Abstract
Objective
We aimed to describe the characteristics, outcomes and resource utilisation of patients being cared for in an ICU after undergoing elective surgery in Australia and New Zealand (ANZ).
Methods
This was a point prevalence study involving 51 adult ICUs in ANZ in June 2021. Patients met inclusion criteria if they were being treated in a participating ICU on he study dates. Patients were categorised according to whether they had undergone elective surgery, admitted directly from theatre or unplanned from the ward. Descriptive and comparative analysis was performed according to the source of ICU admission. Resource utilisation was measured by Length of stay, organ support and occupied bed days.
Results
712 patients met inclusion criteria, with 172 (24%) have undergone elective surgery. Of these, 136 (19%) were admitted directly to the ICU and 36 (5.1%) were an unplanned admission from the ward. Elective surgical patients occupied 15.8% of the total ICU patient bed days, of which 44.3% were following unplanned admissions. Elective surgical patients who were an unplanned admission from the ward, compared to those admitted directly from theatre, had a higher severity of illness (AP2 17 vs 13, p<0.01), require respiratory or vasopressor support (75% vs 44%, p<0.01) and hospital mortality (16.7% vs 2.2%, p < 0.01).
Conclusions
ICU resource utilisation of patients who have undergone elective surgery is substantial. Those patients admitted directly from theatre have good outcomes and low resource utilisation. Patient admitted unplanned from the ward, although fewer, were sicker, more resource intensive and had significantly worse outcomes.
Keywords: Intensive Care Medicine, Post operative intensive care, Resource utilisation, Failure to rescue, Critical care
1. Introduction
2.3 million elective surgical procedures take place in Australia and New Zealand each year,1 with 85,000 of these resulting in an admission to an Intensive Care Unit (ICU) post operatively, accounting for approximately 36 % of all ICU admissions.2 The optimal utilisation of ICU resources for patients undergoing an elective surgical procedure has not been well established and is listed as a priority research question.3 ICU resource utilisation refers to both ICU admission and the broader array of services potentially offered to those patients admitted to an ICU.
Observational studies have identified variation in ICU admission practices following elective surgery, both within, and between healthcare systems. No association has been identified between routine ICU admission and improved patient outcomes.[4], [5], [6] The described variation in ICU admission practices does not appear to correlate with differences in patient outcomes.[7], [8], [9]
Patients who undergo elective surgery may experience adverse events, some of which necessitate an unanticipated ICU admission from the ward. Although there is no universally agreed definition,10 this concept in which there is an adverse outcome following a failure to respond to a patient deterioration has been termed “Failure to Rescue” (FtR) and has been validated as a health system quality measure.[10], [11], [12] In this study, we refer to FtR as an unplanned ICU admission from ward level care following a hospital admission involving an elective surgical procedure. It is known that patients who experience FtR have higher odds of poor outcomes13 and ICU resource utilisation. The impact of FtR patients on ICU utilisation and on outcomes has not been fully described and is not known in Australia and New Zealand (ANZ).
Our primary objective was to record the prevalence of elective surgical patients admitted post-operatively to an ANZ ICUs and their associated ICU resource utilisation and outcomes. Secondary objectives were to characterise and describe the prevalence of patients that have experienced FtR, requiring an ICU admission.
2. Materials and methods
This was a cross-sectional, observational cohort study of 51 ICUs in Australia and New Zealand, part of the Australian and New Zealand Intensive Care Society (ANZICS) Point Prevalence Program (PPP).14
Participating sites collected data on all patients over the age of 16, present in their ICU at 10am on one of two study days (8th or 23rd of June 2021). Participating sites and site specific investigators are described in the supplementary material. Data were collected from patient records at each study site and entered into the REDCap data collation software (Vanderbilt University, TN),15 hosted at the George Institute for Global Health, Sydney.
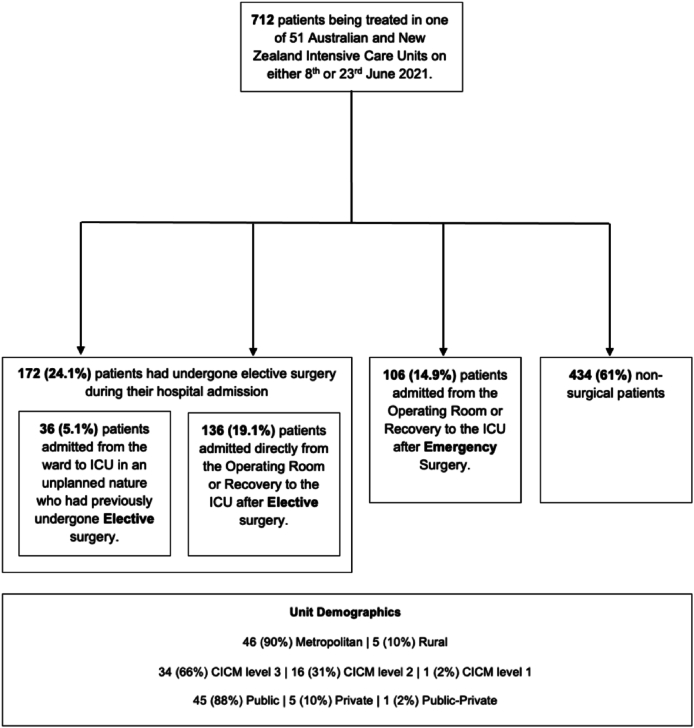
Demographic, physiological, and administrative variables were collected which allowed the following four patient categories to be established and compared (Fig. 1): 1: Patients admitted to ICU from the ward in an unplanned nature after previously having undergone elective surgery; 2: Patients admitted directly to the ICU following elective surgery; 3: Patients admitted directly to an ICU following emergency surgery; 4: Admit Other (admitted from the Emergency Department (ED), Other Hospital, or Other ICU).
Fig. 1.
Patient groups and unit demographics.
An additional comparative analysis was performed on those patients admitted to the ICU in an unplanned nature from the ward. We sub-categorised these patients into those who had previously undergone elective surgery and those who had not (emergency surgery or medical diagnoses).
Admission codes on ICU admission were extracted via the Acute Physiology and Chronic Health Evaluation iii–J16,17 (APACHEiii-J) score collected at the time of admission. This provides additional detail regarding surgical procedure sub-type and the nature of the procedure (planned vs unplanned). Those admitted in an unplanned nature from the ward had data related to any previous elective surgical procedure such as date and surgical code collected, as well as their ICU APACHEiii-J admission code. ICU interventions, such as mechanical ventilation, respiratory support, vasopressor support, and Renal Replacement Therapy (RRT), were collected. Hospital and ICU outcome data, admission time, date, length of stay (LOS), and source (ward, ED, other hospital, other ICU) were collected.
For data that had a longitudinal component (mortality, LOS), censure was applied at 30 days.
Physiological data collected for each patient included the variables contributing to the APACHEiii-J score. Pre-existing chronic health disease were collected as part of the chronic health evaluation of the APACHEiii-J score.
2.1. Statistical methods
Normally distributed data are presented as mean with standard deviations (SD) and non-normally distributed data with median values and inter-quartile ranges (IQR). Data analysis was performed on R - A Program for statistical computing.18 Wilcox Sum tests were used for comparing medians, with the Fishers exact test used for comparing proportions. Appropriate statistical tests (Analysis of Variance) were used to compare variation between groups.
2.2. Ethical approval
Ethical approval was overseen by the George Institute and was granted by Sydney Local Health District – Royal Prince Alfred Zone Ethics Committee, New South Wales.
3. Results
Demographic characteristics of participating ICUs are described in figure 1.0. 88 % of contributing units were College of Intensive Care Medicine Level 3 ICUs19 in public hospitals, with the majority located in metropolitan centres. These unit level demographics are similar to ANZ as a whole.20
712 patients were being treated in 51 separate ICUs on the study dates contributing a total of 4618 occupied bed days. 278 (39 %) patients had undergone a surgical procedure during their hospital stay. Patients who had a surgical procedure contributed to 1580 (34 %) of the total ICU occupied bed days. Of those who had a surgical procedure, 242 (34 %) patients were admitted directly to ICU from the operating theatre, of which 136 (19 %) were following elective and 106 (14.9 %) emergency surgery.
36 (5.1 %) patients were admitted to the ICU from the ward in an unplanned nature having previously had elective surgery within their current hospital admission. This patient group (FtR) accounted for 324 (7 %) of occupied bed days. Six of this group died in hospital, resulting in a 16.7 % crude in-hospital mortality rate.
Coronary artery bypass surgery was the most common surgical procedure for both elective and emergency surgical patients admitted directly to ICU and gastrointestinal obstruction surgery for patients admitted from the ward. Surgical patients admitted from the ward were older, more likely to be males, with a higher severity of illness. They experienced a longer ICU stay and higher odds of hospital mortality than the other three patient groups (patients admitted directly to ICU after elective surgery, patients admitted to ICU after emergency surgery, and all other patient types) (Table 1).
Table 1.
Baseline characteristics of 712 patients being cared for in an ICU, by patient type on day of Point Prevalence Study.
| Variable | Patients admitted to ICU from the ward after having undergone elective surgery | Patients admitted directly to the ICU following elective surgery. | Patients admitted to ICU after emergency surgery. | Admit other (Emergency Department, Other Hospital or Other ICU) | p |
|---|---|---|---|---|---|
| Number (% total ICU admissions) | 36 (5.1 %) | 136 (19.1 %) | 106 (14.9 %) | 434 (61 %) | |
| Age | 72.5 [61.5, 79.0] | 64.0 [55.8, 73.0] | 65.5 [45.5, 75.0] | 62.0 [48.0, 73.0] | 0.011 |
| Male gender | 18 (50.0) | 96 (70.6) | 76 (71.7) | 258 (59.4) | 0.008 |
| Body Mass Index | 28.9 [23.2, 32.0] | 27.9 [24.3, 31.5] | 29.2 [25.0, 30.5] | 29.7 [24.8, 32.1] | 0.496 |
| Top five diagnostic codes | G.I. Obstruction (n = 7) G.I. neoplasm (n = 2) Orthopaedic surgery (n = 2) Other respiratory diseases (n = 2) Other G.I. inflam disease (n = 2) |
CABG (n = 33) GI neoplasm (n = 14) Valvular heart surgery (n = 10) Other CV diseases (n = 10) Other respiratory disease (n = 6) |
CABG (n = 11) Head trauma ± multi trauma (n = 11) Multiple trauma excluding head (n = 9) G.I. bleeding (n = 7) G.I. Obstruction (n = 7) |
Sepsis with shock (non-urinary) (n = 42) Cardiac Arrest (n = 28) Other Respiratory Diseases (n = 19) Bacterial pneumonia (n = 19 Multiple trauma excluding head (n = 18) |
|
| APACHEii | 17.0 [12.0, 21.8] | 13.0 [9.0, 17.0] | 16.0 [12.0, 20.0] | 18.0 [12.0, 23.0] | <0.001 |
| SOFA | 7.5 [3.0, 12.2] | 6.5 [3.8, 11.0] | 9.0 [5.0, 13.0] | 9.0 [5.0, 13.0] | 0.011 |
| Mechanically ventilated | 13 (36.1) | 39 (28.7) | 47 (44.3) | 175 (40.3) | 0.051 |
| Other respiratory support | 13 (36.1) | 30 (22.1) | 38 (35.8) | 129 (29.7) | 0.092 |
| Vasopressors administered | 11 (30.6) | 36 (26.5) | 44 (41.5) | 144 (33.2) | 0.102 |
| No organ supports required | 9 (25.0) | 76 (55.9) | 26 (24.5) | 32 (7.4) | <0.001 |
| Pre-existing chronic health disease | |||||
| Long term dialysis dependence | 0 (0.0) | 2 (1.5) | 0 (0.0) | 14 (3.2) | 0.137 |
| Proven cirrhosis. | 1 (2.8) | 4 (2.9) | 2 (1.9) | 16 (3.7) | 0.811 |
| NYHA Class IV symptoms | 1 (2.8) | 1 (0.7) | 4 (3.8) | 16 (3.7) | 0.695 |
| Significant respiratory disease | 2 (5.6) | 12 (8.8) | 7 (6.6) | 34 (7.8) | 0.882 |
| Immunosuppression | 8 (22.2) | 14 (10.3) | 10 (9.4) | 59 (13.6) | 0.175 |
| No chronic health disease | 11 (30.6) | 33 (24.3) | 19 (17.6) | 118 (27.2) | 0.216 |
| ICU Length of stay | 9.0 [3.8, 12.5] | 3.0 [1.0, 9.0] | 8.0 [4.0, 12.0] | 7.0 [3.0, 13.0] | <0.001 |
| Occupied ICU bed days (% total) | 324 (7 %) | 408 (8.8 %) | 848 (18.4 %) | 3038 (65.8 %) | |
| ICU discharge status | 0.073 | ||||
| Died | 3 (8.3) | 3 (2.2) | 4 (3.8) | 20 (4.6) | |
| Unknown/remain in ICU | 0 (0) | 8 (5.9) | 4 (3.8) | 7 (1.6) | |
| Hospital discharge status | 0.005 | ||||
| Died | 6 (16.7) | 3 (2.2) | 11 (10.4) | 46 (10.6) | |
| Unknown/remain in hospital | 12 (33.3) | 28 (20.6) | 32 (30.2) | 117 (27.0) |
Numbers are No.(%), mean (SD), median [IQR] unless otherwise noted. SD, standard deviation; IQR, interquartile range.
Overall, 172 (24 %) patients of ICU admissions had elective surgery, of which 9 (5.2 %) patients died during their hospital stay. In comparison, 15 (14.2 %) of 106 emergency surgery patients died during their hospital stay.
Of patients admitted to ICU from the ward, 36 (22 %) patients had prior elective surgery. Surgical patients were similar to non-surgical patients with regards to patient demographics, severity of illness, ICU stay, and ICU and hospital outcome. Cardiovascular disease (rhythm disturbance, cardiac arrest, acute coronary syndromes) and non-urinary tract sepsis were the most common ICU admission APACHEiii diagnostic categories for the surgical patients (Table 2).
Table 2.
Comparison of ICU admissions from the ward stratified by whether they have had elective surgery during hospital admission.
| Variable | Admissions from ward after elective surgery | Admissions from ward (no elective surgery) | p |
|---|---|---|---|
| Number | 36 (22.1) | 127 (77.9) | |
| Age | 72.5 [61.5, 79.0] | 65.0 [53.5, 75.0] | 0.057 |
| Male gender | 18 (50.0) | 78 (61.4) | 0.300 |
| Post rapid response team call | 23 (63.9) | 95 (74.8) | 0.279 |
| Top 5 APACHEiii – J admission diagnoses | Other CV disease (n = 4) Sepsis other than urinary (n = 4) Rhythm disturbance (n = 3) Respiratory neoplasm (n = 3) Other neurological disease (n = 2) |
Sepsis with shock other than urinary (n = 14) Pancreatitis (n = 7) Sepsis other than urinary (n = 7) Other respiratory diseases (n = 6) 403 Stroke (n = 6) |
|
| BMI | 28.9 [23.2, 32.0] | 29.6 [24.5, 31.1] | 0.519 |
| APACHEii | 17.0 [12.0, 21.8] | 18.0 [14.0, 22.5] | 0.762 |
| SOFA | 7.5 [3.0, 12.2] | 9.0 [5.0, 11.0] | 0.391 |
| Mechanically ventilated | 13 (36.1) | 48 (37.8) | 1.000 |
| Other respiratory support | 13 (36.1) | 40 (31.5) | 0.749 |
| Vasopressive support | 11 (30.6) | 47 (37.0) | 0.605 |
| No organ supports | 9 (25.0) | 32 (25.2) | 1.000 |
| Pre-existing health conditions | |||
| Respiratory disease | 2 (5.6) | 10 (7.9) | 0.913 |
| Renal disease (Dialysis dependent) | 0 (0.0) | 6 (4.7) | 0.408 |
| Liver disease (Proven cirrhosis) | 1 (2.8) | 5 (3.9) | 1.000 |
| Cardiovascular disease (NYHA IV) | 1 (2.8) | 7 (5.5) | 1.000 |
| Immunosuppression | 8 (22.2) | 26 (20.5) | 1.0 |
| ICU Length of stay | 9.0 [3.8, 12.5] | 8.0 [3.0, 13.0] | 0.641 |
| ICU bed days | 324 | 1016 | |
| ICU discharge alive | 29 (80.6) | 108 (85.0) | 0.696 |
| Hospital discharge status | 0.723 | ||
| Died | 6 (16.7) | 15 (11.8) | |
| Unknown/still in hospital | 12 (33.3) | 42 (33.1) |
Numbers are No.(%), mean (SD), median [IQR] unless otherwise noted. SD, standard deviation; IQR, interquartile range.
Table 3 compares those patients admitted directly to the ICU after elective surgery with those admitted to ICU following a period of care on the ward. Patients with unplanned ward admissions were older, more likely to be males, had a higher severity of illness, more likely to require organ supports, a longer ICU stay, and higher ICU and hospital mortality. Median time to ICU admission after elective surgery was 5 (IQR 3–10) days. 64 % were admitted followed a Rapid Response Team (RRT) review.
Table 3.
Comparison of Failure-to-Rescue patients with non Failure-to-Rescue patients after planned surgery on day of Point Prevalence Study.
| Variable | Direct to ICU after elective surgery | Failure to rescue group | p |
|---|---|---|---|
| No. | 136 (79.1) | 36 (20.9) | |
| Age | 64.0 [55.8, 73.0] | 72.5 [61.5, 79.0] | 0.009 |
| Male gender | 96 (70.6) | 18 (50.0) | 0.034 |
| Post Rapid Response Team review | 0 (0.0) | 23 (63.9) | <0.001 |
| BMI | 27.9 [24.3, 31.5] | 28.9 [23.2, 32.0] | 0.868 |
| APACHEii | 13.0 [9.0, 17.0] | 17.0 [12.0, 21.8] | <0.001 |
| SOFA | 6.5 [3.8, 11.0] | 7.5 [3.0, 12.2] | 0.696 |
| Mechanically ventilated | 39 (28.7) | 13 (36.1) | 0.509 |
| Other respiratory supports | 30 (22.1) | 13 (36.1) | 0.130 |
| Vasopressor requirements | 36 (26.5) | 11 (30.6) | 0.780 |
| No organ supports | 76 (55.9) | 9 (25.0) | 0.002 |
| Pre-existing chronic health conditions | |||
| Dialysis dependent | 2 (1.5) | 0 (0.0) | 1.000 |
| Proven cirrhosis | 4 (2.9) | 1 (2.8) | 1.000 |
| NYHA IV Heart disease | 1 (0.7) | 1 (2.8) | 0.887 |
| Respiratory disease | 12 (8.8) | 2 (5.6) | 0.768 |
| Immunosuppressed | 14 (10.3) | 8 (22.2) | 0.104 |
| ICU LOS | 3.0 [1.0, 9.0] | 9.0 [3.8, 12.5] | <0.001 |
| ICU bed days | 408 | 324 | |
| ICU discharge status | 0.075 | ||
| Unknown/still in ICU | 8 (5.9) | 0 (0.0) | |
| Died in ICU | 3 (2.2) | 3 (8.3) | |
| Hospital discharge status | <0.001 | ||
| Unknown/still in hospital | 28 (20.6) | 12 (33.3) | |
| Died in hospital | 3 (2.2) | 6 (16.7) |
Numbers are No.(%), mean (SD), median [IQR] unless otherwise noted. SD, standard deviation; IQR, interquartile range.
4. Discussion
This Point Prevalence Study prospectively collected data from a representative cross section of 51 Australian and New Zealand Intensive Care Units in June 2021. The data allow a contemporary description of resource utilisation of patients who have undergone elective surgery preceding their ICU admission on a typical day in ANZ in June 2021.
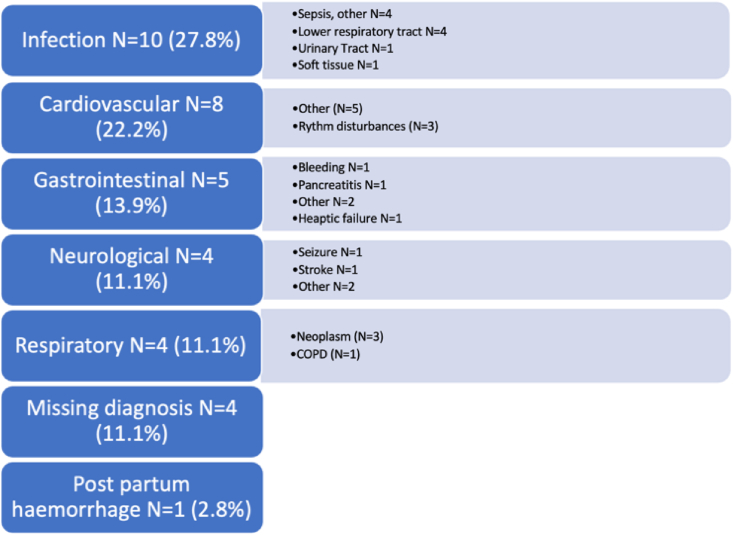
In this Point Prevalence Study, 19 % of ICU patients had undergone an elective surgical procedure directly before their ICU admission (see Fig. 2). These patients had a lower severity of illness than ICU patients as a whole, almost half did not receive organ support, and accounted for 408 (8.8 %) of total ICU bed days. In contrast, elective surgical patients who met the FtR definition being 36 (5.1 %) of the ICU admissions were older, had a higher severity of illness on ICU admission, longer ICU stay, greater intensity of ICU care, and higher hospital mortality.
Fig. 2.
Admission diagnoses of patients admitted to an ICU from the ward after unplanned surgery having previously undergone elective surgery. ICU, intensive care unit.
A fundamental question arising as a result of our analysis is whether greatest benefit comes from a “prophylactic” ICU admission for the higher risk post-operative surgical patient than “waiting” for the need for organ support to be required on the ward. Our data demonstrate that waiting for the organ support to be required on the ward results in poor outcomes. Of the 36 (5.1 %) post-operative elective surgical patients who deteriorated on the ward requiring an ICU admission, six (16.7 %) patients died. This is strikingly higher than the 2.2 % mortality rate experienced among those admitted to the ICU directly from the Operating Theatre.
Defining the need for ICU admission post operatively is nuanced and should be an individualised, patient centred decision. Indeed, defining what constitutes organ support and where certain therapies can safely be offered has not been fully elucidated. There is a lack of data around how the decision is made regarding Operating Theatre discharge destination.21,22 Understanding illness severity, certain patient characteristics on discharge from the Operating Theatre would help predict those patients at higher risk of deterioration. Getting the balance right between ICU and ward discharge destination from the Operating Theatre is a key challenge facing contemporary peri-operative medicine. Our data demonstrate the implications of inappropriate ward transfer at both the individual and system level.
Our analysis has important implications for the care of all critically unwell patients, as ICU services are a precious and expensive resource that is in increasing demand in ANZ23 and internationally.24 As such, it is surprising that currently, what is considered as optimal ICU utilisation after elective surgery remains uncertain.25 This is despite elective surgical admissions being a significant amount of total ICU workload, representing up to 36 % of patient admissions in ANZ.2 This uncertainty is a likely contributor to the variation of ICU utilisation at the local, regional, and international level.4,8,26
The significant mortality and morbidity associated with emergency surgery and direct post-operative ICU admission (10.4 % mortality) is in stark contrast with the direct to ICU elective surgical cohort (2.2 % mortality). This suggests a need for optimising our approach to the emergency surgical patient, potentially in a manner similar to higher risk elective surgical cases, such as is common with cardiac surgical patients. Measures that could be explored include a formal rapid peri-operative MDT decision making process, optimising case selection, pre-, intra-, and post-operative monitoring, and evaluation of handover processes.
Key characteristics of the patients that met our FtR criteria were that they were more likely to be older (median age of 72 years), immunosuppressed (22 %), and have the longest LOS (median 9 days) of the four patient groups analysed. The most common reason for ICU admission after a ward deterioration were dysrhythmias, other cardiovascular issues and non-urinary sepsis. The older age of this patient group is notable and raises questions regarding how patient age influences decisions regarding location and intensity of care. The poor outcomes in this FtR cohort following elective surgery are consistent with previously published studies27,28 and emphasise the need to focus on appropriate triaging and risk prediction of patients undergoing higher risk surgery in ANZ.29
The median time from elective surgery to ICU admission in our data of 5 days (IQR 3–9) is an important finding. It highlights that the most “at risk” period following elective surgery for those first transferred to a ward may not be in the immediate post-operative period, but a period beyond that. This “delayed deterioration” raises the possibility that elective ICU admission post-operatively may not have resulted in patient rescue. It demonstrates the dynamic, unpredictable, and individualised nature of a high risk elective surgical patient's peri-operative journey. Further investigation is required to identify risk factors for deterioration before surgery is undertaken and to investigate whether deterioration can be predicted on the ward, specific to this patient cohort.
Our data describe good patient centred outcomes and low ICU resource utilisation of those patients admitted directly to an ICU after their elective surgical procedure. This group had the shortest median ICU stay and least severity of illness compared to other admitted ICU patients. 60 % of these patients did not receive any organ support during their ICU stay. Of those that did require organ supports, 39 (28.7 %) were mechanically ventilated and 36 (27 %) required vasopressive support (27 %). The low 2.2 % crude in-hospital mortality rate of this patient group is comparable to that of previously published international observational studies.4,8,30,31
As the evidence base in this area has matured, it has become established that routine ICU admission after elective surgery is not associated with improved outcomes in certain lower risk patient cohorts.8,32 There is now an increased effort to define which interventions may improve outcomes at both a patient and system level and understand the way that such ICU resources are used, whether variation exists, and whether such variation influences patient outcomes.
Our data contribute to this evidence from the ANZ perspective. Patients in our investigation required “typical ICU level supports” such as mechanical ventilation, other respiratory supports, and vasopressive support. An important finding from our data is that a substantial proportion of patients did not require any organ supports in ICU after their elective surgical procedure. It is hypothesised that these patients were admitted for ICU level care for an increased level of monitoring or for a higher degree of nursing, medical, or allied health input. Establishing the value that ICU admission adds in this setting should be explored. Further work to define this cohort of patients in ANZ who never receive organ support in ICU after their elective surgery may provide means to streamline and introduce efficiencies of care.
This study highlights the importance of optimising patient selection regarding who and when patients should be cared for in ICU after elective surgery. Further questions remain regarding which therapies, and the degree of monitoring that should be offered to post-operative elective surgical patients.33 At present, no standardised formal risk stratification involving Intensivists exists in ANZ regarding who and what therapies should be offered care in ICU after elective surgery.22,34
We acknowledge that limitations exist with regards to this study. This is a descriptive study of relatively low patient numbers, designed to give a cross sectional “snapshot” of ICU resource utilisation over two days in ANZ. Temporal and regional variation may exist, which limits external generalisability, particularly beyond the ANZ setting. Despite this, the 51 ICUs that contributed to the study do seem to be broadly representative of the ANZ units as a whole.
This study utilised the combination of the Australian and New Zealand Intensive Care Society (ANZICS) Adult Patient Database (APD) and the ANZICS Clinical Trial Group PPP. A key strength of this Point Prevalence Study is that we collected specific data relating to the elective surgical procedure for all patients admitted to the ICU—not just those admitted in a planned nature from the operating theatre—as the APD currently does. This adds and important layer of granularity to our analysis.
Our data were provided by the ANZICS Clinical Trial Group PPP which produces robust, auditable data from 51 different ICUs across ANZ, with low rates of missing data. This has allowed us to provide contemporary data relating to ICU utilisation and patient characteristics in the post-elective surgical setting in ANZ. We have described and analysed an ICU FtR cohort due to the prospective data collection method, which is not currently possible through the ANZICS Centre for Outcome and Resource Evaluation Adult Patient Database.
5. Conclusion
In this selection of ANZ ICUs, elective surgical admission to ICU were common, had low severity of illness, and 60 % did not require organ support. Elective surgical patients admitted unplanned from the ward, following acute clinical deterioration, although much fewer had a disproportionally higher severity of illness and ICU resource consumption. Our findings indicate that further understanding of elective surgical admissions to ICU may result in better utilisation of ICU resources with respect to choice of elective surgical admission, and its timing for ICU utilisation.
Credit authorship contribution statement
Criteria for authorship was met by all co-authors for this study.
Funding
Nil funding sources to declare.
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ccrj.2023.10.010.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Australian Institute of Health and Welfare . 2016. Admitted patient care 2014-2015. [Google Scholar]
- 2.Australian and New Zealand Intensive Care Society. ANZICS Centre for outcome and resource evaluation and Monash University SPRINT-SARI Australia combined report on COVID-19 admissions to Australian and New Zealand ICUs. [Melbourne].
- 3.Gillies M.A., Sander M., Shaw A., Wijeysundera D.N., Myburgh J., Aldecoa C., et al. Current research priorities in perioperative intensive care medicine [Internet] Intensive Care Med. Springer Verlag. 2017 [cited 2020 Sep 21];43:1173–1186. doi: 10.1007/s00134-017-4848-3. www.isrctn.com Available from: [DOI] [PubMed] [Google Scholar]
- 4.Kahan B.C., Koulenti D., Arvaniti K., Beavis V., Campbell D., Chan M., et al. Critical care admission following elective surgery was not associated with survival benefit: prospective analysis of data from 27 countries. Intensive Care Med. 2017 Jul 1;43(7):971–979. doi: 10.1007/s00134-016-4633-8. [DOI] [PubMed] [Google Scholar]
- 5.Pearse R.M., Clavien P.A., Demartines N., Fleisher L.A., Grocott M., Haddow J., et al. Global patient outcomes after elective surgery: prospective cohort study in 27 low-, middle- and high-income countries. Br J Anaesth. 2016 Nov 1;117(5):601–609. doi: 10.1093/bja/aew316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jawad M., Baigi A., Oldner A., Pearse R.M., Rhodes A., Seeman-Lodding H., et al. European Journal of Anaesthesiology. Lippincott Williams and Wilkins; 2016. Swedish surgical outcomes study (SweSOS) pp. 317–325. [DOI] [PubMed] [Google Scholar]
- 7.Wunsch H., Gershengorn H.B., Cooke C.R., Guerra C., Angus D.C., Rowe J.W., et al. Use of intensive care services for medicare beneficiaries undergoing major surgical procedures. Anesthesiology. 2016;124(4):899–907. doi: 10.1097/ALN.0000000000001024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jerath A., Laupacis A., Austin P.C., Wunsch H., Wijeysundera D.N. Intensive care utilization following major noncardiac surgical procedures in Ontario, Canada: a population-based study. Intensive Care Med. 2018;44:1427–1435. doi: 10.1007/s00134-018-5330-6. [DOI] [PubMed] [Google Scholar]
- 9.Gillies M.A., Power G.S., Harrison D.A., Fleming A., Cook B., Walsh T.S., et al. Regional variation in critical care provision and outcome after high-risk surgery. Intensive Care Med. 2015 Oct 22;41(10):1809–1816. doi: 10.1007/s00134-015-3980-1. [DOI] [PubMed] [Google Scholar]
- 10.Hall K.K., Shoemaker-Hunt S., Hoffman L., Richard S., Gall E., Schoyer E., et al. In: Making healthcare safer III: a critical analysis of existing and emerging patient safety practices. Aline Holmes R.N., DNP, Kristen Miller DrPH., CPPS, Sam Watson M.H.A., editors. 2020. Making healthcare safer III: a critical analysis of existing and emerging patient safety practices. Chapter 2: failure to rescue.https://www.ncbi.nlm.nih.gov/books/NBK555526/ [Internet] [cited 2023 Aug 13]; Available from: [PubMed] [Google Scholar]
- 11.Ahmad T., Bouwman R.A., Grigoras I., Aldecoa C., Hofer C., Hoeft A., et al. Use of failure-to-rescue to identify international variation in postoperative care in low-, middle- and high-income countries: a 7-day cohort study of elective surgery. Br J Anaesth. 2017 Aug 1;119(2):258–266. doi: 10.1093/bja/aex185. [DOI] [PubMed] [Google Scholar]
- 12.Ghaferi A.A., Birkmeyer J.D., Dimick J.B. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009 Dec;250(6):1029–1033. doi: 10.1097/sla.0b013e3181bef697. [DOI] [PubMed] [Google Scholar]
- 13.Ghaferi A.A., Birkmeyer J.D., Dimick J.B. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009 Oct 1;361(14):1368–1375. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 14.Point Prevalence Program | The George Institute for Global Health [Internet]. [cited 2023 May 18]. Available from: https://www.georgeinstitute.org.au/projects/point-prevalence-program.
- 15.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O'Neal L., et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019 Jul 1:95. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zimmerman J.E., Wagner D.P., Draper E.A., Wright L., Alzola C., Knaus W.A. Evaluation of acute physiology and chronic health evaluation III predictions of hospital mortality in an independent database. Crit Care Med. 1998;26(8):1317–1326. doi: 10.1097/00003246-199808000-00012. [DOI] [PubMed] [Google Scholar]
- 17.ANZICS Score Calculator [Internet] https://www.anzics.com.au/wp-content/uploads/2018/08/apache.html [cited 2023 May 6]. Available from:
- 18.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2016. R: a language and environment for statistical computing.https://www.R-project.org/ 2016. [Google Scholar]
- 19.CICM. College . 2016. Of intensive care medicine of Australia and New Zealand. [Google Scholar]
- 20.Australian and New Zealand intensive care Society. ANZICS Centre for Outcome and Resource Evaluation 2020 Report Melbourne, Australia; Melbourne: 2021. [Google Scholar]
- 21.Nicholson J.J., Reilly J., Shulman M.A., Ferguson M., Burke J.A., Lehane D.N., et al. Perioperative outcomes in intermediate and high-risk patients after major surgery following introduction of a dedicated perioperative medicine team: a single centre cohort study. Anaesth Intensive Care [Internet] 2023;51(2):120–129. doi: 10.1177/0310057X221119814. https://research.monash.edu/en/publications/perioperative-outcomes-in-intermediate-and-high-risk-patients-aft Mar 1 [cited 2023 Aug 14] Available from: [DOI] [PubMed] [Google Scholar]
- 22.Selwood A., Blakely B., Senthuran S., Lane P., North J., Clay-Williams R. Variability in clinicians' understanding and reported methods of identifying high-risk surgical patients: a qualitative study. BMC Health Serv Res [Internet] 2020 May 15;20(1):427. doi: 10.1186/s12913-020-05316-0. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-05316-0 [cited 2022 Feb 25] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bihari S., McElduff P., Pearse J., Cho O., Pilcher D. Intensive care unit strain and mortality risk in patients admitted from the ward in Australia and New Zealand. J Crit Care. 2022 Apr 1;68:136–140. doi: 10.1016/j.jcrc.2021.07.018. [DOI] [PubMed] [Google Scholar]
- 24.Lanken P.N., Terry P.B., Adler D.C., Brooks-Brunn J.A., Crawford S.W., Danis M., et al. Fair allocation of intensive care unit resources. Am J Respirat Crit Care Med. 2012 Dec 14;156(4 PART I):1282–1301. doi: 10.1164/ajrccm156.4.ats7-97. [DOI] [PubMed] [Google Scholar]
- 25.Ghaffar S., Pearse R.M., Gillies M.A. ICU admission after surgery. Curr Opin Crit Care. 2017 Oct 1;23(5):424–429. doi: 10.1097/MCC.0000000000000448. [DOI] [PubMed] [Google Scholar]
- 26.Vestergaard A.H.S., Christiansen C.F., Nielsen H., Christensen S., Johnsen S.P. Geographical variation in use of intensive care: a nationwide study. Intensive Care Med. 2015 Nov 29;41(11):1895–1902. doi: 10.1007/s00134-015-3999-3. [DOI] [PubMed] [Google Scholar]
- 27.Gillies M.A., Pearse R.M. Intensive care after high-risk surgery what's in a name? Anesthesiology. 2016 Apr 1;124(4):761–762. doi: 10.1097/ALN.0000000000001025. [DOI] [PubMed] [Google Scholar]
- 28.Haller G. Indirect admission to intensive care after surgery: what should be considered? Br J Anaesth. 2017;118(2):153–157. doi: 10.1093/bja/aew433. [DOI] [PubMed] [Google Scholar]
- 29.Reilly J.R., Deng C., Brown W.A., Brown D., Gabbe B.J., Hodgson C.L., et al. Towards a national perioperative outcomes registry: a survey of perioperative electronic medical record utilisation to support quality assurance and research at Australian and New Zealand College of Anaesthetists Clinical Trials Network hospitals in Australia. Anaesth Intensive Care. 2022 May 1;50(3):189–196. doi: 10.1177/0310057X211030284. [DOI] [PubMed] [Google Scholar]
- 30.Vincent J.L., Pearse R., Pearse R.M., Moreno R.P., Bauer P., Pelosi P., et al. Mortality after surgery in Europe: a 7 day cohort study. Lancet. 2012;380 doi: 10.1016/S0140-6736(12)61148-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gillies M.A., Harrison E.M., Pearse R.M., Garrioch S., Haddow C., Smyth L., et al. Intensive care utilization and outcomes after high-risk surgery in Scotland: a population-based cohort study. Br J Anaesth [Internet] 2017;118(1):123–131. doi: 10.1093/bja/aew396. https://pubmed.ncbi.nlm.nih.gov/28039249/ [cited 2020 Sep 30] Available from: [DOI] [PubMed] [Google Scholar]
- 32.Wunsch H., Gershengorn H.B., Guerra C., Rowe J., Li G. Association between age and use of intensive care among surgical Medicare beneficiaries. J Crit Care. 2013 Oct;28(5):597–605. doi: 10.1016/j.jcrc.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Costa-Pinto R., Yanase F., Kennedy L.M., Talbot L.J., Flanagan J.P.M., Opdam H.I., et al. Characteristics and outcomes of surgical patients admitted to an overnight intensive recovery unit: a retrospective observational study. Anaesth Intensive Care. 2022 Oct 10;51(1):29–37. doi: 10.1177/0310057X22199. [DOI] [PubMed] [Google Scholar]
- 34.Jon D., Wong N., Popham S., Wilson A.M., Barneto L.M., Lindsay H.A., et al. Postoperative critical care and high-acuity care provision in the United Kingdom, Australia, and New Zealand on behalf of SNAP-2: EPICCS collaborators. Br J Anaesth. 2019;122:460–469. doi: 10.1016/j.bja.2018.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.