Abstract
Management of patellofemoral conditions in children and adolescents can be extremely challenging. Apart from the patellofemoral instability patients, there are several other disorders that can cause significant morbidity, patellofemoral maltracking, patellar tilt, and Hoffa's fat pad impingement syndrome are common problems that may not respond to nonoperative management. Understanding the exact pathology and apply the appropriate management is critical for successful outcome. Identification of novel surgical interventions that can provide symptom relief in a safe manner is important. This technical note describes a surgical technique for patella realignment in young patients that combines safety, simplicity, and reproducibility.
Technique Video
Patellofemoral conditions are extremely common in children and young adults with a point prevalence ranging between 5.7% to 28% for patellofemoral pain.1 Patellofemoral instability is also extremely common, with incidence rates ranging from 23 to 69 per 100,000 person per year but can be much higher in adolescence, identified as 147.7 per 100,000 persons per year.2,3 Patellofemoral conditions can result in severe morbidity and inability to participate in athletic activities but may also affect daily life activities. Persistent patellofemoral instability, maltracking, and cartilage lesions can lead to osteoarthritis long term.4, 5, 6, 7 Several different techniques have been described for recurrent patellofemoral instability, with medial patellofemoral ligament (MPFL) reconstruction recently gaining a leading role in the management of recurrent instability because of its effectiveness and ability to restore anatomy and isometry.8, 9, 10, 11
Pediatric patients with first-time dislocation can also be treated with MPFL reconstruction with good results depending on associated risk factors such as age, hyperlaxity, trochlear dysplasia, and more.8 However, for very young pediatric patients with open physis, there is a risk of growth disturbance with the bone tunnels and concerns for graft isometry with the growing skeleton.12,13 When these risk factors are not present, typical management of young patients with first-time instability is nonoperative, unless there is a specific reason to intervene, such as an avulsion fracture or a loose body. For these young patients with a single instability event, the role of MPFL reconstruction is controversial. Similarly, there are patellofemoral conditions, such as patella maltracking, patellar tilt, and Hoffa pad impingement syndrome where there are no frank instability events, and therefore an MPFL reconstruction is not indicated. In these conditions, a minimally invasive arthroscopic intervention can result in favorable outcome for cases refractory to nonoperative management. Hereby, this article presents an arthroscopic patella realignment technique via a single portal incision.
Surgical Technique
The patient is positioned supine on the operating table with a lateral knee post to assist for arthroscopy. A nonsterile tourniquet can be used for adequate visualization based on surgeon’s preference. The arthroscopy is performed in a standard manner via anterolateral and anteromedial portals. After a complete diagnostic knee arthroscopy confirming the presence of the associated pathology and its indicated treatment, such as removal of loose body, plica excision, etc., the arthroscopic patella realignment can be performed. Please see the details of the technique in Video 1.
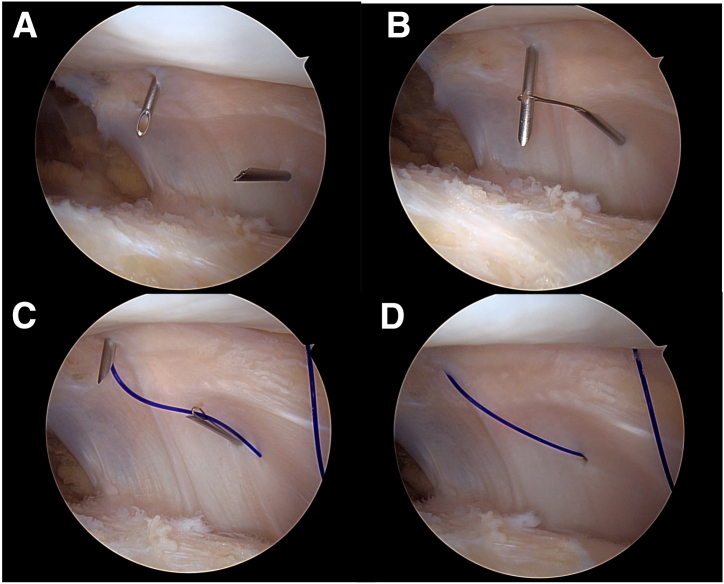
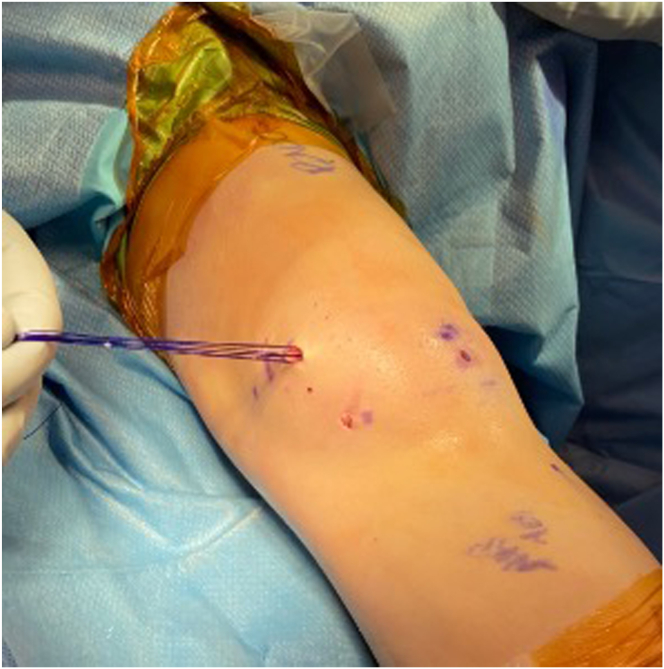
An outside-in technique configuration like that used for meniscus repair can be used. The outside-in meniscus repair system (Smith and Nephew, Andover MA) can be applied for this technique, using straight and curve arthroscopic needles for suture passing. Under arthroscopic visualization the attachment sites of the MPFL are recognized as well as the anatomic landmarks of the patella and the MPFC. Then, depending on the degree of patella maltracking, a different number of PDS no. 0 sutures (typically 2-7) are placed at the attenuated medial patellofemoral ligament. Extreme care should be taken to place the sutures close to the attachment points of the MPFL to allow proper tensioning of the repair. The sutures are inserted via 1 needle and are retrieved using a loop retriever via a different arthroscopic needle (Fig 1). The configuration of the sutures can differ depending on the degree of maltracking or the condition treated (Fig 2). After all sutures are passed, a small 1 cm longitudinal incision was made just medial to the medial border of the patella (Fig 3). Via this small incision, a straight Kelly clamp is used to bluntly dissect into the medial aspect of the knee, reaching into the second layer. Extreme care is taken to protect the capsule and avoid dissection into the joint. Then all sutures are retrieved via this incision with a suture loop retriever and an arthroscopic probe (Fig 4). Then, under direct visualization and with the patella being positioned at the center of trochlear groove, the sutures are tied at the level of the capsule. Direct arthroscopic visualization is necessary to ensure proper tension of the repair that confirms proper tension, normal tilt, and normal tracking of the patella. The knee is placed at 30° to 40° of flexion. After the repair, the knee undergoes full range of motion assessment to ensure proper patella tracking and positioning without overload.
Fig 1.
Arthroscopic visualization of the medial aspect of the patellofemoral joint of the right knee, viewing from the anterolateral portal. (A) The arthroscopic needles are inserted at the patella attachment and the midsubstance of the medial patellofemoral ligament. (B). The loop is used to assist suture passage. (C). A PDS suture is retrieved from one side with the use of the loop. (D). The needles are removed, and the repair suture has been placed intra-articularly.
Fig 2.
Parallel (A) or crossover (B) configuration of suture placement for patella realignment can be used depending on the condition treated. In this example, the right knee is viewed from the anterolateral portal.
Fig 3.
With the patient supine, standard arthroscopic portals are made. The patella realignment portal is marked just medial to the medial border of the patella (arrow). In this example, the left knee is treated.
Fig 4.
All sutures are retrieved via a single incision. Care should be taken to avoid overlap or crossing of the sutures. In this example, the left knee is treated.
After surgery, patients are partial weightbearing for 2 weeks and then advance to weightbearing as tolerated with crutches. A hinged knee brace is used for the first 2 weeks, and, after demonstrating adequate quadriceps strength recovery and control, the patient is weaned off the brace, under the directions of physical therapy. At 8 to 10 weeks, depending on meeting the strength criteria, the patient is allowed to start impact, and a return to running protocol is provided. Pivoting and cutting is allowed at 3 months, and return to all athletic activities is allowed at 4 months after surgery.
Discussion
The arthroscopic patella realignment technique described in this article offers the advantages of minimally invasive approach via a single incision, direct arthroscopic visualization of the repair, and use of absorbable sutures without intra-articular knots. This technique can be used for cases of patella maltracking and patellofemoral pain and offers a safe alternative for anatomic restoration of the patellofemoral kinematics. Pearls and pitfalls for the details of this technique are presented in Table 1.
Table 1.
Pearls and Pitfalls
| Pearls |
| Ensure that the level of the capsule is reached, so the sutures will be between layers 2 and 3. |
| Place the sutures close to the attachment of the MPFL at the patella to allow proper control and tensioning. |
| Test the mobility of the patella to ensure that the sutures are addressing patella maltracking and add a lateral release—only if necessary. |
| Pitfalls |
| Do not over tighten your repair. |
| Place the knee at 30° 40° of flexion and do not forget to complete a full ROM assessment after the repair is done. |
MPFL, medial patellofemoral ligament; ROM, range of motion.
Open and arthroscopic medial plication has been described in the past for patellofemoral instability.14,15 There are certain limitations for these techniques, and in the past they were used for patella instability combined with lateral release. Lateral release has shown that it may increase the risk of patella instability and is associated with poor outcomes.16, 17, 18 The technique described here is not designed to act as an alternative procedure for recurrent patella instability. MPFL reconstruction is probably a better solution due to its effectiveness and the use of a graft that restores the medial patellofemoral complex.9,19 However, MPFL reconstruction has some limitations, such as the need for use of autograft with the associated morbidity and invasiveness, and the risk of complications, including a low risk for growth disturbance in skeletally immature patients.13,20 As a result, in patients with patellofemoral symptoms of maltracking without frank instability, the arthroscopic patella realignment described above can be a safe and effective solution in a carefully selected patient population. Additional advantages and disadvantages are presented in Table 2.
Table 2.
Advantages and Disadvantages
| Advantages |
| Minimally invasive with a single incision |
| Direct arthroscopic visualization of the repair |
| Use of absorbable sutures without intra-articular knots |
| Safe for skeletally immature patients |
| Disadvantages |
| The technique is not designed to treat patellofemoral instability |
| Extreme care is required to ensure isometry |
Several patellofemoral conditions apart from patellofemoral instability can cause significant morbidity in young patients.1 Patellofemoral pain presenting one of the most common conditions in adolescents, reaching an annual prevalence of 28.9%.1 During growth patellofemoral anatomy appears to change and influences maltracking in adolescents with patellofemoral pain.21 Hoffa's fat pad impingement, patella tilt and plica syndrome have been associated with anterior knee pain in children and young adults, but their association with patella maltracking remains unclear.21, 22, 23, 24, 25 Understanding the spectrum of conditions under the term patellofemoral pain syndrome is critical to providing patient care with successful outcome. When nonoperative management fails, application of minimally invasive and safe surgical techniques such the one described in this technical note could be considered.
Disclosures
The author reports the following potential conflicts of interest or sources of funding: N.K.P reports personal fees from AANA, during the conduct of the study. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic patella realignment technique via a single portal incision. In this example, the patient is supine and the right knee is viewed from the anterolateral portal.
References
- 1.Smith B.E., Selfe J., Thacker D., et al. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS One. 2018;13(1) doi: 10.1371/journal.pone.0190892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsiao M., Owens B.D., Burks R., Sturdivant R.X., Cameron K.L. Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010;38:1997–2004. doi: 10.1177/0363546510371423. [DOI] [PubMed] [Google Scholar]
- 3.Sanders T.L., Pareek A., Hewett T.E., Stuart M.J., Dahm D.L., Krych A.J. Incidence of first-time lateral patellar dislocation: A 21-year population-based study. Sports Health. 2018;10:146–151. doi: 10.1177/1941738117725055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant J.A. Editorial commentary: Stabilize the patella to achieve functional gain but don’t neglect the cartilage that may cause long-term pain! Trochlear dysplasia plays a role in both. Arthroscopy. 2021;37:3477–3478. doi: 10.1016/j.arthro.2021.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Paschos N.K. Editorial commentary: Patellofemoral instability results in osteoarthritis, and nonanatomic surgery and surgical over-constraint may also cause osteoarthritis. Arthroscopy. 2023;39:358–359. doi: 10.1016/j.arthro.2022.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Douiri A., Lavoué V., Galvin J., Boileau P., Trojani C. Arthroscopic lateral patellar facetectomy and lateral release can be recommended for isolated patellofemoral osteoarthritis. Arthroscopy. 2022;38:892–899. doi: 10.1016/j.arthro.2021.06.021. [DOI] [PubMed] [Google Scholar]
- 7.Shatrov J., Vialla T., Sappey-Marinier E., et al. At 10-year minimum follow-up, one-third of patients have patellofemoral arthritis after isolated medial patellofemoral ligament reconstruction using gracilis tendon autograft. Arthroscopy. 2023;39:349–357. doi: 10.1016/j.arthro.2022.07.021. [DOI] [PubMed] [Google Scholar]
- 8.Bremond N., Prima R., Rabattu P.Y., et al. Isolated MPFL reconstruction with soft tissue femoral fixation technique in 54 skeletally immature patients: Clinical outcomes at 2 years follow-up. A French multicenter retrospective study. Orthop Traumatol Surg Res. 2023;109(8) doi: 10.1016/j.otsr.2022.103530. [DOI] [PubMed] [Google Scholar]
- 9.Husen M., Milbrandt T.A., Shah V., Krych A.J., Stuart M.J., Saris D.B.F. Medial patellofemoral ligament reconstruction using allografts in skeletally immature patients. Am J Sports Med. 2023;51:1513–1524. doi: 10.1177/03635465231164400. [DOI] [PubMed] [Google Scholar]
- 10.Hohmann E. Editorial commentary: From lateral release and medial plication to complex medial patellofemoral ligament reconstruction techniques: Medial quadriceps tendon femoral ligament reconstruction is the most anatomic repair. Arthroscopy. 2023;39:670–672. doi: 10.1016/j.arthro.2022.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Shi W.L., Hu F.Y., Xu M.T., et al. Arthroscopic anatomical double-bundle medial patellofemoral complex reconstruction improves clinical outcomes in treating recurrent patellar dislocation despite trochlear dysplasia, elevated tibial tubercle–Trochlear groove distance, and patellar alta. Arthroscopy. 2023;39:102–111. doi: 10.1016/j.arthro.2022.06.038. [DOI] [PubMed] [Google Scholar]
- 12.Keyes S., Price M., Green D.W., Parikh S.N. Special considerations for pediatric patellar instability. Am J Orthop (Belle Mead NJ) 2018;47(3) doi: 10.12788/ajo.2018.0017. [DOI] [PubMed] [Google Scholar]
- 13.Uppstrom T.J., Price M., Black S., Gausden E., Haskel J., Green D.W. Medial patellofemoral ligament (MPFL) reconstruction technique using an epiphyseal femoral socket with fluoroscopic guidance helps avoid physeal injury in skeletally immature patients. Knee Surg Sports Traumatol Arthrosc. 2019;27:3536–3542. doi: 10.1007/s00167-019-05412-7. [DOI] [PubMed] [Google Scholar]
- 14.Nam E.K., Karzel R. Mini-open medial reefing and arthroscopic lateral release for the treatment of recurrent patellar dislocation: A long-term follow-up (SS-52) Arthroscopy. 2004;20:e24. doi: 10.1177/0363546504267803. [DOI] [PubMed] [Google Scholar]
- 15.Prasathaporn N., Kuptniratsaikul S., Kongrukgreatiyos K. Arthroscopic medial retinacular plication with a needle-hole technique. Arthrosc Tech. 2014;3(4):e483–e486. doi: 10.1016/j.eats.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clifton R., Ng C.Y., Nutton R.W. What is the role of lateral retinacular release? J Bone Joint Surg Br. 2010;92-B(1):1–6. doi: 10.1302/0301-620X.92B1.22909. [DOI] [PubMed] [Google Scholar]
- 17.Ricchetti E.T., Mehta S., Sennett B.J., Huffman G.R. Comparison of lateral release versus lateral release with medial soft-tissue realignment for the treatment of recurrent patellar instability: A systematic review. Arthroscopy. 2007;23:463–468. doi: 10.1016/j.arthro.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 18.Malatray M., Magnussen R., Lustig S., Servien E. Lateral retinacular release is not recommended in association to MPFL reconstruction in recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc. 2019;27:2659–2664. doi: 10.1007/s00167-018-5294-7. [DOI] [PubMed] [Google Scholar]
- 19.Platt B.N., Bowers L.C., Magnuson J.A., et al. Return to sport after medial patellofemoral ligament reconstruction: A systematic review and meta-analysis. Am J Sports Med. 2022;50:282–291. doi: 10.1177/0363546521990004. [DOI] [PubMed] [Google Scholar]
- 20.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fick C.N., Grant C., Sheehan F.T. Patellofemoral pain in adolescents: Understanding patellofemoral morphology and its relationship to maltracking. Am J Sports Med. 2020;48:341–350. doi: 10.1177/0363546519889347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rathleff M.S., Rathleff C.R., Olesen J.L., Rasmussen S., Roos E.M. Is knee pain during adolescence a self-limiting condition? Prognosis of patellofemoral pain and other types of knee pain. Am J Sports Med. 2016;44:1165–1171. doi: 10.1177/0363546515622456. [DOI] [PubMed] [Google Scholar]
- 23.Subhawong T.K., Eng J., Carrino J.A., Chhabra A. Superolateral Hoffa’s fat pad edema: Association with patellofemoral maltracking and impingement. Am J Roentgenol. 2010;195:1367–1373. doi: 10.2214/AJR.10.4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kamel S.I., Kanesa-Thasan R.M., Dave J.K., et al. Prevalence of lateral patellofemoral maltracking and associated complications in patients with Osgood Schlatter disease. Skeletal Radiol. 2021;50:1399–1409. doi: 10.1007/s00256-020-03684-6. [DOI] [PubMed] [Google Scholar]
- 25.Hufeland M., Treder L., Kubo H.K., Verde P.E., Krauspe R., Patzer T. Symptomatic medial synovial plica of the knee joint: an underestimated pathology in young patients. Arch Orthop Trauma Surg. 2019;139:1625–1631. doi: 10.1007/s00402-019-03249-w. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic patella realignment technique via a single portal incision. In this example, the patient is supine and the right knee is viewed from the anterolateral portal.