Abstract
Introduction
Patients requiring coronary artery bypass grafting (CABG) and carotid endarterectomy (CEA) can be managed with staged (CEA before CABG), reverse staged (CABG before CEA) or synchronous treatment. This single-center retrospective study evaluated the outcomes in patients undergoing planned synchronous CEA and CABG.
Methods
Between 2000 and 2020 a total of 185 patients with symptomatic triple-vessel or left main coronary artery disease associated with 70–99% asymptomatic or 50–99% symptomatic uni- or bilateral internal carotid artery (ICA) stenosis underwent synchronous CEA and CABG at our institution. Study endpoints were defined as mortality, stroke and myocardial infarction at 30 days. Additionally, the composite endpoint of these events was investigated.
Results
At 30 days, mortality, stroke and myocardial infarction rates were 5.9%, 8.1% (permanent [unresolved deficit at discharge] 5.4%) and 3.8%, respectively, and the composite endpoint was reached in 13.0% of patients. Patients suffering from a stroke more frequently had a contralateral 70–99% ICA stenosis (60.0% vs. 17.3%; p < 0.001), peripheral artery disease (73.3% vs. 38.9%; p = 0.013) and prolonged cardiopulmonary bypass time (mean 119 ± 62 min vs. 84 ± 29 min; p = 0.012). Multivariate logistic regression analysis revealed the duration of cardiopulmonary bypass (odds ratio [OR] 1.024; 95% confidence interval [CI] 1.002–1.046; p = 0.034), a history of type 2 diabetes mellitus (OR 5.097; 95% CI 1.161–22.367; p = 0.031) and peripheral artery disease (OR 5.814; 95% CI 1.231–27.457; p = 0.026) as independent risk factors for reaching the composite endpoint.
Conclusion
Patients undergoing synchronous CEA and CABG face an elevated risk of perioperative cardiovascular events, particularly an increased stroke risk in patients with symptomatic and bilateral ICA stenosis.
Graphical Abstract available for this article.
Graphical Abstract
Keywords: Coronary artery bypass grafting, Carotid endarterectomy, Internal carotid artery stenosis, Perioperative stroke, Long-term survival
Key Summary Points
| Why carry out this study? |
| To evaluate the outcomes of patients undergoing planned synchronous carotid endarterectomy (CEA) and coronary artery bypass grafting (CABG) in a heterogeneous group of high-risk patients. |
| The most efficient operative strategy remains unknown because of conflicting evidence, the lack of randomized controlled studies and the disparate inclusion criteria in prior trials. |
| This study aimed to assess the 30-day mortality, stroke and myocardial infarction rates as well as the composite endpoint of these events. |
| What was learned from the study? |
| The study found that in this high-risk patient group, the 30-day mortality, stroke and myocardial infarction rates were 5.9%, 8.1% (permanent [unresolved deficit at discharge] 5.4%) and 3.8%, respectively, with a composite endpoint reached in 13.0% of patients. |
| Patients undergoing synchronous CEA and CABG are at increased risk, often associated with severe generalized atherosclerosis and a higher likelihood of perioperative vascular events. Risk factors for reaching the composite endpoint included the duration of cardiopulmonary bypass, a history of type 2 diabetes mellitus and peripheral artery disease. |
Digital Features
This article is published with digital features, including a graphical abstract, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.25104092.
Introduction
Patients undergoing coronary artery bypass grafting (CABG) present with internal carotid artery (ICA) stenosis in 6–8% of cases, which is associated with an increased risk of perioperative stroke [1]. Patients requiring CABG and carotid endarterectomy (CEA) are managed by staged (prophylactic CEA before CABG), reverse staged (CABG before delayed CEA) or synchronous treatment. Previous reports suggested that staged and synchronous treatment have a lower risk of postoperative stroke than the reverse staged sequence [2]. However, the most efficient operative strategy remains unknown because of conflicting evidence, the lack of randomized controlled studies and the disparate inclusion criteria in prior trials. This large single-center retrospective study evaluated the perioperative and long-term outcomes in patients undergoing planned synchronous CEA and CABG.
Methods
Ethical Statement
This study followed the tenets of the Declaration of Helsinki. The protocol and methods were reviewed and approval has been granted by the institutional Ethics Committee of the Federal State Upper Austria for this retrospective study (license no. 1213/2019). Requisite patient consent was waived.
Patients and Study Design
Between 2000 and 2020, 185 consecutive patients with triple-vessel or left main coronary artery disease associated with uni- or bilateral 70–99% asymptomatic or 50–99% symptomatic (ischemic symptoms within the last 6 months or silent cerebral embolization on imaging) ICA stenosis underwent elective CABG and synchronous CEA at our institution. Severity of the ICA stenosis was measured by means of duplex ultrasound and confirmed with conventional angiography (initial study period), computed tomography or magnetic resonance imaging scan according to the North American Symptomatic Carotid Endarterectomy (NASCET) methodology (Fig. 1A) [3].
Fig. 1.
A Magnetic resonance imaging scan indicating the severity of the internal carotid artery stenosis, B carotid endarterectomy with intraluminal shunting prior to patch angioplasty, C diffusion-weighted imaging of a 75-year-old man with left-sided hemiparesis after on-pump synchronous treatment with endarterectomy of the left carotid artery showing multiple diffusion abnormalities scattered throughout the brain
CEA was performed prior to CABG under the same anesthesia. Eversion endarterectomy was the standard operative technique. In the presence of contralateral ICA stenosis or occlusion, known poor intracerebral collateralization (interrupted circle of Willis) and/or a decrease in oxygen saturation (measured by near infrared spectroscopy monitoring) > 20% after carotid artery clamping patch angioplasty with intraluminal shunting was carried out (Fig. 1B). All CABG procedures were performed using cardiopulmonary bypass (CPB) with aortic cross clamping and cardioplegic arrest.
Primary study endpoints were defined as the rate of stroke, myocardial infarction (MI) and mortality at 30 days (early endpoints). In addition, the composite endpoint of these events was investigated. Stroke was defined as any focal or global neurological deficit lasting > 24 h and was clinically assessed by a neurologist. Permanent stroke was considered as stroke not fully recovered before discharge. Events occurring after 30 days were defined as late endpoints.
Statistical Analysis
All data of continuous variables were checked for normal distribution (test of normality: Kolmogorov-Smirnov with Lilliefors significance correction, type I error = 10%) and in the case of normal distribution also for heteroscedasticity (Levene test, type I error = 5%). If normality and variance homogeneity could be assumed, the independent two-sample t-test was used for subgroup comparisons. If normality and no variance homogeneity could be assumed, Welch’s t-test was used. If normality could not be assumed, the exact Mann-Whitney U test was used. Categorical variables were compared by the Fisher’s exact test or by the exact chi-square test. Time to event variables were depicted by Kaplan-Meier plots.
For the comparative depiction of the survival times of the study population and the total population a matched pair approach with age-related estimations of total population survival times (source: http://www.statistik-austria.at) censored at 20 years was used.
The influence of age, preoperative estimated glomerular filtration rate, preoperative left ventricle ejection fraction, CPB time, preoperative N-terminal pro-B-type natriuretic peptide, sex, type 2 diabetes mellitus (T2DM), peripheral artery disease (PAD), preoperative atrial fibrillation, contralateral ≥ 70% ICA stenosis and patient’s clinical history (e.g., previous transient ischemic attack or stroke) on the combined endpoint of mortality, stroke and MI at 30 days was investigated by multivariate logistic regression analysis and reported as odds ratio (OR) with 95% confidence interval (CI).
The type I error was not adjusted for multiple testing. Therefore, the results of inferential statistics are descriptive only. Statistical analysis was performed using the open-source R statistical software package, version 3.6.1 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Clinical and demographic data are summarized in Table 1; operative data are depicted in Table 2. Mean age of the study population was 70.5 ± 8.3 years. T2DM was present in 66 patients (35.7%) and symptomatic PAD in 77 patients (41.6%). The mean logarithmic EuroSCORE (predicted mortality according to a logistic regression equation) was 9.2 ± 7.2%. Symptomatic ICA stenosis was present in 15 patients (8.1%). Seventy-eight patients (42.2%) had a contralateral ≥ 50% ICA stenosis, including six patients (3.2%) with a complete occlusion of the contralateral carotid artery. The mean CPB time was 87 ± 34 min. The calculated median perioperative red blood cell loss was 749 (IQR 558–1023) ml.
Table 1.
Demographic and clinical data of study population (n = 185)
| Parameter | |
|---|---|
| Age, years | 70.5 ± 8.3 |
| Female | 50 (27.0) |
| BMI, kg/m2 | 27.7 ± 4.1 |
| Smoker | 55 (29.7) |
| Comorbidities | |
| Hypertension | 162 (87.6) |
| Type 2 diabetes mellitus | 66 (35.7) |
| Hyperlipidemia | 165 (89.2) |
| Chronic obstructive pulmonary disease | 26 (14.1) |
| Peripheral arterial disease | 77 (41.6) |
| Chronic kidney disease | 78 (42.2) |
| Preoperative atrial fibrillation | 28 (15.1) |
| Previous myocardial infarction | 77 (41.6) |
| Preoperative pulmonal hypertension | 4 (2.2) |
| Previous cardiac surgery | 3 (1.6) |
| Preoperative blood values | |
| Serum creatinine, mg/dl | 1.0 (0.9–1.3) |
| Estimated glomerular filtration rate, ml/min | 66.2 (47.9–89.4) |
| Hemoglobin, g/dl | 13.6 (12.3–14.5) |
| NT-proBNP, ng/l | 610.6 (198.0–1765.0) |
| Preoperative LVEF, % | 60 (45–65) |
| ICA stenosis | |
| Asymptomatic | 170 (91.9) |
| Symptomatic | 15 (8.1) |
| Contralateral ≥ 50% | 78 (42.2) |
| Contralateral ≥ 70% | 39 (21.1) |
| Logarithmic EuroSCORE, % | 9.2 ± 7.2 |
Continuous data are presented in mean ± standard deviation as well as in median (interquartile range) as appropriate and categorical data as counts (and percentages)
BMI body mass index, ICA internal carotid artery, LVEF left ventricle ejection fraction, NT-proBNP N-terminal pro-B-type natriuretic peptide
Table 2.
Perioperative data of study population (n = 185)
| Parameter | |
|---|---|
| Blood transfusion need, ml | 480 (0–960) |
| Perioperative RBC loss, ml | 749 (558–1023) |
| Cross-clamp time, min | 40 ± 14 |
| CPB time, min | 87 ± 34 |
| ICU stay, days | 2 (1–5) |
| IABP | 11 (5.9) |
| ECMO | 2 (1.1) |
| Hemofiltration at ICU | 6 (3.2) |
| Hemoglobin at discharge, g/dl | 10.1 (9.4–10.9) |
| In-hospital stay, days | 17.2 ± 9.2 |
Continuous data are presented in mean ± standard deviation as well as in median (interquartile range) as appropriate and categorical data as counts (and percentages)
CPB cardiopulmonary bypass, ECMO extracorporeal membrane oxygenation, IABP intra-aortic balloon pump, ICU intensive care unit, RBC red blood cell
At 30 days, mortality, stroke and MI rates were 5.9% (11 patients), 8.1% (15 patients; permanent neurological deficit was present in 10 patients, 5.4%) and 3.8% (7 patients), respectively (Table 3). The early composite endpoint was reached in 13.0% (24 patients) of the study population.
Table 3.
Primary and combined endpoints at 30 days and stroke location
| Parameter | |
|---|---|
| Mortality | 11 (5.9) |
| Stroke | 15 (8.1) |
| Myocardial infarction | 7 (3.8) |
| Combined endpoint | 24 (13.0) |
| Stroke location | |
| Ipsilateral | 4 (26.7) |
| Contralateral | 4 (26.7) |
| Bilateral | 7 (46.7) |
Categorical data are presented as counts (and percentages)
Patients suffering from a perioperative stroke more frequently had a contralateral 70–99% ICA stenosis (60.0% vs. 17.3%; p < 0.001), PAD (73.3% vs. 38.9%; p = 0.013), prolonged duration of CPB (mean 119 ± 62 min vs. 84 ± 29 min; p = 0.012), increased blood transfusion needs (median 1200 (IQR 480–2160) ml vs. 240 (IQR 0–720) ml; p = 0.001) and impaired renal function (estimated glomerular filtration rate 56 ± 22 ml/min vs. 73 ± 31 ml/min; p = 0.041). In-hospital mortality of stroke patients was 40% (6 patients). Five patients (33.3%) had complete neurological restitution ad integrum at discharge.
Multivariate logistic regression analysis revealed the duration of CPB (OR 1.024; 95% CI 1.002–1.046; p = 0.034), a history of T2DM (OR 5.097; 95% CI 1.161–22.367; p = 0.031) and PAD (OR 5.814; 95% CI 1.231–27.457; p = 0.026) as independent risk factors for the early composite endpoint (Table 4). In-hospital mortality was 7% (13 patients). Reasons for early death included stroke in five patients, multi-organ failure in three patients, MI in two patients, arrhythmia in two patients and cardiac tamponade in one patient.
Table 4.
Multivariate logistic regression analysis showing predictors of the combined endpoint of mortality, stroke and myocardial infarction at 30 days
| Parameter | Coeff B | p value | OR (95% CI) |
|---|---|---|---|
| CPB time | 0.024 | 0.034 | 1.024 (1.002–1.046) |
| T2DM | 1.629 | 0.031 | 5.097 (1.161–22.367) |
| PAD | 1.760 | 0.026 | 5.814 (1.231–27.457) |
Coeff B regression coefficient B, CI confidence interval, CPB cardiopulmonary bypass, OR odds ratio, PAD peripheral artery disease, T2DM type 2 diabetes mellitus
The 30-day stroke risk among the 170 patients with asymptomatic ICA stenosis was 7.1% (12 patients). For patients undergoing CEA for unilateral, asymptomatic 70–99% ICA stenosis, the stroke risk was 2% (2 of 100 patients). However, if CEA was performed for an asymptomatic 70–99% ICA stenosis in the presence of a contralateral ≥ 50% stenosis, the stroke risk was 14.3% (10 of 70 patients). The 30-day stroke risk among 15 patients with symptomatic 50–99% ICA stenosis, including 8 cases with bilateral disease, was 20% (3 patients). All strokes were ischemic and occurred within 30 days after surgery. On computed tomography or magnetic resonance imaging scan, brain lesions were detected ipsilateral to the CEA distribution site in 4 patients (26.7%) and contra- or bilateral to the CEA distribution site in 11 patients (73.3%). Among the 15 stroke cases, two patients had a known occlusion of the contralateral carotid artery, two patients had been resuscitated postoperatively because of cardiac arrest and one patient was on extracorporeal life support. In one stroke patient, the brachiocephalic trunk was cannulated unplanned because of a porcelain aorta. In another patient, a bilateral mesencephalic infarct occurred after hospital discharge.
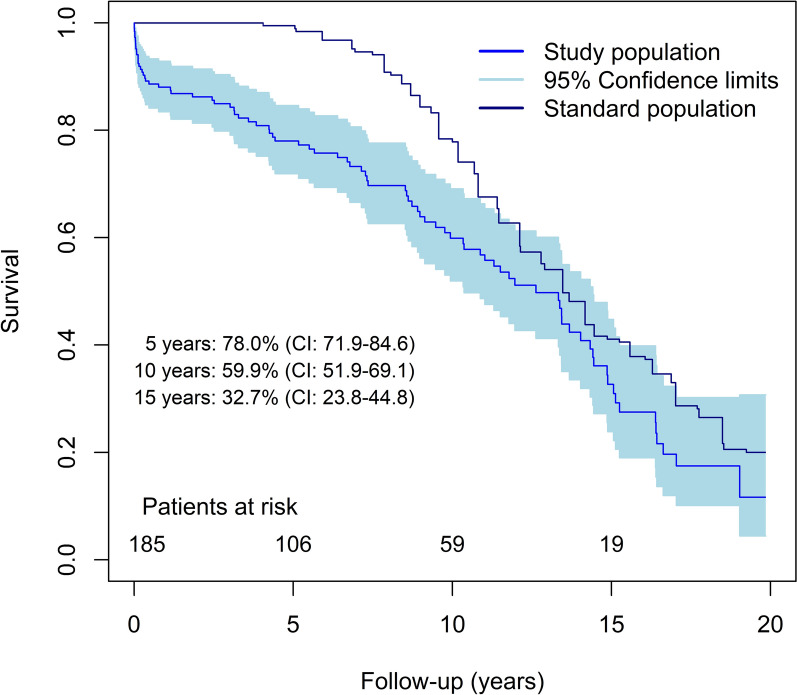
Mean survival during follow-up was 7.1 ± 5.6 years (Fig. 2). Overall mortality within the observational period was 46.5% (86 patients). Reasons for late death were mainly related to cardiovascular diseases. The 10-year survival probability of the study population was 59.9% (95% CI 51.9–69.1) compared with 77.8% (95% CI 72.1–84.1) in the age-matched general population (p = 0.001).
Fig. 2.
Kaplan-Meier long-term survival analysis of study population compared with the survival probability of the general Austrian population matched for gender and age. CI confidence interval
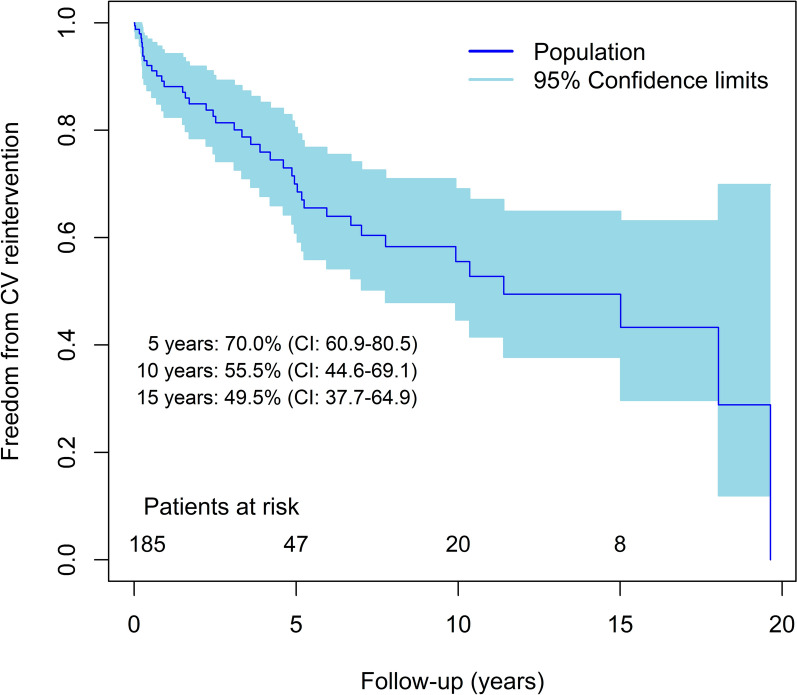
Forty-one patients (22.2%) had at least one cardiovascular reintervention during follow-up, including 28 reinterventions for PAD, 10 reinterventions for carotid artery disease, 7 operations for contralateral ICA stenosis, 2 transcatheter aortic valve replacements and 9 other procedures. Freedom from any cardiovascular reintervention at 10 years was 55.5% (95% CI 44.6–69.1; Fig. 3).
Fig. 3.
Kaplan-Meier estimates of freedom from any cardiovascular reintervention. CI confidence interval, CV cardiovascular
Discussion
Perioperative stroke is a devastating complication of cardiac surgery and is associated with prolonged ventilator support, delayed discharge from the intensive care unit, in-hospital mortality of up to 24% and impaired quality of life due to neurological sequelae [4]. The risk of major stroke during isolated CABG is 1.9–3.8% [5]. Clinically silent cerebral embolization detected by imaging is much more frequent [6]. Cerebrovascular occlusive disease increases the risk of stroke, especially if bilateral or symptomatic ICA stenoses are present [7]. Other risk factors for perioperative stroke are prior neurological events, duration of CPB and atrial fibrillation [8]. Age, left main coronary artery disease, PAD, T2DM, chronic kidney disease, smoking and arterial hypertension probably do not play a direct role in the pathogenesis of perioperative stroke but are associated with atherosclerosis of the ascending aorta, which has been identified as strong predictor for focal neurological deficit after isolated CABG [9, 10].
In patients scheduled for CABG, ICA stenosis is a frequent incidental finding during routine preoperative assessment. Because of concerns about impaired cerebral perfusion during CPB and the anticipated risk of procedural stroke in patients with high-grade ICA stenosis, we routinely performed CEA ahead of CABG. Moreover, untreated carotid artery disease has also been identified as a risk factor for stroke during long-term follow-up after CABG [11]. Due to the collaborative efforts of cardiac and vascular surgeons in one department, we preferred synchronous CEA and CABG. This approach requires only one anesthesia exposure and the risk of MI during awaiting CABG is reduced compared to staged CEA [12]. However, the operative time is prolonged and mortality may be increased in patients undergoing synchronous CEA and CABG; however, this was not a uniform finding in previous reports [13]. Compared to the reverse staged approach, the risk of stroke is reduced in CABG patients with prior (staged or synchronous) CEA [2].
The composite endpoint of death, MI and stroke within 30 days after surgery was 13.0% in our patients, which is comparable to community-wide outcomes of synchronous CEA and CABG [14]. In accordance with previous publications, we found that these patients are at increased risk of perioperative cardiovascular events including stroke, frequently undergo reinterventions from multi-territorial atherosclerosis and have reduced long-term survival. The risk of permanent stroke in our study, which included consecutive and unselected patients, was 5.4%. Half of the patients in our series had bilateral or symptomatic carotid artery disease, which is clearly associated with an increased risk of perioperative stroke [7]. Among patients with unilateral, asymptomatic ICA stenosis the stroke risk was 2% at 30 days, lower compared to single institutional reviews and controlled studies [1, 2]. However, staged or synchronous CEA for unilateral ICA stenosis is no longer recommended as routine clinical practice in current guidelines [15, 16]. Asymptomatic unilateral ICA stenosis is not a proven independent risk factor for procedural, ipsilateral ischemic stroke in patients undergoing CABG, and prophylactic CEA failed to demonstrate a clear benefit in those patients [7, 17]. Moreover, a substantial proportion of strokes after CABG occurs in patients without cerebrovascular occlusive disease, is bihemispheric or contralateral to the hemispheric distribution of a significant ICA stenosis or occurs after an uneventful recovery from surgery [8, 17, 18]. For the latter patients, arrhythmias in the perioperative period such as atrial fibrillation may play a causative role in the development of neurological events.
Cerebral hypoperfusion accounts for 8.8% of strokes after CABG [19]. Patients with impaired cerebral blood flow reserve due to extra- and/or intracranial cerebrovascular occlusive disease have an increased risk of brain hypoperfusion and watershed infarcts during CPB [20]. To improve patient selection for prophylactic CEA, we now routinely assess CABG patients with known high-grade ICA stenosis by means of magnetic resonance angiography and transcranial Doppler ultrasound performed by a specially trained neurologist. If cerebral blood flow reserve is impaired (increase in middle cerebral artery blood flow velocity < 10% on breath holding), we perform synchronous CEA and CABG. For remaining CABG patients with unilateral, asymptomatic 70–99% ICA stenosis, the carotid revascularization strategy is decided by multidisciplinary discussion and individualized. In general, we advise synchronous CEA for patients with an increased risk for late stroke, including those with ipsilateral silent cerebral embolization on neuroimaging, documented progression to an ≥ 80% ICA stenosis or high-risk morphological features of the carotid plaque. In all patients with high-grade ICA stenosis and especially in those not scheduled for CEA, general measures to reduce procedural stroke risk during CABG include a mean arterial pressure > 70 mmHg during CPB, avoiding intraoperative drops in blood pressure, avoiding a nadir hematocrit < 25%, optimizing perioperative hemodynamics, patient blood management strategies to avoid transfusions, aggressive treatment of arrhythmias and proper anticoagulation.
Seventy-three percent of strokes in our series occurred contra- or bilateral to the CEA distribution site, indicating that they were not caused by temporary hypoperfusion during carotid artery clamping (Fig. 1C). There is an increasing amount of evidence that points towards ascending aorta atherosclerosis as the principal culprit lesion for perioperative strokes in CABG patients. With a reported OR of 3 to 4.5, an atheromatous proximal aorta is the strongest independent predictor for perioperative strokes in isolated CABG procedures [4, 21, 22]. Uni- or bihemispheric plaque material embolization may occur during manipulation, cannulation, cross or side clamping of the aorta as well as a “sandblasting” effect of the jet derived from the inflow cannula [23–25]. We now routinely perform preoperative imaging of the aorta with computed tomography in patients > 60 years and those suspected to have severe generalized atherosclerosis (high cardiovascular risk profile, on dialysis, symptomatic PAD, visible aortic calcification on preoperative chest x-ray or angiography). Epiaortic ultrasonography is also highly sensitive in the detection of even non-calcified atheroma of the ascending aorta [26]. Ultrasound-guided aortic cannulation and cross clamping have been shown to reduce perioperative stroke and death rate associated with on-pump coronary surgery [27]. Additionally, porcelain aorta is present in up to 9.3% of patients undergoing elective CABG and may preclude any aortic manipulation [28]. If such severe calcifications in the ascending aorta are detected by preoperative imaging, we favor off-pump coronary artery bypass grafting (OPCAG) in hemodynamically stable patients with good quality target coronary vessels and on-pump beating heart CABG with direct axillary artery cannulation for unstable patients as well as those with diffuse carotid artery disease or poor quality target vessels. Preferentially all arterial in situ bypass conduits or Y-grafts are used. In patients with atheromatous aortas, OPCAG is associated with a reduced risk of stroke and in-hospital mortality [29]. However, the graft number is reduced and the risk of incomplete revascularization increased compared to on-pump surgery. Adequate patient selection is therefore mandatory for OPCAG. Axillary artery cannulation has been shown to reduce cerebral microembolization from the aorta, especially into the right hemisphere by flow reversal in the innominate artery [30]. Even in the presence of severe atherosclerosis of the aorta, the axillary artery is most often disease free. We prefer direct axillary artery cannulation; alternatively, a side graft can be used.
Nevertheless, the limitations of this single-center experience study include its retrospective nature. Additionally, the absence of a comparison group undergoing staged procedures makes it challenging to draw definitive conclusions about the superiority of synchronous CEA and CABG.
Conclusion
Patients with concomitant severe coronary and carotid artery disease are at increased risk of perioperative cardiovascular events including stroke, frequently undergo reinterventions from multi-territorial atherosclerosis and have reduced long-term survival. A multidisciplinary approach, proper patient selection and the full armamentarium of surgical techniques should improve outcomes in these patients.
Acknowledgements
We thank the participants of the study.
Author Contributions
Thomas Ratschiller was involved in the conceptualization and design of the study, and Paimann Nawrozi was involved in data collection as well as drafting the article. Wolfgang Schimetta was involved in statistical analysis. Paimann Nawrozi, Thomas Ratschiller, Wolfgang Schimetta, Gregor Gierlinger, Markus Pirklbauer, Hannes Müller and Andreas Zierer were involved in the interpretation of data and revising the article critically, and in the final approval of the version to be submitted. All authors attest that they meet the current ICMJE criteria for authorship.
Funding
Open access funding provided by Johannes Kepler University Linz. The journal’s Rapid Service and Open Access fees were funded by the Department of Cardiac, Vascular and Thoracic Surgery, Kepler University Hospital, Linz.
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Declarations
Conflict of Interest
Paimann Nawrozi, Thomas Ratschiller, Wolfgang Schimetta, Gregor Gierlinger, Markus Pirklbauer, Hannes Müller and Andreas Zierer declare no conflicts of interest related to this study.
Ethical Approval
This study followed the tenets of the Declaration of Helsinki. The protocol and methods were reviewed and approval has been granted by the institutional Ethics Committee of the Federal State Upper Austria for this retrospective study (license no. 1213/2019). Requisite patient consent was waived.
Footnotes
Prior Presentation: Part of this work was presented as an abstract at Herzmedizin 2021 Digital (DGTHG–DGPK) in February 2021 and at the ÖGHTG annual meeting in Salzburg in May 2021.
Paimann Nawrozi and Thomas Ratschiller contributed equally to this work.
References
- 1.Weimar C, Bilbilis K, Rekowski J, et al. Safety of simultaneous coronary artery bypass grafting and carotid endarterectomy versus isolated coronary artery bypass grafting: a randomized clinical trial. Stroke. 2017;48(10):2769–2775. doi: 10.1161/STROKEAHA.117.017570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Illuminati G, Ricco J-B, Caliò F, et al. Short-term results of a randomized trial examining timing of carotid endarterectomy in patients with severe asymptomatic unilateral carotid stenosis undergoing coronary artery bypass grafting. J Vasc Surg. 2011;54(4):993–999. doi: 10.1016/j.jvs.2011.03.284. [DOI] [PubMed] [Google Scholar]
- 3.Barnett HJM, Taylor DW, Haynes RB, et al. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325(7):445–453. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 4.Filsoufi F, Rahmanian PB, Castillo JG, Bronster D, Adams DH. Incidence, topography, predictors and long-term survival after stroke in patients undergoing coronary artery bypass grafting. Ann Thorac Surg. 2008;85(3):862–870. doi: 10.1016/j.athoracsur.2007.10.060. [DOI] [PubMed] [Google Scholar]
- 5.Bucerius J, Gummert JF, Borger MA, et al. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg. 2003;75(2):472–478. doi: 10.1016/S0003-4975(02)04370-9. [DOI] [PubMed] [Google Scholar]
- 6.Nah H-W, Lee J-W, Chung C-H, et al. New brain infarcts on magnetic resonance imaging after coronary artery bypass graft surgery: lesion patterns, mechanism, and predictors. Ann Neurol. 2014;76(3):347–355. doi: 10.1002/ana.24238. [DOI] [PubMed] [Google Scholar]
- 7.Naylor AR, Bown MJ. Stroke after cardiac surgery and its association with asymptomatic carotid disease: an updated systematic review and meta-analysis. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg. 2011;41(5):607–624. doi: 10.1016/j.ejvs.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 8.Stamou SC, Hill PC, Dangas G, et al. Stroke after coronary artery bypass: incidence, predictors, and clinical outcome. Stroke. 2001;32(7):1508–1513. doi: 10.1161/01.STR.32.7.1508. [DOI] [PubMed] [Google Scholar]
- 9.van der Linden J, Hadjinikolaou L, Bergman P, Lindblom D. Postoperative stroke in cardiac surgery is related to the location and extent of atherosclerotic disease in the ascending aorta. J Am Coll Cardiol. 2001;38(1):131–135. doi: 10.1016/S0735-1097(01)01328-6. [DOI] [PubMed] [Google Scholar]
- 10.Kronzon I, Tunick PA. Aortic atherosclerotic disease and stroke. Circulation. 2006;114(1):63–75. doi: 10.1161/CIRCULATIONAHA.105.593418. [DOI] [PubMed] [Google Scholar]
- 11.Schachner T, Zimmer A, Nagele G, Laufer G, Bonatti J. Risk factors for late stroke after coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2005;130(2):485–490. doi: 10.1016/j.jtcvs.2004.12.038. [DOI] [PubMed] [Google Scholar]
- 12.Naylor AR, Cuffe RL, Rothwell PM, Bell PRF. A systematic review of outcomes following staged and synchronous carotid endarterectomy and coronary artery bypass. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg. 2003;25(5):380–389. doi: 10.1053/ejvs.2002.1895. [DOI] [PubMed] [Google Scholar]
- 13.Giannopoulos S, Texakalidis P, Charisis N, et al. Synchronous carotid endarterectomy and coronary artery bypass graft versus staged carotid artery stenting and coronary artery bypass graft for patients with concomitant severe coronary and carotid stenosis: a systematic review and meta-analysis. Ann Vasc Surg. 2020;62:463–473.e4. doi: 10.1016/j.avsg.2019.06.018. [DOI] [PubMed] [Google Scholar]
- 14.Brown KR, Kresowik TF, Chin MH, Kresowik RA, Grund SL, Hendel ME. Multistate population-based outcomes of combined carotid endarterectomy and coronary artery bypass. J Vasc Surg. 2003;37(1):32–39. doi: 10.1067/mva.2003.60. [DOI] [PubMed] [Google Scholar]
- 15.Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;124(23):2610–2642. doi: 10.1161/CIR.0b013e31823b5fee. [DOI] [PubMed] [Google Scholar]
- 16.Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution. Eur Heart J. 2014;35(37):2541–2619. doi: 10.1093/eurheartj/ehu278. [DOI] [PubMed] [Google Scholar]
- 17.Li Y, Walicki D, Mathiesen C, et al. Strokes after cardiac surgery and relationship to carotid stenosis. Arch Neurol. 2009;66(9):1091–1096. doi: 10.1001/archneurol.2009.114. [DOI] [PubMed] [Google Scholar]
- 18.Schoof J, Lubahn W, Baeumer M, et al. Impaired cerebral autoregulation distal to carotid stenosis/occlusion is associated with increased risk of stroke at cardiac surgery with cardiopulmonary bypass. J Thorac Cardiovasc Surg. 2007;134(3):690–696. doi: 10.1016/j.jtcvs.2007.03.018. [DOI] [PubMed] [Google Scholar]
- 19.Likosky DS, Marrin CAS, Caplan LR, et al. Determination of etiologic mechanisms of strokes secondary to coronary artery bypass graft surgery. Stroke. 2003;34(12):2830–2834. doi: 10.1161/01.STR.0000098650.12386.B3. [DOI] [PubMed] [Google Scholar]
- 20.Tsuda K, Shiiya N, Washiyama N, et al. Carotid stenosis with impaired brain flow reserve is associated with an increased risk of stroke in on-pump cardiovascular surgery. Interact Cardiovasc Thorac Surg. 2018;27(1):75–80. doi: 10.1093/icvts/ivy049. [DOI] [PubMed] [Google Scholar]
- 21.John R, Choudhri AF, Weinberg AD, et al. Multicenter review of preoperative risk factors for stroke after coronary artery bypass grafting. Ann Thorac Surg. 2000;69(1):30–36. doi: 10.1016/S0003-4975(99)01309-0. [DOI] [PubMed] [Google Scholar]
- 22.Roach GW, Kanchuger M, Mangano CM, et al. Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med. 1996;335(25):1857–1863. doi: 10.1056/NEJM199612193352501. [DOI] [PubMed] [Google Scholar]
- 23.Katz ES, Tunick PA, Rusinek H, Ribakove G, Spencer FC, Kronzon I. Protruding aortic atheromas predict stroke in elderly patients undergoing cardiopulmonary bypass: experience with intraoperative transesophageal echocardiography. J Am Coll Cardiol. 1992;20(1):70–77. doi: 10.1016/0735-1097(92)90139-E. [DOI] [PubMed] [Google Scholar]
- 24.Barbut D, Hinton RB, Szatrowski TP, et al. Cerebral emboli detected during bypass surgery are associated with clamp removal. Stroke. 1994;25(12):2398–2402. doi: 10.1161/01.STR.25.12.2398. [DOI] [PubMed] [Google Scholar]
- 25.Sabik JF, Lytle BW, McCarthy PM, Cosgrove DM. Axillary artery: an alternative site of arterial cannulation for patients with extensive aortic and peripheral vascular disease. J Thorac Cardiovasc Surg. 1995;109(5):881–885. doi: 10.1016/S0022-5223(95)70312-8. [DOI] [PubMed] [Google Scholar]
- 26.Gaudino M, Benesch C, Bakaeen F, et al. Considerations for reduction of risk of perioperative stroke in adult patients undergoing cardiac and thoracic aortic operations: a scientific statement from the American Heart Association. Circulation. 2020;142(14):e193–e209. doi: 10.1161/CIR.0000000000000885. [DOI] [PubMed] [Google Scholar]
- 27.Gold JP, Torres KE, Maldarelli W, Zhuravlev I, Condit D, Wasnick J. Improving outcomes in coronary surgery: the impact of echo-directed aortic cannulation and perioperative hemodynamic management in 500 patients. Ann Thorac Surg. 2004;78(5):1579–1585. doi: 10.1016/j.athoracsur.2004.05.051. [DOI] [PubMed] [Google Scholar]
- 28.Sirin G. Surgical strategies for severely atherosclerotic (porcelain) aorta during coronary artery bypass grafting. World J Cardiol. 2021;13(8):309–324. doi: 10.4330/wjc.v13.i8.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharony R, Bizekis CS, Kanchuger M, et al. Off-pump coronary artery bypass grafting reduces mortality and stroke in patients with atheromatous aortas: a case control study. Circulation. 2003;108(Suppl II):15–20. doi: 10.1161/01.cir.0000087448.65888.21. [DOI] [PubMed] [Google Scholar]
- 30.Hedayati N, Sherwood JT, Schomisch SJ, Carino JL, Markowitz AH. Axillary artery cannulation for cardiopulmonary bypass reduces cerebral microemboli. J Thorac Cardiovasc Surg. 2004;128(3):386–390. doi: 10.1016/j.jtcvs.2004.01.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.