Abstract
This study aimed to evaluate and compare the impact of additives such as ZrO2 and SiO2 nanoparticles (ZrO2NP or SiO2NP) on the hardness, surface roughness, and color stability of 3D printed provisional restorations. Two hundred samples in total were printed using 3D printed resins (ASIGA, and NextDent). Each resin was modified with ZrO2NPs or SiO2NPs in two different concentrations (0.5 wt% and 1 wt%), while one group was kept unmodified (n = 10). Disc-shaped (15 × 2.5 mm) samples were designed and printed in accordance with the manufacturer’s recommendation. Printed discs were evaluated for color changes through parameters CIELAB 2000 system (ΔE00), hardness using Vickers hardness test, and surface roughness (Ra) using a noncontact profilometer. After calculating the means and standard deviations, a three-way ANOVA and Tukey post hoc test were performed at α = 0.05. The addition of ZrO2NPs or SiO2NPs to ASIGA and NextDent resins significantly increased the hardness at a given level of concentration (0.5% or 1%) in comparison with pure (p < 0.001), with no significant difference between the two modified groups per resin type (p > 0.05). The highest hardness value was detected in 1% ZrO2NPs with 29.67 ± 2.3. The addition of ZrO2NPs or SiO2NPs had no effect on the Ra (p > 0.05), with 1% ZrO2NPs showing the highest value 0.36 ± 0.04 µm with NextDent resin. ZrO2NPs induced higher color changes (∆E00), ranging from 4.1 to 5.8, while SiO2NPs showed lower values, ranging from 1.01 to 1.85, and the highest mean ∆E00 was observed in the 1% ZrO2NPs group and NextDent resin. The incorporation of ZrO2NPs and SiO2NPs in 3D printed provisional resins increased the hardness without affecting the surface roughness. The optical parameters were significantly affected by ZrO2NPs and less adversely affected by SiO2NPs. Consequently, care must be taken to choose a concentration that will improve the materials’ mechanical performance without detracting from their esthetic value.
Keywords: 3D printing, CAD-CAM, provisional resins, nanoparticles, surface properties, optical properties
1. Introduction
Provisional restorations are tooth-shaped shells that are used for a limited period until they are replaced by a definitive prosthesis [1]. They are often referred to as temporary restorations and they are made to temporarily protect and maintain the mechanical and biological integrity of the prepared teeth and the surrounding tissues during the treatment [2,3]. They safeguard the prepared tooth from thermal insults, provide stable occlusal contacts, and help in assessing the ultimate treatment’s therapeutic, functional, and cosmetic efficacy [3,4].
Three-dimensional (3D) printing technologies have opened many possibilities in a variety of areas, including healthcare [5]. A key element of this technology is 3D printed resins, used for provisional restorations, which have distinct advantages [5]. When it comes to making complicated geometry, traditional manufacturing processes frequently have restrictions, but 3D printing allows for detailed designs that may be adjusted to individual demands [5,6]. Furthermore, resins offer a wide range of qualities, including flexibility, strength, and transparency [6,7]. This adaptability permits the production of objects with a vast range of functions and applications [6,8]. However, there are also disadvantages associated with 3D printed resins. One of the major drawbacks is the limited range of available materials and their associated mechanical properties [8,9]. While this technology is continuously evolving, the variety of materials currently offered is lower compared to that of the conventional manufacturing techniques [8]. This restriction may limit certain applications and industries that require specific material properties [5].
Provisional restorations serve as placeholders until the permanent dental prosthetics’ placement, offering patients both functional and esthetic benefits during the interim period [2,3,10]. Commonly utilized provisional materials include polymethyl methacrylate (PMMA) resins, bis-acryl composites, and light-cured materials [4]. The most popular provisional restorations, known as (PMMA), are composed of prepared synthetic polymer [8]. At the moment, these are the materials that are most frequently used. The enhanced (Bis-GMA) material later made its way into various industries, and Bis-acryl resins are now widely used in the production of provisional fixed prostheses [2,3]. The selection of a suitable provisional material is dependent on many factors, including the intended duration of use, esthetic demands, and the clinical case scenario [10]. The issue of creating heat during the process of polymerization is a concern shared by dentists when using all provisional resins [11,12]. Since the hardness and yield strength diminish with increasing temperature, abrasive wear would increase [12]. Temperature-related decreases in yield strength and hardness occur in most materials. When tribological and dynamic mechanical analysis were used in the problem-solving process, the researchers discovered that using nano liquid reduced the amount of heat produced during wear and tear when compared to standard fluid [11,12]. The fillers or fibers that are added to polymers to help reinforce the surface were shown to improve the polymer’s tribological performance. This essentially covers the loading parameters for adhesive wear in dry contact situations [11,12].
Moreover, advanced manufacturing techniques have fundamentally impacted the development of provisional materials, enabling the creation of more precise and durable provisional restorations [7,8]. Computer-aided design and computer-aided manufacturing (CAD/CAM) technologies, including 3D printing, have revolutionized production, enhancing the accuracy and efficiency of provisional restorations [8,9]. These advancements contribute to the overall success of dental treatments by providing patients with well-fitted and esthetically pleasing temporary solutions.
A high-quality definitive fixed dental prosthesis (FDP) depends on a well-made provisional restoration [13,14]. The function and esthetics of a provisional FDP must be established while preserving the periodontal relationship and the alignment of the tooth [13]. The materials’ composition and manufacturing method influence the properties of 3D printed provisional restoration [14,15]. Comparing the physical properties of 3D printed provisional resins to conventional and subtractive techniques to fabricate provisional materials revealed inferior results. The main cause of poor mechanical properties, such as low hardness values in 3D printed materials, was reported to be due to shrinkage during the layering and post-processing steps [16,17]. Physical properties like increased surface roughness in 3D printed materials resulted in rapid material discoloration that intensified as time elapsed, resulting in a perceptible color change (ΔE) [15]. In order to enhance these qualities for long-term provisionalization, modifications such as the addition of different ingredients to 3D printed provisional resin may be attempted.
Nanoparticles have emerged as a promising method to address drawbacks associated with conventional provisional resin materials [17]. Integrating nanoparticles, particularly those composed of zirconia and silica, into provisional resin provides improved mechanical properties, enhanced wear resistance, and increased stability [15,18,19]. Zirconia nanoparticles, known for being non-toxic, holding high mechanical-physical properties, and having high strength and toughness, contribute to the enhancement of provisional resin, minimizing the risk of fracture and reinforcing the overall durability. These are added to improve strength by reducing the porosity and surface roughness, and increasing the hardness [20,21]. Previous investigations evaluating the mechanical effects of zinc oxide particles found that NP-modified dental-restorative-composite materials showed improved properties [22]. Silica nanoparticles, on the other hand, aid in achieving a smoother and more polished surface, improving the esthetic qualities of provisional restorations [23,24]. The distinctive properties of these nanoparticles, such as their high surface area and reactivity, contribute to the modification of the material’s characteristics [25]. The controlled incorporation of zirconia and silica nanoparticles into provisional resins can result in materials with superior mechanical performance and esthetic outcomes [24,25]. This innovative approach showcases the potential of nanotechnology in overcoming the limitations associated with traditional provisional materials, paving the way for improved clinical success and patient satisfaction [21,22,23,24].
The color and surface properties of provisional resins are crucial aspects that significantly impact the esthetic outcome and patient satisfaction of a provisional dental restoration [25]. Provisional resins, often used as interim crowns or FPDs, should exhibit color stability, mimic natural teeth, and possess desirable surface characteristics to ensure harmonious integration with the patient’s dentition [2,3]. Any alteration in the provisional resin color over time can result in an unesthetic appearance [25,26]. Resin composition, and exposure to environmental factors may disturb the color of provisional resins [23]. Studies have investigated the degree of color change of various provisional materials and the possible advancements in resin technology in an attempt to improve their esthetic longevity [15,16,23]. Surface properties, including roughness and polishability, play an important role in patient comfort, hygiene, and satisfaction. A smooth and polished surface helps resist plaque accumulation, decreases pigmentation, enhances esthetics, and contributes to the overall longevity of the provisional restoration [15,16].
Based on these studies, the 3D printed nanocomposite provisional showed superior wear resistance compared to the available provisional restorations [15,16]. However, further investigations to assess the physical properties are needed. In the literature, no prior studies investigated and compared the concept of ZrO2NPs and SiO2NPs incorporation in different 3D printed provisional material. Therefore, this article’s objective is to explore the effects of ZrO2NPs and SiO2NPs addition on the hardness, roughness, and color change of 3D printed provisional resins. The null hypothesis stated that the addition of ZrO2NPs and SiO2NPs to 3D printed resin at varying concentrations will not have significant effects on the surface properties and color of 3D printed nanocomposite provisional resins.
2. Materials and Methods
2.1. Sample Size and Grouping According to Materials and Nanoparticle Type and Concentrations
A recent study [27] that assessed the properties of 3D printed provisional resin was used as a guide to calculate the sample size. A total of 200 (100 for hardness and 100 for roughness and color changes) specimens [50/resin, 10/pure, 20/0.5%, and 20/1% (10/ZrO2NP and 10/SiO2NPs)] were tested for hardness, surface roughness, and color change [28,29]. The power analysis was calculated using the WHO formula, with 80% study power, 5% level of significance, and a 5% marginal error.
2.2. Preparation of Nanocomposite
Two different NPs were surface-treated as described in Table 1, and each NP was added to a single bottle containing nanocomposite liquid resin. Nanocomposite mixtures were prepared with NPs/resin filling ratios by weight as follows: 0.5% group (0.5% NP/99.5% fluid resin) and 1% group (1% NP/99% fluid resin) resulted in total 100 g nanocomposite per group. The weight of the salinized NPs was determined using a digital scale (S-234; Denver Instrument, Gottingen, Germany), followed by mixing with two resin types [NextDent (Shade N1) and ASIGA (Shade A1)]. According to NPs type and concentration, 5 groups (n = 50) were prepared per resin; 1 pure with no additions (control), and 4 groups with NP additions (0.5% ZrO2NPs, 1% ZrO2NPs, 0.5% SiO2NPs, and 1% SiO2NPs).
Table 1.
Nanoparticles details.
| Nanoparticles | Manufacturer | Description | Surface Treatment | Mixing and Addition |
|---|---|---|---|---|
| ZrO2NPs | Shanghai Richem International Co., Ltd., Shanghai, China | 0.5% and 1% weight spherical, white, and tetragonal particles (12 ± 3 nm; purity > 99%) |
Silane coupling agent (3-(trimethoxysilyl) propyl methacrylate); Shanghai Richem International Co., Ltd., Shanghai, China | NPs powder was meticulously stirred with resin fluid for 30 min to ensure homogeneity |
| SiO2NPs | AEROSIL R812; Evonik-Degussa, Essen, Germany |
2.3. Printing Parameters
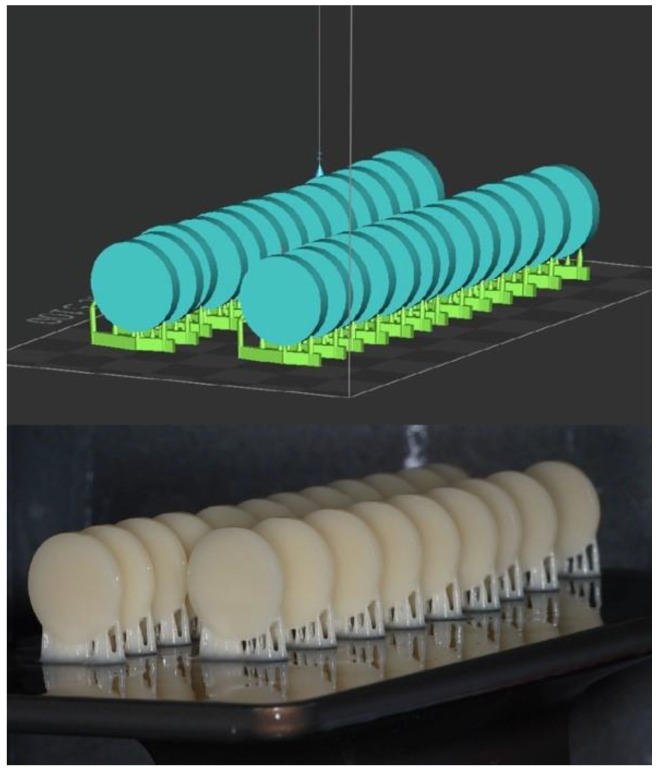
A disc specimen with dimensions of 15 × 2 ± 0.2 mm was designed using CAD software (123D design, Autodesk, version 2.2.14, San Francisco, CA, USA) [27,28]. The file of the design was saved as a standard tessellation language (STL) file (Figure 1). Using the STL file, 100 discs were 3D printed using the corresponding 3D printer for each resin type as listed in Table 2 and shown in Figure 1. Samples were put into curing machines after being submerged in a glycerol-based bath for the post-curing time, which was set at 30 min at 80 °C, to obtain the final material characteristics. Afterwards, the 3D printed discs were trimmed from the lattice support with a diamond disc to obtain the final shape and remove unpolymerized resin [28,29]. Specimens were wet-ground using an automated polishing machine (EcoMetTM 30 Semi-Automatic Grinder Polisher, Buehler, IL, USA) with a standard grinding paper (grit range of 320–1200) to achieve smooth surfaces while maintaining the same dimensions [28,29]. The samples were immersed in 37 °C distilled water for 48 h prior to testing. Each laboratory step was conducted by a single investigator for both resin materials.
Figure 1.
Specimens’ design (STL file) and printed specimens in printing plate.
Table 2.
Printing details.
| Material | Manufacturer | |
|---|---|---|
| NextDent/Printer | NextDent (C&B NextDent, Shade N1, Soesterberg, The Netherlands) | |
| NextDent 5100 3D printer (3D Systems, Rock Hill, SC, USA) | ||
| ASIGA/Printer | ASIGA (Asiga DentaTOOTH, Shade A1, ASIGA, Erfurt, Germany) | |
| ASIGA MAX printer (Asiga, Alexandria, NSW, Australia) | ||
| Printing parameters | printing layer thickness | 50 µm |
| printing orientation | 90 degrees | |
| post-curing time | 30 min at 80 °C | |
2.4. Testing Procedures
2.4.1. Hardness
The discs were subjected to Vickers hardness indenter (HMV-2 Shimadzu Corp., Tokyo, Japan) [28,29] at 100 g of force for 15 s (ASTM C1327-03 standard [30]) [29,31] at three random locations on the specimen’s surface. The specimen’s hardness value (VH) was the average of the three readings.
2.4.2. Surface Roughness (Ra, µm)
A noncontact profilometer (Contour GT-K 3D Optical Microscope, Bruker, Billerica, MA, USA) was utilized to determine the surface roughness. The Ra value of each specimen was determined by averaging the values of 3 readings at different locations on the surface [32,33].
2.4.3. Color Stability
Color measurements were obtained with a standard illuminant C and calibrated spectrophotometer (Color-Eye® 7000 A, X-Rite, Carlstadt, NJ, USA) in the visible spectrum range (380–780 nm) [32,34]. The color difference between the specimens was calculated using the following equation:
where ΔL′, ΔC′, and ΔH′ are the differences in lightness, chroma, and hue between the control and modified specimens, RT is a function that accounts for differences in chroma and hue in the blue region, and SL, SC, SH adjust for variation in the location of color difference of samples in L′, a′, b′ values, while KL, KC, KH are correction terms set at 2:1:1 [15,32,33]. ΔE00 was assessed on perceptibility (PT) basis and acceptability (AT) thresholds, which were set at 50:50%; PT ranged from 0.8 to 1.30 and 50:50% AT ranged from 1.80 to 2.25 ΔE00 [35].
2.5. Data Analysis
The statistical package for social sciences (SPSS v.23) was used for statistical analysis. Means and standard deviations were calculated. The insignificant results of the Shapiro–Wilk test suggested a normal distribution of the data. Therefore, parametric tests were used for the inferential analysis. One-way ANOVA was used to study the difference between the means of the groups followed by Tuckey post hoc test for the pair-wise comparisons where applicable. Three-way ANOVA was used to assess the effect of the interaction between factors (loading level, NP, and material) on the tested properties. p-values of less than 0.05 were considered statistically significant.
3. Results
Table 3 demonstrates the variation in the hardness caused by the NPs’ concentration levels. The ANOVA results showed significant differences between the groups for both resins (p ≤ 0.01). The addition of ZrO2NPs or SiO2NPs significantly increased the hardness in comparison with pure groups (p = 0.01, p < 0.001), respectively. For pairwise comparisons of modified groups, no significant differences between the two concentrations in both NPs and resin type were detected (p > 0.05). The collective effect of two and three factors was evaluated using three-way ANOVA and the results were tabulated in Table 4. It was found that none of the combined factors were statistically significant, whether two or three factors.
Table 3.
Three-way ANOVA for the interaction effects of the factors on the hardness and roughness.
| Tested Properties | Interaction | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|---|
| Hardness | Intercept | 65,026.748 | 1 | 65,026.748 | 4012.617 | 0.000 * |
| NP × concentration | 57.562 | 1 | 57.562 | 3.552 | 0.064 | |
| NP × material | 22.770 | 1 | 22.770 | 1.405 | 0.240 | |
| concentration × material | 3.630 | 1 | 3.630 | 0.224 | 0.637 | |
| NP × concentration × material | 5.222 | 1 | 5.222 | 0.322 | 0.572 | |
| Error | 1166.801 | 72 | 16.206 | |||
| Total | 66,307.356 | 80 | ||||
| Surface roughness Ra (µm) |
Intercept | 7.776 | 1 | 7.776 | 2562.904 | 0.000 * |
| NP × concentration | 0.002 | 1 | 0.002 | 0.601 | 0.441 | |
| NP × material | 0.013 | 1 | 0.013 | 4.153 | 0.045 * | |
| concentration × material | 0.002 | 1 | 0.002 | 0.798 | 0.375 | |
| NP × concentration × material | 0.000 | 1 | 0.000 | 0.063 | 0.802 | |
| Error | 0.218 | 72 | 0.003 | |||
| Total | 8.114 | 80 | ||||
| ΔE00 | Intercept | 1012.180 | 1 | 1012.180 | 3196.520 | 0.000 * |
| NP × concentration | 3.297 | 1 | 3.297 | 10.411 | 0.002 * | |
| NP × material | 6.028 | 1 | 6.028 | 19.037 | 0.000 * | |
| concentration × material | 0.002 | 1 | 0.002 | 0.005 | 0.943 | |
| NP × concentration × material | 1.152 | 1 | 1.152 | 3.638 | 0.060 | |
| Error | 22.799 | 72 | 0.317 | |||
| Total | 1296.009 | 80 |
* statistically significant at 0.05 level of significance.
Table 4.
Effect of different concentration levels of nanoparticles on the hardness and roughness and color changes of provisional resins.
| Tested Properties | NP | Concentration | ASIGA | NextDent | p -Value |
| Hardness (VHN) |
ZrO2NP | Pure | 22.3 (3.2) | 23.4 (0.9) | 0.621 |
| 0.5% | 29.59 (9.1) a | 26.78 (2.7) a | 0.073 | ||
| 1% | 29.67 (2.3) a | 28.74 (1.4) a | 0.077 | ||
| p-value | 0.01 * | 0.000 * | |||
| SiO2NP | Pure | 22.3 (3.2) | 23.4 (0.9) | 0.621 | |
| 0.5% | 29.33 (0.7) a | 29.69 (2.6) a | 0.531 | ||
| 1% | 27.0 (1.6) a | 27.23 (4.8) a | 0.334 | ||
| p-value | <0.001 * | 0.001 * | |||
| Surface roughness (Ra, µm) |
ZrO2NP | Pure | 0.26 (0.04) | 0.33 (0.08) | 0.032 * |
| 0.5% | 0.23 (0.03) | 0.33 (0.05) | 0.001 * | ||
| 1% | 0.28 (0.07) | 0.36 (0.04) | 0.042 * | ||
| p-value | 0.119 | 0.395 | |||
| SiO2NP | Pure | 0.26 (0.04) | 0.33 (0.08) | 0.032 * | |
| 0.5% | 0.28 (0.04) | 0.33 (0.03) | 0.044 * | ||
| 1% | 0.32 (0.09) | 0.34 (0.05) | 0.472 | ||
| p-value | 0.058 | 0.92 | |||
| Color changes ∆E00 |
ZrO2NP | 0.5% | 4.1 (0.4) | 4.3 (0.3) | 0.941 |
| 1% | 5.8 (0.4) | 5.2 (0.4) | 0.429 | ||
| p-value | 0.000 * | 0.000 * | |||
| SiO2NP | 0.5% | 1.01 (0.4) | 1.51 (0.5) | 0.040 * | |
| 1% | 1.14 (0.2) | 1.85 (0.1) | 0.038 * | ||
| p-value | 0.430 | 0.051 |
* statistically significant at 0.05 level of significance. Same small letters in each column showed statistical insignificance between the pairs.
The means and standard deviations of Ra of tested groups are presented in Table 3. The ANOVA results showed no significant differences in Ra between the groups for both resins and both NPs (p > 0.05). While 1% SiO2NPs recorded the highest Ra value (0.32 ± 0.09 µm) between the ASIGA groups, 1% ZrO2NPs showed the highest Ra value (0.36 ± 0.04 µm) for NextDent. Generally, NextDent showed higher values in comparison to ASIGA for all NP concentrations. The ANOVA results for surface roughness are shown in Table 3. The results indicated that only the combined effect of NP × material had a significant effect on the surface roughness (p = 0.045). Otherwise, none of the factors (two or three) were statistically significant.
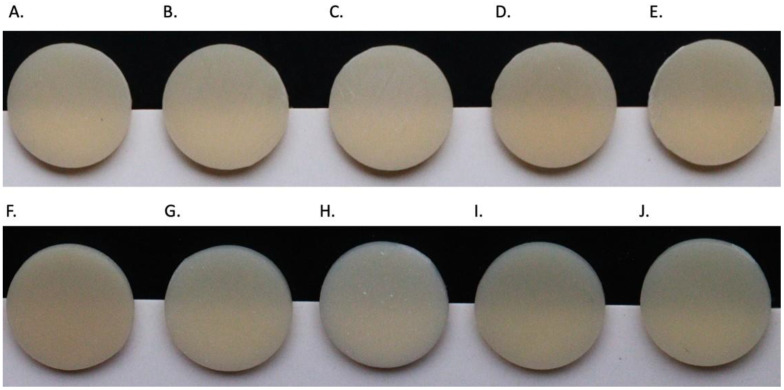
Table 4 presents the color change results (ΔE00) for resins with different percentages of ZrO2NPs and SiO2NPs additions. Significant color changes were observed with ZrO2NPs, and this change was concentration dependent. In addition, 1% ZrO2NPs specifically showed a substantial increase in ΔE00 compared to 0.5% ZrO2NPs in both resins. Regarding SiO2NPs, no significant difference in ΔE00 was observed. When comparing the NPs, ZrO2NPs induced higher color changes (ΔE00) ranging between 4.1 ± 0.4 and 6.2 ± 0.6 in contrast to 1.01 ± 0.4 and 2.12 ± 0.4 for SiO2NPs. Also, the findings were supported by actual images of representative specimens per group (Figure 2). The combined effects of two and three factors on ΔE00 were studied using three-way ANOVA (Table 3). The results showed that the combined effect of NP × concentration (p = 0.000) and NP × material (p = 0.000) in addition to the effect of all three factors combined (p = 0.004) had significant effects on ∆E00.
Figure 2.
Photographs of the samples (A) ASIGA (pure), (B) ASIGA (0.5% ZrO2NPs), (C) ASIGA (1% ZrO2NPs), (D) ASIGA (0.5% SiO2NPs), (E) ASIGA (1% SiO2NPs), (F) NextDent (pure), (G) NextDent (0.5% ZrO2NPs), (H) NextDent (1% ZrO2NPs), (I) NextDent (0.5% SiO2NPs), and (J) NextDent (1% SiO2NPs).
4. Discussion
In a previous systematic review by Gad and Fouda, the elements influencing the mechanical properties of 3D printed resins were extensively explored [36]. Within the context of resin modifications, nanoparticles in 3D printed resins represent a noteworthy factor impacting their overall properties, as previously reported and classified [24,25,36]. This investigation assessed the hardness, surface roughness, and color change of 3D printed provisional resins modified with ZrO2NPs and SiO2NPs. This study’s results dictated a partial rejection of the null hypothesis, indicating significant differences in hardness and color change, while no statistically significant effect was observed on the roughness of 3D printed nanocomposite provisional resins.
Prior research has demonstrated that using nanoparticles as reinforcement can enhance the qualities of materials [17,27]. The advantageous effects of modified materials incorporating nanoparticles are limited by several criteria, including size, shape, ratio, homogeneous dispersion within the matrix of the resin, and salinization phase [17,27]. The filler’s weight percentages had an even more noticeable effect on the mechanical and physical characteristics [27]. To improve the chemical interaction between the filler phase and polymer matrix, the NPs’ surfaces were silanized [27]. The optical characteristics of the modified material would be improved by acceptable chemical bonding since the fillers and their quantity are important factors [31]. ZrO2NPs and SiO2NPs have been shown in earlier studies to improve the mechanical qualities of 3D printed materials [31]. Resin with high concentrations of ZrO2NPs is whitish in color, while SiO2NPs might limit light transmission and lower translucency [27,31]. Therefore, it is crucial to figure out the exact concentration of the filler to guarantee that it adheres to the resin matrix without forming clusters [34,37]. The use of NPs at high concentrations may have unfavorable effects resulting from the particles’ potential to cluster [34,37]. Previous studies reported that low quantities of SiO2NPs improved 3D printed resin, while 3 wt% ZrO2NPs resulted in maximum improved properties. On the other hand, concentrations above 7% were avoided due to the possibility of remarkable color change [27,31]. To compare the two nanoparticles and lessen the color change effect in terms of esthetic requirements with ZrO2NPs, 0.5 wt% and 1 wt% were introduced in the current study.
Hardness is likewise impacted by the ratio of organic to inorganic substance. It is used to determine a material’s ability to withstand abrasion, resist indentations, and abrade the opposing structure, and as an indirect way to determine the degree of polymerization [14,38,39,40]. This investigation revealed that the addition of ZrO2NPs and SiO2NPs increased the hardness at a given level of concentration (0.5% or 1%). This significance was found for NPs and both materials (NextDent and ASIGA). The results are compatible with the findings of Aati et al. [27], who found that the hardness of ZrO2NPs-modified 3D printed materials increased positively in relation to the filler weight increase [27]. In this study, the lowest and highest hardness values were 22.3 and 29.67, respectively. However, Aati et el., in a previous study, reported the highest hardness value of 20.02 [27]. The positive effects of ZrO2NPs in our study can be explained by their small diameter and ability to spread stresses within the resin more effectively [27]. Similarly, Gad et al. [41] discovered that, despite a barely noticeable variation in concentration, the hardness of 3D printed denture resin modified with SiO2NPs increased significantly [41]. In this study, disregarding the type of additive, microhardness increased in a direct relation with filler proportion. This increase might be linked to the advantages of the nanosized fillers used [27,42]. The nanosize of the particles and their homogenous dispersion within the material helped in reducing interparticle spacing and enhancing the microhardness of the modified nanocomposite, leading to higher capacity of indentation resistance [41,43]. The oxidative metals ZrO2NPs and SiO2NPs used in this study are considered to exhibit superior mechanical strength and hardness [27,42]. In contrast to pure resin, it is anticipated that various fractional enhancements of nanofillers would greatly improve the durability of 3D printed resin, with higher filler content translating into higher microhardness [41,43]. The nanofillers are predicted to significantly improve the mechanical properties due to high interfacial shear strength, which was increased by appropriate silanization and interphase interaction [41,44].
The physical and chemical characteristics of the 3D printed provisional material control how long the restorations last [43]. When fabricating restorations, surface roughness is a significant physical attribute that should be considered. Lack of esthetics, possibility of staining and loss of glossy appearance are strongly associated with rough surfaces [45,46]. Furthermore, a strong correlation has been demonstrated between roughness and other concerns like plaque accumulation, gingival inflammation, and caries [45,46,47]. Consequently, smooth surfaces are required. It was determined that different manufacturing processes may influence the material’s susceptibility to plaque adherence, and the established Ra threshold was 0.2 μm [47]. In this study, the Ra value range of pure specimens was between 0.26 µm and 0.33 µm, and the Ra values of tested samples varied between 0.23 µm and 0.36 µm. In addition, the statistical analysis revealed no significant change in surface roughness at all ZrO2NPs and SiO2NPs levels for both resins (NextDent and ASIGA). These findings are consistent with earlier research stating that the addition of ZrO2NPs had no effect on surface roughness [48]. Previously, investigations have added ZrO2NPs and SiO2NPs to a 3D printed provisional at 5% and 10% loading level and concluded that the incorporation increased the surface roughness values, especially 10%SiO2NPs [43]. In a different investigation, an interim prosthesis with loaded with 1% ZrO2NPs demonstrated no change in surface roughness compared to the control [45].
According to the literature, the influence of nanoparticles on surface roughness varied depending on the amount of nanofiller used [43,45]. The hardness of 3D printed resin was enhanced after the incorporation of 0.5% and 1% SiO2NPs, but Ra was not notably changed. This is in alignment with the fact presented in a previous study where the Ra of all 3D printed resin groups was significantly higher than that of the PMMA group (p < 0.001), with little variation observed among the 3D printed groups [41]. This noted increase in roughness with SiO2NPs loading compared to PMMA was attributed to cluster formations at the samples’ surfaces [41]. In contrast, loading 3D printed resin with ZrO2NPs did not affect the roughness owing to the filler’s homogenous distribution within the polymer matrix, which is less likely to affect the surface roughness [27,31,41]. A variety of factors affected the surface roughness, such as the nanoparticles’ tendency to cluster when the concentration rises, which frequently results in lower homogeneity of the composite resin [27,39,42]. During the polishing process, the superficial clustered particles disengage, creating voids and holes [44]. The printing technique (layer by layer and manufacturing direction) could be another cause of the alternation in Ra. When the sample surfaces are inclined or tilted in relation to the platform, the layered structure of the resin may create a stair-stepping effect [41]. In certain cases, the removal of the support structures leaves residues on the surface that degrade the surface properties. These effects are highly dependent on how a part surface is oriented during the building process. Also, surface properties reflect any errors or irregularities that might arise during the process of NPs’ mixing and printing [41]. Nevertheless, the surface roughness in the current investigation was not impacted by the loading level nor by the nanofiller type or concentration.
The potential influence of nanoparticle surface treatment or coupling agents on the optical properties and color stability of 3D printed provisional resins is an important consideration in understanding the overall performance of these materials [36,41]. Surface treatment, such as silane coupling agents, can improve the adhesion between nanoparticles and the resin matrix, leading to better dispersion and reduced agglomeration of nanoparticles [36]. This improved dispersion can result in more uniform optical properties and color distribution within the resin, ultimately enhancing color stability [36,41,44]. Additionally, surface treatment can also modify the surface chemistry of nanoparticles, influencing their interaction with light and thus affecting the overall optical properties of the resin. Moreover, the choice of coupling agent or surface treatment can affect the degree of light scattering and absorption within the resin matrix, which, in turn, influences its translucency and color appearance [36,37]. For example, certain surface treatments may enhance light transmission through the resin, resulting in a more translucent material with improved color stability, while others may reduce light transmission and increase opacity, leading to color changes [36]. Studies have shown that the selection of appropriate surface treatments or coupling agents is critical in optimizing the optical properties and color stability of nanoparticle-modified resins [37]. For instance, silane coupling agents have been found to effectively improve the dispersion of nanoparticles within resin matrices, resulting in enhanced color stability and translucency [36,41]. Similarly, other surface treatments, such as plasma treatment or functionalization, have been shown to positively impact the optical properties of nanoparticle-modified resins [36,43]. In summary, surface treatment or coupling agents play a significant role in determining the optical properties and color stability of nanoparticle-modified resins. By carefully selecting and optimizing these surface treatments, researchers can enhance the overall performance and esthetic qualities of 3D printed provisional restorations [37].
The selection of color measurement method, namely ΔE00, stems from the need to comprehensively evaluate color changes in dental resins modified with ZrO2NPs and SiO2NPs [25,33]. ΔEab, representing the traditional CIELAB color difference formula, is widely used in dentistry and provides a straightforward and practical assessment based on perceptual color differences [43,49]. However, the accuracy of color assessment is improved by the use of the ΔE00 formula that includes adjustments for perceptual uniformity [43,49]. This method approximates the human eye’s nonlinear sensitivity to color differences, providing a more accurate representation of perceived color changes [45,46]. Therefore, using the ΔE00 method offers a robust analysis, accounting for contemporary approaches to color measurement in dental materials [45,48] and those selected in the present study.
ZrO2NPs showed a statistically significant color change with both concentrations. These results match those of a previous report which concluded that ZrO2NPs addition reduced the material’s translucency in proportion to its concentrations [50]. Aszrin et al. [51] indicated that the combination of varying concentrations of ZrO2, AlO2, and SiO2 fillers had an unanticipated negative affect on translucency. Variations in the optical properties of ZrO2NPs and their dispersion in the matrix could be the source of decreased translucency [50,51]. The opacity and crystallinity of these nanofillers is thought to be the cause of light diffusion impedance [43,45]. Additionally, ZrO2NPs cluster formations can reduce translucency by obstructing light transmission [51].
The addition of SiO2NPs showed a statistically insignificant change in color in both concentrations, with a greater color change at 1% reinforcement in both materials. However, all values for color change in both materials were clinically insignificant. A previous study has demonstrated that NPs had a minor effect on the optical properties of the auto-polymerizing provisional resin with no clinical perceptibility, with values ranging between 2.7 and 3.3 in darker shades. The A3 shade, on the other hand, expressed an acceptability threshold value of 1.8 with 0.25 wt% SiO2NPs [15]. As this study only tested A1 shade, both concentrations of SiO2NPs did not affect the optical properties. The ability to transmit light through the resin was not significantly reduced with these NPs [15,41,43]. The additive agent concentration, shape, size, and distribution in the mixture, all directly correlate with light scattering [15,41,43]. One likely explanation is the variation in refraction index between the different materials, which does not diffuse transmitted light equally. ZrO2NPs with a tetragonal shape had a significant impact on the color of the modified specimens in this investigation. According to Arikawa et al. [52], materials with small irregular fillers showed a sharper peak of light diffusion than those with large spherical fillers. The materials with the least amount of light scattering within the matrix and the highest degree of light transmission are those with the smallest-size reinforcing agent [53]. For the materials under evaluation, this could account for the varying degrees of translucency alterations brought on by the different NPs [52,53,54,55,56].
According to a previous report, clinical perceptibility and acceptability thresholds, this study revealed that the color variations in the ZrO2NPs-reinforced-resin were substantially greater than the average for ΔE00 for SiO2NPs. In both resins, ASIGA and NextDent, 0.5% ZrO2NPs resulted in ΔE00 values of 4.1 and 4.3, respectively, while 1% ZrO2NPs produced ΔE00 values of 5.8 and 5.2, respectively. In contrast, SiO2NPs in both concentrations presented the lowest color change perceptibility. These results are aligned with prior investigations that assessed the ΔΕ00 values after the addition of NPs [43,51].
The color change per NPs’ addition exhibited both high and low variations in the modified resins. Notably, a comparison between the two types of NPs indicated that ZrO2NPs induced more pronounced color changes than SiO2NPs. A closer examination of physical images revealed the emergence of a whitish color associated with ZrO2NPs, contributing to the overall color alterations in the provisional resins. These findings are supported by the ZrO2NPs-reinforced groups having ΔE00 values above the perceptible threshold compared to the SiO2NPs with values at the limit of the threshold. Among the other factors that affect the color is the loading ratio of NPs, which had a significant effect on the degree of color change (p = 0.002). Another element is the light absorption and scattering off the outer layer of the prosthesis and from within [53]. Translucency and perception of color are closely linked to light scattering [55,56]. Printed samples typically consist of multiple layers, each of which may have a different refractive index [53,55]. Light is reflected and transmitted by each layer and interface that make up the sample. The layers may reflect or transmit light at their interfaces, or scatter and/or absorb it within the layers [51,53,55]. Translucency variations from the same resin may be based on printing angle, different orientation of layers, scattering or absorption values and different overall measures from the contact points in the layers [53].
Due to the fact that discs from different brands vary in strength, this study’s findings advise clinicians that understanding the benefits, limitations, and quirks of the many provisional restoration fabrication procedures is essential to achieving these outcomes and preventing failures and difficulties. Test results for the tested NPs are satisfactory, and they can be recommended for long-term provisionalization in clinical practice. This might hold true for specimens that were disc-shaped printed provisional restorations, such as bridges and single units. As a result, caution should be taken when interpreting the results of this study to implement in real life until more research is undertaken using actual tooth-shaped temporary dental prostheses. This study emphasizes the importance of balance between strength, surface properties, and esthetics when selecting NPs for provisional resin reinforcement. It enables healthcare providers to draw comparisons between various systems in terms of how effectively the examined materials function under uniform settings. Because of their improved mechanical qualities, ease of handling, and consistency in results, new generations of these materials are expected to become more practical. When esthetics are the concern, clinicians are advised to use SiO2NPs more than ZrO2NPs due to their clinical color acceptability thresholds and enhanced patient satisfaction and acceptance. Both are recommended in esthetically undemanding areas like posterior provisional restorations. In addition, the modified provisional restoration has advantages over the pure group as it showed improvements in the properties that will result in better practical outcomes and patient satisfaction. The use of two different resin materials and two nanoparticles makes up for the strength of this study.
The limitations of this in vitro study include using disc-shape specimens that are different in configuration than the actual prostheses. In addition, the absence of simulated oral environment, such as saliva, bacteria, and masticatory load may affect the interpretation of this study’s results. Future investigations of provisional restoration made using other printing technologies in addition to aging processes such as thermal cycling and cyclic loading are required to mimic intraoral conditions. It is advised in future studies to analyze the effects on various aging processes, upon different printing technologies, to assess the long-term performance of the materials and different thermal, tribological properties’ analysis, as well as to compare alternate types of NPs or combinations of them, on different additional analysis techniques.
5. Conclusions
The incorporation of ZrO2NPs and SiO2NPs in 3D printed provisional resins increased hardness, while surface roughness was not affected. Regardless of the 3D printed provisional material type, ZrO2NPs’ addition produced noticeable color change, while 0.5% SiO2NPs showed small color changes not exceeding perceptibility thresholds. Consequently, care must be taken to choose a concentration that will improve the materials’ mechanical qualities without detracting from their esthetic value.
Author Contributions
Conceptualization, M.M.G.; methodology, F.M.A., R.F.A., Z.H.A.D., F.Y.A. and S.Y.A.; software, F.M.A. and R.F.A.; validation, Z.H.A.D., F.Y.A. and S.Y.A.; formal analysis, S.Q.K.; investigation, F.M.A., R.F.A., Z.H.A.D., F.Y.A. and S.Y.A.; resources, M.A.A.; data curation, F.M.A. and R.F.A.; writing—original draft preparation, F.M.A., R.F.A., Z.H.A.D. and F.Y.A.; writing—review and editing, R.A. and M.M.G.; visualization, M.M.G.; supervision, M.A.A., R.A. and M.M.G.; project administration, M.A.A., F.M.A. and M.M.G.; funding acquisition, M.A.A. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
The data are available upon request via email or phone to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Chiramana S., Dev R.R.J., Banka M., Pssv S., Rao K., Chvn S.K. Provisional Restoration in Prosthodontics: A Review. J. Adv. Med. Dent. Sci. Res. 2019;7:46–51. [Google Scholar]
- 2.Burke F.T., Murray M.C., Shortall A.C. Trends in Indirect Dentistry: 6. Provisional Restorations, More than Just a Temporary. Dent. Updat. 2005;32:443–452. doi: 10.12968/denu.2005.32.8.443. [DOI] [PubMed] [Google Scholar]
- 3.Anusavice K.J., Philips R. Phillips’ Science of Dental Materials. 11th ed. Elsevier; St. Louis, MO, USA: 2003. pp. 145–146. [Google Scholar]
- 4.Rosenstiel S.F., Land M.F. Contemporary Fixed Prosthodontics. 3rd ed. Elsevier; St. Louis, MO, USA: 2000. p. 381. [Google Scholar]
- 5.Gross B.C., Erkal J.L., Lockwood S.Y., Chen C., Spence D.M. Evaluation of 3D Printing and Its Potential Impact on Biotechnology and the Chemical Sciences. Anal. Chem. 2014;86:3240–3253. doi: 10.1021/ac403397r. [DOI] [PubMed] [Google Scholar]
- 6.Bompolaki D., Lubisich E.B., Fugolin A.P. Resin-Based Composites for Direct and Indirect Restorations: Clinical Applications, Recent Advances, and Future Trends. Dent. Clin. N. Am. 2022;66:517–536. doi: 10.1016/j.cden.2022.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Helal M., Fadl-Alah A., Baraka Y., Gad M., Emam A.-N. In-vitro comparative evaluation for the surface properties and impact strength of CAD/CAM milled, 3D printed, and polyamide denture base resins. J. Int. Soc. Prev. Community Dent. 2022;12:126–131. doi: 10.4103/jispcd.JISPCD_293_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alghazzawi T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016;60:72–84. doi: 10.1016/j.jpor.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Li Y., Han W., Cao J., Iv Y., Zhang Y., Han Y., Shen Y., Ma Z., Liu H. Design of Complete Dentures by Adopting CAD Developed for Fixed Prostheses. J. Prosthodont. 2018;27:212–219. doi: 10.1111/jopr.12554. [DOI] [PubMed] [Google Scholar]
- 10.Jain S., Sayed M.E., Shetty M., Alqahtani S.M., Al Wadei M.H.D., Gupta S.G., Othman A.A.A., Alshehri A.H., Alqarni H., Mobarki A.H., et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers. 2022;14:2691. doi: 10.3390/polym14132691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Das P.P., Chaudhary V. Tribological and dynamic mechanical analysis of bio-composites: A review. Mater. Today Proc. 2020;25:729–734. doi: 10.1016/j.matpr.2019.08.233. [DOI] [Google Scholar]
- 12.Yadav R., Meena A., Lee H.-H., Lee S.-Y., Park S.-J. Tribological behavior of dental resin composites: A comprehensive review. Tribol. Int. 2023;190:109017. doi: 10.1016/j.triboint.2023.109017. [DOI] [Google Scholar]
- 13.Lee E.-H., Ahn J.-S., Lim Y.-J., Kwon H.-B., Kim M.-J. Effect of post-curing time on the color stability and related properties of a tooth-colored 3D-printed resin material. J. Mech. Behav. Biomed. Mater. 2022;126:104993. doi: 10.1016/j.jmbbm.2021.104993. [DOI] [PubMed] [Google Scholar]
- 14.Perea-Lowery L., Gibreel M., Vallittu P.K., Lassila L. Characterization of the mechanical properties of CAD/CAM polymers for interim fixed restorations. Dent. Mater. J. 2020;39:319–325. doi: 10.4012/dmj.2019-042. [DOI] [PubMed] [Google Scholar]
- 15.Kotanidis A., Kontonasaki E., Koidis P. Color alterations of a PMMA resin for fixed interim prostheses reinforced with silica nanoparticles. J. Adv. Prosthodont. 2019;11:193–201. doi: 10.4047/jap.2019.11.4.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shin J.-W., Kim J.-E., Choi Y.-J., Shin S.-H., Nam N.-E., Shim J.-S., Lee K.-W. Evaluation of the Color Stability of 3D-Printed Crown and Bridge Materials against Various Sources of Discoloration: An In Vitro Study. Materials. 2020;13:5359. doi: 10.3390/ma13235359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madhav V.N.V., Digholkar S., Palaskar J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J. Indian Prosthodont. Soc. 2016;16:328–334. doi: 10.4103/0972-4052.191288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vallittu P.K. Flexural properties of acrylic resin polymers reinforced with unidirectional and woven glass fibers. J. Prosthet. Dent. 1999;81:318–326. doi: 10.1016/S0022-3913(99)70276-3. [DOI] [PubMed] [Google Scholar]
- 19.Zacher J., Bauer R., Strasser T., Rosentritt M. Laboratory performance and fracture resistance of CAD/CAM implant-supported tooth-coloured anterior FDPs. J. Dent. 2020;96:103326. doi: 10.1016/j.jdent.2020.103326. [DOI] [PubMed] [Google Scholar]
- 20.Maji P., Choudhary R., Majhi M. Structural, optical and dielectric properties of ZrO2 reinforced polymeric nanocomposite films of polymethylmethacrylate (PMMA) Optik. 2016;127:4848–4853. doi: 10.1016/j.ijleo.2016.02.025. [DOI] [Google Scholar]
- 21.Reyes-Acosta M., Torres-Huerta A., Domínguez-Crespo M., Flores-Vela A., Dorantes-Rosales H., Ramírez-Meneses E. Influence of ZrO2 nanoparticles and thermal treatment on the properties of PMMA/ZrO2 hybrid coatings. J. Alloys Compd. 2015;643:S150–S158. doi: 10.1016/j.jallcom.2014.10.040. [DOI] [Google Scholar]
- 22.Pratap B., Nag M., Yadav R., Althahban S., Wal J.C. Dynamic mechanical analysis of zinc oxide and hydroxyapatite particulate filled dental restorative composite materials. AIP Conf. Proc. 2023;2782:020212. doi: 10.1063/5.0154476. [DOI] [Google Scholar]
- 23.Atai M., Pahlavan A., Moin N. Nano-porous thermally sintered nano silica as novel fillers for dental composites. Dent. Mater. 2012;28:133–145. doi: 10.1016/j.dental.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 24.Al-Thobity A.M., Gad M.M. Effect of silicon dioxide nanoparticles on the flexural strength of heat-polymerized acrylic denture base material: A systematic review and meta-analysis. Saudi Dent. J. 2021;33:775–783. doi: 10.1016/j.sdentj.2021.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sham A.S.K., Chu F.C.S., Chai J., Chow T.W. Color stability of provisional prosthodontic materials. J. Prosthet. Dent. 2004;91:447–452. doi: 10.1016/j.prosdent.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 26.De Castro E.F., Nima G., Rueggeberg F.A., Giannini M. Effect of build orientation in accuracy, flexural modulus, flexural strength, and microhardness of 3D-Printed resins for provisional restorations. J. Mech. Behav. Biomed. Mater. 2022;136:105479. doi: 10.1016/j.jmbbm.2022.105479. [DOI] [PubMed] [Google Scholar]
- 27.Aati S., Akram Z., Ngo H., Fawzy A.S. Development of 3D printed resin reinforced with modified ZrO2 nanoparticles for long-term provisional dental restorations. Dent. Mater. 2021;37:e360–e374. doi: 10.1016/j.dental.2021.02.010. [DOI] [PubMed] [Google Scholar]
- 28.Alrahlah A., Khan R., Vohra F., Alqahtani I.M., Alruhaymi A.A., Haider S., Al-Odayni A.-B., Saeed W.S., Murthy H.C.A., Bautista L.S. Influence of the Physical Inclusion of ZrO2/TiO2 Nanoparticles on Physical, Mechanical, and Morphological Characteristics of PMMA-Based Interim Restorative Material. BioMed Res. Int. 2022;2022:1743019. doi: 10.1155/2022/1743019. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 29.Fouda S.M., Gad M.M., Abualsaud R., Ellakany P., AlRumaih H.S., Khan S.Q., Akhtar S., Al-Qarni F.D., Al-Harbi F.A. Flexural Properties and Hardness of CAD-CAM Denture Base Materials. J. Prosthodont. 2023;32:318–324. doi: 10.1111/jopr.13535. [DOI] [PubMed] [Google Scholar]
- 30.Standard Test Method for Vickers Indentation Hardness of Advanced Ceramics. ASTM International; West Conshohocken, PA, USA: 2019. [Google Scholar]
- 31.Kim D., Shim J.-S., Lee D., Shin S.-H., Nam N.-E., Park K.-H., Shim J.-S., Kim J.-E. Effects of Post-Curing Time on the Mechanical and Color Properties of Three-Dimensional Printed Crown and Bridge Materials. Polymers. 2020;12:2762. doi: 10.3390/polym12112762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Song S.-Y., Shin Y.-H., Lee J.-Y., Shin S.-W. Color stability of provisional restorative materials with different fabrication methods. J. Adv. Prosthodont. 2020;12:259–264. doi: 10.4047/jap.2020.12.5.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perchyonok V.T., Souza J., Küll M.F., Suzuki T.Y.U., Maluly-Proni A.T., dos Santos P.H. Color stability and surface roughness of chitosan- and nanodiamond-modified bisacrylic resin. Braz. Oral Res. 2019;33:e024. doi: 10.1590/1807-3107bor-2019.vol33.0024. [DOI] [PubMed] [Google Scholar]
- 34.Tahayeri A., Morgan M., Fugolin A.P., Bompolaki D., Athirasala A., Pfeifer C.S., Ferracane J.L., Bertassoni L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018;34:192–200. doi: 10.1016/j.dental.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bagis B., Turgut S., Kilinc H., Eyupoglu G. Color relationships of natural anterior teeth: An in vivo study. Niger. J. Clin. Pract. 2018;21:925–931. doi: 10.4103/njcp.njcp_361_17. [DOI] [PubMed] [Google Scholar]
- 36.Gad M.M., Fouda S.M. Factors affecting flexural strength of 3D-printed resins: A systematic review. J. Prosthodont. 2023;32((Suppl. S1)):96–110. doi: 10.1111/jopr.13640. [DOI] [PubMed] [Google Scholar]
- 37.Zhang L., He G. Advances in Civil Engineering. Springer; Berlin/Heidelberg, Germany: 2020. Fabrication and Application of Nanosilica Modified Asphalt Binder; pp. 493–515. [Google Scholar]
- 38.Ferracane J.L. Correlation between hardness and degree of conversion during the setting reaction of unfilled dental restorative resins. Dent. Mater. 1985;1:11–14. doi: 10.1016/S0109-5641(85)80058-0. [DOI] [PubMed] [Google Scholar]
- 39.Münchow E.A., Correa M.B., Ogliari F.A., Piva E., Zanchi C.H. Correlation between Surface Roughness and Microhardness of Experimental Composites with Varying Filler Concentration. J. Contemp. Dent. Pract. 2012;13:299–304. doi: 10.5005/jp-journals-10024-1141. [DOI] [PubMed] [Google Scholar]
- 40.Alzahrani S.J., Hajjaj M.S., Azhari A.A., Ahmed W.M., Yeslam H.E., Carvalho R.M. Mechanical Properties of Three-Dimensional Printed Provisional Resin Materials for Crown and Fixed Dental Prosthesis: A Systematic Review. Bioengineering. 2023;10:663. doi: 10.3390/bioengineering10060663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gad M.M., Al-Harbi F.A., Akhtar S., Fouda S.M. 3D-Printable Denture Base Resin Containing SiO2 Nanoparticles: An In Vitro Analysis of Mechanical and Surface Properties. J. Prosthodont. 2022;31:784–790. doi: 10.1111/jopr.13483. [DOI] [PubMed] [Google Scholar]
- 42.El-Tamimi K.M., Bayoumi D.A., Ahmed M.M.Z., Albaijan I., El-Sayed M.E. The Effect of Salinized Nano ZrO2 Particles on the Microstructure, Hardness, and Wear Behavior of Acrylic Denture Tooth Nanocomposite. Polymers. 2022;14:302. doi: 10.3390/polym14020302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Al-Dwairi Z.N., Ebrahim A.A.A.H., Baba N.Z. A Comparison of the Surface and Mechanical Properties of 3D Printable Denture-Base Resin Material and Conventional Polymethylmethacrylate (PMMA) J. Prosthodont. 2023;32:40–48. doi: 10.1111/jopr.13491. [DOI] [PubMed] [Google Scholar]
- 44.Gad M., ArRejaie A.S., Abdel-Halim M.S., Rahoma A. The Reinforcement Effect of Nano-Zirconia on the Transverse Strength of Repaired Acrylic Denture Base. Int. J. Dent. 2016;2016:7094056. doi: 10.1155/2016/7094056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alshahrani F.A. Effect of treated zirconium oxide (ZrO2) nanoparticles on the color and surface properties of interim fixed prostheses. J. Int. Soc. Prev. Community Dent. 2022;12:404–410. doi: 10.4103/jispcd.JISPCD_24_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Taşın S., Ismatullaev A., Usumez A. Comparison of surface roughness and color stainability of 3-dimensionally printed interim prosthodontic material with conventionally fabricated and CAD-CAM milled materials. J. Prosthet. Dent. 2022;128:1094–1101. doi: 10.1016/j.prosdent.2021.01.027. [DOI] [PubMed] [Google Scholar]
- 47.Bollenl C.M., Lambrechts P., Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent. Mater. 1997;13:258–269. doi: 10.1016/S0109-5641(97)80038-3. [DOI] [PubMed] [Google Scholar]
- 48.Alshaikh A.A., Khattar A., Almindil I.A., Alsaif M.H., Akhtar S., Khan S.Q., Gad M.M. 3D-Printed Nanocomposite Denture-Base Resins: Effect of ZrO2 Nanoparticles on the Mechanical and Surface Properties In Vitro. Nanomaterials. 2022;12:2451. doi: 10.3390/nano12142451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Paravina R.D., Ghinea R., Herrera L.J., Bona A.D., Igiel C., Linninger M., Sakai M., Takahashi H., Tashkandi E., Perez M.d.M. Color Difference Thresholds in Dentistry. J. Esthet. Restor. Dent. 2015;27:S1–S9. doi: 10.1111/jerd.12149. [DOI] [PubMed] [Google Scholar]
- 50.Gad M.M., Abualsaud R., Rahoma A., Al-Thobity A.M., Alabidi K., Akhtar S. Effect of zirconium oxide nanoparticles addition on the optical and tensile properties of polymethyl methacrylate denture base material. Int. J. Nanomed. 2018;13:283–292. doi: 10.2147/IJN.S152571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Aszrin F.N., Takarini V., Hasratiningsih Z., Purwasasmita B.S. Translucency Evaluation of Polymethyl Methacrylate (PMMA) Reinforced with ZrO₂-Al₂O₃-SiO₂ Filler System in Fabricating Indirect Restoration. UIP Health Med. 2016;1:1–7. doi: 10.7454/uiphm.v1i0.23. [DOI] [Google Scholar]
- 52.Arikawa H., Kanie T., Fujii K., Takahashi H., Ban S. Effect of Filler Properties in Composite Resins on Light Transmittance Characteristics and Color. Dent. Mater. J. 2007;26:38–44. doi: 10.4012/dmj.26.38. [DOI] [PubMed] [Google Scholar]
- 53.Hébert M., Hersch R.D., Becker J.-M. Compositional reflectance and transmittance model for multilayer specimens. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 2007;24:2628–2644. doi: 10.1364/JOSAA.24.002628. [DOI] [PubMed] [Google Scholar]
- 54.Emami N., Sjödahl M., Söderholm K.-J.M. How filler properties, filler fraction, sample thickness and light source affect light attenuation in particulate filled resin composites. Dent. Mater. 2005;21:721–730. doi: 10.1016/j.dental.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 55.Espinar C., Della Bona A., Pérez M.M., Tejada-Casado M., Pulgar R. The influence of printing angle on color and translucency of 3D printed resins for dental restorations. Dent. Mater. 2023;39:410–417. doi: 10.1016/j.dental.2023.03.011. [DOI] [PubMed] [Google Scholar]
- 56.Da Silva J.D., Park S.E., Weber H.-P., Ishikawa-Nagai S. Clinical performance of a newly developed spectrophotometric system on tooth color reproduction. J. Prosthet. Dent. 2008;99:361–368. doi: 10.1016/S0022-3913(08)60083-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available upon request via email or phone to the corresponding author.