Abstract
Background:
Even though a few years have passed since the coronavirus disease 2019 (COVID-19) outbreak, information regarding certain aspects of the disease, such as post-infection immunity, is still quite limited. This study aimed to evaluate post-infection protection and COVID-19 features among healthcare workers (HCWs), during three successive surges, as well as the rate of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) reinfection, reactivation, re-positivity, and severity.
Methods:
This cross-sectional population-level observational study was conducted from 20 April 2020 to 18 February 2021. The study population included all HCWs in public or private hospitals in Fars Province, Southern Iran. The infection rate was computed as the number of individuals with positive polymerase chain reaction (PCR) tests divided by the total number of person-days at risk. The re-infection was evaluated after 90 days.
Results:
A total of 30,546 PCR tests were performed among HCWs, of which 13,749 (61.94% of total HCWs) were positive. Considering the applied 90-day threshold, there were 44 (31.2%) cases of reactivation and relapse, and 97 (68.8% of infected and 1.81% of total HCWs) cases of reinfection among 141 (2.64%) diagnosed cases who experienced a second episode of COVID-19. There was no significant difference in symptoms (P=0.65) or the necessity for ICU admission (P=0.25). The estimated protection against repeated infection after a previous SARS-CoV-2 infection was 94.8% (95% CI=93.6-95.7).
Conclusion:
SARS-CoV-2 re-positivity, relapse, and reinfection were rare in the HCW population. After the first episode of infection, an estimated 94.8% protection against recurring infections was achieved.
A preprint version of this manuscript is available at DOI:10.21203/rs.3.rs-772662/v1 (https://www.researchsquare.com/article/rs-772662/v1).
Keywords: COVID-19, Healthcare worker, Polymerase chain reaction, Reinfection, Relapse
What’s Known
The novel coronavirus pandemic has affected many countries worldwide and has become a public health emergency. Health authorities in Iran have made substantial efforts to control the disease using a variety of approaches. However, since the beginning of the pandemic, healthcare workers have been at a very high risk of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
What’s New
We found that after an episode of SARS-CoV-2 infection, healthcare workers have an estimated 94.8% protection against recurrent infections. The findings of this study provide useful insight into the events that occur after each coronavirus disease 2019 episode, and they may also affect how we formulate appropriate and optimal protective measures.
Introduction
While the absence of a pre-existing immunity prior to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) exposure plays a key role in the rapid spread of coronavirus disease 2019 (COVID-19), the duration and degree of protection acquired after infection of this type, or after vaccination, is also important. In investigating post-infection immunity, certain considerations are critical; identification of measurable surrogate markers and correlates of protection along with providing a proper definition for endpoints, i.e., onward transmission, disease prevention, or death, are among such considerations that arrange for a more precise investigation. 1 - 3
Currently, evidence of SARS-CoV-2 post-infection immunity is on the rise. While several single and small case studies reported instances of COVID-19 reinfection, 4 - 7 two large studies in the United Kingdom (UK) found that protective immunity could extend for approximately 5-6 months. 1 , 8 This suggested that most people develop some levels of immunity after the initial infection, and acquiring secondary and recurring infections was considered to be quite rare.
With healthcare workers (HCWs) being at the epicenter of the COVID-19 pandemic, they are at a higher risk of contracting the disease. Furthermore, numerous studies found that COVID-19 had a negative impact on the wellness of HCWs. 9 - 11 With this in mind, this study was designed to assess reinfection, relapse, and re-positivity of SARS-CoV-2 in HCWs, as well as compare manifested clinical symptoms during each episode of a patient’s infection, based on available information and the undeniable concern regarding the possibility of a recurrence of COVID-19.
Materials and Methods
Study Design and Surveillance System
This cross-sectional population-level observational study was conducted from 20 April 2020 to 18 February 2021 (305 days). The study population included all healthcare personnel working in either public or private hospitals in Fars Province, Southern Iran. The individual-level data regarding infected cases among HCWs, including hospital staff and personnel working in Fars Province, were collected. During this period, Fars Province experienced three surges of COVID-19 cases, including the first surge: 23 February 2020-4 May 2020, the second surge: June 2020-15 August 2020, and the third surge: 28 September 2020-12 December 2020.
These data were recorded from 44 private and public hospitals throughout the Province. The inclusion criteria were all HCWs in Fars Province public or private hospitals. HCWs who were unavailable for evaluation during follow-up were excluded from the study. Individuals were screened and tested based on the presentation of symptoms or in cases of unprotected close contact with confirmed COVID-19 cases, as previously described, 12 , 13 and all personnel were screened at least once, with additional tests given to those who developed COVID-19-related symptoms. Monthly SARS-CoV-2 PCR testing was also performed for personnel with working shifts in COVID-19-specific wards. In addition, if a patient who was not initially diagnosed with COVID-19 and was admitted to a non-COVID ward, was later diagnosed as COVID-19, all personnel in contact with that patient underwent PCR test for SARS-CoV-2. Real-time PCR (RT-PCR) assays were performed in accordance with the protocol established by the World Health Organization (WHO) and previous studies. 12 , 14 - 17 Deidentified data were obtained from the database that was approved by a generic research ethics committee, Health Research Authority, and Confidentiality Advisory Group approvals.
Written informed consent was obtained from all the patients in our study. The purpose of this study was completely explained to the patients, and they were assured that their information would be kept confidential. The present study was conducted in compliance with local regulatory standards, good clinical practice (GCP), and the Declaration of Helsinki. Moreover, the study was approved by the Ethics Committee of Shiraz University of Medical Sciences (code: IR.SUMS.REC.1399.034).
Data Collection Procedure
The patient’s demographic information, signs and symptoms, radiological findings, occupation, and working place, were all documented through contacting the patients and filling out a pre-designed form. Following the recovery, signs and symptoms were also documented. Furthermore, data regarding the total number of HCWs who performed tests, as well as the total number of infected cases in the studied centers within the specified timeline, along with features such as age, sex, and occupation were recorded for making comparisons.
In addition, the patient’s computed tomography (CT) scans were deidentified and evaluated individually by a specialist who was blinded to the patient’s condition and previous/further CT scans.
Definition of Infections, Re-positivity, Relapse, and Reinfections
A COVID-19 episode was defined as (i) having at least one recent major clinical sign of COVID-19, such as fever or chills, febrile flu-like syndrome, dyspnea, anosmia, or dysgeusia; and (ii) a positive SARS-CoV-2 RT-PCR test. Patients were not included if a different diagnosis could explain the recurrence of symptoms.
The definition of reinfection, relapse, and re-positivity of COVID-19 was assigned based on previous reports. 18 , 19
● According to the Centers for Disease Control and Prevention (CDC), re-positivity is defined as a positive PCR for COVID-19 during a 90-day period that most probably represents prolonged shedding rather than reinfection. 19 Positive RT-PCR following negative tests in an asymptomatic patient up to 90 days from the initial episode is referred to as SARS-CoV-2 RT-PCR re-positivity. These cases probably do not represent replicative viruses and do not necessitate isolation. Low viral load is typically associated with re-positivity.
● COVID-19 relapse (also known as ‘recrudescence’ or ‘recurrence’ or ‘reactivation’) is a clinical recurrence of symptoms compatible with COVID-19, accompanied by positive/persisting RT-PCR within 90 days of primary infection, and supported by the absence of epidemiological exposure or another cause of the illness. 18
● In the context of clinical practice, Yahav and others defined reinfection with COVID-19 as the clinical recurrence of symptoms compatible with COVID-19, accompanied by a positive PCR test (Ct<35), more than 90 days after the onset of the primary infection, supported by close-contact exposure or outbreak settings, and no evidence of another cause of infection. 18 In the presence of epidemiological risk factors, such as significant exposure, reinfection should be considered during the first 90 days, if clinical symptoms of the first episode resolved, and two PCR tests were negative before the new episode. For epidemiological purposes, reinfection could be defined as any positive RT-PCR test (Ct<35) more than 90 days from the first episode, regardless of symptoms. Since genotypic assay confirmation is time- and resource-consuming, any case of suspected reinfection should be considered for isolation.
The healthcare workers were classified based on their baseline RT-PCR status. Individuals with only negative RT-PCR results for SARS-CoV-2 were considered to be at risk for infection from the time of their first test until either the end of the study or their first PCR-positive test result, whichever occurred earlier. Regardless of subsequent seroreversion (i.e., any negative PCR tests that occurred later), individuals with a positive PCR were considered to be at risk for infection (or reinfection) from 90 days after their first positive antibody result either until the end of the study or their next PCR-positive test, whichever occurred earlier, regardless of subsequent seroreversion (i.e., any negative PCR tests that occurred later). Patients with a positive PCR during the initial 90 days of our study were considered previously infected unless they had a negative PCR. Regarding the days at risk, the exposed and unexposed periods are periods of follow-up time contributed by individuals with and without the previous infection, respectively. In cases where the status of an individual changed from uninfected to infected, the patient remained in the follow-up while contributing to the previously infected group. The adapted method was based on a population-based study by Hansen and others. 20
To evaluate reinfection, we included all HCWs with a COVID-19 diagnosis either based on positive PCR or clinical assessment during our study period. The date of the first COVID-19 diagnosis in each individual was documented, as well as their follow-up and further PCR or clinical evaluations. Each individual with a diagnosis of COVID-19, whether based on PCR or clinical assessment, was followed up from the time of their first test, regardless of the date or whether they had a positive or negative result, until the end of the present study period. Based on previous reports and evidence, the study and analytic design, as well as the 90-day cut-off, were allocated. 18 - 20 We subcategorized probable reinfections based on symptom status to emphasize those with more evidence and enable comparability with other classifications.
Statistical Analysis
The Data were analyzed using SPSS, version 26 (IBM Corp., Armonk, New York, United States) and Excel software (Microsoft Co., version 8.0). The categorical variables were expressed as frequencies and percentages, and continuous variables as median and interquartile range (IQR) or mean±SD. Basic statistical analysis was performed using Chi square and Fisher’s exact tests. The infection rate was computed as the number of individuals with positive PCR tests divided by the total number of person-days at risk. The number of days at risk for each individual in the sample was determined as the number of days from 90 days after the first positive test until the first positive test or the end of our study period, whichever occurred earlier. In the event of death, follow-up time was censored. This non-informative censoring mechanism essentially assumed a similar infection rate would have been detected among those who died if they had survived, as it was observed among survivors with the same exposure status (whether previously infected or uninfected). Moreover, the rate ratio (RR) and accompanying 95% CI were estimated. The approach of assessing vaccination effectiveness by using observational data was used to compute protection against recurring infections and was calculated as 1–RR. The incidence of PCR-positive infections per at-risk day according to baseline antibody status was also calculated. The calculated proportions were reported using exact 95% CIs (Clopper-Pearson). P<0.05 was considered statistically significant.
Results
From the first tests on 20 April 2020 to 18 February 2021, Iran’s capacity for COVID-19 screening and performing PCR testing for SARS-CoV-2 increased significantly, with approximately a daily average of 45.22 tests among HCWs and 1,947 tests among the general population was performed. By the end of this study period, 13,749 HCWs were tested at least once, accounting for more than two-thirds of the population of 22,195 active HCWs in the Province. Besides, a total of 30,546 PCR tests were performed during the study period. Figure 1 demonstrates the frequency and proportion of positive COVID-19 among HCWs in comparison to the total test performed among healthcare workers.
Figure 1.
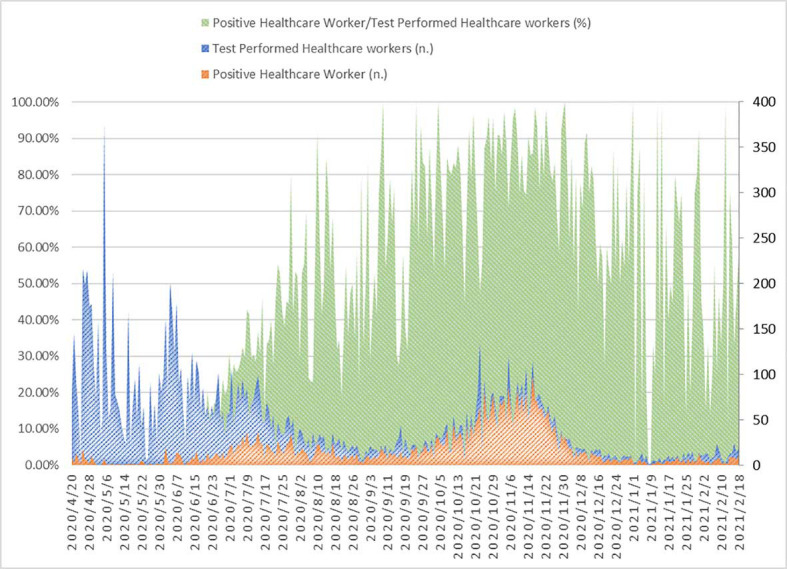
The proportion of healthcare workers that tested positive for coronavirus disease 2019 (COVID-19) compared to the total number of performed tests among healthcare workers. (Primary axis, Percentage); along with the frequency of positive COVID-19 among healthcare workers compared to the total tests performed among healthcare workers. (Secondary axis, Frequency). Green: Positive healthcare worker/test performed healthcare workers (%); Blue: Test performed healthcare workers (n); Orange: Positive healthcare worker (n)
In the present study, there were no cases of mortality. Patients who were diagnosed with COVID-19 remained in follow-up. Based on the database, 5,349 (38.9%) HCWs contracted COVID-19, and 8,400 (61.1%) remained virus-free. During the first 90 days of the study, 943 (17.6%) of the infected patients had a positive PCR test and therefore contributed to the previously infected group. Figure 2 demonstrates the frequency of positive COVID-19 in the general population and healthcare workers, while figure 3 demonstrates the related proportion. It is worth mentioning that in the present study, the ratio of HCWs to the general population was 5-1000 people.
Figure 2.
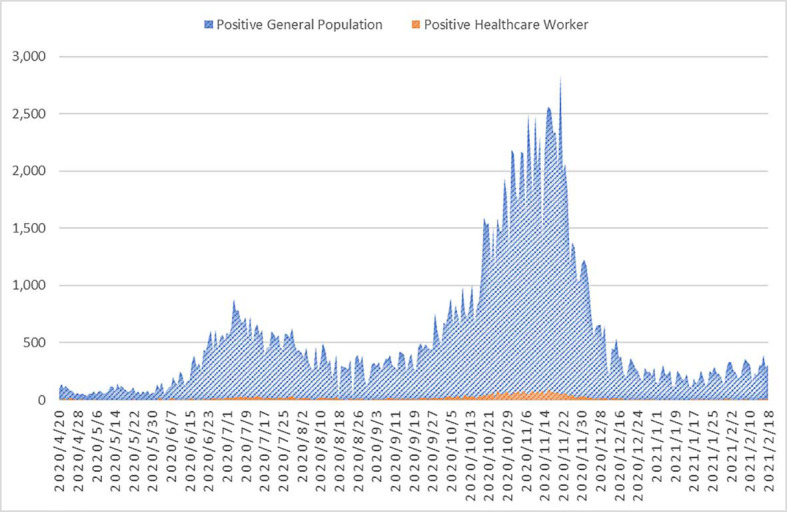
The prevalence of positive coronavirus disease 2019 (COVID-19) among the general population and healthcare workers is shown. Blue: Positive general population; Orange: Positive healthcare worker
Figure 3.
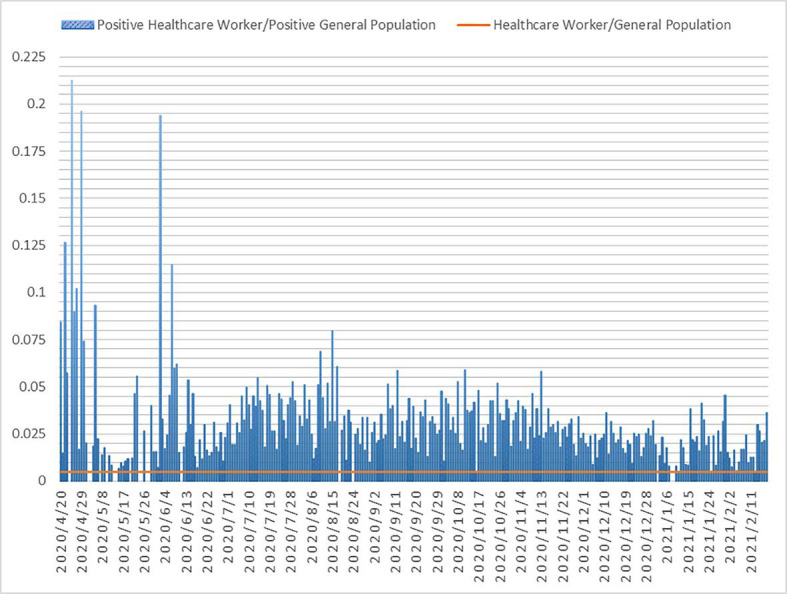
The proportion of positive coronavirus disease 2019 (COVID-19) cases among healthcare workers was compared to the total number of positive cases of COVID-19 in the general population. Blue: Positive healthcare worker/positive general population; Orange: Healthcare worker/general population
141 (2.64%) of the patients in our follow-up had a second episode of COVID-19 diagnosis after the complete alleviation of symptoms and/or a negative SARS-CoV-2 PCR following the treatment of the first episode. The interval between COVID-19 diagnosis was classified as 90 or more or less than 90 days and was labeled as reinfection or reactivation, respectively. Based on the data, 44 (31.2%) cases of reactivation and relapse, and 97 (68.8% of infected and 1.81% of total HCWs) cases of reinfection were observed among 141 diagnosed cases of COVID-19. Table 1 summarizes the overall features of the HCWs with COVID-19, and table 2 compares the first and second episodes of COVID-19 in these patients.
Table 1.
Overall features of the healthcare workers with COVID-19
| Variables | Total | Reinfection | Relapse | Re-positivity | P value* | |
|---|---|---|---|---|---|---|
| Age (y, mean±SD) | 35.00±7.18 | 35.70±7.43 | 33.46±7.95 | 33.43±5.75 | 0.29 | |
| Age group n (%) | 21-30 | 49 (35) | 31 (63.2) | 6 (12.2) | 12 (24.4) | 0.79 |
| 31-40 | 64 (45.7) | 44 (68.7) | 7 (10.9) | 13 (20.3) | ||
| 41-50 | 23 (16.4) | 17 (73.9) | 1 (4.3) | 5 (21.5) | ||
| 51-60 | 4 (2.9) | 3 (75) | 1 (25) | 0 (0) | ||
| Sex n (%) | Male | 53 (37.6) | 36 (67.9) | 6 (11.3) | 11 (20.7) | 0.99 |
| Female | 88 (62.4) | 59 (67.0) | 10 (11.3) | 19 (21.5) | ||
| Occupation n (%) | Specialist and GP | 8 (5.6) | 5 (62.5) | 1 (12.5) | 2 (25) | 0.85 |
| Nurse | 76 (53.1) | 48 (63.15) | 10 (13.15) | 18 (23.68) | ||
| Technician | 16 (11.2) | 12 (75.0) | 1 (6.25) | 3 (18.75) | ||
| Office | 43 (30.1) | 32 (74.41) | 5 (11.62) | 6 (13.95) | ||
| Hospital n (%) | COVID-19 Specific | 46 (31.9) | 24 (52.17) | 7 (15.21) | 15 (32.60) | 0.02 |
| Non-COVID-19 hospital | 98 (68.1) | 73 (74.48) | 10 (10.20) | 15 (15.30) | ||
| Comorbid diseases n (%) | Yes | 25 (17.4) | 17 (68.0) | 3 (12.0) | 5 (20.0) | 0.99 |
| No | 119 (82.6) | 80 (67.22) | 14 (11.76) | 25 (21.0) | ||
Chi square test or Fisher’s exact test.
Re-positivity: Positive RT-PCR following negative tests in an asymptomatic patient up to 90 days from the first episode; Relapse: Clinical recurrence of symptoms compatible with COVID-19 accompanied by positive/ persisting RT-PCR within 90 days of primary infection, and supported by the absence of epidemiological exposure or another cause of the illness; Reinfection: >90 days or <90 days+if clinical symptoms of the first episode resolved, and two PCR tests were negative before the new episode. GP: General physician
Table 2.
Comparison of the first and second episodes of COVID-19 among healthcare workers
| Variable | Frequency (%) | |||
|---|---|---|---|---|
| Reinfection (n=97) | Total | First episode | Second episode | Overlap |
| Symptoms | ||||
| Gastrointestinal | 56 (57.7) | 29 (29.9) | 49 (50.5) | 22 (22.7) |
| Neurological | 81(83.5) | 46 (47.4) | 75 (77.3) | 40 (41.2) |
| Respiratory | 75 (77.3) | 42 (43.3) | 71 (73.2) | 38 (39.2) |
| Asymptomatic | 23 (23.7) | 22 (22.7) | 1 (1) | 0 (0) |
| Flu-like symptom | 96 (99) | 65 (67) | 95 (97.9) | 64 (66) |
| Cardiovascular | 50 (51.5) | 19 (19.6) | 47 (48.5) | 16 (16.5) |
| Others | 14 (14.4) | 8 (8.2) | 8 (8.2) | 2 (2.1) |
| CT and CXR involvement | 49 (50.5) | 26 (27) | 38 (39) | 15 (14) |
| Hospitalization | 14 (14.4) | 8 (8) | 7 (7) | 1 (1) |
| ICU Admission | 3 (3.1) | 0 (0) | 3 (3.1) | 0 (0) |
| O2 therapy | 2 (2) | 2 (2) | 0 (0) | 0 (0) |
| Relapse (n=15) | ||||
| Symptoms | ||||
| Gastrointestinal | 13 (87) | 5 (29.4) | 12 (70.6) | 4 (23.5) |
| Neurological | 15 (100) | 11 (64.7) | 14 (82.4) | 10 (58.8) |
| Respiratory | 13 (87) | 6 (35.3) | 12 (70.6) | 5 (29.4) |
| Asymptomatic | 4 (23.5) | 4 (23.5) | 1 (5.9) | 1 (5.9) |
| Flu-like symptom | 14 (93.3) | 12 (70.6) | 14 (93.3) | 12 (70.6) |
| Cardiovascular | 9 (6) | 4 (23.5) | 8 (47.1) | 3 (17.6) |
| Others | 2 (13.3) | 1 (5.9) | 1 (5.9) | 0 (0) |
| CT and CXR involvement | 12 (8) | 8 (53) | 9 (60) | 5 (33) |
| Hospitalization | 2 (13.3) | 1 (6.7) | 2 (13.3) | 1 (6.7) |
| ICU Admission | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| O2 therapy | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Re-positivity (n=29) | ||||
| Symptoms | ||||
| Gastrointestinal | 17 (58.6) | 8 (26.7) | 14 (46.7) | 5 (16.7) |
| Neurological | 23 (79) | 13 (43.3) | 20 (66.7) | 10 (33.3) |
| Respiratory | 22 (76) | 7 (23.3) | 19 (63.3) | 4 (13.3) |
| Asymptomatic | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Flu-like symptom | 29 (100) | 24 (80) | 27 (90) | 22 (75.8) |
| Cardiovascular | 14 (48.2) | 4 (13.3) | 14 (46.7) | 4 (13.3) |
| Others | 3 (10.3) | 2 (6.7) | 1 (3.3) | 0 (0) |
| CT and CXR involvement | 16 (55.2) | 5 (17) | 14 (48) | 3 (10) |
| Hospitalization | 6 (20.7) | 1 (3.4) | 6 (20.7) | 1 (3.4) |
| ICU Admission | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| O2 therapy | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Overlap: Patients who presented with a similar set of symptoms in both the first and second surge. Flu-like symptoms: Fever, chills, sore throat, sweating, myalgia, severe weakness, rhinorrhea, nasal congestion; Cardiovascular: palpitation, chest pain; Gastrointestinal: Abdominal pain, diarrhea, vomiting, loss of appetite; Neurological: Headache, anosmia, decreased level of consciousness, redness of the eye; Respiratory: Cough, dyspnea. ICU: Intensive care unit; COVID-19: coronavirus disease 2019; CT: Computed tomography; CXR: Chest X-ray.
Based on the patient’s clinical features, repositivity and relapse were classified into one group and compared with reinfection. There was no significant difference between these two groups in terms of total symptoms or each episode of infection (first, second, or overlapping) of patients with COVID-19 reinfection compared with HCWs with relapse/repositivity (P=0.65, 0.44, 0.054, and 0.16, respectively). Similarly, radiologic involvement did not reveal any significant correlation (P=0.44, 0.80, 0.37, and 0.73, respectively). Furthermore, there was no significant difference between the two groups in terms of total hospitalization, frequency of hospitalization during the first and second episode, or hospitalization overlap (P=0.12, 0.46, 0.09, and 0.19, respectively). When comparing the two groups, admission to the intensive care unit (ICU) was similarly a non-significant predictor (P=0.25). As previously established, there was no significant difference in the clinical presentation between HCWs with reinfection and those with relapse/repositivity.
The participants of the present study were followed for a period of 304 days, with 5349 (38.90%) individuals contributing exposed periods, 12,806 (93.14%) contributing unexposed periods, and 4406 contributing both, with a total of 97 reinfections. During the study, 4406 of the 12,806 participants had an infection (contributing 41,571 days), while 8400 remained uninfected (contributing 1,965,106 days). The infection rate during follow-up was estimated based on confirmed new/person days/1000; in which the daily rate of infection was 4.72 for previously infected HCWs, while it was 2.20 for HCWs without previous infection. When individuals who had previously tested positive were compared with those who had previously only tested negative, the RR of infection was 0.052 (95% CI: 0.043-0.064). As shown in table 3, the estimated protection against subsequent SARS-CoV-2 infection was 94.8% (95% CI: 93.6-95.7).
Table 3.
Comparison of infection and reinfection rates and estimated protection against reinfection with severe acute respiratory syndrome coronavirus 2 in healthcare workers
| Period | Population | Confirmed new infection during follow-up | Person days of follow-up | Rate ratio (95% CI) | Estimated protection (95% CI) |
|---|---|---|---|---|---|
| Exposed | 5,349 | 97 | 20,562 | 0.052 (0.043-0.064) | 94.8% (93.6-95.7) |
| Unexposed | 12,806a | 4406 | 2,006,677b | 1 (ref) | - |
The comparison is made based on days of exposure and during follow-ups based on Poisson regression analysis. Exposed periods are periods of follow-up time contributed by individuals with previous infection; unexposed periods are contributed by individuals without a previous infection;
: 4,406 were infected during the study and 8,400 uninfected;
: 41,571 related to the infected group and 1,965,106 related to the uninfected group.
The proportion of SARS-CoV-2 infection among HCWs to the general population during and between surges was evaluated; and the findings are presented in figure 4. During and after the first surge (i.e., 23 February 2020-4 May 2020, and before June 2020), 1,115 and 2301 people were PCR positive, including 75 (6.72%) and 33 (1.43%) HCWs, respectively. During the second surge (i.e., before June 2020-15 August 2020), 32,001 people were PCR-positive, of whom 1075 (3.35%) HCWs were PCR-positive. After the surge (i.e., before 28 September 2020), 461 (3.15%) HCWs were PCR-positive in a total of 14,608 people with positive tests. In the third surge (i.e., 28 September 2020-12 December 2020), 102,294 people were PCR positive, with 3,370 (3.29%) HCWs were included, 14,897 people were positive after the surge (before 18 February 2021), with 335 (1.92%) HCWs were included. Interestingly, there was a significant difference in the proportion of HCWs to the general population between the first surge and the second surge (P<0.001), as well as the first surge and the third surge (P<0.001). However, there was no significant difference between the second and the third surges (P=0.60).
Figure 4.
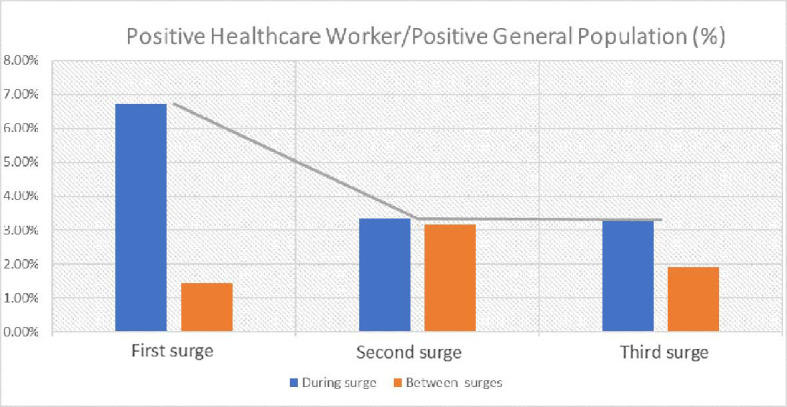
Based on the three COVID-19 surges in Fars Province, Southern Iran, the proportion of coronavirus disease 2019 (COVID-19) among HCWs was compared to the general population. (First surge: 23 February 2020-4 May 2020, Second surge: June 2020-15 August 2020, Third surge: 28 September 2020-12 December 2020), as well as the interval between the surges (between first and second, second and third, and third till the end of the study period, respectively). Blue: During surge; Orange: Between surges
In the present study, to further evaluate the reinfection rate between surges, we calculated the number of cases of reinfection and divided it by the different periods, which included 72, 76, and 78 days for the first, second, and third surges, respectively, and also 27 and 45 for the first two, and second and third intervals, respectively. The number of reinfections during our time period based on the surges included 0, 7, and 82 for the first, second, and third surges, respectively, as well as eight cases of reinfection between the second and third surges. Figure 5 demonstrates the reinfection rates in our study over different time periods.
Figure 5.
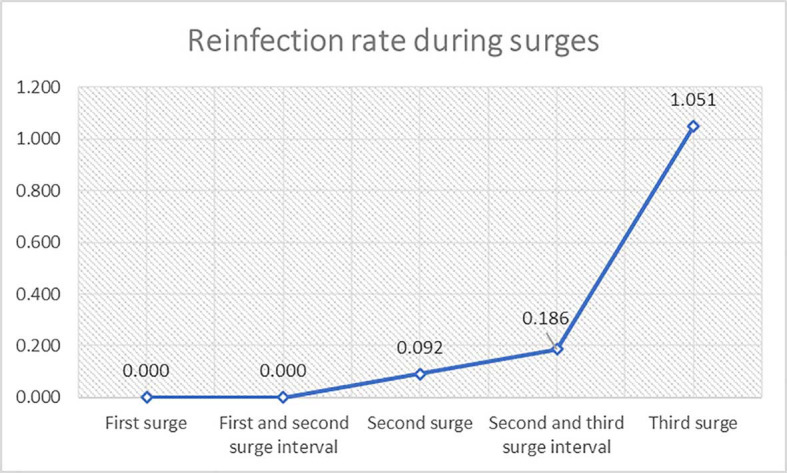
Number of cases of reinfection with severe acute respiratory syndrome coronavirus 2 during each surge and interval among healthcare workers in Fars Province.
It is also worth mentioning that 5,855 HCWs underwent one PCR, 470 had two PCRs, 42 had three PCRs, and three underwent four episodes of PCR.
Discussion
In this study, different episodes of COVID-19 in HCWs using terms provided by recent reports, 18 such as re-positivity, relapse, and reinfection, as appropriate investigative measures were evaluated. Following the main objective of this study, it was found that after an episode of SARS-CoV-2 infection, HCWs had an estimated 94.8% protection against recurring infections. The finding of this study provided useful insight into the events that occur after each COVID-19 episode, and they may also influence how we consider our approaches to providing proper and optimum preventative measures.
Since the beginning of the pandemic, HCWs have been at a very high risk of SARS-CoV-2 infection. A study of Australian HCWs found that the risk of SARS-CoV-2 infection was threefold higher in HCWs than in the general population. 21 While the present study indicated that during the three surges of COVID-19 occurring from 20 April 2020 to 18 February 2021, in Fars Province, 6.72%, 3.35%, and 3.29% of the total population were HCWs, respectively. Similarly, Laursen and others reported positive PCR tests in 4.9% of Danish and Swedish HCWs from June to August 2020, while also suggesting that customer/patient contact was a significant predictor contributing to seropositivity. 22 In a previous study, we reported an infection rate of 5.62% among HCWs in our Province. However, this report was prepared during the early stages of the pandemic, when sufficient efficient protective measures were not implemented. 12
The risk of SARS-CoV-2 infection and/or reinfection was higher in HCWs than in the general population. While a number of seroprevalence studies indicated comparable observations, 23 - 26 high occupational exposure and ease of access to testing equipment (PCR, CT) were regarded to be the two main causes for the discrepancy between this group and the general population. According to an Australian simulation study, 6 to 14 staff members contact an infected patient in the emergency room per day. 27 In addition, Iversen and others found that front-line HCWs were at 1.3 times higher risk of infection than other HCWs. 28 Furthermore, due to higher knowledge about COVID-19 and its symptoms, and also easier access to testing equipment, more tests are performed by HCWs, deeming it less likely for an infection to go unreported. In this regard, Hansen and others conducted a study using Denmark’s national database and found that each HCW had a median of 10 PCR tests (IQR 9–12) performed in the year 2020. 20 While HCWs have higher knowledge of COVID-19 and its symptoms, Erfani and colleagues showed that despite having this awareness, this group had lower levels of positive COVID-19 practice. 29 This can also be a matter of concern in case of reinfection, where a false sense of safety following earlier infection might cause HCWs to underestimate their need for protective measures.
As previously stated, the main finding of the present study suggested that after an episode of SARS-CoV-2 infection, HCWs gain an estimated 94.8% protection against subsequent infections of this type. Our findings supported the findings of numerous previous studies conducted in the US, the UK, Denmark, and Qatar, which reported reinfections were rare, occurring in less than 1% of all COVID-19 cases. 1 , 8 , 20 , 30 , 31 In a study in Denmark, 28,875 individuals contributed to exposed time periods, 138 of them were later diagnosed with reinfections. This study reported an estimated protection of 78.8% among the participants. 20 A research in the UK on 20,000 HCWs, indicated that the risk of SARS-CoV-2 infection was reduced by 83% after 5 months. 8 One explanation for the high estimated rates of protection in HCWs against recurring infections might be that they were at a higher risk of primary infection than the general population, resulting in higher levels of acquired post-infection immunity lasting up to 6 months. 1 , 8 Therefore, it was considered less likely to be prone to reinfections. Nevertheless, further investigation is required to validate this statement.
According to certain research, reinfections may occur at a more severe level due to antibody-dependent enhancements, or the development of other strains of the virus with higher virulence. 7 , 32 A more severe reinfection event may occur as the result of antibody-dependent enhancement, or it may rely on the virulence of the strain and its inoculum. 7 , 32 Furthermore, observations of more severe cases might reflect a bias toward testing symptomatic cases. 33
One of the limitations of the present study was recall bias, in which the participants may or may not recall the specifics of their previous infections. Another limitation was the lack of information on infection rates in the general population, which made it difficult to compare the demographic features of HCWs to those of the general population. Moreover, the short duration of follow-up was considered another limitation of this study. Hansen and others reported little evidence that the degree of protection against recurring infection, as measured by PCR positivity, conferred by the previous infection varied by age group below age 65 years. However, protection against recurring infection was lower in those aged 65 and older than in younger age groups. 20 However, further larger-scale research is required.
Considering that this study was conducted while vaccination among HCWs in Fars Province (Iran) had not yet been initiated, the rate and features of infection and reinfection among vaccinated HCWs could be a subject of interest for further research.
Conclusion
SARS-CoV-2 re-positivity, relapse, and reinfection were quite rare in the HCWs population. Besides, after the first episode of infection, an estimated 94.8% protection against recurring infections was achieved.
Acknowledgment
We would like to thank all the medical staff and healthcare workers for their help during data collection. We express our gratitude to the Statistics & GIS office of Shiraz University of Medical Sciences and its members (managed by Mohammad Habibi, Masoumeh Khosravi, and Mohammadreza Serati) for providing us with the necessary supplementary data to complete our study, and also all the healthcare workers for their assistance in filling out our questionnaire. An academic grant was obtained for the current study (Grant number: 98-01-106-22120; Approved: 11-04-2020)
Authors’ Contribution
R.S. and G.S. designed the study. L.H., M.M., M.A., and P.J. collected the data while R.S., S.S., and N.A. analyzed the data. S.S. and R.S. wrote the first draft of the manuscript while other authors participated in the revisions. All authors have read and approved the final manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflict of Interest
Naeimehossadat Asmarian, as the Editorial Board Member, was not involved in any stage of handling this manuscript. A team of independent experts was formed by the Editorial Board to review the article without her knowledge.
References
- 1.Lumley SF, O’Donnell D, Stoesser NE, Matthews PC, Howarth A, Hatch SB, et al. Antibody Status and Incidence of SARS-CoV-2 Infection in Health Care Workers. N Engl J Med. 2021;384:533–40. doi: 10.1056/NEJMoa2034545. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Plotkin SA. Vaccines: correlates of vaccine-induced immunity. Clin Infect Dis. 2008;47:401–9. doi: 10.1086/589862. [DOI] [PubMed] [Google Scholar]
- 3.Shahriarirad R, Sarkari B. COVID-19: clinical or laboratory diagnosis? A matter of debate. Trop Doct. 2021;51:131–2. doi: 10.1177/0049475520945446. [DOI] [PubMed] [Google Scholar]
- 4.Gupta V, Bhoyar RC, Jain A, Srivastava S, Upadhayay R, Imran M, et al. Asymptomatic Reinfection in 2 Healthcare Workers From India With Genetically Distinct Severe Acute Respiratory Syndrome Coronavirus 2. Clin Infect Dis. 2021;73:e2823–e5. doi: 10.1093/cid/ciaa1451. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee JS, Kim SY, Kim TS, Hong KH, Ryoo NH, Lee J, et al. Evidence of Severe Acute Respiratory Syndrome Coronavirus 2 Reinfection After Recovery from Mild Coronavirus Disease 2019. Clin Infect Dis. 2021;73:e3002–e8. doi: 10.1093/cid/ciaa1421. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.To KK, Hung IF, Ip JD, Chu AW, Chan WM, Tam AR, et al. Coronavirus Disease 2019 (COVID-19) Re-infection by a Phylogenetically Distinct Severe Acute Respiratory Syndrome Coronavirus 2 Strain Confirmed by Whole Genome Sequencing. Clin Infect Dis. 2021;73:e2946–e51. doi: 10.1093/cid/ciaa1275. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tillett RL, Sevinsky JR, Hartley PD, Kerwin H, Crawford N, Gorzalski A, et al. Genomic evidence for reinfection with SARS-CoV-2: a case study. Lancet Infect Dis. 2021;21:52–8. doi: 10.1016/S1473-3099(20)30764-7. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall V, Foulkes S, Charlett A, Atti A, Monk EJ, Simmons R, et al. Do antibody positive healthcare workers have lower SARS-CoV-2 infection rates than antibody negative healthcare workers? Large multi-centre prospective cohort study (the SIREN study), England: June to November 2020. Medrxiv. 2021:2021.01. 13.21249642. doi: 10.1101/2021.01.13.21249642. [DOI] [Google Scholar]
- 9.Shreffler J, Petrey J, Huecker M. The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review. West J Emerg Med. 2020;21:1059–66. doi: 10.5811/westjem.2020.7.48684. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Styra R, Hawryluck L, Mc Geer A, Dimas M, Sheen J, Giacobbe P, et al. Surviving SARS and living through COVID-19: Healthcare worker mental health outcomes and insights for coping. PLoS One. 2021;16:e0258893. doi: 10.1371/journal.pone.0258893. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young KP, Kolcz DL, Ferrand J, O’Sullivan DM, Robinson K. Healthcare Worker Mental Health and Wellbeing During COVID-19: Mid-Pandemic Survey Results. Front Psychol. 2022;13:924913. doi: 10.3389/fpsyg.2022.924913. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sabetian G, Moghadami M, Hashemizadeh Fard Haghighi L, Shahriarirad R, Fallahi MJ, Asmarian N, et al. COVID-19 infection among healthcare workers: a cross-sectional study in southwest Iran. Virol J. 2021;18:58. doi: 10.1186/s12985-021-01532-0. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shahriarirad R, Khodamoradi Z, Erfani A, Hosseinpour H, Ranjbar K, Emami Y, et al. Epidemiological and clinical features of 2019 novel coronavirus diseases (COVID-19) in the South of Iran. BMC Infect Dis. 2020;20:427. doi: 10.1186/s12879-020-05128-x. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Organization WH. Laboratory testing for coronavirus disease 2019 (COVID-19) in suspected human cases: interim guidance, 2 March 2020. Genova: World Health Organization; 2020. [Google Scholar]
- 15.Organization WH. Coronavirus disease (COVID-19) technical guidance: Laboratory testing for 2019-nCoV in humans 31 March 2020. Genova: World Health Organization; 2020. [Google Scholar]
- 16.Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shafiekhani M, Niknam T, Tara SA, Mardani P, Mirzad Jahromi K, Jafarian S, et al. COVID-19 versus applied infection control policies in a Major Transplant Center in Iran. Cost Eff Resour Alloc. 2023;21:17. doi: 10.1186/s12962-023-00427-x. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yahav D, Yelin D, Eckerle I, Eberhardt CS, Wang J, Cao B, et al. Definitions for coronavirus disease 2019 reinfection, relapse and PCR re-positivity. Clin Microbiol Infect. 2021;27:315–8. doi: 10.1016/j.cmi.2020.11.028. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Control CfD, Prevention. Duration of isolation and precautions for adults with COVID-19. Atlanta: Centers for Disease Control Prevention; 2020. [Google Scholar]
- 20.Hansen CH, Michlmayr D, Gubbels SM, Molbak K, Ethelberg S. Assessment of protection against reinfection with SARS-CoV-2 among 4 million PCR-tested individuals in Denmark in 2020: a population-level observational study. Lancet. 2021;397:1204–12. doi: 10.1016/S0140-6736(21)00575-4. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quigley AL, Stone H, Nguyen PY, Chughtai AA, MacIntyre CR. Estimating the burden of COVID-19 on the Australian healthcare workers and health system during the first six months of the pandemic. Int J Nurs Stud. 2021;114:103811. doi: 10.1016/j.ijnurstu.2020.103811. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laursen J, Petersen J, Didriksen M, Iversen K, Ullum H. Prevalence of SARS-CoV-2 IgG/IgM Antibodies among Danish and Swedish Falck Emergency and Non-Emergency Healthcare Workers. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18030923. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rostami A, Sepidarkish M, Leeflang MMG, Riahi SM, Nourollahpour Shiadeh M, Esfandyari S, et al. SARS-CoV-2 seroprevalence worldwide: a systematic review and meta-analysis. Clin Microbiol Infect. 2021;27:331–40. doi: 10.1016/j.cmi.2020.10.020. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poustchi H, Darvishian M, Mohammadi Z, Shayanrad A, Delavari A, Bahadorimonfared A, et al. SARS-CoV-2 antibody seroprevalence in the general population and high-risk occupational groups across 18 cities in Iran: a population-based cross-sectional study. Lancet Infect Dis. 2021;21:473–81. doi: 10.1016/S1473-3099(20)30858-6. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rudberg AS, Havervall S, Manberg A, Jernbom Falk A, Aguilera K, Ng H, et al. SARS-CoV-2 exposure, symptoms and seroprevalence in healthcare workers in Sweden. Nat Commun. 2020;11:5064. doi: 10.1038/s41467-020-18848-0. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Seroprevalence of SARS-CoV-2 antibodies and associated factors in healthcare workers: a systematic review and meta-analysis. J Hosp Infect. 2021;108:120–34. doi: 10.1016/j.jhin.2020.11.008. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitchell R, Ogunremi T, Astrakianakis G, Bryce E, Gervais R, Gravel D, et al. Impact of the 2009 influenza A (H1N1) pandemic on Canadian health care workers: a survey on vaccination, illness, absenteeism, and personal protective equipment. Am J Infect Control. 2012;40:611–6. doi: 10.1016/j.ajic.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 28.Iversen K, Bundgaard H, Hasselbalch RB, Kristensen JH, Nielsen PB, Pries-Heje M, et al. Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. Lancet Infect Dis. 2020;20:1401–8. doi: 10.1016/S1473-3099(20)30589-2. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Erfani A, Shahriarirad R, Ranjbar K, Mirahmadizadeh A, Moghadami M. Knowledge, attitude, and practice toward the novel coronavirus (COVID-19) outbreak: a population-based survey in Iran. Journal of Health Sciences & Surveillance System. 2023;11:578–91. [Google Scholar]
- 30.Harvey RA, Rassen JA, Kabelac CA, Turenne W, Leonard S, Klesh R, et al. Association of SARS-CoV-2 Seropositive Antibody Test With Risk of Future Infection. JAMA Intern Med. 2021;181:672–9. doi: 10.1001/jamainternmed.2021.0366. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abu-Raddad LJ, Chemaitelly H, Coyle P, Malek JA, Ahmed AA, Mohamoud YA, et al. SARS-CoV-2 reinfection in a cohort of 43,000 antibody-positive individuals followed for up to 35 weeks. MedRxiv. 2021 doi: 10.1101/2021.01.15.21249731. [DOI] [Google Scholar]
- 32.Larson D, Brodniak SL, Voegtly LJ, Cer RZ, Glang LA, Malagon FJ, et al. A Case of Early Reinfection With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) . Clin Infect Dis. 2021;73:e2827–e8. doi: 10.1093/cid/ciaa1436. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Iwasaki A. What reinfections mean for COVID-19. Lancet Infect Dis. 2021;21:3–5. doi: 10.1016/S1473-3099(20)30783-0. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]


