HIGHLIGHTS
-
•
Higher residential density was associated with lower 3-year BMI increase in girls.
-
•
Nearby fast food was associated with higher BMI increase for teen girls and younger boys.
-
•
Built environment has limited impact on BMI trajectory in children and adolescents.
-
•
Independent effects are small but may accumulate over the life course.
Keywords: Built environment, obesity, child, adolescent, geographic information systems, natural experiment
Abstract
Introduction
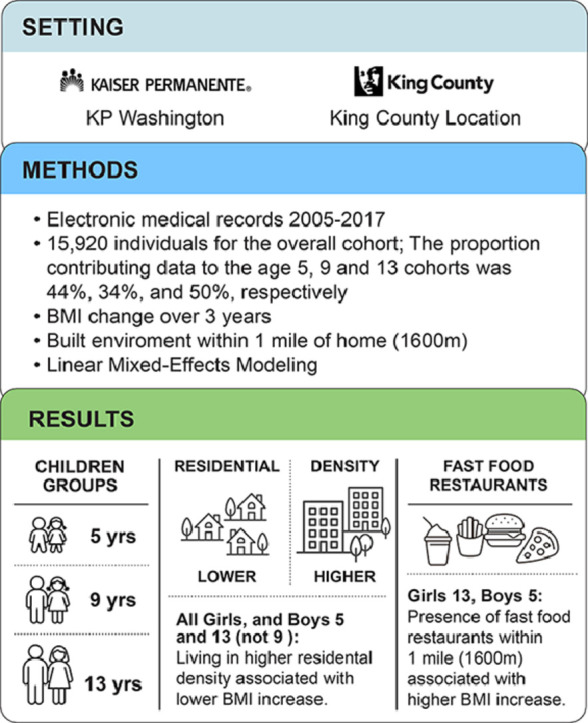
This study investigates the associations between built environment features and 3-year BMI trajectories in children and adolescents.
Methods
This retrospective cohort study utilized electronic health records of individuals aged 5–18 years living in King County, Washington, from 2005 to 2017. Built environment features such as residential density; counts of supermarkets, fast-food restaurants, and parks; and park area were measured using SmartMaps at 1,600-meter buffers. Linear mixed-effects models performed in 2022 tested whether built environment variables at baseline were associated with BMI change within age cohorts (5, 9, and 13 years), adjusting for sex, age, race/ethnicity, Medicaid, BMI, and residential property values (SES measure).
Results
At 3-year follow-up, higher residential density was associated with lower BMI increase for girls across all age cohorts and for boys in age cohorts of 5 and 13 years but not for the age cohort of 9 years. Presence of fast food was associated with higher BMI increase for boys in the age cohort of 5 years and for girls in the age cohort of 9 years. There were no significant associations between BMI change and counts of parks, and park area was only significantly associated with BMI change among boys in the age cohort of 5 years.
Conclusions
Higher residential density was associated with lower BMI increase in children and adolescents. The effect was small but may accumulate over the life course. Built environment factors have limited independent impact on 3-year BMI trajectories in children and adolescents.
Graphical abstract
INTRODUCTION
Elevated BMI is associated with health risks for children and adolescents globally. In the U.S., age-specific BMI and obesity prevalence in individuals aged <18 years has increased over several decades.1 Built environment (BE) features have been proposed as drivers of weight gain and obesity risk in children and adolescents—and have been considered as intervention targets. Cross-sectional studies have found associations between lower BMI or obesity prevalence and a range of BE characteristics; negative associations between residential density2,3 and obesity have consistently been identified, whereas evidence is mixed regarding availability of healthy foods—supermarkets, fast-food4—and recreational facilities.3,5
Longitudinal studies have found modest associations between residential density6,7 and lower child and adolescent BMI; findings have been inconsistent for food environment8 and null for count of parks.9 Methodologic challenges such as the diversity of methods used to characterize individual BE exposures,10 variable spatial approaches, and lack of large longitudinal pediatric datasets may have led to mixed findings and limited the extent to which these studies can inform policy.
Moving to Health11 (M2H) is a 12-year retrospective cohort formed by linking Kaiser Permanente Washington (KPW) electronic health records (EHRs) with geographic administrative data. Analyses of adults in M2H found that residential density was strongly associated with body weight and obesity prevalence at baseline but had relatively small associations with weight gain over time. Associations between BE and changes in BMI earlier in life could potentially contribute to cross-sectional associations among adults. This study sought to determine whether BE features at baseline were associated with BMI trajectories of children and adolescents at 1, 2, and 3 years of follow-up, adjusting for individual-level demographics and residential property values. BE features of interest, including physical aspects such as residential density (as a proxy for walkability), proximity to supermarkets, fast food, and parks, were examined using a single analytic approach, allowing comparison of their respective associations with BMI trajectory.
METHODS
Study Population
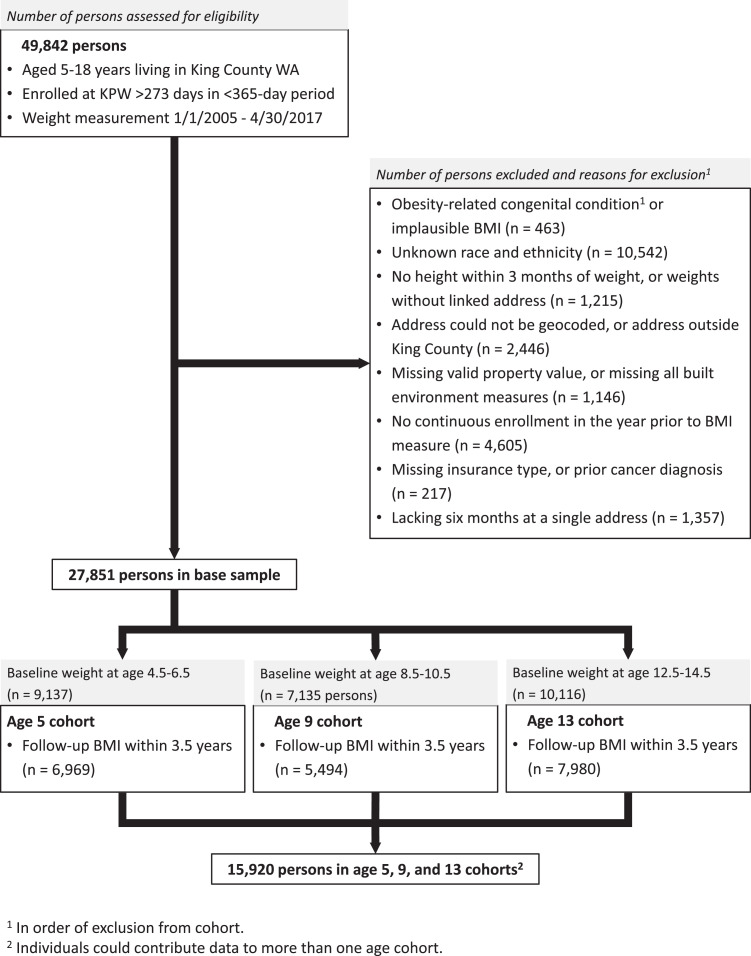
The authors identified children and adolescents aged 5–18 years living in King County (KC), Washington, who had ≥273 days of continuous enrollment at KPW and at least 1 weight measurement between January 1, 2005 and April 30, 2017, parallel to the development of the M2H adult cohort11 (Figure 1). BMI was computed using weight and height (within ≤3 months of the weight) measures. The authors excluded individuals with the following conditions strongly related to BMI: pro-opiomelanocortin processing disorders, Asperger's syndrome, Albright hereditary osteodystrophy, Down syndrome, Prader–Willi syndrome, Bardet–Biedl syndrome, and Alström syndrome. They limited the cohort to children with known sex (female, male) and race and ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, non-Hispanic Native Hawai'ian/Pacific Islander, non-Hispanic American Indian/Alaskan Native, other) and to those living at a geocodable home address within KC with a valid parcel-level residential property value (≥$10,000) for ≥182 days, nonmissing insurance status, and no history of cancer or bariatric surgery at baseline. The authors use boy and girl to refer to EHR-defined sex. The ability to account for more diverse sex, race, and ethnic identities was limited by data available in the EHR. The authors excluded observations when patients were pregnant or within 3 months after delivery as well as biologically implausible values of weight, height, or BMI for age and sex (i.e., observations with extreme modified z-scores relative to 2000 Centers for Disease Control and Prevention growth charts).12
Figure 1.
CONSORT diagram and creation of age cohorts.
KPW, Kaiser Permanente Washington; WA, Washington.
The authors used change in BMI as the outcome for longitudinal analyses (instead of BMI z-scores or percentiles) because it better reflects within-child growth and changes in adiposity,13, 14, 15 especially for children and adolescents with very high BMI.16,17 Because interpretation of change in BMI differs depending on age (and the authors hypothesized that effects could be different in these different cohorts), they authors created 3 age-specific cohorts, starting at ages 5, 9, and 13 years (Figure 1). For each age cohort, they identified patients with an eligible BMI during a 2-year period around the age defining the beginning of the cohort (4.5–6.5 years, 8.5–10.5 years, and 12.5–14.5 years). Patients’ baseline BMI was defined as the eligible BMI closest to age (5, 9, 13) years and 0 days. Patients could be in multiple cohorts. After baseline, patients contributed follow-up BMIs to a given age-specific cohort for up to 3.5 years. Individuals without any follow-up BMIs were excluded. Patients were censored if they moved residence, had a bariatric surgery or cancer, disenrolled from KPW or had a gap in residential address history (≥13 months), or were at the end of the study period.
Measures
Home addresses were geocoded to determine each person's baseline BE exposures18 (details in Appendix A, available online). All BE exposure variables—selected because they are closely related to energy balance related behaviors—were captured within 1,600-meter Euclidean buffers of the home address (representing a 20-minute walking distance or a short drive). Residential density, a walkability proxy associated with obesity prevalence,19, 20, 21, 22, 23, 24, 25 was computed as units per hectare (from KC tax assessor) and, given its highly skewed distribution, were categorized into tertiles. The authors also dichotomized residential density at 18 units per hectare, the density considered necessary for efficient provision of public transit.22,26,27 They created variables indicating proximity to supermarkets and fast-food restaurants (defined as establishments where one pays before eating) and neighborhood parks (measured using the count of unique parks and total park area with slope below 5%, the maximum running slope in accessible routes by 2010 Americans with Disabilities Act standards,28 categorized in tertiles). Property values from KC assessor's tax parcel data were used as a measure of SES (on the basis of known correlation between KC residential property values and income)29, 30, 31 and categorized into calendar year–specific tertiles because children entered the cohort at different times.
Statistical Analysis
Within age-specific cohorts, the authors calculated median BMI and IQR, proportion of children and adolescents by BMI percentile categories, and percentage with BMI ≥95th percentile for age and sex overall and by BE levels at 1, 2, and 3 years after baseline. Statistical modeling followed an analogous framework as developed for the authors's prior analyses among the adult cohort.11,18 The authors fit separate linear mixed-effects models of the change in BMI over time for each age-specific cohort and each BE variable. Models included a person-specific random intercept to account for correlation of repeated measures within children, modeled using an exponential correlation structure to account for irregularly spaced follow-up (in prior modeling work, this correlation structure achieved the best fit to the longitudinal data—compared with the conditional autoregressive structure—and was therefore selected for the current analysis). Interaction terms between sex, the categorical BE exposure variable, and time since baseline were included to allow the association between BE and BMI change to vary smoothly by sex over time; time was flexibly modeled using natural cubic splines with 5 degrees of freedom and knots at quantiles. This functional form was found to adequately allow for nonlinear temporal trends. The authors estimated the (adjusted) mean change in BMI from baseline to 1, 2, and 3 years at each BE level separately for boys and girls and conducted Wald tests of the difference in mean BMI change comparing the highest with the lowest BE level (e.g., third versus first tertile or any versus none for dichotomous variables). Conditional on correct specification of the model, use of mixed models ensures that estimates are unbiased if data are missing at random.
Models adjusted for race and ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, non-Hispanic Native Hawai'ian/Pacific Islander, non-Hispanic American Indian/Alaskan Native, and other), Medicaid insured (binary), property value deciles, and baseline BMI (allowing the association to differ by sex) and adjusted for the difference between baseline age and the start of the age cohort (through spline terms with 3 degrees of freedom). Because residential density could plausibly influence both change in BMI and presence of fast-food restaurants, supermarkets, and parks, the authors adjusted for residential density in models where food environment and neighborhood parks were the main exposure and did not adjust for food environment and parks in models where residential density was the main exposure. Mixed models were fit using the nlme R package with R, version 4.0.232,33 (Vienna, Austria). Analyses were conducted in 2022.
Human Subjects
The KPW IRB approved this study.
RESULTS
This study identified 15,920 individuals for the overall sample (Table 1). The proportion contributing data to the age cohorts of 5, 9, and 13 years was 44%, 34%, and 50%, respectively (Figure 1). Demographics are shown in Table 1 and Appendix B (available online). Twelve percent of individuals had a BMI at or above the 95th percentile. All age-specific cohorts had a median of 4 observations per individual. Median follow-up time was 2.0, 2.3, and 2.3 years for age cohorts of 5, 9, and 13 years, respectively. Patients insured by Medicaid had fewer BMI measurements, as did those reporting either non-Hispanic Black or non-Hispanic Hawai'ian/Pacific Islander race and ethnicities and participants residing in homes in the lowest property value tertile. Patients with asthma had slightly more BMI measures.
Table 1.
Baseline Characteristics, Number of BMI Measurements and Years Between Measurements (All Age Cohorts, Combined)
| Number of BMI measures |
Years between BMI measures |
|||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic1 | n | % | Median | 25% | 75% | Median | 25% | 75% |
| Total | 15,920 | 100 | 6.0 | 3.0 | 10.0 | 3.9 | 1.8 | 6.2 |
| Sex | ||||||||
| Female | 7,756 | 48.7 | 6.0 | 4.0 | 10.0 | 4.0 | 1.8 | 6.3 |
| Male | 8,164 | 51.3 | 6.0 | 3.0 | 10.0 | 3.9 | 1.8 | 6.2 |
| Race and ethnicity | ||||||||
| Non-Hispanic White | 8,544 | 53.7 | 6.0 | 4.0 | 10.0 | 4.0 | 1.9 | 6.3 |
| Non-Hispanic Black | 1,679 | 10.5 | 5.0 | 3.0 | 9.0 | 3.8 | 1.7 | 6.1 |
| Hispanic | 1,232 | 7.7 | 6.0 | 3.0 | 9.0 | 3.4 | 1.2 | 5.9 |
| Non-Hispanic Asian | 3,629 | 22.8 | 6.0 | 3.0 | 9.0 | 4.0 | 1.9 | 6.4 |
| Non-Hispanic Native Hawai'ian/Pacific Islander | 307 | 1.9 | 5.0 | 3.0 | 9.0 | 3.6 | 1.7 | 5.8 |
| Non-Hispanic American Indian/Alaskan Native | 215 | 1.4 | 6.0 | 3.0 | 11.0 | 3.5 | 1.3 | 6.0 |
| Other | 314 | 2.0 | 6.0 | 3.0 | 10.0 | 3.9 | 1.8 | 6.4 |
| Insurance | ||||||||
| Commercial | 14,749 | 92.6 | 6.0 | 4.0 | 10.0 | 4.0 | 2.0 | 6.4 |
| Medicaid | 1,048 | 6.6 | 4.0 | 2.0 | 7.0 | 2.4 | 0.7 | 4.9 |
| Other | 123 | 0.8 | 3.0 | 2.0 | 4.5 | 1.1 | 0.3 | 2.3 |
| CDC BMI percentile, category | ||||||||
| (0, 25) | 2,485 | 15.6 | 6.0 | 4.0 | 9.0 | 3.8 | 1.5 | 6.1 |
| (25, 50) | 3,161 | 19.9 | 6.0 | 3.0 | 10.0 | 4.0 | 1.9 | 6.3 |
| (50, 75) | 3,988 | 25.1 | 6.0 | 3.0 | 10.0 | 3.9 | 1.8 | 6.3 |
| (75, 95) | 4,365 | 27.4 | 6.0 | 3.0 | 10.0 | 3.9 | 1.8 | 6.3 |
| (95, 99) | 1,468 | 9.2 | 6.0 | 4.0 | 10.0 | 4.0 | 1.9 | 6.2 |
| (99, 100) | 453 | 2.8 | 7.0 | 3.0 | 11.0 | 4.0 | 1.7 | 6.3 |
| Property value, tertile2 | ||||||||
| 1 | 5,586 | 35.1 | 6.0 | 3.0 | 9.0 | 3.4 | 1.3 | 5.9 |
| 2 | 5,350 | 33.6 | 6.0 | 4.0 | 10.0 | 4.0 | 2.0 | 6.3 |
| 3 | 4,984 | 31.3 | 6.0 | 4.0 | 10.0 | 4.2 | 2.1 | 6.5 |
| Comorbidities3 | ||||||||
| Asthma | 1,178 | 7.4 | 7.0 | 4.0 | 12.0 | 3.5 | 1.5 | 6.0 |
| Anxiety | 316 | 2.0 | 6.0 | 3.0 | 11.0 | 3.3 | 1.6 | 4.9 |
| Depression | 118 | 0.7 | 6.0 | 3.0 | 10.0 | 2.7 | 1.0 | 4.4 |
Smoking self-report is not shown is the table owing to high proportion of missing data in electronic health record (43.6%). Of the analytic sample, 0.1% reported smoking currently, 0.2% reported smoking in the past, and 56% reported never smoking.
Property value tertiles varied from year to year. For 2017, the tertiles were ≤$337,405; $337,406–$530,965; and ≥$530,966.
Other comorbidities that occurred in 0.3% or fewer patients were psychoses, sleep apnea, eating disorders, diabetes, and kidney disease.
Appendix B (available online) shows the above data, by age cohort.
CDC, Center for Disease Control and Prevention
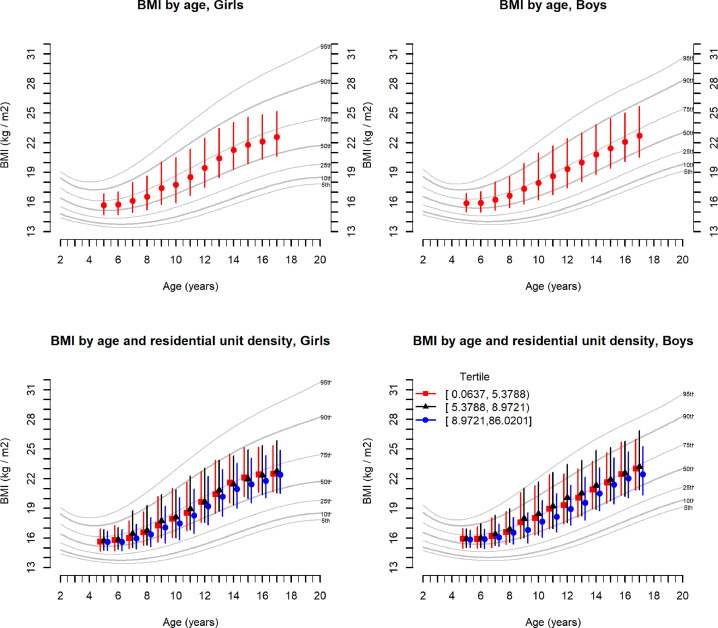
Table 2 describes the cross-sectional relationships between baseline BE characteristics and baseline BMI, BMI percentile, and obesity prevalence for each age cohort. Median BMI was 15.8, 17.3, and 20.1 for the age cohorts of 5, 9, and 13 years, respectively. Median BMI percentile was 63.3, 65.1, and 66.6 for the 3 cohorts, respectively. Baseline obesity prevalence was slightly lower in children and adolescents living in denser neighborhoods (all age cohorts) when residential density was dichotomized at the transit threshold, but the relationship appeared inverse U-shaped when residential density was categorized in tertiles. Figure 2 shows baseline BMI by age and residential density. Children and adolescents living within 1,600 meters of a fast-food restaurant had slightly higher median BMI percentile and greater obesity prevalence (all ages). Those living near more parks had lower obesity prevalence at baseline (all ages). However, overall, the relationship between parks and obesity prevalence was inverse U-shaped, with middle tertile having the highest obesity prevalence. Property value had the strongest cross-sectional association with BMI, BMI percentile, and obesity prevalence than any of the BE variables examined. Children in the age cohort of 5 years living in homes in the lowest residential property value tertile had 2.6 times the obesity prevalence of those in the highest property value tertile (14.4% vs 5.5%). This obesity prevalence difference was 2.7-fold and 3.2-fold for age cohorts of 9 and 13 years, respectively.
Table 2.
BE Characteristics in Relation to Baseline BMI, BMI Percentile, and Obesity Prevalence, by Age Cohort
| BMI |
BMI percentile1 |
Obesity prevalence1 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | n | % | Median | 25% | 75% | Median | 25% | 75% | n | % |
| Age cohort of 5 years, total | 6,969 | 100 | 15.8 | 14.9 | 16.8 | 63.3 | 36.2 | 84.3 | 691 | 9.9 |
| BE2 | ||||||||||
| Residential density (tertiles) | ||||||||||
| (0.0637, 5.3788) | 1,971 | 28.3 | 15.8 | 14.8 | 16.9 | 63 | 34.5 | 85.1 | 211 | 10.7 |
| (5.3788, 8.9721) | 2,181 | 31.3 | 15.8 | 14.9 | 16.9 | 64.9 | 37 | 85.2 | 254 | 11.6 |
| (8.9721, 86.0201) | 2,817 | 40.4 | 15.7 | 14.9 | 16.7 | 62.6 | 36.7 | 83.1 | 226 | 8.0 |
| Residential density (dichotomized at transit threshold) | ||||||||||
| (0.0637, 18.0000) | 6,315 | 90.6 | 15.8 | 14.9 | 16.8 | 63.3 | 36.1 | 84.4 | 635 | 10.1 |
| (18.0000, 86.0201) | 654 | 9.4 | 15.8 | 15.0 | 16.6 | 64.8 | 38.9 | 82.0 | 56 | 8.6 |
| Supermarket (binary) | ||||||||||
| None | 3,255 | 46.7 | 15.7 | 14.8 | 16.7 | 62.7 | 34.7 | 83.8 | 320 | 9.8 |
| Any | 3,714 | 53.3 | 15.8 | 14.9 | 16.8 | 64.3 | 37.4 | 84.6 | 371 | 10.0 |
| Fast food (binary) | ||||||||||
| None | 2,773 | 39.8 | 15.7 | 14.9 | 16.7 | 62.7 | 35.9 | 83.4 | 260 | 9.4 |
| Any | 4,196 | 60.2 | 15.8 | 14.9 | 16.9 | 63.9 | 36.3 | 84.8 | 431 | 10.3 |
| Park count (tertiles) | ||||||||||
| (0, 7) | 1,852 | 26.6 | 15.8 | 14.9 | 16.8 | 63.3 | 35.5 | 84.5 | 199 | 10.7 |
| (7, 11) | 2,192 | 31.5 | 15.8 | 14.9 | 16.9 | 64.3 | 37.1 | 86.0 | 254 | 11.6 |
| (11, 45) | 2,925 | 42.0 | 15.8 | 14.9 | 16.7 | 62.7 | 36.0 | 82.7 | 238 | 8.1 |
| Park area (hectares) with <5% slope (tertiles) | ||||||||||
| (0.0, 10.5) | 2,355 | 33.8 | 15.8 | 14.9 | 16.8 | 63.6 | 36.7 | 84.5 | 232 | 9.9 |
| (10.5, 23.1) | 2,386 | 34.2 | 15.8 | 14.9 | 16.8 | 63.8 | 36.7 | 84.4 | 238 | 10.0 |
| (23.1, 342.0) | 2,228 | 32.0 | 15.7 | 14.8 | 16.7 | 62.5 | 35.6 | 83.5 | 221 | 9.9 |
| SES | ||||||||||
| Property value (tertiles3) | ||||||||||
| 1 | 2,474 | 35.5 | 15.9 | 14.9 | 17.1 | 66.7 | 38.6 | 88.1 | 357 | 14.4 |
| 2 | 2,452 | 35.2 | 15.7 | 14.8 | 16.7 | 62.2 | 33.9 | 83.3 | 221 | 9.0 |
| 3 | 2,043 | 29.3 | 15.7 | 14.9 | 16.5 | 62.1 | 36.3 | 80.1 | 113 | 5.5 |
| Age cohort of 9 year, total | 5,494 | 100 | 17.3 | 15.8 | 19.8 | 65.1 | 35.7 | 88.1 | 779 | 14.2 |
| BE | ||||||||||
| Residential density (tertiles) | ||||||||||
| (0.0637, 5.3788) | 1,788 | 32.5 | 17.4 | 15.8 | 20 | 67.1 | 36.4 | 89.6 | 283 | 15.8 |
| (5.3788, 8.9721) | 1,765 | 32.1 | 17.7 | 15.9 | 20.4 | 69.5 | 39.3 | 91.0 | 297 | 16.8 |
| (8.9721, 86.0201) | 1,941 | 35.3 | 17.0 | 15.6 | 18.9 | 60.5 | 32.4 | 83.0 | 199 | 10.3 |
| Residential density (dichotomized at transit threshold) | ||||||||||
| (0.0637, 18.0000) | 5,047 | 91.9 | 17.4 | 15.8 | 19.9 | 66.0 | 36.5 | 88.7 | 743 | 14.7 |
| (18.0000, 86.0201) | 447 | 8.1 | 16.7 | 15.4 | 18.7 | 54.9 | 26.5 | 81.5 | 36 | 8.1 |
| Supermarket (binary) | ||||||||||
| None | 2,796 | 50.9 | 17.4 | 15.8 | 20 | 66.7 | 36.0 | 89.2 | 422 | 15.1 |
| Any | 2,698 | 49.1 | 17.2 | 15.7 | 19.6 | 63.6 | 35.3 | 87.0 | 357 | 13.2 |
| Fast-food (binary) | ||||||||||
| None | 2,421 | 44.1 | 17.3 | 15.7 | 19.7 | 64.9 | 35.4 | 87.8 | 342 | 14.1 |
| Any | 3,073 | 55.9 | 17.3 | 15.8 | 19.9 | 65.4 | 36.1 | 88.3 | 437 | 14.2 |
| Park count (tertiles) | ||||||||||
| (0, 7) | 1,616 | 29.4 | 17.4 | 15.8 | 19.9 | 66.4 | 36.0 | 88.5 | 244 | 15.1 |
| (7, 11) | 1,701 | 31.0 | 17.5 | 15.8 | 20.4 | 67.1 | 37.0 | 90.3 | 277 | 16.3 |
| (11, 45) | 2,177 | 39.6 | 17.1 | 15.7 | 19.3 | 63.1 | 34.4 | 85.6 | 258 | 11.9 |
| Park area (hectares) with <5% slope (tertiles) | ||||||||||
| (0.0, 10.5) | 1,804 | 32.8 | 17.3 | 15.7 | 19.8 | 65.5 | 35.0 | 88.0 | 241 | 13.4 |
| (10.5, 23.1) | 1,842 | 33.5 | 17.3 | 15.8 | 19.6 | 64.7 | 36.3 | 87.8 | 256 | 13.9 |
| (23.1, 342.0) | 1,848 | 33.6 | 17.3 | 15.8 | 19.9 | 65.2 | 35.5 | 88.5 | 282 | 15.3 |
| SES | ||||||||||
| Property value (tertiles) | ||||||||||
| 1 | 1,873 | 34.1 | 17.9 | 16.0 | 21.0 | 72.9 | 42.0 | 93.2 | 390 | 20.8 |
| 2 | 1,859 | 33.8 | 17.2 | 15.7 | 19.6 | 63.1 | 35.0 | 87.5 | 253 | 13.6 |
| 3 | 1,762 | 32.1 | 16.9 | 15.5 | 18.8 | 59.3 | 30.9 | 82.2 | 136 | 7.7 |
| Age cohort of 13 years, total | 7,980 | 100 | 20.1 | 18.1 | 23.1 | 66.6 | 40.3 | 87.8 | 1,065 | 13.3 |
| BE | ||||||||||
| Residential density (tertiles) | ||||||||||
| (0.0637, 5.3788) | 2,667 | 33.4 | 20.2 | 18.2 | 23.3 | 67.0 | 41.0 | 88.3 | 389 | 14.6 |
| (5.3788, 8.9721) | 2,752 | 34.5 | 20.5 | 18.4 | 23.7 | 70.5 | 43.6 | 90.3 | 425 | 15.4 |
| (8.9721, 86.0201) | 2,561 | 32.1 | 19.7 | 17.8 | 22.4 | 62.4 | 35.4 | 84.8 | 251 | 9.8 |
| Residential density (dichotomized at transit threshold) | ||||||||||
| (0.0637, 18.0000) | 7,442 | 93.3 | 20.2 | 18.2 | 23.2 | 67.4 | 40.8 | 88.2 | 1,022 | 13.7 |
| (18.0000, 86.0201) | 538 | 6.7 | 19.3 | 17.6 | 21.6 | 58.2 | 32.2 | 80.3 | 43 | 8.0 |
| Supermarket (binary) | ||||||||||
| None | 4,196 | 52.6 | 20.1 | 18.2 | 23.2 | 66.7 | 40.6 | 88.2 | 578 | 13.8 |
| Any | 3,784 | 47.4 | 20.1 | 18.1 | 23.0 | 66.2 | 39.7 | 87.4 | 487 | 12.9 |
| Fast-food (binary) | ||||||||||
| None | 3,709 | 46.5 | 20.0 | 18.1 | 22.9 | 65.4 | 39.7 | 86.9 | 453 | 12.2 |
| Any | 4,271 | 53.5 | 20.2 | 18.2 | 23.2 | 67.7 | 40.9 | 88.7 | 612 | 14.3 |
| Park count (tertiles) | ||||||||||
| (0, 7) | 2,416 | 30.3 | 20.2 | 18.1 | 23.4 | 68.2 | 40.3 | 88.8 | 336 | 13.9 |
| (7, 11) | 2,487 | 31.2 | 20.3 | 18.3 | 23.5 | 68.5 | 42.7 | 89.2 | 371 | 14.9 |
| (11, 45) | 3,077 | 38.6 | 19.8 | 18.0 | 22.6 | 64.1 | 38.4 | 85.9 | 358 | 11.6 |
| Park area with <5% slope (tertiles) | ||||||||||
| (0.0, 10.5) | 2,676 | 33.5 | 20.0 | 18.1 | 22.8 | 65.4 | 39.5 | 86.8 | 336 | 12.6 |
| (10.5, 23.1) | 2,700 | 33.8 | 20.1 | 18.2 | 23.2 | 66.7 | 41.1 | 88.3 | 379 | 14.0 |
| (23.1, 342.0) | 2,604 | 32.6 | 20.2 | 18.1 | 23.3 | 67.6 | 40.1 | 88.5 | 350 | 13.4 |
| SES | ||||||||||
| Property value (tertiles) | ||||||||||
| 1 | 2,537 | 31.8 | 21.3 | 18.8 | 25.2 | 77.7 | 49.7 | 93.6 | 539 | 21.2 |
| 2 | 2,591 | 32.5 | 20.0 | 18.2 | 22.9 | 65.9 | 41.5 | 87.2 | 339 | 13.1 |
| 3 | 2,852 | 35.7 | 19.4 | 17.6 | 21.8 | 57.6 | 32.2 | 80.9 | 187 | 6.6 |
Note: Three quarters (75.5%) of 15,920 children in the overall sample contributed data to only 1 age cohort, 20.5% contributed to 2, and 3.9% contributed to all 3 cohorts.
CDC BMI charts can be found at https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm#values.
All BE characteristics are measured at a 1,600-meter buffer.
Property value tertiles varied from year to year. For 2017, the tertiles were ≤$337,405; $337,406–$530,965; and ≥$530,966.
BE, built environment; CDC, Center for Disease Control and Prevention.
Figure 2.
Baseline BMI overlaid on CDC BMI percentiles, for boys and girls, by age and age and residential density. (A) By age. (B) By age and residential density.
CDC, Center for Disease Control and Prevention
Table 3 shows the adjusted point estimates and 95% CIs for BMI change associated with BE exposures for each age cohort, at years 2 and 3. Overall, girls’ mean BMI at 3 years increased from baseline by 1.0 unit in the age cohort of 5 years (95% CI=1.0, 1.1), 2.5 units in the age cohort of 9 years (95% CI=2.4, 2.6), and 2.0 units in the age cohort of 13 years (95% CI=1.9, 2.0). Overall, boys’ mean BMI at 3 years increased by 1.0 unit in the age cohort of 5 years (95% CI=0.9, 1.1), 2.1 units in the age cohort of 9 years (95% CI=2.0, 2.1), and 2.2 units in the age cohort of 13 years (95% CI=2.1, 2.3). No statistically significant associations between BMI change and BE were seen at Year 1 (data not shown). Across all BE variables, somewhat larger associations were seen at Year 3 than at Year 2.
Table 3.
BE Characteristics and Their Relationship With Change in BMI at 2 and 3 Years From Baseline (Mean Difference) in the 3 Age Cohorts, After Adjusting for Baseline Demographics, BMI, and Year-Specific Residential Property Values
| Female |
Male |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Year 2 |
Year 3 |
Year 2 |
Year 3 |
||||||
| BE characteristic1 | Level | Estimate | p-value2 | Estimate | p-value | Estimate | p-value | Estimate | p-value |
| Age cohort of 5 years, overall | 0.5 (0.5, 0.6) | 1.0 (1.0, 1.1) | 0.5 (0.4, 0.5) | 1.0 (0.9, 1.1) | |||||
| Residential density (tertiles) | |||||||||
| 1 | (0.0637, 5.3788) | 0.6 (0.5, 0.7) | 1.1 (1.0, 1.2) | 0.6 (0.5, 0.7) | 1.2 (1.1, 1.3) | ||||
| 2 | (5.3788, 8.9721) | 0.6 (0.5, 0.7) | 1.1 (1.0, 1.2) | 0.5 (0.4, 0.6) | 1.1 (0.9, 1.2) | ||||
| 3 | (8.9721, 86.0201) | 0.5 (0.4, 0.6) | 0.074 | 0.9 (0.8, 1.0) | 0.004 | 0.3 (0.2, 0.4) | <0.0001 | 0.8 (0.7, 0.9) | <0.0001 |
| Residential density (dichotomized at transit threshold) | |||||||||
| 1 | (0.0637, 18.0000) | 0.6 (0.5, 0.6) | 1.1 (1.0, 1.1) | 0.5 (0.4, 0.6) | 1.0 (1.0, 1.1) | ||||
| 2 | (18.0000, 86.0201) | 0.4 (0.2, 0.6) | 0.21 | 0.9 (0.7, 1.1) | 0.078 | 0.3 (0.1, 0.5) | 0.063 | 0.7 (0.5, 0.9) | 0.0003 |
| Supermarket (binary) | |||||||||
| 0 | None | 0.6 (0.5, 0.7) | 1.1 (1.0, 1.2) | 0.4 (0.3, 0.5) | 1.0 (0.9, 1.1) | ||||
| 1 | Any | 0.5 (0.4, 0.5) | 0.009 | 1.0 (0.9, 1.1) | 0.12 | 0.5 (0.4, 0.6) | 0.11 | 1.0 (1.0, 1.1) | 0.2 |
| Fast food (binary) | |||||||||
| 0 | None | 0.6 (0.5, 0.7) | 1.1 (1.0, 1.2) | 0.4 (0.3, 0.5) | 0.9 (0.8, 1.0) | ||||
| 1 | Any | 0.5 (0.5, 0.6) | 0.62 | 1.0 (0.9, 1.1) | 0.49 | 0.6 (0.5, 0.6) | 0.005 | 1.1 (1.0, 1.2) | 0.0003 |
| Park count (tertiles) | |||||||||
| 1 | (0, 7) | 0.6 (0.4, 0.7) | 1.0 (0.9, 1.1) | 0.4 (0.3, 0.6) | 0.9 (0.8, 1.1) | ||||
| 2 | (7, 11) | 0.5 (0.4, 0.6) | 1.0 (0.9, 1.1) | 0.5 (0.4, 0.6) | 1.1 (1.0, 1.2) | ||||
| 3 | (11, 45) | 0.6 (0.5, 0.7) | 0.88 | 1.1 (1.0, 1.2) | 0.55 | 0.5 (0.4, 0.6) | 0.91 | 1.0 (0.9, 1.1) | 0.35 |
| Park area (hectares) with <5% slope (tertiles) | |||||||||
| 1 | (0.0, 10.5) | 0.5 (0.4, 0.6) | 1.0 (0.9, 1.1) | 0.5 (0.4, 0.6) | 0.9 (0.8, 1.0) | ||||
| 2 | (10.5, 23.1) | 0.6 (0.5, 0.7) | 1.1 (1.0, 1.2) | 0.4 (0.3, 0.5) | 1.1 (1.0, 1.1) | ||||
| 3 | (23.1, 342.0) | 0.6 (0.5, 0.7) | 0.37 | 1.1 (1.0, 1.2) | 0.34 | 0.5 (0.4, 0.6) | 0.24 | 1.1 (1.0, 1.2) | 0.045 |
| Age cohort of 9 years, overall | 1.6 (1.5, 1.7) | 2.5 (2.4, 2.6) | 1.4 (1.3, 1.5) | 2.1 (2.0, 2.1) | |||||
| Residential density (tertiles) | |||||||||
| 1 | (0.0637, 5.3788) | 1.6 (1.5, 1.8) | 2.7 (2.5, 2.8) | 1.4 (1.3, 1.6) | 2.1 (2.0, 2.2) | ||||
| 2 | (5.3788, 8.9721) | 1.7 (1.5, 1.8) | 2.6 (2.4, 2.7) | 1.4 (1.3, 1.5) | 2.1 (2.0, 2.3) | ||||
| 3 | (8.9721, 86.0201) | 1.5 (1.4, 1.6) | 0.16 | 2.4 (2.2, 2.5) | 0.002 | 1.4 (1.2, 1.5) | 0.34 | 2.0 (1.8, 2.1) | 0.16 |
| Residential density (dichotomized at transit threshold) | |||||||||
| 1 | (0.0637, 18.0000) | 1.6 (1.5, 1.7) | 2.5 (2.5, 2.6) | 1.4 (1.3, 1.5) | 2.1 (2.0, 2.1) | ||||
| 2 | (18.0000, 86.0201) | 1.6 (1.3, 1.8) | 0.7 | 2.3 (2.1, 2.6) | 0.2 | 1.2 (1.0, 1.5) | 0.12 | 2.0 (1.7, 2.2) | 0.4 |
| Supermarket (binary) | |||||||||
| 0 | None | 1.5 (1.4, 1.6) | 2.5 (2.4, 2.6) | 1.4 (1.3, 1.5) | 2.1 (2.0, 2.2) | ||||
| 1 | Any | 1.7 (1.6, 1.8) | 0.052 | 2.6 (2.4, 2.7) | 0.48 | 1.4 (1.3, 1.5) | 0.58 | 2.0 (1.9, 2.2) | 0.56 |
| Fast food (binary) | |||||||||
| 1 | None | 1.5 (1.4, 1.6) | 2.4 (2.3, 2.5) | 1.4 (1.3, 1.5) | 2.0 (1.9, 2.2) | ||||
| 2 | Any | 1.7 (1.6, 1.8) | 0.075 | 2.6 (2.5, 2.7) | 0.024 | 1.4 (1.3, 1.5) | 0.39 | 2.1 (2.0, 2.2) | 0.75 |
| Park count (tertiles) | |||||||||
| 1 | (0, 7) | 1.5 (1.4, 1.6) | 2.4 (2.3, 2.6) | 1.4 (1.3, 1.5) | 2.1 (2.0, 2.3) | ||||
| 2 | (7,11) | 1.6 (1.5, 1.8) | 2.5 (2.4, 2.7) | 1.4 (1.3, 1.5) | 2.1 (1.9, 2.2) | ||||
| 3 | (11, 45) | 1.7 (1.6, 1.8) | 0.065 | 2.6 (2.5, 2.7) | 0.12 | 1.4 (1.3, 1.5) | 0.93 | 2.0 (1.9, 2.1) | 0.34 |
| Park area (hectares) with <5% slope (tertiles) | |||||||||
| 1 | (0.0, 10.5) | 1.5 (1.4, 1.6) | 2.5 (2.4, 2.6) | 1.4 (1.3, 1.5) | 2.1 (1.9, 2.2) | ||||
| 2 | (10.5, 23.1) | 1.7 (1.6, 1.8) | 2.6 (2.5, 2.7) | 1.5 (1.4, 1.6) | 2.2 (2.1, 2.4) | ||||
| 3 | (23.1, 342.0) | 1.6 (1.5, 1.7) | 0.45 | 2.5 (2.3, 2.6) | 0.75 | 1.3 (1.2, 1.4) | 0.38 | 1.9 (1.8, 2.0) | 0.077 |
| Age cohort of 13 years, overall | 1.5 (1.4, 1.5) | 2.0 (1.9, 2.0) | 1.6 (1.5, 1.6) | 2.2 (2.1, 2.3) | |||||
| Residential density (tertiles) | |||||||||
| 1 | (0.0637, 5.3788) | 1.6 (1.5, 1.7) | 2.2 (2.1, 2.3) | 1.6 (1.5, 1.7) | 2.4 (2.2, 2.5) | ||||
| 2 | (5.3788, 8.9721) | 1.4 (1.2, 1.5) | 1.9 (1.7, 2.0) | 1.5 (1.4, 1.6) | 2.2 (2.1, 2.3) | ||||
| 3 | (8.9721, 86.0201) | 1.4 (1.3, 1.6) | 0.047 | 1.8 (1.7, 2.0) | <0.0001 | 1.6 (1.5, 1.7) | 0.89 | 2.1 (1.9, 2.2) | 0.002 |
| Residential density (dichotomized at transit threshold) | |||||||||
| 1 | (0.0637, 18.0000) | 1.5 (1.4, 1.5) | 2.0 (1.9, 2.0) | 1.6 (1.5, 1.7) | 2.2 (2.2, 2.3) | ||||
| 2 | (18.0000, 86.0201) | 1.5 (1.2, 1.8) | 0.74 | 1.9 (1.6, 2.2) | 0.7 | 1.5 (1.2, 1.7) | 0.39 | 1.8 (1.5, 2.1) | 0.003 |
| Supermarket (binary) | |||||||||
| 1 | None | 1.4 (1.3, 1.5) | 2.0 (1.9, 2.1) | 1.5 (1.4, 1.6) | 2.2 (2.1, 2.3) | ||||
| 2 | Any | 1.5 (1.4, 1.6) | 0.25 | 2.0 (1.9, 2.1) | 0.72 | 1.6 (1.5, 1.7) | 0.3 | 2.3 (2.1, 2.4) | 0.44 |
| Fast-food (binary) | |||||||||
| 1 | None | 1.5 (1.4, 1.6) | 2.0 (1.9, 2.1) | 1.6 (1.4, 1.7) | 2.2 (2.1, 2.3) | ||||
| 2 | Any | 1.4 (1.3, 1.5) | 0.69 | 2.0 (1.9, 2.1) | 0.93 | 1.6 (1.5, 1.7) | 0.55 | 2.2 (2.1, 2.3) | 0.92 |
| Park count (tertiles) | |||||||||
| 1 | (0, 7) | 1.4 (1.3, 1.6) | 1.9 (1.7, 2.0) | 1.6 (1.4, 1.7) | 2.2 (2.1, 2.3) | ||||
| 2 | (7, 11) | 1.5 (1.3, 1.6) | 2.0 (1.8, 2.1) | 1.6 (1.4, 1.7) | 2.2 (2.0, 2.3) | ||||
| 3 | (11, 45) | 1.5 (1.4, 1.6) | 0.57 | 2.0 (1.9, 2.2) | 0.071 | 1.6 (1.5, 1.7) | 0.89 | 2.3 (2.1, 2.4) | 0.52 |
| Park area (hectares) with <5% slope (tertiles) | |||||||||
| 1 | (0.0, 10.5) | 1.4 (1.3, 1.6) | 2.1 (1.9, 2.2) | 1.6 (1.5, 1.7) | 2.2 (2.1, 2.4) | ||||
| 2 | (10.5, 23.1) | 1.5 (1.4, 1.6) | 1.9 (1.8, 2.1) | 1.5 (1.4, 1.7) | 2.2 (2.0, 2.3) | ||||
| 3 | (23.1, 342.0) | 1.5 (1.4, 1.6) | 0.64 | 1.9 (1.8, 2.0) | 0.057 | 1.6 (1.5, 1.7) | 0.73 | 2.3 (2.1, 2.4) | 0.94 |
All BE characteristics are measured at a 1,600-meter buffer.
p-values compare the third with the first tertile (or any vs none) at Years 2 and 3 of follow-up, separately by sex.
BE, built environment.
Higher residential density was associated with lower BMI increases for girls at Year 3 across all age cohorts. The 3-year association between residential density (comparing third with first tertile) for girls amounts to a decrement of 0.2 (95% CI=0.1, 0.3; p=0.004), 0.3 (95% CI=0.1, 0.5; p=0.002), and 0.3 BMI units (95% CI=0.2, 0.5; p<0.0001) in the age cohorts of 5, 9, and 13 years, respectively. Higher residential density was also significantly associated with less BMI gain for boys at Year 3 in the age cohorts of 5 and 13 years. There was a similar pattern at Year 3 for boys in the age cohort of 9 years, but estimates were imprecise and crossed the null value. The 3-year association between residential density (comparing third with first tertile) for boys amounts to a 0.3 BMI unit decrement for the age cohort of 5 years (95% CI=0.2, 0.5; p<0.0001) and 0.3 BMI units for the age cohort of 13 years (95% CI=0.1, 0.5; p=0.002). Similar findings were observed for residential density dichotomized at the transit threshold.
Fast-food presence was associated with a 0.2 BMI unit larger increase for boys in the age cohort of 5 years at Years 2 (95% CI=0.1, 0.3; p=0.005) and 3 (95% CI=0.1, 0.4; p=0.0003) and at Year 3 for girls in the age cohort of 9 years (95% CI=0.0, 0.4; p=0.02). The authors observed no associations for fast food for adolescents. Supermarket presence was associated with a significant difference in BMI for girls in the age cohort of 5 years at Year 2.
There were no significant associations between BMI change and counts of parks. There were no significant associations between BMI change and park area with a <5% grade, except for boys in the age cohort of 5 years at Year 3, where those in the highest tertile of park area had greater BMI increases. Appendix A (available online) provides the exploratory analyses to inform operationalization of parks area and slope variables.
DISCUSSION
The M2H study is one of the largest pediatric cohorts to examine cross-sectional and longitudinal associations of neighborhood residential density, food environment, and parks with BMI change in children and adolescents. This study linked clinical data and home addresses to county BE data and affords comparison with adult findings from the same population. Among these 15,920 insured children and adolescents in KC, those who live in denser neighborhoods, without fast-food restaurants, and near more parks have lower BMI and less likely to have obesity.
These cross-sectional findings align with prior studies that found associations between residential density and lower BMI in children and adolescents. This relationship could be mediated by physical activity (PA),34, 35, 36, 37 although residential density could also be a proxy for residual confounding by SES (because the authors did not have access to measures of SES besides property values, such as household income or parental education). Others have found cross-sectional associations between proximity to fast food and adult BMI.38 This study's findings did not reveal cross-sectional associations between supermarket count and BMI; indeed, the literature on this association in children has been mixed.39 The cross-sectional association between parks and lower BMI is consistent with findings of several cross-sectional studies reporting the presence of (and proximity to) neighborhood parks and green spaces to be associated with PA,37,40, 41, 42, 43 although others have yielded mixed findings.44 Baseline BMI was strongly associated with residential property value, even in the youngest age cohort, and these associations were stronger than associations with BE measures. This is consistent with prior work45,46 suggesting that household socioeconomic roots of childhood obesity are not primarily explained by environmental factors and suggests that future work should focus on economic determinants of childhood energy balance behaviors beyond residential BE.
Longitudinally, greater residential density was independently associated with smaller BMI increase for girls (all age groups) and boys (youngest and oldest age groups) over 2–3 years. The lack of significant associations at Year 1 may be because BE exerts influence over a longer period of time. For illustrative purposes, the results suggest that a girl aged 13 years who is 1.6 m tall (5 feet 3 inches) and weighs 55.4 kg (BMI=21.6 kg/m2) who lives in a high-density neighborhood would be expected to weigh 62.9 kg (BMI=23.4 kg/m2) at age 16 years, whereas another girl of the same height and weight at age 13 years living in a low-density neighborhood would be expected to weigh 64.0 kg (23.8 kg/m2) at age 16 years. For girls aged 13 years, the average 3-year difference in BMI change comparing highest with lowest residential density (0.4 kg/m2) is one fifth of the 3-year difference in BMI change in the overall sample (2.0 kg/m2). Compared with findings18 in the adult M2H cohort, the 1.1 kg difference at 3 years for average girls aged 13 years is almost quadruple the difference in 3-year weight change (0.28 kg) for adults, between lowest and highest residential density tertiles,18 suggesting that walkability (or other correlates of density) has greater impact on children and adolescents than on adults.
In a national sample of U.S. kindergarteners,6 residential density was associated with lower prevalence of obesity at 9 years. A Massachusetts study7 also found an inverse relationship between residential density and BMI z-score. Taken together, these findings support the importance of urban form in shaping BMI; in denser neighborhoods, the shorter distances between origins and destinations support walking,19 an important source of PA for children and adolescents, which in turn is associated with lower weight status. Over the life course, these associations may contribute to the cross-sectional associations observed among adults.
Longitudinal associations of fast food and supermarkets with BMI change in children and adolescents in the M2H cohort were weak and mixed. Analyses of the M2H adult cohort similarly did not find a consistent association between food environment and weight change.18 This study's results differ from those of a recent New York City study47 that used randomly assigned public housing as a natural experiment and found that childhood obesity increased with proximity to fast food, with larger effects for younger children who attended nearby schools. Differences in study findings may be driven by differences in the SES of the 2 samples.
Presence of neighborhood parks and park area with <5% slope were not associated with change in BMI in most of the main comparisons. Steeper slopes (and smaller <5% slope area) in the Seattle area are often associated with views and may be a proxy for higher SES in ways not captured by property values, resulting in residual confounding by SES that attenuates the associations of interest. In the Massachusetts longitudinal cohort,7 recreational open spaces were similarly not associated with BMI z-score change in a similar age range. These findings in 2 different geographic regions call for further consideration of the mechanisms by which recreational environment support PA in children and adolescents.
Limitations
This study has several limitations, including various potential uncontrolled confounders. Duration of residence at baseline is unknown, so it is not possible to adjust for varying periods of BE exposure. Although 1,600-meter Euclidean buffers have been widely used to define the physical and social neighborhood, the extent to which they capture use of resources may vary by individual, social, cultural, economic, and other factors. Family behaviors play an important role in determining how children and adolescents interact with their BE. Simply residing in a neighborhood does not mean one is uniformly engaging with its BE characteristics—for example, eating at a nearby fast-food restaurant, shopping at a local grocery store, visiting parks, or walking around the neighborhood. Data on access to a car—which strongly affects access to BE resources—were not available. Using EHR-derived addresses does not account for children who split time between multiple homes or time spent in school, resulting in measurement error. Analyses were adjusted for residential property values, which only capture 1 dimension of individual SES. The findings’ generalizability may be limited by the stringent inclusion criteria and the fact that all individuals in the cohort had commercial or public health insurance.
Future research should integrate behavioral data that reflect how young residents of a neighborhood engage with the BE. Accelerometry, tracking devices, mobile phones, and survey data could be used for a more holistic view of actual behaviors related to PA and nutrition,29 both to understand the roots of childhood and adolescent obesity and to improve conceptual frameworks regarding BE measurement.
CONCLUSIONS
In the M2H study, lower residential density, presence of fast food, and lower property values were cross-sectionally associated with BMI and obesity prevalence in children and adolescents. Longitudinal associations between residential density and changes in BMI exceed those seen in the adults in the same population and may have a cumulative life course effect.
CRediT authorship contribution statement
Paula Maria Lozano: Conceptualization, Writing – original draft, Funding acquisition. Jennifer F. Bobb: Conceptualization, Methodology, Software, Formal analysis, Data curation, Writing – review & editing, Visualization, Funding acquisition. Flavia P. Kapos: Conceptualization, Methodology, Writing – original draft. Maricela Cruz: Methodology, Software, Data curation, Writing – review & editing. Stephen J. Mooney: Conceptualization, Methodology, Writing – review & editing, Supervision. Philip M. Hurvitz: Software, Resources, Data curation. Jane Anau: Project administration, Resources. Mary Kay Theis: Data curation. Andrea Cook: Conceptualization, Methodology. Anne Vernez Moudon: Conceptualization, Writing – review & editing, Supervision. David E. Arterburn: Conceptualization, Methodology, Writing – review & editing, Supervision, Funding acquisition. Adam Drewnowski: Conceptualization, Funding acquisition, Writing – review & editing.
ACKNOWLEDGMENTS
This study was supported by 3 grants from the NIH: 1 R01 DK 114196, 5 R01 DK076608, and 4 R00 LM012868.
AD has received grants, honoraria, and consulting fees from numerous food, beverage, and ingredient companies and from other commercial and nonprofit entities with an interest in diet quality and nutrient density of foods. The University of Washington receives research funding from public and private sectors. No other disclosures were reported.
The authors gratefully acknowledge SB Brush for her assistance in manuscript preparation.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.focus.2024.100225.
Appendix. Supplementary materials
REFERENCES
- 1.Goto R, Nianogo R, Okubo Y, Inoue K. Evaluation of obesity trends among US adolescents by socioeconomic status, 1999–2018. JAMA Pediatr. 2022;176(9):937–940. doi: 10.1001/jamapediatrics.2022.1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grant LP, Gennings C, Wickham EP, Chapman D, Sun S, Wheeler DC. Modeling pediatric body mass index and neighborhood environment at different spatial scales. Int J Environ Res Public Health. 2018;15(3):473. doi: 10.3390/ijerph15030473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saelens BE, Sallis JF, Frank LD, et al. Obesogenic neighborhood environments, child and parent obesity: the Neighborhood Impact on Kids study. Am J Prev Med. 2012;42(5):e57–e64. doi: 10.1016/j.amepre.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ribeiro AI, Santos AC, Vieira VM, Barros H. Hotspots of childhood obesity in a large metropolitan area: does neighbourhood social and built environment play a part? Int J Epidemiol. 2020;49(3):934–943. doi: 10.1093/ije/dyz205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pereira M, Nogueira H, Padez C. The role of urban design in childhood obesity: a case study in Lisbon, Portugal. Am J Hum Biol. 2019;31(3):e23220. doi: 10.1002/ajhb.23220. [DOI] [PubMed] [Google Scholar]
- 6.Jia P, Xue H, Cheng X, Wang Y, Wang Y. Association of neighborhood built environments with childhood obesity: evidence from a 9-year longitudinal, nationally representative survey in the US. Environ Int. 2019;128:158–164. doi: 10.1016/j.envint.2019.03.067. [DOI] [PubMed] [Google Scholar]
- 7.Duncan DT, Sharifi M, Melly SJ, et al. Characteristics of walkable built environments and BMI z-scores in children: evidence from a large electronic health record database. Environ Health Perspect. 2014;122(12):1359–1365. doi: 10.1289/ehp.1307704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rummo P, Sze J, Elbel B. Association between a policy to subsidize supermarkets in underserved areas and childhood obesity risk. JAMA Pediatr. 2022;176(7):646–653. doi: 10.1001/jamapediatrics.2022.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hobbs M, Griffiths C, Green MA, Christensen A, McKenna J. Examining longitudinal associations between the recreational physical activity environment, change in body mass index, and obesity by age in 8864 Yorkshire Health Study participants. Soc Sci Med. 2019;227:76–83. doi: 10.1016/j.socscimed.2018.06.027. [DOI] [PubMed] [Google Scholar]
- 10.Wilkins E, Radley D, Morris M, et al. A systematic review employing the GeoFERN framework to examine methods, reporting quality and associations between the retail food environment and obesity. Health Place. 2019;57:186–199. doi: 10.1016/j.healthplace.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Mooney SJ, Bobb JF, Hurvitz PM, et al. Impact of built environments on body weight (the moving to health study): protocol for a retrospective longitudinal observational study. JMIR Res Protoc. 2020;9(5):e16787. doi: 10.2196/16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.SAS program for 2000 CDC Growth Charts (Ages 0–20 years). Growth chart training. Division of Nutrition, Physical Activity, and Obesity of the Centers for Disease Control and Prevention. https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Updated January 9, 2023. Accessed April 19, 2023.
- 13.Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? [published correction appears in Eur J Clin Nutr. 2005;59(6):807] Eur J Clin Nutr. 2005;59(3):419–425. doi: 10.1038/sj.ejcn.1602090. [DOI] [PubMed] [Google Scholar]
- 14.Berkey CS, Colditz GA. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol. 2007;17(1):44–50. doi: 10.1016/j.annepidem.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 15.Vanderwall C, Eickhoff J, Randall Clark R, Carrel AL. BMI z-score in obese children is a poor predictor of adiposity changes over time. BMC Pediatr. 2018;18(1):187. doi: 10.1186/s12887-018-1160-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly AS, Daniels SR. Rethinking the use of body mass index z-score in children and adolescents with severe obesity: time to kick it to the curb? J Pediatr. 2017;188:7–8. doi: 10.1016/j.jpeds.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Freedman DS, Butte NF, Taveras EM, Goodman AB, Ogden CL, Blanck HM. The limitations of transforming very high body mass indexes into z-scores among 8.7 million 2- to 4-year-old children. J Pediatr. 2017;188:50–56.e1. doi: 10.1016/j.jpeds.2017.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buszkiewicz JH, Bobb JF, Hurvitz PM, et al. Does the built environment have independent obesogenic power? Urban form and trajectories of weight gain. Int J Obes (Lond) 2021;45(9):1914–1924. doi: 10.1038/s41366-021-00836-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mooney SJ, Hurvitz PM, Moudon AV, Zhou C, Dalmat R, Saelens BE. Residential neighborhood features associated with objectively measured walking near home: revisiting walkability using the Automatic Context Measurement Tool (ACMT) Health Place. 2020;63 doi: 10.1016/j.healthplace.2020.102332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pouliou T, Elliott SJ. Individual and socio-environmental determinants of overweight and obesity in Urban Canada. Health Place. 2010;16(2):389–398. doi: 10.1016/j.healthplace.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 21.Huang R, Moudon AV, Cook AJ, Drewnowski A. The spatial clustering of obesity: does the built environment matter? J Hum Nutr Diet. 2015;28(6):604–612. doi: 10.1111/jhn.12279. [DOI] [PubMed] [Google Scholar]
- 22.Sarkar C, Webster C, Gallacher J. Association between adiposity outcomes and residential density: a full-data, cross-sectional analysis of 419 562 UK Biobank adult participants [published correction appears in Lancet Planet Health. 2017;1(8):e315] Lancet Planet Health. 2017;1(7):e277–e288. doi: 10.1016/S2542-5196(17)30119-5. [DOI] [PubMed] [Google Scholar]
- 23.Lopez RP. Neighborhood risk factors for obesity. Obesity (Silver Spring) 2007;15(8):2111–2119. doi: 10.1038/oby.2007.251. [DOI] [PubMed] [Google Scholar]
- 24.Lovasi GS, Neckerman KM, Quinn JW, Weiss CC, Rundle A. Effect of individual or neighborhood disadvantage on the association between neighborhood walkability and body mass index. Am J Public Health. 2009;99(2):279–284. doi: 10.2105/AJPH.2008.138230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rundle A, Field S, Park Y, Freeman L, Weiss CC, Neckerman K. Personal and neighborhood socioeconomic status and indices of neighborhood walk-ability predict body mass index in New York City. Soc Sci Med. 2008;67(12):1951–1958. doi: 10.1016/j.socscimed.2008.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pushkarev BS, Zupan JM. Public Transportation and Land Use Policy. Indiana University Press; Bloomington, IN: 1977. [Google Scholar]
- 27.Frank LD, Pivo G. Impacts of mixed used and density on utilization of three modes of travel: single-occupant vehicle, transit, walking. Transp Res Rec. 1994;1466:44–52. [Google Scholar]
- 28.U.S. Department of Justice, Civil Rights Division . U.S. Department of Justice, Civil Rights Division; Washington, DC: Published September 15, 2010. ADA standards for accessible design.https://www.ada.gov/law-and-regs/design-standards/2010-stds/ Accessed April 19, 2023. [Google Scholar]
- 29.Drewnowski A, Buszkiewicz J, Aggarwal A, Rose C, Gupta S, Bradshaw A. Obesity and the built environment: a reappraisal. Obesity (Silver Spring) 2020;28(1):22–30. doi: 10.1002/oby.22672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Drewnowski A, Aggarwal A, Cook A, Stewart O, Moudon AV. Geographic disparities in Healthy Eating Index scores (HEI-2005 and 2010) by residential property values: findings from Seattle Obesity Study (SOS) Prev Med. 2016;83:46–55. doi: 10.1016/j.ypmed.2015.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moudon AV, Cook AJ, Ulmer J, Hurvitz PM, Drewnowski A. A neighborhood wealth metric for use in health studies. Am J Prev Med. 2011;41(1):88–97. doi: 10.1016/j.amepre.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pinheiro J, Bates D, R Core Team . R Foundation for Statistical Computing; Vienna, Austria: Published 2022. nlme: linear and nonlinear mixed effects models.https://CRAN.R-project.org/package=nlme Accessed July 28, 2022. [Google Scholar]
- 33.Pinheiro J, Bates D. Springer-Verlag; Berlin, Germany: 2000. Mixed-Effects Models in S & S-PLUS. [DOI] [Google Scholar]
- 34.Ding D, Sallis JF, Kerr J, Lee S, Rosenberg DE. Neighborhood environment and physical activity among youth a review. Am J Prev Med. 2011;41(4):442–455. doi: 10.1016/j.amepre.2011.06.036. [DOI] [PubMed] [Google Scholar]
- 35.Carlson JA, Sallis JF, Kerr J, et al. Built environment characteristics and parent active transportation are associated with active travel to school in youth age 12–15. Br J Sports Med. 2014;48(22):1634–1639. doi: 10.1136/bjsports-2013-093101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carlson JA, Saelens BE, Kerr J, et al. Association between neighborhood walkability and GPS-measured walking, bicycling and vehicle time in adolescents. Health Place. 2015;32:1–7. doi: 10.1016/j.healthplace.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buck C, Tkaczick T, Pitsiladis Y, et al. Objective measures of the built environment and physical activity in children: from walkability to moveability. J Urban Health. 2015;92(1):24–38. doi: 10.1007/s11524-014-9915-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Erpecum CL, van Zon SKR, Bültmann U, Smidt N. The association between fast-food outlet proximity and density and Body Mass Index: findings from 147,027 Lifelines Cohort Study participants. Prev Med. 2022;155 doi: 10.1016/j.ypmed.2021.106915. [DOI] [PubMed] [Google Scholar]
- 39.Zhou Q, Zhao L, Zhang L, et al. Neighborhood supermarket access and childhood obesity: a systematic review. Obes Rev. 2021;22(suppl 1):e12937. doi: 10.1111/obr.12937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bell JF, Wilson JS, Liu GC. Neighborhood greenness and 2-year changes in body mass index of children and youth. Am J Prev Med. 2008;35(6):547–553. doi: 10.1016/j.amepre.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kowaleski-Jones L, Fan JX, Wen M, Hanson H. Neighborhood context and youth physical activity: differential associations by gender and age. Am J Health Promot. 2017;31(5):426–434. doi: 10.1177/0890117116667353. [DOI] [PubMed] [Google Scholar]
- 42.Nordbø ECA, Raanaas RK, Nordh H, Aamodt G. Neighborhood green spaces, facilities and population density as predictors of activity participation among 8-year-olds: a cross-sectional GIS study based on the Norwegian mother and child cohort study. BMC Public Health. 2019;19(1):1426. doi: 10.1186/s12889-019-7795-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clary C, Lewis D, Limb E, et al. Longitudinal impact of changes in the residential built environment on physical activity: findings from the ENABLE London cohort study. Int J Behav Nutr Phys Act. 2020;17(1):96. doi: 10.1186/s12966-020-01003-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morgan Hughey S, Kaczynski AT, Child S, Moore JB, Porter D, Hibbert J. Green and lean: is neighborhood park and playground availability associated with youth obesity? Variations by gender, socioeconomic status, and race/ethnicity. Prev Med. 2017;95(Suppl):S101–S108. doi: 10.1016/j.ypmed.2016.11.024. [DOI] [PubMed] [Google Scholar]
- 45.Drewnowski A, Aggarwal A, Tang W, Moudon AV. Residential property values predict prevalent obesity but do not predict 1-year weight change. Obesity (Silver Spring) 2015;23(3):671–676. doi: 10.1002/oby.20989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Buszkiewicz JH, Rose CM, Ko LK, et al. Associations between neighborhood built environment, residential property values, and adult BMI change: the Seattle Obesity Study III. SSM Popul Health. 2022;19 doi: 10.1016/j.ssmph.2022.101158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Han J, Schwartz AE, Elbel B. Does proximity to fast food cause childhood obesity? Evidence from public housing. Reg Sci Urban Econ. 2020;84 doi: 10.1016/j.regsciurbeco.2020.103565. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.