Abstract
Crimean-Congo hemorrhagic fever virus (CCHFV) is a widely distributed hemorrhagic fever virus found throughout Eastern Europe, Africa, the Middle East and Asia. It is spread through bites from infected ticks, animal husbandry and can also be acquired in the healthcare setting during care of infected patients. In humans, CCHFV can cause a sudden onset of a non-specific febrile illness that can rapidly progress to severe hemorrhagic manifestations. Currently, there is no widely available vaccine and although ribavirin has been suggested for the treatment of CCHFV, clinical efficacy in both animal models and humans is inconsistent suggesting more potent antivirals are needed for CCHFV. Favipiravir is approved in Japan for the treatment of influenza virus infections and has shown promise against other highly pathogenic RNA viruses including CCHFV with demonstrated efficacy in the type I interferon deficient mouse model. In this report we utilized the cynomolgus macaque model to evaluate the efficacy of once- and twice-daily favipiravir treatment against CCHFV infection. We found that favipiravir treatment suppressed viremia and viral shedding when treatment was initiated 24 h post-infection and viral burdens in key tissues trended lower in favipiravir-treated animals. Our data indicate that favipiravir has efficacy against CCHFV in vivo in a non-human primate model of infection.
Keywords: Crimean-Congo hemorrhagic Fever, Favipiravir, Antiviral, Macaques
1. Introduction
Crimean-Congo hemorrhagic fever virus (CCHFV) is a widely distributed tick-borne virus in the Nairoviridae family, order Bunyavirales. Its reservoir and vector are ticks of the Hyalomma genus which are found throughout Europe, Africa, the Middle East and Asia (Bente et al., 2013). Humans can become infected through tick bites, butchering of livestock and nosocomial transmission in health care settings (Ergonul, 2006). Crimean-Congo hemorrhagic fever (CCHF) begins with a non-specific febrile illness and then may progress to a serious hemorrhagic disease with uncontrolled bleeding from various sites around the body in which the case fatality rate can vary between 5 and 30% (Bente et al., 2013). Risk factors for death include high viral loads, elevated liver enzymes and clotting deficiencies (Swanepoel et al., 1989; Cevik et al., 2008; Duh et al., 2007; Ergonul et al., 2006). Currently, treatment of CCHFV is limited to supportive care although the nucleoside analog ribavirin is recommended by the World Health Organization for the treatment of CCHF (Crimean-Congo haemorrhagic fever, 2017). However, clinical evidence for the efficacy of ribavirin treatment is inconsistent (Soares-Weiser et al., 2010; Koksal et al., 2010; Johnson et al., 2018; Ascioglu et al., 2011) and has attracted significant debate among clinicians and researchers (Ascioglu et al., 2009; Ergonul, 2009, 2014; Arda et al., 2012). A recent meta-analysis of ribavirin treatment for cases of CCHF suggests that early treatment, within 48 h of symptom onset, is needed for clinical benefit (Ergonul et al., 2018). This may be difficult to achieve as the early symptoms of CCHF are non-specific and may not prompt patients to seek treatment unless they have an obvious likely exposure to CCHFV. Mouse model data for ribavirin treatment against CCHFV also suggests that treatment must be started soon after infection to see clinical benefit (Bente et al., 2010), however, two other studies, including one from our group, showed that even early ribavirin treatment (within 6 h post infection (HPI)) could not protect CCHFV-infected mice from death (Oestereich et al., 2014a; Hawman et al., 2018). Therefore, an antiviral that can exhibit clinical benefit even when patients are exhibiting the more serious signs of CCHF is needed.
Favipiravir is licensed in Japan for the treatment of influenza virus and has been shown in multiple animal models to have antiviral efficacy against several highly pathogenic RNA viruses including Ebola, Lassa, Hantavirus, Nipah and others (Furuta et al., 2013, 2017; Dawes et al., 2018). Favipiravir has been evaluated against CCHFV in the type I interferon-deficient mouse model. In both a study by Oestereich et al. and our group, favipiravir treatment effectively suppressed viral replication in several tissues and could prevent lethality (Oestereich et al., 2014a; Hawman et al., 2018) suggesting favipiravir is an effective antiviral against CCHFV.
Our group recently developed a cynomolgus macaque model in which animals infected with the clinical isolate strain Hoti recapitulate many aspects of human CCHF cases (Haddock et al., 2018). With our previously reported potent antiviral efficacy of favipiravir in Hoti-infected mice we therefore evaluated the efficacy of favipiravir treatment against CCHFV in the cynomolgus macaque model. We found that once-or twice-daily favipiravir treatment suppressed viral loads in the blood and reduced viral shedding in the oral and nasal cavities. Further, viral loads within key tissues of favipiravir-treated animals trended lower than placebo-treated animals. Cumulatively, our data suggest that favipiravir has modest clinical benefits in CCHFV-infected macaques.
2. Materials and methods
2.1. Ethics and biosafety
All animal experiments were approved by the Institutional Animal Care and Use Committee of Rocky Mountain Laboratories, NIH and carried out by certified staff in an Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) International ac-credited facility, according to the institution's guidelines for animal use, and followed the guidelines and basic principles in the United States Public Health Service Policy on Humane Care and Use of Laboratory Animals, and the Guide for the Care and Use of Laboratory Animals. Cynomolgus macaques were housed in adjacent individual primate cages allowing social interactions, in a climate-controlled room with a fixed light-dark cycle (12-hr light/12-hr dark). Animals were monitored at least twice daily throughout the experiment. Commercial monkey chow, treats, and fruit were provided twice daily by trained personnel. Water was available ad libitum. Environmental enrichment consisted of a variety of human interaction, commercial toys, videos, and music. The Institutional Biosafety Committee (IBC) approved work with infectious CCHF under BSL4 conditions. Sample inactivation was performed according to IBC-approved standard operating procedures for removal of specimens from high containment.
2.2. Virus
CCHFV strain Hoti used in this study was described previously (Hawman et al., 2018).
2.3. Animals
Twenty adult cynomolgus macaques (6 males and 14 females) were divided into placebo or favipiravir treatment groups. Animals were infected with 105 tissue culture infectious dose 50s (TCID50s) of CCHFV strain Hoti simultaneously via the subcutaneous (SC) and intravenous (IV) routes as described previously (Haddock et al., 2018). Animals were monitored and evaluated by research and veterinary staff at least twice a day. At time of clinical exams on days 0, 1, 3, 5, 7 and 8 post-infection (PI), blood was collected for virology, hematology and serum chemistry analysis. Hematology was completed on a Procyte DX (IDEXX Laboratories, Westbrook, ME, USA) and the following parameters were evaluated: red blood cells (RBC), hemoglobin (Hb), hematocrit (HCT), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), red cell distribution weight (RDW), platelets, mean platelet volume (MPV), white blood cells (WBC), neutrophil count (abs and %), lymphocyte count (abs and %), monocyte count (abs and %), eosinophil count (abs and %), and basophil count (abs and %). Serum chemistries were completed on a Vetscan VS2 Chemistry Analyzer (Abaxis, Union City, CA) and the following parameters were evaluated: glucose, blood urea nitrogen (BUN), creatinine, calcium, albumin, total protein, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), total bilirubin, globulin, sodium, potassium, chloride, and total carbon dioxide. Animals were euthanized on day + 8.
2.4. Drug treatment
Favipiravir was generously provided by the FUJIFILM Toyama Chemical Co. Ltd. Vehicle was United States Pharmacopeia grade meglumine (Sigma) solution at 74.6 mg/mL in sterile water (Gibco). Favipiravir was dissolved in vehicle at 60 mg/mL. For the once daily-treatment regimen, a loading dose of 300 mg/kg favipiravir was administered IV 24 HPI and thereafter 300 mg/kg was administered SC every 24 h. For the twice-daily regimen, a loading dose of 300 mg/kg was given 24 HPI IV and thereafter 150 mg/kg was administered SC every 12 h. Placebo treated animals received similar injections of meglumine vehicle alone. The pH of the meglumine-alone solution was adjusted to physiologic pH with hydrochloric acid (Sigma). Treatment appeared to be well tolerated with no overt adverse events attributable to the treatment.
2.5. Virus quantification
Virus in the blood or tissues was quantified by qRT-PCR as previously described (Hawman et al., 2018).
2.6. Drug quantification
Serum was collected and stored promptly at −80C. Serum was then subjected to 8 megarads of gamma irradiation according to approved procedures to inactivate infectious CCHFV (Feldmann et al., 2019) and drug quantified in the serum by liquid-chromatography mass-spectrometry. A standard-curve of known concentrations of favipiravir spiked into healthy cynomolgus macaque serum (Innovative Research) was prepared and irradiated in parallel to experimental samples. For detailed methods see supplemental material.
2.7. Histopathology
Histopathology on hematoxylin and eosin stained sections and immunohistochemistry for CCHFV antigen was performed as previously described (Haddock et al., 2018).
3. Results
3.1. Favipiravir treatment suppresses viremia and viral shedding
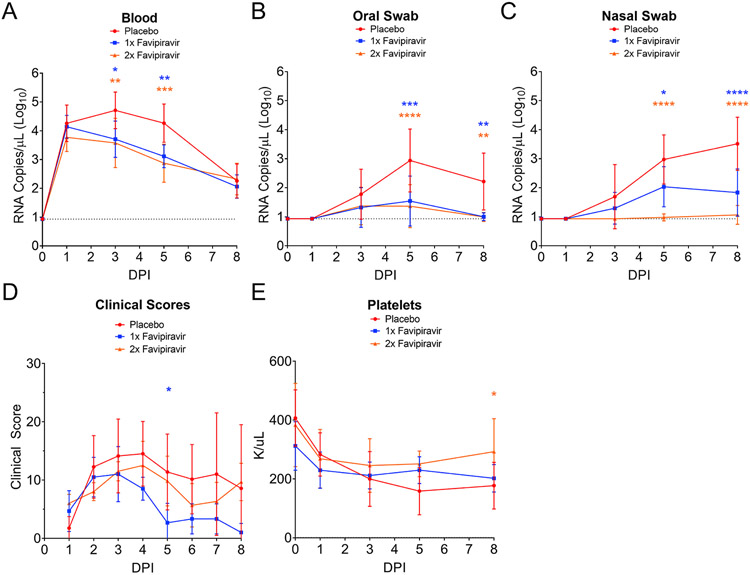
Prior to infection, animals were randomly assigned to favipiravir or placebo-treatment groups. In the first study, groups of six adult cynomolgus macaques, 3 males and 3 females, were infected simultaneously by the IV and SC routes with 100,000 TCID50 as previously described (Haddock et al., 2018). Twenty-four HPI, favipiravir treatment (300 mg/kg) was initiated with treatments occurring once-daily. As control, 6 placebo-treated animals, 3 males and 3 females, received vehicle (meglumine) alone on a similar schedule. In the second study a group of six adult female cynomolgus macaques were similarly infected and 24 HPI favipiravir treatment was initiated with treatments occurring every 12 h. Two female placebo-treated animals received vehicle on the twice-daily schedule. Animals were monitored for clinical signs of disease and blood and oral and nasal swabs collected for analysis of viremia and viral shedding. We found that both groups achieved similar viral RNA titers in the blood at day 1, prior to initiation of treatment. However, thereafter the favipiravir treated animals had significantly reduced viremia on days 3 (10-fold reduction) and 5 PI (20-fold reduction) (Fig. 1A and Supplemental Fig. 1A). Furthermore, viral RNA loads in the blood of placebo treated animals peaked at day 3 PI (mean = 4.7 log10 copies/mL) while viral RNA loads in the blood of favipiravir treated animals peaked at day 1 (mean 3.7 to 4.1 log10 copies/mL), prior to start of treatment. Similarly, favipiravir treated animals had significantly reduced viral shedding in the oral and nasal cavities (30–100-fold reductions at day 5 PI) (Fig. 1B and C and Supplemental Fig. 1B and C). Clinically, placebo-treated animals had clinical scores that trended higher than favipiravir-treated animals although significant differences were only observed on day 5 between placebo and once-daily treated animals (Fig. 1D and Supplemental Fig. 1D). Clinical scores of twice-daily favipiravir treated animals trended higher than once-daily favipiravir animals, although this may have been due to the twice-daily anesthesia this group received. Common clinical findings in the placebo-treated group were hunched posture, decreased appetite and piloerection. In the favipiravir-treated group, clinical findings were most often decreased appetite. Thrombocytopenia is often associated with severe CCHF (Swanepoel et al., 1989; Cevik et al., 2008). Compared to twice-daily favipiravir-treated animals, placebo-treated animals, had significantly decreased platelet counts on day 8 (Fig. 1E).
Fig. 1. Favipiravir treatment reduces viremia and viral shedding.
(A–C) Viral RNA loads in the blood, oral swabs and nasal swabs of once-daily (1x favipiravir), twice-daily (2x favipiravir) and placebo-treated groups were quantified by qRT-PCR. Quantification was performed against an RNA standard of known copy number. Dashed line indicates limit of detection. (D) Animals were scored for clinical disease at least daily by trained personal. (E) Platelet counts were determined from EDTA-treated whole blood on a ProCyte DX hematology analyzer. (A–E) Statistical comparison was performed using a two-way ANOVA with Sidak's multiple comparison test. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
One animal in the once-daily placebo treated group reached euthanasia criteria on day 5 PI. Clinical signs at time of euthanasia were significant lethargy, no response to human presence, no interest in treats, hunched posture, piloerection and petechiae and ecchymosis on the face. Upon necropsy the animal was found to have an enlarged, pale liver with mottled lipidosis. In addition to these clinical findings, at time of euthanasia, the animal had high viral loads in multiple tissues, elevated liver enzymes and decreased platelets, non-regenerative anemia, electrolyte derangement, low albumin, low total protein and lymphopenia (Table S1). Histologically, the animal had marked liver necrosis along with depletion of lymphocytes in the white pulp and fibrin deposition in the red pulp of the spleen (Table S1). In addition, one animal in the twice-daily placebo treated group showed progressively worsening liver enzymes and increasing clinical scores through day 8 PI (Supplemental Fig. 1D – F) suggesting a worsening of disease in this animal. Nevertheless, due to declining viremia in the remaining animals between day 5 and 8 PI, we elected to perform a necropsy on all remaining animals on day 8 PI to quantify viral loads within tissues.
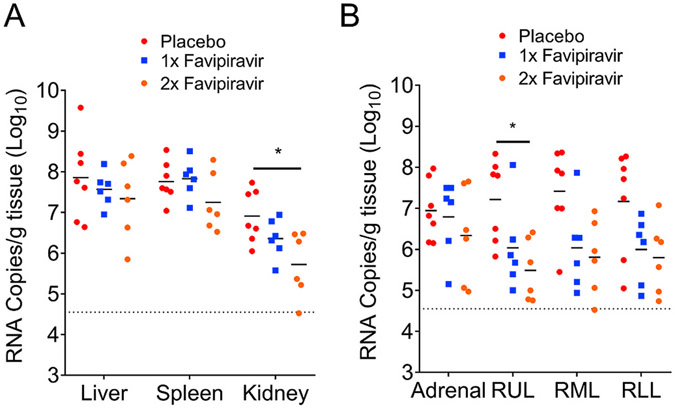
3.2. Viral loads and histopathology in favipiravir-treated animals
As the cynomolgus macaque model of CCHF is not uniformly lethal and we could not power the study to determine differences in survival, on day 8 PI, animals were euthanized, and tissues collected for viral load analysis. We found that once-daily favipiravir-treated animals had viral loads that were similar to placebo-treated animals in the liver and spleen. In the kidney, significantly reduced viral loads were seen in the twice-daily favipiravir-treated animals compared to placebo-treated animals, and overall a trend towards reduced viral loads in several tissues was seen in twice-daily favipiravir-treated animals (Fig. 2A). In several lobes of the lungs, the viral loads in the favipiravir-treated animals trended lower but we only detected significant reductions in viral loads in the right upper lung lobe between placebo and twice-daily favipiravir-treated animals (Fig. 2B). In the once-daily treatment study we attempted to detect infectious virus in the liver and spleen by focus forming assay but we were unable to detect infectious virus in either placebo- or favipiravir-treated animals (data not shown).
Fig. 2. Quantification of viral loads within tissues of favipiravir-treated animals.
(A–B) Viral loads in the indicated tissues collected at necropsy on day 8 PI were quantified by qRT-PCR. Dashed line indicates limit of detection. “Adrenal” = adrenal gland. RUL, RML, RLL = right upper, right middle and right lower lung lobe, respectively. Statistical comparison was performed using a two-way ANOVA with Sidak's multiple comparison test. *p < 0.05.
Immunohistochemistry to detect viral antigen identified rare infected hepatocytes in 4 of 8 placebo-treated animals but only 2 of 12 favipiravir-treated animals (Table 1). Histological examination of the liver identified necrosis in 4 of the 8 placebo-treated animals and none of the favipiravir-treated animals (Table 1) suggesting favipiravir may prevent liver necrosis following CCHFV-infection. Interestingly, histological examination of the liver showed mild-to-moderate vacuolar degeneration in 5 of 6 twice-daily favipiravir-treated animals compared to only 1 of 6 once-daily favipiravir-treated animals. Similarly, 2 of 2 twice-daily placebo treated and only 1 of 6 once-daily placebo-treated animals showed vacuolar degeneration. We hypothesize that this pathology may be due to the more frequent anesthesia in the twice-daily treated groups. Examination of the spleen showed no pathology in any animals. The histological findings and presence of viral antigen in the liver for all animals is shown in Table 1. Cumulatively, these data suggest that favipiravir treatment may reduce viral antigen expression in the liver. However, our data is limited due to the low amount of antigen present even within placebo-treated animals.
Table 1.
Summary of histology and IHC results. Sections of liver collected at necropsy were fixed with formalin, stained with hematoxylin and eosin and scored by pathologists. To detect presence of CCHFV antigen positive cells by IHC, formalin fixed sections of liver were stained with an antibody against the CCHFV nucleoprotein and scored by pathologists. 0 = absent, 1 = minimal, 2 = mild, 3 = moderate, 4 = marked, 5 = severe. * = Animal necropsied on day 5 PI. All others necropsied on day 8 PI.
| 1x Placebo | 2x Placebo | 1x Favipiravir | 2x Favipiravir | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Liver histology | ||||||||||||||||||||
| necrosis | 1 | 4* | 3 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| vacuolar degeneration, lipid type | 0 | 0* | 2 | 0 | 0 | 0 | 1 | 3 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 | 1 | 2 | 1 | 1 |
| Immunohisto-chemistry | 0 | 2* | rare | rare | rare | 0 | 0 | rare | rare | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | rare |
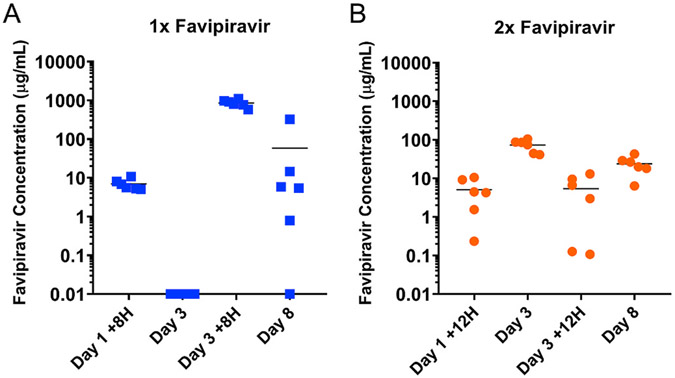
3.3. SC favipiravir treatment resulted in significant concentrations of favipiravir in the serum
Cumulatively, our clinical and virological data suggest that favipiravir had moderate impact on CCHFV replication and overt pathogenesis. To exclude the possibility that subcutaneous delivery of favipiravir was inefficient, we evaluated the serum concentrations of favipiravir in once- and twice-daily treated animals to determine whether the modest impact on CCHFV we observed in treated animals was due to insufficient favipiravir concentrations. Favipiravir has a reported 50% effective concentration 50 (EC50) against CCHFV in vitro of 1.1 μg/mL or less (Oestereich et al., 2014a; Welch et al., 2017; Madelain et al., 2017). Concentration of favipiravir in gamma irradiated serum of placebo- or favipiravir-treated animals at several timepoints was quantified by mass spectrometry in comparison to a standard curve of known concentrations of favipiravir spiked into healthy cynomolgus macaque serum (Fig. 3). As expected, all placebo-treated animals had undetectable levels of favipiravir at all timepoints evaluated (data not shown). Quantification of favipiravir in the serum of the once-daily treated animals indicated that just prior to treatment on day 3, 24 h after last treatment, concentrations of favipiravir were undetectable (Fig. 3A). These data suggest trough concentrations of favipiravir early in the treatment course were below effective concentrations to inhibit viral replication. However, 8 h post-treatment on day 3 favipiravir concentrations in several hundred-fold excess of the EC50 were detected (mean 856 μg/mL) (Fig. 3A) indicating SC administration of favipiravir effectively delivered favipiravir to the circulation. Further, mean serum concentration on day 8, 24 h after treatment on day 7 was 58.7 μg/mL (Fig. 3A) suggesting trough concentrations increased later in treatment. However, one animal had undetectable levels of favipiravir (assay limit of detection 10 ng/mL) at this timepoint (Fig. 3A) indicating in at least some animals, once-daily favipiravir treatment was insufficient to maintain effective concentrations of favipiravir in the serum. Compared to once-daily treatment, twice-daily administration of favipiravir resulted in higher trough concentrations with favipiravir detected in the serum of all animals at all timepoints (Fig. 3B). However, twice-daily treatment resulted in lower peak concentrations at the timepoints evaluated (Fig. 3B). Cumulatively, our data suggests that once-daily treatment results in peak serum concentrations of favipiravir well in excess of the reported EC50 for CCHFV but several days of treatment are needed until trough concentrations are maintained above this value in most animals. In contrast, twice-daily treatment results in lower peak concentrations of favipiravir but trough concentrations of at least the reported EC50 were achieved by the third day of treatment. In addition, our data demonstrate that subcutaneous administration of favipiravir is a viable route of drug delivery for non-human primates, an important consideration for non-human primate studies conducted at BSL-4 conditions.
Fig. 3. SC administration of favipiravir results in significant concentrations of favipiravir in the serum.
At indicated timepoints for animals receiving once-daily (A) or twice-daily (B) favipiravir treatment serum was collected and concentration of favipiravir quantified by LC-MS. On days 1 and 3 PI, blood was collected at 8 or 12 h post-treatment, + 8H or +12H respectively. ND = not done. N = 6 per timepoint. Limit of detection was 0.01 μg/mL.
4. Discussion
Favipiravir has been successfully used to treat several highly pathogenic RNA virus infections including Ebola and Lassa virus in small animal models (Oestereich et al., 2014b; Safronetz et al., 2015; Smither et al., 2014). Similarly, in the mouse model of CCHF, favipiravir has shown remarkable efficacy, protecting mice from lethal disease even when started late in the clinical course of disease. Both a previous study from our group (Hawman et al., 2018) and a study by Oestereich et al. (2014a) demonstrated that favipiravir treatment could significantly inhibit CCHFV replication, suppressing viral loads in several tissues and protect from lethal disease in the type I interferon deficient mouse model of CCHF (Oestereich et al., 2014a; Hawman et al., 2018). CCHFV infection in this model results in a rapid onset of disease with high viral burden in multiple tissues, high levels of inflammatory cytokines and death within 4–8 DPI. It therefore represents a stringent test for the ability of candidate antivirals to protect against CCHFV. In particular, previous data from our group demonstrated that favipiravir could be administered as late as 6 DPI, a time point at which some mice had already started to succumb, and still offer significant clinical benefit (Hawman et al., 2018). Furthermore, the studies by our group and those by Oestereich et al. have together evaluated favipiravir against three distinct strains of CCHFV and found significant clinical benefit (Oestereich et al., 2014a; Hawman et al., 2018) suggesting favipiravir is broadly effective against diverse CCHFV strains (Bente et al., 2013). These data from the mouse model of CCHF suggest favipiravir is a potent antiviral against CCHFV in vivo.
Therefore, it was surprising that we only observed a modest benefit of favipiravir treatment in the cynomolgus macaques even though we initiated treatment 24 HPI. We observed a significant reduction in the kidney and the right upper lung with favipiravir treatment, with a trend towards reduced viral RNA in many of the once-daily treatments and all of the twice-daily treatments at time of necropsy at day 8 PI. Further, we observed reduced RNA viremia and viral shedding in the oral and nasal cavities indicating that favipiravir exerted anti-viral effect against CCHFV. Levels of virus in the blood or serum of patients often negatively correlates with disease outcome (Duh et al., 2007; Hasanoglu et al., 2016) suggesting favipiravir treatment may improve this clinical parameter. Lastly, while 4 of 8 placebo-treated animals had signs of liver necrosis, no favipiravir-treated animals had evidence of necrosis. Cumulatively, our data suggest favipiravir has efficacy against CCHFV in vivo in the cynomolgus macaque model of CCHF.
An important consideration of this study is that, in contrast to the type I interferon deficient mouse model, the cynomolgus macaque model of CCHF is not uniformly lethal. In this study we observed lethal disease in one placebo-treated animal while the remainder developed more moderate disease, surviving to necropsy on day 8. At the time of necropsy on day 8 PI, placebo-treated animals had exhibited at least 3 days of declining viremia suggesting host responses were controlling the virus independent of any treatment. Thus, it is possible that by the time animals were necropsied on day 8 PI, differences in viral RNA loads between placebo- and favipiravir-treated animals had diminished. This is further supported by the lack of infectious virus in the liver and spleens of placebo-treated animals at day 8 PI and IHC for viral antigen which identified only rarely infected hepatocytes in the livers of the placebo-treated animals.
One explanation for the modest benefit of favipiravir observed in our study was the SC administration of favipiravir. Favipiravir in humans is typically given IV or orally (Sissoko et al., 2016) and previous pharmacokinetic studies in cynomolgus macaques have evaluated repeated IV treatments (Madelain et al., 2017). However, practical considerations of non-human primate studies conducted in the BSL-4 make repeated IV administration difficult. The solubility of favipiravir necessitates larger treatment volumes resulting in prolonged anesthesia due to lengthened infusion times and venous access can also become difficult upon repeated venipuncture. For these reasons, in our study, following the IV loading dose, treatment was administered SC. Our data indicates that SC administration of favipiravir effectively delivered favipiravir to the circulation with serum concentrations similar to what has been reported in non-human primate studies evaluating IV or oral favipiravir against other viral hemorrhagic fevers (Bixler et al., 2018; Guedj et al., 2018). Lastly, a once-daily SC regimen of favipiravir treatment was shown to effectively inhibit Lassa virus replication and protect from lethal disease in cynomolgus macaques (Kyle et al., 2018), a virus for which favipiravir has a similarly reported EC50 compared to CCHFV (Madelain et al., 2017). Together, these data argue against the explanation that our SC treatment regimen was responsible for the modest clinical benefit observed in the animals. However, an important consideration of our data is that in vitro EC50 values may not reflect the in vivo concentrations of favipiravir necessary for therapeutic efficacy against CCHFV. Further, favipiravir is a pro-drug, requiring intracellular metabolism to an active triphosphate form to inhibit viral replication (Furuta et al., 2005). We did not evaluate tissue concentrations of this metabolite in our study and it has been shown that viral infections can alter the metabolism of favipiravir (Gowen et al., 2015) although this was not seen in Ebola virus infected cynomolgus macaques (Guedj et al., 2018).
5. Conclusion
In summary, we found that favipiravir treatment had modest clinical benefit in CCHFV-infected cynomolgus macaques. We found that favipiravir treatment suppressed viral loads in the blood and viral shedding in the oral and nasal cavities along with trends towards reduced viral loads in several tissues demonstrating favipiravir has anti-viral effects upon CCHFV in vivo in non-human primates. To our knowledge, this is the first evaluation of an antiviral therapy against CCHFV in non-human primates. Cumulatively, our data suggest favipiravir may have clinical benefit for CCHF patients and highlights the importance of the cynomolgus macaque model in evaluating candidate antivirals for treatment of CCHFV.
Supplementary Material
Acknowledgements
We wish to thank Rocky Mountain Veterinary Branch for their support of this study. This study was supported by the Intramural Research Program of the NIAID/NIH. Funders had no role in study design, data interpretation or decision to publish.
Footnotes
Declaration of competing interest
T. Komeno, N. Nakajima and Y. Furuta are employees of FUJIFILM Toyama Chemical Co., Ltd., the manufacturer of favipiravir.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.antiviral.2020.104858.
References
- Arda B, Aciduman A, Johnston JC, 2012. A randomised controlled trial of ribavirin in Crimean Congo haemorrhagic fever: ethical considerations. J. Med. Ethics 38, 117–120. 10.1136/medethics-2011-100107. [DOI] [PubMed] [Google Scholar]
- Ascioglu S, Leblebicioglu H, Elaldi N, Bodur H, Vahaboglu H, 2009. Response to Ergonul: scientific evidence versus personal beliefs in crimean-Congo haemorrhagic fever treatment. J. Infect 59, 286–289. 10.1016/j.jinf.2009.08.017. [DOI] [Google Scholar]
- Ascioglu S, Leblebicioglu H, Vahaboglu H, Chan KA, 2011. Ribavirin for patients with Crimean–Congo haemorrhagic fever: a systematic review and meta-analysis. J. Antimicrob. Chemother 66, 1215–1222. 10.1093/jac/dkr136. [DOI] [PubMed] [Google Scholar]
- Bente DA, et al. , 2010. Pathogenesis and immune response of Crimean-Congo hemorrhagic fever virus in a STAT-1 knockout mouse model. J. Virol 84, 11089–11100. 10.1128/jvi.01383-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bente DA, et al. , 2013. Crimean-Congo hemorrhagic fever: history, epidemiology, pathogenesis, clinical syndrome and genetic diversity. Antivir. Res 100, 159–189. 10.1016/j.antiviral.2013.07.006. [DOI] [PubMed] [Google Scholar]
- Bixler SL, et al. , 2018. Efficacy of favipiravir (T-705) in nonhuman primates infected with Ebola virus or Marburg virus. Antivir. Res 151, 97–104. 10.1016/j.antiviral.2017.12.021. [DOI] [PubMed] [Google Scholar]
- Çevik MA, et al. , 2008. Clinical and laboratory features of Crimean-Congo hemorrhagic fever: predictors of fatality. Int. J. Infect. Dis 12, 374–379. 10.1016/j.ijid.2007.09.010. [DOI] [PubMed] [Google Scholar]
- Crimean-Congo haemorrhagic fever, 2017. http://www.who.int/emergencies/diseases/crimean-congo-haemorrhagic-fever/en/.
- Dawes BE, et al. , 2018. Favipiravir (T-705) protects against Nipah virus infection in the hamster model. Sci. Rep 8, 7604. 10.1038/s41598-018-25780-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duh D, et al. , 2007. Viral load as predictor of crimean-Congo hemorrhagic fever outcome. Emerg. Infect. Dis 13, 1769–1772. 10.3201/eidl311.070222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ergonul O., 2006. Crimean-Congo haemorrhagic fever. Lancet Infect. Dis 6. 10.1016/s1473-3099(06)70435-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ergonul O., 2009. DEBATE (see Elaldi N et al, Efficacy of oral ribavirin treatment in Crimean-Congo haemorrhagic fever: a quasi-experimental study from Turkey. Journal of Infection 2009; 58: 238–244): biases and misinterpretation in the assessment of the efficacy of oral ribavirin in the treatment of Crimean–Congo hemorrhagic fever. J. Infect 59, 284–286. 10.1016/j.jinf.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Ergonul O., 2014. Evidence supports ribavirin use in Crimean-Congo hemorrhagic fever. Int. J. Infect. Dis 29, 296. 10.1016/j.ijid.2014.08.016. [DOI] [PubMed] [Google Scholar]
- Ergonul O, Celikbas A, Baykam N, Eren S, Dokuzoguz B, 2006. Analysis of risk-factors among patients with Crimean-Congo haemorrhagic fever virus infection: severity criteria revisited. Clin. Microbiol. Infect 12, 551–554. 10.1111/j.1469-0691.2006.01445.x. the official publication of the European Society of Clinical Microbiology and Infectious Diseases. [DOI] [PubMed] [Google Scholar]
- Ergonul O, et al. , 2018. Systematic review and meta-analysis of postexposure prophylaxis for crimean-Congo hemorrhagic fever virus among healthcare workers. Emerg. Infect. Dis 24, 1642–1648. 10.3201/eid2409.171709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldmann F, Shupert WL, Haddock E, Twardoski B, Feldmann H, 2019. Gamma irradiation as an effective method for inactivation of emerging viral pathogens. 10.4269/ajtmh.18-0937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuta Y., et al. , 2005. Mechanism of action of T-705 against influenza virus. Antimicrob. Agents Chemother 49, 981–986. 10.1128/aac.49.3.981-986.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuta Y., et al. , 2013. Favipiravir (T-705), a novel viral RNA polymerase inhibitor. Antivir. Res 100, 446–454. 10.1016/j.antiviral.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furuta Y, Komeno T, Nakamura T, 2017. Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci 93, 449–463. 10.2183/pjab.93.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gowen BB, et al. , 2015. Alterations in favipiravir (T-705) pharmacokinetics and bio-distribution in a hamster model of viral hemorrhagic fever. Antivir. Res 121, 132–137. 10.1016/j.antiviral.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guedj J., et al. , 2018. Antiviral efficacy of favipiravir against Ebola virus: a translational study in cynomolgus macaques. PLoS Med. 15, e1002535. 10.1371/journal.pmed.1002535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock E., et al. , 2018. A cynomolgus macaque model for Crimean-Congo haemorrhagic fever. Nat. Microbiol 3, 556–562. 10.1038/s41564-018-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasanoglu I., et al. , 2016. Crucial parameter of the outcome in Crimean Congo hemorrhagic fever: viral load. J. Clin. Virol 75, 42–46. 10.1016/j.jcv.2015.12.006. the official publication of the Pan American Society for Clinical Virology. [DOI] [PubMed] [Google Scholar]
- Hawman DW, et al. , 2018. Favipiravir (T-705) but not ribavirin is effective against two distinct strains of Crimean-Congo hemorrhagic fever virus in mice. Antivir. Res 157, 18–26. 10.1016/j.antiviral.2018.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson S., et al. , 2018. Ribavirin for treating Crimean Congo haemorrhagic fever. Cochrane Database Syst. Rev 6, Cd012713. 10.1002/14651858.CD012713.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koksal I., et al. , 2010. The efficacy of ribavirin in the treatment of Crimean-Congo hemorrhagic fever in Eastern Black Sea region in Turkey. J. Clin. Virol 47, 65–68. 10.1016/j.jcv.2009.11.007. the official publication of the Pan American Society for Clinical Virology. [DOI] [PubMed] [Google Scholar]
- Kyle R, et al. , 2018. Use of favipiravir to treat Lassa virus infection in macaques. Emerg. Infect. Dis. J 24. 10.3201/eid2409.180233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madelain V, et al. , 2017. Favipiravir pharmacokinetics in nonhuman primates and insights for future efficacy studies of hemorrhagic fever viruses. Antimicrob. Agents Chemother. 61. 10.1128/aac.01305-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oestereich L., et al. , 2014a. Evaluation of antiviral efficacy of ribavirin, arbidol, and T-705 (favipiravir) in a mouse model for crimean-Congo hemorrhagic fever. PLoS Neglected Trop. Dis 8, e2804. 10.1371/journal.pntd.0002804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oestereich L., et al. , 2014b. Successful treatment of advanced Ebola virus infection with T-705 (favipiravir) in a small animal model. Antivir. Res 105, 17–21. 10.1016/j.antiviral.2014.02.014. [DOI] [PubMed] [Google Scholar]
- Safronetz D, et al. , 2015. The broad-spectrum antiviral favipiravir protects guinea pigs from lethal Lassa virus infection post-disease onset. 5 10.1038/srep14775. 14775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sissoko D., et al. , 2016. Experimental treatment with favipiravir for Ebola virus disease (the JIKI trial): a historically controlled, single-arm proof-of-concept trial in Guinea. PLoS Med. 13 10.1371/journal.pmed.1001967. e1001967–e1001967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smither SJ, et al. , 2014. Post-exposure efficacy of Oral T-705 (Favipiravir) against inhalational Ebola virus infection in a mouse model. Antivir. Res 104, 153–155. 10.1016/j.antiviral.2014.01.012. [DOI] [PubMed] [Google Scholar]
- Soares-Weiser K, Thomas S, Thomson G, Garner P, 2010. Ribavirin for Crimean-Congo hemorrhagic fever: systematic review and meta-analysis. BMC Infect. Dis 10, 207. 10.1186/1471-2334-10-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanepoel R., et al. , 1989. The clinical pathology of Crimean-Congo hemorrhagic fever. Rev. Infect. Dis 11 (Suppl. 4), S794–S800. [DOI] [PubMed] [Google Scholar]
- Welch SR, et al. , 2017. Identification of 2′-deoxy-2′-fluorocytidine as a potent inhibitor of Crimean-Congo hemorrhagic fever virus replication using a recombinant fluorescent reporter virus. Antivir. Res 147, 91–99. 10.1016/j.antiviral.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.