Abstract
With persistent foot-and-mouth disease virus (FMDV) in BHK-21 cells, there is coevolution of the cells and the resident virus; the virulence of the virus for the parental BHK-21 cells is gradually increased, and the cells become partially resistant to FMDV. Here we report that variants of FMDV C3Arg/85 were selected in a single infection of partially resistant BHK-21 cells (termed BHK-Rb cells). Indirect immunofluorescence showed that the BHK-Rb cell population was heterogeneous with regard to susceptibility to C3Arg/85 infection. Infection of BHK-Rb cells with C3Arg/85 resulted in an early phase of partial cytopathology which was followed at 6 to 10 days postinfection by the shedding of mutant FMDVs, termed C3-Rb. The selected C3-Rb variants showed increased virulence for BHK-21 cells, were able to overcome the resistance of modified BHK-21 cells to infection, and had acquired the ability to bind heparin and to infect wild-type Chinese hamster ovary (CHO) cells. A comparison of the genomic sequences of the parental and modified viruses revealed only two amino acid differences, located at the surface of the particle, at the fivefold axis of the viral capsid (Asp-9→Ala in VP3 and either Gly-110→Arg or His-108→Arg in VP1). The same phenotypic and genotypic modifications occurred in a highly reproducible manner; they were seen in a number of independent infections of BHK-Rb cells with viral preparation C3Arg/85 or with clones derived from it. Neither amino acid substitutions in other structural or nonstructural proteins nor nucleotide substitutions in regulatory regions were found. These results prove that infection of partially permissive cells can promote the rapid selection of virus variants that show alterations in cell tropism and are highly virulent for the same cells.
Foot-and-mouth disease virus (FMDV) is an important animal pathogen of the genus aphthovirus of the Picornaviridae family (48). FMDV usually causes an acute, systemic infection in cloven-hooved animals and cytolytic infections in cell culture. However, FMDV can also establish persistent infections in ruminants (3, 29, 36, 50, 53, 55, 56) and in cell cultures (9, 12, 21). Persistence in cell cultures was established by infecting cloned BHK-21 cells (a population derived from a single cell) with an FMDV of serotype C (clone C-S8c1) that was plaque purified three times (9). The carrier cultures were obtained by growing the cells that survived the cytolytic infection (at a frequency of about 10−3) (9, 37). At the critical step of initiation of persistence, the prevailing event ensuring cell survival and viral replication was the rapid variation of the cells, which became partially resistant to FMDV (37). The FMDV then became increasingly virulent for BHK-21 cells (12, 37). In a virulence assay that measures the minimal amount of virus needed to kill 104 BHK-21 cells in 24 h under standard conditions, the virus shed by persistently infected cells at passage 100, termed R100, was 1,000-fold more virulent than the parental C-S8c1 (51).
The evolution of BHK-21 cells during FMDV persistence could be characterized because treatment of the carrier cells with ribavirin [(1-β-d-ribofuranosyl)-1-H-1,2,4-triazole-3-carboxamide] eliminated the virus from the cells (8). Cured cells, in which virus could not be detected by reverse transcription (RT)-PCR (37), were partially resistant to infection by several isolates of FMDV of serotypes C, O, and A but produced normal yields of other RNA viruses, such as vesicular stomatitis virus, encephalomyocarditis virus, and Semliki Forest virus (9, 12, 37). The degree of resistance to FMDV of carrier cells increased with the passage number of the persistently infected culture (11, 12). The evolving cell populations were heterogeneous with regard to susceptibility to FMDV, as revealed by the analysis of 248 stable cell clones isolated from carrier cells at passages 17, 19, 62, and 74 (11). At least six distinct cell phenotypes were identified, the most-resistant clones producing 104 times less FMDV C-S8c1 progeny than the standard BHK-21 cells (11).
In the present study we have examined the ability of cloned FMDV C3Arg/85 to overcome the resistance of modified BHK-21 cells. C3Arg/85 is a standard South American type C FMDV of which several isolates and cloned preparations have been previously characterized genetically (39, 43) and antigenically (38, 54). The results show a surprising adaptability of FMDV to overcome the cellular barrier in a single infection of a monolayer of modified BHK-21 cells. The selected progeny virus displayed increased virulence for BHK-21 cells and modified BHK-21 cells along with a number of additional phenotypic alterations. Two amino acid substitutions located at the surface of the viral capsid are associated with the dramatic phenotypic changes.
MATERIALS AND METHODS
Cells, viruses, and infections.
The origin of BHK-21 cells and the procedures used for infection of BHK-21 and Chinese hamster ovary (CHO) cell monolayers with FMDV in liquid and in semisolid media have been previously described (2, 12, 16, 52). BHK-Rb cells derive from a subline of BHK-21 cells persistently infected with FMDV C-S8c1. They were cured of FMDV by ribavirin treatment (8) at cell passage 70 after the initiation of persistence. BHK-Rb cells correspond to the population termed C1BHK-Rc1-p70 Rbv in de la Torre et al. (11). BHK-Rb cells were used between passages 9 and 15 after curing with ribavirin. Cell clone BHK-R74-A4 was obtained by growth of a single cell from passage 74 of the persistently infected cell population C1-BHK-Rcip74, as described by de la Torre et al. (11). Cell populations BHK-Rb and BHK-R74-A4 were routinely monitored by RT-PCR amplification with primers corresponding to different regions of FMDV RNA, with negative results. Wild-type CHO cells and the two glycosaminoglycan-deficient CHO mutants pgs D-677 and pgs A-745 were kindly provided by J. D. Esko (27, 35).
The FMDV C3Arg/85 isolate used was passaged twice in BHK-21 cells and plaque purified in BHK-21 cells, and then the cloned virus was passaged three times in BHK-21 cells to produce the viral preparation (working stock) for the experiments described here.
Generation of FMDV C3-Rb.
Subconfluent BHK-Rb cell monolayers were infected either with C3Arg/85 or with plaque-purified viral clones derived from the C3Arg/85 working stock and incubated with Dulbecco modified Eagle medium (DMEM) containing 2% fetal calf serum until the cell monolayer became partially lysed at 2 to 3 days postinfection. At this time, the medium was replaced by DMEM containing 10% fetal calf serum, and the incubation was continued, with the medium changed every 24 h. Virus rescued from the supernatants at 8 to 10 days postinfection was generically designated C3-Rb.
Virulence assay.
The virulence of FMDV for BHK-21 cells and for modified BHK-21 cells is defined as the minimum number of PFU required to kill a designated number of cells in a given time (both parameters are indicated for each experiment) under standard infection conditions (51).
Indirect immunofluorescence assays.
Cells were grown on coverslips, washed extensively with phosphate-buffered saline, placed on ice, rinsed, fixed in acetone (10 min at −20°C), air dried, and stored at −20°C. Immunofluorescence was performed as previously described (28), with a 1:50 dilution of anti-FMDV C3 polyclonal antiserum raised in guinea pigs used as the primary antibody. The secondary antibody was a 1:100 dilution of a fluorescein-conjugated anti-guinea pig immunoglobulin G (Sigma).
Heparin-Sepharose binding of FMDV.
Heparin-Sepharose CL-6B and control Sepharose CL-6B beads (ligand density, ∼2 mg of porcine heparin/ml of drained gel; Pharmacia Biotech) were equilibrated with a combination of DMEM, 25 mM HEPES, and 0.1% fetal calf serum (binding buffer) and resuspended as a 10% (vol/vol) slurry; 200 μl of the slurry was mixed with 300 μl of the virus diluted in binding buffer (105 to 106 PFU). The virus-heparin-Sepharose and virus-Sepharose mixtures were incubated for 1 h at room temperature with gentle stirring and centrifuged at 1,000 × g for 2 min. Virus recovered in the supernatants was quantitated by plaque assay. In all cases, 100% of the input PFU was recovered from the supernatant of the Sepharose CL-6B control beads, indicating stability of the virus during the procedure.
Isolation of viral RNA, cDNA synthesis, PCR amplification, nucleotide sequencing, and determination of the size of the poly(C) tract.
Viral RNA from the supernatants of infected cultures was obtained by treatment with proteinase K and sodium dodecyl sulfate, followed by phenol extraction, as previously described (26). To determine the length of the poly(C) tract, the supernatants of infected cells were treated with 2 μg of DNase per ml and 4.5 μg of pancreatic RNase per ml in 50 mM Tris (pH 7.5)–10 mM MgCl2 for 50 min at 37°C prior to treatment with proteinase K as described above. Amplification of FMDV RNA fragments by RT-PCR was carried out as described by Escarmís et al. (26) either with the sets of primers that have been previously described (2, 25, 26, 51) or with those designed for efficient RT-PCR amplification of the C3Arg/85 genome. The sequences of the oligonucleotide primers used will be provided upon request. DNA fragments were purified from unincorporated deoxynucleoside triphosphates and primers by treatment with shrimp alkaline phosphatase and exonuclease I (Amersham). Nucleotide sequencing was performed on overlapping DNA fragments with either the thermosequenase kit from Amersham or the femtomole DNA cycle sequencing kit from Promega (26). A few sequences were determined with an automatic sequencer (model no. ABI373). To our knowledge, these results provide the first entire genomic sequence of an FMDV of subtype C3. To determine the size of the polyribocytidylate [poly(C)] tract of the FMDV RNA, we treated about 10 ng with 5 U of RNase T1 in TE (10 mM Tris-HCl [pH 8.0], 1 mM EDTA) in a volume of 5 μl for 30 min at 37°C. Then, 1 μl of a 10× kinase buffer (500 mM Tris-HCl [pH 7.5], 100 mM MgCl2, 100 mM dithiothreitol, 8 U of RNasin), 45 μCi of [γ-32P]ATP (150 μCi/μl; 6,000 Ci/mmol), and 2.5 U of T4 polynucleotide kinase were added, and the mixture (final volume, 10 μl) was incubated 30 min at 37°C. The size of the poly(C) tract was determined by electrophoresis in a 6% polyacrylamide–7 M urea gel, with a nucleotide sequence ladder used as a size marker (25).
Extraction and quantification of intracellular FMDV RNA.
To quantify relative amounts of intracellular FMDV RNA, total cellular RNA was extracted by the procedure of Chomczynski and Sacchi (7). Aliquots of RNA corresponding to 105, 104, and 103 cells were spotted onto nitrocellulose filters and hybridized onto a probe covering the entire P1 region of FMDV C3Arg/85. The probe was labelled with [32P]phosphate by using the oligolabelling kit (Pharmacia). Autoradiographs were quantitated by the Fotoanalyst image analysis system (Fotodyne, Inc.).
Positioning of amino acid replacements on the three-dimensional structure of FMDV.
The crystallographic coordinates of C-S8c1 (pdb entry, 1fmd [34]) have been used as a reference to model the amino acid replacements found in FMDV C3-Rb. The substituted residues have been modeled with the program TURBO (47) by placing the side-chain atoms in one of their standard conformations. The structure has been optimized by removing the close contacts by using the same program.
Nucleotide sequence accession numbers.
The nucleotide sequences determined in the present study were deposited in GenBank under accession no. AJ007347 and AJ007572.
RESULTS
Rapid evolution of FMDV C3Arg/85 in BHK-Rb cells.
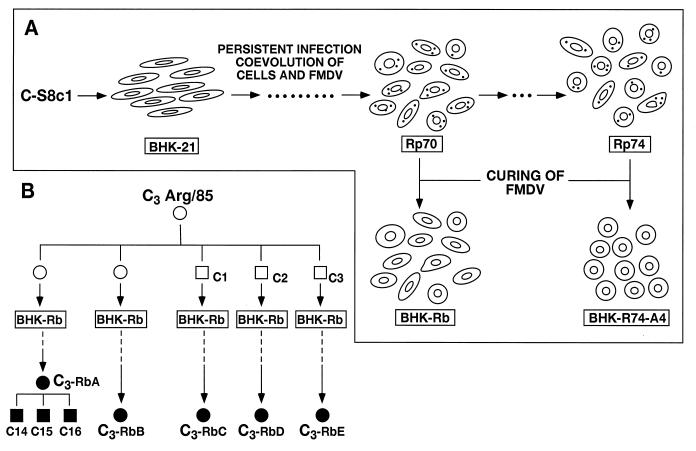
BHK-Rb cells, obtained by eliminating FMDV from persistently infected C1-BHK-Rc1p70 cells (11) (Fig. 1A), were partially resistant to infection by FMDV C3Arg/85. While parental BHK-21 cells infected with C3Arg/85 at a multiplicity of infection of 5 to 10 PFU/cell developed a complete cytopathic effect at 16 to 20 h postinfection, parallel infections in BHK-Rb cells did not show signs of cytopathology until 2 to 3 days after infection. At that time, partial cell lysis was observed. Five independent infections of BHK-Rb cells with either the initial clonal preparation of C3Arg/85 or three clonal derivatives of the same preparation (-c1, -c2, and -c3) (Fig. 1B) were carried out. The 20 to 50% of cells surviving at 2 to 3 days postinfection did not reach confluence in subsequent days and shed virus that was increasingly virulent for the host cells. This finding was revealed by a virulence assay that measures the minimal amount of virus needed to kill BHK-Rb cells under standard infection conditions (51) (Table 1). While 104 to 105 PFU of virus shed at 6 to 10 days postinfection was sufficient to kill the BHK-Rb cells in each of five independent experiments, a 100-fold-higher amount of the parental C3Arg/85 either did not affect or only partially killed the BHK-Rb cells (Table 1). The C3-Rb viruses shed by the BHK-Rb-infected cells at 8 or 10 days postinfection were termed C3-RbA, C3-RbB, C3-RbC, C3-RbD, and C3-RbE (Fig. 1B). In addition to increased virulence for BHK-Rb cells, all these viruses displayed a small-plaque phenotype compared with that of the parental virus in BHK-21 cells and acquired the ability to form plaques on BHK-Rb cell monolayers. The parental working stock of FMDV C3Arg/85 and its three clonal derivatives did not form visible plaques on BHK-Rb cells but formed normal size plaques on BHK-21 cell monolayers. The three subclones C3Rb-Ac14, -c15, and -c16 and the parental C3-RbA population (Fig. 1B) showed identical phenotypes regarding virulence for modified and parental BHK-21 cells and plaque morphology (Table 2).
FIG. 1.
Diagram of the origin of the cells and viruses used in the present study. (A) Persistent infection of BHK-21 cells with FMDV C-S8c1 (9). At passage 70, the persistently infected culture was cured of FMDV by ribavirin treatment (8), yielding the uncloned population BHK-Rb. At passage 74, many cell clones free of FMDV were obtained by terminal dilution (11). One clone that is highly resistant to FMDV is BHK-R74-A4. (B) The C3Arg/85 used is a plaque-purified preparation derived from the natural isolate C3Arg/85 (39, 43) as described in Materials and Methods. Either this preparation (open circles) or one of three plaque-purified subpopulations (-c1, -c2, or -c3 [empty squares]) was used to infect BHK-Rb cells. Viruses rescued from the supernatant of infected BHK-Rb cells at 8 or 10 days postinfection are designated C3-RbA (8 days postinfection), -B, -C, -D, and -E (10 days postinfection) (filled circles). The letters correspond to experiments A to E listed in Table 1. c14, c15, and c16 (filled squares) are clonal subpopulations obtained by plating population C3-RbA onto a BHK-Rb cell monolayer, isolating virus from three single plaques and then passaging the virus twice in BHK-Rb cells. Further details about experimental procedures are given in Materials and Methods.
TABLE 1.
Generation of FMDV variants in BHK-Rb cells
| Expta | FMDVb | Infecting FMDV | Virus shed by BHK-Rb cells at indicated day postinfectionb
|
||
|---|---|---|---|---|---|
| 2 | 6 | 10 | |||
| A | C3Arg/85 | >106d | 106 | 104 | 104 |
| B | C3Arg/85 | >106d | 106 | 104 | 104 |
| C | C3Arg/85c1 | >106c | NDe | >106d | 104 |
| D | C3Arg/85c2 | >106d | ND | 104 | 104 |
| E | C3Arg/85c3 | >106c | ND | >106d | 5 × 104 |
BHK-Rb cells were infected with the FMDVs indicated in the second column at a multiplicity of infection of 5 PFU/cell (experiment A) or 20 PFU/cell (experiments B to E), as described in Materials and Methods. The origins of the infecting FMDV C3Arg/85 and its clonal derivatives -c1, -c2, and -c3 are depicted schematically in Fig. 1 and described in Materials and Methods.
The infecting FMDV C3Arg/85 and virus shed by the infected BHK-Rb cells at the indicated days postinfection were tested for ability to kill BHK-Rb cells in an adaptation of a previously described virulence assay (51). Numbers represent the minimum amount of PFU required to kill 7 × 104 BHK-Rb cells in 48 h.
106 PFU of virus caused no lysis of the cells.
106 PFU of virus caused partial lysis of the cells.
ND, not determined.
TABLE 2.
Properties of FMDV C3Arg/85 and variants selected in BHK-Rb cells
| FMDVa | No. of PFU required to kill indicated cellsb
|
Diameter of plaque (mm)c | ||
|---|---|---|---|---|
| BHK-21 | BHK-Rb | BHK-R74-A4 | ||
| C3Arg/85 | 106 | >106d | >106e | 2–6 |
| C3-RbA | 103 | 104 | NDf | ≤2 |
| C3-RbAc14 | 103 | 104 | 106 | ≤2 |
| C3-RbAc15 | 103 | 104 | 106 | ≤2 |
| C3-RbAc16 | 103 | 104 | 106 | ≤2 |
Virulence for the indicated cells was measured as previously described (51) but with modifications depending upon cell number and time of infection for the three types of cells tested. Numbers represent the minimum number of PFU required to kill 5 × 104 BHK-21 cells in 24 h, 7 × 104 BHK-Rb cells in 48 h, or 105 BHK-R74-A4 cells in 54 h.
The sizes of the plaques were measured at 30 h after plating onto a BHK-21 cell monolayer as previously described (16). For C3Arg/85, ≤5% of the plaques were 2 to 3 mm in diameter, and ≥95% ranged from 3 to 6 mm in diameter.
106 PFU of C3Arg/85 caused a partial cytopathic effect.
106 PFU of C3Arg/85 did not affect cells.
ND, not determined.
Growth characteristics of FMDV C3Arg/85 and C3-Rb in BHK-21, BHK-Rb, and BHK-R74-A4 cells.
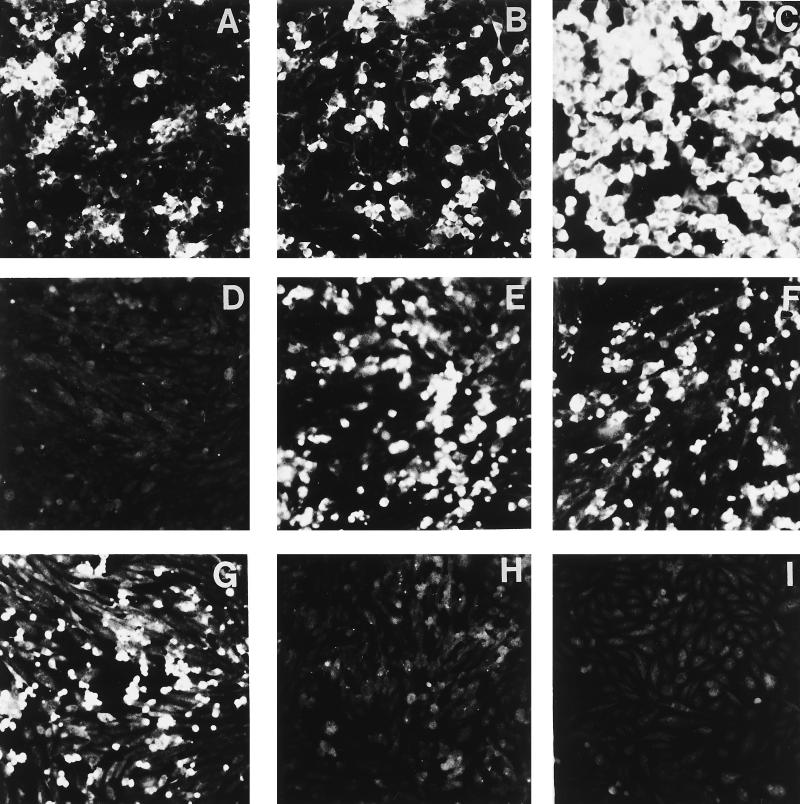
The infection of BHK-21, BHK-Rb, and BHK-R74-A4 cells by C3Arg/85 and its C3-Rb derivatives was studied by immunofluorescence and by a comparative analysis of virus yields and levels of intracellular viral RNA. The limited permissivity of BHK-Rb cells to FMDV C3Arg/85 was due at least in part to the heterogeneity of cells with regard to susceptibility to this virus, as indicated by immunofluorescence analysis. Clusters of brightly fluorescent BHK-Rb cells amounted to only half of the cell population, even at 24 h postinfection (Fig. 2A and B). In contrast, in infections of BHK-Rb cells with FMDV C3-Rb, viral antigens were detected in the majority of cells at 5 h postinfection (Fig. 2C). These results are in agreement with the higher yield of virus in infections with the C3-Rb variants in comparison to that in infections with the parental C3Arg/85 and with the observation of complete killing of BHK-Rb cells at 10 h after infection with C3-Rb variant FMDVs (Fig. 3B and E).
FIG. 2.
Indirect immunofluorescence analysis of BHK-Rb and CHO cells infected with different FMDVs. Cells were infected at a multiplicity of infection of 10 PFU/cell. After virus adsorption (1 h, 37°C) the cell monolayers were extensively washed with DMEM and overlaid with DMEM-fetal calf serum (2% for BHK-Rb cells and 5% for CHO cells). At the time postinfection indicated for each experiment (panels A to I), the presence of FMDV antigens was revealed by indirect immunofluorescence analysis performed as indicated in Materials and Methods. (A to C) BHK-Rb cells were infected with either FMDV C3Arg/85 for 5 h (A) or 24 h (B) or FMDV C3-Rbc15 for 5 h (C). (D to G) Wild-type CHO cells infected for 24 h with C3Arg/85 (D), C3-Rbc15 (E), C3-RbB (F), and C3-RbE (G). (H and I) Mutant CHO pgs D-677 (H) or CHO pgs A-745 (I) infected for 24 h with C3-Rbc15. Results indistinguishable from those shown with C3Arg/85 (panels A, B, and D) were obtained with C3Arg/85c1, -c2, and -c3. Likewise, results indistinguishable from those shown with C3-Rbc15, C3-RbB, and C3-RbE (panels E to I) were obtained with the other C3-Rb viruses selected in BHK-Rb cells (data not shown). The origins of the cells and the FMDVs are described in Materials and Methods, Fig. 1, and Table 1.
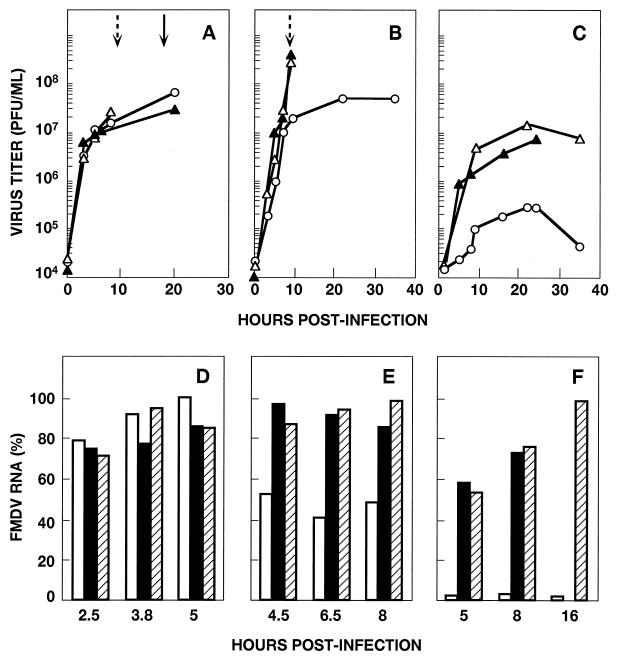
FIG. 3.
Determination of virus production (A to C) and intracellular viral RNA (D to F) upon infection of BHK-21 and modified BHK-21 cells with different FMDVs. BHK-21 cells (A and D) or BHK-Rb cells (B and E) or BHK-R74-A4 cells (C and F) were infected with C3Arg/85 (○), C3-Rbc15 (▵), or C3-Rbc16 (▴) at a multiplicity of infection of 10 PFU/cell. At the indicated times postinfection, samples from the culture medium were withdrawn and titrated (panels A to C). The time at which a complete cytopathic effect was observed is indicated by dotted arrows (infections with C3-Rbc15 or C3-Rbc16) or by a complete arrow (infection with C3Arg/85). For other infections the cytopathic effect observed at the indicated times postinfection was not complete (Table 2). The viral yields from infections with other C3-Rb viruses were very similar to those shown for C3-Rbc15 and -c16. In parallel infections, total cellular RNA was extracted at the indicated times (panels D to F). FMDV RNA was extracted and quantitated by dot blot hybridization as described in Materials and Methods. In panels D to F, numbers on the ordinate represent the accumulated amount of FMDV RNA expressed as the percentage of the maximum value in each experiment. Infections were with C3Arg/85 (empty columns), C3-Rbc15 (columns with stripes), or C3-Rbc16 (filled columns). Procedures for infection with FMDV, titrations with plaque assays, and quantification of FMDV RNA are detailed in Materials and Methods.
The ability of C3-Rb viruses to overcome the BHK-Rb cells’ resistance to infection was further tested with BHK-R74-A4 cells, one of the stable cell clones isolated from an FMDV-C-S8c1 carrier culture that was very resistant to infection by FMDV C-S8c1 (11) (Fig. 1A). Single-step growth curves revealed that while BHK-R74-A4 cells produce 100-fold-lower yields of FMDV C3Arg/85 than the standard BHK-21 cells do, both cell types yield similar amounts of C3-Rb virus (Fig. 3A and C). The resistance of BHK-R74-A4 cells to C3Arg/85 and their permissivity to C3-Rb viruses were confirmed by comparing the levels of intracellular FMDV RNA in infections with either virus (Fig. 3F). In addition, C3-Rb viruses, but not the parental C3Arg/85, were able to kill BHK-R74-A4 cells, although their virulence was lower for these cells than for BHK-Rb or BHK-21 cells (Table 2).
In the parental, unmodified BHK-21 cells, both C3-Rb viruses and the parental C3Arg/85 replicated equally well as indicated by the equivalent amounts of virus yields and by the levels of intracellular FMDV RNA at early times postinfection (Fig. 3A and D). C3-Rb viruses, however, produced complete cell killing at around 9 h postinfection, in contrast to the 16 to 20 h required in infections with C3Arg/85. It should be noted that, in agreement with the latter observation, C3-Rb viruses are 1,000-fold more virulent than the parental C3Arg/85 for BHK-21 cells (Table 2). This finding indicates that the hypervirulence for BHK-21 cells of FMDV C3-Rb is related to factors other than an increase in virus production.
Replication of C3-Rb viruses in CHO cells.
CHO cells under standard conditions cannot be infected by natural FMDV isolates (2, 32, 41, 49). However, adaptation of FMDV to cell culture often leads to populations that can infect CHO cells via interaction with the surface glycosaminoglycan heparan sulfate (2, 32, 41, 49). Thus, it was of interest to determine whether FMDV C3-Rb had acquired the ability to infect CHO cells and to bind heparin. Infection of wild-type CHO cells with C3Arg/85 or with its clonal derivatives -c1, -c2, and -c3 did not produce virus progeny (Table 3). Furthermore, immunofluorescence assays indicated an absence of detectable FMDV antigen in the cells, suggesting an early block in infection (Fig. 2D). In contrast, C3-Rb viruses selected in five independent experiments were able to replicate in wild-type CHO cells as indicated by virus production and by immunofluorescence analysis (Table 3 and Fig. 2E to G). Mutant CHO cells pgs D-677 and pgs A-745, which are deficient in glycosaminoglycans (27, 35), were negative for FMDV antigens by immunofluorescence assays (Fig. 2H and I) and did not yield C3-Rb progeny (results not shown).
TABLE 3.
Replication in wild-type CHO cells and binding to heparin-Sepharose of parental and variant FMDV C3Arg/85 populations
| FMDVa | PFU/PFU ratio
|
|
|---|---|---|
| Replication in wild-type CHO cellsb | Binding to heparin-Sepharosec | |
| C3Arg/85 | 0.9 | 1 |
| C3Arg/85c1 | <0.1 | 1.5 |
| C3Arg/85c2 | <0.1 | 1 |
| C3Arg/85c3 | 1 | 1.6 |
| C3-RbA | 5 × 103 | 16 |
| C3-RbAc15 | 1 × 103 | 10 |
| C3-RbAc16 | 8 × 103 | 13 |
| C3-RbB | 6 × 103 | 10 |
| C3-RbC | 1 × 104 | 18 |
| C3-RbD | 1 × 103 | 11 |
| C3-RbE | 3 × 103 | 20 |
Wild-type CHO cells were infected with virus at a multiplicity of infection of 10 PFU/cell. After virus adsorption (1 h, 37°C), cell monolayers were extensively washed with DMEM–1% fetal calf serum and maintained with DMEM–5% fetal calf serum. Results are expressed as the ratio of PFU/ml in supernatants of the infected cells at 36 h postinfection divided by the PFU/ml in the supernatants at 1 h postinfection (around 103 PFU/ml). In a parallel experiment, replication of C3Arg/85 in BHK-21 cells gave a ratio of 4 × 104 PFU at 20 h postinfection.
Binding experiments were performed as indicated in Materials and Methods. Numbers represent the ratio of PFU in the supernatant of the Sepharose beads after centrifugation divided by the PFU in the corresponding supernatant of the heparin-Sepharose beads after centrifugation (2). Results are the means of at least two independent titrations.
Since infection of CHO cells by C3-Rb viruses required the presence of cell surface heparan sulfate, the abilities of the different virus populations to bind heparin were analyzed. The results (Table 3) show that all variants tested acquired the ability to bind to heparin, although the extent of binding was lower than that reported for FMDV C1 with a long history of passages in cell culture (2).
Few genetic changes are associated with the phenotypic modifications of C3-Rb viruses.
To define the molecular basis of the phenotypic modifications undergone by FMDV C3Arg/85 in its replication in BHK-Rb cells, the entire genomic nucleotide sequence of the working stock of FMDV C3Arg/85 and that of the virulent clone C3-RbAc15 were determined and compared. Only two amino acid substitutions were identified in the viral proteins as follows (Table 4): Asp-9→Ala in VP3 and Gly-110→Arg in VP1. In addition, one silent mutation was identified at position 7624. To determine whether the two amino acid substitutions were consistently found in selected C3Arg/85 variants, the genomic regions corresponding to amino acids 9 of VP3 and 110 of VP1 were sequenced for FMDVs C3-RbA, C3-RbAc16, C3-RbB, C3-RbC, C3-RbD, and C3-RbE. All C3-Rb viruses included an Asp-9→Ala substitution in VP3 and either a His-108→Arg substitution or a Gly-110→Arg substitution in VP1. In particular, C3-RbC was a mixed population containing both His and Arg at position 108 of VP1 and Gly and Arg at position 110 of VP1, with only Ala at position 9 of VP3. C3-RbE included an Asp-9→Ala substitution in VP3 and only a His-108→Arg substitution in VP1. The sequencing of the entire P1-coding region of C3-RbE revealed no other mutations (Table 4). An analysis of 22 molecular clones from population C3-RbC showed that each clone included Arg at either position 108 or position 110 in VP1. None of the clones obtained had sequences with Arg in both positions 108 and 110 of VP1 (44). The size of the poly(C) tract was determined for FMDV C3Arg/85c1, C3Arg/85c2, C3Arg/85c3, C3-RbA, C3-RbAc15, C3-RbAc16, C3-RbB, C3-RbC, C3-RbD, and C3-RbE. No significant variations were seen between the C3-Rb viruses and the parental C3Arg/85; the length of the poly(C) tract in all the genomes analyzed ranged from 204 to 214 C residues.
TABLE 4.
Mutations found in the FMDV C3-Rb genomesa
| FMDV | Nucleotide substitutionb | Amino acid substi-tution (protein)b | Region of the viral genome analyzedb |
|---|---|---|---|
| C3-RbAc15 | A-2619→C | Asp-9→Ala (VP3) | Entire genome |
| G-3578→A | Gly-110→Arg (VP1) | ||
| T-7624→C | — | ||
| C3-RbA | A-2619→C | Asp-9→Ala (VP3) | Residues around posi-tions 2619 and 3578 |
| C3-RbAc16 | G-3578→A | Gly-110→Arg (VP1) | |
| C3-RbB | |||
| C3-RbD | |||
| C3-RbC | A-2619→C | Asp-9→Ala (VP3) | Residues around posi-tions 2619 and 3578 |
| A-3573→G/A | His-108→Arg/His (VP1) | ||
| G-3578→A/G | Gly-110→Arg/Gly (VP1) | ||
| C3-RbE | A-2619→C | Asp-9→Ala (VP3) | Capsid-coding region (P1) |
| A-3573→G | His-108→Arg (VP1) |
The origin of each FMDV analyzed is described in Materials and Methods, Fig. 1, and Table 1. Mutations are defined by comparing the relevant sequences with those of the parental FMDV C3Arg/85. All parental C3Arg/85 preparations (Fig. 1B) showed the wild-type sequence.
Nucleotide numbering is from the 5′ end of the genomic RNA of FMDV C3Arg/85, as described in reference 26;2. Amino acids are numbered independently for each capsid protein. —, silent mutation. In C3-RbC, nucleotides and amino acids separated by lines indicate mixed populations according to the bands in sequencing gels. The locations of the replaced amino acids in the three-dimensional structure of the FMDV capsid are shown in Fig. 4.
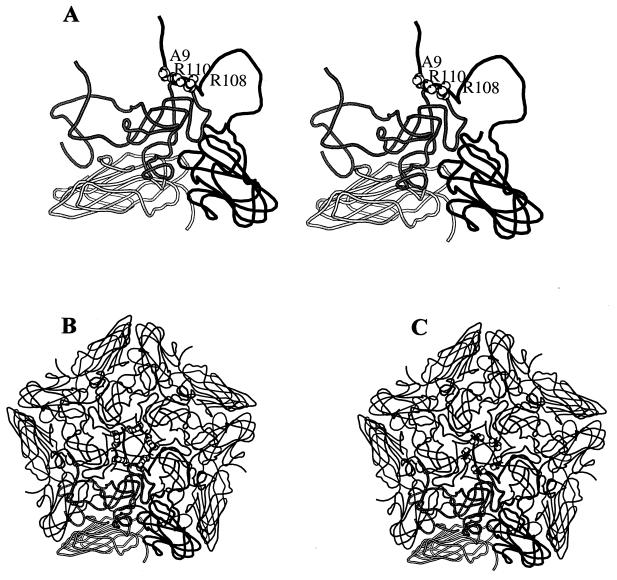
The three amino acid substitutions found in C3-Rb viruses cluster at the virion fivefold axis (Fig. 4) and represent a net increase of positive charges on the virion surface. We conclude that the same two capsid replacements at position 9 of VP3 and at position 108 or position 110 of VP1 were repeatedly selected during infection of BHK-Rb cells by populations of FMDV C3Arg/85 and that these substitutions were associated with the phenotypic modifications of C3-Rb viruses.
FIG. 4.
Location in the three-dimensional structure of FMDV of serotype C (34) of the amino acids replaced in the C3-Rb FMDVs (Asp-9→Ala in VP3 and His-108→Arg in VP1 or Gly-110→Arg in VP1). (A) Stereodiagram of a crystallographic protomer of C-S8c1 in which the three amino acid substitutions are modeled. The capsid proteins VP1, VP2, and VP3 are depicted as grey, white/stippled, and black ribbons, respectively. The substituted residues are shown as spheres and indicated by the single-letter amino acid code (A = Ala; R = Arg). (B) Diagram of the pentamer subunit showing substitutions Asp-9→Ala in VP3 and His-108→Arg in VP1. (C) Pentamer with substitutions Asp-9→Ala in VP3 and Gly-110→Arg in VP1. A reference protomer (lower part of the structure) is depicted as in panel A. The cluster of positive charges around the fivefold axis is apparent in both cases. The procedures used to model the amino acid substitutions are described in Materials and Methods. The structures were drawn by using a modified version of MOLSCRIPT (33).
DISCUSSION
The modified BHK-Rb cells were selected during the course of a persistent infection of cloned BHK-21 cells with FMDV clone C-S8c1 (9, 11, 12). The system selects for variant cells which are partially resistant to the virus and for viruses which are hypervirulent for the cells. This coevolution favors the survival of both the host cells and the resident virus (11, 12, 37). Coevolution of cells and viruses has been described for a number of other viral systems (1, 4–6, 40, 45, 46) and thus cannot be regarded as a rare phenomenon. BHK-Rb cell populations are heterogeneous in that they are composed of cell types that differ in degree of cellular transformation and of resistance to infection by FMDV (11, 12). Upon infection of this heterogeneous cell population with FMDV C3Arg/85, an initial round of partial cell lysis took place on the second to third day postinfection. The more-resistant cells persisted for several additional days, supporting viral replication, as suggested by their continuing viability and the shedding of virus into the culture medium. The cell-to-cell variation in FMDV susceptibility within the BHK-Rb cell population was previously documented by cell cloning and phenotypic testing (11). The cellular heterogeneity has been confirmed and extended in the present study by indirect immunofluorescence analysis of infections with C3Arg/85 (Fig. 2). The negative immunofluorescence of about 50% of the BHK-Rb cells upon infection with C3Arg/85 suggests a block in an early step of the infectious cycle of FMDV in this cell subpopulation (receptor recognition, entry, uncoating, or early protein or RNA synthesis). In the more-resistant BHK-Rb cell subpopulations, variant viruses depicting minimal genetic changes but increased virulence for their host cells were selected. The same amino acid substitutions were selected in independent infections by clonal C3Arg/85 preparations, and therefore were the result of independent mutational events (Fig. 1B and Table 4).
The adaptation of RNA viruses is based on the continuous generation of mutant genomes, resulting in extremely heterogeneous and dynamic mutant swarms, termed viral quasispecies (14, 17, 18, 23, 24, 30). Average mutation rates for a number of RNA viruses have been estimated at 10−3 to 10−5 substitutions per nucleotide and round of copying (reviewed in references 17 and 22). Thus, for an RNA genome of about 8 kb, such as FMDV, with a mutation rate of 10−4 substitutions per nucleotide copied, every progeny RNA molecule produced during a replication process might contain an average of about one mutation. The number of mutations per genome could theoretically follow a Poisson distribution assuming that the occurrence of mutations along the genome is random and assuming their neutral character (15, 20). Obviously, mutations may not occur at random, and many of them will be deleterious and therefore eliminated by negative, or purifying, selection (17). The evolution of a viral quasispecies will be influenced not only by mutational input but also by the number of rounds of genome copying and by the population size of the replicating genomes (17, 20, 23, 24, 30). The quasispecies structure and dynamics predict that variants with one mutation or a few mutations will be common in mutant distributions and thus will be selected whenever they give the virus a selective advantage in the environment at hand (14). This scenario provides a plausible interpretation for the observations described in the present study. Furthermore, repetitive, or deterministic, to use a more fundamental term, selection of the same variants will occur when a limited number of molecular solutions are available to a virus for coping with a selective constraint (17, 19). Had the molecular solutions of C3Arg/85 required a constellation of mutations beyond the reach of the sequence space (23, 24) being explored by the virus to replicate in BHK-Rb cells, adaptation would not have been feasible and the selection of C3-Rb variants would not have occurred. We have previously suggested that functional and structural constraints are probably the main limitations of the evolution of RNA viruses given their high mutation potential (17, 19).
In capsids with icosahedral symmetry, surface residues tend to be more tolerant to replacements than internal capsid residues engaged in interactions with other amino acids (34). The residues at the surface are those that are the most frequently replaced in the course of large population passages of FMDV (26). The two amino acid substitutions found in all the C3-Rb populations analyzed (Asp-9→Ala in VP3 and His-108→Arg or Gly-110→Arg in VP1) cluster at the fivefold axis of the FMDV particle (Fig. 4). This is the site at which the persistent FMDV R100 (13) also includes a cluster of amino acid substitutions, e.g., Asp-9→Ala in VP3. It is interesting that both R100 and the C3-Rb viruses described here have high virulence for BHK-21 cells and a small-plaque morphology (13). Remarkably, the two amino acid substitutions in the capsid of C3Arg/85, without any other substitution in any viral protein, conferred to the C3-Rb viruses an increased virulence for BHK-21 cells, the ability to infect modified BHK-21 cells, a small-plaque morphology, and the potential to bind heparin and infect wild-type CHO cells. This latter change represents a modification of cell tropism that has been documented with a number of different FDMV isolates (2, 32, 41, 49). Jackson et al. (32) showed that binding to cellular heparan sulfate was required by FMDV of serotype O for the efficient infection of cells in culture. Sa-Carvalho et al. (49) documented that heparin binding and cell culture adaptation of FMDV O1 Campos entailed the acquisition of positively charged residues at VP2 residue 134 and VP3 residue 56. In an FMDV of serotype C1 which was subjected to 213 serial cytolytic passages in BHK-21 cells (MARLS virus [2]), two amino acid substitutions (Lys-173→Met in VP3 and Ser-144→Leu in VP1) were associated with the loss of the ability of the virus to bind heparin and infect CHO cells (2). These substitutions affect a capsid region around the G-H loop of VP1, away from the fivefold axis (34). Comparison of results with MARLS and the C3-Rb viruses reinforces the view that the FMDV capsid is an important determinant of virulence for BHK-21 cells (2) and that increased affinity for heparin and alterations in cell tropism may be mediated by a number of independent sites on the viral capsid (2). The systematic selection of the same types of variant C3Arg/85 in BHK-Rb cells shows that when selective forces are strong and the genetic modifications needed to respond to a selective constraint are attainable within the sequence space available to the virus (23, 24), phenotypic shifts can be reproducible and rapid (31).
The repeated selection of two capsid mutations was also observed during persistent infections of poliovirus in primary cultures of human fetal brain cells (42). de la Torre et al. (10) found that transfection of HeLa cells with independent clones of a temperature-sensitive poliovirus mutant resulted not only in the expected transition that eliminated temperature sensitivity but also in four additional silent substitutions that precisely reverted the mutant sequence to that of the wild-type poliovirus. The results with FMDV prove that the replication of viruses in partially permissive cells may promote the selection of genetic and phenotypic variants, including viral mutants with an altered host range. This selection need not be the result of a prolonged persistent infection but can occur during the short-term survival of a virus with a partially permissive host cell. The results of the present study illustrate the impressive adaptive potential of viral quasispecies.
ACKNOWLEDGMENTS
We are indebted to M. Dávila for expert technical assistance and to José Pizarro for help with sequencing experiments.
Work in Madrid was supported by grant PM97-0060-C02 from DEGS, grant PSS0885 from the EU, and the Fundación Ramón Areces. Work in Buenos Aires was supported by CONICET and INTA. M.T.F.-F. thanks Laboratorios BAGO (Buenos Aires, Argentina) for support. Visits to Madrid and Buenos Aires were funded by a CSIC-CONICET cooperative grant. M.T.F.-F.’s sabbatical leave in Madrid was funded by MEC (Spain).
REFERENCES
- 1.Ahmed R, Canning W M, Kauffman R S, Sharpe A H, Hallum J V, Fields B N. Role of the host cell in persistent viral infection: coevolution of L cells and reovirus during persistent infection. Cell. 1981;25:325–332. doi: 10.1016/0092-8674(81)90050-7. [DOI] [PubMed] [Google Scholar]
- 2.Baranowski E, Sevilla N, Verdaguer N, Ruiz-Jarabo C M, Beck E, Domingo E. Multiple virulence determinants of foot-and-mouth disease virus in cell culture. J Virol. 1998;72:6362–6372. doi: 10.1128/jvi.72.8.6362-6372.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burrows R. Studies on the carrier state of cattle exposed to foot-and-mouth disease virus. J Hyg. 1966;64:81–90. doi: 10.1017/s0022172400040365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calvez V, Pelletier I, Couderc T, Pavio-Guédo N, Blondel B, Colbère-Garapin F. Cell clones cured of persistent poliovirus infection display selective permissivity to the wild-type poliovirus strain Mahoney and partial resistance to the attenuated Sabin 1 strain and Mahoney mutants. Virology. 1995;212:309–322. doi: 10.1006/viro.1995.1488. [DOI] [PubMed] [Google Scholar]
- 5.Charini A, Arista S, Giammanco A, Sinatra A. Rotavirus persistence in cell cultures: selection of resistant cells in the presence of fetal calf serum. J Gen Virol. 1983;64:1101–1110. doi: 10.1099/0022-1317-64-5-1101. [DOI] [PubMed] [Google Scholar]
- 6.Chen W, Baric R S. Molecular anatomy of mouse hepatitis virus persistence: coevolution of increased host cell resistance and virus virulence. J Virol. 1996;70:3947–3960. doi: 10.1128/jvi.70.6.3947-3960.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987;162:156–159. doi: 10.1006/abio.1987.9999. [DOI] [PubMed] [Google Scholar]
- 8.de la Torre J C, Alarcón B, Martínez-Salas E, Carrasco L, Domingo E. Ribavirin cures cells of a persistent infection with foot-and-mouth disease virus. J Virol. 1987;61:233–235. doi: 10.1128/jvi.61.1.233-235.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de la Torre J C, Dávila M, Sobrino F, Ortín J, Domingo E. Establishment of cell lines persistently infected with foot-and-mouth disease virus. Virology. 1985;145:24–35. doi: 10.1016/0042-6822(85)90198-9. [DOI] [PubMed] [Google Scholar]
- 10.de la Torre J C, Giachetti C, Semler B L, Holland J J. High frequency of single-base transitions and extreme frequency of precise multiple-base reversion mutations in poliovirus. Proc Natl Acad Sci USA. 1992;89:2531–2535. doi: 10.1073/pnas.89.7.2531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de la Torre J C, Martínez-Salas E, Díez J, Domingo E. Extensive cell heterogeneity during a persistent infection with foot-and-mouth disease virus. J Virol. 1989;63:59–63. doi: 10.1128/jvi.63.1.59-63.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de la Torre J C, Martínez-Salas E, Díez J, Villaverde A, Gebauer F, Rocha E, Dávila M, Domingo E. Coevolution of cells and viruses in a persistent infection of foot-and-mouth disease virus in cell culture. J Virol. 1988;62:2050–2058. doi: 10.1128/jvi.62.6.2050-2058.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Díez J, Dávila M, Escarmís C, Mateu M G, Domínguez J, Pérez J J, Giralt E, Melero J A, Domingo E. Unique amino acid substitutions in the capsid proteins of foot-and-mouth disease virus from a persistent infection in cell culture. J Virol. 1990;64:5519–5528. doi: 10.1128/jvi.64.11.5519-5528.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Domingo E. Biological significance of viral quasispecies. Viral Hepatitis Rev. 1996;2:247–261. [Google Scholar]
- 15.Domingo E. RNA virus evolution, population dynamics, and nutritional status. Biol Trace Elem Res. 1997;56:23–30. doi: 10.1007/BF02778981. [DOI] [PubMed] [Google Scholar]
- 16.Domingo E, Dávila M, Ortín J. Nucleotide sequence heterogeneity of the RNA from a natural population of foot-and-mouth disease virus. Gene. 1980;11:333–346. doi: 10.1016/0378-1119(80)90073-6. [DOI] [PubMed] [Google Scholar]
- 17.Domingo E, Holland J J. Mutation rates and rapid evolution of RNA viruses. In: Morse S S, editor. Evolutionary biology of viruses. New York, N.Y: Raven Press; 1994. pp. 161–184. [Google Scholar]
- 18.Domingo E, Holland J J, Biebricher C, Eigen M. Quasispecies: the concept and the word. In: Gibbs A, Calisher C, García-Arenal F, editors. Molecular basis of virus evolution. Cambridge, United Kingdom: Cambridge University Press; 1995. pp. 171–180. [Google Scholar]
- 19.Domingo E, Mateu M G, Escarmís C, Martínez-Salas E, Andreu D, Giralt E, Verdaguer N, Fita I. Molecular evolution of aphthoviruses. Virus Genes. 1996;11:197–207. doi: 10.1007/BF01728659. [DOI] [PubMed] [Google Scholar]
- 20.Domingo E, Sabo D L, Taniguchi T, Weissmann C. Nucleotide sequence heterogeneity of an RNA phage population. Cell. 1978;13:735–744. doi: 10.1016/0092-8674(78)90223-4. [DOI] [PubMed] [Google Scholar]
- 21.Donn A, Castagnaro M, Donaldson A I. Ultrastructural and replicative features of foot-and-mouth disease virus in persistently infected BHK-21 cells. Arch Virol. 1995;140:13–25. doi: 10.1007/BF01309720. [DOI] [PubMed] [Google Scholar]
- 22.Drake J W. Rates of spontaneous mutations among RNA viruses. Proc Natl Acad Sci USA. 1993;90:4171–4175. doi: 10.1073/pnas.90.9.4171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eigen M. Steps towards life. Oxford, United Kingdom: Oxford University Press; 1992. [Google Scholar]
- 24.Eigen M, Biebricher C. Sequence space and quasispecies distribution. In: Domingo E, Holland J J, Ahlquist P, editors. RNA genetics. Boca Raton, Fla: CRC Press, Inc.; 1988. pp. 211–245. [Google Scholar]
- 25.Escarmís C, Toja M, Medina M, Domingo E. Modifications of the 5′ untranslated region of foot-and-mouth disease virus after prolonged persistence in cell culture. Virus Res. 1992;26:113–125. doi: 10.1016/0168-1702(92)90151-x. [DOI] [PubMed] [Google Scholar]
- 26.Escarmís C, Dávila M, Charpentier N, Bracho A, Moya A, Domingo E. Genetic lesions associated with Muller’s ratchet in an RNA virus. J Mol Biol. 1996;264:255–267. doi: 10.1006/jmbi.1996.0639. [DOI] [PubMed] [Google Scholar]
- 27.Esko J D, Stewart T E, Taylor W H. Animal cell mutants defective in glycosaminoglycans biosynthesis. Proc Natl Acad Sci USA. 1985;82:3197–3201. doi: 10.1073/pnas.82.10.3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferrer M, Hémar A, Duprez V, Hellio R, Dantry-Varsat A. Both the α and β chains of high affinity interleukin 2 receptors are located in intracellular vesicles when their ligand is endocytosed. Eur J Cell Biol. 1993;60:276–282. [PubMed] [Google Scholar]
- 29.Gebauer F, de la Torre J C, Gomes I, Mateu M G, Barahona H, Tiraboschi B, Bergmann I, Augé de Mello M G, Domingo E. Rapid selection of genetic and antigenic variants of foot-and-mouth disease virus during persistence in cattle. J Virol. 1988;62:2041–2049. doi: 10.1128/jvi.62.6.2041-2049.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holland J J, de la Torre J C, Steinhauer D A. RNA viral populations as quasispecies. Curr Top Microbiol Immunol. 1992;176:1–20. doi: 10.1007/978-3-642-77011-1_1. [DOI] [PubMed] [Google Scholar]
- 31.Holland J J, Spindler K, Horodyski F, Grabau E, Nichol S, Van dePol S. Rapid evolution of RNA genomes. Science. 1982;215:1577–1585. doi: 10.1126/science.7041255. [DOI] [PubMed] [Google Scholar]
- 32.Jackson T, Ellard F M, Abu Ghazaleh R, Brookes S M, Blakemore W E, Corteyn A H, Stuart D I, Newman J W I, King A M Q. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J Virol. 1996;70:5282–5287. doi: 10.1128/jvi.70.8.5282-5287.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kraulis P F. MOLSCRIPT: a program to produce both detailed and schematic plots of protein structures. J Appl Crystallogr. 1991;24:946–950. [Google Scholar]
- 34.Lea S, Hernández J, Blakemore W, Brocchi E, Curry S, Domingo E, Fry E, Ghazaleh R A, King A, Newman J, Stuart D, Mateu M G. The structure and antigenicity of a type C foot-and-mouth disease virus. Structure. 1994;2:123–139. doi: 10.1016/s0969-2126(00)00014-9. [DOI] [PubMed] [Google Scholar]
- 35.Lidholt K, Weinke J L, Kiser C S, Lugemwa F N, Bame K J, Cheifetz S, Massagué J, Lindahl U, Esko J D. A single mutation affects both N-acetylglucosaminyltransferase and glucuronosyltransferase activities in a chinese hamster ovary cell mutant defective in heparin sulfate biosynthesis. Proc Natl Acad Sci USA. 1992;89:2267–2271. doi: 10.1073/pnas.89.6.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marilat V, Augé de Mello P, Tiraboschi B, Beck E, Gomes I, Bergmann I E. Genetic variation of foot-and-mouth disease virus during persistent infection in cattle. Virus Res. 1994;34:31–48. doi: 10.1016/0168-1702(94)90117-1. [DOI] [PubMed] [Google Scholar]
- 37.Martín Hernández A M, Carrillo E C, Sevilla N, Domingo E. Rapid cell variation can determine the establishment of a persistent viral infection. Proc Natl Acad Sci USA. 1994;91:3705–3709. doi: 10.1073/pnas.91.9.3705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mateu M G, Da Silva J L, Rocha E, De Brum D L, Alonso A, Enjuanes L, Domingo E, Barahona H. Extensive antigenic heterogeneity of foot-and-mouth disease virus of serotype C. Virology. 1988;166:113–124. doi: 10.1016/0042-6822(88)90060-8. [DOI] [PubMed] [Google Scholar]
- 39.Mateu M G, Hernández J, Martínez M A, Feigelstock D, Lea S, Pérez J J, Giralt E, Stuart D, Palma E L, Domingo E. Antigenic heterogeneity of a foot-and-mouth disease virus serotype in the field is mediated by very limited sequence variation at several antigenic sites. J Virol. 1994;68:1407–1417. doi: 10.1128/jvi.68.3.1407-1417.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mrukowicz J Z, Wetzel J D, Goral M I, Fogo A B, Wright P F, Dermody T S. Viruses and cells with mutations affecting viral entry are selected during persistent rotavirus infections of MA104 cells. J Virol. 1998;72:3088–3097. doi: 10.1128/jvi.72.4.3088-3097.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Neff S, Sa-Carvalho D, Rieder E, Mason P, Blystone S D, Brown E J, Baxt B. Foot-and-mouth disease virus virulent for cattle utilizes the integrin αvβ3 as its receptor. J Virol. 1998;72:3587–3594. doi: 10.1128/jvi.72.5.3587-3594.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pavio N, Buc-Caron M-H, Colbère-Garapin F. Persistent poliovirus infection of human fetal brain cells. J Virol. 1996;70:6395–6401. doi: 10.1128/jvi.70.9.6395-6401.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Piccone M E, Kaplan G, Giavedoni L, Domingo E, Palma E L. VP1 of serotype C foot-and-mouth disease viruses: long-term conservation of sequences. J Virol. 1988;62:1469–1473. doi: 10.1128/jvi.62.4.1469-1473.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rocha, C., and C. Escarmís. 1998. Unpublished results.
- 45.Ron D, Tal J. Coevolution of cells and virus as a mechanism for the persistence of lymphotropic minute virus of mice in L cells. J Virol. 1985;55:424–430. doi: 10.1128/jvi.55.2.424-430.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ron D, Tal J. Spontaneous curing of a minute virus of mice carrier state by selection of cells with an intracellular block of viral replication. J Virol. 1986;58:26–30. doi: 10.1128/jvi.58.1.26-30.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roussel A, Cambillau C. Silicon Graphics geometry partners directory. Mountain View, Calif: Silicon Graphics; 1989. TURBO-FRODO; pp. 77–78. [Google Scholar]
- 48.Rueckert R R. Picornaviridae: the viruses and their replication. In: Fields B N, et al., editors. Fields virology. Philadelphia, Pa: Lippincott-Raven Publishers; 1996. pp. 609–654. [Google Scholar]
- 49.Sa-Carvalho D, Rieder E, Baxt B, Rodarte R, Tanuri A, Mason P. Tissue culture adaptation of foot-and-mouth disease virus selects viruses that bind to heparin and are attenuated in cattle. J Virol. 1997;71:5115–5123. doi: 10.1128/jvi.71.7.5115-5123.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Salt J S. The carrier state in foot-and-mouth disease—an immunological review. Br Vet J. 1993;149:207–223. doi: 10.1016/S0007-1935(05)80168-X. [DOI] [PubMed] [Google Scholar]
- 51.Sevilla N, Domingo E. Evolution of a persistent aphthovirus in cytolytic infections: partial reversion of phenotypic traits accompanied by genetic diversification. J Virol. 1996;70:6617–6624. doi: 10.1128/jvi.70.10.6617-6624.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sobrino F, Dávila M, Ortín J, Domingo E. Multiple genetic variants arise in the course of replication of foot-and-mouth disease virus in cell culture. Virology. 1983;128:310–318. doi: 10.1016/0042-6822(83)90258-1. [DOI] [PubMed] [Google Scholar]
- 53.Sutmoller P, McVicar J W, Cottral G E. The epizootical importance of foot-and-mouth disease carriers. I. Experimentally produced foot-and-mouth disease carriers in susceptible and immune cattle. Arch Gesamte Virusforsch. 1968;23:227–235. doi: 10.1007/BF01241895. [DOI] [PubMed] [Google Scholar]
- 54.Taboga O, Tami C, Carrillo E, Núñez J I, Rodríguez A, Saiz J C, Blanco E, Valero M-L, Roig X, Camarero J A, Andreu D, Mateu M G, Giralt E, Domingo E, Sobrino F, Palma E L. A large-scale evaluation of peptide vaccines against foot-and-mouth disease: lack of solid protection in cattle and isolation of escape mutants. J Virol. 1997;71:2606–2614. doi: 10.1128/jvi.71.4.2606-2614.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van Bekkum J G, Frenkel H S, Frederiks H H J, Frenkel S. Observations on the carrier state of cattle exposed to foot-and-mouth disease virus. Tijdschr Diergeneeskd. 1959;84:1159–1164. [Google Scholar]
- 56.Woodbury E L. A review of the possible mechanisms for the persistence of foot-and-mouth disease virus. Epidemiol Infect. 1995;114:1–13. doi: 10.1017/s0950268800051864. [DOI] [PMC free article] [PubMed] [Google Scholar]