Abstract
With the increasing volume of diagnostic imaging undertaken in an ageing population, adrenal incidentalomas (AIs) are increasingly commonly seen. These masses are most likely to be benign, but a small proportion may be malignant. Similarly, they are usually non-functional, but ∼14% are functional, ie hormone-secreting tumours. Clinical, biochemical and radiological assessment is mandated to stratify patients into those requiring radiological surveillance, medical management or surgical intervention or who can be discharged. Mass characteristics on cross-sectional (CT/MRI) imaging influence the need for radiological surveillance. Functional tumours where excess cortisol, aldosterone or catecholamine are secreted should be excluded, with mild autonomous cortisol secretion (MACS) and primary aldosteronism (PA) as the two most common functional states. MACS and PA are associated with an increased risk of cardiometabolic disease (eg hypertension, type 2 diabetes) and cardiovascular morbidity/mortality (eg coronary heart disease). Multidisciplinary management is critical for selected cases; the majority of adrenal incidentalomas only require a single assessment.
KEYWORDS: Adrenal incidentaloma, hormone excess, CT/MRI, primary aldosteronism, mild autonomous cortisol secretion
Key points
-
•
Adrenal incidentalomas are common and mutidisciplinary expertise is critical to triage them effectively into the most appropriate clinical pathway.
-
•
Cross-sectional imaging with CT/MRI can characterise the vast majority of masses but occasionally functional imaging may be needed.
-
•
Functional imaging with 18F-FDG PET-CT, 123I-MIBG SPECTCT and 11C-metomidate PET-CT can be performed if there are concerns regarding malignancy, phaeochromocytoma or primary aldosteronism.
-
•
Mild autonomous cortisol excess (MACS) is frequently associated with cardiometabolic comorbidities.
-
•
Primary hypoaldosteronism work up is complex and requries screening, confirmation and lateralisation with may require adrenal venous sampling and/or 11C-metomidate PET/CT.
Introduction
Adrenal incidentalomas are increasingly being recognized, due to the widespread use of high-resolution, cross-sectional imaging combined with an ageing population. An adrenal incidentaloma is 'an adrenal mass ≥1 cm in diameter, not apparent clinically, detected during imaging without prior clinical suspicion of disease’.1 There is a large differential diagnosis for these masses, ranging from a benign, non-functioning adrenal adenoma to an adrenocortical carcinoma. An adrenal mass <1 cm typically does not require further investigation unless clinical signs/symptoms are evident or there are features that raise concern regarding malignancy or a phaeochromocytoma.
Two broad clinical considerations are important in the triage of these patients: functional status, and the risk of primary or secondary malignancy. Those with non-functional tumours need follow-up to assess the risk of progression to malignant disease. A rigorous clinical, biochemical and radiological approach is needed to direct patients to the most appropriate clinical pathway. Such patients may require multidisciplinary involvement that could span endocrinology and endocrine surgery, radiology and interventional radiology, nuclear medicine and clinical genetics.
Prevalence of adrenal masses
Adrenal incidentalomas represent a common, complex problem. Prevalence in the general population is ∼1–6%, increasing with age: they are rare in childhood but affect ∼3% of those aged over 50 years and >7% in those aged over 70 years.1, 2 NHS Diagnostic Imaging Datasets report 6 million CT scans, and 3.8 million MRI scans (any anatomical region) being performed in 2018. The overwhelming majority of adrenal incidentalomas are benign, but ∼2% represent primary adrenal malignancies. Furthermore, ∼14% of adrenal incidentalomas are functional tumours that may secrete excess cortisol, aldosterone, catecholamines or (rarely) androgens. Considering their high prevalence and the volume of diagnostic imaging, the public health challenge is managing this 'disease of modern technology’.3
Aetiology of adrenal masses
Classification of these masses can be based on anatomical factors (cortical versus medullary; Box 1) or aetiology (benign versus malignant or non-functional versus functional; Box 2). However, based on structural appearances there are five categories:
-
•
adrenal adenomas and nodular hyperplasia
-
•
other benign lesions (myelolipomas, cysts, haematomas etc)
-
•
adrenocortical carcinomas (ACC)
-
•
other malignant tumours (metastases, sarcomas, lymphoma etc) (adrenal cancers ∼4%)
-
•
phaeochromocytomas (∼7%).
Box 1.
Aetiology by anatomy
Cortical tumours
|
Box 2.
Aetiology by nature
Benign FunctioningNon-functioning
|
May secrete cortisol, aldosterone, sex hormone secretion.
Usually benign, but maybe malignant; catecholamine secreting.
Radiological assessment of adrenal lesions
CT, MRI and functional imaging constitute the main imaging techniques.
Initial radiological assessment is with cross-sectional evaluation by CT/MRI. Using multi-phase, contrast-enhanced CT and multi-sequence MRI scanning it is possible to differentiate the likely aetiology. Various clinical and radiological factors increase the likelihood of malignancy, including older age, previous malignancy, size (>4 cm) and morphological characteristics (homogenous versus heterogenous density). The absence of tumour growth during 6–12 months’ longitudinal follow-up also provides reassurance; criteria indicative of significant growth are >20% relative change with a >5 mm absolute size increase.
Normal adrenal anatomy
On CT/MRI, adrenal glands are surrounded by fat in the peri-renal space. The right adrenal gland lies medial to the liver (right lobe), lateral to the diaphragm (right crus) and superior to the right kidney; the left adrenal gland lies anteromedial to the upper pole of the left kidney, lateral to the left crus of the diaphragm and posterior to the pancreas. On CT, adrenal glands are shaped like an inverted ‘V’ or ‘Y’ with a body, medial and lateral limb. Each limb has a smooth outline and is uniform in thickness, (∼5–7 mm), with each gland up to 3 cm in length.
CT scan
CT can detect lesions >5 mm. On unenhanced or post-contrast CT, a lesion with an average Hounsfield unit (HU) <10 is likely to be a lipid-rich adenoma. However, as 30% of adenomas are lipid-poor, further assessment may be necessary. An adrenal lesion containing fat (<0 HU) can generally be considered benign and either due to a myelolipoma or adenoma. Adenomas and benign lesions also display 'contrast enhancement washout’ (a relative washout of >40% and an absolute washout of >60%).
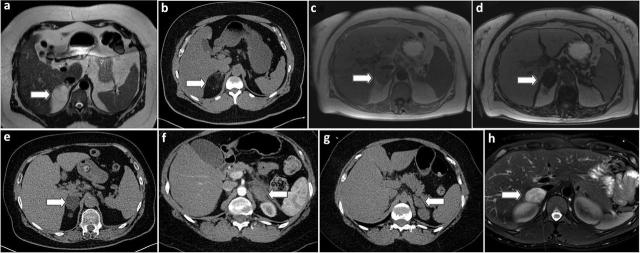
MRI scan
MRI offers non-ionising radiation and superior tissue contrast resolution. Chemical shift imaging relies on protons in water and lipids vibrating at different frequencies. Adrenal (lipid rich) adenomas will often have signal drop out, losing signal intensity on out of phase vs. in phase imaging (Fig 1). Myelolipomas contain extracellular fat and are therefore seen as high signal (the same as normal fat) on both T1 and T2 sequences (Fig 1).
Fig 1.
Representative adrenal CT and MRI images. (a) Right-sided adrenal myelolipoma (MRI image) (white arrow). (b) Right-sided adrenal myelolipoma (CT image) (white arrow). (c) MRI scan of right sided adrenal adenoma (in phase) (white arrow). (d) MRI scan of right sided adrenal adenoma (out of phase)shows loss of signal compared with in-phase image (white arrow). (e) CT scan of right sided adrenal adenoma (white arrow). (f) CT showing left sided adrenal haemorhage with adjacent fat stranding (white arrow). (g) CT showing resolution of left sided adrenal haemorhage (white arrow). (h) MRI scan (T2 fat suppressed) right sided phaeochromocytoma (white arrow).
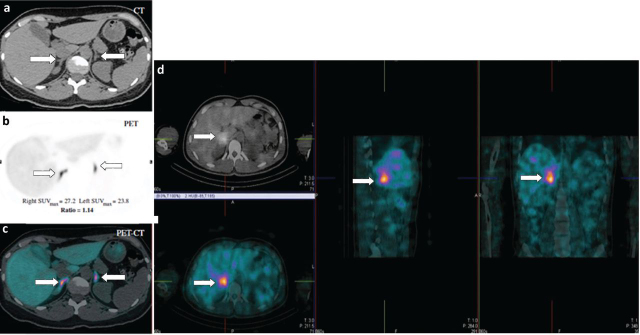
Functional imaging
PET/CT with Fluorine-18-fluorodeoxyglucose (18F-FDG) maybe needed to evaluate indeterminate masses (Fig 2). Importantly, even in patients with cancer, adrenal tumours are frequently benign. 18F-FDG PET-CT is particularly useful to exclude extra-adrenal disease burden. Iodine-123-labeled metaiodobenzylguanidine (123I-MIBG) SPECT-CT is used for diagnosis and staging of phaeochromocytomas. MIBG SPECT-CT is useful for surgical planning by confirming/excluding extra-adrenal disease and for post-surgical evaluation with persistent abnormal biochemistry. More recently, 11C-metomidate PET/CT is used as an adjunct/substitute for lateralisation of primary aldosteronism, when adrenal venous sampling has not been performed, technically challenging or the results inconclusive.4
Fig 2.
Left 11C-metomidate PET-CT scan (a-c) and MIBG scan (d). (a) CT: thickening/nodular change in the body/proximal medial limb of both adrenal glands (white arrows). (b) PET findings suggest maximal tracer uptake bilaterally in the same locations, greater uptake on the right (white arows). (c) Merged PET-CT image confirming co-localisation of cross-sectional and functional imaging findings (white arrows). (d) MIBG scan showing right sided phaeochromocytoma (white arrows).
Biochemical assessment of adrenal incidentalomas
Every patient with an adrenal incidentaloma should undergo clinical examination for symptoms/signs of adrenal hormone excess and biochemical assessment. There are three main functioning types of adrenal masses: excess mineralocorticoid (independent of renin secretion), excess glucocorticoid (independent of ACTH secretion), and excess catecholamine secretion.
Mineralocorticoid excess
Primary aldosteronism (PA) describes a group of closely related conditions characterised by an autonomous excess secretion of aldosterone (ie independent of the renin–angiotensin system) with resultant decreased plasma renin activity. The aetiology may be unilateral (aldosterone producing adenoma – APA or unilateral adrenal hyperplasia), which is treated surgically, or bilateral (bilateral hyperplasia), which is treated medically. Hypertension is the most common manifestation of PA, accounting for 1–2% of mild hypertension and up to 20% of resistant hypertension. Hypokalaemia is a late and variable manifestation; >50% are normokalaemic. PA carries an excess cardiovascular and renal risk mediated by both hypertension, and direct tissue effects of aldosterone to target organs, with an increased risk of cardiovascular events and target organ damage; risk of stroke, coronary artery disease, atrial fibrillation, and heart failure) are higher compared with essential hypertension.5
PA should be screened for by measuring the aldosterone/renin ratio (ARR) in patients with adrenal masses who also have hypertension or unexplained hypokalaemia. Caution must be taken around hypokalaemia or prescribed anti-hypertensive medication that can interfere with an accurate ARR interpretation.6 To ensure the validity of ARR, hypokalaemia should be rectified to minimise false negative results. Mineralocorticoid receptor antagonists (eg spironolactone, eplerenone, amiloride) should be withdrawn for 4 weeks before ARR testing. It is ideal if there is a washout of all interfering medications (β-adrenergic blockers, central α-2 agonists (eg clonidine, α-methyldopa), NSAIDS, ACE inhibitors, ARBs, renin inhibitors and calcium channel blockers (eg amlodipine, felodipine); other medications that have minimal effect on the ARR, can be substituted (eg doxazosin, hydralazine).7 However, in some circumstances, withdrawal or substitution of drugs may be considered unsafe or complex and in such circumstances it is preferable to screen the patients on their usual medications rather than not screening at all. ARR can be confidently interpreted in many cases even with the patient taking multiple anti-hypertensive drugs. When ARR is found to be elevated, then a confirmatory test is performed, eg saline infusion. Confirmation of the diagnosis should then proceed to subtype classification with lateralisation of the source to distinguish between an APA (treated surgically) and bilateral adrenal hyperplasia (treated with lifelong mineralocorticoid receptor antagonists, spironolactone or eplerenone). For lateralisation, adrenal venous sampling should be considered unless the patient is <40 years with a clear unilateral >1 cm adenoma.7 Recently [11C]metomidate PET-CT has shown to be suitable in selected cases.8
Glucocorticoid excess
All patients should undergo a 1 mg overnight dexamethasone suppression test to exclude cortisol excess. Serum cortisol concentration post-dexamethasone ≤ 50 nmol/L is the diagnostic threshold for exclusion of autonomous cortisol secretion. Cortisol concentrations between 51–138 nmol/L (without clinical signs of overt Cushing's syndrome) indicate possible mild autonomous cortisol secretion (MACS) and >138 nmol/L indicates MACS in the absence of clinical features of Cushing's syndrome. Adrenocorticotropin (ACTH) quantification following overnight dexamethasone suppression may be useful in the verification of MACS with ACTH measurements of 2 pmol/L (<10 ng/L) principally confirming ACTH-independent Cushing's syndrome.
Autonomous cortisol secretion has a number of comorbidities including obesity, hypertension, dyslipidaemia, type 2 diabetes and osteoporosis.9, 10 A systematic review/meta-analysis of 32 studies of 4,121 patients with adrenal incidentalomas, with/without MACS, with mean follow-up 50.2 months, showed a higher prevalence of cardiovascular events in MACS (15.5%) than non-functioning adrenal tumours (NFAT) (6.4%), although with similar mortality of 11.2%.10 Mean tumour growth was only 2 mm over 52.8 months, clinically significant tumour enlargement (≥10 mm) occurred in only 2.5% of patients, and none developed adrenal cancer. Clinically overt hormone excess was unlikely to develop (<0.1%) in patients with NFAT or MACS, only 4.3% of patients with NFAT developed MACS, and pre-existing MACS was unlikely to resolve (<0.1%). Thus, the most important consideration is to aggressively treat cardiovascular risk factors/co-morbidities in these patients.
Connshing syndrome
Adrenal synchronous aldosterone and cortisol secretion has been reported, dubbed 'Connshing syndrome’;11 this has metabolic and therapeutic implications and can influence interpretation of adrenal venous sampling results for PA.12
Catecholamine excess (phaeochromocytomas)
Presenting symptoms includes the classic triad of headaches, palpitations and profuse sweating with signs of resistant or paroxymal hypertension.13 Initial biochemical screening with plasma free or total fractionated urinary metadrenalines is recommended, although both false-positive and false-negative results may arise.14, 15 CT is suggested for initial imaging, with MRI in patients with metastatic disease or to limit radiation exposure; 123I-metaiodobenzylguanidine (MIBG) scintigraphy is useful for metastatic phaeochromocytomas. All patients should be considered for genetic testing.16
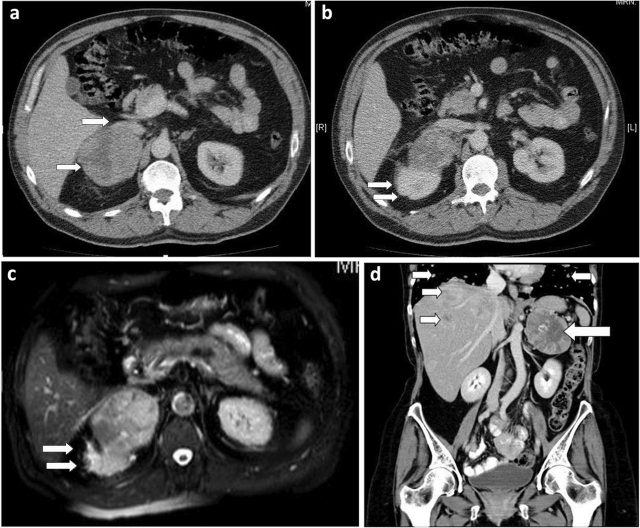
Adrenocortical carcinoma (ACC)
ACCs is a rare but aggressive malignancy presenting with hormone excess (eg virilisation, Cushing's syndrome) or with a mass (appearing as large, irregular, heterogenous tumours with peripheral contrast enhancement) (Fig 3). The median tumour size at diagnosis is 10 cm.17 Surgical resection offers the only chance of definitive treatment, adjuvant medical management with mitotane and irradiation may also be considered.
Fig 3.
Adrenocortical carcinoma. (a) A right adrenal mass 9 × 8 × 7 cm with a central hypodense area (white arrows). (b,c) The heterogeneous adrenal mass is causing inferior displacement of the right kidney. (d) Liver and lung metastases (white arrows). Images are authors’ own, reproduced with permission8
Miscellaneous adrenal pathology
Other adrenal pathologies to consider, reviewed elsewhere including adrenal haemorrhage,18 adrenal myelolipoma19 and bilateral adrenal masses.20
Conclusion
Adrenal incidentalomas are common and a thorough and systematic clinical, biochemical and radiological evaluation, often with multidisciplinary input, should be undertaken to address the functional status and potential for malignancy.
References
- 1.Kebebew E. Adrenal incidentaloma. N Eng J Med. 2021;384:1542–1551. doi: 10.1056/NEJMcp2031112. [DOI] [PubMed] [Google Scholar]
- 2.Jing Y, Hu J, Luo R, et al. Prevalence and characteristics of adrenal tumors in an unselected screening population: a cross-sectional study. Ann Intern Med. 2022;175:1383–1391. doi: 10.7326/M22-1619. [DOI] [PubMed] [Google Scholar]
- 3.Angeli A, Terzolo M. Adrenal incidentaloma – a modern disease with old complications. J Clin Endocrinol Metabolism. 2002;87:4869–4871. doi: 10.1210/jc.2002-021436. [DOI] [PubMed] [Google Scholar]
- 4.Wu X, Senanayake R, Goodchild E, et al. [11C]metomidate PET-CT versus adrenal vein sampling for diagnosing surgically curable primary aldosteronism: a prospective, within-patient trial. Nat Med. 2023;29:190–202. doi: 10.1038/s41591-022-02114-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Monticone S, D’Ascenzo F, Moretti C, et al. Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2018;6:41–50. doi: 10.1016/S2213-8587(17)30319-4. [DOI] [PubMed] [Google Scholar]
- 6.Mulatero P, Bertello C, Veglio F, Monticone S. Approach to the Patient on Antihypertensive Therapy: Screen for Primary Aldosteronism. J Clin Endocrinol Metab. 2022;107:3175–3181. doi: 10.1210/clinem/dgac460. [DOI] [PubMed] [Google Scholar]
- 7.Funder JW, Carey RM, Mantero F, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:1889–1916. doi: 10.1210/jc.2015-4061. [DOI] [PubMed] [Google Scholar]
- 8.Ouyang J, Hardy R, Brown M, Helliwell T, Gurnell M, Cuthbertson DJ. 11C-metomidate PET-CT scanning can identify aldosterone-producing adenomas after unsuccessful lateralisation with CT/MRI and adrenal venous sampling. J Hum Hypertens. 2017;31:483–484. doi: 10.1038/jhh.2017.9. [DOI] [PubMed] [Google Scholar]
- 9.Prete A, Subramanian A, Bancos I, et al. Cardiometabolic disease burden and steroid excretion in benign adrenal tumors: a cross-sectional multicenter study. Ann Intern Med. 2022;175:325–334. doi: 10.7326/M21-1737. [DOI] [PubMed] [Google Scholar]
- 10.Elhassan YS, Alahdab F, Prete A, et al. Natural history of adrenal incidentalomas with and without mild autonomous cortisol excess: a systematic review and meta-analysis. Ann Intern Med. 2019;171:107–116. doi: 10.7326/M18-3630. [DOI] [PubMed] [Google Scholar]
- 11.Arlt W, Lang K, Sitch AJ, et al. Steroid metabolome analysis reveals prevalent glucocorticoid excess in primary aldosteronism. JCI Insight. 2017;2:e93136. doi: 10.1172/jci.insight.93136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goupil R, Wolley M, Ahmed AH, Gordon RD, Stowasser M. Does concomitant autonomous adrenal cortisol overproduction have the potential to confound the interpretation of adrenal venous sampling in primary aldosteronism? Clin Endocrinol. 2015;83:456–461. doi: 10.1111/cen.12750. [DOI] [PubMed] [Google Scholar]
- 13.Neumann HPH, Young WF, Jr, Eng C. Pheochromocytoma and paraganglioma. N Engl J Med. 2019;381:552–565. doi: 10.1056/NEJMra1806651. [DOI] [PubMed] [Google Scholar]
- 14.Lenders JW, Keiser HR, Goldstein DS, et al. Plasma metanephrines in the diagnosis of pheochromocytoma. Ann Intern Med. 1995;123:101–109. doi: 10.7326/0003-4819-123-2-199507150-00004. [DOI] [PubMed] [Google Scholar]
- 15.Lenders JW, Duh QY, Eisenhofer G, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99:1915–1942. doi: 10.1210/jc.2014-1498. [DOI] [PubMed] [Google Scholar]
- 16.Muth A, Crona J, Gimm O, et al. Genetic testing and surveillance guidelines in hereditary pheochromocytoma and paraganglioma. J Intern Med. 2019;285:187–204. doi: 10.1111/joim.12869. [DOI] [PubMed] [Google Scholar]
- 17.Allolio B, Fassnacht M. Clinical review: Adrenocortical carcinoma: clinical update. J Clin Endocrinol Metab. 2006;91:2027–2037. doi: 10.1210/jc.2005-2639. [DOI] [PubMed] [Google Scholar]
- 18.Elhassan YS, Ronchi CL, Wijewickrama P, Baldeweg SE. Approach to the patient with adrenal hemorrhage. J Clin Endocrinol Metab. 2022 doi: 10.1210/clinem/dgac672. in press (doi:10.1210/clinem/dgac672). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calissendorff J, Juhlin CC, Sundin A, Bancos I, Falhammar H. Adrenal myelolipomas. Lancet Diabetes Endocrinol. 2021;9:767–775. doi: 10.1016/S2213-8587(21)00178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pasternak JD, Seib CD, Seiser N, et al. Differences between bilateral adrenal incidentalomas and unilateral lesions. JAMA Surgery. 2015;150:974–978. doi: 10.1001/jamasurg.2015.1683. [DOI] [PubMed] [Google Scholar]