This systematic review and meta-analysis evaluates the complication, emergency department, and hospital readmission rates associated with telemedicine vs conventional care in patients who underwent abdominal surgery.
Key Points
Question
Can perioperative telemedicine reduce the incidence of adverse events in abdominal surgery?
Findings
In this systematic review and meta-analysis of 19 randomized trials and nonrandomized studies with 10 536 patients, significant reduction in readmission rates and emergency department visits was found with telemedicine interventions compared with conventional care after abdominal surgery. There was no difference in complication rates between patients in telehealth and conventional care groups.
Meaning
Findings of this study suggest that perioperative telemedicine may play a role in reduced incidence of readmissions and emergency department visits after abdominal surgery; however, further research is needed to elucidate specific mechanisms of action.
Abstract
Importance
Over the past 2 decades, several digital technology applications have been used to improve clinical outcomes after abdominal surgery. The extent to which these telemedicine interventions are associated with improved patient safety outcomes has not been assessed in systematic and meta-analytic reviews.
Objective
To estimate the implications of telemedicine interventions for complication and readmission rates in a population of patients with abdominal surgery.
Data Sources
PubMed, Cochrane Library, and Web of Science databases were queried to identify relevant randomized clinical trials (RCTs) and nonrandomized studies published from inception through February 2023 that compared perioperative telemedicine interventions with conventional care and reported at least 1 patient safety outcome.
Study Selection
Two reviewers independently screened the titles and abstracts to exclude irrelevant studies as well as assessed the full-text articles for eligibility. After exclusions, 11 RCTs and 8 cohort studies were included in the systematic review and meta-analysis and 7 were included in the narrative review.
Data Extraction and Synthesis
Data were extracted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guideline and assessed for risk of bias by 2 reviewers. Meta-analytic estimates were obtained in random-effects models.
Main Outcomes and Measures
Number of complications, emergency department (ED) visits, and readmissions.
Results
A total of 19 studies (11 RCTs and 8 cohort studies) with 10 536 patients were included. The pooled risk ratio (RR) estimates associated with ED visits (RR, 0.78; 95% CI, 0.65-0.94) and readmissions (RR, 0.67; 95% CI, 0.58-0.78) favored the telemedicine group. There was no significant difference in the risk of complications between patients in the telemedicine and conventional care groups (RR, 1.05; 95% CI, 0.77-1.43).
Conclusions and Relevance
Findings of this systematic review and meta-analysis suggest that perioperative telehealth interventions are associated with reduced risk of readmissions and ED visits after abdominal surgery. However, the mechanisms of action for specific types of abdominal surgery are still largely unknown and warrant further research.
Introduction
The past decade has been marked by the widespread use of digital health technologies. Limited access to health care resources, mobility restrictions of individuals, and disruptions in the provision of health services during pandemics have encouraged the adoption of telehealth technologies in previously limited areas, such as surgery.1 The diversity of digital health interventions and the variety of applications in surgery make an overall assessment of benefits and effectiveness difficult. Most available studies have focused on assessing patient satisfaction and clinician experience as well as time and cost savings related to telemedicine interventions.2,3
Abdominal and pelvic surgery (including colorectal and gynecological) is one of the most common types of surgery, with its own specific complications and recovery conditions. Due to its potential to reduce the delay between complication onset and medical intervention, telemedicine may facilitate the early detection of postoperative complications by providing options for patient-clinician communication and remote patient monitoring.2,3 In general, telemedicine may be used as an instrument of patient safety that can identify and prevent health hazards from the provision of health services.4 Although patient safety can be assessed with different indicators, the most frequent indicators may include complications, readmissions, emergency department (ED) visits, nosocomial infections, and adverse events.
Despite the increasing number of telemedicine interventions in abdominal surgery, to our knowledge, the implications of digital health interventions for patient safety in abdominal surgery have not been quantitatively assessed. Therefore, in this systematic review and meta-analysis, we aimed to estimate the implications of telemedicine interventions for complication and readmission rates in a population of patients with abdominal surgery.
Methods
The review protocol was registered in PROSPERO (identifier: CRD42022338147). We followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.
Eligibility Criteria
Articles were included in this meta-analysis if they met the following inclusion criteria: (1) randomized clinical trials (RCTs), nonrandomized controlled trials, and observational (cohort and case-control) studies; (2) adult patients with abdominal and pelvic surgical procedures (including colorectal, gynecological, and urological), without sex or any age restrictions; (3) digital health interventions provided in the preoperative and postoperative periods, including remote consultations via video or telephone call, digital follow-up and recovery programs delivered via a mobile application, and remote monitoring of health status; and (4) at least 1 of the reported primary outcomes related to patient safety, including complications and adverse events, readmissions, and ED visits. The exclusion criteria were (1) studies without a comparable group; (2) other types of digital health interventions without patient-clinician communication; (3) studies reporting less than 2 outcomes measurement; and (4) reviews, commentaries, letters, editorials, case reports, and non-peer-reviewed sources.
Following the World Health Organization5 classification, we categorized the studies into 4 types of interventions: health care consultations between patient and clinician, remote monitoring of patient health or diagnostic data by clinician, transmission of medical data to clinician, and case management consultations between clinicians.
Search Strategy and Selection Process
A systematic literature search was conducted of MEDLINE (via PubMed and Ovid), Cochrane Library, and Web of Science databases for all articles published up to February 2, 2023. The search strategy was based on types of telemedicine interventions, outcomes, and population. The terms telemedicine, patient safety, and surgery were the basic concepts used to specify the query strings for the databases. Keywords and MeSH (Medical Subject Headings) terms were used to refine the database queries. A search strategy developed for PubMed is provided in the eAppendix in Supplement 1. This protocol was applied to all database searches, with some modifications to search terms and operators.
Two of us (A.G., M.F.) independently screened the titles and abstracts obtained from the searches to exclude irrelevant studies. After the interrater reliability was deemed appropriate (κ = 0.998), 2 of us (A.G., M.F.) separately and independently assessed the full-text articles for eligibility against the predetermined inclusion criteria. Any disagreements were resolved by consensus, in consultation with another reviewer (D.M.). The database queries did not yield records that had to be excluded for language reasons, although 1 of the selection criteria was publication language (only articles published in English, German, French, Italian, Spanish, Portuguese, Russian, and Ukrainian were included).
Data Extraction and Quality Assessment
Data were extracted using a standardized extraction form. This form sought information on publication details (eg, title), study design and population, participant characteristics, description of intervention, and outcomes.
Two of us (A.G., M.F.) independently assessed risk of bias using validated tools, and discrepancies were resolved by consensus and involved a third reviewer if necessary. The Physiotherapy Evidence Database (PEDro) Scale was used for the risk-of-bias assessment of RCTs. The PEDro Scale is based on 11 criteria, which are scored ranging from 0 to 10, with higher values indicating higher quality (less risk of bias).6 Risk of bias of nonrandomized controlled trials, cohort studies, and case-control studies was assessed using the Cochrane Risk-of-Bias in Non-randomized Studies of Intervention (ROBINS-I) tool.7 The ROBINS-I tool includes 7 domains (confounding, selection, classification of interventions, deviations from intended interventions, missing data, outcome measurement, and reporting) that are assessed as having low, moderate, high, or critical risk of bias.
Outcome Measures and Data Synthesis
Primary outcomes were the number of postoperative complications, 30-day ED visits, and 30-day hospital readmissions. Secondary outcomes were patient satisfaction with digital health interventions and hospital length of stay (LOS), which was used as a proxy for the occurrence of adverse events.
Statistical Analysis
For the primary outcomes, which were reported as contingency tables, risk ratios (RRs) comparing the telemedicine and conventional care groups were calculated. For LOS (a secondary outcome), standardized mean differences (SMDs) were calculated between the treatment and control groups. The SMDs were used instead of the raw differences due to variations in measurement scales across studies. The calculation and interpretation of SMD are described in the eMethods in Supplement 1. The meta-analytic RR estimates and their corresponding 95% CIs were obtained with a random-effects model and Mantel-Haenszel test. Der Simonian-Laird estimates were used as the default option of the RevMan software (Cochrane Collaboration) (eMethods in Supplement 1). The meta-analytic estimates were stratified by study design (RCTs vs non-RCTs) to assess the magnitude of potential biases due to nonrandomization of participants. In addition, subgroup analyses by type of telemedicine intervention were performed for primary outcomes. Heterogeneity of effect sizes was assessed using the I2 statistic. The number needed to treat (NNT) was estimated using the formulae described by McQuay et al.8
The level of significance for all tests was set to P = .05. Analyses were performed using RevMan v.5.4 (Cochrane Collaboration) and the R environment (R Project for Statistical Computing). The results concerning patient satisfaction (a secondary outcome) were summarized in narrative form because the measures in the original studies were not comparable and, therefore, not amenable to a quantitative analysis.
Results
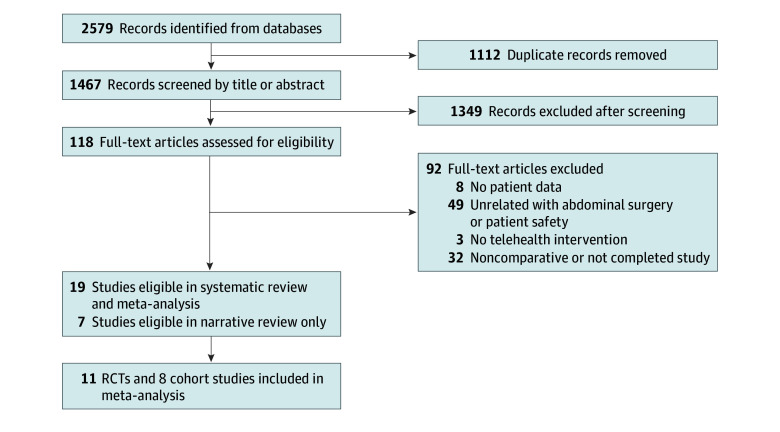
The search and selection flowchart is presented in Figure 1. A total of 2579 records were identified in the initial search, and 1467 records remained after removal of duplicates. Of the 118 articles assessed for eligibility, 19 were eligible for the systematic review and meta-analysis and another 7 for the narrative review only. Finally, 11 RCTs9,10,11,12,13,14,15,16,17,18,19,20 and 8 cohort studies21,22,23,24,25,26,27,28 were included in this meta-analysis.
Figure 1. PRISMA Flow Diagram of Study Search and Selection.
RCT indicates randomized clinical trial.
Study Characteristics
The selected studies were published between 2013 and 2023 (Table). Fourteen (73.7%) of these studies were from North America (US and Canada),10,12,14,15,16,17,18,21,23,24,25,26,27,28 and the other 5 (26.3%) were from the UK, Australia, the Netherlands, Sweden, and Spain.9,11,13,19,20,22 The studies selected for the current meta-analysis included a total of 10 536 patients (3885 in the RCTs and 6651 in the nonrandomized cohort studies). In the RCTs, 1946 patients were in the telemedicine group and 1939 were in the conventional care group. The non-randomized studies included 3376 patients in the telemedicine cohort and 3275 in the conventional care group. Abdominal surgical procedures were represented in 7 studies (36.8%),9,19,22,24,25,26,28 7 studies (36.8%) included patients who underwent colorectal procedures,10,15,17,20,21,23,27 3 studies (15.8%) recruited patients who underwent gynecological procedures,12,14,18 and 2 studies (10.5%) included patients with different types of surgical procedures.11,16
Table. Studies Included in the Meta-Analysis.
| Source | Study design | Sample size (n = telemedicine group; conventional care group) | Type of intervention | Description of intervention | Type of surgery |
|---|---|---|---|---|---|
| Bednarski et al,10 2019 | RCT | 30 (14; 16) | Mobile application for follow-up or recovery program | Monitoring of recovery via mobile application messaging with surgical team and videoconferencing, in addition to regular ERAS program | Colorectal |
| Cremades et al,9 2020 | RCT | 200 (100; 100) | Telemedicine consultation | Follow-up via video call, with clinical and wound condition assessed and pathology discussed | Abdominal |
| Dahlberg et al,11 2017 and Jaensson et al,13 2017 | RCT | 997 (494; 503) | Mobile application for follow-up or recovery program | Smartphone application assessment of postoperative recovery using the symptoms questionnaire system, with daily reminder and contact with surgery team via the application | Different types |
| Halder et al,12 2022 | RCT | 143 (70; 73) | Telemedicine consultation | Preoperative scripted telephone call, based on the enhanced-recovery program | Gynecological |
| Lee et al,14 2021 | RCT | 54 (27; 27) | Telemedicine consultation | Virtual video follow-up visits at 3-4 d after discharge and 30 postoperative days | Gynecological |
| Mata et al,15 2020 | RCT | 100 (50; 47) | Mobile application for follow-up or recovery program | Mobile application for postoperative education and self-assessment of recovery; the application included 3 sections: milestones checklist, daily clinical questionnaire, and education | Colorectal |
| McGilion et al,16 2021 | RCT | 905 (451; 454) | Telemetry or telediagnostic | Remote monitoring technology measurement of biophysical variables and completion of daily recovery survey; participants interacted daily with a nurse virtually through the tablet | Different types |
| Pooni et al,17 2022 | RCT | 253 (128; 125) | Mobile application for follow-up or recovery program | Postdischarge monitoring with the application, which included daily health check-up questions, image-uploading module for wound and stoma photos, and self-management postoperative recommendations | Colorectal |
| Thompson et al,18 2019 | RCT | 103 (52; 51) | Telemedicine consultation | Scripted telephone follow-up to review specific assessment criteria, including evaluation of pain, bowel and bladder function, and return to daily activities | Gynecological |
| van der Meij et al,19 2018 | RCT | 344 (173; 171) | Mobile application for follow-up or recovery program | Mobile application consisting of a personalized recovery plan, educational information, activity tracking, and recovery monitoring, with functions of active feedback and e-consultation | Abdominal |
| Young et al,20 2013 | RCT | 756 (387; 369) | Telemedicine consultation | Five scheduled, structured telephone calls on days 3 and 10 and then at months 1, 3, and 6 after hospital discharge; included 22 standardized screening questions | Colorectal |
| Borsuk et al,21 2019 | Nonrandomized | 281 (168; 113) | Mobile application for follow-up or recovery program | Mobile application for home prerehabilitation or rehabilitation and monitoring, including text messages with recommendations to recovery, patient-reported outcomes collection, and contacts with treatment team | Colorectal |
| Daliya et al,22 2022 | Nonrandomized | 510 (210; 300) | Telemedicine consultation | Digital follow-up via videoconferencing or telephone follow-up | Abdominal |
| Eustache et al,23 2023 | Nonrandomized | 350 (94; 256) | Mobile application for follow-up or recovery program | Mobile application with patient education material, daily questionnaires assessing postdischarge recovery, and patient-clinician chat function | Colorectal |
| Liu et al,24 2021 | Nonrandomized | 2009 (1688; 321) | Telemedicine consultation | Follow-up telephone call after inguinal hernia surgery | Abdominal |
| Lovasik et al,25 2020 | Nonrandomized | 528 (217; 311) | Telemedicine consultation | Follow-up telephone call, with additional call for high-risk patients | Abdominal |
| Nikolian et al,26 2018 | Nonrandomized | 718 (233; 485) | Telemedicine consultation | Secure videoconferencing on cellular phone, tablet, or laptop, using the virtual medical platform | Abdominal |
| Stapler et al,27 2022 | Nonrandomized | 1720 (668; 1052) | Mobile application for follow-up or recovery program | Extended recovery program included postoperative monitoring using a mobile application, with health status and wound care questionnaire and physical therapy and nutrition advice | Colorectal |
| Uppal et al,28 2022 | Nonrandomized | 535 (98; 437) | Telemedicine consultation | Virtual, video, or audio contact for the first follow-up visit after hospital discharge | Abdominal |
Abbreviations: ERAS, Enhanced Recovery After Surgery; RCT, randomized clinical trial.
The risk-of-bias assessment of the RCTs using the PEDro Scale revealed that the risk of bias was mainly due to the inability to blind participants, therapists, and assessors. The main source of the risk of bias in non-randomized studies assessed with the ROBINS-I tool was the selection of participants given that most cohort studies were retrospective and the selection process was not fully clarified. Another common source of potential bias was missing data due to the authors’ reported inability to completely follow up patients’ visits to other clinicians.22,24,25,26,28 The risk-of-bias assessment results are provided in eFigures 1 and 2 in Supplement 1.
Primary Outcomes
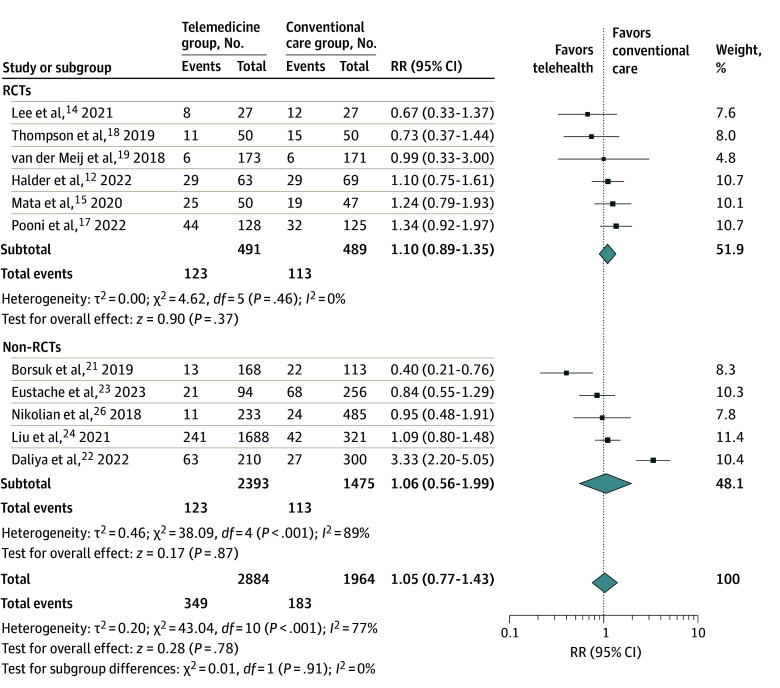
Eleven of 19 studies (57.9%) reported the occurrence of complications as an outcome.12,14,15,17,18,19,21,22,23,24,26 There was no significant difference in complication rate between the telemedicine group and the conventional care group (16.4% vs 15.1%). The meta-analytic RR estimate (Figure 2) did not suggest any differences between the 2 groups (RR, 1.05; 95% CI, 0.77-1.43). The heterogeneity among these studies for complication rate was large (I2 = 77%). Subgroup analysis comparing RCTs vs non-randomized studies did not suggest any differences in meta-analytic RR estimates (1.10 [95% CI, 0.89-1.35] vs 1.06 [95% CI, 0.56-1.99]).
Figure 2. Complications of All Studies and Subgroups.
Error bars represent 95% CIs, square sizes represent the weight of the study, and diamonds represent the pooled risk ratio (RR) estimate (the width of the diamond indicates the 95% CI of the pooled RR). RCT indicates randomized clinical trial.
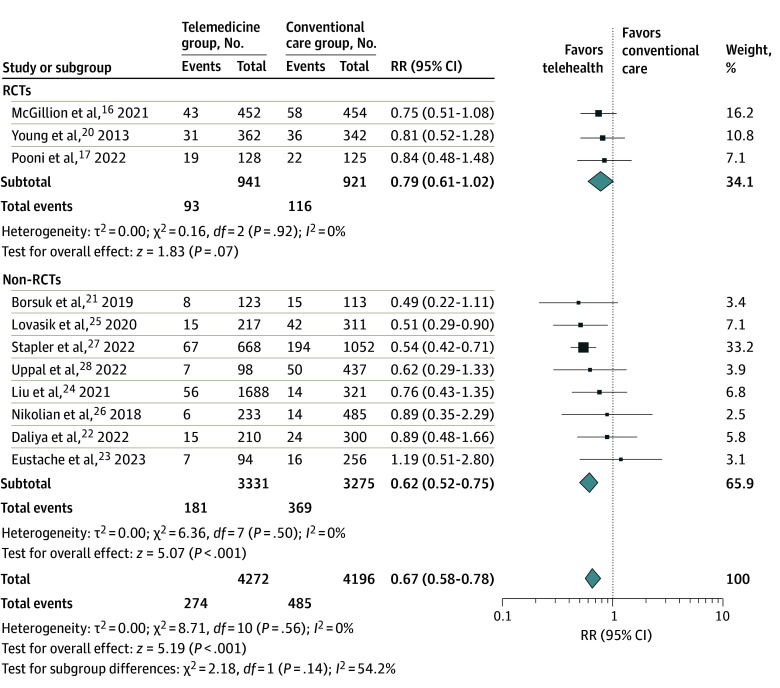
Rates of hospital readmissions were reported in 11 studies (Figure 3).16,17,20,21,22,23,24,25,26,27,28 A lower incidence of readmissions was observed in the telemedicine group (RR, 0.67; 95% CI, 0.58-0.78) with low heterogeneity (I2 = 0%). However, whereas differences in the RCT subgroup were not substantial (RR, 0.79; 95% CI, 0.61-1.02), the meta-analytic RR estimates obtained from nonrandomized studies revealed a significant reduction in readmission rates (RR, 0.62; 95% CI, 0.52-0.75). Nonetheless, in an additional moderation analysis, the differences between RCTs and non-randomized studies were not significant, suggesting a similar direction in associations.
Figure 3. Readmissions of All Studies and Subgroups.
Error bars represent 95% CIs, square sizes represent the weight of the study, and diamonds represent the pooled risk ratio (RR) estimate (the width of the diamond indicates the 95% CI of the pooled RR). RCT indicates randomized clinical trial.
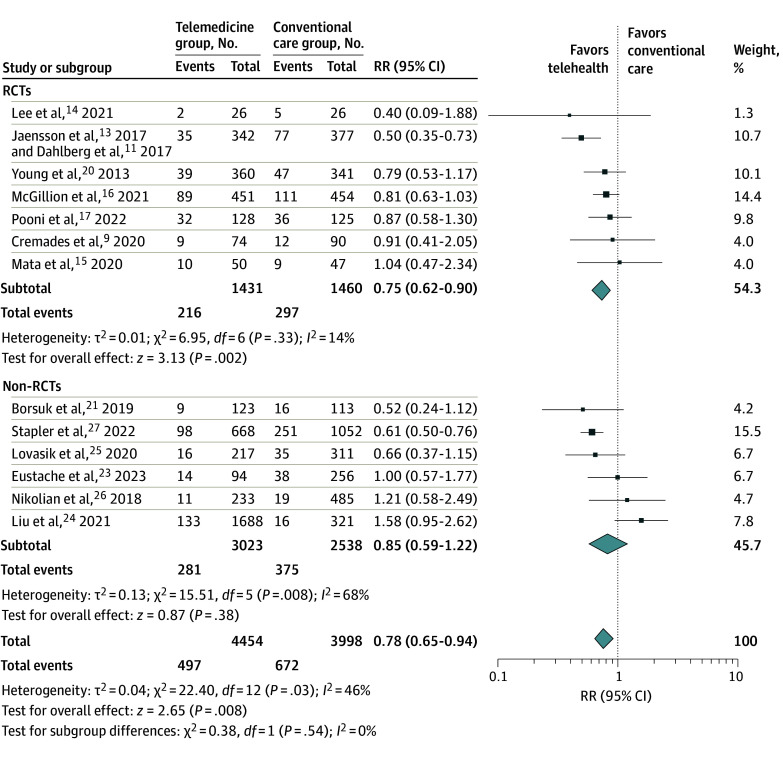
Seven RCTs and 6 nonrandomized cohort studies reported appropriate data on ED visits (Figure 4).9,11,14,15,16,17,20,21,23,24,25,26,27 The pooled estimate for all studies revealed a decrease in the number of ED visits in the telemedicine group (RR, 0.78; 95% CI, 0.65-0.94). This result showed moderate heterogeneity (I2 = 46%). Analysis of the RCTs also demonstrated a reduction in ED visits in favor of the telemedicine group (RR, 0.75; 95% CI, 0.62-0.90).
Figure 4. Emergency Department Visits of All Studies and Subgroups.
Error bars represent 95% CIs, square sizes represent the weight of the study, and diamonds represent the pooled risk ratio (RR) estimate (the width of the diamond indicates the 95% CI of the pooled RR). RCT indicates randomized clinical trial.
Subgroup analysis for RCTs with NNT calculations showed a small to medium effect size (NNT = 37 [95% CI, –640 to 17] for avoiding readmissions; NNT = 19 [95% CI, 12-40] for avoiding ED visits) in comparing telemedicine interventions with conventional care (eTable 1 in Supplement 1). Negative NNT values corresponded to the number needed to harm.
Secondary Outcomes
Nine studies reported LOS as an outcome,10,14,15,16,17,21,23,26,28 of which 7 presented data appropriate for meta-analytic synthesis (eFigure 3 in Supplement 1). Five studies reported a decrease in LOS in the telemedicine group.10,21,23,26,28 Two of these studies focused primarily on reducing LOS with an enhanced postoperative recovery and monitoring program.10,21 The pooled estimate of the SMD showed a significant shortening of LOS in the telehealth group (SMD, −0.43 [95% CI, −0.65 to −0.22] days). The overall heterogeneity was high (I2 = 74%).
Fourteen studies presented different types of patient satisfaction measures.9,10,12,14,15,17,18,19,20,23,26,29,30,31 Patient satisfaction data are available in eTable 2 in Supplement 1. Overall, the studies reported high levels of patient compliance and satisfaction with telehealth technologies in perioperative management. Patient feedback was related to overall satisfaction with treatment, discharge, and follow-up after surgery as well as to usability and satisfaction with the telemedicine application. Most studies compared patient satisfaction in the telemedicine intervention and conventional care groups. Three of them showed significant advantages with telemedicine over conventional care,12,17,31 while the others found no difference between the groups. Based on qualitative feedback and patient comments, the most frequently cited advantages were ease of contact with the surgical team and cost and time savings from traveling to the site for follow-up.14,23,26 Furthermore, in some instances, patients were willing to recommend telehealth as an alternative to the traditional approach.23,26,31
Types of Interventions
We found 3 types of interventions in the included studies: (1) telemedicine consultations via video call9,14,22,25,26,28 or scripted telephone call,18,20,24,25 which were conducted in 10 studies; (2) perioperative recovery program, patient education, follow-up, and health monitoring delivered via a mobile application, which was used in 8 studies10,11,15,17,19,21,23,27; and (3) remote monitoring of physiological variables using a telemedicine device, which was conducted in 1 study.16 Subgroup analysis by intervention type was performed to assess the change in primary outcomes associated with methodological diversity (eTable 3 in Supplement 1). The results suggest that telemedicine consultation and use of mobile applications may play a role in reduced rates of readmission; whereas for ED visits, only mobile applications seemed to be associated with lower rates.
Discussion
This systematic review and meta-analysis included 19 studies that assessed the implications of telemedicine interventions for complication and readmission rates in patients who underwent abdominal surgery. There was no difference in complication rates in favor of telemedicine intervention compared with conventional care, and heterogeneity for this outcome was high. The pooled RR estimates showed a reduction in readmission rates and ED visits in the telemedicine group compared with conventional care group, with low to moderate heterogeneity.
Most telemedicine interventions consisted of consultations via video calls9,14,22,25,26,28; scripted telephone calls18,20,24,25; and mobile applications11,15,17,19,21,23,27 of varying functionality, including messaging, videoconferencing, perioperative education, monitoring of symptoms and recovery, and activity tracking. Thus, the most common feature of digital health interventions seemed to be the facilitation of communication between patients and health professionals with different levels of information, including clinical parameters (symptoms monitoring), feedback (face-to-face consultation and messaging), and knowledge transmission (education and training). Given the multifaceted character of the technologies implemented in the telemedicine interventions themselves and the lack of information on how each facet may be associated with patient safety outcomes, surgery types, and patient characteristics, it is not feasible to draw a conclusion on how digital health technologies play a role in the reduced burden of complications in abdominal surgery.
For instance, the reduction in the number of readmissions and ED visits may be associated with patients’ or clinicians’ assessment of the improved severity of symptoms either via the messaging system, video calls, postoperative education, or all of those components together. A similar difficulty can arise concerning telemedicine’s associated complication rates, since the expected reduction in the number of complications may be difficult to detect due to substantial heterogeneity in assessment methods and patient populations. Thus, Daliya et al22 found more complications in their telemedicine care group than the no follow-up group. However, on closer inspection, the increased complication rate was associated with more accurate and frequent recording of even minor events, which are not reported by patients in traditional postoperative follow-up. This finding seemed to point out that digital technology for reporting complications (eg, mobile applications and telemedicine consultations) is associated with increased probability of reporting less severe complications compared with nondigital procedures. Given the lack of a detailed qualification of the severity of complications in the included studies, the findings from the present study suggest that the complex interactions among the reporting behavior of patients, degree of seriousness and severity of complications, and functionality of digital technologies need further scrutiny.
The role of telehealth in the decreased incidence of complications may depend on the selected patient populations. For example, if the overall rate of complications is usually low after a minor 1-day procedure, such as cholecystectomy or hernioplasty, the outcome of telemedicine would also be difficult to observe.32 On the other hand, after major surgery, such as multivisceral and hepatopancreatobiliary surgical procedures, the rate of complications requiring hospitalization is usually higher and may offset the potential effectiveness of telehealth interventions. However, a retrospective study by Lovasik et al25 of a single hepatopancreatobiliary surgeon’s practice showed a 76% reduction in 30-day readmission rates after implementation of a program for perioperative patient education and structured telephone symptom assessment after discharge. Lovasik et al25 attributed this outcome to early detection and reduction in avoidable readmissions.
Additionally, the considerable heterogeneity in the design of telemedicine interventions (eg, services delivered by telephone or video call and by mobile applications with different functionalities) impedes a more detailed analysis of the most effective types of telemedicine services. Although some telehealth interventions may focus only on postoperative follow-up and detection of complications, others may also include patient education materials and individualized recovery programs. These factors can affect the patient’s experience of use and, consequently, their adherence to treatment and the effectiveness of the intervention.
The implications of telemedicine for LOS may be associated with clinicians discharging patients earlier based on the ability to monitor patients’ postdischarge health status using a web application, along with the potential for patients to use the application to report developing symptoms. However, given that some telehealth interventions started before admission and some after discharge, further research is needed.
Strengths and Limitations
The strength of this systematic review and meta-analysis is that, to our knowledge, it was the first to provide an overview of the implications of digital medical interventions for patient safety in abdominal surgery. However, there are some limitations to this study that warrant some caution in the interpretation of results.
First, we included some nonrandomized studies whose results were more prone to confounding than those of the RCTs. However, for the primary outcomes, we found that the significance and direction of the effect sizes were consistent in both RCTs and nonrandomized studies, despite differences in the point estimates. Furthermore, retrospective design and large samples of observational studies have ecological validity and provide additional information on how different technologies and settings may affect the outcomes. In addition, some nonrandomized studies have an appropriate prospective design, sufficient power, and adjustments for several potential sources of bias.21,23,27 Second, it was not possible to identify the specific mechanisms of action underlying the observed differences between telemedicine and conventional care groups; however, this study provided some indications of specific mechanisms that may inform future research. For instance, the use of mobile applications can reduce the time delays between complication onset and treatment; increase the monitoring of the recovery process (particularly in the first days after hospital discharge); or provide a more informative remote assessment of the patient’s status via pictures, videoconferences, and other media. Therefore, findings from the present study provide some avenues for future research that focus on specific mechanisms, which may be more effective in reducing adverse events in abdominal surgery.
Conclusions
In this systematic review and meta-analysis of 19 RCTs and nonrandomized studies, decreased rates of 30-day readmissions and ED visits were found in the telemedicine group vs the conventional care group after abdominal surgical procedures. There was no reduction in complication rates or LOS. However, the specific mechanisms of action for particular types of abdominal surgery are still largely unknown, warranting further research.
eAppendix. Search Strategy
eMethods.
eFigure 1. RCTs Risk of Bias Assessment (PEDro Scale)
eFigure 2. Non-RCTs Risk of Bias Assessment (ROBINS-I Tool)
eFigure 3. Length of Hospital Stay of All Studies and Subgroups
eTable 1. Number Needed to Treat, Randomized Controlled Studies
eTable 2. Patient Satisfaction for All Studies
eTable 3. Subgroup Analysis by Type of Intervention
eReferences.
Data Sharing Statement
References
- 1.Ghomrawi HMK, Holl JL, Abdullah F. Telemedicine in surgery-beyond a pandemic adaptation. JAMA Surg. 2021;156(10):901-902. doi: 10.1001/jamasurg.2021.2052 [DOI] [PubMed] [Google Scholar]
- 2.Asiri A, AlBishi S, AlMadani W, ElMetwally A, Househ M. The use of telemedicine in surgical care: a systematic review. Acta Inform Med. 2018;26(3):201-206. doi: 10.5455/aim.2018.26.201-206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams AM, Bhatti UF, Alam HB, Nikolian VC. The role of telemedicine in postoperative care. Mhealth. 2018;4:11. doi: 10.21037/mhealth.2018.04.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim L, Lyder CH, McNeese-Smith D, Leach LS, Needleman J. Defining attributes of patient safety through a concept analysis. J Adv Nurs. 2015;71(11):2490-2503. doi: 10.1111/jan.12715 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization . Classification of Digital Health Interventions. World Health Organization; 2018. [Google Scholar]
- 6.de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129-133. doi: 10.1016/S0004-9514(09)70043-1 [DOI] [PubMed] [Google Scholar]
- 7.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McQuay HJ, Moore RA. Using numerical results from systematic reviews in clinical practice. Ann Intern Med. 1997;126(9):712-720. doi: 10.7326/0003-4819-126-9-199705010-00007 [DOI] [PubMed] [Google Scholar]
- 9.Cremades M, Ferret G, Parés D, et al. Telemedicine to follow patients in a general surgery department. A randomized controlled trial. Am J Surg. 2020;219(6):882-887. doi: 10.1016/j.amjsurg.2020.03.023 [DOI] [PubMed] [Google Scholar]
- 10.Bednarski BK, Nickerson TP, You YN, et al. Randomized clinical trial of accelerated enhanced recovery after minimally invasive colorectal cancer surgery (RecoverMI trial). Br J Surg. 2019;106(10):1311-1318. doi: 10.1002/bjs.11223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dahlberg K, Philipsson A, Hagberg L, Jaensson M, Hälleberg-Nyman M, Nilsson U. Cost-effectiveness of a systematic e-assessed follow-up of postoperative recovery after day surgery: a multicentre randomized trial. Br J Anaesth. 2017;119(5):1039-1046. doi: 10.1093/bja/aex332 [DOI] [PubMed] [Google Scholar]
- 12.Halder GE, White AB, Brown HW, et al. A telehealth intervention to increase patient preparedness for surgery: a randomized trial. Int Urogynecol J. 2022;33(1):85-93. doi: 10.1007/s00192-021-04831-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaensson M, Dahlberg K, Eriksson M, Nilsson U. Evaluation of postoperative recovery in day surgery patients using a mobile phone application: a multicentre randomized trial. Br J Anaesth. 2017;119(5):1030-1038. doi: 10.1093/bja/aex331 [DOI] [PubMed] [Google Scholar]
- 14.Lee DD, Arya LA, Andy UU, Harvie HS. Video virtual clinical encounters versus office visits for postoperative care after pelvic organ prolapse surgery: a randomized clinical trial. Female Pelvic Med Reconstr Surg. 2021;27(7):432-438. doi: 10.1097/SPV.0000000000000909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mata J, Pecorelli N, Kaneva P, et al. A mobile device application (app) to improve adherence to an enhanced recovery program for colorectal surgery: a randomized controlled trial. Surg Endosc. 2020;34(2):742-751. doi: 10.1007/s00464-019-06823-w [DOI] [PubMed] [Google Scholar]
- 16.McGillion MH, Parlow J, Borges FK, et al. ; PVC-RAM-1 Investigators . Post-discharge after surgery Virtual Care with Remote Automated Monitoring-1 (PVC-RAM-1) technology versus standard care: randomised controlled trial. BMJ. 2021;374(2209):n2209. doi: 10.1136/bmj.n2209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pooni A, Brar MS, Anpalagan T, et al. Home to stay: a randomized controlled trial evaluating the effect of a post-discharge mobile app to reduce 30-day readmission following elective colorectal surgery. Ann Surg. 2023;277(5):e1056-e1062. doi: 10.1097/SLA.0000000000005527 [DOI] [PubMed] [Google Scholar]
- 18.Thompson JC, Cichowski SB, Rogers RG, et al. Outpatient visits versus telephone interviews for postoperative care: a randomized controlled trial. Int Urogynecol J. 2019;30(10):1639-1646. doi: 10.1007/s00192-019-03895-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van der Meij E, Anema JR, Leclercq WKG, et al. Personalised perioperative care by e-health after intermediate-grade abdominal surgery: a multicentre, single-blind, randomised, placebo-controlled trial. Lancet. 2018;392(10141):51-59. doi: 10.1016/S0140-6736(18)31113-9 [DOI] [PubMed] [Google Scholar]
- 20.Young JM, Butow PN, Walsh J, et al. Multicenter randomized trial of centralized nurse-led telephone-based care coordination to improve outcomes after surgical resection for colorectal cancer: the CONNECT intervention. J Clin Oncol. 2013;31(28):3585-3591. doi: 10.1200/JCO.2012.48.1036 [DOI] [PubMed] [Google Scholar]
- 21.Borsuk DJ, Al-Khamis A, Geiser AJ, et al. S128: Active post discharge surveillance program as a part of Enhanced Recovery After Surgery protocol decreases emergency department visits and readmissions in colorectal patients. Surg Endosc. 2019;33(11):3816-3827. doi: 10.1007/s00464-019-06725-x [DOI] [PubMed] [Google Scholar]
- 22.Daliya P, Carvell J, Rozentals J, Lobo DN, Parsons SL. Digital follow-up after elective laparoscopic cholecystectomy: a feasibility study. World J Surg. 2022;46(11):2648-2658. doi: 10.1007/s00268-022-06684-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eustache JH, Latimer EA, Liberman AS, et al. A mobile phone app improves patient-physician communication and reduces emergency department visits after colorectal surgery. Dis Colon Rectum. 2023;66(1):130-137. doi: 10.1097/DCR.0000000000002187 [DOI] [PubMed] [Google Scholar]
- 24.Liu N, Greenberg JA, Xu Y, Shada AL, Funk LM, Lidor AO. Phone follow-up after inguinal hernia repair. Surg Endosc. 2021;35(9):5159-5166. doi: 10.1007/s00464-020-08005-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lovasik BP, Blair CM, Little LA, Sellers M, Sweeney JF, Sarmiento JM. Reduction in post-discharge return to acute care in hepatopancreatobiliary surgery: results of a quality improvement initiative. J Am Coll Surg. 2020;231(2):231-238. doi: 10.1016/j.jamcollsurg.2020.03.034 [DOI] [PubMed] [Google Scholar]
- 26.Nikolian VC, Williams AM, Jacobs BN, et al. Pilot study to evaluate the safety, feasibility, and financial implications of a postoperative telemedicine program. Ann Surg. 2018;268(4):700-707. doi: 10.1097/SLA.0000000000002931 [DOI] [PubMed] [Google Scholar]
- 27.Stapler SJ, Brockhaus KK, Battaglia MA, Mahoney ST, McClure AM, Cleary RK. A single-institution analysis of targeted colorectal surgery enhanced recovery pathway strategies that decrease readmissions. Dis Colon Rectum. 2022;65(7):e728-e740. doi: 10.1097/DCR.0000000000002129 [DOI] [PubMed] [Google Scholar]
- 28.Uppal A, Kothari AN, Scally CP, et al. ; D3CODE Team . Adoption of telemedicine for postoperative follow-up after inpatient cancer-related surgery. JCO Oncol Pract. 2022;18(7):e1091-e1099. doi: 10.1200/OP.21.00819 [DOI] [PubMed] [Google Scholar]
- 29.Fink T, Chen Q, Chong L, Hii MW, Knowles B. Telemedicine versus face-to-face follow up in general surgery: a randomized controlled trial. ANZ J Surg. 2022;92(10):2544-2550. doi: 10.1111/ans.18028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goedeke J, Ertl A, Zöller D, Rohleder S, Muensterer OJ. Telemedicine for pediatric surgical outpatient follow-up: a prospective, randomized single-center trial. J Pediatr Surg. 2019;54(1):200-207. doi: 10.1016/j.jpedsurg.2018.10.014 [DOI] [PubMed] [Google Scholar]
- 31.Ma Y, Jones G, Tay YK, et al. Post-operative telephone review is safe and effective: prospective study - Monash outpatient review by phone trial. ANZ J Surg. 2018;88(5):434-439. doi: 10.1111/ans.14280 [DOI] [PubMed] [Google Scholar]
- 32.Hwa K, Wren SM. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg. 2013;148(9):823-827. doi: 10.1001/jamasurg.2013.2672 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Search Strategy
eMethods.
eFigure 1. RCTs Risk of Bias Assessment (PEDro Scale)
eFigure 2. Non-RCTs Risk of Bias Assessment (ROBINS-I Tool)
eFigure 3. Length of Hospital Stay of All Studies and Subgroups
eTable 1. Number Needed to Treat, Randomized Controlled Studies
eTable 2. Patient Satisfaction for All Studies
eTable 3. Subgroup Analysis by Type of Intervention
eReferences.
Data Sharing Statement