Abstract
We present the results of the 2022 Census of the Federation of Royal Colleges of Physicians of Edinburgh, Glasgow and London on whether physicians undertake research and the barriers they have encountered. 40% of physicians reported that they undertook research alongside their clinical work. Multivariate analysis of the responses showed that men were 1.6 times more likely to say they undertake research than women. The main barriers to undertaking research were having enough time, organisational factors and a lack of confidence. In this opinion piece we discuss some of the challenges and how they could be addressed.
KEYWORDS: research, census, physicians
Background
The COVID-19 pandemic demonstrated resilience among physicians particularly in delivering research alongside clinical care. According to the UK government's vision published in March 2021, clinical research should be ‘at the heart of patient care across the NHS, making participation as easy as possible and ensuring all health and care staff feel empowered to support research’.1 The Royal College of Physicians (RCP) and National Institute for Health and Care Research (NIHR) subsequently produced a joint position statement in 2022 – ‘Making research everybody's business: a position statement of the Royal College of Physicians and the National Institute of Health and Care Research’.2
Who responded to the census?
The Federation of the Royal Colleges of Physicians of Edinburgh, Glasgow and London undertakes an annual census of all physicians in the UK. The survey for 2022 was sent on 24 October 2022 via email using Verint (Enterprise feedback management) software and closed on 2 January 2023. 19,044 surveys were sent and questions on participation in research were answered by 4,201 consultants currently practising in the UK. Based on what we know about the entire consultant physician demographic, these responses were broadly representative. It is likely that those also employed by academic institutions are underrepresented as compared to those employed solely by an NHS provider, as we may not have the best email address for them.
Who is undertaking ‘research’ and why?
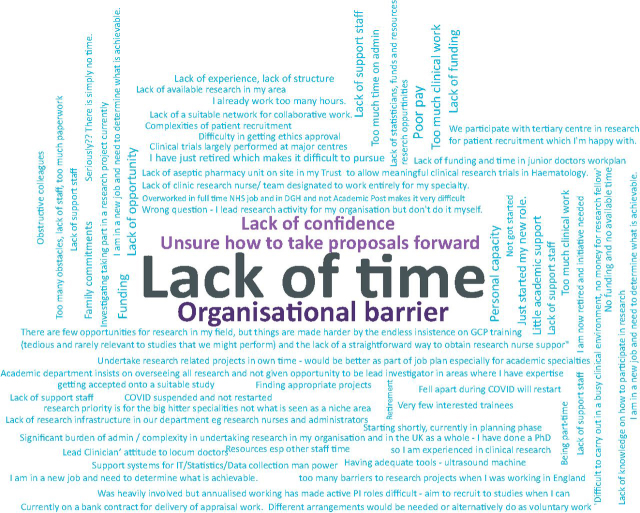
The first question on research consultants were asked was ‘Do you undertake any research activity?’ 40% replied that they did. On first glance this is good news but only half (49%) are paid for their research as part of their job plan. Of the 60% who did not undertake research, a third (38%) of these would be interested in doing so. The main barriers were having sufficient time and understanding local processes for getting started (Fig 1). If employers really want to value research to improve patient outcomes and the wellbeing of clinicians, none of these barriers are insurmountable.
Fig 1.
The main barriers reported by consultant physicians who were interested in research but currently not undertaking any research activity.
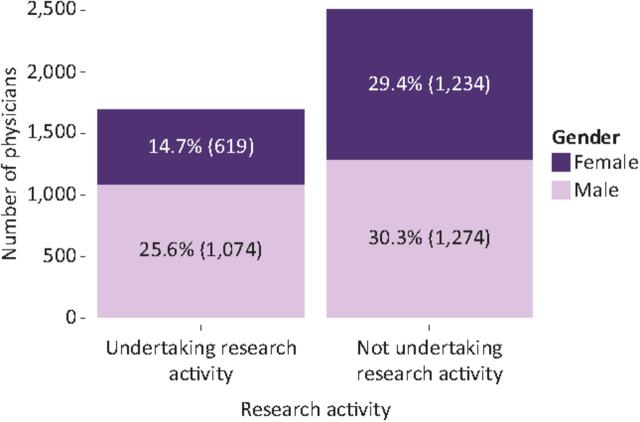
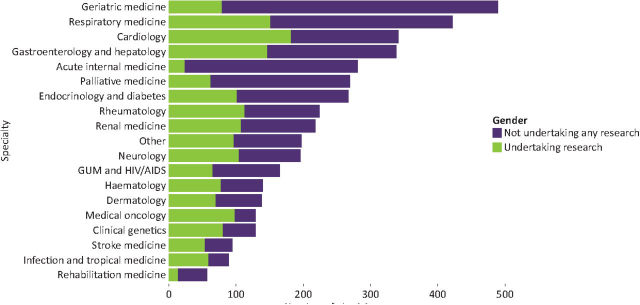
The responses were analysed in more detail through multiple logistic regression analysis using R statistical software.3 Of the 4,201 responses, male consultants were 1.6 times more likely to say they undertook research than female consultants (OR 1.60, 95% CI (1.40–1.84), p<0.001). (Fig 2, Table 1). Working full time as compared to less than full time (fewer than 10 programmed activities (PAs) per week) was also positively associated with undertaking research. Consultants working 10 PAs or more were twice as likely to say they were undertaking research activity than those working fewer PAs (OR 0.50, 95% CI (0.43–0.58), p<0.0001). Working in a specialty that participates in care of general medical inpatients and working outside of London were negatively associated with undertaking research (Fig 3, Table 1). Neither the ethnicity of consultants nor age was associated with the likelihood of undertaking research. It is noteworthy that 16% of the consultants undertaking research were 60 years or older.
Fig 2.
Consultant physicians’ research activity by their gender.
Table 1.
Estimated coefficients and odds ratios by multiple logistic regression for undertaking research
| Variable | Coefficient | Adjusted odds ratio | 95% CI | P value |
|---|---|---|---|---|
| Gender | ||||
| Female | Reference | |||
| Male | 0.47 | 1.60 | 1.40–1.84 | <0.001 |
| Region in the UK | ||||
| London | Reference | |||
| Midlands and East | −0.30 | 0.73 | 0.60–0.89 | <0.001 |
| North | −0.26 | 0.76 | 0.63–0.93 | <0.001 |
| Northern Ireland | −0.79 | 0.45 | 0.29–0.69 | <0.001 |
| Scotland – North and East | −0.61 | 0.54 | 0.34–0.83 | <0.001 |
| Scotland – West and South | −0.45 | 0.63 | 0.48–0.84 | <0.001 |
| South | −0.37 | 0.68 | 0.56–0.83 | <0.001 |
| Wales | −0.34 | 0.71 | 0.52–0.97 | <0.01 |
| Job plan | ||||
| Full time | Reference | |||
| Full time flexible | −0.20 | 0.81 | 0.50–1.30 | 0.39 |
| Less than full time | −0.69 | 0.50 | 0.43–0.58 | <0.001 |
| Specialty | ||||
| Specialties contributing most to acute or general internal medicine | Reference | |||
| Other specialties | 0.65 | 1.91 | 1.67–2.20 | <0.001 |
Fig 3.
Consultant physicians' research activity by their primary specialty.
For those that do undertake research, the main reasons were positive and altruistic, contributing to the field and improving patient care, making the individual a better doctor with a wider set of skills and bringing variety and enjoyment to the job.
What are the challenges for physicians who want to undertake research?
A few key questions need to be considered:
-
•
In reality, how can we enable all clinicians to get involved in research while there is such pressure from clinical workload?
-
•
How can providers prioritise research activity above activity that contributes to an elective recovery plan?
-
•
Is it realistic to think that a physician working fewer than 10 PAs per week should be able to undertake research within their remunerated job plan?
Some of these questions have been addressed within the RCP and NIHR position statement with key recommendation to stakeholders–time will determine if these have been enacted.2
Gender gap
In this survey of consultant physicians, men were 1.6 times more likely to say they undertake research than women. This reflected the findings of the January 2020 ‘Research for all’ survey of RCP London members,4 where of the 1,137 responses 66% of men were involved in research as compared to 55% of women. The BMJ recently reviewed their publications in nine specialist and two general medical journals and reported that the gender gap had worsened from 38.9% from women pre-pandemic to 22.9% post-pandemic.5
Addressing this gender gap in research activity is beyond the scope of a survey of physicians but acknowledging that it is an issue is the start of the conversation.
Regional variation in research activity
There was a wide variation in the number of physicians undertaking research across the UK – working outside of London was negatively associated with undertaking research (Fig 4). We know that with the multiple changes within the current government, the priority of levelling up, especially in the North, has taken a step back, and there is even concern that the whole agenda may be abandoned.6 We thus have to wait to see what transpires following the next general election.
Fig 4.
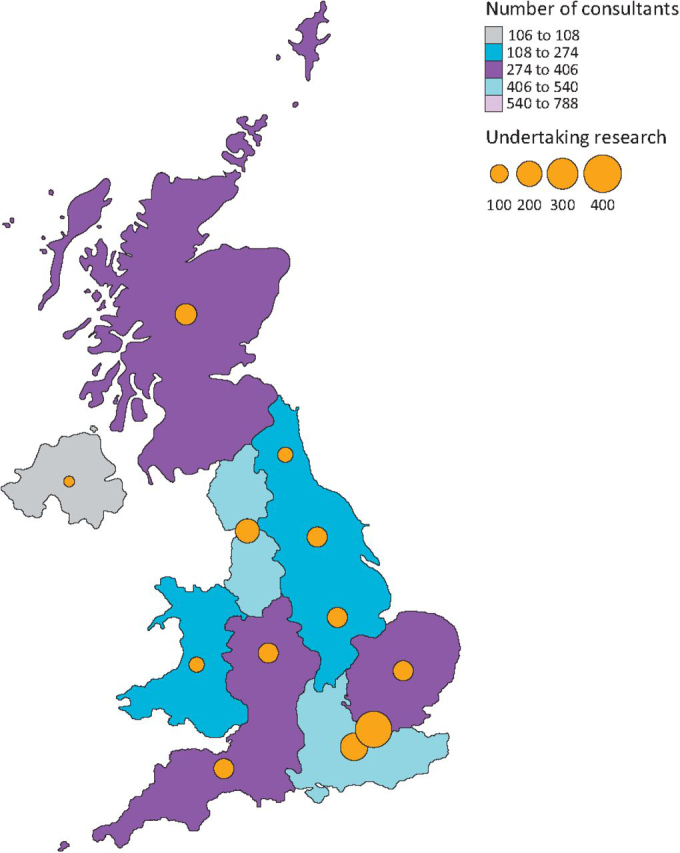
A geographical plot demonstrating the distribution of consultant physicians across the UK. The bubbles represent the number of consultant physicians undertake research.
Survey limitations
There are limitations to this survey; it may not be representative of the whole cohort of physicians in the UK and there will be unidentifiable confounders that we cannot adjust for. It does however act as a benchmark against which the impact of initiatives such as within the position statement from the RCP and NIHR can be measured.
What can be done?
Job planning for research activity and describing it as direct clinical care to reflect the importance a provider places on it would be a good start. After all, the evidence suggests that organisations that undertake research provide better care for their patients,7 supporting the premise that delivering research should be considered part of clinical activity. There are opportunities for seed funding by regional comprehensive networks that could be explored to enable protected time for those interested in undertaking research. The survey has also demonstrated the variation in consultants that undertake research according to specialty – in particular, how much care of general medical patients they do and where in the UK they work. Enabling trainees to engage with research, promoting initiatives such as flexible portfolio training, and championing role models among research-active consultants (particularly those in specialties with lower rates of research activity and outside of London) will help.
To keep consultants working in the NHS we need to make them feel truly valued and that goes beyond a pay-slip. In this survey 88% of consultants found their work in their specialty enjoyable often or all the time as compared to 83% of those that did not undertake research. Increasing engagement in research brings more ‘value’ to the role of a consultant physician, both personally and more widely. This value is fundamental to retention in the NHS workforce of these senior clinicians.
References
- 1.Department of Health and Social Care . DHSC; 2021. Saving and improving lives: the future of UK clinical research delivery.www.gov.uk/government/publications/the-future-of-uk-clinical-research-delivery/saving-and-improving-lives-the-future-of-uk-clinical-research-delivery [Accessed 17 June 2023] [Google Scholar]
- 2.Arasaradnam R, Clarke S, Van't Hoff W, Chappell L. Making research everybody's business: a position statement of the Royal College of Physicians and the National Institute of Health and Care Research. Clin Med. 2023;23:102–105. doi: 10.7861/clinmed.2022-0482. [DOI] [PubMed] [Google Scholar]
- 3.3 R: The R Project for Statistical Computing. https://www.r-project.org/ [Accessed 8 May, 2023].
- 4.Royal College of Physicians . RCP; 2020. Research for all: Developing, delivering and driving better research.www.rcplondon.ac.uk/projects/outputs/research-all-developing-delivering-and-driving-better-research [Accessed 17 June 2023] [Google Scholar]
- 5.Clark J. How pandemic publishing struck a blow to the visibility of women's expertise. BMJ. 2023;381:p788. doi: 10.1136/bmj.p788. [DOI] [PubMed] [Google Scholar]
- 6.Forbes C, Liddle J, Shutt J. Northumbria University; 2022. Levelling-up in the north east region: What has been achieved in the last three years? An Assessment.https://northumbria-cdn.azureedge.net/about-us/news-events/news/is-levelling-up-working-for-the-north-east/ [Accessed 17 June 2023]. [Google Scholar]
- 7.Downing A, Morris EJA, Corrigan N, et al. High hospital research participation and improved colorectal cancer survival outcomes: a population-based study. Gut. 2017;66:89–96. doi: 10.1136/gutjnl-2015-311308. [DOI] [PMC free article] [PubMed] [Google Scholar]