Abstract
Background:
The adverse effects of pulmonary arterial hypertension (PAH) on physical, emotional, and health-related quality of life (HRQoL) remain primarily unrecognized, especially in resource-limited settings.
Objectives:
This study aims to characterize the HRQoL of patients with PAH in this area and also identify the potential role of clinically relevant characteristics, including the 6-min walk distance test (6MWD), WHO-Functional Classification (WHO-FC), and mental health in the occurrence of lowering quality of life.
Design:
This was a cross-sectional observational study.
Methods:
Inpatients with PAH were chosen from a tertiary hospital located in Gansu province, China. All participants were interviewed face-by-face by using questionnaires, including items from the 36-Item Short Form Health Survey (SF-36), the self-rating anxiety scale, and the self-rating depression scale. Data on demographic and clinically relevant characteristics, including WHO-FC and 6MWD, were also collected by tracing medical recorders. Multiple linear regression analysis was used to determine the association between demographic, clinically relevant characteristics data, and physical component summary (PCS) or mental component summary (MCS) in SF-36.
Results:
Of the 152 participants, SF-36 differed significantly from Chinese norms in all eight domains, with role-physical (21.55 ± 9.87) less than one-third of the norm (88.79 ± 28.49). Multiple linear regression results showed that the factors with the greatest impact on PCS were anxiety scores (β = −0.22, p = 0.001), followed by WHO-FC (β = −0.16, p = 0.014) and 6MWD (β = 0.15, p = 0.036). The factors with the greatest impact on MCS were WHO-FC (β = −0.30, p < 0.001), followed by anxiety (β = −0.23, p = 0.001) and depression scores (β = −0.16, p = 0.013).
Conclusion:
HRQoL was substantially reduced among PAH patients in the resource-limited area, mainly the physiological functions. WHO-FC and anxiety scores were independently associated with both PCS and MCS in SF-36. Clinicians should make reasonable rehabilitation programs and plans for patients according to their cardiac function grade and the severity of clinical symptoms. In addition, psychological interventions should also be taken, especially for those with anxiety symptoms, so as to improve their HRQoL.
Keywords: HRQoL, MCS, 6MWD, PAH, PCS, WHO-FC
Background
Disease overview and treatment advances
Pulmonary arterial hypertension (PAH) is a rare, progressive pulmonary vascular disease 1 with a median survival of 5–7 years. 2 Patients with PAH may exhibit features of heart failure due to the decompensation of the right ventricle in the face of elevated pulmonary vascular resistance. 1 Despite traditionally considered to be a rapidly progressive and fatal disease, 1 new PAH-targeted treatments have shown reduced mortality rates, symptom burden, and increased functional capacity in PAH to varying degrees. 2 Consequently, the goals of PAH therapy have shifted from therapeutic objectives to longer-term improvements and health-related quality of life (HRQoL) benefits. 3
HRQoL importance
HRQoL is an important clinical end-point, economic factor, and predictor of prognosis in PAH.1,4 Although the adverse effect of disease symptoms on the physical, emotional, and HRQoL remained largely unrecognized, some clinical factors seem to be highly associated with these outcomes, such as 6-min walk distance test (6MWD), WHO-Functional Classification (WHO-FC), and mental health (MH) (anxiety and depression).2,5,6 Studies have shown that a decline in 6MWD associated with poor HRQoL in PAH.4,7–9 Also, one study indicated that each increase in WHO-FC was associated with a 10-point decline in the overall HRQoL among PAH. 10 In addition, depression and anxiety were common in patients with PAH, which have been shown to have a negative impact on HRQoL in PAH.11,12 Thus, these clinically relevant characteristics become significant predictors for assessing HRQoL or monitoring the disease in PAH.
In addition, the distribution of factors related to HRQoL in PAH varies widely in different regions, levels of economic development, and urbanization.8,13,14 For example, a study in Gansu, China, reported an apparent heterogeneity in the quality of rural life toward hypertension depending on urbanization and altitude. 15 In contrast, depression prevalence seems to decrease with altitude. 16 A study in Colombia also found that living at high altitudes was associated with lower QoL for older adults. 17 A study reported that chronic exposure to high-altitude environments might impact cardiovascular health and disease development, 18 and also the high altitude was positively related to the prevalence of PAH.14,19 All these findings encourage further study of health outcomes with populations living at higher altitudes.
Research gap
For establishing health priorities, especially in resource-constrained settings, it is important to understand the local epidemiology of HRQoL, including within-country heterogeneity. 20 This information may provide evidence to establish suitable interventions, goals, and targets. The present study was produced in Gansu province, China. Gansu lies in the western part of the Loess Plateau and is a transitional area from the Tibetan Plateau to the Loess Plateau. Its altitude ranges between 1500 and 2500 m above sea level, which is commonly defined as high altitude (1500–3500 m). 21 In 2017, Gansu Provincial Hospital took the lead in setting up a pulmonary hypertension clinic in the province, so this group of people has been paid attention. As affected by the regional conditions, the economy and information in Gansu have been relatively less developed, which may further impact the awareness and management of PAH. Currently, the prevalence of PAH in the residents has not been reported. With the standardization of diagnosis and treatment, the number of patients with PAH is increasing. There is also an increasing awareness of the importance of clinical data on PAH to inform decisions on patient management and policy makers. However, the data on HRQoL in these populations are largely unknown; as a result, the purpose of this study is to investigate the characteristics of HRQoL in these groups of patients and subsequently to determine the potential role of 6MWD and WHO-FC in the occurrence of HRQoL impairment. In addition, the effects of depression and anxiety on perceived HRQoL will also be studied. These findings will provide clues to policymakers and researchers to help better manage HRQoL of PAHs in resource-constrained and high-altitude areas.
Methods
Study design
This was a cross-sectional, observational study conducted between March 2020 and April 2022. Patients diagnosed with PAH were recruited from a tertiary hospital located in Lanzhou, the capital city of Gansu province. The reporting of this study conforms to the Strengthening the Reporting of Observational Studies in Epidemiology statement. 22
Study subjects
Inpatients diagnosed with PAH were selected from the chosen hospital. Eligible participants were those aged above 18 years who had undergone clinical treatments with PAH-specific oral compounds or intravenous/subcutaneous prostacyclin analogs and had residency in Gansu province. Subjects were excluded if they presented with severe arrhythmia, acute right heart failure, history of exercise syncope, or any condition that would hinder their ability to complete the study measurements or questionnaires, such as non-ambulatory or visual/hearing impaired.
Study methods
Two trained researchers performed the assessment. The patient’s demographic information (age, gender, marital status, home location, and educational level), lifestyle factors (alcohol drinking and smoking), and clinical-relevant data (WHO-FC, 6MWD) were obtained from electronic medical records. For analysis, smoking and drinking were categorized as non-smokers (never-smokers or ex-smokers) or non-drinkers (never-drinkers or ex-drinkers), and current smokers (at least within the past month) or current drinkers (at least once per week within the past month). Educational level was self-reported and divided into three groups: Junior high school or below, high school, and college/university. Home location was divided into two levels: rural and urban. Then, each participant was interviewed face-by-face at the bedside using a structured questionnaire designed to elicit data on HRQoL and symptoms of anxiety and depression. If the respondent was unable to answer or could not answer correctly for some reason (such as illiteracy), the family carers were invited to fill in the questionnaire. The survey took up to 30 min for each patient. Each time, after completing the questionnaire, one researcher collected it and placed it in a sealed bag for safekeeping. After all patients completed the questionnaire, the other two researchers entered the data into Excel 2016.
Assessment
HRQoL was determined using the Chinese version of the Short Form 36 questionnaire (SF-36), which comprised a physical component score (PCS) and a mental component summary (MCS) score. 23 Following eight domains: physical functioning (PF), role limitations due to physical problems (RP), body pain (BP), general health (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and MH. The PCS comprised PF, RP, BP, and GH scores, while the MCS comprised VT, SF, RE, and MH scores. Item scores were coded, summed, and transformed along a scale from 0 (worst possible health) to 100 (best possible health) for each domain, with higher scores indicating greater satisfaction with QoL. The questionnaire was administered orally to all of the patients by the same therapist.
Most of the detailed data on symptoms of anxiety and depression was published previously by our team. 24 The Self-Rating Anxiety Scale (SAS), which is composed of 20 easily understood questions, was used to assess the frequency of anxiety-related symptoms. 25 For evaluation, the total score (rough score) was obtained by adding the scores of the 20 items. Subsequently, the standard score is obtained through conversion. That is, the crude score is multiplied by 1.25, and then the integer part is taken. The higher the standard score, the more serious the anxiety symptoms. The self-rating depression scale consists of 20 items, and the scoring method is similar to that of SAS. 26 There were 10 positively worded questions and 10 negatively worded questions. Total scores range from 20 to 80. 26
The sample size was computed by following statistical formula with Zα/2 = 1.96, allowable error δ = 2.
Where ‘n’ is the estimated sample size, and ‘σ’ is the standard deviation (SD) of PAH patients’ quality of life score. According to the analysis of pre-survey results, σ = 11.72. Plug the above data into the calculation formula, n=132. To compensate for questionnaires that were discarded due to insufficient information and filling errors, the sample size was increased by 10–20%, with a required sample size of 145–158. In the end, the sample size collected was 152.
Statistical analysis
Statistical analyses were undertaken using the SPSS 21.0 software (IBM Corp, Armonk, NY, USA). First, variables were summarized using descriptive statistics, namely absolute (n) and relative (%) frequencies for categorical variables and mean and SD for numerical variables. Independent sample t test and one-way analysis of variance were used to analyze the differences in demographic characteristics and clinical parameters between PCS and MCS. Pearson correlation analysis was used to analyze the correlation between PCS, MCS, and anxiety and depression scores. Each dimension scores of the SF-36 were calculated, and T test was used to compare them with the norms of the general Chinese population. 27 Multiple linear regression analyses were used to determine the association between WHO-FC, 6MWD, anxiety, depression scores, and PCS and MCS scores. The statistically significant factors in the results of univariate analysis and correlation analysis were included in the multiple linear regression model. During multivariable modeling, the variance inflation factor (VIF) was used to detect multicollinearity. Any predictor with a VIF above 10 was excluded from the final model. For all analyses, the statistical significance level was set at p < 0.05.
Results
Demographic, WHO-FC, and 6MWD
In total, 152 of the patients completed the questionnaire. The median age of the participants was 54.78 ± 14.20 years; 54.6% were female, and 84 (55.3%) were from rural, 44 (29%) had an educational level of high school or above. The mean 6MWD was 353.43 ± 58.65 (205–476) m among the participants. Over 55% of the queues belong to WHO-FC III/IV (Table 1).
Table 1.
Univariate analysis of general characteristics and PCS/MCS in SF-36 (N = 152).
| Characteristics | N (%)/ ± SD | PCS | MCS | ||||
|---|---|---|---|---|---|---|---|
| ± SD | F/t/r | p | ± SD | F/t | p | ||
| Age (years) | 54.78 ± 14.20 | −0.109 a | 0.183 | 0.073 a | 0.369 | ||
| Gender | 8.969 b | <0.001** | 7.167 b | <0.001** | |||
| Male | 69 (45.4) | 56.23 ± 17.05 | 63.95 ± 16.71 | ||||
| Female | 83 (54.6) | 32.32 ± 15.78 | 45.49 ± 15.01 | ||||
| Home location | −2.540 b | 0.012* | −1.431 b | 0.154 | |||
| Rural | 68 (44.7) | 47.83 ± 22.32 | 56.22 ± 17.46 | ||||
| Urban | 84 (55.3) | 39.40 ± 17.59 | 51.97 ± 18.76 | ||||
| Educational level | 1.106 c | 0.334 | 0.005 c | 0.995 | |||
| Junior high school or below | 108 (71.1) | 44.47 ± 20.60 | 53.78 ± 17.92 | ||||
| High school | 15 (9.9) | 36.50 ± 17.88 | 53.96 ± 16.63 | ||||
| College degree or above | 29 (19.1) | 41.81 ± 19.77 | 54.16 ± 20.77 | ||||
| Smoking | −4.386 b | <0.001** | −3.054 b | 0.003** | |||
| Yes | 126 (82.9) | 40.10 ± 20.59 | 51.87 ± 17.15 | ||||
| No | 26 (17.1) | 58.08 ± 14.98 | 63.56 ± 20.60 | ||||
| Drinking | −3.773 b | <0.001** | −3.380 b | 0.001** | |||
| Yes | 132 (86.8) | 41.47 ± 20.59 | 51.99 ± 17.19 | ||||
| No | 20 (13.2) | 54.44 ± 13.12 | 66.30 ± 20.59 | ||||
| WHO-FC | 3.084 b | 0.003** | 3.881 b | <0.001** | |||
| Class I/II | 67 (44.1) | 48.88 ± 22.40 | 60.06 ± 18.69 | ||||
| Class III/IV | 85 (55.9) | 38.68 ± 17.15 | 48.99 ± 16.43 | ||||
| 6MWD (m) | 360.91 ± 11.41 | 0.323 a | <0.001** | 0.249 a | 0.002** | ||
| PCS | 43.73 ± 19.58 | ||||||
| MCS | 55.32 ± 18.92 | ||||||
Pearson correlation coefficient.
Equal to t value.
Equal to F value.
MAP, mean arterial pressure; MCS, Mental Component Total Score; 6MWD, 6-min walk distance; PCS, Physical Component Total Score; SD, standard deviation; WHO-FC, World Health Organization-functional class.
p < 0.05, **p < 0.01.
HRQoL domains and summary scores
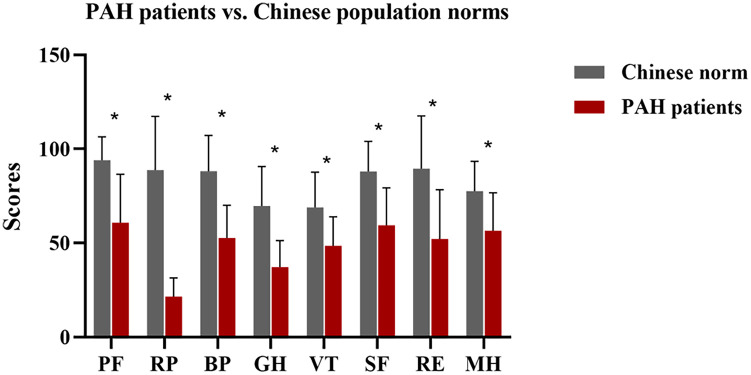
The average PCS and MCS scores in SF-36 were 43.73 ± 19.58 and 55.32 ± 18.92, respectively (Table 1). As shown in Figure 1, HRQoL differed significantly from Chinese normative values in all eight domains (p < 0.05), among which RP (21.55 ± 9.87) was less than one-third of the Chinese norms (88.79 ± 28.49).
Figure 1.
Mean scores of SF-36 for PAH patients versus Chinese population norms.
BP, bodily pain; GH, general health; MH, mental health; PAH, pulmonary arterial hypertension; PF, physical functioning; RE, role-emotional; RP, role-physical; SF, social functioning; VT, vitality.
*p < 0.05.
Univariate analysis of the relationship between WHO-FC, 6MWD, and PCS/MCS
The univariate analysis of the relationship between WHO-FC, 6MWD, and PCS/MCS scores is presented in Table 1. WHO-FC and 6MWD were significantly correlated with PCS, and MCS showed significant correlations with gender, smoking, drinking, WHO-FC, and 6MWD (all p < 0.05).
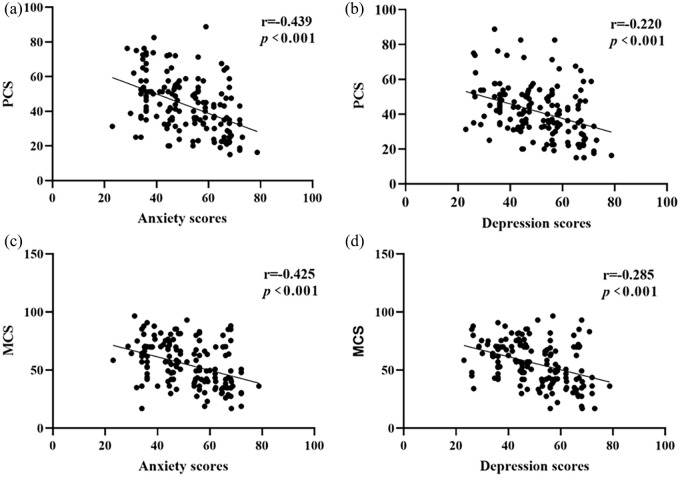
As shown in Figure 2, PCS and MCS scores exhibited a consistent decline with increasing anxiety and depression scores, and there was a strong negative correlation between anxiety scores and PCS (r = −0.439, p < 0.001), as well as MCS (r = −0.425, p < 0.001).
Figure 2.
Associations between the anxiety and depression scores and PCS (a, b) and MCS (c, d).
MCS, Mental Component Total Score; PCS, Physical Component Total Score.
Multiple linear regression analysis of the relationship between WHO-FC, 6MWD, and the PCS/MCS
To exclude the interference of confounding factors, we included statistically significant factors in the univariate analysis results in the multiple linear regression model. The results showed that the most crucial factor influencing PCS was WHO-FC (β = −0.22, p = 0.001), and for every 1-point increase in anxiety scores, PCS decreased by 0.33 points, followed by WHO-FC (β = −0.16, p = 0.014) and 6MWD (β = 0.15, p = 0.036) (Table 2). The factor with the most significant impact on MCS was anxiety scores (β = −0.30, p < 0.001), and PCS decreased by 6.04 points for each grade increase in cardiac function, followed by anxiety scores (β = −0.23, p = 0.001) and depression scores (β = −0.16, p = 0.013) (Table 3). Other parameters associated with the summarized scores of HRQoL were gender and home location for PCS gender for MCS (all p < 0.05).
Table 2.
Multiple linear regression analysis of PCS and general characteristics, anxiety, and depression scores.
| Characteristics | Unstandardized coefficients | Standardized coefficients | t | p | 95% CI | ||
|---|---|---|---|---|---|---|---|
| B | SE | Beta | Lower | Upper | |||
| Gender (female) | −19.40 | 2.80 | −0.48 | −6.93 | <0.001** | −24.93 | −13.86 |
| Home location (rural) | 7.08 | 2.43 | 0.17 | 2.91 | 0.004** | 2.27 | 11.89 |
| Smoking (no) | 1.18 | 4.62 | 0.02 | 0.256 | 0.798 | −7.95 | 10.32 |
| Drinking (no) | −0.12 | 4.96 | −0.00 | −0.03 | 0.980 | −9.93 | 9.68 |
| WHO-FC (class III/IV) | −3.30 | 1.33 | −0.16 | −2.48 | 0.014* | −5.93 | −0.67 |
| 6MWD | 0.05 | 0.02 | 0.15 | 2.11 | 0.036* | 0.00 | 0.09 |
| Anxiety scores | −0.33 | 0.09 | −0.22 | −3.49 | 0.001** | −0.51 | −0.14 |
| Depression scores | −0.08 | 0.10 | −0.05 | −0.78 | 0.439 | −0.27 | 0.12 |
95% CI, 95% confidence interval for B; MAP, mean arterial pressure; 6MWD, 6-min walk distance; SE, standard error; WHO-FC, World Health Organization-functional class.
p < 0.05, **p < 0.01.
Table 3.
Multiple linear regression analysis of MCS and general characteristics, anxiety, and depression scores.
| Characteristics | Unstandardized coefficients | Standardized coefficients | t | p | 95% CI | ||
|---|---|---|---|---|---|---|---|
| B | SE | Beta | Lower | Upper | |||
| Gender (female) | −13.87 | 2.99 | −0.35 | −4.65 | <0.001** | −19.77 | −7.97 |
| Smoking (no) | −3.44 | 4.85 | −0.07 | −0.71 | 0.480 | −13.03 | 6.15 |
| Drinking (no) | 8.61 | 5.16 | 0.15 | 1.67 | 0.097 | −1.59 | 18.82 |
| WHO-FC (class III/IV) | −6.04 | 1.41 | −0.30 | −4.29 | <0.001** | −8.83 | −3.25 |
| 6MWD | 0.02 | 0.02 | 0.07 | 0.91 | 0.366 | −0.02 | 0.07 |
| Anxiety scores | −0.34 | 0.10 | −0.23 | −3.43 | 0.001** | −0.54 | −0.15 |
| Depression scores | −0.25 | 0.10 | −0.16 | −2.50 | 0.013* | −0.45 | −0.05 |
95% CI, 95% confidence interval for B; MCS, Mental Component total Score; 6MWD, 6-min walk distance; SE, standard error; WHO-FC, World Health Organization-functional class.
p < 0.05, **p < 0.01.
Discussion
Although being a PAH population living in a resource-limited and as well as high-altitude area, we have found higher mean PCS and MCS scores than that reported in a systematic review. 13 Our study challenges the notion that altitude and development level significantly impact HRQoL in PAH patients. Previous observation reported a negative relationship between altitude and QoL among older adults, 17 also there is study that found no association between PCS and high altitude. 28 Since contrary results and no previous findings have elucidated the difference in PAH patients in different altitudes areas, further studies are warranted to explore the effectiveness of different altitudes on HRQoL with PAH. Despite the differences, a significant decrease in HRQoL in our sample was observed when compared with the Chinese norms. In addition, contrary to other studies, those from rural areas tended to have higher PCS in SF-36 compared to those from urban areas.5,29 Indeed, while providing benefits like healthcare access, urban living may also lead to stress due to a lack of green spaces and intense social interactions. In addition, a lack of social connections between individuals of a given geographic area in urban may significantly affect their HRQoL. Our study found that higher WHO-FC, shorter 6MWD, and elevated anxiety and depression scores, all indicative of higher risk, were associated with significant PCS and MCS impairment.
Similar to other studies,30–32 our study found that 6MWD was significantly reduced in PAH patients. As indicated in previous studies, 30 this condition was expected to impact HRQoL. Furthermore, in our study, the degree to which 6MWD predicted MCS in the linear regression model was not obvious, indicating that patients’ exercise capacity was more related to PCS than to MCS, which may also be related to the fact that more than 60% of the patients in our study were WHO-FC III/IV. The WHO-FC severity and an overall decrease in 6MWD (mean distance 353.43 ± 58.65 m) may further induce the risk of death and hospitalization. 33 Previous surveys by our team found a significant delay in PAH diagnosis in Gansu, which was also reported in others.24,34,35 The delayed diagnosis may be a significant challenge in the future, especially where resources are limited. In addition, high altitude may also affect 6MWD and WHO-FC in PAH patients. Previous studies have shown that higher pulmonary artery pressure and impaired ventricular function limit exercise capacity in patients chronically exposed to high altitudes.36,37 Studies also found that exposure to moderate altitudes can lead to hypoxemia and reduced exercise capacity. 36 Meanwhile, daily activities in patients at higher altitudes may require relatively higher work rates, resulting in significantly impaired functional capacity. 38
In the context of improved vital and clinical outcomes, enhancing HRQoL will be a primary treatment goal. Thus, these factors must be monitored and assessed within PAH patients, especially when WHO-FC is increasing, to establish better strategies for evaluating patient outcomes. A previous study showed that low altitude positively affects areas of physical and functional status, and those living at lower altitudes reported better overall well-being. 17 In addition, PCS in SF-36 is a significant predictor of follow-up outcomes among PAH. 31 However, a study in Latin America reported that less than 50% of the institutions evaluate QoL in PAH as usual, 39 we suggest HRQoL evaluation deserves more attention in routine care visits, especially in the PCS-related domains. In addition, non-pharmacological strategies such as exercise training and palliative care have remarkably improved 6MWD and the QoL in PAH patients.40–44 Therefore, clinicians should make reasonable rehabilitation programs for PAH patients according to their WHO-FC and 6MWD to improve their HRQoL.
PAH patients are more likely to have anxiety and depression emotions. 45 Patients with anxiety have significantly lower 6MWD, which seriously affects their HRQoL. 45 Our study showed that SF-36 HRQoL scores, including PCS and MCS, were all negatively correlated with anxiety scores. Meanwhile, anxiety scores also showed the most significant on PCS in our study; therefore, enhancing anxiety management could potentially contribute to improved HRQoL among PAH patients. In addition, unlike the results of other studies46,47 that reported an association between depression score and PCS/MCS, we found that depression score was only correlated to MCS in multiple linear regression. Several other investigators have also reported this relationship.48,49 The strength of this relationship is very significant and suggests the possibility that MCS could be significantly improved if it was possible to improve depression. In our previous survey, 24 we found no additional treatment beyond anxiety and depression for PAH in Gansu province, which may suggest that these symptoms were either inadequately recognized or else they were felt to be a natural consequence of the disease. Similar to our findings, several previous studies have emphasized the lack of recognition and treatment of depressive symptoms.48,50 It is important to note that any adverse psychological symptoms can interfere with the management of the disease and affect health outcomes.51,52 Meanwhile, European Society of Cardiology/European Respiratory Society guidelines recommend psychological support for all patients with PAH. 53 This highlights the need for those caring for patients with PAH to screen for depression and anxiety, familiarize themselves with the diagnosis and management of depression and anxiety, and consider referral to MH professionals.
Limitations
There are several limitations to this study. First, as the PAH clinic in Gansu province has been established briefly and PAH is a rare disease, the sample is small, resulting in low statistical power and limited ability to analyze and measure the correlation between clinical parameters and SF-36 in multivariate analysis. In addition, there was no subgroup analysis of the differences in altitude level so that patients may differ in clinical symptoms, psychological problems, and HRQoL with varying altitudes. Finally, we use a generic, rather than PAH-specific, quality of life scale. However, despite these limitations, this study provided clinical data on HRQoL in patients with PAH in this high-altitude and underdeveloped area.
Conclusion
We used the SF-36 to assess the HRQoL and its association with WHO-FC, 6MWT, and MH among PAH patients in a underdeveloped and high-altitude area. The study showed that HRQoL was substantially reduced in these populations compared to healthy ones. Significantly PCS was markedly decreased, and the RF score was less than a third of the general Chinese population. WHO-FC, 6MWT, and anxiety scores were independently associated with summarized PCS, whereas those with lower WHO-FC, higher anxiety, and depression scores had lower summarized scores of MCS for HRQoL. Clinicians should develop tailored rehabilitation programs based on WHO-FC and symptom severity to enhance HRQoL in PAH patients.
Supplemental Material
Supplemental material, sj-docx-1-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-docx-2-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-docx-3-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-docx-5-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-4-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease
Acknowledgments
We are grateful to all participants in this study.
Appendix
Non-standard abbreviations and acronyms
MCS mental component summary
6MWD 6-minute walk test
PAH Pulmonary arterial hypertension
PCS physical component summary
SF-36 36-Item Short Form Health Survey
WHO-FC WHO Functional Classification
Footnotes
ORCID iD: Juxia Zhang  https://orcid.org/0009-0001-0184-4630
https://orcid.org/0009-0001-0184-4630
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Juxia Zhang, Clinical Educational Department, Gansu Provincial Hospital, Lanzhou, Gansu 730000, China.
Yujie Wen, Cardiovascular Department, Gansu Provincial Hospital, Lanzhou, Gansu, China.
Yuhuan Yin, School of Nursing, Gansu University of Chinese Medicine, Lanzhou, Gansu, China.
Yiyin Zhang, School of Nursing, Gansu University of Chinese Medicine, Lanzhou, Gansu, China.
Rong Zhang, School of Nursing, Gansu University of Chinese Medicine, Lanzhou, Gansu, China.
Xiaoli Zhang, School of Nursing, Gansu University of Chinese Medicine, Lanzhou, Gansu, China.
Jianying Ye, School of Nursing, Gansu University of Chinese Medicine, Lanzhou, Gansu, China.
Yuping Feng, School of Nursing, Gansu University of Chinese Medicine, Lanzhou, Gansu, China.
Hongyan Meng, School of Nursing, Gansu University of Chinese Medicine, Lanzhou, Gansu, China.
Declarations
Ethics approval and consent to participate: The study was conducted in accordance with the Declaration of Helsinki. The research proposal was approved by the research committee of Gansu Provincial Hospital (Approval Number: 2019-068). The written consent of the participants was obtained.
Consent for publication: We obtained the participants’ written consent for publication.
Author contributions: Juxia Zhang: Conceptualization; Data curation; Formal analysis; Resources; Validation; Writing – original draft; Writing – review & editing.
Yujie Wen: Conceptualization; Formal analysis; Methodology; Writing – original draft; Writing – review & editing.
Yuhuan Yin: Data curation; Formal analysis; Methodology; Software; Writing – original draft.
Yiyin Zhang: Data curation; Formal analysis; Investigation; Writing – original draft.
Rong Zhang: Formal analysis; Writing – original draft; Writing – review & editing.
Xiaoli Zhang: Data curation; Formal analysis; Investigation.
Jianying Ye: Data curation; Formal analysis; Investigation.
Yuping Feng: Formal analysis; Investigation.
Hongyan Meng: Data curation; Investigation.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the China Medical Education Association Project (2022KTZ010), the Natural Science Foundation of Gansu Province (21JR7RA607 and 21JR7RA613), the Scientific Research Foundation of Gansu Provincial Hospital (22GSSYD-69 and 22GSSYD-70).
The authors declare that there is no conflict of interest.
Availability of data and materials: The datasets used and/or analyzed during the current study are in Chinese and are available from the corresponding author on reasonable request but will require translation to English.
References
- 1. Deshwal H, Weinstein T, Sulica R. Advances in the management of pulmonary arterial hypertension. J Investig Med 2021; 69: 1270–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J 2015; 46: 903–975. [DOI] [PubMed] [Google Scholar]
- 3. Helgeson SA, Menon D, Helmi H, et al. Psychosocial and financial burden of therapy in USA patients with pulmonary arterial hypertension. Diseases 2020; 8: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen Y, Li F, Luo J, et al. Comparative efficacy and safety of targeted therapies for chronic thromboembolic pulmonary hypertension: a systematic review and network meta-analysis. Can Respir J 2021; 2021: 1626971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reis A, Santos M, Vicente M, et al. Health-related quality of life in pulmonary hypertension and its clinical correlates: a cross-sectional study. Biomed Res Int 2018; 2018: 3924517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tamada N, Nakayama K, Yanaka K, et al. Pulmonary endarterectomy and balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension-similar effects on health-related quality of life. Circ Rep 2019; 1: 228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schmidt C, Monteiro M, Furtado I, et al. Physical activity and its clinical correlates in chronic thromboembolic pulmonary hypertension. Pulm Circ 2022; 12: e12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Samaranayake CB, Warren C, Siewers K, et al. Impact of cyanosis on ventilatory responses during stair climb exercise in Eisenmenger syndrome and idiopathic pulmonary arterial hypertension. Int J Cardiol 2021; 341: 84–87. [DOI] [PubMed] [Google Scholar]
- 9. Aueyingsak S, Khrisanapant W, Kukongviriyapun U, et al. Correlation between N-terminal pro-brain natriuretic peptide levels and cardiopulmonary exercise testing in patients with pre-capillary pulmonary hypertension: a pilot study. Clin Med Insights Circ Respir Pulm Med 2020; 14: 1179548420954049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Saglam M, Vardar-Yagli N, Calik-Kutukcu E, et al. Functional exercise capacity, physical activity, and respiratory and peripheral muscle strength in pulmonary hypertension according to disease severity. J Phys Ther Sci 2015; 27: 1309–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Park DH, Meltendorf T, Kahl KG, et al. Health disparities and differences in health-care-utilization in patients with pulmonary arterial hypertension. Front Psychiatry 2022; 13: 813506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dering MR, Lepsy N, Fuge J, et al. Prevalence of mental disorders in patients with chronic thromboembolic pulmonary hypertension. Front Psychiatry 2022; 13: 821466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sarzyńska K, Świa̧toniowska-Lonc N, Dudek K, et al. Quality of life of patients with pulmonary arterial hypertension: a meta-analysis. Eur Rev Med Pharmacol Sci 2021; 25: 4983–4998. [DOI] [PubMed] [Google Scholar]
- 14. Xiong H, Huang Q, He C, et al. Prevalence of chronic obstructive pulmonary disease at high altitude: a systematic review and meta-analysis. PeerJ 2020; 8: e8586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fang F, Ma L, Fan H, et al. The spatial differentiation of quality of rural life based on natural controlling factors: a case study of Gansu Province, China. J Environ Manage 2020; 264: 110439. [DOI] [PubMed] [Google Scholar]
- 16. Wang F, Liu S, Zhang Q, et al. Prevalence of depression in older nursing home residents in high and low altitude regions: a comparative study. Front Psychiatry 2021; 12: 669234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pinzón-Rondón AM, Botero JC, Mosquera-Gómez LE, et al. Altitude and quality of life of older people in Colombia: a multilevel study. J Appl Gerontol 2022; 41: 1604–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mallet RT, Burtscher J, Richalet JP, et al. Impact of high altitude on cardiovascular health: current perspectives. Vasc Health Risk Manag 2021; 17: 317–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Guo Y, Xing Z, Shan G, et al. Prevalence and risk factors for COPD at high altitude: a large cross-sectional survey of subjects living between 2,100–4,700 m above sea level. Front Med (Lausanne) 2020; 7: 581763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bernabe-Ortiz A, Carrillo-Larco RM. Urbanization, altitude and cardiovascular risk. Glob Heart 2022; 17: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Netzer N, Strohl K, Faulhaber M, et al. Hypoxia-related altitude illnesses. J Travel Med 2013; 20: 247–255. [DOI] [PubMed] [Google Scholar]
- 22. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453–1457. [DOI] [PubMed] [Google Scholar]
- 23. Tang Z, Liu C, Guan L, et al. Testing of validity and reliability of simplified Chinese SF-36v2 scale for evaluating the quality-of-life of people immigrating to high altitude. J PLA Med 2017; 42: 1006–1010 (in Chinese). [Google Scholar]
- 24. Zhang J, Yin Y, Wen Y, et al. Anxiety and depression in patients with pulmonary arterial hypertension in Northwest China: a cross-sectional study. Front Psychiatry 2022; 12: 758120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dunstan DA, Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatry 2020; 1: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry 2017; 1: 329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rui Wang, Cheng Wu, Ma XQ, et al. Health-related quality of life in Chinese people: a population-based survey of five cities in China. Scand J Public Health 2011; 39: 410–418. [DOI] [PubMed] [Google Scholar]
- 28. Urrunaga-Pastor D, Runzer-Colmenares FM, Arones TM, et al. Factors associated with poor physical performance in older adults of 11 Peruvian high Andean communities. F1000Research 2019; 8: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mathai SC, Suber T, Khair RM, et al. Health-related quality of life and survival in pulmonary arterial hypertension. Ann Am Thorac Soc 2016; 13: 31–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yagi K, Asakura T, Namkoong H, et al. Association between six-minute walk test parameters and the health-related quality of life in patients with pulmonary Mycobacterium avium complex disease. BMC Pulm Med 2018; 18: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shi Y, Meng Y, Dong X, et al. Quality of life in ambulatory pulmonary arterial hypertension in connective tissue diseases and its relationship with risk stratification. Pulm Circ 2021; 11: 20458940211029899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sharif K, Watad A, Bragazzi NL, et al. Physical activity and autoimmune diseases: get moving and manage the disease. Autoimmun Rev 2018; 17: 53–72. [DOI] [PubMed] [Google Scholar]
- 33. Aldalaan AM, Saleemi SA, Weheba I, et al. Prospective clinical assessment of patients with pulmonary arterial hypertension switched from bosentan to macitentan (POTENT). Pulm Circ 2022; 12: e12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Strange G, Gabbay E, Kermeen F, et al. Time from symptoms to definitive diagnosis of idiopathic pulmonary arterial hypertension: the delay study. Pulm Circ 2013; 3: 89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Maarman GJ. Pulmonary hypertension in developing countries: limiting factors in time to diagnosis, specialised medications and contextualised recommendations. Afr J Thorac Crit Care Med 2022; 28: 10.7196/AJTCCM.2022.v28i1.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Naeije R. Physiological adaptation of the cardiovascular system to high altitude. Prog Cardiovasc Dis 2010; 52: 456–466. [DOI] [PubMed] [Google Scholar]
- 37. Yang T, Li X, Qin J, et al. High altitude-induced borderline pulmonary hypertension impaired cardiorespiratory fitness in healthy young men. Int J Cardiol 2015; 181: 382–388. [DOI] [PubMed] [Google Scholar]
- 38. Levine BD, Zuckerman JH, deFilippi CR. Effect of high-altitude exposure in the elderly: the Tenth Mountain Division study. Circulation 1997; 96: 1224–1232. [DOI] [PubMed] [Google Scholar]
- 39. Benavides-Cordoba V, Barros-Poblete M, Vieira RP, et al. Provision of pulmonary rehabilitation in Latin America 18 months after the COVID-19 pandemic: a survey of the Latin American Thoracic Association. Chron Respir Dis 2022; 19: 14799731221104102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Buys R, Avila A, Cornelissen VA. Exercise training improves physical fitness in patients with pulmonary arterial hypertension: a systematic review and meta-analysis of controlled trials. BMC Pulm Med 2015; 15: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Arena R, Cahalin LP, Borghi-Silva A, et al. The effect of exercise training on the pulmonary arterial system in patients with pulmonary hypertension. Prog Cardiovasc Dis 2015; 57: 480–488. [DOI] [PubMed] [Google Scholar]
- 42. Fenstad ER, Shanafelt TD, Sloan JA, et al. Physician attitudes toward palliative care for patients with pulmonary arterial hypertension: results of a cross-sectional survey. Pulm Circ 2014; 4: 504–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Swetz KM, Shanafelt TD, Drozdowicz LB, et al. Symptom burden, quality of life, and attitudes toward palliative care in patients with pulmonary arterial hypertension: results from a cross-sectional patient survey. J Heart Lung Transplant 2012; 31: 1102–1108. [DOI] [PubMed] [Google Scholar]
- 44. Zeng X, Chen H, Ruan H, et al. Effectiveness and safety of exercise training and rehabilitation in pulmonary hypertension: a systematic review and meta-analysis. J Thorac Dis 2020; 12: 2691–2705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Delcroix M, Howard L. Pulmonary arterial hypertension: the burden of disease and impact on quality of life. Eur Respir Rev 2015; 24: 621–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhou X, Shi H, Yang Y, et al. Anxiety and depression in patients with pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension: results from a Chinese survey. Exp Ther Med 2020; 19: 3124–3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Li MT, Wu M, Xie QL, et al. The association between vascular access satisfaction and quality of life and depression in maintained hemodialysis patients. J Vasc Access 2024; 25: 439–447. [DOI] [PubMed] [Google Scholar]
- 48. Chalhoub NE, Luggen ME. Depression-, pain-, and health-related quality of life in patients with systemic lupus erythematosus. Int J Rheumatol 2022; 2022: 6290736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Schmeding A, Schneider M. Fatigue, health-related quality of life and other patient-reported outcomes in systemic lupus erythematosus. Best Pract Res Clin Rheumatol 2013; 27: 363–375. [DOI] [PubMed] [Google Scholar]
- 50. Zhang L, Fu T, Yin R, et al. Prevalence of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. BMC Psychiatry 2017; 17: 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry 2003; 54: 216–226. [DOI] [PubMed] [Google Scholar]
- 52. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med 2000; 160: 2101–2017. [DOI] [PubMed] [Google Scholar]
- 53. Galiè N, Humbert M, Vachiery JL, et al.; ESC Scientific Document Group. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 2016; 37: 67–119. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-docx-2-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-docx-3-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-docx-5-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-pdf-4-tar-10.1177_17534666241246428 for Impression life with pulmonary hypertension: clinically relevant characteristics and quality of life among patients in Gansu, China by Juxia Zhang, Yujie Wen, Yuhuan Yin, Yiyin Zhang, Rong Zhang, Xiaoli Zhang, Jianying Ye, Yuping Feng and Hongyan Meng in Therapeutic Advances in Respiratory Disease