Abstract
At present, the repair pattern of upper third of subscapularis tendon partial-thickness tears (upper-third tendon tears) is performed in the glenohumeral joint and conventional subacromial viewing portal, but the visualization of subscapularis tendon and footprint is poor when using a 30° scope. The modified subacromial viewing portal presented in this Technical Note is a modified surgical technique for the repair of upper-third tendon tears. Since the scope forms an angle of 70° with the subscapularis tendon and footprint of lesser tuberosity, satisfactory visualization can be obtained when using 30° scope; the predesigned surgical portal and working space without bony barrier can offer a smooth surgical procedure. Our surgical technique is described in pearls, pitfalls, advantages, and disadvantages.
Technique Video
Upper third of subscapularis tendon partial-thickness tears (upper-third tendon tears) are described by some authors as “hidden lesions of the subscapular tendon.”1, 2, 3 Although good clinical outcomes following arthroscopic repair have been reported,4 missed diagnoses of subscapularis tendon tears during surgery also have been widely documented.3,5,6
Good visualization of the subscapularis tendon and footprint of lesser tuberosity is crucial to receive the desired anatomical reattachment7,8; however, the visualization of the tendon and footprint in the glenohumeral joint and conventional subacromial viewing portal is poor when using a 30° scope.9,10 The intra-articular repair procedure also possesses other shortcomings, such as a narrow working space and restricted surgical portals, all of which will have a negative impact on outcomes following tendon repair.8,11
The modified subacromial viewing (MSV) portal presented in this study is a modified surgical technique for the repair of upper-third tendon tears. Since the scope forms an angle of 70° with the subscapularis tendon and footprint of lesser tuberosity, the satisfactory visualization can be obtained when using a 30° scope; the predesigned surgical portal and working space without bony barrier offer a smooth surgical procedure.
Surgical Technique (With Video Illustration)
Preparation
All patients are operated under general anesthesia and positioned in the lateral decubitus position with the arm in 20° flexion and 30° abduction; a 30° scope (Smith & Nephew) is acceptable. The surgical technique is described in Table 1 (pearls, pitfalls), and Table 2 lists advantage sand disadvantages. This research was approved by the ethical department in our hospital, and all patients gave informed consent.
Table 1.
Surgical Pearls and Pitfalls
Surgical visualization considerations (1)Opening rotator interval is the initial procedure in exposing the subscapularis tendon.
|
Table 2.
Advantages and Disadvantages
Advantages
|
Diagnosis and Evaluation
During arthroscopy of the glenohumeral joint through the posterior portal, the integrity of subscapularis tendon and other lesions are examined. The extension of subscapularis tendon tear in transverse and coronal planes is analyzed with the arm in flexion with internal rotation (Video 1 and Fig 1). The rotator interval is opened with radiofrequency. Either tenotomy or tenodesis is performed for cases with evidence of biceps tear, subluxation, and dislocation.
Fig 1.

The extension of subscapularis tendon tear in the transverse and coronal planes is analyzed with the arm in flexion with internal rotation. The asterisk indicates the rupture portion of the tendon. (GL, glenoid labrum; H, head of the humerus; SSC, the subscapularis tendon.)
Surgical Portal Creation
Arthroscopic MSV portal repair of upper-third tendon tears is designed with 4 subacromial portals (Fig 2). The “A” portal (MSV portal) is the specific viewing portal for the tendon repair procedure, created between the coracoid process and anterolateral corner of the acromion. The “B” portal is the specific access for suture anchor insertion, created approximately 2 cm medial to the A portal. The “C” portal specifically is for applying suture hooks and is created approximately 3 cm distal to A portal. The “D” portal is the conventional subacromial viewing (CSV) portal, created at the midpoint between anterior and posterior corner of the acromion.
Fig 2.
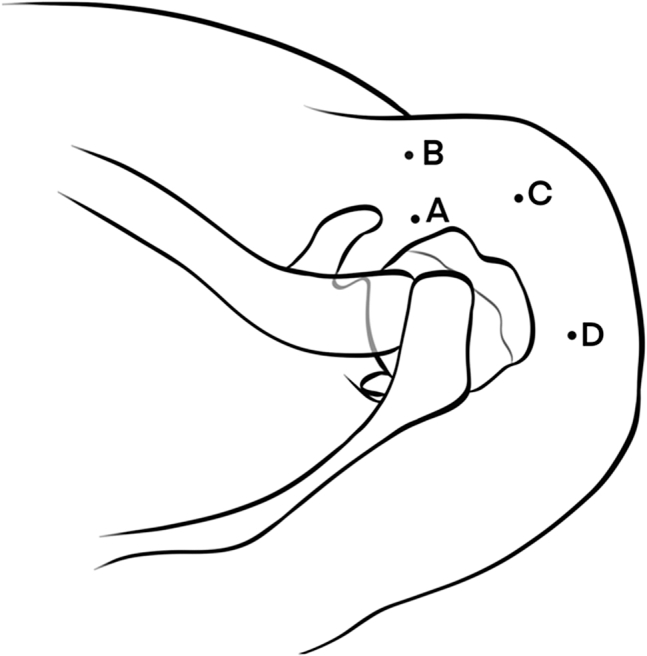
Arthroscopic MSV portal repair of upper third tendon tears is designed with 4 subacromial portals. (MSV, modified subacromial viewing.)
Viewing From the CSV Portal
The scope is introduced into the CSV portal (i.e., D portal) (Fig 3). Bursectomy is performed. Find the coracoid process along coracoacromial ligament, then debride the synovium between undersurface of coracoid process and subscapularis tendon. Identify the presence of the accompanying tear on the bursal side of the subscapularis tendon. Since the scope forms an angle of 10° with subscapularis tendon and footprint of lesser tuberosity (Fig 4), poor visualization of the tendon will be obtained (Fig 5); the footprint is invisible due to the obstruction of medial suspensory ligament.
Fig 3.

The scope is introduced into the CSV portal (D portal). (CSV, conventional subacromial viewing.)
Fig 4.

The scope located in the CSV portal (D portal) forms an angle of 10° with the subscapularis tendon and footprint of lesser tuberosity. (CSV, conventional subacromial viewing.)
Fig 5.
The poor visualization of the subscapularis tendon will be obtained from CSV portal (D portal). (CP, coracoid process; CSV, conventional subacromial viewing; G, glenoid; SSC, the subscapularis tendon.)
Viewing From the MSV Portal
The scope is moved from the CSV portal (D portal) to the MSV portal (A portal) (Fig 6). Since the scope forms an angle of 70° with the footprint of lesser tuberosity (Fig 7), satisfactory visualization of the bare footprint can be obtained just by moving the medial suspensory ligament anteriorly and distally (Fig 8), instead of removing this site. The B portal is designed by guidance with a spinal needle. After preparing the footprint, a 5.0-mm suture anchor (Corkscrew Anchor; Arthrex, Naples, FL) is inserted into the bleeding footprint near the cartilage rim with the angle of 45° through the B portal (Fig 9). The optimal location of suture anchor insertion can be adjusted by the arm rotation.
Fig 6.

The scope is introduced into the MSV portal (A portal). (MSV, modified subacromial viewing.)
Fig 7.

The scope located in the MSV portal (A portal) forms an angle of 70° with the subscapularis tendon and footprint of lesser tuberosity. (MSV, modified subacromial viewing.)
Fig 8.
The satisfactory visualization of the bare footprint of lesser tuberosity can be obtained from the MSV portal (A portal) just by pushing the medial suspensory ligament anteriorly and distally. (H, head of the humerus; LT, the footprint of lesser tuberosity; MSV, modified subacromial viewing; SSC, the subscapularis tendon.)
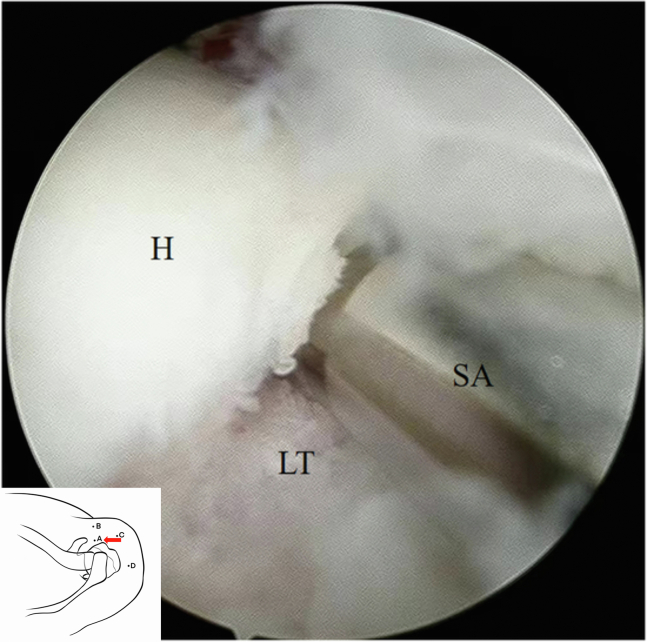
Fig 9.
A 5.0-mm suture anchor is inserted into the bleeding footprint near cartilage rim with the angle of 45° through the B portal. (H, head of the humerus; LT, the footprint of lesser tuberosity; SA, suture anchor.)
The scope remains in the MSV portal (A portal). Since the scope forms an angle of 70° with the subscapularis tendon, the tendon from tear portion to medial edge of coracoid process can be well visualized (Fig 10). The C portal is designed by guidance with a spinal needle (Fig 11). Although the challenge of the coracoid process obstructing the suture hook is inherent in the MSV portal, this problem can be solved by internal rotation of the arm. The tendon is sewn with a suture hook (Smith & Nephew) approximately 2 to 3 mm distal to the edge of tendon tear (Fig 12). Satisfactory visualization of subscapular tendon, predesigned working access, and working space without a bony barrier will offer a smooth repair.
Fig 10.
The subscapularis tendon from tear portion to medial edge of coracoid process can be wonderfully visualized from the MSV portal (A portal). The asterisk indicates the ruptured portion of the tendon. (CP, coracoid process; H, head of the humerus; MSV, modified subacromial viewing; SSC, the subscapularis tendon.)
Fig 11.
The tear portion of subscapularis tendon from tear portion can be well visualized from the MSV portal (A portal). The asterisk indicates the ruptured portion of the tendon. (H, head of the humerus; MSV, modified subacromial viewing; SSC, the subscapularis tendon.)
Fig 12.
The tendon is sewn approximately 2 to 3 mm distal to the edge of tendon tear. (H, head of the humerus; SSC, the subscapularis tendon.)
Reattachment Confirmation
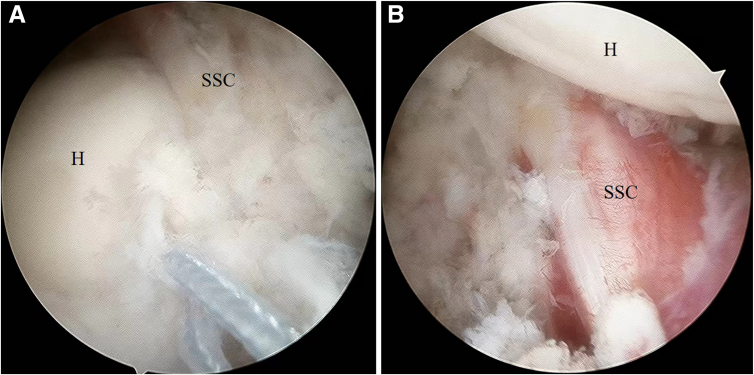
The pattern of tendon fixation depends on the tear extension of the subscapularis tendon; single-row or Mason–Allen fashion is the optional choice. The scope is placed in the joint and the reattached tendon is examined eventually. The subscapularis tendon receives the desired anatomical reattachment in the subacromial space and glenohumeral joint (Fig 13).
Fig 13.
(A) The subscapularis tendon receives the desired anatomical reattachment in the subacromial space. (B) The subscapularis tendon receives the desired anatomical reattachment in the joint. (H, head of the humerus; SSC, the subscapularis tendon.)
Discussion
Missed diagnosis of subscapularis tendon tears during arthroscopy is an intractable problem that needs to be solved urgently. Yoon et al.3 reported 25 concomitant subscapularis tendon tears in 58 patients who underwent revision repair procedure. Piasecki et al.5 described the presence of neglected subscapularis tendon tears in 9 of 54 patients who underwent revision cuff surgery. Lädermann et al.6 emphasized that neglected subscapularis tendon tears were found in more than one half of patients who underwent revision, but whether the tendon tears were neglected in the primary surgery or retears was not described.
The poor visualization of subscapular tendon and footprint of lesser tuberosity is thorny problem in intra-articular repair procedures. The footprint of the partial subscapularis tendon is difficult to visualize during surgery due to the multiple planes of insertion on lesser tuberosity.12 Wright et al.13 described that only 26% of subscapularis tendon could be visualized with a 30° scope. The flexing and internally rotating the arm is helpful for the visualization of hidden subscapularis tendon.14 Removing the medial biceps sling is vital to obtain better visualization of the subscapularis attachment; however, the procedure will result in iatrogenic damage.3,15 The 70° scope is often applied for better visualization of subscapularis tendon tear and bare footprint in the joint.16
Insufficient visualization of subscapularis tendon and footprint is obtained from the conventional subacromial viewing portal with 30° scope. Tears of subscapularis tendon are difficult to visualize in the subacromial space because the lesion initially begins on the articular side of the tendon.1 The scope forms an angle of 10° with subscapularis tendon, resulting in the poor visualization of the tendon. The footprint of lesser tuberosity will also be overlooked due to the obstructed visualization from the medial suspensory ligament; better visualization will be obtained when the medial suspensory ligament is partially removed, but iatrogenic loss is inevitable.
The MSV portal described in the present study is a modified surgical technique for repairing upper-third tendon tears. Since the scope forms an angle of 70° with the subscapularis tendon and footprint of lesser tuberosity, satisfactory visualization of tendon and footprint can be obtained when using a 30° scope; the predesigned surgical portal and working space without bony barrier can offer a smooth surgical procedure. The viewpoints are as follows: First, the angle of 70° between the scope and subscapularis tendon is equivalent of using a 70° scope for the tendon visualization; the tendon from tear portion to medial edge of coracoid process can be well visualized. Satisfactory visualization of the tendon is the prerequisite for smooth work of the instruments such as suture hook. Second, the angle of 70° between the scope and footprint of lesser tuberosity is equivalent to using a 70° scope for the footprint visualization; satisfactory visualization of the bare footprint can be obtained just by pushing the medial suspensory ligament anteriorly and distally instead of removing this site. Satisfactory visualization of the footprint is the prerequisite for precise insertion of suture anchor. Third, compared with the restricted surgical portals in the joint, the predesigned working portals provided by the MSV portal can offer easy suture hook and suture anchor insertion. Fourth, although the challenge of coracoid process blocking the suture hook is inherent in the surgical procedure, this problem can be solved by internal rotation of the arm.
Nevertheless, the arthroscopic MSV portal repair of upper-third tendon tears still has some shortcomings. First, although satisfactory visualization of the subscapularis tendon and footprint of lesser tuberosity can be obtained in the subacromial space, the improved surgical component does not include the visualization of tendon and footprint within the glenohumeral joint. Second, the 2 additional incisions on the shoulder joint are considered iatrogenic injuries. Third, since the deltoid muscle loses the bony support of the acromion, surgical visualization may be impeded by the drooping deltoid fascia, and the sutures will also be hindered when knotting.
Availability of Data and Materials
Data and materials of the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Disclosures
All authors (P.H., X.W., C.H., X.T.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peiguan Huang is the first author.
Supplementary Data
Surgical technique demonstration of upper third of subscapularis tendon partial-thickness tears. The patient is positioned in lateral decubitus position. The diagnosis of subscapularis tendon tear is performed in the joint, the tendon repair procedure is performed in the MSV portal. A portal (MSV portal) is the specific viewing portal for tendon repair procedure, created between coracoid process and anterolateral corner of the acromion. Since the scope forms an angle of 70 degrees with the footprint of lesser tuberosity and tendon, the satisfactory visualization of footprint can be obtained just by pushing the medial suspensory ligament anteriorly and distally, the tendon from tear portion to medial edge of coracoid process can be wonderfully visualized. One 5.0 mm suture anchor is inserted into the footprint, the tendon is sewn with suture hook approximately 2 to 3 mm distal to the edge of tendon tear, single-row is used for tendon fixation. Satisfactory visualization of subscapular tendon, pre-designed working access and working space without bony barrier will offer the smooth work of repair procedure.
References
- 1.Koo S.S., Burkhart S.S. Subscapularis tendon tears: Identifying mid to distal footprint disruptions. Arthroscopy. 2010;26:1130–1134. doi: 10.1016/j.arthro.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 2.Neyton L., Daggett M., Kruse K., Walch G. The hidden lesion of the subscapularis: Arthroscopically revisited. Arthrosc Tech. 2016;5:e877–e881. doi: 10.1016/j.eats.2016.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoon T.H., Kim S.J., Choi Y.R., Cho J.T., Chun Y.M. Arthroscopic revision rotator cuff repair: The role of previously neglected subscapularis tears. Am J Sports Med. 2021;49:3952–3958. doi: 10.1177/03635465211047485. [DOI] [PubMed] [Google Scholar]
- 4.Meshram P., Rhee S.M., Park J.H., Oh J.H. Comparison of functional and radiological outcomes of tears involving the subscapularis: Isolated subscapularis versus combined anterosuperior rotator cuff tears. Orthop J Sports Med. 2020;8 doi: 10.1177/2325967119899355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piasecki D.P., Verma N.N., Nho S.J., et al. Outcomes after arthroscopic revision rotator cuff repair. Am J Sports Med. 2010;38:40–46. doi: 10.1177/0363546509346401. [DOI] [PubMed] [Google Scholar]
- 6.Lädermann A., Denard P.J., Burkhart S.S. Midterm outcome of arthroscopic revision repair of massive and nonmassive rotator cuff tears. Arthroscopy. 2011;27:1620–1627. doi: 10.1016/j.arthro.2011.08.290. [DOI] [PubMed] [Google Scholar]
- 7.Huang J., Cheng J., Tang S., Shi B., Liu G., Xie G. Arthroscopic subscapularis tendon repair using the Mason-Allen technique. Z Orthop Unfall. 2022;160:431–434. doi: 10.1055/a-1387-8079. [DOI] [PubMed] [Google Scholar]
- 8.Lee B., Patel V., Itamura J. Subscapularis tears: Evolution in treatment options. J Am Acad Orthop Surg. 2022;30:485–492. doi: 10.5435/JAAOS-D-21-00155. [DOI] [PubMed] [Google Scholar]
- 9.Denard P.J., Burkhart S.S. Arthroscopic recognition and repair of the torn subscapularis tendon. Arthrosc Tech. 2013;2:e373–e379. doi: 10.1016/j.eats.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee J., Shukla D.R., Sánchez-Sotelo J. Subscapularis tears: Hidden and forgotten no more. JSES Open Access. 2018;2:74–83. doi: 10.1016/j.jses.2017.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hasler A, Ker A, Passon T, Tondelli T, Gerber C, Wieser K. Nonoperatively managed small- to medium-sized subscapularis tendon tears: Magnetic resonance imaging evaluation with a minimum of 5 years of follow-up. JSES Int 202;6:84-90. [DOI] [PMC free article] [PubMed]
- 12.Yoo J.C., Rhee Y.G., Shin S.J., Park Y.B., McGarry M.H., Jun B.J., Lee T.Q. Subscapularis tendon tear classification based on 3-dimensional anatomic footprint: A cadaveric and prospective clinical observational study. Arthroscopy. 2015;31:19–28. doi: 10.1016/j.arthro.2014.08.015. [DOI] [PubMed] [Google Scholar]
- 13.Wright J.M., Heavrin B., Hawkins R.J., Noonan T. Arthroscopic visualization of the subscapularis tendon. Arthroscopy. 2001;17:677–684. doi: 10.1053/jars.2001.25274. [DOI] [PubMed] [Google Scholar]
- 14.Yoon J.S., Kim S.J., Choi Y.R., Kim S.H., Chun Y.M. Arthroscopic repair of the isolated subscapularis full-thickness tear: Single- versus double-row suture-bridge technique. Am J Sports Med. 2019;47:1427–1433. doi: 10.1177/0363546519838281. [DOI] [PubMed] [Google Scholar]
- 15.Kim J.H., Do W.S., Lim J.R., Yoon T.H., Chun Y.M. Subscapularis tendon tears hidden by the medial biceps sling can be missed on arthroscopic examination. Arch Orthop Trauma Surg. 2023;143:3251–3258. doi: 10.1007/s00402-022-04681-1. [DOI] [PubMed] [Google Scholar]
- 16.Bell J.P., Field L.D. Combined intra-articular and extra-articular visualization for repair of a complete subscapularis tear: The "blended view" technique. Arthrosc Tech. 2021;10:e1879–e1882. doi: 10.1016/j.eats.2021.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique demonstration of upper third of subscapularis tendon partial-thickness tears. The patient is positioned in lateral decubitus position. The diagnosis of subscapularis tendon tear is performed in the joint, the tendon repair procedure is performed in the MSV portal. A portal (MSV portal) is the specific viewing portal for tendon repair procedure, created between coracoid process and anterolateral corner of the acromion. Since the scope forms an angle of 70 degrees with the footprint of lesser tuberosity and tendon, the satisfactory visualization of footprint can be obtained just by pushing the medial suspensory ligament anteriorly and distally, the tendon from tear portion to medial edge of coracoid process can be wonderfully visualized. One 5.0 mm suture anchor is inserted into the footprint, the tendon is sewn with suture hook approximately 2 to 3 mm distal to the edge of tendon tear, single-row is used for tendon fixation. Satisfactory visualization of subscapular tendon, pre-designed working access and working space without bony barrier will offer the smooth work of repair procedure.
Data Availability Statement
Data and materials of the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.