Abstract
Objective:
To examine parent and family outcomes of a randomized controlled trial (RCT) comparing Teen Online Problem-Solving with Family (TOPS-F), Teen Online Problem-Solving-Teen Only (TOPS-TO), or access to Internet resources alone (Internet resource comparison [IRC]).
Design:
Three-arm RCT.
Setting:
Four children’s hospitals and 1 general medical center in Ohio and Colorado.
Participants:
Children and adolescents (N = 152), 11–18 years old, hospitalized for complicated mild to severe traumatic brain injury in the previous 18 months.
Interventions:
Intervention groups: TOPS-F, TOPS-TO, and IRC.
Main Outcome Measure:
Parental depression (CES-D), parental psychological distress (SCL-90-GSI), family functioning (FAD-GF), cohesiveness (PARQ), and conflict (IBQ) were assessed pre- and post-treatment. Treatment effects and the moderating effect of the number of parents in the home (single vs 2-parent families).
Results:
Number of parents moderated treatment effects with effects ranging from trending to statistically significant for depression, family functioning, cohesion, and conflict. Among single parents, TOPS-TO reported better family functioning than TOPS-F and greater cohesion and less conflict than IRC. Among 2-parent families, TOPS-F reported less depression than IRC and less depression and greater cohesion than TOPS-TO. The effect of family composition was also noted within TOPS-TO and TOPS-F. In TOPS-F, 2-parent families reported less depression than single-parent families. In TOPS-TO single parents reported greater cohesion and better family functioning than 2-parent families.
Conclusions:
Findings support the TOPS intervention improves family outcomes, with differential effects noted for single vs 2-parent households. The TOPS-TO format appeared more beneficial for single-parent households, while TOPS-F was more beneficial for 2-parent households, highlighting the importance of considering family composition when determining the best treatment modality.
Keywords: Adolescent, Brain injuries, traumatic, Family, Problem solving, Rehabilitation, Single-parent family
Traumatic brain injury (TBI) is the leading cause of death and disability in childhood, with adolescence representing a period of heightened risk.1 Children and adolescents who sustain a TBI are at risk of a range of short- and long-term psychosocial challenges. These include internalizing problems, externalizing behavior problems, and experiencing changes in personality.2–4 Internalizing and externalizing behavior problems that emerge after a TBI may abate over time, though for some youth, they may persist or intensify.2,5–7
Effects of pediatric TBI often extend beyond the injured child or adolescent and affect family functioning. Parents of children or adolescents with TBI report poorer psychological functioning including greater stress and anxiety8,9 and feelings of guilt and grief.10 Factors that contribute to poorer parent psychological functioning following pediatric TBI include chronic family stress and fewer resources, poor coping strategies, and increased child or adolescent mood and behavioral problems.11–14
In pediatric TBI samples, parent and family functioning affects adolescent psychological functioning and behavioral recovery following injury.15 For example, poorer parental psychological functioning within the first 6 months post TBI predicted increased adolescent behavior problems, while greater parental communication of warmth was associated with fewer behavior problems.16 Despite elevated risk of TBI in adolescence, significant burden of injury on family functioning, and the influence of parent and family functioning on optimal recovery, few interventions target the unique and evolving needs of adolescents and their families post TBI.17 Given the importance of parental mental health and family functioning to recovery, parenting or family-centered interventions may be an effective strategy to improve family functioning, parental mental health, and child outcomes after TBI. Further, families managing sequelae of TBI may struggle to access traditional in-office psychological interventions. Lack of transportation or living far from centers of care may also affect access to services.18
To improve access to care and promote functioning of adolescents and families affected by pediatric TBI, Wade et al developed a web-based family problem-solving intervention targeting challenges and needs of this population. Although problem solving therapy was originally developed as a cognitive behavioral treatment to promote more effective coping with life stresses and reduce distress and/or depressive symptoms,19–22 it may be particularly beneficial for children with TBI and their families because it provides the injured individual with an executive function heuristic for addressing postinjury challenges. The intervention teaches the adolescent and their family cognitive reframing, problem solving, communication skills, and behavior management. It helps families define goals and involves real-life exercises and continual practice of learned skills to systematically resolve challenges that are causing distress. Problem-solving interventions may be particularly suited to the needs of families affected by adolescent TBI because it teaches skills that are generalizable beyond the intervention setting and can address challenges that may emerge over time. Findings from a randomized controlled trial (RCT) of the family-based Teen Online Problem-Solving (TOPS) intervention indicated positive effects of this intervention.23,24 However, findings to date suggest that some adolescents and families may be more poised to benefit. For example, greater improvements in parental depression were seen in families from lower income households,23 and greater gains in adolescent executive functioning were found in older adolescents.25–27
Additionally, evidence suggests that among certain subsets of families, participating in a family-based intervention soon after injury may add to burden, and parents may not be responsive to treatment. For example, Raj et al28 found that parents from single-parent homes were more likely to drop out of a family-based problem-solving intervention delivered within 6 months of adolescent TBI. This is consistent with findings among other clinical populations that suggest single parents experience greater barriers to participation and are more likely to drop out of treatment.29–31 However, single parents who participate generally report improved functioning,32 maintaining improvements over time.33
In the present study, the TOPS intervention was reconfigured to be delivered as a teen-only intervention (TOPS-TO) or a family-based format (TOPS-F). We were particularly interested in examining whether the number of parents (ie, single- vs dual-parent homes) would moderate intervention effects. In general, we expected that parents receiving the family-based intervention (TOPS-F) would report greater psychological gains than those in the teen-only intervention (TOPS-TO) or the active control condition (ie, Internet resource comparison [IRC]). Further, based on findings from our pilot study and previous literature highlighting limited effectiveness among single-parent families, we hypothesized that parents from 2-parent homes would experience the greatest treatment gains in both the TOPS-TO and TOPS-F conditions. The family outcomes assessed in this paper are secondary outcomes of this RCT. The trial was powered to detect child behavioral outcomes, and these primary outcomes are published elsewhere.34
Methods
The study used a 3-armed (TOPS-F, TOPS-TO, IRC), multisite RCT. Participants were recruited from 4 children’s hospitals and 1 general medical center in Ohio and Colorado. Recruitment occurred between March 2010 and August 2014, and follow-up assessments were completed between December 2010 and July 2015. The study was approved by institutional review boards of all participating institutions and was registered with clinicaltrials.gov.35
Participants
Inpatient admissions and trauma registries at participating institutions were screened for participants aged 11–18 years. Inclusion criteria included (1) hospitalization of at least 1 night because of TBI in the previous 18 months, (2) history of moderate to severe TBI as characterized by a lowest Glasgow Coma Scale score of <13 or evidence of brain injury visible on clinical imaging, (3) completion of inpatient rehabilitation, (4) residence with parent or primary parent, and (5) English as the main language in the home. Exclusion criteria included (1) nonblunt head trauma, (2) history of child abuse, (3) adolescent psychiatric hospitalization prior to their TBI, or (4) parental hospitalization for a psychiatric disorder in the previous 5 years. In addition, adolescents who had not recovered sufficiently to verbally participate were excluded. A total of 152 adolescents (11–18 years; mean ± SD, 14.87±2.04 years; 70% male) and their primary parents completed the baseline assessment. Enrollment, group assignment, and attrition are detailed in the Consolidated Standards of Reporting Trials diagram (fig 1).
Fig 1.
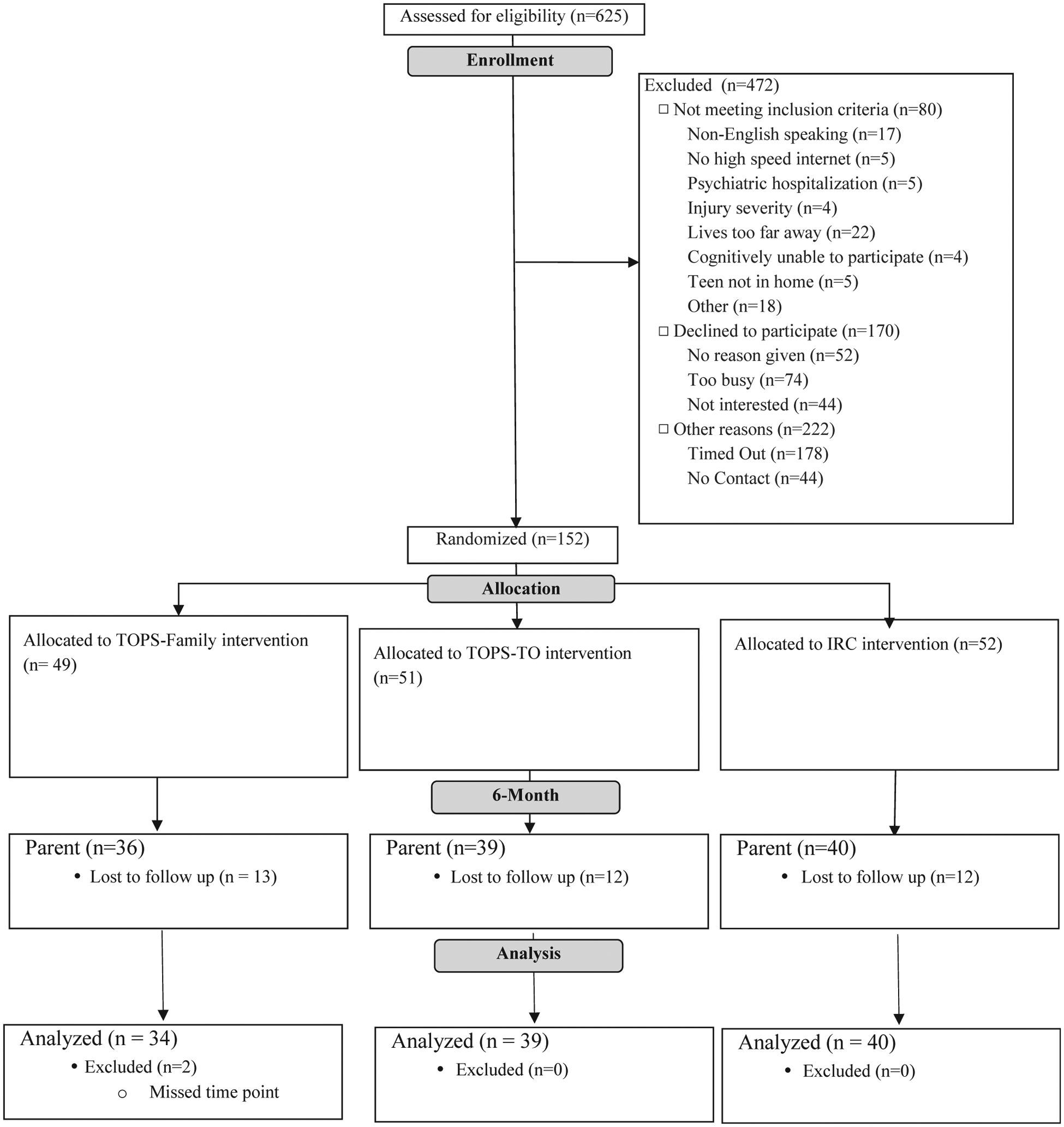
Consolidated Standards of Reporting Trials (CONSORT) flow diagram.
Procedures
Baseline visits were conducted in the families’ homes within 18 months of injury (mean ± SD, 5.7±4.0 months post injury) to complete baseline measures with adolescents and their primary parent. Families were randomly assigned to 1 of the 3 conditions: TOPS-F (n=49), TOPS-TO (n=51), or IRC (n=52). Group assignment was stratified by adolescent sex and race/ethnicity and were generated prior to study initiation using a computer program developed by biostatisticians at the primary site. While we were unable to conceal group assignment from the families or research staff, parent and teen report served as the primary outcome measure, minimizing potential researcher bias. Postintervention data were collected approximately 6 months after baseline. Families in all 3 groups were provided with Internet service for the duration of the study, and families without a computer were provided one, ensuring that families had equal access to web-based resources.
Intervention conditions
TOPS-Family (TOPS-F)
TOPS-F was a web-based, family-centered problem-solving intervention designed to support adolescent and family outcomes following pediatric TBI. The intervention addressed common challenges following TBI by providing psychoeducation as well as teaching adolescents and their parents a 5-step problem solving process (Aim, Brainstorm, Choose, Do, and Evaluate) that was generalizable to concerns beyond those addressed during the study. This problem-solving framework was grounded in Nezu and D’Zurilla’s19 problem-solving therapy model. The intervention consisted of 10 core sessions addressing topics such as staying positive, organization, managing anger, coping with stress, and improving self-care. In addition to core content, families selected up to 4 of 8 supplemental sessions (eg, marital communication, managing guilt and/or grief, and pain management). The intervention website included information and links to resources for TBI (eg, Brain Injury Association, Brain Injury Partners, and the Center on Brain Injury Research and Training).
The first session took place in the family’s home so that the clinician could orient the family to the program and manage technological aspects of the intervention (eg, accessing the website and setting up a Skype account). All subsequent sessions were conducted via Skype and consisted of 2 parts. First, families accessed the website and reviewed the self-guided web content (eg, psychoeducation, videos, interactive activities). Families then met with their clinician via Skype to discuss session content and practice problem-solving. Families completed 1 session each week or every other week.
Therapists were advanced clinical psychology graduate students or licensed clinical psychologists. All therapists were trained to deliver the intervention and participated in weekly or biweekly supervision with the developer of the intervention (a licensed clinical psychologist). Supervision served to enhance fidelity and adherence. In addition, all therapists referred to a detailed manual with step-by-step guidance to facilitate each session and completed a session checklist at the end of each session (fidelity on these checklists were 90% and higher). The intervention was designed to be completed within 6 months. Further details about the intervention, including a table of sessions, are presented by Wade et al.35
TOPS-Teen Only (TOPS-TO)
Content for TOPS-TO was adapted from the TOPS-F intervention based on focus groups with adolescents with TBI and their parents. These adaptations and refinements included shortening sessions (or dividing content into 2 sessions), editing content to make it more applicable for teen-only delivery, and increasing interactive activities. Although primarily an adolescent-based intervention, parents were asked to participate in Session 1 (introduction session held in the family home), Session 2 (staying positive), and Session 10 (planning for the future). The general structure and delivery of TOPS-TO was similar to TOPS-F described above. See research by Wade et al35 for further details about the intervention.
Internet Resource Comparison (IRC)
Families in the IRC condition were provided access to a web page with external links to the same online resources that were provided to families in TOPS-F and TOPS-TO. Adolescents and families were encouraged to spend 1 hour each week using the Internet to access information regarding pediatric TBI. The IRC families did not have access to the intervention content or therapist-guided sessions.
Measures
All measures were collected at both baseline and follow-up visits.
Background and demographics
Primary caregivers were interviewed to obtain demographic information on factors such as family income, relationship status, and level of education. This information was collected at baseline and follow-up visits; however, demographic information collected at the baseline visit was used to characterize the sample and in analyses. Data were collected from secondary caregivers when possible; however, because of the limited number of secondary caregivers who responded (n=42), their varied relationship to the participant, and their inconsistent participation in the intervention, only the primary caregiver reports were used. The number of parents in the home was determined by parental report of individuals living in the household. A family was characterized as being a 2-parent household if both biological parents lived in the home or a parent’s significant other resided in the home (regardless of whether they were legally married). While the sample does not include any same-sex couples, they were not excluded from the study.
Parental functioning
Global psychological distress
The Symptom Checklist-90R: Global Severity Index (SCL-90R:GSI)36 was used to measure global psychological distress among parents. The GSI scores are reported as t values, with higher scores indicating greater levels of distress.
Depression
The Center for Epidemiological Studies Depression Scale (CES-D37) was used to measure parent depression. Scores on the CES-D range from 0–60, with higher scores reflective of greater depressive symptomatology.37
Family functioning
Global family functioning
The 12-item General Functioning scale from the McMaster Family Assessment Device (FAD-GF)38 was used to assess family functioning. Scores on the FAD-GF range from 1–4, with higher scores indicating poorer family functioning.
Family cohesion
The Cohesion scale of the Parent Adolescent Relationship Questionnaire (PAR-Q)39 was used to assess family cohesion. The Cohesion scale consists of 15 true/false items. Scores range from 0–15, with higher scores suggesting greater family cohesion.
Parent-adolescent conflict
The Interaction Behavior Questionnaire-Short Form (IBQ)40 was used to measure parent-adolescent conflict. The IBQ is comprised of 20 true/false questions. Scores range from 0–20, with higher scores indicating greater parent-adolescent conflict.
Analyses
Separate general linear models were used to assess the relative effectiveness of treatment groups (TOPS-F, TOPS-TO, IRC) by examining post-treatment outcomes while controlling for baseline scores of the outcome variable being examined in the model. To examine the moderating effect of the number of parents, the interaction of treatment group and number of parents (single- vs 2-parent household) were included in the models. We controlled for relevant demographic variables including injury severity, participant age, and socioeconomic status (as measured by maternal education). Separate models were run for each of the outcomes of interest, which included parental distress (SCL-90:GSI), parental depression (CES-D), family functioning (FAD-GF), parent-reported cohesion (PARQ), and parent-reported conflict (IBQ). For example, the models examining the effectiveness of treatment group and moderating effect of number of parents on parental distress included (1) post-treatment SCL-90 scores as the dependent variable; (2) treatment group, number of parents in the home, and their interaction as main effects and moderation effect (interaction); and (3) baseline SCL-90 scores, injury severity, participant age, and socioeconomic status as control variables. All statistical analyses were conducted using SAS version 9.1.3.a
Results
Group differences at baseline
Families in the 3 treatment conditions were well matched at baseline, with no significant differences in demographic (eg, age at injury and baseline, household income, parental education) or outcome variables (table 1). Rates of attrition were equivalent across groups. With the exception of child race (χ2(1)=6.12; P=.01), no demographic or parent and/or family functioning differences were observed between those who completed the follow-up assessment and those who dropped out. White participants were more likely to complete follow-up (79%) than were nonwhite participants (57%).
Table 1.
Demographic information and baseline scores for each intervention group
| Characteristic | TOPS-Family (n=49) | TOPS-Teen Only (n = 51) | IRC (n = 52) |
|---|---|---|---|
| Child age at baseline (y) | 14.72±2.08 | 14.77±1.95 | 15.11±2.11 |
| Time since injury at baseline (y) | 0.44±0.33 | 0.49±0.36 | 0.51±0.32 |
| Child sex (% male) | 71.4 | 68.6 | 71.2 |
| Child race (% white) | 79.6 | 82.4 | 78.8 |
| No. of parents in the home (% of families with 2 caregivers in the home) | 67.3 | 72.5 | 69.2 |
| Primary caregiver education (%) | |||
| No college | 36.7 | 33.4 | 51.9 |
| At least 2 years of college | 34.7 | 35.3 | 28.8 |
| Bachelor’s or graduate degree | 28.6 | 31.3 | 19.3 |
| Census tract annual income ($) | 67,801±28,690 | 71,148±29,363 | 64,078±26,413 |
| Caregiver/family functioning | |||
| CES-D | 13.94±9.79 | 13.02±9.56 | 10.57±8.18 |
| SCL-90-R: GSI | 53.27±12.22 | 53.94±12.05 | 51.82±10.40 |
| FAD | 1.91±.44 | 1.87±.42 | 1.86±.46 |
| IBQ: Caregiver report | 4.75±5.40 | 4.67±5.29 | 4.71±5.42 |
| PARQ: Caregiver report | 11.43±3.54 | 12.04±3.23 | 11.65±3.52 |
Abbreviation: CESD, Center for Epidemiological Studies Depression Scale.
Parental functioning
Global psychological distress (SCL-90R:GSI)
There was no effect of treatment group, number of parents, or their interaction on parent-reported distress at the 6-month follow-up.
Parental depression (CES-D)
The number of parents moderated the effect of treatment group at the 6-month follow-up (F[2,96]=4.44; P=.01). As depicted in figure 2, parents from 2-parent households in TOPS-F reported fewer depressive symptoms at follow-up than those in TOPS-TO (P=.03; d=.44) and IRC (P=.01; d=.56) and single parents in TOPS-F (P=.03; d=.45). There were no treatment group differences in depression among single parents.
Fig 2.
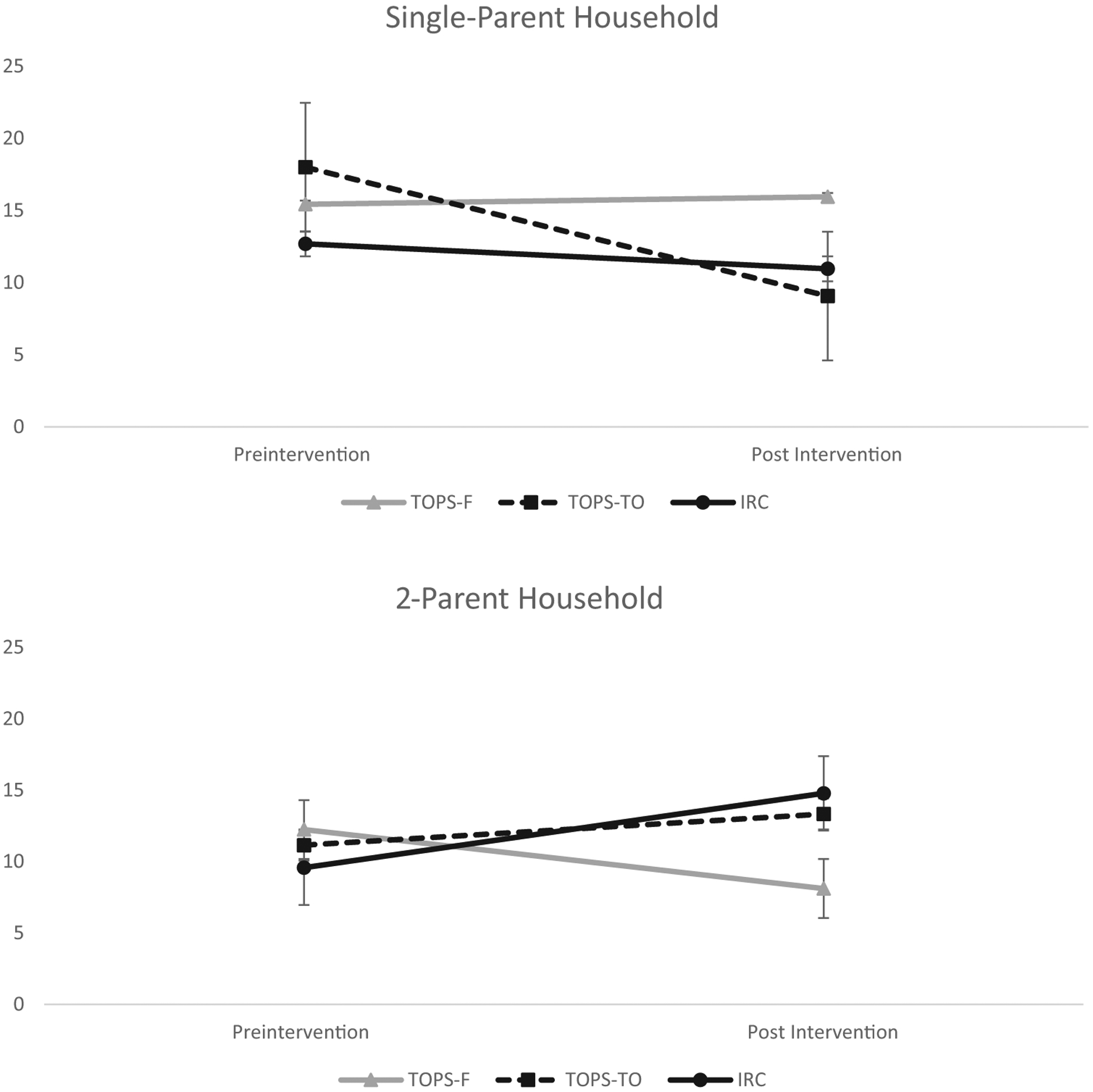
Parent-reported depression on Center for Epidemiologic Studies Depression Scale (CESD) at follow-up by treatment group among single-parent household vs 2-parent household.
Family functioning
Global family functioning (FAD-GF)
The moderating effect of the number of parents was not significant (F[2,97]=2.59; P=.08). As depicted in figure 3, at follow-up single parents in the TOPS-TO intervention group reported marginally less family dysfunction than parents from 2-parent households in TOPS-TO (P=.07; d=.37) and significantly less than single parents in TOPS-F (P=.045; d=.41). There were no treatment group differences noted in 2-parent households.
Fig 3.
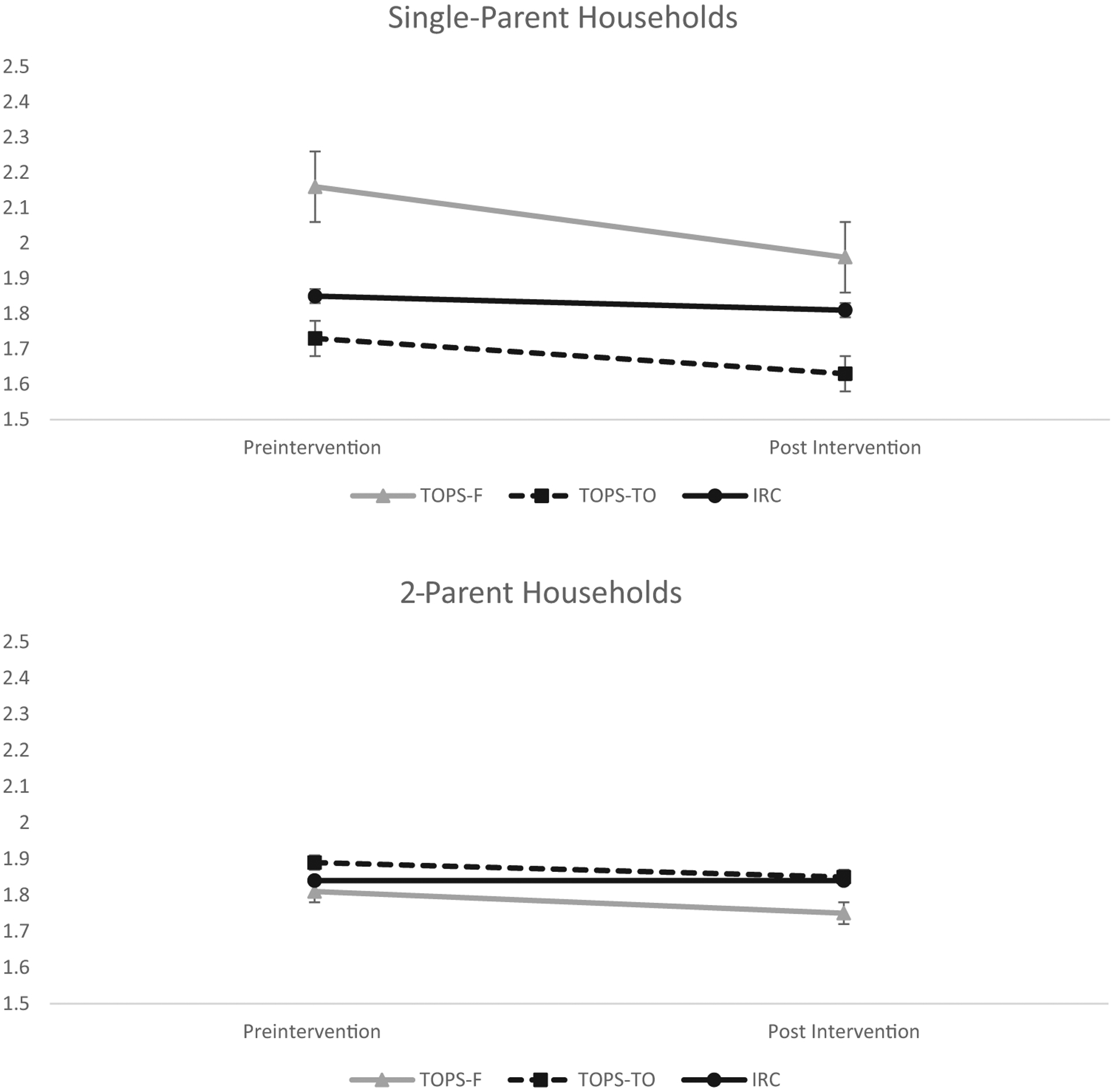
Parent-reported family functioning on FAD-GF at follow-up by treatment group among single-parent households vs 2-parent households.
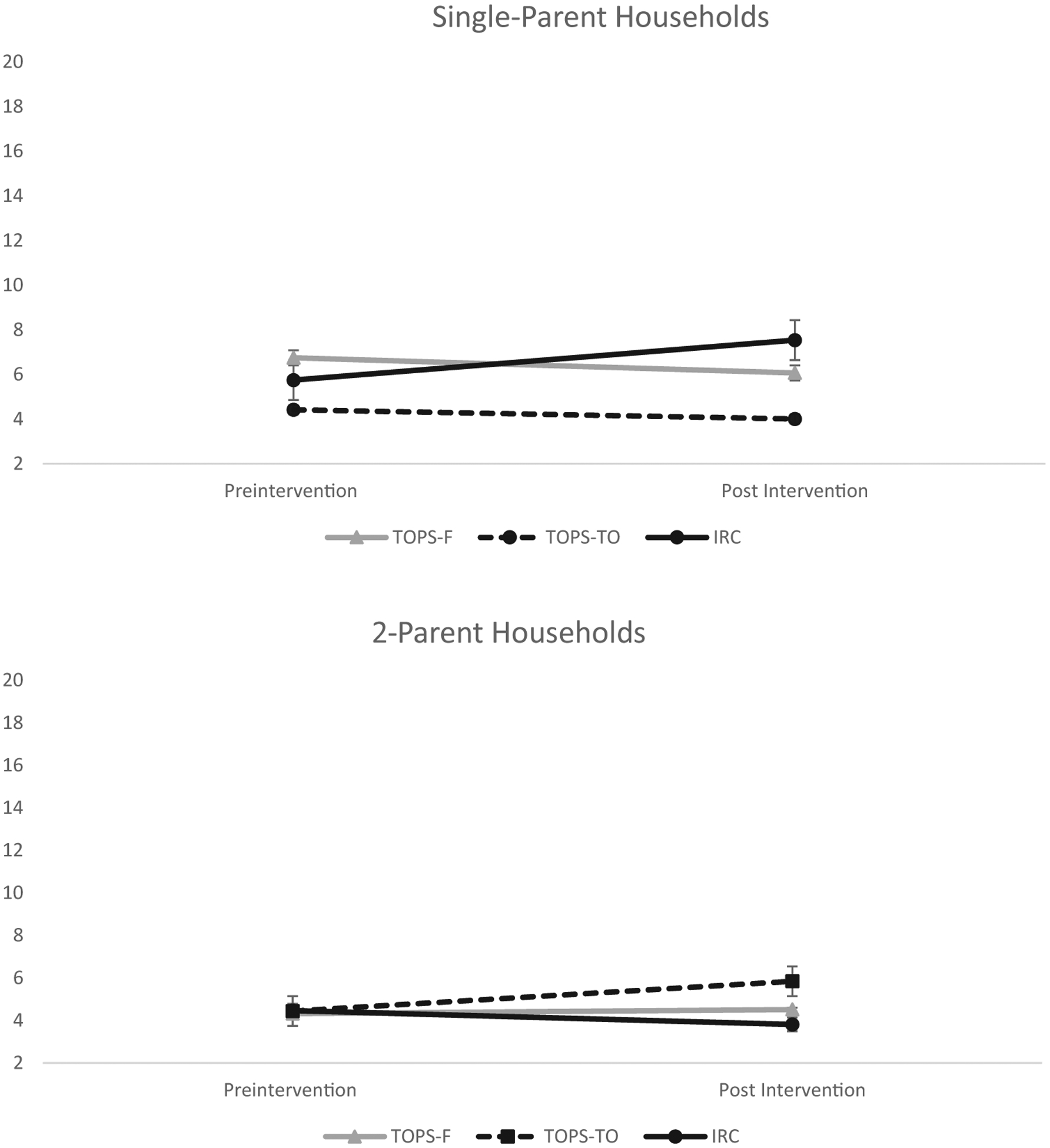
Family cohesion (PAR-Q)
The moderating effect of the number of parents in the home on family cohesion was not significant (F[2,98]=2.85; P=.06; fig 4). At follow-up, single parents in TOPS-TO reported marginally greater family cohesion than parents from 2-parent households also in TOPS-TO (P=.05; d=.39). Additionally, among single parents, those in TOPS-TO reported greater family cohesion than those in IRC (P=.02; d=.47), while single parents in TOPS-F reported similar levels of cohesion as single parents in the IRC group. In contrast, among parents from 2-parent households, those in the TOPS-F intervention reported greater cohesion that those in TOPS-TO (P=.04; d=.43).
Fig 4.
Parent-reported family cohesion on PAR-Q at follow-up by treatment group among single-parent households vs 2-parent households.
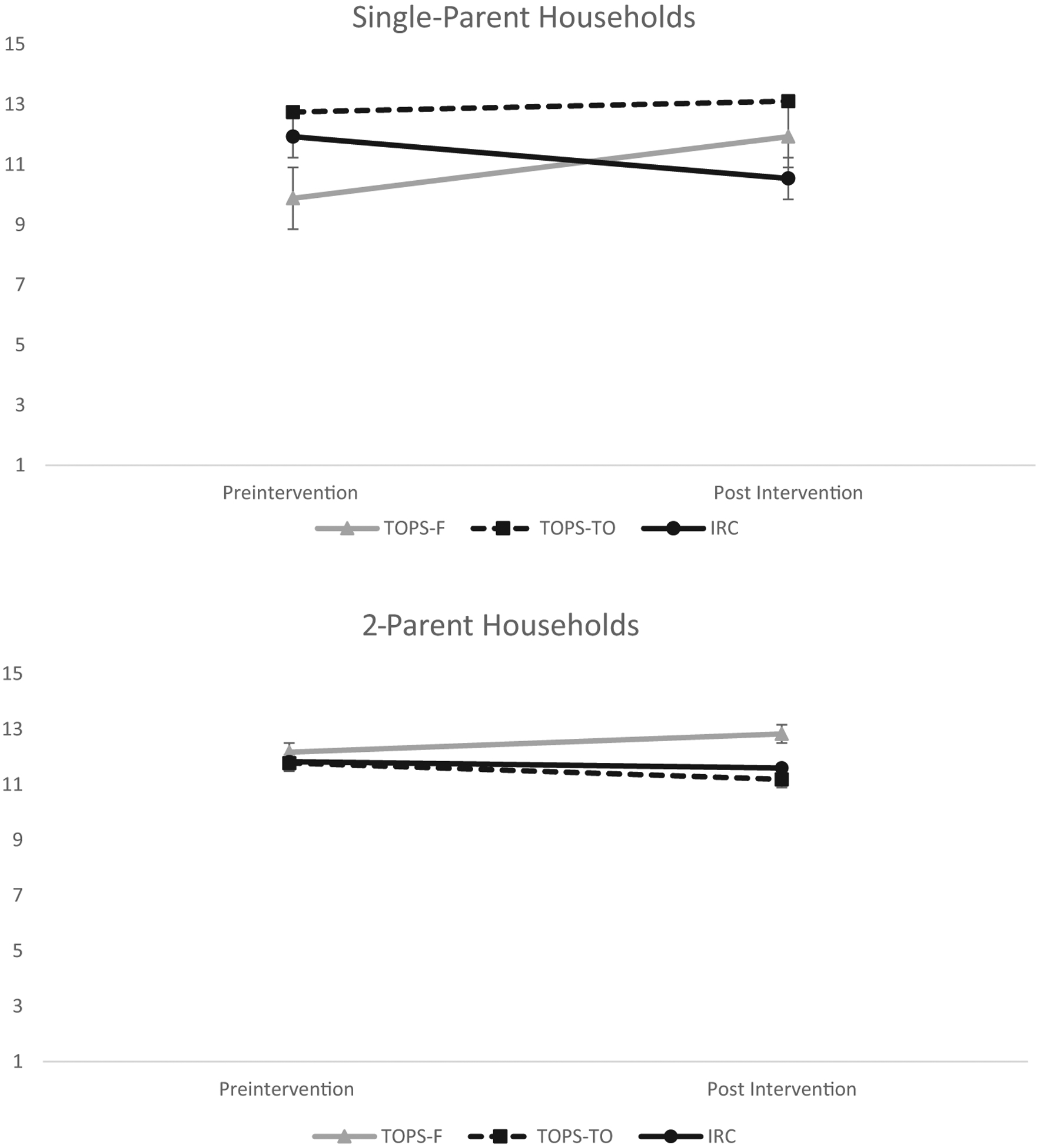
Parent-adolescent conflict (IBQ)
Number of parents moderated the effect of treatment group on parent-adolescent conflict (F(2,99)=3.33; P=.04; fig 5). At follow-up, single parents in IRC reported greater conflict than parents from 2-parent households in IRC (P=.01; d=.53). Finally, single parents in TOPS-TO reported marginally less conflict than single parents in IRC (P=.05; d=.40); however, no treatment group differences were noted in 2-parent households.
Fig 5.
Parent-reported conflict on IBQ at follow-up by treatment group among single-parent households vs 2-parent households.
Discussion
We examined the effects of the number of parents (ie, single- vs dual-parent homes) on parent and family outcomes within a 3-armed RCT of an online problem-solving intervention for adolescents with a history of TBI. Consistent with expectations, the efficacy of the family and teen-only treatments was moderated by the number of parents living in the home, with little evidence of main effects of problem-solving therapy over access to Internet resources on parent distress, depression, or family functioning. Parents from 2-parent households who received the family-based intervention (TOPS-F) experienced the greatest improvement, reporting less depression then those from 2-parent households in the teen-only intervention and control condition as well as single parents in the family-based intervention. Additionally, 2-parent families in the family-based intervention reported greater family cohesion post intervention than those who received the teen-only intervention. In contrast, the teen-only format (TOPS-TO) was more efficacious in single-parent households. Following the intervention, single parents in TOPS-TO reported marginally greater family cohesion than those in the IRC condition and significantly greater cohesion than 2-parent families in the teen-only intervention. Further, single parents in the teen-only intervention reported less family dysfunction than single parents in the family-based intervention and 2-parent households in the teen-only intervention. Finally, single parents in the teen-only group reported marginally less conflict than those in the control group. These findings support the notion that adolescents from single-parent households in the teen-only condition learned and implemented new skills without adding to parent burden. This highlights the importance of considering the number of parents in the home and resources when determining treatment modality for adolescents with TBI.
A number of factors may explain the effect of the number of parents in the home on treatment outcomes. Single parents are more likely be burdened with daily stressors and stressful life events while receiving lower levels of social, emotional, and parental support,41,42 and TBI may exacerbate these burdens. While single parents completed a similar number of sessions as parents in 2-parent households across treatment groups, single parents shouldering multiple responsibilities may have struggled to engage in the intervention and practice newly learned skills. Single parents reported comparable levels of psychological distress to those of parents from 2-parent households at the baseline assessment; however, there was a trend for single parents to report greater levels of interpersonal stress than 2-parent families at this visit (P=.06). As a consequence, the intervention may have constituted an additional burden on them. In a manuscript examining adolescent outcomes of this RCT,34 we found that at lower levels of parent stress, adolescents in the TOPS-F group reported significantly less executive dysfunction than those in the TOPS-TO group at follow-up. However, at high levels of parental stress, the pattern was reversed with participants in the TOPS-TO group reporting less executive dysfunction than those in the TOPS-F group at follow-up. Together, these findings suggest that levels of parental stress may indicate the format of intervention best suited to a given family. The teen-only format was more efficacious in improving family conflict in single-parent households, indicating that aspects of the intervention were helpful in single-parent homes. Parental scaffolding of the adolescent’s problem-solving may serve as an important support in 2-parent families, whereas it may create additional conflict in already stressed, single-parent households. In the latter situation, the adolescent’s independent mastery of self-regulation and problem-solving skills may serve to reduce conflict and boost cohesion.
More than 25% of children and/or adolescents <18 years live in single-parent homes,43 yet there is limited research addressing the effects of household composition on treatment acceptability and outcomes in pediatric populations. Findings from this study underscore the need to further examine the effect of the number of parents in the home on response to intervention post TBI and to provide families with the support that is most likely to benefit them. For example, in single-parent homes with high levels of reported stressors, addressing sources of stress and developing parental coping strategies may be beneficial prior to engaging in a problem-solving intervention. This may be especially true in cases where the adolescent needs a high level of support and scaffolding from a parent to access and apply strategies from treatment.
Study limitations
Findings from this study should be considered in the context of some limitations. First, families were recruited for the study regardless of parent and family functioning, with a majority of parents and families reporting functioning within normal limits. Intervention effects may have been larger if the study had specifically recruited parents and families experiencing a higher level of problems post TBI. Similarly, as with all clinical trials, these findings relate to children and families who agree to participate in an intervention trial, who may differ from families who declined participation. As such, generalizability of the findings may be somewhat limited. In addition, the intervention was designed to address and support adolescent behavioral and executive functioning, rather than directly improve parent and family functioning. While the effects of the TOPS-F and TOPS-TO on parent and family outcomes are promising, additional content directly addressing parents or separate treatment for distressed parents may be useful complements to the intervention. Along these lines, we did not assess parental problem-solving skills and thus are unable to examine whether improvements in problem-solving skills mediated reductions in parental distress, as was demonstrated in the original trial of TOPS.23 Further, we did not measure whether or how frequently families in the IRC group accessed the Internet resources provided to them; therefore, we are unable to determine whether families were in fact accessing new online resources through the program. In addition, only data collected from the primary caregiver, who were nearly all mothers, were used in the current study; therefore, fathers’ perspectives did not inform the current findings. Next, although there were no statistically significant differences between treatment groups at baseline, the TOPS-TO group did appear to have better functioning than the other groups, which may have limited our ability to detect improvements in this group. Finally, the sample was relatively heterogeneous, which may have limited the ability to detect more subtle treatment differences, and white participants were more likely to complete the follow-up assessment than nonwhite participants, further limiting potential generalizability of findings.
Conclusions
Despite these limitations, findings from this study are encouraging and suggest that different configurations of treatment delivery resulted in improvements in parental and family functioning. Adapting the family-based format to reduce family involvement and burden did not have a negative effect on parental and family outcomes and highlights the importance of considering the family environment and the number of parents in the home when examining treatment outcomes in this pediatric population.
Acknowledgments
Supported by the National Institute on Disability, Independent Living, and Rehabilitation Research, formerly known as the National Institute on Disability and Rehabilitation Research (grant no. H133B090010). Megan Narad was supported by NIH grant no. 1F32HD088011 from the National Institute on Child Health and Human Development. This material does not necessarily represent the policy of these agencies, nor is the material necessarily endorsed by the federal government.
List of abbreviations:
- CES-D
Center for Epidemiological Studies-Depression Scale
- FAD-GF
Family Assessment Device-General Functioning
- IBQ
interaction behavior questionnaire
- IRC
Internet resource comparison
- PARQ
Parent Adolescent Relationship Questionnaire
- RCT
randomized controlled trial
- SCL-90-GSI
Symptom Checklist-90R-Global Severity Index
- TBI
traumatic brain injury
- TOPS-F
Teen Online Problem Solving-Family
- TOPS-TO
Teen Online Problem Solving-Teen Only
Footnotes
Supplier
a. SAS, version 9.1.3; SAS Institute, Inc.
Clinical Trial Registration No.: NCT01042899.
Disclosures: none.
References
- 1.Faul M, Xu L, Wald M, Coronado V. Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Atlanta (GA): Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. Available at: http://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf. AccessedSeptember 9, 2013. [Google Scholar]
- 2.Bloom DR, Levin HS, Ewing-Cobbs L, et al. Lifetime and novel psychiatric disorders after pediatric traumatic brain injury. J Am Acad Child Psy 2001;40:572–9. [DOI] [PubMed] [Google Scholar]
- 3.Luis CA, Mittenberg W. Mood and anxiety disorders following pediatric traumatic brain injury: a prospective study. J Clin Exp Neuropsychol 2002;24:270–9. [DOI] [PubMed] [Google Scholar]
- 4.Max JE, Arndt S, Castillo CS, et al. Attention-deficit hyperactivity symptomatology after traumatic brain injury: a prospective study. J Am Acad Child Psy 1998;37:841–7. [DOI] [PubMed] [Google Scholar]
- 5.Li L, Liu J. The effect of pediatric traumatic brain injury on behavioral outcomes: a systematic review. Dev Med Child Neurol 2013;55:37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fay TB, Yeates KO, Wade SL, Drotar D, Stancin T, Taylor HG. Predicting longitudinal patterns of functional deficits in children with traumatic brain injury. Neuropsychology 2009;23:271–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kinsella G, Ong B, Murtagh D, Prior M, Sawyer M. The role of the family for behavioral outcome in children and adolescents following traumatic brain injury. J Consult Clin Psych 1999;67:116–23. [DOI] [PubMed] [Google Scholar]
- 8.Hawley CA. Reported problems and their resolution following mild, moderate and severe traumatic brain injury amongst children and adolescents in the UK. Brain Injury 2003;17:105–29. [DOI] [PubMed] [Google Scholar]
- 9.Wade SL, Taylor HG, Drotar D, Stancin T, Yeates KO. Family burden and adaptation during the initial year after traumatic brain injury in children. Pediatrics 1998;102(1 Pt 1):110–6. [DOI] [PubMed] [Google Scholar]
- 10.Aitken ME, Mele N, Barrett KW. Recovery of injured children: parent perspectives on family needs. Arch Phys Med Rehabil 2004;85:567–73. [DOI] [PubMed] [Google Scholar]
- 11.Aitken ME, McCarthy ML, Slomine BS, et al. Family burden after traumatic brain injury in children. Pediatrics 2009;123:199–206. [DOI] [PubMed] [Google Scholar]
- 12.Wade SL, Borawski EA, Taylor HG, Drotar D, Yeates KO, Stancin T. The relationship of caregiver coping to family outcomes during the initial year following pediatric traumatic injury. J Consult Clin Psych 2001;69:406–15. [DOI] [PubMed] [Google Scholar]
- 13.Wade SL, Stancin T, Taylor HG, Drotar D, Yeates KO, Minich NM. Interpersonal stressors and resources as predictors of parental adaptation following pediatric traumatic injury. J Consult Clin Psych 2004; 72:776–84. [DOI] [PubMed] [Google Scholar]
- 14.Yeates KO, Taylor HG, Woodrome SE, Wade SL, Stancin T, Drotar D. Race as a moderator of parent and family outcomes following pediatric traumatic brain injury. J Pediatr Psychol 2002;27:393–403. [DOI] [PubMed] [Google Scholar]
- 15.Lax Pericall MT, Taylor E. Family function and its relationship to injury severity and psychiatric outcome in children with acquired brain injury: a systematized review. Dev Med Child Neurol 2014;56:19–30. [DOI] [PubMed] [Google Scholar]
- 16.Raj SP, Wade SL, Cassedy A, et al. Parent psychological functioning and communication predict externalizing behavior problems after pediatric traumatic brain injury. J Pediatr Psychol 2014;39:84–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown FL, Whittingham K, Boyd R, Sofronoff K. A systematic review of parenting interventions for traumatic brain injury: child and parent outcomes. J Head Trauma Rehab 2013;28:349–60. [DOI] [PubMed] [Google Scholar]
- 18.Ronzio CR, Guagliardo MF, Persaud N. Disparity in location of urban mental service providers. Am J Orthopsychiat 2006;76:37–43. [DOI] [PubMed] [Google Scholar]
- 19.Nezu AM, D’Zurilla TJ. Problem-solving therapy: a positive approach to clinical intervention. New York: Springer Publishing Company; 2006. [Google Scholar]
- 20.Nezu AM, Perri MG. Social problem-solving therapy for unipolar depression: an initial dismantling investigation. J Consult Clin Psych 1989;57:408–13. [PubMed] [Google Scholar]
- 21.Nezu AM. Efficacy of a social problem-solving therapy approach for unipolar depression. J Consult Clin Psychol 1986;54:196–202. [DOI] [PubMed] [Google Scholar]
- 22.Bell AC, D’Zurilla TJ. Problem-solving therapy for depression: a meta-analysis. Clin Psychol Rev 2009;29:348–53. [DOI] [PubMed] [Google Scholar]
- 23.Wade SL, Walz NC, Carey J, McMullen KM. A randomized trial of teen online problem solving: efficacy in improving caregiver outcomes after brain injury. Health Psychol 2012;31:767. [DOI] [PubMed] [Google Scholar]
- 24.Wade SL, Walz NC, Carey J, et al. Effect on behavior problems of teen online problem-solving for adolescent traumatic brain injury. Pediatrics 2011;128:e947–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wade SL, Stancin T, Kirkwood M, Brown TM, McMullen KM, Taylor HG. Counselor-assisted problem solving (CAPS) improves behavioral outcomes in older adolescents with complicated mild to severe TBI. J Head Trauma Rehab 2014;29:198–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wade SL, Walz NC, Carey J, et al. A randomized trial of teen online problem solving for improving executive function deficits following pediatric traumatic brain injury. J Head Trauma Rehab 2010;25:409–15. [DOI] [PubMed] [Google Scholar]
- 27.Kurowski BG, Wade SL, Kirkwood MW, Brown TM, Stancin T, Taylor HG. Online problem-solving therapy for executive dysfunction after child traumatic brain injury. Pediatrics 2013;132:e158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raj SP, Zhang N, Kirkwood MW, et al. Online family problem solving for pediatric traumatic brain injury: influences of parental marital status and participation on adolescent outcomes. J Head Trauma Rehab 2017;33:158–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kazdin AE, Holland L, Crowley M. Family experience of barriers to treatment and premature termination from child therapy. J Consult Clin Psych 1997;65:453. [DOI] [PubMed] [Google Scholar]
- 30.Cunningham CE, Boyle M, Offord D, et al. Tri-ministry study: correlates of school-based parenting course utilization. J Consult Clin Psych 2000;68:928–33. [PubMed] [Google Scholar]
- 31.Kazdin AE, Mazurick JL. Dropping out of child psychotherapy: distinguishing early and late dropouts over the course of treatment. J Consult Clin Psych 1994;62:1069–74. [DOI] [PubMed] [Google Scholar]
- 32.Webster-Stratton C, Hammond M. Predictors of treatment outcome in parent training for families with conduct problem children. Behav Ther 1990;21:319–37. [Google Scholar]
- 33.Bagner DM, Eyberg SM. Father involvement in parent training: when does it matter? J Clin Child 2003;32:599–605. [DOI] [PubMed] [Google Scholar]
- 34.Wade SL, Taylor HG, Yeates KO, et al. Online problem solving for adolescent brain injury: a randomized trial of 2 approaches. J Dev Behav Pediatr 2018;39:154–62. [DOI] [PubMed] [Google Scholar]
- 35.Wade SL, Narad ME, Kingery KM, et al. Teen online problem solving for teens with traumatic brain injury: rationale, methods, and preliminary feasibility of a teen only intervention. Rehabil Psychol 2017; 62:290–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Derogatis LR. The Brief Symptom Inventory (BSI) administration, scoring, and procedures manual. Minneapolis: National Computer Systems; 1993. [Google Scholar]
- 37.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psych Meas 1977;1: 385–401. [Google Scholar]
- 38.Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. J Marital Fam Ther 1983;9:171–80. [Google Scholar]
- 39.Robin AL, Koepke T, Moye AW, Gerhardstein R. Parent adolescent relationship questionnaire. PAR; 2009. [Google Scholar]
- 40.Robin AF, Foster SL. Negotiating parent-adolescent conflict: a behavioral-family systems approach. New York: Guiliford Press; 1989. [Google Scholar]
- 41.Cairney J, Boyle M, Offord DR, Racine Y. Stress, social support and depression in single and married mothers. Soc Psychiatry Psychiatr Epidemiol 2003;38:442–9. [DOI] [PubMed] [Google Scholar]
- 42.Weinraub M, Wolf BM. Effects of stress and social supports on mother-child interactions in single- and two-parent families. Child Dev 1983;54:1297–311. [PubMed] [Google Scholar]
- 43.United States Census Bureau. The majority of children live with two parents, census bureau reports [press release]. Washington (DC): United States Census Bureau; 2016. [Google Scholar]


