Abstract
Most cancer-related deaths are due to metastatic disease. There is now an emerging evidence base suggesting that a subgroup of metastatic patients benefit significantly from local resection (surgery) or ablation (stereotactic ablative body radiation, SABR) of their metastatic sites. These patients are in what has been termed the 'oligometastatic state’, a transitional window between local and disseminated disease where locally ablative, metastasis-directed therapy prolongs progression-free survival, improves overall survival and sometimes achieves cure. Appropriately selecting those who fit this oligometastatic phenotype, while integrating advances in ablative technologies such as SABR with modern systemic treatments, is an evolving challenge for oncologists.
Keywords: oligometastatic, oligoprogression, metastasectomy, SABR, RFA
Key points
-
•
Cancer rates globally are estimated to increase by 47% in 2040, with most cancer-related deaths resulting from metastasis.
-
•
Oligometastatic disease can be defined as a patient with a limited burden of metastatic disease.
-
•
Metastases-directed locally ablative treatment in cancer patients with oligometastatic disease can improve cancer clinical outcomes. Advances in SABR radiotherapy technology (immobilisation and organ motion tracking, image guidance and adaptive planning) have allowed ablative treatments to be given to metastatic sites not previously safe to do so.
-
•
Predictive factors for patients who may benefit from SABR include the size, site and number of metastases, the length of interval between progression, primary tumour histology, number of lines of previous systemic treatment and performance status.
-
•
The oligometastatic phenotype will evolve with further retrospective data analysis, prospective randomized clinical trials, advances in diagnostic radiology, new biomarkers and further study exploring the optimisation of SABR with systemic and immune-oncology treatments.
Introduction
Globally, cancer rates expected to increase by 47% by 2040.1 In the UK each year there are 140,000 new metastatic cases diagnosed.2 Most cancer deaths (up to 90%) result from the metabolic and immunological sequalae of metastatic disease.3 The focus of treatment in the metastatic setting has conventionally been palliative systemic therapy aimed at prolonging survival, with low-dose radiotherapy used for palliation of symptoms only.
There is now a growing evidence base defining a subgroup of metastatic patients in a transitional state between localised and widespread disease, known as the 'oligometastatic state’. Patients with a limited burden of metastatic disease can achieve a significant improvement in long-term outcome (progression-free survival, overall survival), and in some cases cure, with metastasis-directed surgical resection or more recently stereotactic ablative radiotherapy (SABR).4 SABR treatment, the result of advances in radiotherapy technology over the years, can now deliver very high doses of radiation to metastatic sites while sparing normal tissue. In selected patients SABR can also be used as a strategy to delay burdensome systemic treatment with time to/time off chemotherapy or hormone treatment being considered a valuable endpoint for patients quality of life.5, 6 These interventions have been coupled with improvements in diagnostic imaging, with gains seen in the sensitivity of detecting early metastatic cancer, PSMA PET in prostate cancer being a prominent example.7 Appropriately identifying oligometastatic patients and integrating SABR with their systemic treatments is an ongoing challenge for oncologists.
Defining oligometastatic disease
There is no consensus on the definition of oligometastatic cancer, but no more than five radiologically visible metastases is considered a reasonable benchmark.8 A more qualitative approach to categorising oligometastatic disease, factoring in tumour type, timing of progression/recurrence, systemic treatment options and expected outcome of treatment, is seen in recently published guidelines.9 Oligometastatic disease can be further subcategorised based on disease chronicity: synchronous, in which oligometastatic disease presents at the time of initial diagnosis; metachronous, in which oligometastatic recurrence presents after treatment of the initial primary site; and oligoprogressive, where disease progresses at a few metastatic sites while other sites are stable (Box 1).
Box 1.
Common terms associated with the oligometastatic disease state and its treatment
|
The biological basis of the oligometastatic state is thought to be due to the existence of different cell phenotypes within a tumour's population. Genomic studies have demonstrated that metastatic tumour is composed of differing subclones of cells and that there is intra-tumour heterogeneity between different metastatic sites.10 Certain subclones may be resistant to chemotherapy or acquire resistance after treatment due to selective pressure.11 These aggressive subclones may be responsible for the further disease progression and, in turn, be the source of further metastatic dissemination. Because metastases can arise not just from the primary tumour but also from existing metastases, targeting and ablating the resistant subclones present in oligometastatic disease may halt or delay further progression.
Selecting metastatic patients to undergo SABR treatment
Several tumour- and patient-specific factors are considered when deciding on which patients may benefit from ablative treatment:
-
•
The number of metastases: Generally, having fewer than five metastases has been considered an important factor in predicting that a patient is in the oligometastatic state.9
-
•
What organ is involved: Patients with lung and nodal metastases have longer overall survival (OS) compared to liver and brain metastases.12
-
•
The size of individual metastases: Large cohort studies have demonstrated that metastases under 3 cm are associated with improved OS,13 with a lung metastasis size >2 cm having been shown to predict a short time to disseminated disease.14
-
•
Progression-free survival length: Short intervals between disease progression infer poor prognostic outcomes.15
-
•
The number of previous systemic treatment lines: Patients who received three or more lines of chemotherapy before SABR have a worse progression-free survival outcome.16
-
•
The primary tumour histology: There is a strong correlation with both prostate and breast primary cancer and improved survival with SABR.17
-
•
The patient's performance status (PS): Patients with better PS have an increased OS benefit with SABR.18 Most PS assessments include parameters of age, cognition, mobility, comorbidities and sarcopenia, with formal scoring assessments available.19
Metastasis-directed ablative treatment
SABR is highly focused radiation treatment that delivers a high dose to the tumour while limiting the dose to surrounding organs. Multiple technological advances have led to the development of this innovative treatment. These include linear accelerators (LINACs) that can deliver radiation with multiple small-field photon beams of various shapes and intensities at different angles to precisely target the tumour. Advances in patient immobilisation, body motion tracking and image guidance have facilitated safe ablative radiation approaches; Table 1 sets out SABR doses recommended by the SABR UK Consortium.
Table 1.
Typical prescriptions for oligometastatic sites recommended by the SABR UK Consortium.27 The dose prescribed depends on a number of factors including therapeutic goal, tumour location, histopathological subtype, and radiation dose to adjacent organs at risk
| Oligometastatic site | Dose ranges |
|---|---|
| Spine | 24 Gy in 2 fractions 27 Gy in 3 fractions 30 Gy in 5 fractions (re-irradiation) |
| Lung (peripheral, away from chest wall) | 54 Gy in 3 fractions |
| Lung (peripheral, abutting/overlapping chest wall) | 60 Gy in 5 fractions 55 Gy in 5 fractions |
| Lung (centrally located tumours, not invading central structures and not ultra-central) | 60 Gy in 8 fractions |
| Liver | 45-60 Gy in 3 fractions 50-60 Gy in 5 fractions |
| Adrenal | 30-36 Gy in 3 fractions 45 Gy in 5 fractions |
MRI-guided stereotactic adaptive radiotherapy (SMART) has the potential to further expand the ablative prowess of SABR. By providing enhanced soft tissue definition through MRI, the radiation treatment plan delivered to the patient can be changed to account for temporal changes in anatomical organ and tumour position (eg internal organ motion, tumour shrinkage, etc). These adapted plans can now be delivered on LINACs that can track in real time the position of the target and normal tissue, only delivering radiation when the target is within a certain treatment boundary. This increased accuracy allows for the investigation of whether larger radiation doses delivered in shorter treatment courses can achieve higher rates of local control. For example, the Emerald trial is a currently recruiting phase I non-randomised study in patients with localised pancreatic cancer. The trial will be looking at the safety of dose-escalated SABR to the pancreas with 50Gy in five fractions, 39Gy in three fractions and 25Gy in a single fraction.20
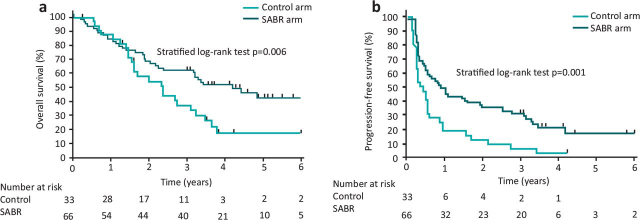
Overall, post-SABR local control of 80% at 2–3 years can be expected.21 A landmark phase II randomised trial (SABR COMET) has shown a significant survival benefit in oligometastatic patients, across a range of primary tumour types, who have undergone SABR. The 5-year OS rate was 42% compared to 18% in oligometastatic patients in the SABR versus non-SABR treatment arms respectively, with no detrimental impact on quality of life after SABR treatment (Fig 1).4 Furthermore, in selected patients SABR can also be used as a strategy to delay burdensome systemic treatment with time to/time off chemotherapy/hormone treatment being considered a valuable endpoint for patients quality of life.5, 6 One study, for example, demonstrated a median 8-month extra androgen-deprivation free survival in metastatic prostate patients treated with metastasis directed SABR as an initial substitute to commencing systemic treatment.
Fig 1.
Kaplan-Meier plots for a) overall survival and b) progression-free survival seen in the SABR COMET Trial.4
Non-SABR metastasis-directed treatment such as surgical metastasectomy and interventional-radiology-led procedures, eg radiofrequency ablation (RFA), microwave ablation (MWA) and irreversible electroporation (IRE), are valuable alternative therapeutic options in oligometastatic patients. One large surgical series, exploring outcomes after lung metastasectomy, demonstrated an OS rate of 36% at 5 years and 26% at 10 years.22 This series included a broad range of primary tumour histology sites including epithelial tumours, sarcomas, germ cell tumours and metastatic melanomas.22 Resection of brain metastasis can improve OS and local control in selected patients.23 Neurosurgical resection is often accompanied by adjuvant stereotactic radiation to the surgical cavity, which improves local control.24 Interventional radiologists also have an important role in the management of oligometastatic disease. Various directly ablative procedures are available, the most frequently used being percutaneous RFA, a technique of tissue ablation that is used to treat lung, liver, and kidney metastases.25 It involves placing a needle-type electrode that uses heat generated by radio waves to destroy tissue directly into the tumour site. The CLOCC trial explored its use in unresectable CRC liver metastasis and showed an OS benefit (median 45.6 months) compared to systemic treatment alone (median 40.5 months).26 There is currently no randomised evidence comparing SABR to RFA treatment in the oligometastatic setting.
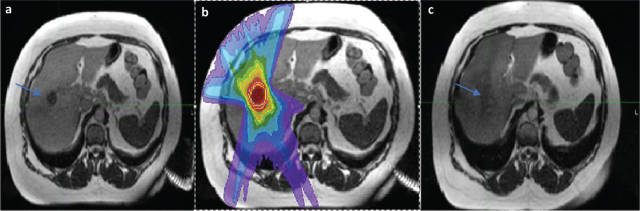
Fig 2 shows a case example of a complete response to treatment in a patient undergoing SABR for a solitary liver metastasis following breast cancer.
Fig 2.
Case example oligometastatic SABR. (a) A 53-year-old woman with a background history of triple-negative local breast cancer presents, 2 years after her initial diagnosis, with a solitary biopsy-proven liver metastasis (arrow). (b) She undergoes 45 Gy in 3 fractions SABR to this oligometastatic site. (c) A 6-month post treatment MRI shows a complete response to treatment (arrow).
Future developments and conclusion
The definition, treatment, and subcategorisation of the oligometastatic phenotype will evolve as the following developments occur:
-
•
Further randomised clinical trials are completed. The SABR COMET 10 trial, for example, is investigating clinical outcomes in patients with 4–10 metastatic lesions treated with SABR, asking the question whether there is benefit with SABR in patients with more than three metastatic lesions. Other clinical trials will explore the combination and optimisation of SABR with immunotherapies.
-
•
Imaging modalities become more sensitive. It may become possible to detect and locally ablate what is currently occult disease, as shown in the development of PSMA PET CT prostate cancer.
-
•
Novel biomarkers emerge, for example blood circulating tumour DNA (ct DNA), that might identify patients who are more likely to benefit from local ablative therapies.
Appropriately selecting those who fit the oligometastatic phenotype, while integrating advances in ablative radiotherapy technologies with modern systemic treatments, will continue to be an increasingly important paradigm in improving survival in the metastatic stage.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.2 NHS England,. Stereotactic ablative radiotherapy (SABR) for patients with metachronous extracranial oligometastatic cancer (all ages). www.england.nhs.uk/publication/stereotactic-ablative-radiotherapy-sabr-for-patients-with-metachronous-extracranial-oligometastatic-cancer-all-ages/. Accessed December 12, 2022.
- 3.Dillekås H, Rogers MS, Straume O. Are 90% of deaths from cancer caused by metastases? Cancer Med. 2019;8:5574–5576. doi: 10.1002/cam4.2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palma DA, Olson R, Harrow S, et al. Stereotactic ablative radiotherapy for the comprehensive treatment of oligometastatic cancers: long-term results of the SABR-COMET phase II randomized trial. J Clin Oncol. 2020;38:2830–2838. doi: 10.1200/JCO.20.00818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siva S, Louie AV. Substituting SABR for systemic therapy in oligometastatic renal cell carcinoma — buying time or time to change? Nat Rev Urol. 2022;19:197–198. doi: 10.1038/s41585-021-00560-3. [DOI] [PubMed] [Google Scholar]
- 6.Ost P, Reynders D, Decaestecker K, et al. Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: a prospective, randomized, multicenter Phase II trial. J Clin Oncol. 2018;36:446–453. doi: 10.1200/JCO.2017.75.4853. [DOI] [PubMed] [Google Scholar]
- 7.Tsechelidis I, Vrachimis A. PSMA PET in imaging prostate cancer. Front Oncol. 2022;12:831429. doi: 10.3389/fonc.2022.831429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dingemans A-MC, Hendriks LEL, Berghmans T, et al. Definition of synchronous oligometastatic non-small cell lung cancer – a consensus report. J Thorac Oncol. 2019;14:2109–2119. doi: 10.1016/j.jtho.2019.07.025. [DOI] [PubMed] [Google Scholar]
- 9.Lievens Y, Guckenberger M, Gomez D, et al. Defining oligometastatic disease from a radiation oncology perspective: An ESTRO-ASTRO consensus document. Radiother Oncol. 2020;148:157–166. doi: 10.1016/j.radonc.2020.04.003. [DOI] [PubMed] [Google Scholar]
- 10.Gerlinger M, Rowan AJ, Horswell S, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med. 2012;366:883–892. doi: 10.1056/NEJMoa1113205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Savas P, Teo ZL, Lefevre C, et al. The subclonal architecture of metastatic breast cancer: results from a prospective community-based rapid autopsy program ‘CASCADE.’. PLoS Med. 2016;13:e1002204. doi: 10.1371/journal.pmed.1002204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Franceschini D, De Rose F, Franzese C, et al. Predictive factors for response and survival in a cohort of oligometastatic patients treated with stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2019;104:111–121. doi: 10.1016/j.ijrobp.2018.12.049. [DOI] [PubMed] [Google Scholar]
- 13.Sharma A, Duijm M, Oomen-de Hoop E, et al. Survival and prognostic factors of pulmonary oligometastases treated with stereotactic body radiotherapy. Acta Oncol. 2019;58:74–80. doi: 10.1080/0284186X.2018.1521986. [DOI] [PubMed] [Google Scholar]
- 14.Nicosia L, Franceschini D, Perrone-Congedi F, et al. A multicenter LArge retrospectIve daTabase on the personalization of stereotactic ABlative radiotherapy use in lung metastases from colon-rectal cancer: The LaIT-SABR study. Radiother Oncol. 2022;166:92–99. doi: 10.1016/j.radonc.2021.10.023. [DOI] [PubMed] [Google Scholar]
- 15.Chen H, Poon I, Atenafu EG, et al. Development of a prognostic model for overall survival in patients with extracranial oligometastatic disease treated with stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2021;114:892–901. doi: 10.1016/j.ijrobp.2021.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Klement RJ, Guckenberger M, Alheid H, et al. Stereotactic body radiotherapy for oligo-metastatic liver disease - Influence of pre-treatment chemotherapy and histology on local tumor control. Radiother Oncol. 2017;123:227–233. doi: 10.1016/j.radonc.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 17.Franzese C, Di Brina L, D'Agostino G, et al. Predictive factors for survival outcomes of oligometastatic prostate cancer patients treated with metastases-directed therapy: a recursive partitioning-based analysis. J Cancer Res Clin Oncol. 2019;145:2469–2479. doi: 10.1007/s00432-019-03007-w. [DOI] [PubMed] [Google Scholar]
- 18.Yamamoto T, Niibe Y, Aoki M, et al. Analyses of the local control of pulmonary Oligometastases after stereotactic body radiotherapy and the impact of local control on survival. BMC Cancer. 2020;20:997. doi: 10.1186/s12885-020-07514-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.West H, Jin JO. Performance status in patients with cancer. JAMA Oncol. 2015;1:998. doi: 10.1001/jamaoncol.2015.3113. [DOI] [PubMed] [Google Scholar]
- 20.20 University of Oxford Medical Sciences Division,. Evaluation of hypofractionated adaptive radiotherapy using the MR Linac in localised pancreatic cancer. www.oncology.ox.ac.uk/clinical-trials/oncology-clinical-trials-office-octo/current-trials/emerald-pancreas (Accessed 24 November 2022).
- 21.Royal College of Radiology . Radiotherapy dose fractionation. Third edition. RCR; 2019. www.rcr.ac.uk/publication/radiotherapy-dose-fractionation-third-edition [Google Scholar]
- 22.Pastorino U, Buyse M, Friedel G, et al. Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. J Thorac Cardiovasc Surg. 1997;113:37–49. doi: 10.1016/s0022-5223(97)70397-0. [DOI] [PubMed] [Google Scholar]
- 23.Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990;322:494–500. doi: 10.1056/NEJM199002223220802. [DOI] [PubMed] [Google Scholar]
- 24.El Shafie RA, Dresel T, Weber D, et al. Stereotactic cavity irradiation or whole-brain radiotherapy following brain metastases resection – outcome, prognostic factors, and recurrence patterns. Front Oncol. 2020;10:693. doi: 10.3389/fonc.2020.00693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Winkelmann MT, Clasen S, Pereira PL, Hoffmann R. Local treatment of oligometastatic disease: current role. Br J Radiol. 2019;92:20180835. doi: 10.1259/bjr.20180835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruers T, Van Coevorden F, Punt CJA, et al. Local treatment of unresectable colorectal liver metastases: results of a randomized phase II trial. J Natl Cancer Inst. 2017;109:djx015. doi: 10.1093/jnci/djx015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.27 SABR UK Consortium,. Stereotactic Ablative Body Radiation Therapy (SABR): a resource. www.sabr.org.uk/wp-content/uploads/2019/04/SABRconsortium-guidelines-2019-v6.1.0.pdf [Accessed 30 January 2023].