2006 and 2010. PLoS One. 2014;9(4) doi: 10.1371/journal.pone.0095299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karki N., Singh V., Verma V.K. Pattern, management, and outcome of poisoning in a tertiary care hospital. Journal of Lumbini Medical College. 2018;6(1):32–35. [Google Scholar]
- 21.Teklemariam E., Tesema S., Jemal A. Pattern of acute poisoning in Jimma University specialized hospital, south West Ethiopia. World Journal of Emergency Medicine. 2016;7(4):290. doi: 10.5847/wjem.j.1920-8642.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adinew G.M., Woredekal A.T., DeVos E.L., Birru E.M., Abdulwahib M.B. Poisoning cases and their management in emergency centers of government hospitals in northwest Ethiopia. African Journal of Emergency Medicine. 2017;7(2):74–78. doi: 10.1016/j.afjem.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shumet A., Shiferaw N., Mekonnen D., Asemahagn M.A. Trends and outcomes of acute poisoning in felege hiwot comprehensive specialized hospital medical intensive care units: retrospective study. Open Access Emerg. Med. 2022;14:649–656. doi: 10.2147/OAEM.S385420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehrpour O., Jafarzadeh M., Abdollahi M. A systematic review of aluminum phosphide poisoning. Arh. Hig. Rad. Toksikol. 2012;63(1):61–72. doi: 10.2478/10004-1254-63-2012-2182. [DOI] [PubMed] [Google Scholar]
- 25.Damte T. Trends in pesticide use by smallholder farmers on ‘Meher'Season field and horticultural crops in Ethiopia. Ethiopian Journal of Agricultural Sciences. 2022;32(2):133–156. [Google Scholar]
- 26.Negatu B., Kromhout H., Mekonnen Y., Vermeulen R. Use of chemical pesticides in Ethiopia: a cross-sectional comparative study on knowledge, attitude, and practice of farmers and farm workers in three farming systems. Ann. Occup. Hyg. 2016;60(5):551–566. doi: 10.1093/annhyg/mew004. [DOI] [PubMed] [Google Scholar]
- 27.Kumar M.R., Kumar G.V., Babu P.R., Kumar S.S., Subrahmanyam B., Veeraprasad M., Rammohan P., Srinivas M., Agrawal A. A retrospective analysis of acute organophosphorus poisoning cases admitted to the tertiary care teaching hospital in South India. Ann. Afr. Med. 2014;13(2):71–75. doi: 10.4103/1596-3519.129876. [DOI] [PubMed] [Google Scholar]
- 28.Kharat R.D., Kedare R.V. Analysis of pesticide poisoning cases in a tertiary care hospital, Mumbai. International Journal of Clinical and Biomedical Research. 2019:12–14. [Google Scholar]
- 29.Alzahrani S.H., Alqahtani A.H., Farahat F.M., Elnour M.A.G., Bashawri J. Drug poisoning and associated factors in Western Saudi Arabia: a five-year retrospective chart review (2011–2016) Pakistan J. Med. Sci. 2017;33(5):1188. doi: 10.12669/pjms.335.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molla Y.M., Belachew K.D., Ayehu G.W., Teshome A.A. Acute poisoning in children in Ethiopia: a cross-sectional study. Sci. Rep. 2022;12(1) doi: 10.1038/s41598-022-23193-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mengistie Y. 2022. Outcome and Associated Factors of Acute Adult Poisoning Among Patients Visiting Felege Hiwot Comprehensive Specialized Hospital, Northwest Ethiopia. [Google Scholar]
- 32.Dessie B.K., Sofia, Birhanu Tesfaye. 2021. Assessment of Outcome and Associated Factors of Adult Poisoning Cases at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia from January 1, 2015 to December 31, 2020. [Google Scholar]
- 33.Federal Ministry of Health Ethiopia . In: Guideline for Poison Information & Control Center, Ethiopia. EaC Care., editor. 2018. [Google Scholar]
- 34.Woyessa A.H., Dibaba B.Y., Hirko G.F., Palanichamy T. Spectrum, pattern, and clinical outcomes of adult emergency department admissions in selected hospitals of Western Ethiopia: a hospital-based prospective study. Emergency Medicine International. 2019;2019 doi: 10.1155/2019/8374017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 2021;88 doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 36.Peterson J., Welch V., Losos M., Tugwell P. vol. 2. Ottawa Hospital Research Institute; Ottawa: 2011. pp. 1–12. (The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses). 1. [Google Scholar]
- 37.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 38.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994:1088–1101. [PubMed] [Google Scholar]
- 41.Riley R., Higgins J., Deeks J. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. doi: 10.1136/bmj.d549. [DOI] [PubMed] [Google Scholar]
- 42.Higgins J.P., Thompson S.G., Spiegelhalter D.J. A re‐evaluation of random‐effects meta‐analysis. J. Roy. Stat. Soc. 2009;172(1):137–159. doi: 10.1111/j.1467-985X.2008.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Getnet H. 2022. Mortality and Associated Factors of Acute Poisoning in Adults at Felege Hiwot Comprehensive Specialized Hospital, Bahir Dar, Amhara Region, Northwest Ethiopia. [Google Scholar]
- 44.Melese E.A. 2018. Belete Assessment of Prevalence, Management, and Outcome of Acute Poisoning at St. Paul‘s Hospital Millennium Medical College and Addis Ababa Burn, Emergency and Trauma Hospital. [Google Scholar]
- 45.Adinew G. 2016. Pattern of Acute Poisoning in a Teaching Hospital, Northwest Ethiopia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bogale D.E., Ejigu B.D., Muche T.A. Clinical profile and treatment outcome of aluminum phosphide poisoning in Felege Hiwot Referral Hospital, Northwest Ethiopia: a retrospective study. Open Access Emerg. Med. 2021:239–248. doi: 10.2147/OAEM.S313181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Endayehu Y., Shenkutie E. Magnitude of acute poisoning and associated factors in Debretabor General Hospital, Ethiopia. J. Clin. Toxicol. 2019;9:1–4. [Google Scholar]
- 48.Desalew M., Aklilu A., Amanuel A., Addisu M., Ethiopia T. Pattern of acute adult poisoning at Tikur Anbessa specialized teaching hospital, a retrospective study, Ethiopia. Hum. Exp. Toxicol. 2011;30(7):523–527. doi: 10.1177/0960327110377520. [DOI] [PubMed] [Google Scholar]
- 49.Eyasu M., Dida T., Worku Y., Worku S., Shafie M. Acute poisonings during pregnancy and in other non‐pregnant women in emergency departments of four government hospitals, Addis Ababa, Ethiopia: 2010‐2015. Trop. Med. Int. Health. 2017;22(10):1350–1360. doi: 10.1111/tmi.12940. [DOI] [PubMed] [Google Scholar]
- 50.Chala T.S., Gebramariam H., Hussen M. 2015. Two-year Epidemiologic Pattern of Acute Pharmaceutical and Chemical Poisoning Cases Admitted to Adama Hospital Medical College, Adama, Ethiopia. [Google Scholar]
- 51.Ahmed M.B., Haile M., Tegene E. Prevalence and patterns of poisoning cases among patients presented to Jimma university specialized hospital: a five years retrospective data analysis. J. Clin. Toxicol. 2018;8:1–5. [Google Scholar]
- 52.Nigussie S., Demeke F., Getachew M., Amare F. vol. 10. A cross-sectional study. SAGE Open Medicine; 2022. (Treatment Outcome and Associated Factors Among Patients Admitted with Acute Poisoning in a Tertiary Hospital in Eastern Ethiopia). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Adinew G.M., Asrie A.B., Birru E.M. Pattern of acute organophosphorus poisoning at the university of gondar teaching hospital, northwest Ethiopia. BMC Res. Notes. 2017;10(1):1–6. doi: 10.1186/s13104-017-2464-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sulaj Z., Prifti E., Demiraj A., Strakosha A. Early clinical outcome of acute poisoning cases treated in the intensive care unit. Med. Arch. 2015;69(6):400. doi: 10.5455/medarh.2015.69.400-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Saoraya J., Inboriboon P.C. Acute poisoning surveillance in Thailand: the current state of affairs and a vision for the future. Int. Sch. Res. Notices. 2013;2013 [Google Scholar]
- 56.Alinejad S., Chahkandi T., Mehrpour O., Brent J., Riahi S.M. Epidemiology of pediatric acute poisoning in Iran: a systematic review and meta-analysis. Int. J. Pediatr. 2022;10(5):16082–16100. [Google Scholar]
- 57.Alzahrani S.H., Ibrahim N.K., Elnour M.A., Alqahtani A.H. Five-year epidemiological trends for chemical poisoning in Jeddah, Saudi Arabia. Ann. Saudi Med. 2017;37(4):282–289. doi: 10.5144/0256-4947.2017.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Anthony L., Kulkarni C. Patterns of poisoning and drug overdosage and their outcome among in-patients admitted to the emergency medicine department of a tertiary care hospital. Indian J. Crit. Care Med. 2012;16(3):130–135. doi: 10.4103/0972-5229.102070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen C.-K., Chan Y.-L., Su T.-H. Incidence of intoxication events and patient outcomes in Taiwan: a nationwide population-based observational study. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0244438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bagherian F., Kalani N., Rahmanian F., Abiri S., Hatami N., Foroughian M., Mehramiz N.J., Shahi B. Aluminum phosphide poisoning mortality rate in Iran; a systematic review and meta-analysis. Archives of Academic Emergency Medicine. 2021;9(1) doi: 10.22037/aaem.v9i1.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mew E.J., Padmanathan P., Konradsen F., Eddleston M., Chang S.-S., Phillips M.R., Gunnell D. The global burden of fatal self-poisoning with pesticides 2006-15: a systematic review. J. Affect. Disord. 2017;219:93–104. doi: 10.1016/j.jad.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 62.Alinejad S., Zamani N., Abdollahi M., Mehrpour O. A narrative review of acute adult poisoning in Iran. Iran. J. Med. Sci. 2017;42(4):327. [PMC free article] [PubMed] [Google Scholar]
- 63.Negatu B., Dugassa S., Mekonnen Y. Environmental and health risks of pesticide use in Ethiopia. Journal of Health Pollution. 2021;11(30) doi: 10.5696/2156-9614-11.30.210601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Alebachew F., Azage M., Kassie G.G., Chanie M. Pesticide use safety practices and associated factors among farmers in Fogera district wetland areas, south Gondar zone, Northwest Ethiopia. PLoS One. 2023;18(1) doi: 10.1371/journal.pone.0280185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shegaw T., Habtegiorgis D., Edmew T. Assessment on pesticide utilization and its effect on beekeeping in kafa and benchi-sheko zones, south-western region, Ethiopia. Cogent Food Agric. 2022;8(1) [Google Scholar]
- 66.Prashar A., Ramesh M. Assessment of pattern and outcomes of pesticide poisoning in a tertiary care hospital. Trop. Med. Int. Health. 2018;23(12):1401–1407. doi: 10.1111/tmi.13156. [DOI] [PubMed] [Google Scholar]
- 67.Sharma R., Rawat N., Panwar N. Mortality and morbidity associated with acute poisoning cases in north-east India: a retrospective study. J. Fam. Med. Prim. Care. 2019;8(6):2068. doi: 10.4103/jfmpc.jfmpc_237_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chatterjee S., Verma V.K., Hazra A., Pal J. An observational study on acute poisoning in a tertiary care hospital in West Bengal, India. Perspectives in Clinical Research. 2020;11(2):75. doi: 10.4103/picr.PICR_181_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Asari P.D., Shah S.M., Amin A.J., Patel N.D. Drug utilization study on acute poisoning cases treated at a tertiary care hospital in the western part of India. Asia Pacific Journal of Medical Toxicology. 2016;5(1) [Google Scholar]
- 70.Pagdhune A., Kunal K., Patel K.A., Patel A.B., Mishra S., Palkhade R., Muhamed J. Poisoning cases reported to the poison information center, Ahmedabad, India: a three-year observational study. Cent. Asian J. Global Health. 2020;9(1) doi: 10.5195/cajgh.2020.471. e471-e471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vadury S.C., Sarker H.N., Islam M.M.-U. Pattern of suicidal poisoning in a tertiary care hospital. Insight. 2019;2(2) 6-6. [Google Scholar]
- 72.Esayas Tadesse G., Mariam B.K.G. Global epidemiology of acute poisoning with an emphasis on Ethiopia: a systematic review. International Journal of Pharmaceutical Science & Scientific Research. 2016;2(4):161–171. [Google Scholar]
- 73.Chelkeba L., Mulatu A., Feyissa D., Bekele F., Tesfaye B.T. Patterns and epidemiology of acute poisoning in Ethiopia: a systematic review of observational studies. Arch. Publ. Health. 2018;76(1):34. doi: 10.1186/s13690-018-0275-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Eddleston M. Patterns and problems of deliberate self‐poisoning in the developing world. QJM. 2000;93(11):715–731. doi: 10.1093/qjmed/93.11.715. [DOI] [PubMed] [Google Scholar]
- 75.Moradi M., Ghaemi K., Mehrpour O. A hospital base epidemiology and pattern of acute adult poisoning across Iran: a systematic review. Electron. Physician. 2016;8(9):2860. doi: 10.19082/2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gupta P., Kumar A., Singh S.P., Prakash M., Gupta M., Kumar P. Pattern of cases of acute poisoning in a rural tertiary care center in Northern India. National Journal of Community Medicine. 2016;7(4):307–310. [Google Scholar]
- 77.Mittal C., Singh S., Kumar-M P., Varthya S.B. Toxicoepidemiology of poisoning exhibited in an Indian population from 2010 to 2020: a systematic review and meta-analysis. BMJ Open. 2021;11(5) doi: 10.1136/bmjopen-2020-045182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Albano G.D., Malta G., La Spina C., Rifiorito A., Provenzano V., Triolo V., Vaiano F., Bertol E., Zerbo S., Argo A. Toxicological findings of self-poisoning suicidal deaths: a systematic review by countries. Toxics. 2022;10(11):654. doi: 10.3390/toxics10110654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shakya R.P., Adhikary S., Bajracharya R. Pattern of acute poisoning attending a tertiary care hospital of western Nepal. Journal of Lumbini Medical College. 2016;4(2):90–93. [Google Scholar]
- 80.Z’gambo J., Siulapwa Y., Michelo C. Pattern of acute poisoning at two urban referral hospitals in Lusaka, Zambia. BMC Emerg. Med. 2016;16:1–8. doi: 10.1186/s12873-016-0068-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Prasadi G.A.M., Mohamed F., Senarathna L., Cairns R., Pushpakumara P.H.G.J., Dawson A.H. Paediatric poisoning in rural Sri Lanka: an epidemiological study. BMC Publ. Health. 2018;18(1):1349. doi: 10.1186/s12889-018-6259-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chandran J., Krishna B. Initial management of a poisoned patient. Indian J. Crit. Care Med.: peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2019;23(Suppl 4):S234. doi: 10.5005/jp-journals-10071-23307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Elgamel A., Ahmed N. Complications and management of hair dye poisoning in Khartoum. Sudan Medical Monitor. 2013;8(3):146. [Google Scholar]
- 84.Dayasiri M.B.K.C., Jayamanne S.F., Jayasinghe C.Y. Patterns and outcome of acute poisoning among children in rural Sri Lanka. BMC Pediatr. 2018;18(1):274. doi: 10.1186/s12887-018-1246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable or all data used in this study was presented in this document.