Dear Editor
Rheumatic heart disease (RHD) is the leading cause of heart disease worldwide, accounting for 90% of all heart disorders in women of childbearing age, and also accounts for 10% to 15% of maternal mortality. 1 RHD can cause blood flow problems, which can lead to heart failure, arrhythmia, pulmonary hypertension, recurrence of acute rheumatic fever, and an increased risk of thromboembolism; all of which can result in severe morbidity and increased mortality. As a result of improved medical and surgical care, many women experiencing RHD are reaching childbearing age. Therefore, there is an increased incidence of cardiovascular disease during pregnancy and the risk of major adverse effects for both the mother and her infant.
We present a case of a primigravida with a full-term pregnancy and a known case of RHD who experienced an episode of stroke while receiving postoperative care in our intensive care unit.
A 21-year-old Hindu female primigravida with full-term gestation was admitted to the Department of Obstetrics and Gynecology, at Rajendra Institute of Medical Sciences (RIMS), Ranchi, with complaints of vaginal discharge and palpitations. She was a known case of RHD and had mitral valve replacement surgery five years ago. Prior to her pregnancy, she was on treatment with penicillin G, digoxin, Acitrom, and metoprolol. She had experienced a transient ischemic attack (TIA) 15 days ago. There were no prenatal records available for the patient. On examination, she exhibited a systolic murmur on auscultation and an abnormally erratic heart rate. The results of her laboratory tests were normal. Chest X-ray revealed cardiomegaly with a cardiothoracic ratio (CTR) of 0.82 (figure 1). Echocardiography findings indicated chronic RHD with a large left atrium, mild tricuspid regurgitation, and mild pulmonary arterial hypertension with a left ventricular ejection fraction (LVEF) of 55%. Prior to surgery, anticoagulant therapy was discontinued. Induction attempts for normal delivery failed due to non-reassuring fetal heart rate. After receiving prophylaxis treatment for infective endocarditis, she was taken up for emergency cesarean section under general anesthesia. She delivered a healthy baby before being extubated and sent to our intensive care unit (ICU) for postoperative care. Postoperatively, her heart rate ranged between 150-180 bpm. She continued to be treated for infective endocarditis. An electrocardiogram (ECG) revealed atrial fibrillation with a fast ventricular response. We kept her heart rate under control with a 150 mg loading dose of amiodarone (Neon, India), followed by an amiodarone infusion at 1 mg/min for six hours. Following heart rate stabilization with amiodarone injection (150 mg/3mL), digoxin (0.25 mg tablet, GlaxoSmithKline, India) was started and continued along with amiodarone (100 mg tablet, Pfizer, USA). We controlled her pain with tramadol (50 mg/mL, Abbott, India) and paracetamol (1000 mg/100 mL, Neon, India) injections.
Figure 1.
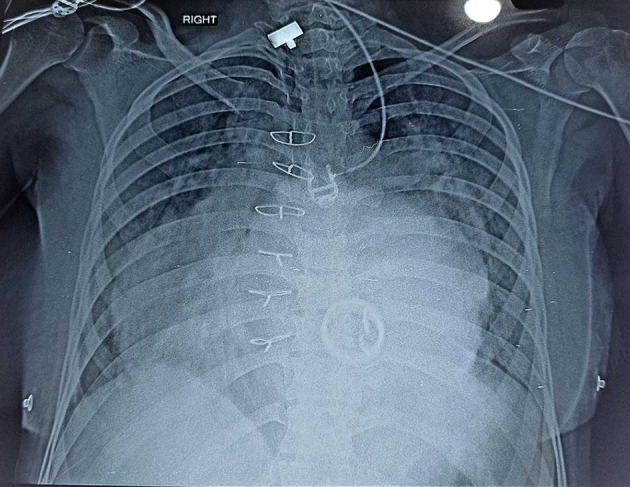
Chest X-ray shows cardiomegaly.
Soon after surgery, following consultation with a cardiologist and obstetrician, penicillin G (400 mg tablet, Abbott, India), 2 mg Acitrom tablet (Abbott, India) once daily, and anticoagulants such as heparin (5000 units, Hipoten, India) thrice daily were started. Although we monitored her coagulation profile, on the third day of the postoperative period, she suddenly became weak on the left side of her body with slurred speech, for which we took immediate neurological consultation. We did a non-contrast computerized tomography (NCCT) of the brain, which revealed a hypodense area involving the right peninsular region, indicating an acute to subacute stroke (figure 2).
Figure 2.
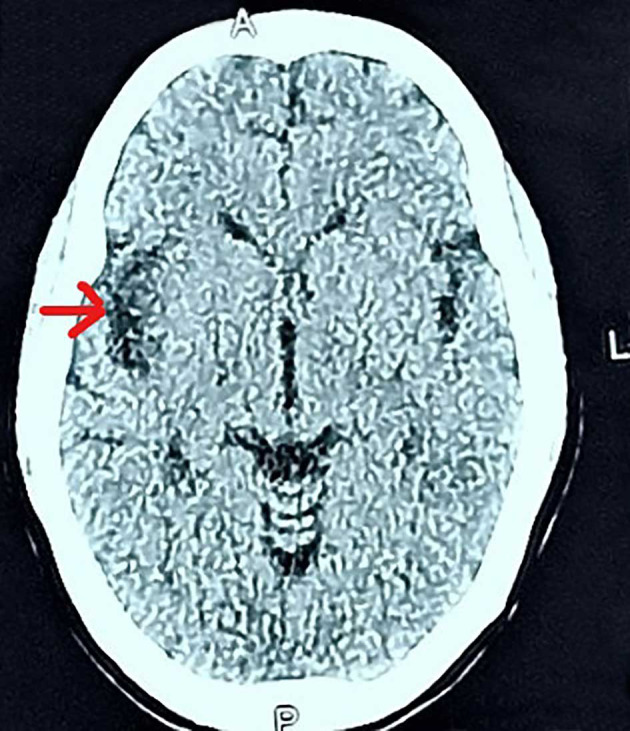
Non-contrast computerized tomography (NCCT) of brain shows a hypodense area in the right peninsular region, which is marked with an arrow.
Following a review session with a cardiologist, the Acitrom dose was increased to 3 mg, and enoxaparin (40 mg/0.4 mL injection, Sanofi, India) was started instead of heparin to keep the target PT INR 2.5. After the incident, she recovered spontaneously on her own. Following consultation with neurologist, cardiologist, and obstetrician; digoxin (0.25 mg tablet), metoprolol (50 mg tablet), and amiodarone (100 mg tablet, Sun Pharma, India) were continued for her. She was discharged after monitoring for 5 days, during which her recovery was uneventful. Written informed consent for the publication of her case was obtained from the patient.
Cardioembolic stroke is rare during pregnancy (incidence 12.2 per 100,000 pregnancies), yet it can be fatal to both the mother and the fetus. 2 According to statistics reported before 2020, the proportion of RHD in patients with ischemic stroke ranged from 3.4% to 23.2% in Asia, and the death rate for RHD-related stroke ranged from 8.5% to 47.4% over the past three decades. 3
This case highlighted the importance of considering cardioembolic stroke in pregnant women with acute neurological symptoms, particularly those with risk factors such as atrial fibrillation or abnormal cardiac structure. Managing the care of pregnant patients with RHD can be challenging, as the risks of anticoagulant therapy to prevent thromboembolism must be balanced against the risk of bleeding during pregnancy and delivery. In most cases, close monitoring and individualized management plans are typically required. Postpartum care is also essential in managing pregnant patients with RHD who have suffered a stroke. Close monitoring for complications, such as bleeding or recurrent stroke, is typically required.
In the present case, she first developed atrial fibrillation, which required multiple anti-arrhythmic medications, including amiodarone infusion. Second, we provided adequate pain management to prevent stress-induced hemodynamic instability. Third, we continuously monitored the hemodynamic stability with the aid of an ultrasound machine and HemoSphere advanced monitor (Edwards Lifesciences, Irvine, CA, USA). The fourth and most crucial complication was the patient’s cardioembolic stroke on the third day. To reduce the risk of thromboembolism, anticoagulation therapy was resumed soon after delivery.
Early diagnosis and management of cardioembolic stroke is critical for reducing morbidity and mortality in both the mother and the fetus. Overall, early interdisciplinary effort is required to manage these patients. The aim is to provide individualized care while weighing the advantages and disadvantages of different treatment modalities to optimize outcomes for both the mother and her unborn baby.
Acknowledgments
Authors’ Contribution
D.S, S.B, B.R, A.M, PK.B, A.J: Data collection, patient management, study design, drafting and reviewing the manuscript; All authors have read and approved the final manuscript and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflict of Interest:
None declared.
References
- 1.Nanna M, Stergiopoulos K. Pregnancy complicated by valvular heart disease: an update. J Am Heart Assoc. 2014;3:e000712. doi: 10.1161/JAHA.113.000712. [ PMC Free Article ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Camargo EC, Feske SK, Singhal AB. Stroke in Pregnancy: An Update. Neurol Clin. 2019;37:131–48. doi: 10.1016/j.ncl.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Wang D, Liu M, Hao Z, Tao W, Lin S, Zhang S, et al. Features of acute ischemic stroke with rheumatic heart disease in a hospitalized Chinese population. Stroke. 2012;43:2853–7. doi: 10.1161/STROKEAHA.112.670893. [DOI] [PubMed] [Google Scholar]


