Abstract
Objectives:
Deep pelvic abscesses are surrounded by the pelvic bones, bladder, gynecological organs, intestinal tract, and nerve and vascular systems, and are approached by various routes for drainage. The transgluteal approach is often performed under computed tomography guidance; however, if ultrasonography can be used to confirm the approach, it is considered more effective because it reduces radiation exposure and allows for real-time puncture under sonographic and fluoroscopic guidance.
Methods:
This retrospective study was conducted at Tobata Kyoritsu Hospital (Fukuoka, Japan) between April 1, 2021, and December 31, 2022. Sonographically guided transgluteal drainage with fluoroscopy was performed in five consecutive cases of deep pelvic abscesses using a 3D image analysis system (SYNAPSE VINCENT) to study the anatomy for safe puncture.
Results:
Three patients had postoperative abscesses from colorectal cancer, one caused by perforation of the appendicitis, and one caused by sigmoid diverticulitis. The average drainage duration was 11 days (SD = 6.7). No complications, such as bleeding or nerve damage, were observed.
Conclusions:
We constructed a 3D image of the puncture route of the trans greater sciatic foramen using SYNAPSE VINCENT to objectively comprehend the anatomy and puncture route. The ideal transgluteal approach is to insert the catheter as close to the sacrum as possible at the level of the infrapiriformis. The parasacrum infrapiriformis approach can be performed safely and easily using ultrasound guidance and fluoroscopy.
Keywords: pelvic abscess, sonography, transgluteal drainage, SYNAPSE VINCENT
Introduction
Deep pelvic abscesses have been approached via various routes, including transvaginal, transrectal, and transgluteal, owing to their proximity to the bowel and bladder, vascular structures, and surrounding pelvis. The transgluteal approach to deep pelvic abscesses was first reported by Butch et al.[1] and has mostly been performed under computed tomography (CT) guidance[1-5], while one report of an ultrasound-guided case series is also recognized[6]. Robert et al.[7] described the infrapiriformis approach to avoid nerve damage in more detail. Although CT-guided approaches are technically simple and safe because of their objective anatomy[5], they are associated with radiation exposure, occupy the CT equipment[6], require transfer to the fluoroscopy room, and require blind manipulation to implant the tube, which requires advanced manipulation techniques.
In recent years, the analysis and application of medical images has advanced, and technologies such as mixed reality, augmented reality, and virtual reality have become indispensable tools for medical image analysis, such as improving spatial awareness and assisting imaging procedures. SYNAPSE VINCENT (Fujifilm Medical Co., Ltd., Tokyo, Japan) analyzes medical images in 3D by applying image recognition technology used for face recognition in digital cameras. The system is frequently used for surgical support, especially in the hepatobiliary and pancreatic regions[8]. This study aimed to evaluate the anatomy of the pelvic cavity, focusing on the route of transgluteal drainage, using a 3D image analysis system (SYNAPSE VINCENT). We report an alternative access to deep pelvic abscess drainage via a transgluteal approach using sonography instead of CT, with safety ensured by understanding the anatomy through three-dimensional (3D) imaging.
Methods
The present study was approved by the Ethics Committee of Tobata Kyoritsu Hospital and complied with the principles of the Declaration of Helsinki. The option to opt out was clearly defined and was always available to patients by presenting this information on the website. This retrospective study was conducted at Tobata Kyoritsu Hospital (Fukuoka, Japan) between April 1, 2021, and December 31, 2022. Consent to publish information, including photographs, was obtained from all patients and relevant persons (such as parents or legal guardians).
We reviewed five cases of deep pelvic fluid accumulation that could not be achieved using an anterior approach. The causes of fluid collections included pelvic abscesses in postoperative patients with colorectal cancer (n = 3) (Figure 1, 2), sigmoid diverticulitis (n = 1) (Figure 3), and perforated appendicitis (n = 1) (Table 1)[9]. Abdominal CT provided an initial diagnosis for all patients with pelvic effusion. Blood tests revealed normal coagulation parameters and platelet counts in all patients. All patients had fluid accumulation located in the rectovesical excavation or Douglas' pouch in the deep pelvis, necessitating a transgluteal approach. A Convex 3-6 MHz transducer was used to scan the pelvis from the parasacral region in the prone position. The patient was administered local anesthesia only, and the fluid pool was punctured under continuous ultrasound guidance. The sacrum or coccyx was palpated as a landmark, and the puncture site was kept as close to this landmark on the caudal side as possible to avoid injury to the neurovascular bundle and piriform muscle[8]. After aspirating the fluid, a guidewire was placed and an 8-French pigtail catheter was advanced into the fluid collection using the Seldinger technique. Fluoroscopy was used for guidewire manipulation and final catheter placement, and a contrast enema was used in two cases. Cultures were obtained from the drained fluid. Contrast studies were performed to confirm reduction in the abscess cavity. The catheter was removed if there was no drainage and no residual lumen remained on the contrast. If residual lumen was found and drainage persisted, the catheter was replaced with a larger-diameter catheter after 7 days. Three patients underwent catheter replacement. Intravenous antibiotic therapy was determined based on culture and sensitivity results.
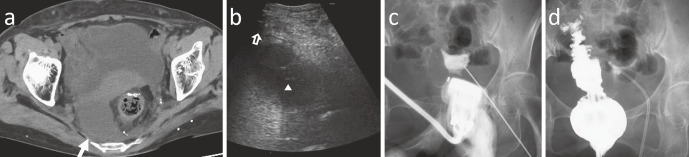
Figure 1.
(a) An 85-year-old woman with pelvic abscess (arrow) after colorectal cancer surgery. (b) The sonogram shows the puncture needle tip (arrow head) in the collected fluid from a transgluteal approach. Shadowing (open arrow) at the left edge of the image is originating from the sacrum (coccyx) (Supplementary-material). (c) Fluoroscopic imaging allows the shape of the abscess cavity to be determined and facilitates the manipulation of guidewire and tube placement. (d) A fluoroscopy can be used in conjunction with irrigoscopy.
Figure 2.
(a) Axial computed tomography (CT) image at the level of the sacrospinous ligament (open arrow) showing the rectum compressed dorsal to the abscess cavity (asterisk). (b) Sonography shows the high echoic lesion (open arrow) originating from the sacrum (coccyx). As with the CT scan, a rectum is visible that had been compressed into the abscess cavity. (c) Tubes can be placed appropriately in the abscess cavity using fluoroscopy.
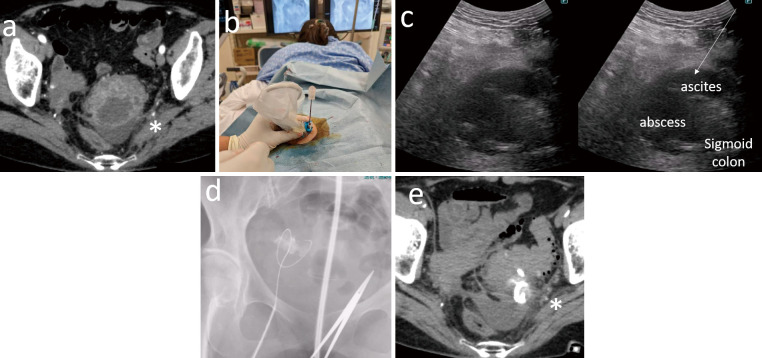
Figure 3.
(a) Axial computed tomography (CT) image at the level of the piriformis muscle (asterisk) of a 73-year-old woman with pelvic abscess due to diverticulitis of the sigmoid colon. (b) Drainage was performed in the prone position under local anesthesia only. The lower end of the sacrum or coccyx is palpated as a merkmal and punctured cephalad and medially from near the sacrum or coccyx. (c) Sonography shows ascites in the Douglas pouch of the rectum and abscess formation in the sigmoid mesentery, similar to CT images. (d) Fluoroscopic imaging allows easy manipulation of the guidewire. (e) CT scan after drainage showing disappearance of the abscess cavity and puncture avoiding the piriform muscle (asterisk).
Table 1.
Details of Each Case in Which Abscess Drainage Was Performed.
| Cases | age | gender | Causes of abscess formation |
Colostomy before drainage |
Duration of catheter drainage |
|---|---|---|---|---|---|
| 1 | 85 | female | Unknown | No | 4 |
| 2 | 68 | female | Anastomotic leak | Yes | 14 |
| 3 | 74 | male | Anastomotic leak | Yes | 9 |
| 4 | 73 | female | Penetration of sigmoid diverticulitis | No | 7 |
| 5 | 78 | female | Complicated appendicitis | No | 14 |
We used the SYNAPSE VINCENT to evaluate the anatomy of the pelvic cavity, focusing on the transgluteal drainage route. First, the pelvic bones and sacrospinous and sacroiliac ligaments were converted into 3D images. Next, the pathways of the piriform muscle, sciatic nerve, and internal and external iliac arteriovenous systems were converted into 3D images. Finally, the abscess cavity was delineated to evaluate the anatomic structures, mainly the puncture pathways (Figure 4).
Figure 4.
(a) The greater sciatic foramen is a large foramen bounded by the ilium and sciaticum, sacrotuberous ligament (connecting the sacrum and sciatic tuberosity), and sacrospinous ligament (connecting the sacrum and sciatic spine). (b) The piriform muscle passes through the center of this foramen and is divided into upper and lower piriform foramina (circle). (c) The superior foramen contains the superior gluteal arteriovenous system and nerves. The inferior foramen is passed through the inferior gluteal arteriovenous system and nerve: the sciatic nerve, the internal genital arteriovenous system, and the genital nerves. These nerves and vessels run in a lateral and anterior direction under the piriform muscle; therefore, an avascular area exists on the inner side. The puncture route passes through this infrapiriform foramen. (d) The parasacral infrapiriformis approach, which passes through the inferior piriform foramen and punctures the cephalad and medially.
Results
Patient details are listed in Table 1. The mean age of patients was 75.6 years (standard deviation [SD] = 6.3), and most were women (n = 4, 80%). Three patients had postoperative abscesses caused due to colorectal cancer (Figure 1, 2), one had an abscess caused by penetration of sigmoid diverticulitis (Figure 3), and one had an abscess caused by perforation of the appendicitis[9]. The average duration of drainage was 11 days (SD = 6.7), of which three patients required catheter replacement with a larger-diameter drain. No complications, such as bleeding or nerve damage, were observed. One patient with perforated appendicitis underwent interval laparoscopic appendectomy[9].
Discussion
The transgluteal approach to deep pelvic abscesses is commonly performed under CT guidance, with more than 95% success rate for CT-guided transgluteal abscess drainage and a 20% complication rate. Since drainage is primarily an alternative to surgery, surgical drainage was performed in unsuccessful cases, or surgical repair was performed for those intestinal fistulas that did not close with transgluteal drainage[1]. The most common complication is buttock pain; however, more serious complications such as radiating leg pain, numbness, and pelvic bleeding have also been reported, and transcatheter embolization may be required in case of bleeding[1,5,10-12]. Because of the similar puncture route, the expected complication in the ultrasound-guided approach are essentially the same as those in the CT-guided approach. In the 12 case series reported, one case of technical failure requiring a CT-guided procedure and one case of sciatic nerve irritation were reported. There were no reports of bleeding requiring transcatheter arterial embolization[6]. Furthermore, there were no adverse events in our study. Regarding nerve and vessel injury, placement of a catheter upward near the piriform muscle or sacral plexus increases the incidence of pelvic and leg pain, so whenever possible, the catheter route should pass below the foramen through the sacrospinous ligament or below it[1,5,11]. Walser et al.[8] performed transgluteal ultrasonography via a parasacral approach. The advantages of ultrasound include a short time in the CT imaging area, short procedure time, low radiation exposure, and real-time color Doppler imaging (CDI) during needle placement to avoid vascular puncture. In addition, the drainage procedure can be performed in a fluoroscopy room and a sinogram can be obtained immediately. One disadvantage of the ultrasound-guided technique is that it is difficult to confirm the abscess cavity in some cases, especially in obese patients, when the penetration of ultrasonography into deep pelvic tissues is poor. Identification may also be difficult in cases of small fluid collection. Therefore, transgluteal drainage should be selected in cases where the diagnosis of a pelvic abscess has been established using other imaging modalities, such as CT or magnetic resonance imaging, and the transgluteal puncture route can be confirmed by ultrasound in non-obese patients[6].
In gastrointestinal surgery, especially hepatobiliary and pancreatic surgery, SYNAPSE VINCENT has been reported to be useful for preoperative simulation and navigation imaging[13,14]. We constructed a 3D image of the puncture route of the trans greater sciatic foramen using SYNAPSE VINCENT to objectively comprehend the anatomy and puncture route. The greater sciatic foramen is a large foramen bound by the ilium and sciaticum, sacrotuberous ligament (connecting the sacrum and sciatic tuberosity), and sacrospinous ligament (connecting the sacrum and sciatic spine) (Figure 4a). The piriform muscle passes through the center of this foramen and is divided into the upper and lower piriform foramina (Figure 4b). The superior foramen contains the superior gluteal arteriovenous system and the nerves. The inferior foramen passes through the inferior gluteal arteriovenous system and nerve: the sciatic nerve, internal genital arteriovenous system, and genital nerves (Figure 4c). The puncture route passes through the infrapiriform foramen. Because a branch of the inferior gluteal artery penetrates the piriform muscle, puncturing the piriform muscle increases the risk of bleeding[1-5]. The obturator nerve and obturator arteriovenous vein pass caudally along the pelvic cavity, lateral to the greater sciatic foramen; therefore, no injury occurs when approaching medially from the inferior to the piriform muscle[15]. In addition, because the vessels of the pubic system and the sciatic nerve travel laterally through the inferior piriformis foramen, there are no major vessels or nerves near or medial to the sacrum (Figure 4d). Therefore, the term aspiration is used near the sacrum and at the level of the sacrospinous ligament as described by Butch[1]. Sonography with CDI can identify vascular branches that are difficult to identify on CT scans, but may be the source of hemorrhage. In some cases, the rectum and sigmoid colon can also be identified by sonography; combined with fluoroscopy, the Seldinger technique facilitates guidewire manipulation and tube placement and can be used to mark the location of colorectal gas or in conjunction with a contrast study of the rectum to more accurately determine the anatomy.
We believe that the use of SYNAPSE VINCENT allows us to objectively understand the anatomy of the deep pelvic region and the safety of the transgluteal approach. The name transgluteal approach is too broad, and it is more accurate to call it the parasacral infrapiriformis approach, which passes through the inferior piriform foramen and punctures in the superomedial direction. This approach is considered safe and easy to perform with the combined use of ultrasound and fluoroscopy. In conclusion, the ideal transgluteal approach involves inserting the catheter as close to the sacrum as possible to the level of the infrapiriformis. This technique can be safely and effectively performed using ultrasound guidance and fluoroscopy. In addition, we propose a new name, the sonography-guided “parasacral infrapiriformis approach” for deep pelvic abscesses.
Conflicts of Interest
There are no conflicts of interest.
Author Contributions
All authors contributed to conceive and design the study. Daisuke Muroya contributed to the concept, design, data acquisition, and analysis and drafted and revised the manuscript; HS, TN, YN, TT, Daiki Miyazaki, SA, and TH contributed to data acquisition, revised the manuscript, and approved the final version.
Approval by Institutional Review Board (IRB)
This research was approved by the institutional review board of Tobata Kyoritsu Hospital (approval code: 22-17)
Data Availability Statement
The datasets for the current study are available from the corresponding author upon reasonable request.
Supplementary Files
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
References
- 1.Butch RJ, Mueller PR, Ferrucci JT Jr, et al. Drainage of pelvic abscesses through the reater sciatic foramen. Radiology. 1986 Feb; 158(2): 487-91. doi: 10.1148/radiology.158.2.3941878. [DOI] [PubMed] [Google Scholar]
- 2.Gervais DA, Hahn PF, O'Neill MJ, Mueller PR. CT-guided transgluteal drainage of deep pelvic abscesses in children: selective use as an alternative to transrectal drainage. AJR. 2000 Nov; 175(5): 1393-6. doi: 10.2214/ajr.175.5.1751393. [DOI] [PubMed] [Google Scholar]
- 3.Ryan JM, Murphy BL, Boland GW, Mueller PR. Use of the transgluteal route for percutaneous abscess drainage in acute diverticulitis to facilitate delayed surgical repair. AJR Am J Roentgenol. 1998 May; 170(5): 1189-93. doi: 10.2214/ajr.170.5.9574582. [DOI] [PubMed] [Google Scholar]
- 4.Mueller PR, Sini S, Wittenburg J, et al. Sigmoid diverticular abscesses: percutaneous drainage as an adjunct to surgical resection in 24 cases. Radiology. 1987 Aug; 164(2): 321-5. doi: 10.1148/radiology.164.2.3602369. [DOI] [PubMed] [Google Scholar]
- 5.Harisinghani MG, Gervais DA, Hahn PF, et al. CT-guided transgluteal drainage of deep pelvic abscesses: indications, technique, procedure-related complications, and clinical outcome. Radiographics. 2002 Nov; 22(6): 1353-67. doi: 10.1148/rg.226025039. [DOI] [PubMed] [Google Scholar]
- 6.Walser E, Raza S, Hernandez A, et al. Sonographically guided transgluteal drainage of pelvic abscesses. AJR Am J Roentgenol. 2003 Aug; 181(2): 498-500. doi: 10.2214/ajr.181.2.1810498. [DOI] [PubMed] [Google Scholar]
- 7.Robert B, Chivot C, Rebibo L, et al. Percutaneous transgluteal drainage of pelvic abscesses in interventional radiology: A safe alternative to surgery. J Visc Surg. 2016 Feb; 153(1): 3-7. doi: 10.1016/j.jviscsurg.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Matsuhashi N, Sato Y, Tajima JY, et al. Evaluation of the SYNAPSE VINCENT for lateral lymph node dissection in rectal cancer with robotic surgery: a preliminary report. World J Surg Oncol. 2022 Feb; 20(1): 56. doi: 10.1186/s12957-022-02532-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arai S, Muroya D, Okabe M, et al. Ultrasound-guided transgluteal drainage of a pelvic abscess complicated with appendicitis: a case report. J Abdom Emerg Med. 2020; 40(1): 103-6. Japanese. [Google Scholar]
- 10.Casola G, vanSonnenberg E, D'Agostino HB, et al. Percutaneous drainage of tubo-ovarian abscesses. Radiology. 1992 Feb; 182(2): 399-402. doi: 10.1148/radiology.182.2.1732956. [DOI] [PubMed] [Google Scholar]
- 11.Zhao N, Li Q, Cui J, et al. CT-guided special approaches of drainage for intraabdominal and pelvic abscesses: One single center's experience and review of literature. Medicine. 2018 Oct; 97(42): e12905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malden ES, Picus D. Hemorrhagic complication of transgluteal pelvic abscess drainage: successful percutaneous treatment. J Vasc Interv Radiol. 1992 May; 3(2): 323-6. doi: 10.1016/s1051-0443(92)72036-3. [DOI] [PubMed] [Google Scholar]
- 13.Oshiro Y, Yano H, Mitani J, et al. Novel 3-dimensional virtual hepatectomy simulation combined with real-time deformation. World J Gastroenterol. 2015 Sep; 21(34): 9982-92. doi: 10.3748/wjg.v21.i34.9982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ohshima S. Volume analyzer SYNAPSE VINCENT for liver analysis. J Hepatobiliary Pancreat Sci. 2014 Feb; 21(4): 235-8. doi: 10.1002/jhbp.81. [DOI] [PubMed] [Google Scholar]
- 15.Harisinghani MG, Gervais DA, Hahn PF, et al. CT-guided transgluteal drainage of deep pelvic abscesses: indications, technique, procedure-related complications, and clinical outcome. Radiographics. 2002 Nov; 22(6): 1353-67. doi: 10.1148/rg.226025039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.